
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 24 June 2021
Sec. Cardiovascular Metabolism
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.704446
This article is part of the Research Topic Insulin Resistance, Metabolic Syndrome and Cardiovascular Disease View all 36 articles
Background: The metabolic syndrome (MS) is significantly associated with the risk of incident heart failure (HF). However, there are still great controversies about the impact of MS on the prognosis in patients with established HF. This meta-analysis aimed to ascertain the effect of MS on the prognosis in patients with HF.
Methods: We searched multiple electronic databases, including PubMed, Opengrey, EMBASE, and Cochran Library, for potential studies up to February 15, 2021. Observational studies that reported the impact of MS on the prognosis in patients with established HF were included for meta-analysis.
Results: Ten studies comprising 18,590 patients with HF were included for meta-analysis. The median follow-up duration of the included studies was 2.4 years. Compared with HF patients without MS, the risk of all-cause mortality and cardiovascular mortality was not increased in HF with MS (HR = 1.04, 95% CI = 0.88–1.23 for all-cause mortality; HR = 1.66, 95% CI = 0.56–4.88 for cardiovascular mortality, respectively). However, there was a significant increase in composited cardiovascular events in the HF patients with MS compared with those without MS (HR = 1.73, 95% CI = 1.23–2.45).
Conclusions: In patients with established HF, the presence of MS did not show an association on the risk of all-cause mortality or cardiovascular mortality, while it may increase the risk of composite cardiovascular events.
Metabolic syndrome (MS) is a cluster of cardiovascular risk factors characterized by insulin resistance, central obesity, elevated blood pressure, and dyslipidemia (1, 2). Epidemiological studies have shown that MS and its components are highly prevalent and significantly associated with the development of diabetes and cardiovascular disease (CVD) (2). Heart failure (HF) is a growing global public health burden, attributed to significantly increased mortality worldwide (3). Detection for the pathophysiological characteristics and novel treatment targets would be important for management of HF (4–6). It is well-documented that MS is an independent risk factor in the development of HF (7). Individuals with MS were associated with a 2-fold risk of HF incidence compared with those without MS (8). However, there are still great controversies about the impact of MS on the prognosis in patients with established HF. Some studies had reported that HF patients with MS had a significantly reduced risk of in-hospital mortality (9), as well as long-term all-cause mortality (10, 11), compared with HF patients without MS. However, such association was not documented in other studies (12, 13), raising concern of whether such “epidemiologic paradox” was true in the HF–MS relationship.
Given these inconsistent results and controversies, we performed a meta-analysis to ascertain the impact of MS on the prognosis in patients with HF, focusing on all-cause mortality, cardiovascular mortality, and composite cardiovascular events.
This study was performed under the recommendations of the Meta-analysis of Observational Studies in Epidemiology group (14). We searched multiple electronic databases, including PubMed, Medline, EMBASE, and Cochran Library, for potential related studies up to February 15, 2021. Items including “metabolic syndrome,” “syndrome X,” “insulin resistance syndrome,” “heart failure,” “myocardial failure,” “cardiac failure,” “cardiac dysfunction,” or “myocardial dysfunction” were searched using a combined MeSH terms and text word search strategy. No language restriction was set in the search strategy. However, we restricted the search to human studies by using the “Humans” filters. The reference lists of included studies were reviewed to identify other potential associated research.
Inclusion criteria of studies for meta-analysis were the following: (1) observational studies (cohort studies, nest case–control studies, or post-hoc analysis of randomized controlled trials) with a follow-up duration ≥6 months; (2) the prognoses in HF patients were reported in those with MS, compared with those without MS. Exclusion criteria were the following: (1) cross-sectional studies without follow-up evaluation; (2) duplicated publications derived from the same observational study. When duplicated publications were derived from the same observational study, we only included the latest published article for analysis.
Two researchers (ZH and WC) screened the titles and abstracts of all the retrieved items and reviewed the full manuscripts of potentially relevant studies independently. Key information of the included studies, such as authors, study design, race, definition and prevalence of MS, sample size, sex proportion, age, follow-up duration, adjusted confounders, and outcome events were recorded. We also contacted the corresponding authors of the original studies for any additional data if required.
We evaluated the quality of the included studies according to the Newcastle–Ottawa Quality Assessment Scale (NOS) for cohort studies (15). The NOS judged the quality based on selection, comparability, and exposure/outcome, with the highest score up to 9. In the present analysis, included studies were graded in quality as good, fair, or poor if they were awarded ≥7, 4–6, or <4 scores, respectively (16, 17).
The primary outcome in our study was the risk of all-cause mortality in HF patients with MS compared with those without MS. The secondary outcomes included the risk of cardiovascular mortality and composite cardiovascular events, respectively. Hazard ratios (HRs) and 95% confidence intervals (CIs) adjusted for the maximal number of confounders were extracted for analysis. If relative risks (RRs) were reported, they were considered as approximate estimate for HRs and used for meta-analysis (18). In situations where outcomes were presented as odds ratios (ORs), data were converted to RRs for analysis, according to previously published method (19). I2 statistics were used to test heterogeneity among studies, and an I2 > 50% was considered to be with significant heterogeneity. We used the inverse variance approach to combine the log HRs and corresponding standard errors (SE). A random-effects model was used for meta-analysis if there was significant heterogeneity. Otherwise, a fixed-effects model was used. Sensitivity analyses were performed by omitting one study and recalculating the estimates of HRs at a time or interchange using random-effects models and fixed-effects models for the meta-analysis. Publication bias was evaluated by inspecting funnel plots for the primary outcome in which the lnHR was plotted against SE and also tested by using Egger's and Begg's tests. Subgroup analyses were performed according to participant's age, follow-up duration, race, the severity of HF, adjusted confounders, and definition of MS.
Analyses were performed using RevMan 5.3 (The Cochrane Collaboration, Copenhagen, Denmark) and Stata 12.0 (StataCorp LP, College Station, TX, USA) for Egger's and Begg's tests. A p < 0.05 was set for statistical significance.
A total of 3,356 items were detected from the online electronic databases. After screening the titles and abstracts, we found that 27 articles were qualified for a full review. Finally, we included 10 studies comprising 18,590 patients with HF for meta-analysis (Figure 1) (10–13, 20–25). The median follow-up duration of the included studies was 2.4 years.
In the 10 studies, 8 were from the United States and Europe; 2 were from Asia. The key messages of the included studies are presented in Table 1. All studies included advanced HF patients, except one study that included patients with asymptomatic HF (stage A/B HF). Five, four, and one study defined MS according to the Third Adult Treatment Panel Report of the National Cholesterol Education Program (NCEP-ATP III), the International Diabetes Federation guideline (IDF), and the Japanese Committee for the Diagnostic Criteria of MS, respectively. Two studies were published as meeting abstracts, and full articles were not available. Therefore, quality assessment was only performed in the eight studies with full published articles. According to NOS criteria, six studies were graded as good quality and two as fair quality (Supplementary Table 1).
There were eight studies that provided data for analysis of the association between MS and all-cause mortality in patients with HF. Due to the significant heterogeneity among the included studies (I2 = 73%, p < 0.001), a random-effects model was used to combined the pooled estimates. Compared with patients without MS, the risk of all-cause mortality was not increased in HF patients with MS (HR = 1.04, 95% CI = 0.88–1.23, p = 0.62) (Figure 2). No evidence of publication bias was found by visual inspection of the funnel plot (Supplementary Figure 1) or using Egger's test or Begg's (all p > 0.05).
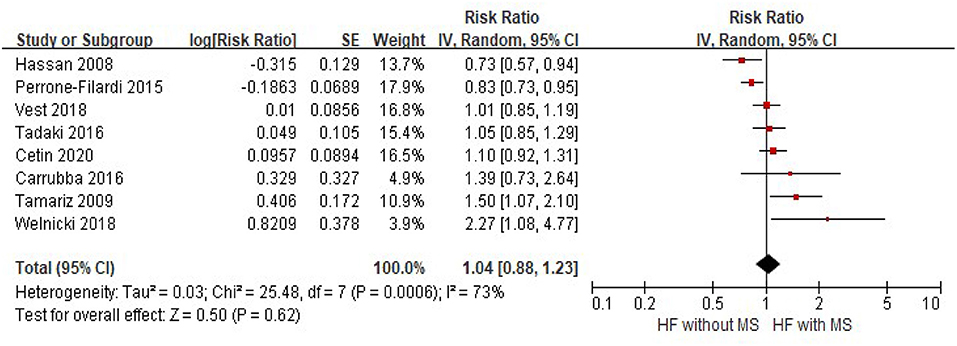
Figure 2. The association of MS and the risk of all-cause mortality in HF patients. CI, confidence interval; HF, heart failure; MS, metabolic syndrome.
Three studies provided the risk of cardiovascular mortality in HF patients with and without MS, and significant heterogeneity was observed among the studies (I2 = 86%, p < 0.001). Random-effects models meta-analysis showed that there was no significant difference in cardiovascular mortality between the groups (HF with MS vs. HF without HF, HR = 1.66, 95% CI = 0.56–4.88, p = 0.36) (Figure 3).
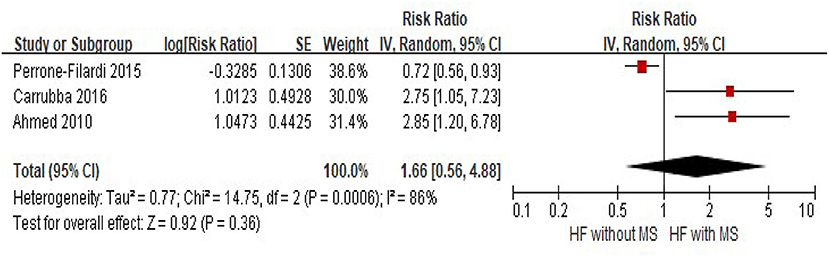
Figure 3. The association of MS and the risk of cardiovascular mortality in HF patients. CI, confidence interval; HF, heart failure; MS, metabolic syndrome.
Although significant heterogeneity existed among three studies that reported composited cardiovascular events (I2 = 64%, p = 0.06), pooled estimates showed that there was a substantial increase in composited cardiovascular events in HF patients with MS, compared with those without HF (HR = 1.73, 95% CI = 1.23–2.45, p = 0.002) (Figure 4).
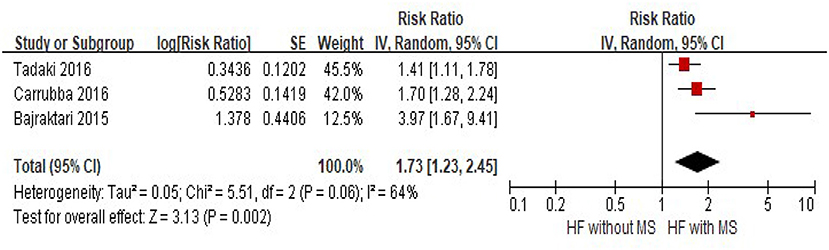
Figure 4. The association of MS and the risk of composite cardiovascular events in HF patients. CVD, cardiovascular disease; CI, confidence interval; HF, heart failure; MS, Metabolic Syndrome.
The subgroup analyses for the relative risk of all-cause mortality in HF patients with MS are presented in Table 2. Patients with HF and MS did not show an association with all-cause mortality in all the subgroup analyses. Furthermore, there was no significant heterogeneity observed among subgroup comparisons (all p > 0.15).

Table 2. Subgroup analyses of the association between MS and risk of all-cause mortality in HF patients.
Several sensitivity analyses confirmed that there was no significant association between MS status and risk of all-cause mortality, using fixed-effects models instead of random-effects models or recalculating the estimated risk by omitting one study at a time.
To the best of our knowledge, this is the first meta-analysis exploring the impact of MS on the prognosis in patients with established HF. Our data showed that MS is not associated with the risk of all-cause mortality or cardiovascular mortality in HF patients, while an increased risk of composite cardiovascular events was observed. Therefore, this study challenges the “epidemiologic paradox” in the relationship between HF and MS.
Observational studies had reported that in patients with established HF, risk factors that contribute to the development of CVD and HF, including hypertension, obesity, and hypercholesterolemia, might have a protective effect on prognosis. This phenomenon was termed as “reverse epidemiology” or “risk factor paradox” (26). However, the nature of observational studies could not exclude “reverse causation” in such observed associations; i.e., it may not be that obesity, hypertension, and hypercholesterolemia can play a protective role, while low body mass index (BMI), blood pressure, or serum cholesterol are “markers” of a severe pathological condition in HF, closely linked to cachexia, frailty, and death (7). In our study, the presence of MS was not associated with a favorable prognosis in the HF population, and no evidence of a “metabolic syndrome survival paradox” was found. Our results were supported by the study of Ozcan et al. (25). which showed that the risk of all-cause mortality was not statistically different in HF patients with and without MS. However, in HF patients with “reverse metabolic syndrome” (i.e., low BMI, blood pressure, and total cholesterol than normal level), the risk of all-cause mortality was increased in metabolically healthy patients. In this view, we should not recommend that MS is a protective factor; rather we should advocate that in HF patients with “reverse metabolic syndrome,” targeting catabolic syndrome by nutritional support and anti-inflammatory treatment should be considered in future studies.
Actually, we found that in HF with MS, the risk of composite cardiovascular events was increased compared with those without MS. This finding further supports that MS is an independent risk of atherosclerotic cardiovascular events (2), even in patients with established HF. Besides the effect of the cluster of atherosclerotic risk factors, activation of the sympathetic nervous system and renin–angiotensin system may also be involved in this process. It had been proposed that in HF patients with MS, activation of the sympathetic nervous system and renin–angiotensin system was higher than those without MS (27, 28). Our study also found that the prevalence of MS was up to 13.0–68.3%, based on different definitions. Considering the high prevalence and association with increased risk of composite cardiovascular events, proper management of this population would be of important clinical effect. During the past decade, the treatment of HF had made great progress, and many patients with severe HF can survive for a long time. In this situation, prevention of CVD in established HF with MS should be considered.
Several limitations of the current study should be mentioned. First, the definitions of MS were different in the included studies. However, our subgroup analysis showed that the risk of all-cause mortality was not increased in HF with MS; neither was defined according to the IDF nor NCEP-ATP III criteria. Second, the definitions of HF among the included studies were with significant heterogeneity. The etiologies of HF are also unknown in the studies. However, we did not observe a difference in the subgroup analysis according to the severity of HF. Even in patients with advanced HF, the risk of all-cause mortality was not associated with the presence of MS. Third, MS is a cluster of cardiovascular risk factors, including obesity, elevated blood pressure, elevated blood glucose, and dyslipidemia. Due to limited data, we did not evaluate the effect of the individual components of MS on the prognosis in HF. Fourth, although we reported that the risk of composite cardiovascular events was increased in HF with MS, only three studies were available for the meta-analysis of this outcome. Further studies are needed to explore the association between MS and the risk of CVD in patients with established HF.
In patients with established HF, the presence of MS did not show a protective effect on the risk of all-cause mortality or cardiovascular mortality, while it may increase the risk of composite cardiovascular events.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Z-MH and W-RC: research idea, study design, and data acquisition. Q-WS and Z-WH: data analysis/interpretation and statistical analysis. W-RC: supervision and mentorship. All authors contributed important intellectual content during manuscript drafting or revision and accept accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.704446/full#supplementary-material
CIs, confidence intervals; CVD, cardiovascular disease; HF, heart failure; HRs, hazard ratios; IDF, International Diabetes Federation; MS, metabolic syndrome; NCEP-ATP III, Third Adult Treatment Panel Report of the National Cholesterol Education Program; NOS, Newcastle–Ottawa Quality Assessment Scale; RRs, relative risks; SE, standard errors.
1. Beltran-Sanchez H, Harhay MO, Harhay MM, McElligott S. Prevalence and trends of metabolic syndrome in the adult U.S. population, 1999-2010. J Am Coll Cardiol. (2013) 62:697–703. doi: 10.1016/j.jacc.2013.05.064
2. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. (2010) 56:1113–32. doi: 10.1016/j.jacc.2010.05.034
3. Cai X, Liu X, Sun L, He Y, Zheng S, Zhang Y, et al. Prediabetes and the risk of heart failure: a meta-analysis. Diabetes Obes Metab. (2021) doi: 10.1111/dom.14388. [Epub ahead of print].
4. Li W, Huang A, Zhu H, Liu X, Huang X, Huang Y, et al. Gut microbiota-derived trimethylamine N-oxide is associated with poor prognosis in patients with heart failure. Med J Aust. (2020) 213:374–9. doi: 10.5694/mja2.50781
5. Yang S, Chen H, Tan K, Cai F, Du Y, Lv W, et al. Secreted frizzled-related protein 2 and extracellular volume fraction in patients with heart failure. Oxid Med Cell Longev. (2020) 2020:2563508. doi: 10.1155/2020/2563508
6. Wu J, Zheng H, Liu X, Chen P, Zhang Y, Luo J, et al. Prognostic value of secreted frizzled-related protein 5 in heart failure patients with and without type 2 diabetes mellitus. Circ Heart Fail. (2020) 13:e7054. doi: 10.1161/CIRCHEARTFAILURE.120.007054
7. Arcopinto M, Schiavo A, Salzano A, Bossone E, D'Assante R, Marsico F, et al. Metabolic syndrome in heart failure: friend or foe? Heart Fail Clin. (2019) 15:349–58. doi: 10.1016/j.hfc.2019.02.004
8. Horwich TB, Fonarow GC. Glucose, obesity, metabolic syndrome, and diabetes relevance to incidence of heart failure. J Am Coll Cardiol. (2010) 55:283–93. doi: 10.1016/j.jacc.2009.07.029
9. Yoon HJ, Ahn Y, Kim KH, Park JC, Choi DJ, Han S, et al. The prognostic implication of metabolic syndrome in patients with heart failure. Korean Circ J. (2013) 43:87–92. doi: 10.4070/kcj.2013.43.2.87
10. Hassan SA, Deswal A, Bozkurt B, Aguilar D, Mann DL, Pritchett AM. The metabolic syndrome and mortality in an ethnically diverse heart failure population. J Card Fail. (2008) 14:590–95. doi: 10.1016/j.cardfail.2008.03.004
11. Perrone-Filardi P, Savarese G, Scarano M, Cavazzina R, Trimarco B, Minneci S, et al. Prognostic impact of metabolic syndrome in patients with chronic heart failure: data from GISSI-HF trial. Int J Cardiol. (2015) 178:85–90. doi: 10.1016/j.ijcard.2014.10.094
12. Tamariz L, Hassan B, Palacio A, Arcement L, Horswell R, Hebert K. Metabolic syndrome increases mortality in heart failure. Clin Cardiol. (2009) 32:327–31. doi: 10.2337/diacare.24.4.683
13. La Carrubba S, Antonini-Canterin F, Fabiani I, Colonna P, Pugliese NR, Caso P, et al. Prevalence and prognostic impact of metabolic syndrome in asymptomatic (stage A and B heart failure) patients. Metab Syndr Relat Disord. (2016) 14:187–94. doi: 10.1089/met.2015.0143
14. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
15. Wells GA, Shea B, O'Connell D, Robertson J, Peterson J, Welch V, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed January 1, 2008)
16. Cai X, Zhang Y, Li M, Wu JH, Mai L, Li J, et al. Association between prediabetes and risk of all-cause mortality and cardiovascular disease: updated meta-analysis. BMJ. (2020) 370:m2297. doi: 10.1136/bmj.m2297
17. Huang Y, Huang W, Mai W, Cai X, An D, Liu Z, et al. White-coat hypertension is a risk factor for cardiovascular diseases and total mortality. J Hypertens. (2017) 35:677–688. doi: 10.1097/HJH.0000000000001226
18. Yang Y, Li W, Zhu H, Pan XF, Hu Y, Arnott C, et al. Prognosis of unrecognised myocardial infarction determined by electrocardiography or cardiac magnetic resonance imaging: systematic review and meta-analysis. BMJ. (2020) 369:m1184. doi: 10.1136/bmj.m1184
19. Cai X, Zheng S, Liu Y, Zhang Y, Lu J, Huang Y. Nonalcoholic fatty liver disease is associated with increased risk of atrial fibrillation. Liver Int. (2020) 40:1594–600. doi: 10.1111/liv.14461
20. Ahmed I, Nelson WB, Dahiya R, House CM, Zhu DW. Metabolic syndrome predicts poor outcome in patients with systolic heart failure who received implantable-cardioverter defibrillator for primary prevention of sudden cardiac death. Heart Rhythm. (2010) 7:S252–53. doi: 10.1016/j.hrthm.2010.03.031
21. Bajraktari G, Berisha G, Bytyci I, Haliti E, Ibrahimi P, Ahmeti A, et al. The presence of metabolic syndrome predicts long-term outcome in heart failure patients. Eur Heart J. (2015) 36:831. doi: 10.2337/dc08-1394
22. Tadaki S, Sakata Y, Miura Y, Miyata S, Asakura M, Shimada K, et al. Prognostic impacts of metabolic syndrome in patients with chronic heart failure-a multicenter prospective cohort study. Circ J. (2016) 80:677–88. doi: 10.1253/circj.CJ-15-0942
23. Vest AR, Young JB, Cho L. The metabolic syndrome, cardiovascular fitness and survival in patients with advanced systolic heart failure. Am J Cardiol. (2018) 122:1513–9. doi: 10.1016/j.amjcard.2018.07.024
24. Welnicki MT, Sliz DI, Szeligowska J, Duda-Król WB, Chomiuk T, Dabrowska D, et al. The influence of metabolic syndrome coexistence on the prognosis of patients with heart failure without atrial fibrillation. analysis of Polish data from the pilot survey for the ESC Heart Failure Registry. Kardiol Pol. (2018) 76:794–6. doi: 10.5603/KP.2018.0077
25. Ozcan CE, Cetin MS, Ozbay MB, Yaman NM, Könte HC, Ekizler FA, et al. The other side of the medallion in heart failure: reverse metabolic syndrome. Nutr Metab Cardiovasc Dis. (2020) 30:2041–50. doi: 10.1016/j.numecd.2020.06.027
26. Gargiulo P, Marsico F, Renga F, Dell'Aversana S, Esposito I, Marciano C, et al. The metabolic syndrome in heart failure: insights to specific mechanisms. Heart Fail Rev. (2020) 25:1–7. doi: 10.1007/s10741-019-09838-6
27. Sarzani R, Salvi F, Dessi-Fulgheri P, Rappelli A. Renin-angiotensin system, natriuretic peptides, obesity, metabolic syndrome, and hypertension: an integrated view in humans. J Hypertens. (2008) 26:831–43. doi: 10.1097/HJH.0b013e3282f624a0
Keywords: heart failure, metabolic syndrome, all-cause mortality, cardiovasclar disease, prognosis
Citation: Huang Z-M, Chen W-R, Su Q-W and Huang Z-W (2021) Prognostic Impact of Metabolic Syndrome in Patients With Heart Failure: A Meta-Analysis of Observational Studies. Front. Cardiovasc. Med. 8:704446. doi: 10.3389/fcvm.2021.704446
Received: 03 May 2021; Accepted: 21 May 2021;
Published: 24 June 2021.
Edited by:
Xiongfei Pan, Vanderbilt University Medical Center, United StatesReviewed by:
Cheng Liu, Guangzhou First People's Hospital, ChinaCopyright © 2021 Huang, Chen, Su and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wen-Rong Chen, NTY1NzI4OTNAcXEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.