- 1Department of Epidemiology/Shandong Provincial Clinical Research Center for Emergency and Critical Care Medicine, School of Public Health/Qilu Hospital, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2Department of Toxicology and Nutrition, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 3Menzies Institute for Medical Research, University of Tasmania, Hobart, TAS, Australia
- 4Research Centre of Applied and Preventive Cardiovascular Medicine, University of Turku, Turku, Finland
- 5Centre for Population Health Research, University of Turku and Turku University Hospital, Turku, Finland
Several prospective cohort studies have assessed the association between multimorbidity and all-cause mortality, but the findings have been inconsistent. In addition, limited studies have assessed the association between multimorbidity and cause-specific mortality. In this study, we used the population based cohort study of National Health Interview Survey (1997–2014) with linkage to the National Death Index records to 31 December 2015 to examine the trends in prevalence of multimorbidity from 1997 to 2014, and its association with the risk of all-cause and cause-specific mortality in the U.S. population. A total of 372,566 adults aged 30–84 years were included in this study. From 1997 to 2014, the age-standardized prevalence of specific chronic condition and multimorbidity increased significantly (P < 0.0001). During a median follow-up of 9.0 years, 50,309 of 372,566 participants died from all causes, of which 11,132 (22.1%) died from CVD and 13,170 (26.2%) died from cancer. Compared with participants without the above-mentioned chronic conditions, those with 1, 2, 3, and ≥4 of chronic conditions had 1.41 (1.37–1.45), 1.94 (1.88–2.00), 2.64 (2.54–2.75), and 3.68 (3.46–3.91) higher risk of all-cause mortality after adjustment for important covariates. Similarly, a higher risk of CVD-specific and cancer-specific mortality was observed as the number of chronic conditions increased, with the observed risk stronger for CVD-mortality compared with cancer-specific mortality. Given the prevalence of multimorbidity tended to increase from 1997 to 2014, our data suggest effective prevention and intervention programs are necessary to limit the increased mortality risk associated with multimorbidity.
Introduction
As the global population ages, multimorbidity (e.g., two or more chronic conditions of hypertension, heart disease, stroke, diabetes, or cancer) are becoming more prevalent (1–3). Multimorbidity, which was associated with poor quality of life and reduced life expectancy (4–6), could challenge existing health care systems with unknown drug interaction and treatment burden (7).
There has been recent attention on the trends in prevalence of multimorbidity that has occurred over time. Data from the National Health Interview Survey (NHIS) found that the prevalence of multimorbidity increased from 21.8 to 26.0% among U.S. adults aged 18 years or older from 2001 to 2010 (2). Moreover, data from general practice (2004–2011) and health surveys (2001–2011) of the Netherlands have also shown a significant increased trend in the prevalence of multimorbidity among adults aged 25 years or older (from 12.7 to 16.2%, and 14.3 to 17.5%, respectively) (3). As those with multimorbidity contribute to significantly higher health care utilization and costs (8), these findings, suggesting an increasing trend in the prevalence in middle-aged and older people, underscore the urgency for effective prevention and control of multimorbidity in the general population.
Although research has shown that the existence of any of these chronic conditions can increase the risk of mortality (9–11), evidence is limited on the risk of mortality for those who have multimorbidity. Where data do exist, the findings have been inconsistent (4, 6, 12, 13). For example, while several studies have shown multimorbidity to be associated with increased risk of all-cause mortality (4, 6, 12), others have shown no association (13, 14). Moreover, limited studies have examined its association with cause-specific mortality (12).
Therefore, using data representative of U.S. adults from the NHIS (1997–2014), we aimed to examine trends in prevalence of multimorbidity from 1997 to 2014 and its association with all-cause, CVD-specific, and cancer-specific mortality until December 31, 2015.
Methods
Study Design and Participants
Since 1957, the NHIS has been administered by the National Center for Health Statistics to collect information on the health and lifestyle behaviors of the civilian, non-institutionalized, U.S. population using personal household interviews. Following an area probability method, a stratified and multistage sampling design was used to select a representative sample of U.S. population annually. Due to a major revision of the questionnaire in 1997, the NHIS data in this study were restricted to the participants recruited from 1997. More detailed information on the NHIS is available online (https://www.cdc.gov/nchs/nhis/index.htm). The de-identified and public NHIS data without including any protected health information are exempt from the ethical board review of Shandong University.
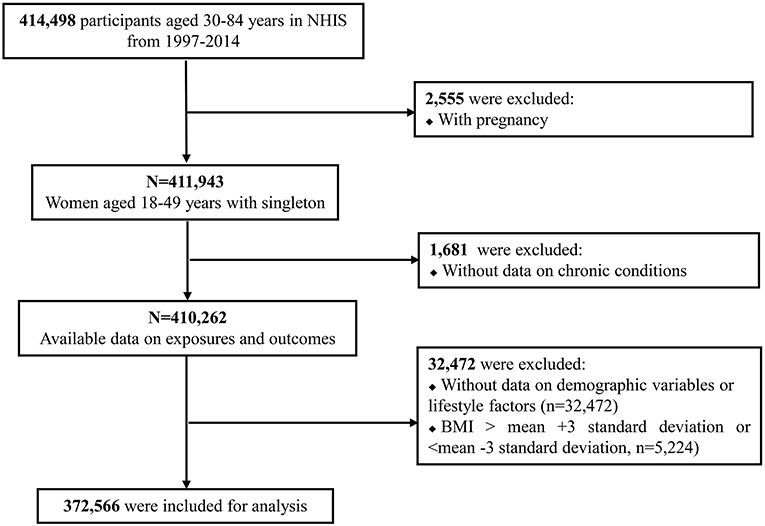
A total of 414,498 participants aged 30–84 years were initially identified from 18 cross-sectional household interview surveys (1997–2014). Among them, 36,708 were excluded because of pregnant women (n = 2,555), missing data on chronic conditions (n = 1,681), missing data on potentially important covariates (i.e., demographic variables and lifestyle factors, n = 32,472), and outliers of BMI (> mean + 3 standard deviation or < mean −3 standard deviation, n = 5,224), resulting in a final analytic sample of 372,566 participants. The included annual sample size ranged from 24,868 in 1997 to 25,704 in 2014. A flowchart of inclusion/exclusion of study participants is presented in Figure 1.
Study Exposure: Chronic Conditions
The information on the chronic conditions in NHIS questionnaires was self-reported by study participants: “Have you ever been told by a doctor or other health professional that you had hypertension/heart disease (including coronary heart disease, angina, myocardial infarction, or other heart disease)/stroke/diabetes/cancer?” The number of these chronic conditions was categorized into 5 subgroups: 0 (reference group), 1, 2, 3, and ≥4.
Study Outcome: Mortality
In this study, all-cause, CVD-specific, and cancer-specific mortality was determined by mortality records in the National Death Index to December 31, 2015. The accuracy of information on all-cause and cause-specific deaths has been validated previously (15). The International Classification of Disease-10th Revision codes were used to identify clinical outcomes including all-cause mortality, CVD-specific mortality (codes I00-I09, I11, I13, and I20-I51, I60-I69) and cancer-specific mortality (codes C00-C97).
Study Covariates
Several demographic and lifestyle variables were included as potentially important covariates in this study. Demographic variables included sex, age, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and others), education (<high school, high school, and >high school), and marital status (married, divorced/separated/widowed, and never married). Lifestyle variables included body mass index (BMI [kg/m2], calculated as self-reported weight divided by the square of height), smoking status, alcohol intake, and physical activity (PA). BMI status was categorized as underweight (<18.5 kg/m2), normal weight (18.5− <25 kg/m2), overweight (25− <30 kg/m2), and obesity (≥30 kg/m2). Smoking status was identified as never, former, and current according to self-reported answers to the following two questions: (1) Have you smoked at least 100 cigarettes in your ENTIRE LIFE? and (2) Do you NOW still smoke cigarettes? Alcohol intake was divided into lifetime abstainer, former drinker, current light-to-moderate, and heavy drinker, according to the self-reported frequency (days per week, month, or year) and quantity (drinks per day) of alcohol intake. The frequency (times per week) and duration (minutes/time) of leisure time PA (vigorous and light- to-moderate intensity) for at least 10 min at a time was self-reported. Based on the recommendation of the 2018 Physical Activity Guidelines for Americans that at least vigorous PA for 75 min/week or moderate PA for 150 min/week or equivalent combination of both, participants were categorized as meeting the recommended PA guidelines or as being physical inactive (16).
Statistical Analyses
Baseline characteristics of categorical variables across the 5 categories of chronic conditions (0 [reference group], 1, 2, 3, and ≥4) were presented as percentages and differences between groups were examined using χ2 analysis Continuous variables including age and BMI were presented as mean ± standard deviation, minimum, and maximum, and the differences between groups were examined using variance analysis. We calculated the crude and age-standardized prevalence of specific chronic condition and multimorbidity to examine the trends of these prevalence estimates over time from 1997 to 2014. The age-standardized prevalence was estimated using the age distribution of the U.S. population in 2010 (17). In total, 47% of adults were aged 30–49 years, 40% were aged 50–69 years, and 13% were aged 70–84 years, and correspondingly, weights of 0.47, 0.40, and 0.13 were used to calculate age-standardization prevalence estimates in each survey (1997–2014). Multivariable logistic regression models were used to estimate the corresponding P values to examine the trends in the prevalence of specific chronic condition and multimorbidity over time, with adjustment for sex, age, race/ethnicity, education, marital status, BMI, smoking status, alcohol intake, and PA. Subgroup analyses were performed by age, sex, and ethnicity/race. Given that subgroup analyses created a multiple testing problem, Bonferroni method was used to correct P values and P < 0.0006 (0.05/81) was considered statistically significant.
After the test of proportional hazards assumption (meeting the assumption) using Kaplan-Meier survival curves for each outcome, Cox proportional hazards regression models were used to estimate the hazard ratios (HRs) with 95% confidence intervals (CIs) of the association between multimorbidity and all-cause, CVD-specific, and cancer-specific mortality among U.S. adults with no chronic condition as the reference. Considering the effect of potential confounding variables on the association, three models were conducted consecutively, including: Model 1: adjusted for sex, age, and race/ethnicity; Model 2: variables in Model 1 plus education and marital status; and Model 3: variables in Model 2 plus BMI, smoking status, alcohol intake, and PA. Based on the index of AIC values, we compared the three models for each outcome and selected Model 3 as the best suited model. Subgroup analyses were conducted stratified by age, sex, race/ethnicity, education, marital status, weight status, smoking, alcohol intake, and PA. In addition, we performed the analysis by excluding participants with cancer at baseline to assess the association between cardiometabolic morbidities and mortality. To test the robustness of results, two sensitivity analyses were performed, respectively. Firstly, the result from each survey was treated as a separate estimate and a meta-analysis of 18 individual NHIS (I2 <50% and P > 0.1 indicate that there was no significant between-study heterogeneity and a fixed effects model was used, otherwise, a random effects model was used) was conducted to calculate the summary HRs with 95% CIs. Secondly, we conducted a sensitivity analysis by excluding individuals who died within the first 2 years of follow-up. All analyses were conducted using SAS 9.3 (SAS Institute, Cary, NC) and a two-tailed P < 0.05 was considered to be statistically significant.
Results
Baseline Characteristics
The baseline characteristics of participants across 5 categories of chronic condition status are shown in Table 1. Of the 372,566 participants aged 30–84 years, 27.0, 12.2, 4.4, and 1.1% had 1, 2, 3, and ≥4 chronic diseases, respectively. Those of older age, men, non-Hispanic white, those who had high school education or below, those who were divorced/separated/widowed, those with obesity, former smokers, lifetime abstainer/former drinkers, and those who failed to meet PA guidelines were more likely to experience multimorbidity (all P < 0.0001). In addition, the prevalence of multimorbidity was very high in those aged 70–84 years (43.6%), medium among those aged 50–69 years (23.6%), and very low in those aged 30–49 years (5.1%).
Trends in Prevalence of Chronic Conditions
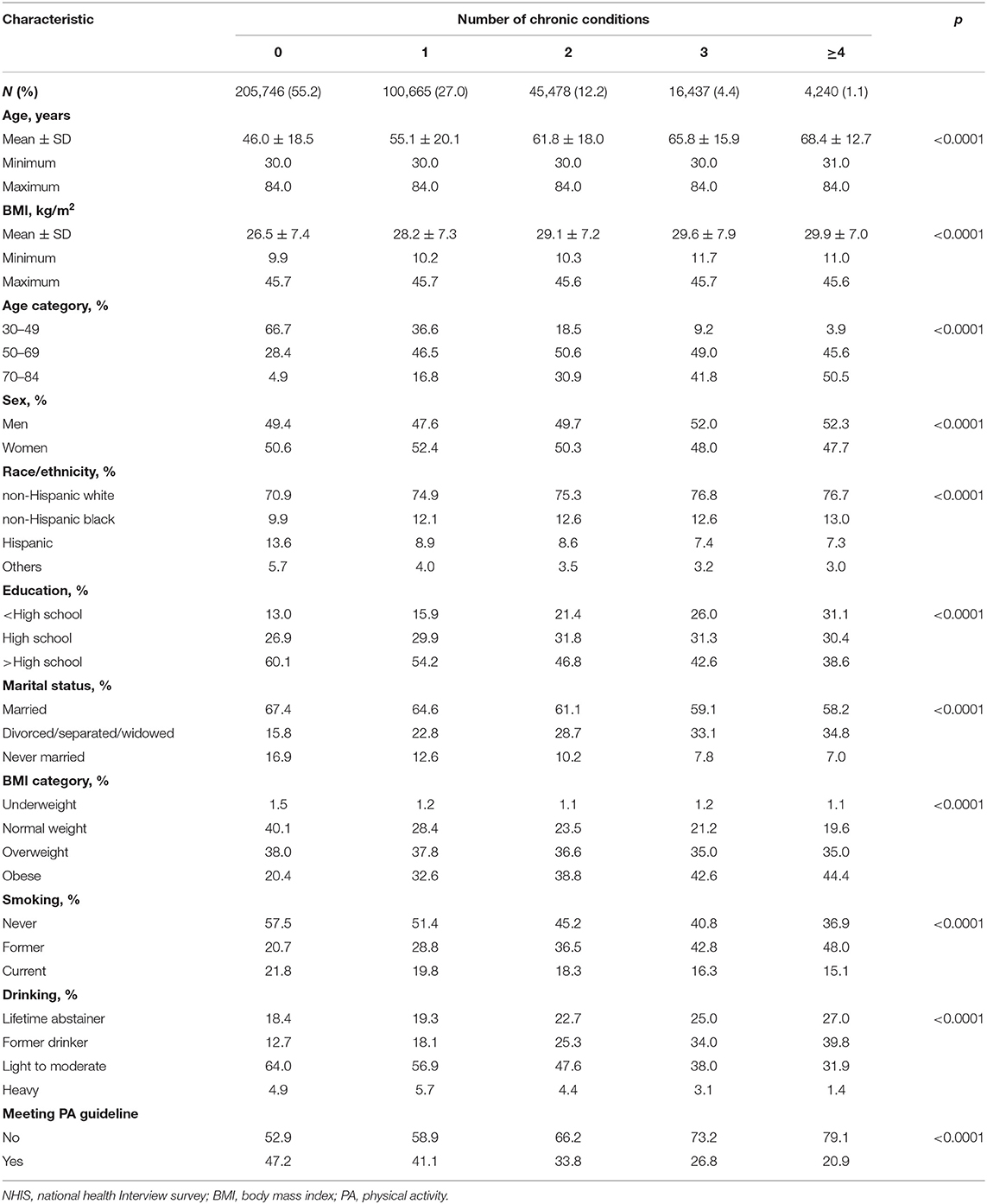
The trends in crude and age-standardized prevalence of chronic conditions are shown in Figure 2. The crude prevalence of having 1, 2, 3, and ≥4 chronic conditions increased from 25.8, 9.5, 3.4%, and 0.7% to 28.3, 12.9, 4.9, and 1.2% from 1997 to 2014, while age-standardized prevalence were 27.0, 10.3, 3.7, and 0.7% in 1997, and increased significantly to 28.0, 12.6, 4.7, and 1.1% in 2014, respectively (all P for trends <0.0001) (Figures 2A,B). For each specific chronic condition, there was an increased trend in the age-standardized prevalence of hypertension (29.3–35.5%), diabetes (6.9–10.7%), cancer (8.3–9.9%), and stroke (2.8–3.0%) (all P for trends <0.0001). However, the trend in heart disease prevalence decreased (P for trend <0.0001) (Figure 2B). Similar trends were seen in the crude prevalence of specific chronic condition and multimorbidity (Figure 2A). Subgroup analyses showed that those aged 70–84 years (vs. 50–69 or 30–49 years), men (vs. women), and non-Hispanic black (vs. Hispanics, Non-Hispanic whites or others) had a greater absolute increase in the prevalence of multimorbidity (Supplementary Table 1).
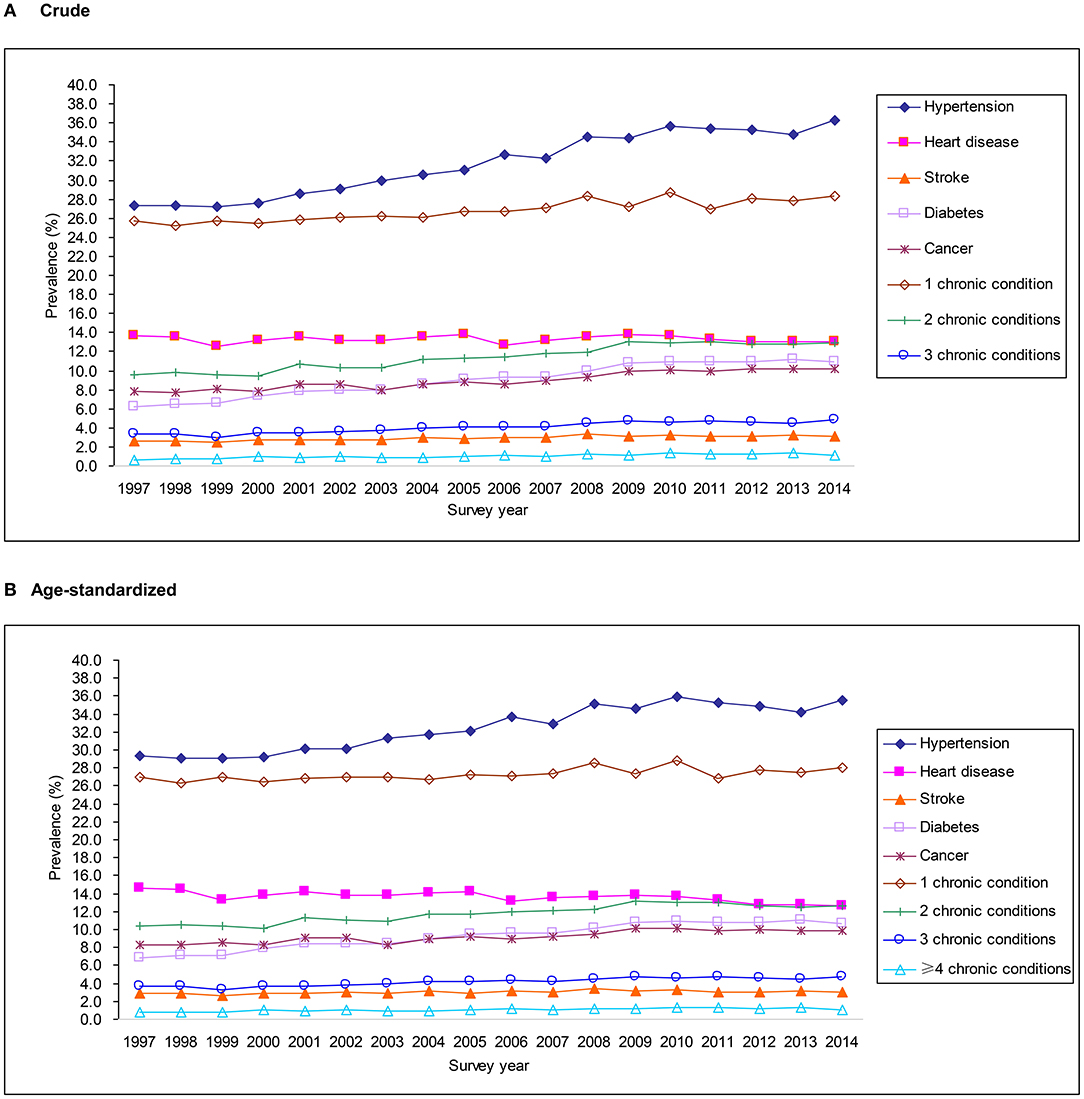
Figure 2. Trends in crude (A) and age-standardized (B) prevalence of chronic conditions from 1997 to 2014 in the National Health Interview Survey.
Survival Analysis of the Association Between Multimorbidity and All-Cause and Cause-Specific Mortality
During a median follow-up of 9.0 years, among 50,309 participants that died from all causes, 11,132 (22.1%) died due to CVD and 13,170 (26.2%) died due to cancer. We found that participants with stroke at baseline had the highest risk of all-cause mortality among all individual chronic conditions (Supplementary Table 2). Compared with participants without any aforementioned chronic conditions, those with 1, 2, 3, and ≥4 of chronic conditions had 1.41 (95% CI 1.37–1.45), 1.94 (1.88–2.00), 2.64 (2.54–2.75), and 3.68 (3.46–3.91) times the risk of all-cause mortality after adjustment for all important covariates (Table 2). Similar patterns were observed for CVD-specific and cancer-specific mortality, with larger effect size for CVD-specific mortality than for cancer-specific mortality (Table 2). Results on association of the number of all covariates with all-cause and cause-specific mortality were presented in Supplementary Table 3. In addition, higher risk of all-cause, CVD-specific, and cancer-specific mortality was also observed across categories of different cardiometabolic multimorbidity after excluding participants who self-reported cancer at baseline (Supplementary Table 4).
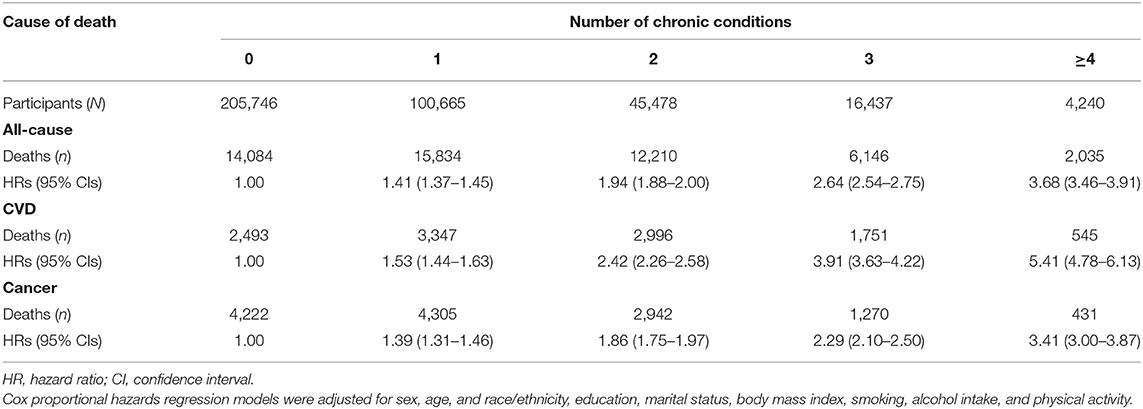
Table 2. Association of the number of chronic conditions with all-cause and cause-specific mortality.
Subgroup Analyses
The association between multimorbidity and all-cause mortality stratified by demographic factors and lifestyle factors is shown in Supplementary Table 5. The risk of all-cause mortality was somewhat stronger among those aged 30–49 years or aged 50–69 years (vs. those aged 70–84 years), women (vs. men), those with high school education level (vs. < high school or >high school), those never married (vs. married or divorced/separated/windowed adults), those with obesity (vs. those with normal weight or overweight), and never smokers (vs. former or current smokers).
Sensitivity Analyses
Sensitivity analysis showed that results from the meta-analysis of all 18 baseline surveys (without significant heterogeneity across the 4 subgroups of different chronic conditions) were similar to our primary results (Supplementary Table 6). In addition, sensitivity analysis that excluded participants who died within the first 2 years of follow-up also showed consistent findings with our primary results (Supplementary Table 7).
Discussion
Using nationally representative samples of U.S. adults, we found that 17.8% participants had multimorbidity (2 or more chronic conditions). The trends in prevalence of multimorbidity increased significantly from 1997 to 2014. Compared with participants who had no chronic conditions, those with 1, 2, 3, and ≥4 chronic conditions were nearly 1.4, 1.9, 2.6, and 3.7 times more likely to die from all causes. Similar associations were observed for CVD-specific and cancer-specific mortality. Of note, although multimorbidity was more prevalent in participants of older age, the risk of death of those with ≥4 chronic conditions were much higher among both young and middle-aged participants than among older ones. These findings underline the clinical importance of preventing and treating individuals with multimorbidity.
In this study, through 18 survey waves, the prevalence of specific chronic condition increased significantly while the prevalence of heart disease decreased slightly. For heart disease, the leading cause of death in the U.S. (18), although its prevalence has decreased totally, however, the prevalence has increased in older and male participants, which must draw enough attention. Our findings also show an increase in the prevalence of multimorbidity from 1997 to 2014 among U.S. adults. Similar to our findings, several studies have shown the prevalence of multimorbidity among the general population to have become more prevalent (2, 3, 19–21). For example, a study of 65,586 participants aged 50 years or older from the English Longitudinal Study of Aging found that the prevalence of multimorbidity increased from 41.6% in 2002/2003 to 46.6% in 2014/2015 (19). Similar increases in the prevalence of multimorbidity over time were also observed in the U.S., the Netherlands, Canada and Belgium (2, 3, 20, 21). The increase of multimorbidity emphasizes that a complementary strategy of common primary care and personal generalist service is imperative for the medical system (22).
Consistent with our findings, a study conducted using combined data from the Emerging Risk Factors Collaboration (including 689,300 participants with a mean age of 53 years) and from the UK Biobank (including 499,808 participants with a mean age of 57 years) found that having 2 or 3 chronic conditions (including diabetes, stroke, and myocardial infarction) gradually increased the risk of all-cause mortality (e.g., presence of 2: HR 3.6, 95% CI 3.2–4.1; presence of 3: HR 6.0, 95% CI 5.0–7.1) (6). However, hypertension, which is a major factor for mortality (23), was not included in that study. In 2016, a meta-analysis of 26 articles published between 2000 and 2014 including 650,967 older adults aged ≥65 years showed that multimorbidity was associated with increased risk of deaths, with HRs (95% CIs) of 1.73 (95% CI: 1.41–2.13) and 2.72 (95% CI: 1.81–4.08) for people with ≥2 and ≥3 chronic conditions, respectively (4). A recent cohort study of 500,769 participants aged 37–73 years from the UK Biobank also indicated a dose-response relationship between increased number of chronic conditions (including 43 non-cardiometabolic and cardiometabolic conditions) and all-cause, cancer, and vascular mortality (12). However, the participants included in that study were mostly with a lower socioeconomic level than the general UK population.
However, inconsistent with our findings, a study conducted in Hong Kong, China including 4,000 participants aged 65 years or older with a median follow-up of 9 years reported a non-significant association between multimorbidity and mortality (HR 1.20, 95% CI 0.89–1.62) (14). Another study including 1,751 community-dwelling adults in Manitoba aged 65 years or older showed a similar null association (HR 1.00, 95% CI 0.96–1.04) after a median follow-up of 5 years (13). Of note, the sample sizes of these two studies were relatively small, and included participants were all aged 65 years or older. Other possible reasons for the inconsistent findings with ours and others might be due to differences in the sampled population, the chronic diseases studied and confounders that were considered in statistical models.
The current focus in our study for multimorbidity including hypertension, heart disease, stroke, diabetes and cancer is mainly prevalent among older people (24, 25). Similar to previous studies (12, 26), our findings showed that multimorbidity was more likely to occur among those of older age than those of younger age. Among those of old age (≥70 years), the risk of all-cause mortality of those with ≥4 of chronic conditions was 3 fold compared with participants without any above-mentioned chronic conditions. However, among young (30–49 years) and relative older (50–69 years) adults, the risk of all-cause mortality of those with ≥4 of chronic conditions were up to 8 and 6 fold compared with participants without any above-mentioned chronic conditions, suggesting more attention should be paid to young people with multimorbidity. Special interventions for the management of multimorbidity in young adults are warranted.
Strengths and Limitations
We used the national and representative samples of U.S. adults from 18 baseline surveys with sufficient power (N = 372,566) to generate reliable statistical estimates. In addition, we adjusted for several important covariates in the statistical models, and the sensitivity analyses confirmed the stability of our findings. However, our study has several limitations. First, the chronic conditions of participants were self-reported, potentially leading to misclassification of participants with chronic conditions into the group of no chronic conditions, which would likely lead to an underestimation of the strength of the observed association. In addition, the limited information on severity of chronic conditions and the lack of data on accruing multimorbidity exposure change over time might potentially affect our findings. Second, we only focused on the association between the number of chronic conditions and mortality, and did not examine the risk of combinations of specific chronic conditions. However, data from the Emerging Risk Factors Collaboration showed that participants with combinations of any two of three chronic conditions (heart disease, stroke, diabetes) had a similar risk of mortality (6). Third, residual or unmeasured confounding might have influenced our findings. Fourth, although National Death Index has been demonstrated to be accurate in determining overall death previously (15), some other studies have indicated that there was discordance between the NDI cause-specific mortality and other sources of data (27, 28), which might have affected our findings possibly.
Conclusions
The prevalence of multimorbidity has increased significantly among U.S. adults from 1997 to 2014, especially for older adults, men, and non-Hispanic blacks. The increasing number of chronic conditions was associated with a higher risk of all-cause, CVD-specific, and cancer-specific mortality. In addition, although multimorbidity was more prevalent among those of older age, the association between multimorbidity and mortality was also strong among young and middle-aged adults. As the prevalence of multimorbidity tended to increase over time, our data suggest effective prevention and intervention programs are necessary to limit the increased mortality risk associated with multimorbidity, and that programs should be targeted at both young and older aged adults.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
BX designed the study and is the principal investigator and guarantor. LY conducted the data analysis and drafted the manuscript. CGM, JS, MZ, and BX critically revised the manuscript for important intellectual content. The corresponding author attests that all the listed authors meet the authorship criteria and that no others meeting the criteria have been omitted. All authors approved the final version of the manuscript.
Funding
BX was supported by the Innovation Team of Climbing Program of Shandong University. CGM was supported by a National Heart Foundation of Australia future leader fellowship (100849). The funders had no role in the study design or implementation; data collection, management, analysis, or interpretation; manuscript preparation, review, or approval; or the decision to submit the manuscript for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the National Center for Health Statistics of the Centers for Disease Control and Prevention for sharing the National Health Interview Survey data. The datasets used and/or analyzed during the current study are available at www.cdc.gov/nchs/nhis/index.htm.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.731240/full#supplementary-material
References
1. Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: trends over the past 10 years. NCHS Data Brief. (2012) 1–8. Available online at: https://www.cdc.gov/nchs/data/databriefs/db100.pdf (accessed April 4, 2021).
2. Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the national health interview survey, 2010. Prev Chronic Dis. (2013) 10:E65. doi: 10.5888/pcd10.120203
3. van Oostrom SH, Gijsen R, Stirbu I, Korevaar JC, Schellevis FG, Picavet HS, et al. Time trends in prevalence of chronic diseases and multimorbidity not only due to aging: data from general practices and health surveys. PLoS ONE. (2016) 11:e0160264. doi: 10.1371/journal.pone.0160264
4. Nunes BP, Flores TR, Mielke GI, Thume E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. (2016) 67:130–8. doi: 10.1016/j.archger.2016.07.008
5. Vogeli C, Shields AE, Lee TA, Gibson TB, Marder WD, Weiss KB, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. (2007) 22:391–5. doi: 10.1007/s11606-007-0322-1
6. Emerging Risk Factors Collaboration, Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. (2015) 314:52–60. doi: 10.1001/jama.2015.7008
7. Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today's healthcare systems. BMC Fam Pract. (2015) 16:129. doi: 10.1186/s12875-015-0344-4
8. Lehnert T, Heider D, Leicht H, Heinrich S, Corrieri S, Luppa M, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev. (2011) 68:387–420. doi: 10.1177/1077558711399580
9. Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. (2011) 364:829–41. doi: 10.1056/NEJMoa1008862
10. Carnevale V, Fontana A, Scillitani A, Sinisi R, Romagnoli E, Copetti M. Incidence and all-cause mortality for hip fracture in comparison to stroke, and myocardial infarction: a fifteen years population-based longitudinal study. Endocrine. (2017) 58:320–31. doi: 10.1007/s12020-017-1423-1
11. Jorgensen P, Langhammer A, Krokstad S, Forsmo S. Mortality in persons with undetected and diagnosed hypertension, type 2 diabetes, and hypothyroidism, compared with persons without corresponding disease - a prospective cohort study; The HUNT Study, Norway. BMC Fam Pract. (2017) 18:98. doi: 10.1186/s12875-017-0672-7
12. Jani BD, Hanlon P, Nicholl BI, McQueenie R, Gallacher KI, Lee D, et al. Relationship between multimorbidity, demographic factors and mortality: findings from the UK Biobank cohort. BMC Med. (2019) 17:74. doi: 10.1186/s12916-019-1305-x
13. St John PD, Tyas SL, Menec V, Tate R. Multimorbidity, disability, and mortality in community-dwelling older adults. Can Fam Physician. (2014) 60:E272–80. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4020665/ (accessed April 4, 2021).
14. Woo J, Leung J. Multi-morbidity, dependency, and frailty singly or in combination have different impact on health outcomes. Age. (2014) 36:923–31. doi: 10.1007/s11357-013-9590-3
15. National Center for Health Statistics. NHANES I Epidemiologic Follow-Up Survey (NHEFS) Calibration Sample for NDI Matching Methodology. Available online at: https://www.cdc.gov/nchs/data/datalinkage/mort_calibration_study.pdf (accessed: April 4, 2021)
16. US Department of Health and Human Services. Physical activity guidelines for Americans. JAMA. (2018) 320:2020–8. doi: 10.1001/jama.2018.14854
17. Howden LM, Meyer JA Age Sex Composition: 2010 (2010 Census Briefs). Available online at: http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf (accessed April 4, 2021).
18. Centers for Disease Control and Prevention. Number of deaths from 113 selected causes, Enterocolitis due to Clostridium difficile, drug-induced causes, alcohol-induced causes, and injury by firearms, by Hispanic origin, race for non-Hispanic population, and sex: United States. Report, Centers for Disease Control and Prevention, USA, 2015 (Table I−24). National Vital Statistics Rep. (2017) 66:63–4. Available online at: https://www.cdc.gov/nchs/data/nvsr/nvsr66/nvsr66_06_tables.pdf (accessed: April 4, 2021).
19. Singer L, Green M, Rowe F, Ben-Shlomo Y, Kulu H, Morrissey K. Trends in multimorbidity, complex multimorbidity and multiple functional limitations in the ageing population of England, 2002-2015. J Comorb. (2019) 9:2235042X19872030. doi: 10.1177/2235042X19872030
20. Lebenbaum M, Zaric GS, Thind A, Sarma S. Trends in obesity and multimorbidity in Canada. Prev Med. (2018) 116:173–9. doi: 10.1016/j.ypmed.2018.08.025
21. van den Akker M, Vaes B, Goderis G, Van Pottelbergh G, De Burghgraeve T, Henrard S. Trends in multimorbidity and polypharmacy in the Flemish-Belgian population between 2000 and 2015. PLoS ONE. (2019) 14:e0212046. doi: 10.1371/journal.pone.0212046
22. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. (2012) 380:37–43. doi: 10.1016/S0140-6736(12)60240-2
23. Bundy JD, Li C, Stuchlik P, Bu X, Kelly TN, Mills KT, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. (2017) 2:775–81. doi: 10.1001/jamacardio.2017.1421
24. Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. (2012) 345:e5205. doi: 10.1136/bmj.e5205
25. Guerra SG, Berbiche D, Vasiliadis HM. Measuring multimorbidity in older adults: comparing different data sources. BMC Geriatr. (2019) 19:166. doi: 10.1186/s12877-019-1173-4
26. Rocca WA, Boyd CM, Grossardt BR, Bobo WV, Rutten LJF, Roger VL, et al. Prevalence of multimorbidity in a geographically defined american population: patterns by age, sex, and race/ethnicity. Mayo Clin Proc. (2014) 89:1336–49. doi: 10.1016/j.mayocp.2014.07.010
27. Olubowale OT, Safford MM, Brown TM, Durant RW, Howard VJ, Gamboa C, et al. Comparison of expert adjudicated coronary heart disease and cardiovascular disease mortality with the national death index: results from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. J Am Heart Assoc. (2017) 6:e004966. doi: 10.1161/JAHA.116.004966
Keywords: multimorbidity, mortality, cardiovascular disease, cancer, trend
Citation: Yang L, Sun J, Zhao M, Magnussen CG and Xi B (2021) Trends in Cardiometabolic and Cancer Multimorbidity Prevalence and Its Risk With All-Cause and Cause-Specific Mortality in U.S. Adults: Prospective Cohort Study. Front. Cardiovasc. Med. 8:731240. doi: 10.3389/fcvm.2021.731240
Received: 27 September 2021; Accepted: 23 November 2021;
Published: 09 December 2021.
Edited by:
Carlo Gabriele Tocchetti, University of Naples Federico II, ItalyCopyright © 2021 Yang, Sun, Zhao, Magnussen and Xi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Xi, eGlibzIwMTBAc2R1LmVkdS5jbg==
 Liu Yang
Liu Yang Jiahong Sun
Jiahong Sun Min Zhao2
Min Zhao2 Bo Xi
Bo Xi