
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 24 September 2021
Sec. Cardiovascular Imaging
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.726307
This article is part of the Research Topic Multimodality Imaging in Acute Coronary Syndrome View all 21 articles
 Hongli Hou1,2
Hongli Hou1,2 Qi Zhao3
Qi Zhao3 Chao Qu4
Chao Qu4 Meng Sun5
Meng Sun5 Qi Liu1
Qi Liu1 Xingtao Huang1
Xingtao Huang1 Xuedong Wang1
Xuedong Wang1 Ruoxi Zhang1*
Ruoxi Zhang1* Lifeng Du6
Lifeng Du6 Jingbo Hou1*
Jingbo Hou1* Bo Yu1
Bo Yu1Introduction: It has been reported that sex has well-established relationships with the prevalence of coronary artery disease (CAD) and the major adverse cardiovascular events. Compared with men, the difference of coronary artery and myocardial characteristics in women has effects on anatomical and functional evaluations. Quantitative flow ratio (QFR) has been shown to be effective in assessing the hemodynamic relevance of lesions in stable coronary disease. However, its suitability in acute myocardial infarction patients is unknown. This study aimed to evaluate the sex differences in the non-infarct-related artery (NIRA)-based QFR in patients with ST-elevation myocardial infarction (STEMI).
Methods: In this study, 353 patients with STEMI who underwent angiographic cQFR assessment and interventional therapy were included. According to contrast-flow QFR (cQFR) standard operating procedures: reliable software was used to modeling the hyperemic flow velocity derived from coronary angiography in the absence of pharmacologically induced hyperemia. 353 patients were divided into two groups according to sex. A cQFR ≤0.80 was considered hemodynamically significant, whereas invasive coronary angiography (ICA) luminal stenosis ≥50% was considered obstructive. Demographics, clinical data, NIRA-related anatomy, and functional cQFR values were recorded. Clinical outcomes included the NIRA reclassification rate between men and women, according to the ICA and cQFR assessments.
Results: Women were older and had a higher body mass index (BMI) than men. The levels of diastolic blood pressure, troponin I, peak creatine kinase-MB, low-density lipoprotein cholesterol, N terminal pro B-type natriuretic peptide, stent diameter, and current smoking rate were found to be significantly lower in the female group than in the male group. Women had a lower likelihood of a positive cQFR ≤0.80 for the same degree of stenosis and a lower rate of NIRA revascularization. Independent predictors of positive cQFR included male sex and diameter stenosis (DS) >70%.
Conclusions: cQFR values differ between the sexes, as women have a higher cQFR value for the same degree of stenosis. The findings suggest that QFR variations by sex require specific interpretation, as these differences may affect therapeutic decision-making and clinical outcomes.
Coronary artery disease (CAD) is the leading cause of death globally, with the majority of affected individuals dying of acute myocardial infarction (1). Evidence from pathologic studies suggest that there are significant differences in coronary obstructive lesions between man and women (2, 3). Women are diagnosed with CAD at a greater age compared to men. In addition, women diagnosed with CAD have specific clinical symptoms, lower cardiovascular risk assessment scores, and a lower incidence of obstructive coronary heart disease, however, they appear to have a worse prognosis. Studies have shown lower utilization of conventional non-invasive imaging in female patients with suspected diagnosis of CAD, which may be related to breast attenuation, the decrease of peak exercise ability, small body size, and lower incidence of obstructive CAD (4). Therefore, sex-specific strategies and interpretations are recommended in the guidelines (5).
More recent evidence suggests that patients with non-infarct-related artery disease (NIRA) may in fact have a worse prognosis, including a higher 30-day mortality, than patients without NIRA disease (6). In addition, there is a lack of consensus regarding the treatment approach (aggressive vs. conservative) that should be implemented in these patients with NIRA disease. For some special research projects, patients with ST-elevation myocardial infarction (STEMI) underwent complete revascularization show lower rates of major cardiovascular events than infarct-related artery (IRA)-only revascularization (7, 8).
In recent years, fractional flow reserve (FFR) testing has become an important step in flow reconstruction decisions in patients with CAD, with the aim of assessing the functional significance of epicardial coronary stenosis on angiography.
Studies have shown that the choice of an FFR-based revascularization strategy is superior to percutaneous coronary intervention (PCI) for infarct-related vessels alone, both in STEMI procedure or in a staged manner (9, 10). However, the cost of the pressure wire and limitations associated with the induction of hyperemia have limited the wide application of FFR. A novel practical tool which calculates FFR indirectly and guides revascularization decision-making without a pressure wire or hyperemic induction was established. Recent studies have shown that the contrast-flow quantitative flow ratio (cQFR) can accurately and reproductively predict FFR values (11). Mechanically, the cQFR was calculated based on a contrast-flow hyperemic flow velocity model derived from coronary angiography without pharmacologically induced hyperemia. The accuracy of the cQFR in comparison with the conventional FFR has already been reported (12), and the software for the cQFR measurement is now commercially available.
Therefore, study aimed to evaluate the sex differences in the NIRA-based cQFR in patients with STEMI. We hypothesized that sex differences in NIRA might be related to the difference in revascularization decision-making based on the quantitative flow ratio (QFR) in patients with STEMI.
This study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, as reflected in a priori approval from the institution's human research committee. This study was also approved by the Research Ethics Committee of the 2nd Affiliated Hospital of Harbin Medical University, China. Informed consent was obtained from all patients.
We identified 353 patients admitted for STEMI who underwent angiographic QFR assessment and interventional therapy at the 2nd Affiliated Hospital of Harbin Medical University between January 2018 and December 2019. The inclusion criteria were as follows: (1) patients presenting within 12 h of symptom onset, defined as typical chest pain lasting for >30 min; (2) ST-segment elevation ≥1 mm in two contiguous electrocardiographic leads or new onset of complete left bundle branch block; and (3) primary PCI including balloon angioplasty, thrombus aspiration, and/or stent implantation. The exclusion criterion included any chronic illness, such as cancer, liver cirrhosis, heart failure, or end-stage renal failure (13).
All primary PCIs were performed at our hospital [Department of Cardiology, The 2nd Affiliated Hospital of Harbin Medical University, a single tertiary interventional treatment center [>5,000 PCI cases per year]] by experienced interventional cardiologists, with experience with >1,000 PCI cases per year, who were not involved in the present study (13, 14). Baseline demographics and angiographic characteristics, as well as laboratory and physical examination data during hospitalization, were recorded by systematically reviewing the patients' files.
Primary PCI was usually performed using the percutaneous radial artery approach; the femoral approach was used when an intra-aortic balloon pump needed to be inserted. All patients' angiographic data from catheterization laboratory records were assessed using the conventional technique. The target artery was defined as clinically significant when vessel stenosis was ≥50%. Blood flow in the IRA that received only primary PCI was graded based on the thrombolysis in myocardial infarction (TIMI) grade. A chewable loading dose of 300 mg of aspirin and 600 mg of clopidogrel was administered before PCI. Success of the procedure was defined as <20% stenosis of the IRA with TIMI grade III flow after primary PCI. Post-operatively, all patients were transferred to our cardiac care unit and received standard treatment for STEMI, which consisted of 100 mg of aspirin, 20 mg of atorvastatin, and 75 mg of clopidogrel once a day (15).
Three-dimensional quantitative coronary angiography (QCA) and QFR analyses were performed by an independent core laboratory with dedicated software (QAngio XA 3D prototype, Medis special by, Leiden, the Netherlands) (Figures 1A–D). Briefly, end-diastolic frames of two optimal angiography projections, which were separated with angles of at least 25°, were selected and used for three-dimensional model reconstruction. Fifteen frames/second acquisition in our software that performs QFR was require. The three-dimensional contour model of the segment of interest and its reference vessel were constructed in an automated manner, and manual correction of the contour was performed. After acquisition of the fixed QFR, estimated contrast coronary flow was calculated using the TIMI frame-count adjustment, which indicated the frames where contrast entered and exited the segmented part of the vessel (12). With the application of the TIMI frame-count adjustment in the calculation method, the software automatically calculated the cQFR value. The cutoff value of the cQFR ≤0.80 was used in the current study (16).
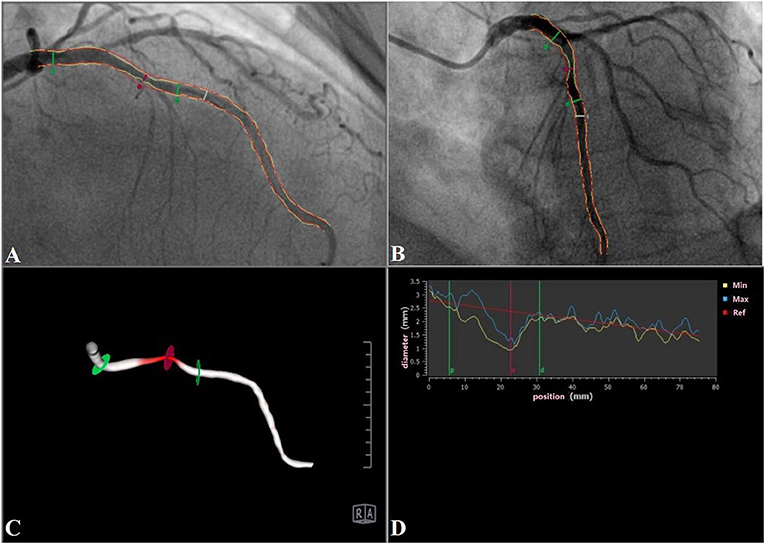
Figure 1. A representative case of LAD (cQFR = 0.71). (A,B) Two-dimensional images; (C) three-dimensional reconstruction (right anterior oblique 50°, caudal 9°); (D) diameter diagram. LAD, left anterior descending artery; cQFR, contrast-flow quantitative flow ratio.
Venous blood was collected from all patients within 72 h of hospitalization. N terminal pro B-type natriuretic peptide (NT-proBNP), creatine kinase-MB (CK-MB), and troponin I levels were measured daily. Blood samples were collected on admission and at 24 and 48 h in every patient. Plasma NT-proBNP levels were measured using an Elecsys 2010 analyzer, a commercially available electrochemiluminescent sandwich immunoassay (Elecsys proBNP; Roche Diagnostics, Mannheim, Germany) (14). High-sensitivity-C-reactive protein levels were measured using a commercially available immunonephelometric kinetic assay (BN ProSpec; Siemens, Tarrytown, NY, USA). The 12-h fasting serum levels of triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were measured using standard methods (15). Other biochemical measurements were performed using the standard methods.
Reperfusion time was defined as the symptom-to-balloon time, and the door-to-balloon time was defined as the time between hospitalization and balloon dilation (14). Diabetes mellitus was diagnosed when a patient was on insulin or oral hypoglycemic drugs or in patients not on insulin or oral hypoglycemic drugs but with a casual plasma glucose level >11.1 mmol/L, fasting plasma glucose level >7 mmol/L, or glycated A1c hemoglobin level >6.5%. Hypertension was diagnosed when the systolic arterial pressure was >140 mmHg and/or diastolic arterial pressure was >90 mmHg, and when the patient had been on antihypertensive drugs for a long time. Hyperlipidemia was defined as a fasting total serum cholesterol level >5.17 mmol/L, LDL-C level >3.15 mmol/L, or serum triglyceride level >1.70 mmol/L, or if the patient was on lipid-lowering agents owing to a medical history of hypercholesterolemia (15). Smoking was defined as current regular use of cigarettes or if the patient had quit smoking within the previous year. Cardiac function deterioration was defined as New York Heart Association (NYHA) functional class leveled up in follow-up compared to in hospital.
Quantitative variables are expressed as the mean ± standard deviation, and qualitative variables are expressed as the total number and percentage. The independent two-sample t-test was used to assess the differences between multiple sets of data. Categorical variables were compared using the chi-square or Fisher exact tests. Independent predictors of NIRA revascularization were identified using multivariate logistic regression analysis. Statistical significance was defined as a two-sided p-value <0.05. All statistical analyses were performed using SPSS version 19.0 (IBM Corp., Armonk, NY, USA).
In our single-center study, we initially screened 515 STEMI patients who underwent angiographic QFR assessment between January 2018 and December 2019. One hundred and sixty-two patients with angiography were excluded because of limited quality of the images or inappropriate angle of projections. A total of 353 patients (224 men and 129 women) were enrolled in the study. Patients were categorized into two groups according to different sex. The baseline demographic and angiographic characteristics of the two groups are presented in Tables 1, 2, respectively. Compared to men, women were older and had a higher body mass index (BMI). The levels of diastolic blood pressure, troponin I, peak CK-MB, LDL cholesterol, and NT-proBNP, stent diameter, and current smoking rate were found to be significantly lower in the female group than in the male group.
There was no significant statistical difference in each anatomical stenosis group (Table 3). Compared to men, women had a lower likelihood of a positive cQFR ≤0.80, a higher cQFR value in similar range of diameter stenosis (DS) (DS ≤30% and DS >70%), and a higher diameter stenosis while cQFR >0.80 (Figure 2). Multivariate logistic regression analysis showed that male sex [odds ratio [OR] = 2.240, 95% confidence interval [CI]: 1.237–3.941, P = 0.005], and DS >70% (OR = 9.407, 95% CI: 2.709–23.178, P = 0.001) were independently associated with positive cQFR (Table 4).
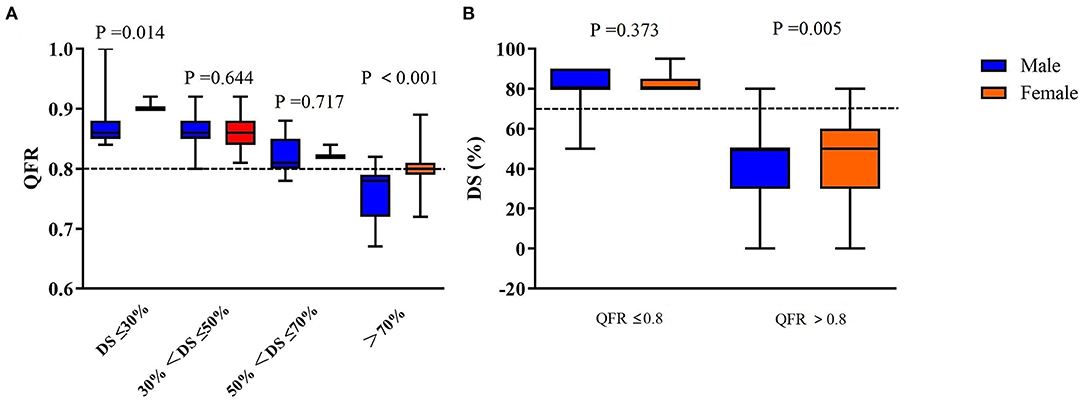
Figure 2. (A) cQFR values according to the severity of ICA stenosis. (B) Box-plot relationship of the anatomical degree of stenosis and cQFR values for men and women in the obstructive CAD categories. QFR, quantitative flow ratio; ICA, invasive coronary angiography; CAD, coronary artery disease; DS, diameter stenosis.
One-year follow-up the cardiac function deterioration events was trendly, but not significantly, higher in male group compared to female group (81.0 vs. 93.2%, P = 0.389; Figure 3).
QCA plays an important role in evaluating the degree of coronary artery stenosis and guiding the operation of PCI (17). However, limitations of anatomy-based techniques have required for a novel physiological technology to assess the severity of coronary stenosis (18, 19). The deep understanding of the anatomy and physiology of coronary circulation is necessary for clinical doctors to assess the hemodynamic consequences of epicardial stenosis and discover the personal clinical treatment strategy (20).
In fact, the adoption rates of invasive FFR-guided PCI remain low in real-world practice (21). In recent years, functional coronary imaging has been progressively applied, which is a new method based on mathematical assumptions of computational fluid dynamics models or coronary blood flow and thus assessing the degree of coronary artery stenosis (22). QFR is a three-dimensional QCA-based computation of FFR, moreover, previous studies have demonstrated excellent correlations and diagnostic agreements with FFR (23, 24). In addition, in some proof-of-concept studies, compared with FFR, QFR showed same excellent diagnostic ability whether in the acute physiological evaluation of non-culprit lesions in patients with STEMI or multivessel disease (25, 26).
Studies have shown that QFR showed good diagnostic agreement with FFR measured in the acute physiological evaluation of non-culprit lesions in patients with ST-segment elevation myocardial infarction (STEMI) and multivessel disease (26). To the best of our knowledge, this is the first time to investigate sex differences in NIRA-based QFR among patients with STEMI. Our results demonstrated several important sex-related differences. Compared to men, women have an inherently higher QFR value, independent of anatomical stenosis, and are less likely to receive revascularization of the NIRA. In the FAME substudy, it was found that the FFR value in women was 0.75 ± 0.18, whereas that in men was 0.71 ± 0.17 (P = 0.001). It is also reported that the proportion of functionally significant stenoses, defined as FFR <0.80, was lower in women than in men (27). For the patient cohort in our study, one-third of the patients were women. Compared to men, women were older, characteristic with higher BMI, and less cardiovascular risk factors (smoking, hypertension, and hypercholesterolemia). The above situation led to women might present with a lower number of coronary segments containing calcified or mixed plaques than men. Previous studies have highlighted sex differences in coronary stenoses, coronary plaque burden, and plaque composition, which may impact functional stenosis evaluation (28). For example, women presented with a lower number of coronary segments containing calcified or mixed plaques than men (29). In some quantitative and qualitative plaque characteristics studies, the number of high-risk plaque characteristics increased with decrease in FFR, and vice versa. Physiological disease burden (FFR) and the number of high-risk plaque characteristics were closely related, and both components had significant association with the risk of clinical events (28, 29). Furthermore, microvascular dysfunction is the most recognized reason for the higher FFR value in women, which is assessed by the coronary flow reserve, and it was reported to be more frequent in women than in men (30, 31). Accordingly, the blunted hyperemic response is considered as the major reason for the higher FFR value in women (20). Besides, compared with man, the smaller heart and myocardial perfusion territories are also important factors that cannot be ignored (32), which result in a relatively lower myocardial mass to coronary volume in women and a higher FFR value compared to men.
As expected in instances of disease severity, our results demonstrate that the average of QFR significantly higher in women, but importantly, the proportion of QFR-positive stenoses was also lower in women than in men (17.05 vs. 36.61%, P < 0.001). These results are highly consistent with those of the invasive Fractional Flow Reserve vs. Angiography for Multivessel Evaluation substudy (27). This difference in the sex-specific QFR/FFR offers new insights that may help to determine the appropriate treatment for women with CAD on interventional therapy. Our results emphasize that a high QFR value in women predicts a reduced likelihood of revascularization. Thus, our study confirms our hypothesis that sex differences in NIRA might be related to the difference in revascularization decision-making based on the QFR in patients with STEMI. Furthermore, because of women have a higher intrinsic FFR value, special consideration is required during PCI procedure: the strategies for revascularization need to be considered from multiple perspectives rather than using dichotomous cutoffs for invasive or non-invasive FFR (4). In our study, actual NIRA management for 90 days showed that women were more likely to receive medical treatment than men (83.70 vs. 66.52%, P < 0.001), and men were more likely to undergo NIRA revascularization than women (33.48 vs. 16.30%, P < 0.001). Therefore, the knowledge that women have a higher intrinsic physiological test value requiring special consideration, leading to suggestions that decisions of revascularization need to be nuanced and multifaceted rather than using dichotomous cutoffs for cQFR.
In previous studies, beyond sex and (as expected) % degree of stenosis, age, the presence of diabetes and vessel under study also showed a weak independent association with FFR data (33). In our study, female sex was significantly associated with positive cQFR after adjustment by DS (Table 4). In follow-up data, cardiac function deterioration rates were trendly, but not significantly, higher in male group compared to female group. There was also paradox that exists in female CAD, characterized by a lower prevalence of obstructive disease but higher prevalence of clinical presentation, ischemia, symptomatic complaints, complications and mortality compared to men (34). However, this difference in sex did not translate into a difference in cardiac function in our study. This might be due to recent advances in revascularization techniques, stent technology and medical therapies and the relatively low-risk population of this study.
The present study has some limitations. First, the number of patients was relatively small. There is a possibility of significant referral bias because of the retrospective and single-center design of the study. Second, we didn't measurement microvascular dysfunction, which leads to a lack of clarity understanding the differences in FFR values between men and women. Third, neither the physicians nor the patients were blinded to the QFR results and whether revascularization was performed. Finally, there is relatively insufficient in data on long-term events and follow-up, and we plan to include this information in a future study.
There is significant different in QFR values between the male and female, as women have higher QFR values for the same degree of stenosis than men. Our findings suggest that QFR variations by sex needs more clinical and basic studies to explain the reasons, as these differences may affect clinical treatment strategy and long-term prognosis. However, the relative paucity of data supports the use of QFR at the NIRA in STEMI, and further investigation of the reliability of the non-culprit vessel QFR in this clinical setting is warranted.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Research Ethics Committee of the 2nd Affiliated Hospital of Harbin Medical University. The patients/participants provided their written informed consent to participate in this study.
HH, RZ, JH, and BY were responsible for the conception and design of the study. HH, RZ, QZ, QL, XW, and XH contributed substantially to data acquisition. HH, QZ, CQ, QL, XW, LD, and XH contributed to data interpretation. MS was responsible for statistical analysis. HH and RZ drafted and revised the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (grant nos. 81900309 to QL; 81801803 to XH; 82000330 to XW; and 8197020581 to JH), China Postdoctoral Science Foundation (grant nos. 2019M661306 to QL and 2018M640310 to XH), and Heilongjiang Postdoctoral Science Foundation (grant no. LBH-Z19032 to XH).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.726307/full#supplementary-material
1. Goff Dc Jr, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. (2014) 129 (25 Suppl. 2):S49–73. doi: 10.1161/01.cir.0000437741.48606.98
2. Mautner SL, Lin F, Mautner GC, Roberts WC. Comparison in women versus men of composition of atherosclerotic plaques in native coronary arteries and in saphenous veins used as aortocoronary conduits. J Am Coll Cardiol. (1993) 21:1312–8. doi: 10.1016/0735-1097(93)90302-H
3. Burke AP, Farb A, Malcom GT, Liang Y, Smialek J, Virmani R. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation. (1998) 97:2110–6. doi: 10.1161/01.CIR.97.21.2110
4. Fairbairn TA, Dobson R, Hurwitz-Koweek L, Matsuo H, Norgaard BL, Rønnow Sand NP, et al. Sex differences in coronary computed tomography angiography-derived fractional flow reserve: lessons from ADVANCE. JACC Cardiovasc Imaging. (2020) 13:2576–87. doi: 10.1016/j.jcmg.2020.07.008
5. Mieres JH, Gulati M, Merz NB, Berman DS, Gerber TC, Hayes SN, et al. Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease: a consensus statement from the American Heart Association. Circulation. (2014) 130:350–79. doi: 10.1161/CIR.0000000000000061
6. Park D-W, Clare RM, Schulte PJ, Pieper KS, Shaw LK, Califf RM, et al. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA. (2014) 312:2019–27. doi: 10.1001/jama.2014.15095
7. Wald DS, Morris JK, Wald NJ, Chase AJ, Edwards RJ, Hughes LO, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. (2013) 369:1115–23. doi: 10.1056/NEJMoa1305520
8. Gershlick AH, Khan JN, Kelly DJ, Greenwood JP, Sasikaran T, Curzen N, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. (2015) 65:963–72. doi: 10.1016/j.jacc.2014.12.038
9. Smits PC, Abdel-Wahab M, Neumann F-J, Boxma-de Klerk BM, Lunde K, Schotborgh CE, et al. Fractional flow reserve-guided multivessel angioplasty in myocardial infarction. N Engl J Med. (2017) 376:1234–44. doi: 10.1056/NEJMoa1701067
10. Engstrøm T, Kelbæk H, Helqvist S, Høfsten DE, Kløvgaard L, Holmvang L, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. (2015) 386:665–71. doi: 10.1016/S0140-6736(15)60648-1
11. Tu S, Barbato E, Köszegi Z, Yang J, Sun J, Holm NR, et al. Fractional flow reserve calculation from 3-dimensional quantitative coronary angiography and TIMI frame count: a fast computer model to quantify the functional significance of moderately obstructed coronary arteries. JACC Cardiovasc Interv. (2014) 7:768–77. doi: 10.1016/j.jcin.2014.03.004
12. Tu S, Westra J, Yang J, von Birgelen C, Ferrara A, Pellicano M, et al. Diagnostic accuracy of fast computational approaches to derive fractional flow reserve from diagnostic coronary angiography: the international multicenter FAVOR pilot study. JACC Cardiovasc Interv. (2016) 9:2024–35. doi: 10.1016/j.jcin.2016.07.013
13. Jiang Z, Zhang R, Sun M, Liu Q, Wang S, Wang W, et al. Effect of clopidogrel vs ticagrelor on platelet aggregation and inflammation markers after percutaneous coronary intervention for ST-elevation myocardial infarction. Can J Cardiol. (2018) 34:1606–12. doi: 10.1016/j.cjca.2018.08.024
14. Zhang R, Chen S, Zhao Q, Sun M, Yu B, Hou J. Fragmented QRS complex is a prognostic marker of microvascular reperfusion and changes in LV function occur in patients with ST elevation myocardial infarction who underwent primary percutaneous coronary intervention. Exp Ther Med. (2017) 13:3231–8. doi: 10.3892/etm.2017.4380
15. Zhao Q, Zhang R, Hou J, Yu B. Relationship between fragmented QRS and NT-proBNP in patients with ST elevation myocardial infarction who underwent primary percutaneous coronary intervention. Acta Cardiol Sin. (2018) 34:13–22. doi: 10.6515/ACS.201801_34(1).20170903A
16. Xu B, Tu S, Qiao S, Qu X, Chen Y, Yang J, et al. Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis. J Am Coll Cardiol. (2017) 70:3077–87. doi: 10.1016/j.jacc.2017.10.035
17. Collet C, Grundeken MJ, Asano T, Onuma Y, Wijns W, Serruys PW. State of the art: coronary angiography. EuroIntervention. (2017) 13:634–43. doi: 10.4244/EIJ-D-17-00465
18. White CW, Wright CB, Doty DB, Hiratza LF, Eastham CL, Harrison DG, et al. Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med. (1984) 310:819–24. doi: 10.1056/NEJM198403293101304
19. Lance Gould K, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. (2013) 62:1639–53. doi: 10.1016/j.jacc.2013.07.076
20. Crystal GJ, Klein LW. Fractional flow reserve: physiological basis, advantages and limitations, and potential gender differences. Curr Cardiol Rev. (2015) 11:209–19. doi: 10.2174/1573403X10666141020113318
21. Dehmer GJ, Weaver D, Roe MT, Milford-Beland S, Fitzgerald S, Hermann A, et al. A contemporary view of diagnostic cardiac catheterization and percutaneous coronary intervention in the United States: a report from the CathPCI Registry of the National Cardiovascular Data Registry, 2010 through June 2011. J Am Coll Cardiol. (2012) 60:2017–31. doi: 10.1016/j.jacc.2012.08.966
22. Hwang D, Choi KH, Lee JM, Mejía-Rentería H, Kim J, Park J, et al. Diagnostic agreement of quantitative flow ratio with fractional flow reserve and instantaneous wave-free ratio. J Am Heart Assoc. (2019) 8:e011605. doi: 10.1161/JAHA.118.011605
23. Collet C, Onuma Y, Sonck J, Asano T, Vandeloo B, Kornowski R, et al. Diagnostic performance of angiography-derived fractional flow reserve: a systematic review and Bayesian meta-analysis. Eur Heart J. (2018) 39:3314–21. doi: 10.1093/eurheartj/ehy445
24. Westra J, Andersen BK, Campo G, Matsuo H, Koltowski L, Eftekhari A, et al. diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve: the FAVOR II Europe-Japan study. J Am Heart Assoc. (2018) 7:e009603. doi: 10.1161/JAHA.118.009603
25. Sejr-Hansen M, Westra J, Thim T, Christiansen EH, Eftekhari A, Kristensen SD, et al. Quantitative flow ratio for immediate assessment of nonculprit lesions in patients with ST-segment elevation myocardial infarction-An iSTEMI substudy. Catheter Cardiovasc Interv. (2019) 94:686–92. doi: 10.1002/ccd.28208
26. Spitaleri G, Tebaldi M, Biscaglia S, Westra J, Brugaletta S, Erriquez A, et al. Quantitative flow ratio identifies nonculprit coronary lesions requiring revascularization in patients with ST-segment-elevation myocardial infarction and multivessel disease. Circ Cardiovasc Interv. (2018) 11:e006023. doi: 10.1161/CIRCINTERVENTIONS.117.006023
27. Kim H-S, Tonino PAL, De Bruyne B, Yong ASC, Tremmel JA, Pijls NHJ The impact of sex differences on fractional flow reserve-guided percutaneous coronary intervention: a FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) substudy. JACC Cardiovasc Interv. (2012) 5:1037–42. doi: 10.1016/j.jcin.2012.06.016
28. Lee JM, Choi KH, Koo BK, Park J, Kim J, Hwang D, et al. Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J Am Coll Cardiol. (2019) 73:2413–24. doi: 10.1016/j.jacc.2019.02.060
29. Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. (2015) 372:1291–300. doi: 10.1056/NEJMoa1415516
30. NoelBairey Merz C, Shaw LJ, Reis SE, Bittner V, Kelsey SF, Olson M, et al. Insights from the NHLBI-sponsored women's ischemia syndrome evaluation (WISE) study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol. (2006) 47(3 Suppl.):S21–9. doi: 10.1016/j.jacc.2004.12.084
31. Reis SE, Holubkov R, Conrad Smith AJ, Kelsey SF, Sharaf BL, Reichek N, et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am Heart J. (2001) 141:735–41. doi: 10.1067/mhj.2001.114198
32. Lin FY, Devereux RB, Roman MJ, Meng J, Jow VM, Jacobs A, et al. Cardiac chamber volumes, function, and mass as determined by 64-multidetector row computed tomography: mean values among healthy adults free of hypertension and obesity. JACC Cardiovasc Imaging. (2008) 1:782–6. doi: 10.1016/j.jcmg.2008.04.015
33. Fineschi M, Guerrieri G, Orphal D, Palmerini E, Münzel T, Warnholtz A, et al. The impact of gender on fractional flow reserve measurements. EuroIntervention. (2013) 9:360–6. doi: 10.4244/EIJV9I3A58
34. Baumann S, Renker M, Schoepf UJ, De Cecco CN, Coenen A, De Geer J, et al. Gender differences in the diagnostic performance of machine learning coronary CT angiography-derived fractional flow reserve -results from the MACHINE registry. Eur J Radiol. (2019) 119:108657. doi: 10.1016/j.ejrad.2019.108657
Keywords: gender differences, non-infarct-related artery, ST-elevation myocardial infarction, quantitative flow ratio, revascularization
Citation: Hou H, Zhao Q, Qu C, Sun M, Liu Q, Huang X, Wang X, Zhang R, Du L, Hou J and Yu B (2021) Sex Differences in the Non-infarct-Related Artery-Based Quantitative Flow Ratio in Patients With ST-Elevation Myocardial Infarction: A Retrospective Study. Front. Cardiovasc. Med. 8:726307. doi: 10.3389/fcvm.2021.726307
Received: 16 June 2021; Accepted: 31 August 2021;
Published: 24 September 2021.
Edited by:
Zhao Wang, University of Electronic Science and Technology of China, ChinaReviewed by:
Krishnaraj Sinhji Rathod, Queen Mary University of London, United KingdomCopyright © 2021 Hou, Zhao, Qu, Sun, Liu, Huang, Wang, Zhang, Du, Hou and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingbo Hou, amluZ2JvaG91QDE2My5jb20=; Ruoxi Zhang, ODk4NzE3MzcyQHFxLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.