
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 04 November 2021
Sec. Cardiovascular Epidemiology and Prevention
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.751910
This article is part of the Research Topic The Biological Impact of Adversity on Cardiovascular Disease Risk and Obesity View all 9 articles
 Xiong Ding1†
Xiong Ding1† Jinfeng Li2†
Jinfeng Li2† Ying Wu1
Ying Wu1 Peng Yang3
Peng Yang3 Dandan Zhao1
Dandan Zhao1 Xiaojie Yuan4
Xiaojie Yuan4 Shuohua Chen2
Shuohua Chen2 Xiaoyan Luo5
Xiaoyan Luo5 Yun Li1*
Yun Li1* Shouling Wu2*
Shouling Wu2*Background: No study has explored the modification effect of ideal cardiovascular health metrics (ICVHMs) on the association between famine exposure and risk of cardiovascular disease (CVD) so far. We aim to examine the effect of ICVHMs on the association between exposure to famine early in life and the risk of CVD in adulthood.
Methods: A total of 61,527 participants free of CVD were included in this study from the Kailuan Study. All participants were divided into three groups, included nonexposed, fetal-exposed, and childhood-exposed groups. Cox regression was used to estimate the effect of famine exposure and ICVHMs on CVD risk.
Results: After a median of 13.0 (12.7–13.2) years follow-up, 4,814 incident CVD cases were identified. Compared with nonexposed participants, the CVD risk increased in participants with fetal famine exposure (hazard ratio [HR]: 1.21; 95% CI: 1.07–1.37), but not in childhood famine-exposed participants. After stratifying by the number of ICVHMs, the increased CVD risk associated with fetal famine exposure was only observed in participants with less ICVHMs ( ≤ 2) (HR: 1.30; 95% CI: 1.11–1.52, P for interaction=0.008), but disappeared in those with three or more ICVHMs. The modified effect of ICVHMs was sex specific (P for sex interaction = 0.031).
Conclusions: Exposing to famine in the fetal period could increase the risk of CVD in late life; however, ICVHMs might modify the effect of famine exposure on CVD risk, especially in men.
Cardiovascular disease (CVD), the most common noncommunicable disease and the leading cause of mortality globally, is an important contributor to the disease burden (1). Reducing the incidence of CVD will be helpful in lowering the burden of this disease and promoting health. Previous studies have demonstrated an association between famine exposure in early life and health effects in adulthood, such as hypertension (2), diabetes mellitus (3), stroke (4, 5), myocardial infarction (MI) (4), and metabolic syndrome (4, 6). The Great Chinese Famine of 1959–1962 was one of the largest famines in human history (7), swiped almost all of the mainland of China. Individuals who were born around the period experienced various severity of famine in early life and were the high-risk populations of CVD. Modifying or reversing the effect of famine exposure on CVD risk might help to reduce the incidence of CVD in these high-risk populations.
Ideal cardiovascular health metrics (ICVHMs) were first proposed in 2010 by the American Heart Association (8), which consisted of seven items, four behavioral metrics (nonsmoking, ideal body mass index [BMI], physical activity at goal levels, and a dietary pattern recommended) and three biological metrics (ideal levels of untreated blood pressure [BP], fasting blood glucose [FBG], and total cholesterol [TC]). Accumulating epidemiological evidence suggested that higher ICVHMs were associated with a lower risk of CVD (9), and all-cause death (10, 11). In 2020, Lu et al. (12) reported that ICVHMs might modify the association between famine exposure in early life and the risk of diabetes mellitus. However, to the best of our knowledge, there have been no studies to explore whether ICVHMs in later life modify the association between famine exposure and risks of CVD in adulthood. We conducted this prospective study in the Kailuan Study, an ongoing cohort enrolled approximately 100,000 participants beginning in 2006, with aims to examine the association between exposure to the Great Chinese Famine in early life and risk of CVD in adults and the modification effect of ICVHMs.
The Kailuan Study (trial registration number ChiCTR-TNC-11001489) is an ongoing longitudinal prospective study conducted in the Kailuan community in Tangshan, Republic of China. A total of 101,510 employees (including the retired, 81,110 men and 20,400 women, mean age = 51.9 y in 2006) of the Kailuan Group were invited and agreed to participate in the Kailuan Study between June 2006 and October 2007 (referred to as the “baseline survey”). Detailed study design and procedures have been described in previous studies (13, 14). All participants completed questionnaire assessments, clinical examinations, and laboratory tests in 11 hospitals responsible for the health care of the Kailuan general hospital. Participants then took physical examination every 2 years, and the incidences of chronic diseases (e.g., stroke, MI, cancer, et al.) were recorded annually. In the current study, data analysis was performed from baseline survey to December 31, 2019.
In the present study, according to previous Chinese famine studies (4, 12), 65,105 participants born between January 1, 1949, and December 31, 1974, were recruited from the Kailuan Study. Participants (n = 1,060) who had a history of MI or stroke at the baseline survey were excluded. Moreover, we excluded participants (n = 2,518) who had incomplete data on health factors or behaviors, leaving 61,527 participants (47,549 men and 13,978 women) available for analyses (Supplementary Figure S1).
We collected information on sociodemographic characteristics (e.g., age, gender, birth date, and education level), lifestyle factors (e.g., smoking, alcohol intake, salt intake, and physical activity), medical history (e.g., CVD, hypertension, diabetes mellitus, family history of CVD), and active treatments such as hypoglycemic, antihypertensive, and lipid-lowering medications through the self-reported questionnaire in the Kailuan Study since the baseline survey, as detailed previously (13). Education was classified as less than high school and high school or above. Drinking status was stratified into two levels: current or never/former. Weight and height were measured, and BMI was calculated as weight (kg)/height (m)2. Moreover, BP was measured on the left arm using an appropriate cuff size after the participant had a rest in a chair for at least 5 min. The average values of at least two readings each of systolic and diastolic BPs were used for further analysis.
The blood sample of each participant was collected on the morning of the survey after at least a 12-h fast. All samples were measured by a Hitachi 747 autoanalyzer at the central laboratory of the Kailuan General Hospital. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration creatinine equation (15).
Because the Chinese Famine occurred from 1959 to 1962, consistent with previous Chinese famine studies (4, 12, 16, 17), birth year was taken as the proxy variable of exposure to famine in this study. We defined those born between January 1, 1959, and December 31, 1962, as fetal exposure group, those born between January 1, 1949, and December 31, 1958, as childhood-exposed group, and those born between January 1, 1963, and December 31, 1974, as a nonexposed group. As a large enterprise group, the employees in the Kailuan group were nationwide. Therefore, the severity of the famine was determined according to the excess death rate for each province, which was calculated as this rate change from the average level in 1956–1958 to the highest value in 1959–1962 (7). Based on the information, an excess mortality rate of 50% was used as a threshold value to define severely and less severely affected areas in the present study.
ICVHMs were adapted from the recommendations of American Heart Association (8): nonsmoking, BMI <24 kg/m2, physical activity at goal (at least 80 min per week of moderate-intensity physical activity), ideal diet (daily salt intake <6 g) (18); TC <5.2 mmol/L (untreated), BP <120/80 mmHg (untreated), FBG <5.6 mmol/L (untreated). Cardiovascular health status was then categorized as high (5–7 metrics), moderate (3–4 metrics), or low (0–2 metrics) levels (19).
The main outcome of this study was the first occurrence of CVD events, including MI, severe coronary artery disease, intracerebral hemorrhagic stroke, and ischemic stroke. CVD events were defined as described (20, 21). Briefly, the Municipal Social Insurance Institution database and Hospital Discharge Register were linked to identify the incidence of CVD based on The International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) (I61 for intracerebral hemorrhagic stroke, I63 for ischemic stroke, and I21 for MI, I25.1 for coronary heart disease). These two databases covered all the Kailuan Study participants. For all suspected CVD cases, a panel of three experienced physicians, consisting of neurologists, cardiologists, and radiologists, reviewed the medical records, blind to exposure status. We defined coronary artery disease and MI cases according to the Multinational Monitoring of Trends and Determinants in CVD criteria of WHO on basis of clinical symptoms and dynamic changes in cardiac enzymes and/or biomarker concentrations and electrocardiogram results. Severe coronary artery disease was defined as coronary heart disease treated with coronary bypass surgery or stent placement. Incident stroke was diagnosed according to the WHO criteria, based on symptoms, neuroimages (from CT or MRI), and other diagnostic reports. Mortality data were collected from provincial vital statistics offices, as described previously (14).
All analyses were performed using SAS, version 9.4 (SAS Institute, Inc, Cary, NC). Two-sided values of P < 0.05 were regarded as significant.
The baseline characteristics of the study population were described by famine exposure status. Continuous variables with normal distribution were expressed as means ± SDs and compared using one-way ANOVA analysis, while those with skewed distribution were expressed as medians and interquartile range and compared by Kruskal-Wallis test. Categorical variables were shown in proportions and compared by Pearson's Chi-Square test.
We computed the person-year of follow-up for each participant from the date of the baseline survey to the date of the CVD onset, death, loss to follow-up (n=2,156, 3.5%), or the end of follow-up (December 31, 2019), whichever came first. The Cox regression model was used to predict the risk of CVD and to estimate the hazard ratio (HR) and 95% CI, after adjustments for age, sex, education attainment (less than high school, high school, or above), drinking (current, never/former), eGFR (<30, 30 ≤ eGFR <60, or ≥ 60 mL/min/1.73 m2), and high-sensitivity C-reactive protein (Hs-CRP) (<1.0, 1.0 ≤ Hs-CRP ≤ 3.0, or > 3.0 mg/L), triglycerides (TG) (<1.7, 1.7 ≤ TG <2.3, or ≥ 2.3 mmol/L), severity famine exposed, family history of CVD, using of antihypertensive, hypoglycemic, lipid-lowering medications (yes/no for each), and individual ICVHMs. Cochran-Armitage trend test was used to investigate the association between the increasing number of ICVHMs and the cumulative incidence of CVD. Missing covariates (drinking, eGFR, Hs-CRP, TG) will be imputed by means of multiple imputations using the Fully Conditional Specification method computing 10 imputed datasets and to prevent case-wise deletion of missing data; 60,874 (98.9%) participants had complete data for all covariates.
To explore the modifying effect of ICVHMs, we evaluated the association between famine exposure and CVD by strata of the individual ICVHMs items and the number of ICVHMs. Other ICVHMs items were adjusted when evaluating individual ICVHMs items. P-value was corrected for multiple testing via false discovery rate using the Benjamini-Hochberg method. To demonstrate potential interactions of famine exposure and ICVHMs on the development of CVD, we generated interaction terms using the cross products of famine exposure and ICVHMs in Cox regression models. To address specific questions on age differences between famine and postfamine births, an “age-balanced” method was used, in which both prefamine and postfamine births were combined as unexposed control subjects, as detailed previously (12, 22).
We further conducted several sensitivity analyses. To assess the impact of imputing missing covariates, we repeated the main analyses in those without imputation. To test the robustness of our finding, we repeated the main analyses excluding those with antihypertensive, hypoglycemic, or lipid-lowering medications treatment, excluding those lost to follow-up, and excluding those who had CVD events or death within the first 2 years of follow-up.
A total of 61,527 participants (mean age 47.9 ± 6.6 y) were recruited in the present analyses, including 47,549 (77.3%) men and 13,978 (22.7%) women. There were 13.9% (n = 8,572), who were exposed to the Great Chinese Famine in the fetal stage. Compared with the nonexposed group (born between January 1, 1963, and December 31, 1974), participants with fetal famine exposure were more likely to be with a family history of CVD, or use antihypertensives or hypoglycemics, had higher BMI, TC, TG, systolic or diastolic BPs, FBG level, Hs-CRP level, had a greater proportion of individuals with ideal physical activity, as well as lower eGFR, education level, less proportion of individuals with other six individual ideal items, and less drinkers (Table 1). Supplementary Table S1 showed baseline information for the age-balanced group with combining of prefamine and postfamine births as the reference group.
During a median of 13.0 (12.7–13.2) years follow-up, 4,814 incident CVD events were identified. Age of CVD onset was 49.5±4.3, 54.2±3.8, 60.8±4.4 for the nonexposed, fetal-exposed, or childhood-exposed group, respectively (Supplementary Table S2). As shown in Table 2, both the incidences of CVD for fetal famine-exposed (5.95/1000 pys) or childhood famine-exposed (8.31/1000 pys) group were greater than that for the nonexposed group (3.10/1000 pys). After adjusting for covariates, the increased CVD risk remained significant in fetal famine-exposed participants (HR: 1.21; 95% CI: 1.07–1.37), but not in childhood famine-exposed participants (HR: 1.00; 95% CI: 0.85–1.17). Furthermore, in the sex stratified analysis (Table 2) and age-balanced analysis (Supplementary Table S3), the results were similar.
The incidence of CVD according to famine exposure and the number of ICVHMs were displayed in Figure 1. There was a reverse correlation between the number of ICVHMs and the incidence of CVD. With the increasing number of ICVHMs, the cumulative incidence of CVD decreased gradually for participants in nonexposed or fetal-exposed groups (all P for trend < 0.001).
After stratifying participants by the number of ICVHMs, we found that in participants with less ICVHMs ( ≤ 2), fetal famine exposure significantly increased the CVD risk after adjusting for all covariates (HR: 1.30; 95% CI: 1.11–1.52, P for interaction=0.008), comparing with a nonexposed group (Table 3). However, we do not observe the association in participants with three or more ICVHMs (HR: 1.14; 95% CI: 0.92–1.40, HR: 0.89; CI: 0.37–2.11). In sensitivity analyses, consistent results were observed without imputing covariates, excluding participants using antihypertensive, hypoglycemic, or lipid-lowering medications, participants lost to follow-up, and who had events or death within 2 years of follow-up (Table 3). Similar results were observed in the age-balanced analysis (Supplementary Table S4).
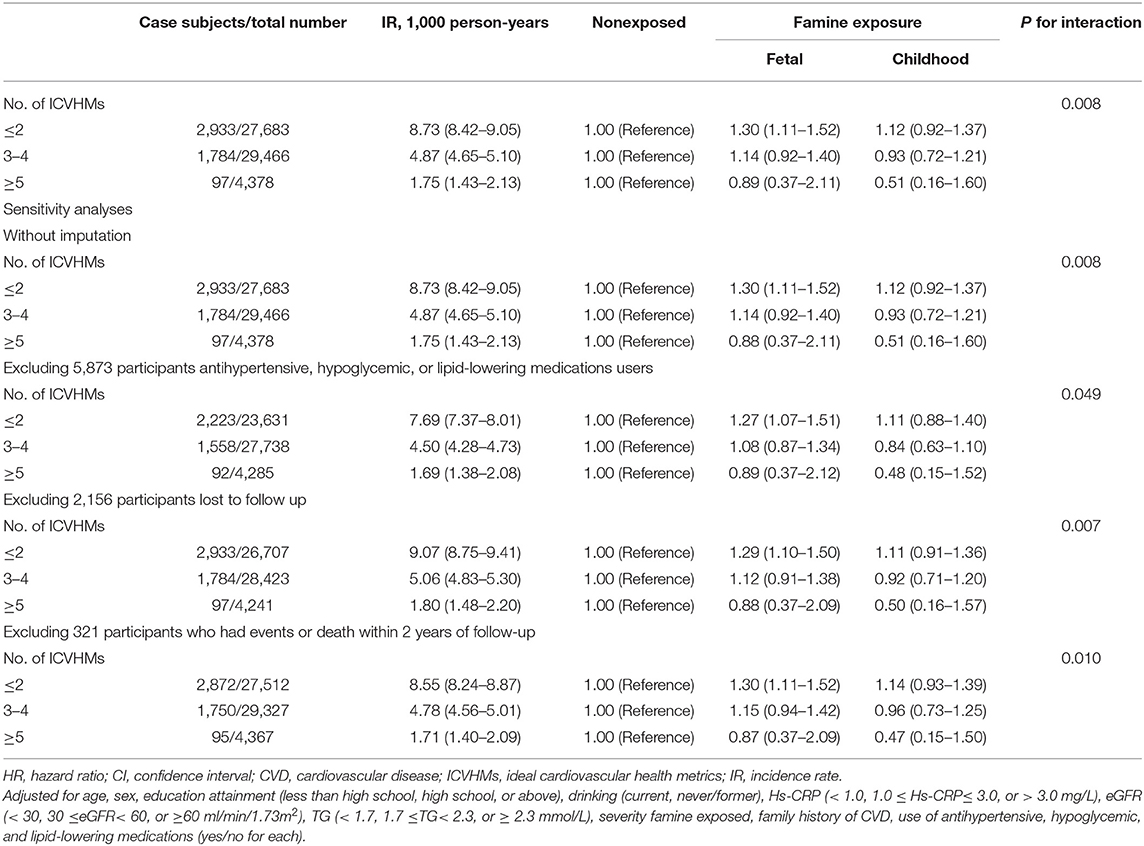
Table 3. Multivariable adjusted HR (95% CI) for incident CVD according to famine exposure and combined ICVHMs.
The sex difference was further explored in stratified analysis. Due to the small sample size of participants with ≥5 ICVHMs items in men or women, we combined and divided men or women into two groups according to the number of ICVHMs: participants with less ICVHMs ( ≤ 2) items or more ICVHMs (≥3) items. Similar results were observed in men, that the association between fetal famine exposure and CVD risk was significant in men with less ICVHMs (HR: 1.26, 95% CI: 1.07–1.49) rather than those with three or more ICVHMs (HR: 1.05, 95% CI: 0.84–1.31). However, results were inverse in women, that the association between fetal famine exposure and CVD risk was significant in women with three or more ICVHMs (HR: 1.65, 95% CI: 1.01–2.69) rather than those with less ICVHMs (HR: 1.58, 95% CI: 0.92–2.70). The interaction between sex and famine exposure was significant (P = 0.031) (Table 4).
We further analyzed the association between famine exposure and CVD risk according to individual ICVHMs items. The associations between famine exposure and CVD risk were observed in participants with nonideal ICVHMs items, except for TC (in ideal TC) and smoking items (in both ideal and nonideal) (Table 5). Multiple testing via false discovery rate analyses showed similar results (Supplementary Table S5). In age-balanced analysis, the risk estimates did not change dramatically (Supplementary Table S6).
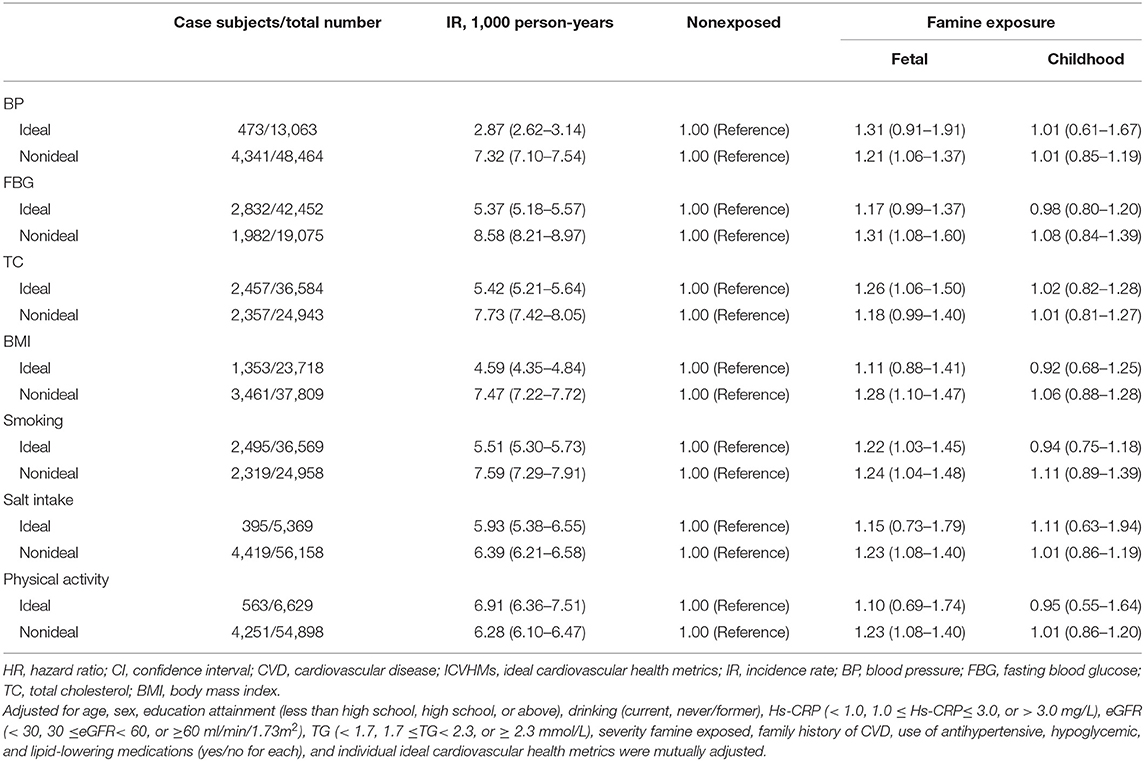
Table 5. Multivariable adjusted HR (95% CI) for incident CVD according to famine exposure and individual ICVHMs items.
In this large community-based prospective study, we observed that fetal exposure to the Great Chinese Famine was associated with an increased risk of CVD in adults. More importantly, ICVHMs may modify the association between fetal exposure to famine and the risk of CVD in adults. The effect of fetal exposure to famine on the CVD risk only occurred in participants with less ICVHMs items but not in those with more ICVHMs items. The results not only emphasized the importance of adequate nutrition in early life but also suggested a healthy lifestyle in late life. The results are of great significance for that experienced famine or malnutrition in early life to reduce the risk of CVD.
Previous epidemiological studies have reported conflicting results regarding the association between famine exposure and CVD (23–25). In a median 10.1 years follow-up of 92,284 participants, in urban areas, compared with nonexposed births, famine births had a higher risk of cerebrovascular disease (HR 1.18; 95% CI: 1.09–1.28) (23). Similarly, in the present study, our results supported the association between famine exposure in early life and CVD risk. However, two studies (24, 25) from the Dutch Famine Birth Cohort have reported that prenatal exposure to the Dutch famine of 1944–1945 was not associated with the subsequent risk of stroke or coronary artery disease in middle-aged adults. Both these two studies were limited with a relatively small sample (~3,000 participants), which might contribute to the different results. In addition, compared with the Dutch famine (~6 months), the Chinese Great Famine lasted longer (~4 years) and had greater severity, affected 600 million population and led to some 30 million premature deaths (7, 26).
There were studies that demonstrated the preventive effect of ICVHMs on CVD risk (19, 27). However, limited researches addressed the modified effect of ICVHMs on the association between famine exposure and CVD risk. In the current study, we examined the effect of ICVHMs on the association between famine exposure in early life and the risk of CVD in a prospective study. We, interestingly, found that the association between famine exposure and CVD risk only showed in participants with less ICVHMs items ( ≤ 2), not in those with ≥3 ICVHMs items, which suggested that the increased risk of CVD owing to famine exposure in early life might be modified by ICVHMs. Individual ICVHMs items also supported the modified effects. There are few studies exploring the modified effect of ICVHMs on the influence of famine exposure. Meng et al. (23) examined physical activity level, one of the ICVHMs items, in 92,284 participants born between 1954 and 1964, and concluded that the increased risk of CVD affected by prenatal famine exposure was only shown in participants with lower physical activity levels, but not in higher ones. Ding et al. (28) demonstrated that a healthy lifestyle, such as adequate physical activity, may partially alleviate the adverse effects of increasing TC in participants with prenatal or early postnatal exposure to famine. Lu et al. (12)reported that ICVHMs might modify the association between famine exposure in early life and the risk of diabetes mellitus.
There are several potential mechanisms by which ICVHMs modify the association between famine exposure in early life and the risk of CVD in adulthood. Stein et al. (29, 30) found that maternal exposure during pregnancy to famine was associated with higher BP, the major risk factor of CVD, in later life. A healthy lifestyle such as moderate physical exercise and a low-salt diet may lower BP (31), and eventually reduced the risk of CVD (32). Fetal exposure to famine was associated with hyperglycemia and diabetes mellitus (3) in adulthood, which could be attenuated by ≥3 ICVHMs (12), and then might reduce the CVD risk. As is well known, higher pulse wave velocity was a risk factor for CVD. The number of ICVHMs items was inversely associated with pulse wave velocity, every one-point increase corresponded to a 0.09-m/s decrease in pulse wave velocity (33), which might be one potential mechanism for our results. Finally, the ICVHMs attained in mid- to late-life could improve the cardiovascular structure and function of blood vessels in late life (34), and subsequently reduce the incidence of CVD.
Sex differences of the associations between early life famine exposure and metabolic diseases were often reported. Similarly, we also observed a sex difference results in the present study. In men, not in women, more ICVHMs items (≥3) might mitigate the effect of fetal famine exposure on the CVD risk (P for interaction = 0.031). Evidence showed that male usually was more susceptible to adverse environmental conditions, and female may be more adaptable to famine (35). Therefore, healthy cardiovascular health has a greater effect on male. In addition, due to the traditional Chinese male-sex-preference culture (36), female may suffer from severer famine and have a lower chance to survive than male after birth. But the female survivors might be healthier, and hence be less affected by the environmental conditions, included ICVHMs. Moreover, lots of studies have confirmed the cardiovascular protective effect of estrogen, which might play a stronger effect on cardiovascular health than ICVHMs in female. All these might contribute to the less protective effect of ICVHMs in female.
The strengths of the current study include a prospective cohort design with a large sample size, detailed information about lifestyle factors, and long follow-up time. The diagnosis of CVD was not self-reported but linked to the Municipal Social Insurance Institution database and Hospital Discharge Register for incidence of CVD. However, there were several limitations to our study. First, misclassification of famine exposure may exist, which might underestimate the effects of famine exposure. However, using the birth date of an individual to define famine exposure was the most common method in studies on the Great Chinese Famine (12, 17). Second, the ideal diet calculated by the AHA Diet Score should be calculated on the basis of consumption of whole grains, fruits, vegetables, fish, sodium, sweets, and sugary beverages. Although no detailed dietary composition data were collected in this study, our previous work found a strong association between higher salt intake and lower healthy eating scores. So, we use daily salt intake as a surrogate indicator of diet quality (37). Third, most of the participants were men (77.3%) in the current study; therefore, the observed results may not be generalizable to other populations. However, similar associations between the exposure to famine in early life and risks of CVD have been shown in other nationwide prospective cohort studies, suggesting the broad generalizable nature of the data (4, 23). Finally, although we used age-balanced analysis, limitations might still exist through combining the age group. Famine exposure has been shown to be associated with adult mortality; thus, survival bias might be possible.
In conclusion, we found that fetal exposure to the Great Chinese Famine significantly increased the risk of CVD in adulthood. However, ICVHMs might modify the effect of famine exposure on CVD risk.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by Ethics Committee of the Kailuan General Hospital. The patients/participants provided their written informed consent to participate in this study.
XD, JL, YW, PY, DZ, XY, SC, XL, YL, and SW: writing—original draft. XD, JL, YW, PY, DZ, SC, and XL: investigation. XD, YW, XY, YL, and SW: writing—review and editing. XD, JL, XY, and SW: methodology. SC, XL, YL, and SW: project administration and funding. All authors contributed to the article and approved the submitted version.
This study was supported by the Natural Science Foundation of Hebei Province (H2021209018) and Tangshan Science and Technology Innovation Team Program (20130206D).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors thank the investigators who made this cohort study possible.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.751910/full#supplementary-material
1. Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P. M, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. The Lancet. (2020) 395:795–808. doi: 10.1016/S0140-6736(19)32008-2
2. Xin X, Yao J, Yang F, Zhang D. Famine exposure during early life and risk of hypertension in adulthood: A meta-analysis. Crit Rev Food Sci Nutr. (2018) 58:2306–13. doi: 10.1080/10408398.2017.1322551
3. Meng R, Lv J, Yu C, Guo Y, Bian Z, Yang L. Y, et al. Prenatal famine exposure, adulthood obesity patterns and risk of type 2 diabetes. Int J Epidemiol. (2018) 47:399–408. doi: 10.1093/ije/dyx228
4. Du R, Zheng R, Xu Y, Zhu Y, Yu X., Li M, et al. Early-life famine exposure and risk of cardiovascular diseases in later life: findings from the REACTION study. J Am Heart Assoc. (2020) 9:e014175. doi: 10.1161/JAHA.119.014175
5. Liu D, Yu DM, Zhao LY, Fang HY, Zhang J, Wang JZ, et al. Exposure to famine during early life and abdominal obesity in adulthood: findings from the great Chinese famine during 1959–1961. Nutrients. (2019) 11:903. doi: 10.3390/nu11040903
6. Wang N, Wang X, Li Q, Han B, Chen Y, Zhu C, et al. The famine exposure in early life and metabolic syndrome in adulthood. Clin Nutr. (2017) 36:253–9. doi: 10.1016/j.clnu.2015.11.010
7. Luo Z, Mu R, Zhang X. Famine and Overweight in China*. Review of Agricultural Economics. (2006) 28:296–304. doi: 10.1111/j.1467-9353.2006.00290.x
8. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L.K, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. (2010) 121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703
9. Ying Y, Lin S, Kong F, Li Y, Xu S, Liang X, et al. Ideal Cardiovascular health metrics and incidence of ischemic stroke among hypertensive patients: a prospective cohort study. Front Cardiovasc Med. (2020) 7:590809. doi: 10.3389/fcvm.2020.590809
10. Corlin L, Short MI, Vasan RS, Xanthakis V. Association of the duration of ideal cardiovascular health through adulthood with cardiometabolic outcomes and mortality in the framingham offspring study. JAMA Cardiol. (2020) 5:549–56. doi: 10.1001/jamacardio.2020.0109
11. N MI, Kunutsor SK, Voutilainen A, Kurl S, Kauhanen J, J AL. Association between ideal cardiovascular health and risk of sudden cardiac death and all-cause mortality among middle-aged men in Finland. Eur J Prev Cardiol. (2020) 28:294–300. doi: 10.1177/2047487320915338
12. Lu J, Li M, Xu Y, Bi Y, Qin Y, Li Q, et al. Early life famine exposure, ideal cardiovascular health metrics, and risk of incident diabetes: findings from the 4C study diabetes care. (2020) 43:1902–9. doi: 10.2337/figshare.12185469
13. Li Y, Li Y, Gurol ME, Liu Y, Yang P, Shi J. In utero exposure to the Great Chinese Famine and risk of intracerebral hemorrhage in midlife. Neurology. (2020) 94:e1996–2004. doi: 10.1212/WNL.0000000000009407
14. Wu S, An S, Li W, Lichtenstein AH, Gao J, Kris-Etherton PM, et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw Open. (2019) 2:e194758. doi: 10.1001/jamanetworkopen.2019.4758
15. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. (2009) 150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006
16. Wang N, Wang X, Han B, Li Q, Chen Y, Zhu C, et al. Is exposure to famine in childhood and economic development in adulthood associated with diabetes? J Clin Endocrinol Metab. (2015) 100:4514–23. doi: 10.1210/jc.2015-2750
17. Wang N, Cheng J, Han B, Li Q, Chen Y, Xia FB, et al. Exposure to severe famine in the prenatal or postnatal period and the development of diabetes in adulthood: an observational study. Diabetologia. (2017) 60:262–9. doi: 10.1007/s00125-016-4148-4
18. Li Y, Huang Z, Jin C, Xing A, Liu Y, Huangfu C, et al. Longitudinal change of perceived salt intake and stroke risk in a Chinese population. Stroke. (2018) 49:1332–9. doi: 10.1161/STROKEAHA.117.020277
19. van Sloten TT, Tafflet M, Périer MC, Dugravot A, Climie RED, Singh-Manoux A, Empana JP. Association of change in cardiovascular risk factors with incident cardiovascular events. JAMA. (2018) 320:1793–804. doi: 10.1001/jama.2018.16975
20. Jin C, Chen S, Vaidya A, Wu Y, Wu Z, Hu FB, et al. Longitudinal change in fasting blood glucose and myocardial infarction risk in a population without diabetes. Diabetes Care. (2017) 40:1565–72. doi: 10.2337/dc17-0610
21. Ma C, Pavlova M, Liu Y, Liu Y, Huangfu C, Wu S, et al. Probable REM sleep behavior disorder and risk of stroke: A prospective study. Neurology. (2017) 88:1849–55. doi: 10.1212/WNL.0000000000003902
22. Li C, Tobi EW, Heijmans BT, Lumey LH. The effect of the Chinese Famine on type 2 diabetes mellitus epidemics. Nat Rev Endocrinol. (2019) 15:313–4. doi: 10.1038/s41574-019-0195-5
23. Meng R, Yu C, Guo Y, Bian Z, Si J, Nie J, et al. Early famine exposure and adult disease risk based on a 10-year prospective study of Chinese adults. Heart. (2020) 106:213–20. doi: 10.1136/heartjnl-2019-315750
24. Horenblas J, de Rooij SR, Roseboom TJ. The risk of stroke after prenatal exposure to famine. J Dev Orig Health Dis. (2017). 8:658–64. doi: 10.1017/S2040174417000472
25. Painter RC, de Rooij SR, Bossuyt PM, Simmers TA, Osmond C, Barker DJ, et al. Early onset of coronary artery disease after prenatal exposure to the Dutch famine. Am J Clin Nutr. (2006) 84:322–7. doi: 10.1093/ajcn/84.2.322
26. Cai Y, Feng W. Famine, social disruption, and involuntary fetal loss: evidence from Chinese survey data. Demography. (2005) 42:301–22. doi: 10.1353/dem.2005.0010
27. Ahmed A, Pinto Pereira SM, Lennon L, Papacosta O, Whincup P, Wannamethee G. Cardiovascular health and stroke in older British Men: prospective findings from the british regional heart study. Stroke. (2020) 51:3286–94. doi: 10.1161/STROKEAHA.120.030546
28. Ding XY, Yang ZY, Zhao LY, Zhao WH. Are lipid profiles in middle age associated with famine exposure during prenatal and early postnatal period? Nutrients. (2020) 12. doi: 10.3390/nu12082266
29. Stein AD, Zybert PA, van der Pal-de Bruin K, Lumey LH, Exposure to famine during gestation size at birth and blood pressure at age 59 y: evidence from the Dutch Famine. Eur J Epidemiol. (2006) 21:759–65. doi: 10.1007/s10654-006-9065-2
30. Li Y, Jaddoe VW, Qi L, He Y, Lai J, Wang J, et al. Exposure to the Chinese famine in early life and the risk of hypertension in adulthood. J Hypertens. (2011) 29:1085–92. doi: 10.1097/HJH.0b013e328345d969
31. Huang L, Trieu K, Yoshimura S, Neal B, Woodward M, Campbell NRC, et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: systematic review and meta-analysis of randomised trials. BMJ. (2020) 368:m315. doi: 10.1136/bmj.m315
32. Yano Y, Reis JP, Colangelo LA, Shimbo D, Viera AJ, Allen NB, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association Blood Pressure Guideline With Cardiovascular Events Later in Life. JAMA. (2018) 320:1774–82. doi: 10.1001/jama.2018.13551
33. Aatola H, Hutri-Kähönen N, Juonala M, Laitinen TT, Pahkala K., Mikkilä VR, et al. Prospective relationship of change in ideal cardiovascular health status and arterial stiffness: the Cardiovascular Risk in Young Finns Study. J Am Heart Assoc. (2014) 3:e000532. doi: 10.1161/JAHA.113.000532
34. Shah AM, Claggett B, Folsom AR, Lutsey PL, Ballantyne CM, Heiss G, et al. Ideal cardiovascular health during adult life and cardiovascular structure and function among the elderly. Circulation. (2015) 132:1979–89. doi: 10.1161/CIRCULATIONAHA.115.017882
35. Song S. Does famine influence sex ratio at birth? Evidence from the 1959–1961 Great Leap Forward Famine in China. Proc Biol Sci. (2012) 279:2883–90. doi: 10.1098/rspb.2012.0320
36. Mu R, Zhang X. Why does the great Chinese Famine affect the male and female survivors differently? Mortality selection versus son preference. Econ Hum Biol. (2011) 9:92–105. doi: 10.1016/j.ehb.2010.07.003
37. Shen L, Li C, Wang Z, Zhang R, Shen Y, Miles T, et al. Early-life exposure to severe famine is associated with higher methylation level in the IGF2 gene and higher total cholesterol in late adulthood: the Genomic Research of the Chinese Famine (GRECF) study. Clin Epigenetics. (2019) 11:88. doi: 10.1186/s13148-019-0676-3
Keywords: fetal, ideal cardiovascular health metrics, China famine, cardiovascular disease, cohort study
Citation: Ding X, Li J, Wu Y, Yang P, Zhao D, Yuan X, Chen S, Luo X, Li Y and Wu S (2021) Ideal Cardiovascular Health Metrics Modify the Association Between Exposure to Chinese Famine in Fetal and Cardiovascular Disease: A Prospective Cohort Study. Front. Cardiovasc. Med. 8:751910. doi: 10.3389/fcvm.2021.751910
Received: 02 August 2021; Accepted: 27 September 2021;
Published: 04 November 2021.
Edited by:
Alika Maunakea, University of Hawaii, United StatesReviewed by:
Zhenghe Wang, Southern Medical University, ChinaCopyright © 2021 Ding, Li, Wu, Yang, Zhao, Yuan, Chen, Luo, Li and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yun Li, bGl5dW44MDIyQDE2My5jb20=; Shouling Wu, ZHJ3dXNsQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.