
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Cardiovasc. Med. , 13 December 2021
Sec. Coronary Artery Disease
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.720597
 Wen-Jing Zhang1,2
Wen-Jing Zhang1,2 Gang-Qiong Liu1,2
Gang-Qiong Liu1,2 Jia-Hong Shangguan1,2
Jia-Hong Shangguan1,2 Xiao-Dan Zhu1,2
Xiao-Dan Zhu1,2 Wei Wang3
Wei Wang3 Qian-Qian Guo1,2
Qian-Qian Guo1,2 Jian-Chao Zhang1,2
Jian-Chao Zhang1,2 Kai Wang1,2
Kai Wang1,2 Zhi-Yu Liu1,2
Zhi-Yu Liu1,2 Feng-Hua Song1,2
Feng-Hua Song1,2 Lei Fan1,2
Lei Fan1,2 Ling Li1*
Ling Li1* Ying-Ying Zheng1,2*
Ying-Ying Zheng1,2* Jin-Ying Zhang1,2*
Jin-Ying Zhang1,2*Objectives: A novel AFR– albumin-derived neutrophil to lymphocyte ratio (dNLR) score (ADS) were reported to associate with clinical outcome in various malignancies, However, the relation between the ADS score and outcomes in coronary artery disease (CAD) patients after percutaneous coronary intervention (PCI) has not been investigated.
Methods: Three thousand five hundred and sixty-one patients were divided into two groups according to ADS score: low group (ADS score <2; n = 2,682) and high group (ADS score ≥ 2; n = 879). Overall, there were 133 all-cause mortality (ACM) during the following up. The incidence of ACM in the low group is 2.7% (72/2,682) and high group is 6.9% (61/879). The ACM incidence was significantly higher in high group compared to that in the low group (P < 0.001). Cardiac mortality (CM) occurred in 82 patients: 44(1.6%) in the low group and 38 (4.3%) in the high group. There was significant difference in the CM incidence between the low group and high group (P < 0.001). Major adverse cardiac and cerebrovascular events (MACCE) occurred in 520 patients: 366 (13.6%) in the low group and 154 (17.5%) in the high group. There was significant difference in the MACCE incidence between the low group and high group (P = 0.005). Major adverse cardiac and events (MACE) occurred in 395 patients: 281(10.5%) in the low group and 114 (13.0%) in the high group. There was significant difference in the MACE incidence between the low group and high group (P = 0.041). The multivariate Cox proportional hazards model showed that ADS score was independently correlated with the ACM [adjusted HR = 2.031 (1.357–3.039), P = 0.001]; CM [adjusted HR = 1.883 (1.127–3.147), P = 0.016]; MACCE [adjusted HR = 1.352 (1.096–1.668), P = 0.005], and MACE [adjusted HR = 1.260 (0.987–1.608), P = 0.063].
Conclusion: The present study indicated that the ADS score was associated with long-term mortality, the MACCE, and the MACE in CAD patients underwent PCI.
Chronic inflammation is considered to play a significant role on the occurrence and development of coronary artery disease (CAD) (1–4). There are a series of biomarkers of systematic inflammation such as inflammation-related immune cell and acute-phase reactive protein (5, 6). The levels of these biomarkers can reflect the degree of chronic inflammation in CAD patients. Previously, several inflammatory biomarkers, such as neutrophil to lymphocyte ratio (NLR) (7, 8), derived neutrophil to lymphocyte ratio (dNLR), fibrinogen (Fib) (9–12), and albumin (Alb) (13, 14), have been reported to be associated with the progress and prognosis of CAD. Fib is one of the vital elements in the coagulation cascade, and hypercoagulation is commonly occurred in CAD patients (15). Meanwhile, hypoalbuminemia was reported to be associated with outcomes of CAD (13, 14). Previous studies also suggested the ratio of Fib to albumin (FAR) was an independent predictor of CAD after percutaneous coronary intervention (PCI) (11, 16).
Previously, Gao et al. (17) developed a novel score system named ADS score which was composed of FAR, Alb, and dNLR to predict the prognosis of esophageal squamous cell carcinoma. As described above, all FAR, dNLR, and Alb were associated with the outcomes of CAD patients who underwent PCI. However, the association of ADS with prognosis of CAD patients has not been investigated up to date. In the present study, we investigated the predictive value of ADS score for the outcomes of CAD patients who underwent PCI.
This study was a single-center retrospective cohort study that investigated the clinical outcomes and risk factors for patients with CAD after PCI (CORFCHD-ZZ, identifier: ChiCTR1800019699). In this study, 3,561 CAD patients who underwent PCI were enrolled and their clinical, angiographic, short-term, and long-term outcome data were collected. All the patients were from the First Affiliated Hospital of Zhengzhou University from 2013 to 2017. The selected criterion for CAD was at least one coronary artery diameter stenosis ≥70%, as confirmed on coronary angiography. An experienced cardiologist performed PCI. We divided these patients into two groups according to ADS score: lower group: ADS <2 (n = 2,682) and higher group: ADS ≥2 (n = 879). A flow chart of inclusion of the patients was shown in Figure 1.
ADS score was established according to the previous study (17). Complete blood cell counts, such as total white blood cells, hemoglobin, neutrophils, platelets, lymphocytes, and monocytes were measured with an auto analyzer. Serum albumin levels were measured using a Roche Diagnostics Cobas 8000 c502 analyzer (Roche Holding AG, Basel, Switzerland). The normal range was 35–52 g/L. The calculation of AFR and dNLR was conducted according to the previous methods (11, 18). Levels of Alb, AFR, and dNLR which were higher or lower than the cut-off values were considered as 0 and 1 point, respectively. The total points with <2 and ≥2 were defined as low and high ADS score, respectively.
The general demographic data, such as smoking, drinking, past medical history, cardiovascular risk factors, and laboratory-related tests were collected. All laboratory-related tests were performed on the second day after admission after fasting for at least 12 h. Serum concentrations of parameters representing liver function, kidney function, and blood lipid profiles were measured using the equipment for chemical analysis (Dimension AR/AVL Clinical Chemistry System, Newark, NJ, USA) employed by the Clinical Laboratory Department of the First Affiliated Hospital of Zhengzhou University.
In the present study, we defined hypertension as blood pressure ≥140/90 mmHg at three different times on the same day or treatment with antihypertensive drugs. The diagnostic criteria for diabetes was a clear history of diabetes, the use of hypoglycemic agents, fasting blood glucose ≥7.1 mmol/L, or 2 h post-load glucose ≥11.1 mmol/L. Persons reporting regular tobacco use in the previous 6 months were considered current smokers. Persons who were ingesting alcohol in the last 6 months were considered alcohol users. All the definitions were established according to the previous study (19).
Coronary angiography, interventional therapy, and post-operative reports were performed by experienced coronary intervention specialists. Patients with CAD who underwent PCI received a loading dose of DAPT (300 mg of aspirin and 300 mg of clopidogrel), and intravenous heparin anticoagulation was routinely used before PCI.
The primary endpoint of the study was long-term mortality, including all-cause mortality (ACM), defined as death caused by any reason and cardiac mortality (CM), death due to coronary heart disease, cardiogenic shock, or sudden death. A combination of cardiac death, recurrent myocardial infarction, and target vessel reconstruction was defined major adverse cardiac events (MACEs) which was one of the secondary endpoints. The major adverse cardiac and cerebrovascular events (MACCEs), which were defined as a combination of cardiac death, recurrent myocardial infarction, target vessel reconstruction, and stroke, as described previously (19).
The follow-up was performed by specially trained professional staff. All patients were followed via outpatient, inpatient, and telephone follow-up and with questionnaire surveys. The mean follow-up time was 37.59 ± 22.24 months.
The SPSS 22.0 for Windows statistical software (SPSS Inc., Chicago, IL, USA) was used to perform the statistical analysis. The patients were divided into two groups according to ADS score. Continuous variables were expressed as the means ± standard deviation. The categorical variables were expressed as a percentage. One-way ANOVA was used to evaluate differences between normally distributed numerical variables, and non-normally distributed numerical variables were analyzed using the Mann–Whitney U-test. The Chi-squared test was used to compare the categorical variables. Kaplan–Meier analysis was utilized to analyze the cumulative incidence of long-term prognosis. The log-rank test was used to compare between groups. A multivariate Cox model was used to adjust the potential confounders. P < 0.05 was considered statistically significant.
In the present study, we enrolled 3,561 patients who were divided into two groups according to ADS: lower group—ADS <2 (n = 2,682) and higher group—ADS ≥2 (n = 879). We found significant differences between the two groups in age, family history, Cr, GLU, TG, TC, HDL-C, medication of CCB, and statins (all Ps < 0.05). However, sex, male, family history, smoking, alcohol drinking, diabetes, hypertension, LDL-C, treatment of β-blockers, ACEI or ARB between groups were not significantly different (all Ps ≥ 0.05, Table 1, Figures 2, 3).
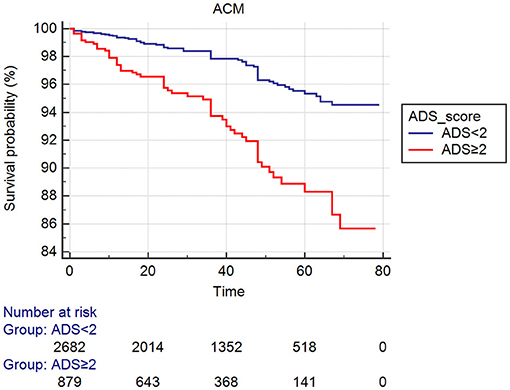
Figure 2. Cumulative Kaplan–Meier estimates of the time to the first adjudicated occurrence of primary endpoints (ACM).
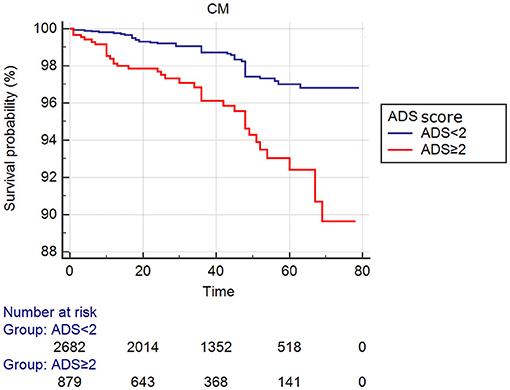
Figure 3. Cumulative Kaplan–Meier estimates of the time to the first adjudicated occurrence of primary endpoints (CM).
As shown in Table 2, 133 patients developed ACM, such as 72 (2.7%) patients in the lower group and 61 (6.9%) patients in the higher group. The incidence of ACM increased gradually with the increase in ADS value, and the ACM incidence of the higher group was significantly increased than the lower group (HR = 2.852; 95% CI: 2.027–4.012, P < 0.001). We also found that the incidence of CM (HR = 2.920; 95% CI: 1.891–4.509, P < 0.001), MACCEs (HR = 1.427; 95% CI: 1.182–1.723, P < 0.001) or MACE (HR = 1.362; 95% CI: 1.095–1.693, P = 0.007) in the higher group was significantly greater compared to that in the lower group. These differences remained significant after multivariable COX regression analysis ACM [HR = 2.031 (95% CI: 1.357–3.039), P = 0.001], CM [HR = 1.883 (95% CI: 1.127–3.147), P = 0.016], and MACCEs [HR = 1.352 (95% CI: 1.096–1.668), P = 0.005]. However, the incidence of MACE was not significantly different between groups in multivariable analysis (HR = 1.260, 95% CI: 0.987–1.608, P = 0.063, Table 3).
Numerous biomarkers and scoring systems are used for prognostic evaluations of patients with CAD. However, some systems are relatively expensive or difficult to apply in clinical practice. The present study is the first to demonstrate the association of elevated ADS scores with an increased risk of adverse outcomes in CAD patients who underwent PCI.
Recent studies reported the association of inflammatory biomarkers with clinical outcomes of CAD (1–4). In our study, we comprehensively investigated the ADS score established with inflammatory related cells and ratios of them to predict the clinical outcomes of CAD. We found that ADS score was an efficacy predictor of CAD patients who underwent PCI. ADS score was established with Alb, dNLR, and AFR. Albumin is a major component of serum proteins. It contributes up to 80% of the total colloid osmotic pressure, transports drugs and endogenous compounds, acts as an antioxidant, and maintains microvascular integrity (20). The serum concentration of Albumin decreases in acute and chronic inflammatory states. Decreased serum albumin is associated with decreased fibrinolysis and enhanced platelet aggregation (21). A high ratio of fibrinogen to albumin accelerates erythrocyte aggregation in capillaries, which is also a cause of the occurrence of thrombotic disease (22). In addition, low albumin levels can facilitate hypercoagulability resulting in thrombotic events (23). Neutrophilia reflects the inflammation and the lymphocyte reflects the body's stress response; therefore, the dNLR represents a balance between these two paths (24, 25). The high dNLR represented an increased inflammatory response and the body's stress response. Previous study suggested that the NLR is an independent predictor of long-term cardiovascular outcome after elective PCI (26). These studies and findings provide strong evidence to support our current research.
Several limitations should be mentioned in the present study. First, there may be some unknown confounding factors, which affect the outcomes since this is a single-center observational study design. Second, the ADS score was constructed using the baseline parameters and its dynamic changes were not observed. Third, the mechanism of action between these parameters requires further study.
The present study demonstrated that ADS was an effective and independent factor for predicting prognosis of CAD patients who underwent PCI.
The datasets presented in this article are not readily available due to confidentiality policies. Requests to access the datasets should be directed to Ying-Ying Zheng, emhlbmd5aW5nNTI3QDE2My5jb20=.
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. Written informed consent was not required for this study, in accordance with the local legislation and institutional requirements.
W-JZ, G-QL, J-HS, and X-DZ made substantial contributions to the study conception, design, and to the drafting and critical revision of the manuscript for important intellectual content. WW, Q-QG, J-CZ, Z-YL, F-HS, LF, and KW made substantial contributions to the study conception, design, and to the critical revision of the manuscript for important intellectual content. LL, J-YZ and Y-YZ made substantial contributions to the study conception, design, drafting, and critical revision of the manuscript for important intellectual content, such as study supervision. All authors contributed to the article and approved the submitted version.
This work was funded by National Natural Science Foundation of China (Nos. 82000238 and 81870328) and Henan Medical Science and Technology Joint Building Program (No.2018020002), Henan Thousand Talents Program (No. ZYQR201912131).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors are grateful to the Department of Cardiology at the First Affiliated Hospital of Zhengzhou University for their help and expertise in conducting this study.
CAD, coronary artery disease; ACM, all-cause mortality; MACE, major adverse cardiovascular events; CM, cardiac mortality; MACCEs, major adverse cardiovascular and cerebrovascular events; PCI, percutaneous coronary intervention.
1. Hemenway G, Frishman WH. Therapeutic implications of NLRP3-mediated inflammation in coronary artery disease. Cardiol Rev. (2021). doi: 10.1097/CRD.0000000000000391. [Epub ahead of print].
2. Liu Y, Ye T, Chen L, Jin T, Sheng Y, Wu G, et al. Systemic immune-inflammation index predicts the severity of coronary stenosis in patients with coronary heart disease. Coron Artery Dis. (2021) 32:715–20. doi: 10.1097/MCA.0000000000001037
3. Agarwal R, Aurora RG, Siswanto BB, Muliawan HS. The prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease. Coron Artery Dis. (2021). doi: 10.1097/MCA.0000000000001040. [Epub ahead of print].
4. Ziaee S, Hosseindokht M, Cheraghi S, Pourgholi L, Ahmadi A, Sadeghian S, et al. Predictive inflammation-related microRNAs for cardiovascular events following early-onset coronary artery disease. Arch Med Res. (2021) 52:69–75. doi: 10.1016/j.arcmed.2020.10.004
5. Mazereeuw G, Herrmann N, Bennett SA, Swardfager W, Xu H, Valenzuela N, et al. Platelet activating factors in depression and coronary artery disease: a potential biomarker related to inflammatory mechanisms and neurodegeneration. Neurosci Biobehav Rev. (2013) 37:1611–21. doi: 10.1016/j.neubiorev.2013.06.010
6. Kim HM, Lee BW, Song YM, Kim WJ, Chang HJ, Choi DH, et al. Potential association between coronary artery disease and the inflammatory biomarker YKL-40 in asymptomatic patients with type 2 diabetes mellitus. Cardiovasc Diabetol. (2012) 11:84. doi: 10.1186/1475-2840-11-84
7. Yang Y, Xu Y, Wang J, Zhai X, Jiang H. Predictive efficacy of neutrophil-to-lymphocyte ratio for long-term prognosis in new onset acute coronary syndrome: a retrospective cohort study. BMC Cardiovasc Disord. (2020) 20:500. doi: 10.1186/s12872-020-01773-x
8. Wada H, Dohi T, Miyauchi K, Nishio R, Takeuchi M, Takahashi N, et al. Neutrophil to lymphocyte ratio and long-term cardiovascular outcomes in coronary artery disease patients with low high-sensitivity C-reactive protein level. Int Heart J. (2020) 61:447–53. doi: 10.1536/ihj.19-543
9. Bronić A, Ferenčak G, Bernat R, Leniček-KrleŽa J, Dumić J, Dabelić S. Association of fibrinogen and plasmin inhibitor, but not coagulation factor XIII gene polymorphisms with coronary artery disease. J Med Biochem. (2021) 40:138–49. doi: 10.5937/jomb0-26839
10. Zhang Y, Jin JL, Cao YX, Liu HH, Zhang HW, Guo YL, et al. Prognostic utility of lipoprotein(a) combined with fibrinogen in patients with stable coronary artery disease: a prospective, large cohort study. J Transl Med. (2020) 18:373. doi: 10.1186/s12967-020-02546-y
11. Zhang DP, Mao XF, Wu TT, Chen Y, Hou XG, Yang Y, et al. The fibrinogen-to-albumin ratio is associated with outcomes in patients with coronary artery disease who underwent percutaneous coronary intervention. Clin Appl Thromb Hemost. (2020) 26:1076029620933008. doi: 10.1177/1076029620933008
12. Liu SL, Wu NQ, Shi HW, Dong Q, Dong QT, Gao Y, et al. Fibrinogen is associated with glucose metabolism and cardiovascular outcomes in patients with coronary artery disease. Cardiovasc Diabetol. (2020) 19:36. doi: 10.1186/s12933-020-01012-9
13. Deveci B, Gazi E. Relation between globulin, fibrinogen, and albumin with the presence and severity of coronary artery disease. Angiology. (2021) 72:174–80. doi: 10.1177/0003319720959985
14. Zheng YY, Wu TT, Chen Y, Hou XG, Yang Y, Ma X, et al. Gamma-glutamyl transferase to albumin ratio as a novel predictor of bleeding events and mortality in patients after percutaneous coronary intervention: a retrospective cohort study. Catheter Cardiovasc Interv. (2020) 95(Suppl. 1):572–8. doi: 10.1002/ccd.28696
15. Saleem W, Salinas C, Watkins B, Garvey G, Sharma AC, Ghosh R. Antibody functionalized graphene biosensor for label-free electrochemical immunosensing of fibrinogen, an indicator of trauma induced coagulopathy. Biosens Bioelectron. (2016) 86:522–9. doi: 10.1016/j.bios.2016.07.009
16. Celebi S, Ozcan Celebi O, Berkalp B, Amasyali B. The association between the fibrinogen-to-albumin ratio and coronary artery disease severity in patients with stable coronary artery disease. Coron Artery Dis. (2020) 31:512–7. doi: 10.1097/MCA.0000000000000868
17. Gao QF, Qiu JC, Huang XH, Xu YM, Li SQ, Sun F, et al. The predictive and prognostic role of a novel ADS score in esophageal squamous cell carcinoma patients undergoing esophagectomy. Cancer Cell Int. (2018) 18:153. doi: 10.1186/s12935-018-0648-2
18. Yang T, Hao L, Yang X, Luo C, Wang G, Lin Cai C, et al. Prognostic value of derived neutrophil-to-lymphocyte ratio (dNLR) in patients with non-small cell lung cancer receiving immune checkpoint inhibitors: a meta-analysis. BMJ Open. (2021) 11:e049123. doi: 10.1136/bmjopen-2021-049123
19. Zheng YY, Wu TT, Gao Y, Guo QQ, Ma YY, Zhang JC, et al. A novel ABC score predicts mortality in Non-ST-segment elevation acute coronary syndrome patients who underwent percutaneous coronary intervention. Thromb Haemost. (2021) 121:297–308. doi: 10.1055/s-0040-1718411
20. Oettl K, Stauber RE. Physiological and pathological changes in the redox state of human serum albumin critically influence its binding properties. Br J Pharmacol. (2007) 151:580–90. doi: 10.1038/sj.bjp.0707251
21. Paar M, Rossmann C, Nusshold C, Wagner T, Schlagenhauf A, Leschnik B, et al. Anticoagulant action of low, physiologic, and high albumin levels in whole blood. PLoS ONE. (2017) 12:e0182997. doi: 10.1371/journal.pone.0182997
22. Dintenfass L, Lake B. Blood viscosity factors in evaluation of submaximal work output and cardiac activity in men. Angiology. (1977) 28:788–98. doi: 10.1177/000331977702801108
23. Bas M, Kirchhartz N, Hochfeld J, Tüllmann C, Kumpf S, Suvorava T, et al. Potential role of vasomotor effects of fibrinogen in bradykinin-induced angioedema. J Allergy Clin Immunol. (2008) 121:969–75.e2. doi: 10.1016/j.jaci.2008.01.071
24. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. (2002) 105:1135–43. doi: 10.1161/hc0902.104353
25. Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther. (2016) 14:573–7. doi: 10.1586/14779072.2016.1154788
Keywords: ADS score, mortality, major adverse cardiovascular and cerebrovascular events, major adverse cardiovascular events, coronary artery disease, percutaneous coronary intervention
Citation: Zhang W-J, Liu G-Q, Shangguan J-H, Zhu X-D, Wang W, Guo Q-Q, Zhang J-C, Wang K, Liu Z-Y, Song F-H, Fan L, Li L, Zheng Y-Y and Zhang J-Y (2021) ADS Score as a Novel Predictor of Outcomes in Patients Who Underwent Percutaneous Coronary Intervention. Front. Cardiovasc. Med. 8:720597. doi: 10.3389/fcvm.2021.720597
Received: 04 June 2021; Accepted: 08 November 2021;
Published: 13 December 2021.
Edited by:
Hendrik Tevaearai Stahel, Bern University Hospital, SwitzerlandReviewed by:
Jinwei Tian, The Second Affiliated Hospital of Harbin Medical University, ChinaCopyright © 2021 Zhang, Liu, Shangguan, Zhu, Wang, Guo, Zhang, Wang, Liu, Song, Fan, Li, Zheng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Li, bGlsaW5nNjMwMzVAc2luYS5jb20=; Ying-Ying Zheng, emhlbmd5aW5nNTI3QDE2My5jb20=; Jin-Ying Zhang, anl6aGFuZ0B6enUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.