
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 25 August 2021
Sec. Atherosclerosis and Vascular Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.726341
 Haiming Wang1†
Haiming Wang1† Min Jiang1†
Min Jiang1† Xin Li2
Xin Li2 Yunzhang Zhao1
Yunzhang Zhao1 Junjie Shao1
Junjie Shao1 Zifan Liu1
Zifan Liu1 Lejian Lin1
Lejian Lin1 Qiang Xu1
Qiang Xu1 Lin Wang1
Lin Wang1 Xuechun Lu3
Xuechun Lu3 Haomin Zhang3
Haomin Zhang3 Yundai Chen1*
Yundai Chen1* Ran Zhang1*
Ran Zhang1*Background: Anti-inflammatory therapy has been proposed as a promising treatment for coronary heart disease (CHD) that could reduce residual inflammation risk (RIR) and therefore major adverse cardiovascular events. We implemented a systematic review and meta-analysis of randomized controlled trials (RCTs) to assess the clinical benefits of anti-inflammatory agents in patients with CHD based on secondary cardiovascular prevention.
Methods: We systemically searched the PubMed, Embase, and Cochrane Library databases for RCTs (published between Jan 1, 1950, and June 1, 2021; no language restrictions) that focused on anti-inflammatory therapy for coronary heart disease. Our primary end points of interest were a composite of all-cause death, recurrent myocardial infarction and stroke. We processed pooled data using a random-effects model.
Results: Of 1497 selected studies, 18 studies with 67,449 participants met our inclusion criteria and were included in the present meta-analysis. Comparing anti-inflammatory agents with placebo, there was no significant decrease in risk of primary end points, secondary end points, all-cause mortality, cardiac mortality, recurrent myocardial infarction, stroke or revascularization. Further subgroup analysis indicated that anti-inflammatory agents led to a significant reduction in secondary end points (OR 0.87, CI 0.77–0.99; P = 0.03), recurrent myocardial infarction (OR 0.86, CI 0.78–0.95; P = 0.003) and revascularization (OR 0.81, CI 0.70–0.92; P = 0.001) in patients with stable CHD compared with placebo. Moreover, stable CHD patients had a lower propensity for recurrent myocardial infarction than acute coronary syndrome (ACS) patients when using anti-inflammatory agents (P = 0.03). The colchicine subgroup analysis showed that colchicine yielded a promising reduction in the primary end points (OR 0.81, CI 0.70–0.95; P = 0.009) compared with placebo. Anti-inflammatory agents were associated with a higher risk of infection (OR 1.13, CI 1.03–1.23; P = 0.007) and negligible effects on cancers (OR 0.98, CI 0.90–1.06; P = 0.61).
Conclusion: Anti-inflammatory agents appear to have beneficial effects in reducing the risk of recurrent myocardial infarction in patients with stable CHD, albeit at the cost of increased infection. Notably, colchicine demonstrates a promising cardioprotective effect with a lower incidence of major cardiovascular events and thus is a potential therapeutic strategy for stable CHD patients.
Systematic Review Registration: PROSPERO, identifier CRD42021245514.
Coronary heart disease (CHD) is a progressive clinical syndrome that is associated with an enhanced risk of fatal myocardial infarction, stroke, revascularization or cardiogenic death (1, 2). The available treatments recommended by the guidelines have not been reliably shown to further alter this clinical course (1, 3). Recent evidence has indicated that residual inflammatory risk (RIR) accelerates the progression of CHD by modulating immune cells and inflammatory cytokines (2, 4). A series of clinical studies have attempted to evaluate the efficacy of various anti-inflammatory agents in CHD patients (5, 6). The CANTOS trial (The Canakinumab Anti-inflammatory Thrombosis Outcomes Study) demonstrated the pivotal role of anti-inflammatory manipulation in improving cardiovascular outcomes by reducing the levels of interleukin-1β (IL-1β) and high-sensitivity C-reactive protein (hsCRP) (7, 8). The latest LoDoCo2 trial (Colchicine in Patients with Chronic Coronary Disease/Low-Dose Colchicine 2) suggested a lower risk of cardiovascular events with the administration of colchicine (9). We therefore sought to collect the latest clinical evidence and objectively assess the potential roles of anti-inflammatory therapy in CHD treatment. However, considering that previous studies of individual anti-inflammatory therapies failed to show distinctive improvements in major cardiovascular events (MACEs) (10), we performed a systematic review and meta-analysis of randomized controlled trials (RCTs) to investigate the effects of anti-inflammatory therapy on cardiovascular outcomes in patients with CHD.
This systematic review and meta-analysis was performed in accord with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (11). We systematically searched the Embase, PubMed and Cochrane Library databases for relevant studies published between Jan 1, 1950, and June 1, 2021, with no language restrictions. We used the following combined text and MeSH terms: “anti-inflammatory agents” and “myocardial ischemia.” We also performed a manual search of the references of relevant meta-analyses and systematic reviews for eligible studies.
RCTs comparing anti-inflammatory agents to placebo in CHD were considered eligible for inclusion. All pre-enrolled studies must contain at least one of the clinical outcomes, including all-cause mortality, cardiac mortality, recurrent myocardial infarction, revascularization and major adverse events (infections and cancers). Our primary end point of interest was a composite of all-cause death, recurrent myocardial infarction and stroke. The secondary end points included the components of the primary end points as well as revascularization. The exclusion criteria were as follows: observational and retrospective studies; RCTs that did not report the cardiovascular outcomes of interest; and RCTs that used nonsteroidal anti-inflammatory drugs or involved cardiopulmonary bypass therapy.
Two independent investigators (HW and MJ) screened the retrieved studies on the basis of titles and abstracts, and the remaining studies that satisfied the inclusion criteria were reviewed for full-text evaluation. Studies selected for subsequent detailed analysis and data extraction were analyzed by two investigators (HW and MJ). Disagreements were settled by a third investigator, if necessary (RZ). We drew the requisite data from each included study via a standardized data extraction form. Quality assessment of the studies was performed according to the PRISMA recommendations.
We assessed the clinical benefits of anti-inflammatory agents on nine categorical variable outcomes: primary end points, secondary end points, all-cause mortality, cardiac mortality, recurrent myocardial infarction, revascularization and major adverse events (infections and cancers). The pooled estimates were presented as odds ratios (ORs) with 95% confidence intervals (CIs) using a random-effects model on the basis of the DerSimonian–Laird method. Given the heterogeneity of the eligible studies and its underlying influences on beneficial effects, both the Cochran Q-test and I2-test were used to assess the magnitude of the heterogeneity between studies for each outcome. When the value of the I2-test was >50%, a study was considered to have high heterogeneity. Sensitivity analyses were performed to identify which studies had increased heterogeneity. In addition, a funnel plot of each study's effect size against the standard error was constructed to assess the potential publication bias, and the trim-and-fill test was used to estimate the effects of publication bias on the interpretation of the outcome. According to the type of CHD or the kind of anti-inflammatory agents, we implemented two subgroup analyses to discover potential clinical benefits. In this meta-analysis, we used Review Manager 5.3 and Stata 14.0 for statistical data processing.
The search strategy identified 1,497 studies, of which 18 studies with 67,449 participants met our inclusion criteria and were selected for the current meta-analysis after the three-level screening processes (Figure 1). The characteristics of all eligible studies that were published between 2003 and 2021 are summarized in Table 1. Nine anti-inflammatory agents, namely, colchicine, anakinra, darapladib, losmapimod, inclacumab, varespladib, pexelizumab, canakinumab, and methotrexate, were administered separately in the included studies. The weighted mean follow-up duration was 18.3 months (range 30 days−3.7 years), and the ages of the patients ranged from 51 to 74 years old. The majority of the patients were male, and all included patients had a high rate of typical risk factors, including hypertension, diabetes and hyperlipidemia. Of 18 studies reporting anti-inflammatory therapy, 5 studies—the LoDoCo trial, the STABILITY trial, the CANTOS trial, the CIRT trial and the LoDoCo2 trial—investigated patients with stable CHD, (7, 9, 12–14) and the remaining 13 trials recruited ACS patients (15–27). The assessment of risk of bias in this meta-analysis is shown in Supplementary Figure 1. All 18 RCTs reported adequate randomization, and only one yielded
incomplete outcome data.
In a pooled analysis of all 18 studies, anti-inflammatory therapy did not statistically show a greater reduction in the primary end points (OR 0.99, CI 0.88–1.13; P = 0.92), secondary end points (OR 0.92, CI 0.82–1.04; P = 0. 02), all-cause mortality (OR 1.02, CI 0.93–1.11; P = 0.73), cardiac mortality (OR 0.94, CI 0.86–1.03; P = 0. 21), recurrent myocardial infarction (OR 0.99, CI 0.85–1.14; P = 0.86), stroke (OR 0.96, CI 0.84–1.10; P = 0.57) or revascularization (OR 0.87, CI 0.74–1.02; P = 0.09) than other therapeutic approaches, with different degrees of significant between-study heterogeneity (Figure 2 and Supplementary Figures 2–7). Visual inspection of the funnel plots intuitively demonstrated obvious graphical asymmetries, and the trim-and-fill test indicated that these publication biases did not impact the estimates (Supplementary Figure 8). Further sensitivity analysis showed that the results were similar when each study was individually excluded.
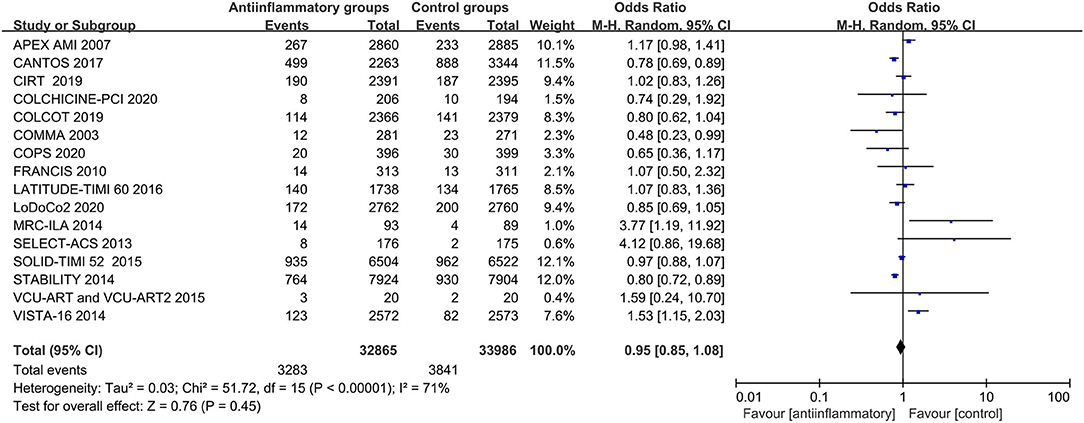
Figure 2. Forest plots of studies evaluating primary end points in patients receiving anti-inflammatory agents vs. placebo.
Anti-inflammatory agents led to a significant reduction in secondary end points (OR 0.87, CI 0.77–0.99; P = 0.03), recurrent myocardial infarction (OR 0.86, CI 0.78–0.95; P = 0.003) and revascularization (OR 0.81, CI 0.70–0.92; P = 0.001) compared with placebo in patients with stable CHD, with different degrees of significant between-study heterogeneity (Figures 3–5). Visual inspection of their funnel plots showed that no publication biases were evident. Additionally, stable CHD patients had a lower propensity for recurrent myocardial infarction than the ACS patients when using anti-inflammatory drugs (P = 0.03; Table 2). No significant differences in primary end points, all-cause mortality, cardiac mortality or stroke were observed in this subgroup analysis (Supplementary Figures 9–12).
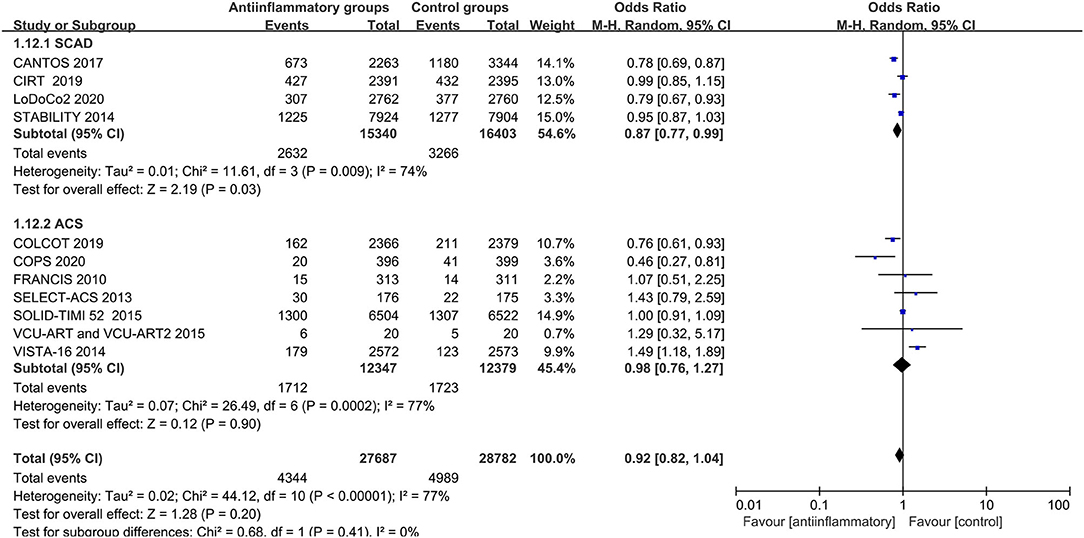
Figure 3. Forest plots of studies evaluating secondary end points in patients with stable CHD vs. ACS.
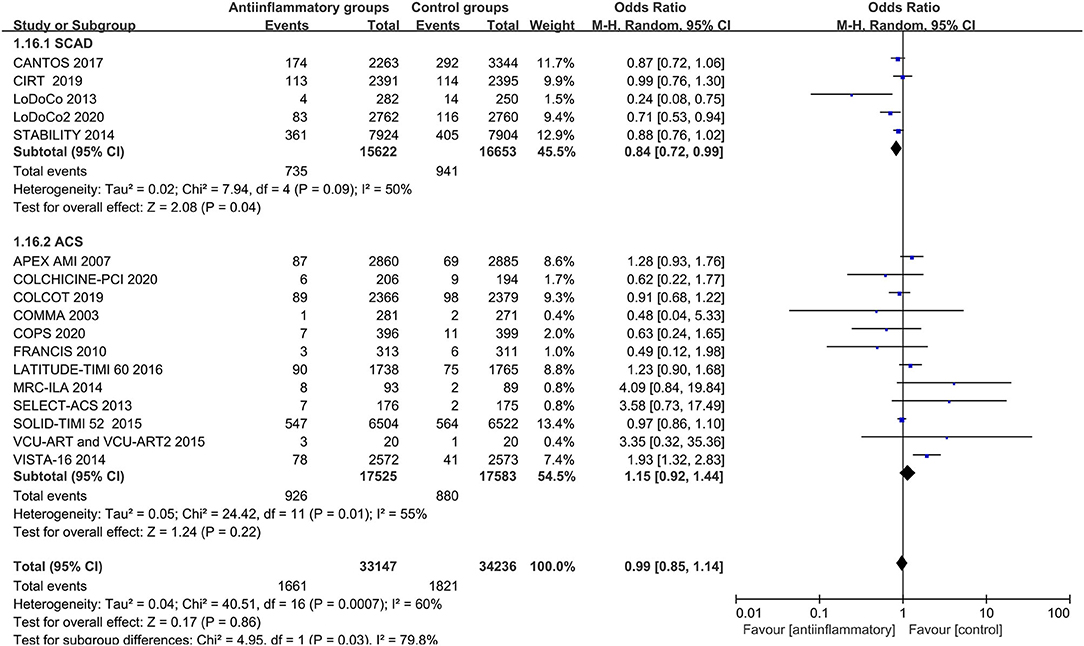
Figure 4. Forest plots of studies evaluating recurrent myocardial infarction in patients with stable CHD vs. ACS.
The subgroup analysis showed that colchicine yielded a promising reduction in the primary end points (OR 0.81, CI 0.70–0.95; P = 0.009) compared with placebo, with no significant between-study heterogeneity (Figure 6 and Supplementary Figure 13).
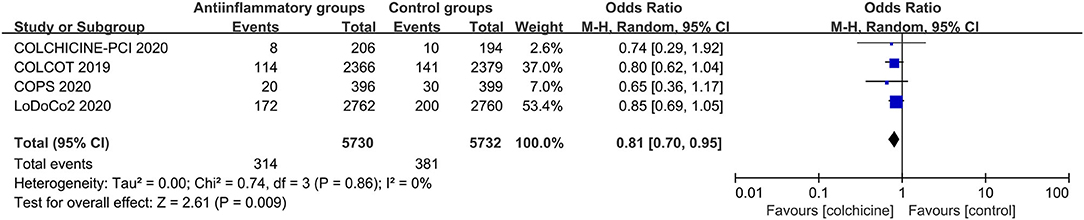
Figure 6. Forest plots of studies evaluating primary end points in patients receiving colchicine vs. placebo.
Anti-inflammatory agents were associated with a higher risk of infections (OR 1.13, CI 1.03–1.23; P = 0.007) and had negligible effects on cancers (OR 0.98, CI 0.90–1.06; P = 0.61), with no significant between-study heterogeneity (Figures 7, 8 and Supplementary Figures 14, 15).
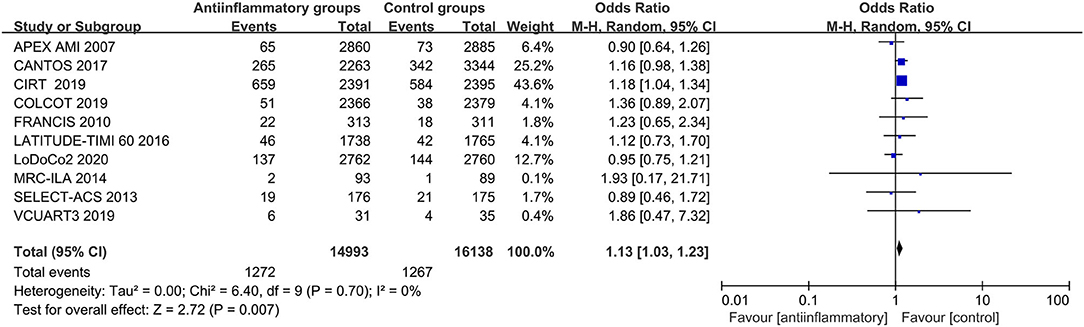
Figure 7. Forest plots of studies evaluating infections in patients receiving anti-inflammatory agents vs. placebo.
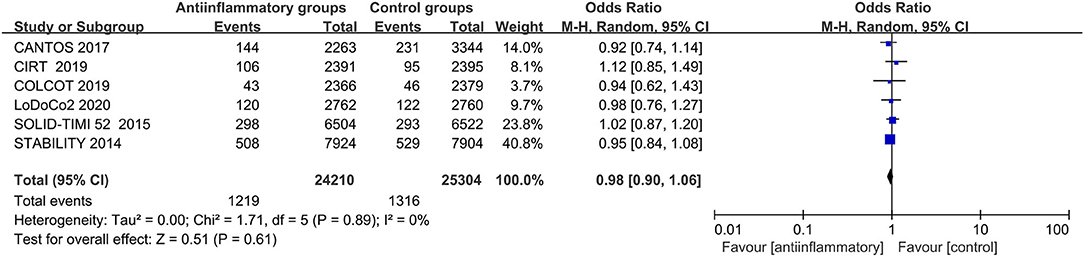
Figure 8. Forest plots of studies evaluating cancers in patients receiving anti-inflammatory agents vs. placebo.
In this systematic review and meta-analysis, we showed that anti-inflammatory agents yield mild cardiovascular protective effects but result in an increased risk of infections. However, further subgroup analysis demonstrated that multiple anti-inflammatory agents reduce the risk of recurrent myocardial infarction and revascularization in stable CHD. Considering the different subtypes of the disease, there was a significant reduction in recurrent myocardial infarction in stable CHD patients compared with the ACS patients. Additionally, among nine anti-inflammatory agents, colchicine had pronounced cardiovascular benefits among patients with all kinds of CHD. Therefore, these data suggest that selective anti-inflammatory therapy is promising in the management of CHD.
The attainment of cardiovascular benefits is compromised by the limitations of available treatment for CHD (1, 2, 8, 28). Although low-density lipoprotein-cholesterol lowering and antiplatelet therapies have been widely recommended by guidelines and administered in clinical practice, more than half of CHD patients have a high level of hsCRP, a direct metric of systemic inflammation, to drive the natural history of this disease (2, 29, 30). Persistent residual inflammatory risk destabilizes atherosclerotic plaques and exacerbates the risk of MACEs (2). In the FOURIER (Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk) trial, patients with CHD were more prone to develop adverse cardiovascular events when proprotein convertase subtilisin-kexin type 9 (PCSK9) inhibitors were used to reduce low-density lipoprotein cholesterol (LDL-C) to a lower level but hsCRP levels exceeded the upper limit of normal (28, 31). In this context, anti-inflammatory therapy emerges as a novel strategy that can make further progress against this residual burden while alleviating long-term cardiovascular risk (29). As anticipated, both the CANTOS trial and the LoDoCo2 trial confirmed the beneficial effects of anti-inflammatory therapy with canakinumab and colchicine (7, 9). However, controversies regarding anti-inflammatory therapy still exist (10). In this meta-analysis, we did not find benefits of anti-inflammatory therapy in all CHD patients. Indeed, it is possible that the pooled OR may be skewed by a few potential chance findings in the present meta-analysis. Importantly, this inconsistency is mainly because the 18 eligible studies differ in several ways, including sample size differences and evaluation of clinical outcomes in individual studies, the time course of anti-inflammatory agents, and background oral secondary prevention medications (5, 10, 32). The between-study heterogeneity that adequately reflected these differences in study design were not attenuated. Future high-quality studies with larger samples should be conducted to obtain accurate estimates of the efficacy of anti-inflammatory agents. Collectively, more evidence is needed before anti-inflammatory therapy changes current clinical practice (10).
To minimize this heterogeneity in the included studies, we conducted additional subgroup analyses by modifying the inclusion criteria and excluding studies with different outcome definitions. Of particular interest, the five studies recruiting patients with stable CHD showed that substantial cardiovascular benefits were primarily attributed to risk reductions of 14, 19, and 13% for recurrent myocardial infarction, revascularization and secondary end points, respectively. This finding was consistent with a recently published meta-analysis focusing on stable CHD patients (5). These data could be interpreted by the pathogenesis of coronary atherosclerotic plaques that consists of a large lipid core and thin fibrous cap involving activated immune cells and inflammatory cytokines (2, 33–35). In the phase of plaque progression, anti-inflammatory therapy targeting inflammatory factors renders patients more susceptible to stabilization (2, 35, 36). When ACS occurs, immune cells and inflammatory cytokines are released from the plaque into the blood or depleted (36), which results in the loss of targets for anti-inflammatory agents. Furthermore, in stable CHD, the reserved microvascular system, intact myocardium and intervenable inflammatory pathways make anti-inflammatory therapy much more feasible and efficient than ACS (1, 5). Therefore, anti-inflammatory therapy is more likely to be beneficial in the early or stable stage of CHD.
The striking result was the CANTOS trial, in which canakinumab therapy successfully reduced cardiovascular risk, which indicates that the key inflammatory targets are most likely focused on the IL-1β to IL-6 to CRP pathway (2, 7, 8). In theory, colchicine, a widely available antitubulin agent, can irreversibly suppress the NLRP3 inflammasome and induce neutrophil dysfunction, and it therefore reduces circulatory levels of IL-1β, IL-6 and CRP (2, 6, 32, 37). Four eligible RCTs compared colchicine with placebo (9, 14, 15, 18, 26). Our data showed that colchicine reduces the risk of cardiovascular events by 19%, which was consistent with a recently published study of colchicine for secondary prevention of cardiovascular diseases (1). However, none of these 4 RCTs used hsCRP as an indicator for therapeutic effect evaluation or CT scans to assess plaque progression. Whether the anti-inflammatory benefits of colchicine are independent of serum lipid lowering remains uncertain (38). A previous study recruiting primary biliary cirrhosis patients showed a decline in the level of oxidized LDL-C after the administration of colchicine (38, 39). The mechanism of the cardiovascular benefit from colchicine needs further evaluation. Most other anti-inflammatory agents showed no significant cardiovascular benefits. This may be caused by different mechanisms and administration approaches of anti-inflammatory agents (10), and anti-inflammatory therapy focuses on regulating the immune balance rather than completely suppressing the inflammatory response (2, 5).
There is a strong association between anti-inflammatory agents and the impaired host defense system (2, 7). The pooled analyses of all included studies showed that anti-inflammatory agents result in a 14% increase in the risk of infections. Secondary pneumonia was the most common; therefore, early monitoring and preventive antibiotic therapy could reconcile this treatment dilemma (2, 5). In addition, our data showed that anti-inflammatory agents conferred no significant risk of new incident cancers. This may indicate that drug-induced immunosuppression is not sufficient to promote tumorigenesis. In contrast, the CANTOS trial demonstrated a significant reduction in lung cancers by canakinumab (7). Ongoing studies are exploring the potential effects of canakinumab on lung cancer patients (29). For colchicine with the most clinical evidence of anti-inflammatory properties, it mainly increases the incidence of diarrhea, which is reversible with drug discontinuation (40). Moreover, combined administration of colchicine and statins in the LoDoCo-2 and COLCOT trials also exhibit no apparent increase in myopathy or rhabdomyolysis (40).
There were several limitations in this study. The mean follow-up duration of all RCTs was 18.3 months, and the minimum period was 30 days. The long-term outcome of anti-inflammatory therapy needs further evidence. Second, raw patient-level data of all selected studies could not be obtained; hence, only modified study-level data were extracted and reanalyzed in the present meta-analysis. Although the assessable end points of interest in this meta-analysis were objective in the recruited studies, some studies were still accompanied by a risk of bias, such as incomplete research data. Meanwhile, we should keep in mind that the implementation of revascularization in CHD patients in all eligible studies depends on the various indications practiced at different hospitals, which renders the decreased risk of revascularization as the softest of all cardiovascular events. Third, the ideal time course and doses of agents have not yet been confirmed in recent clinical trials (10). Whether the timing of drug administration is as early as possible remains uncertain. Finally, 7 trials recruited fewer than 300 people; thus, type I error and small sample size bias should be fully considered (14, 18, 19, 21, 23, 24, 27). More large-scale clinical trials are needed to further verify the effects of anti-inflammatory agents in CHD patients.
Anti-inflammatory therapy reduces the risk of recurrent myocardial infarction in patients with stable CHD. Although uncertainties still exist, the addition of anti-inflammatory therapy to standard medical therapy in patients with CHD is promising for improving long-term cardiovascular outcomes.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
HW, MJ, YC, and RZ contributed to the study conception and design, and writing the manuscript. HW, MJ, XLi, YZ, and ZL performed data collection and analysis. HW, MJ, RZ, LL, QX, LW, XLu and HZ commented on the research design, data analysis, writing the manuscript, and supervision of the study. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (81871516).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.726341/full#supplementary-material
Supplementary Figure 1. Bias risk assessment of the studies.
Supplementary Figure 2. Forest plots of studies evaluating secondary end points in patients receiving anti-inflammatory agents vs. placebo.
Supplementary Figure 3. Forest plots of studies evaluating all-cause mortality in patients receiving anti-inflammatory agents vs. placebo.
Supplementary Figure 4. Forest plots of studies evaluating cardiac mortality in patients receiving anti-inflammatory agents vs. placebo.
Supplementary Figure 5. Forest plots of studies evaluating recurrent myocardial infarction in patients receiving anti-inflammatory agents vs. placebo.
Supplementary Figure 6. Forest plots of studies evaluating stroke in patients receiving anti-inflammatory agents vs. placebo.
Supplementary Figure 7. Forest plots of studies evaluating revascularization in patients receiving anti-inflammatory agents vs. placebo.
Supplementary Figure 8. Funnel plots of odds ratios and standard errors to assess the publication bias of anti-inflammatory agents vs. placebo in primary end points (A), secondary end points (B), all-cause mortality (C), cardiac mortality (D), recurrent myocardial infarction (E), stroke (F) and revascularization (G).
Supplementary Figure 9. Forest plots of studies evaluating primary end points in patients with stable CHD vs. ACS.
Supplementary Figure 10. Forest plots of studies evaluating all-cause mortality in patients with stable CHD vs. ACS.
Supplementary Figure 11. Forest plots of studies evaluating cardiac mortality in patients with stable CHD vs. ACS.
Supplementary Figure 12. Forest plots of studies evaluating stroke in patients with stable CHD vs. ACS.
Supplementary Figure 13. Funnel plots of odds ratios and standard errors to assess the publication bias of colchicine vs. placebo in primary end points.
Supplementary Figure 14. Funnel plots of odds ratios and standard errors to assess the publication bias of anti-inflammatory agents vs. placebo in infections.
Supplementary Figure 15. Funnel plots of odds ratios and standard errors to assess the publication bias of anti-inflammatory agents vs. placebo in cancers.
1. Samuel M, Tardif JC, Bouabdallaoui N, Khairy P, Dubé MP, Blondeau L, et al. Colchicine for secondary prevention of cardiovascular disease: a systematic review and meta-analysis of randomized controlled trials. Can J Cardiol. (2020) 37:776–85. doi: 10.1016/j.cjca.2020.10.006
2. Wang H, Liu Z, Shao J, Lin L, Jiang M, Wang L, et al. Immune and inflammation in acute coronary syndrome: molecular mechanisms and therapeutic implications. J Immunol Res. (2020) 2020:4904217. doi: 10.1155/2020/4904217
3. Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to(2013). Circulation. (2015) 132:1667–78. doi: 10.1161/CIRCULATIONAHA.114.008720
4. Epelman S, Liu PP, Mann DL. Role of innate and adaptive immune mechanisms in cardiac injury and repair. Nat Rev Immunol. (2015) 15:117–29. doi: 10.1038/nri3800
5. Wudexi I, Shokri E, Abo-Aly M, Shindo K, Abdel-Latif A. Comparative effectiveness of anti-inflammatory drug treatments in coronary heart disease patients: a systematic review and network meta-analysis. Mediators Inflamm. (2021) 2021:5160728. doi: 10.1155/2021/5160728
6. Khambhati J, Engels M, Allard-Ratick M, Sandesara PB, Quyyumi AA, Sperling L. Immunotherapy for the prevention of atherosclerotic cardiovascular disease: Promise and possibilities. Atherosclerosis. (2018) 276:1–9. doi: 10.1016/j.atherosclerosis.2018.07.007
7. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for Atherosclerotic disease. N Engl J Med. (2017) 377:1119–31. doi: 10.1056/NEJMoa1707914
8. Ridker PM. From CANTOS to CIRT to COLCOT to clinic: will all atherosclerosis patients soon be treated with combination lipid-lowering and inflammation-inhibiting agents. Circulation. (2020) 141:787–9. doi: 10.1161/CIRCULATIONAHA.119.045256
9. Nidorf SM, Fiolet A, Mosterd A, Eikelboom JW, Schut A, Opstal TSJ, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. (2020) 383:1838–47. doi: 10.1056/NEJMoa2021372
10. Rymer JA, Newby LK. Failure to launch: targeting inflammation in acute coronary syndromes. JACC Basic Transl Sci. (2017) 2:484–97. doi: 10.1016/j.jacbts.2017.07.001
11. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. (2009). 151:264–9, W64. doi: 10.7326/0003-4819-151-4-200908180-00135
12. STABILITY Investigators, White HD, Held C, Stewart R, Tarka E, Brown R, et al. Darapladib for preventing ischemic events in stable coronary heart disease. N Engl J Med. (2014) 370:1702–11. doi: 10.1056/NEJMoa1315878
13. Ridker PM, Everett BM, Pradhan A, MacFadyen JG, Solomon DH, Zaharris E, et al. Low-dose methotrexate for the prevention of atherosclerotic events. N Engl J Med. (2019) 380:752–62. doi: 10.1056/NEJMoa1809798
14. Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. (2013) 61:404–10. doi: 10.1016/j.jacc.2012.10.027
15. Tong DC, Quinn S, Nasis A, Hiew C, Roberts-Thomson P, Adams H, et al. Colchicine in patients with acute coronary syndrome: the australian COPS randomized clinical trial. Circulation. (2020) 142:1890–900. doi: 10.1161/CIRCULATIONAHA.120.050771
16. O'Donoghue ML, Braunwald E, White HD, Lukas MA, Tarka E, Steg PG, et al. Effect of darapladib on major coronary events after an acute coronary syndrome: the SOLID-TIMI 52 randomized clinical trial. JAMA. (2014) 312:1006–15. doi: 10.1001/jama.2014.11061
17. O'Donoghue ML, Glaser R, Cavender MA, Aylward PE, Bonaca MP, Budaj A, et al. Effect of losmapimod on cardiovascular outcomes in patients hospitalized with acute myocardial infarction: a randomized clinical trial. JAMA. (2016) 315:1591–9. doi: 10.1001/jama.2016.3609
18. Shah B, Pillinger M, Zhong H, Aylward PE, Bonaca MP, Budaj A, et al. Effects of acute colchicine administration prior to percutaneous coronary intervention: COLCHICINE-PCI randomized trial. Circ Cardiovasc Interv. (2020) 13:e008717. doi: 10.1161/CIRCINTERVENTIONS.119.008717
19. Tardif JC, Tanguay JF, Wright SR, Duchatelle V, Petroni T, Grégoire JC, et al. Effects of the P-selectin antagonist inclacumab on myocardial damage after percutaneous coronary intervention for non-ST-segment elevation myocardial infarction: results of the SELECT-ACS trial. J Am Coll Cardiol. (2013) 61:2048–55. doi: 10.1016/j.jacc.2013.03.003
20. Rosenson RS, Hislop C, Elliott M, Stasiv Y, Goulder M, Waters D. Effects of varespladib methyl on biomarkers and major cardiovascular events in acute coronary syndrome patients. J Am Coll Cardiol. (2010) 56:1079–88. doi: 10.1016/j.jacc.2010.06.015
21. Abbate A, Trankle CR, Buckley LF, Lipinski MJ, Appleton D, Kadariya D, et al. Interleukin-1 blockade inhibits the acute inflammatory response in patients with ST-segment-elevation myocardial infarction. J Am Heart Assoc. (2020) 9:e014941. doi: 10.1161/JAHA.119.014941
22. APEX AMI Investigators, Armstrong PW, Granger CB, Adams PX, Hamm C, Holmes D Jr, et al. Pexelizumab for acute ST-elevation myocardial infarction in patients undergoing primary percutaneous coronary intervention: a randomized controlled trial. JAMA. (2007) 297:43–51. doi: 10.1001/jama.297.1.43
23. Granger CB, Mahaffey KW, Weaver WD, Theroux P, Hochman JS, Filloon TG, et al. Pexelizumab, an anti-C5 complement antibody, as adjunctive therapy to primary percutaneous coronary intervention in acute myocardial infarction: the COMplement inhibition in Myocardial infarction treated with Angioplasty (COMMA) trial. Circulation. (2003) 108:1184–90. doi: 10.1161/01.CIR.0000087447.12918.85
24. Morton AC, Rothman AM, Greenwood JP, Gunn J, Chase A, Clarke B, et al. The effect of interleukin-1 receptor antagonist therapy on markers of inflammation in non-ST elevation acute coronary syndromes: the MRC-ILA Heart Study. Eur Heart J. (2015) 36:377–84. doi: 10.1093/eurheartj/ehu272
25. Nicholls SJ, Kastelein JJ, Schwartz GG, Bash D, Rosenson RS, Cavender MA, et al. Varespladib and cardiovascular events in patients with an acute coronary syndrome: the VISTA-16 randomized clinical trial. JAMA. (2014) 311:252–62. doi: 10.1001/jama.2013.282836
26. Tardif JC Kouz S Waters DD Bertrand OF Diaz R Maggioni AP . Efficacy and Safety of Low-Dose Colchicine after Myocardial Infarction. N Engl J Med. (2019) 381:2497–505. doi: 10.1056/NEJMoa1912388
27. Abbate A, Kontos MC, Abouzaki NA, Melchior RD, Thomas C, Van Tassell BW, et al. Comparative safety of interleukin-1 blockade with anakinra in patients with ST-segment elevation acute myocardial infarction (from the VCU-ART and VCU-ART2 pilot studies). Am J Cardiol. (2015) 115:288–92. doi: 10.1016/j.amjcard.2014.11.003
28. Ridker PM. Anticytokine Agents: Targeting Interleukin Signaling Pathways for the Treatment of Atherothrombosis. Circ Res. (2019) 124:437–50. doi: 10.1161/CIRCRESAHA.118.313129
29. Lawler PR, Bhatt DL, Godoy LC, Lüscher TF, Bonow RO, Verma S, et al. Targeting cardiovascular inflammation: next steps in clinical translation. Eur Heart J. (2021) 42:113–31. doi: 10.1093/eurheartj/ehaa099
30. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation. (2019) 139:e1082–143. doi: 10.1161/CIR.0000000000000699
31. Bonaca MP, Nault P, Giugliano RP, Keech AC, Pineda AL, Kanevsky E, et al. Low-density lipoprotein cholesterol lowering with evolocumab and outcomes in patients with peripheral artery disease: insights from the FOURIER trial (further cardiovascular outcomes research with PCSK9 inhibition in subjects with elevated risk). Circulation. (2018) 137:338–50. doi: 10.1161/CIRCULATIONAHA.118.034864
32. Hemkens LG, Ewald H, Gloy VL, Arpagaus A, Olu KK, Nidorf M, et al. Colchicine for prevention of cardiovascular events. Cochrane Database Syst Rev. (2016) 2016:CD011047. doi: 10.1002/14651858.CD011047.pub2
33. Libby P, Tabas I, Fredman G, Fisher EA. Inflammation and its resolution as determinants of acute coronary syndromes. Circ Res. (2014) 114:1867–79. doi: 10.1161/CIRCRESAHA.114.302699
34. Frangogiannis NG. The inflammatory response in myocardial injury, repair, and remodelling. Nat Rev Cardiol. (2014) 11:255–65. doi: 10.1038/nrcardio.2014.28
35. Chaldakov GN. Anti-inflammatory drugs and ischemic heart disease: new considerations (a cell biologist's proposal to cardiologists). J Am Coll Cardiol. (1991) 17:1445–6. doi: 10.1016/S0735-1097(10)80161-5
36. Crea F, Libby P. Acute coronary syndromes: the way forward from mechanisms to precision treatment. Circulation. (2017) 136:1155–66. doi: 10.1161/CIRCULATIONAHA.117.029870
37. Chaldakov GN. Colchicine, a microtubule-disassembling drug, in the therapy of cardiovascular diseases. Cell Biol Int. (2018) 42:1079–84. doi: 10.1002/cbin.10988
38. Ma J, Chen X. Anti-inflammatory Therapy for Coronary Atherosclerotic Heart Disease: Unanswered Questions Behind Existing Successes. Front Cardiovasc Med. (2020) 7:631398. doi: 10.3389/fcvm.2020.631398
39. Vuoristo M, Färkkilä M, Karvonen AL, Leino R, Lehtola J, Mäkinen J, et al. A placebo-controlled trial of primary biliary cirrhosis treatment with colchicine and ursodeoxycholic acid. Gastroenterology. (1995) 108:1470–8. doi: 10.1016/0016-5085(95)90696-7
Keywords: anti-inflammatory therapy, coronary heart disease, residual inflammation risk, major cardiovascular events, meta-analysis
Citation: Wang H, Jiang M, Li X, Zhao Y, Shao J, Liu Z, Lin L, Xu Q, Wang L, Lu X, Zhang H, Chen Y and Zhang R (2021) Anti-inflammatory Therapies for Coronary Heart Disease: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 8:726341. doi: 10.3389/fcvm.2021.726341
Received: 22 June 2021; Accepted: 28 July 2021;
Published: 25 August 2021.
Edited by:
Dmitri Sviridov, Baker Heart and Diabetes Institute, AustraliaReviewed by:
George Nikov Chaldakov, Medical University of Varna, BulgariaCopyright © 2021 Wang, Jiang, Li, Zhao, Shao, Liu, Lin, Xu, Wang, Lu, Zhang, Chen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yundai Chen, Y3l1bmRhaUB2aXAuMTYzLmNvbQ==; Ran Zhang, Ymp6aGFuZ3JhbkAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.