- 1Department of Pathology, Institute of Medical Genetics and Pathology, University Hospital Basel, University of Basel, Basel, Switzerland
- 2Intensive Care Unit, University Hospital Basel, Basel, Switzerland
We report on an impressive case of a previously healthy 47-year-old female Caucasian SARS-CoV-2 positive patient who died within 48 h after initial cardiac symptoms. Autopsy revealed necrotizing myocarditis and extensive microthrombosis as the cause of death. The interesting feature of this case is the combination of both myocarditis and extensive localized microthrombosis of cardiac capillaries. Microthrombosis was not present in other organs, and the patient did not show typical features of diffuse alveolar damage in the lungs. Taken together, our morphologic findings illustrate the angiocentric, microangiopathic, thromboinflammatory disease with significant thrombotic diathesis prevalent in COVID-19, which has been previously described in the literature, likely warranting thromboprophylaxis even in oligosymptomatic circumstances. This case also delineates several potential etiologies for microthrombosis, i.e., inflammatory reactions and primary hypercoagulative states. Further systematic analyses on risk stratification for receipt of prophylactic anticoagulation in COVID-19 are urgently required.
Introduction
Based on early empiric evidence and autopsy observations (1–3), anticoagulation has emerged as an important topic in treatment of COVID-19 (4). It is now well-established that thromboses significantly contribute to disease burden in COVID-19 and thus warrant immediate attention by treating physicians regardless of disease severity (5, 6). Myocarditis is also rare but nevertheless an acknowledged comorbidity in COVID-19 (7). Few cases have been examined by histopathology so far, and they showed divergent features ranging from subtle inflammatory infiltrates not fulfilling diagnostic criteria for borderline myocarditis to overt necrotizing inflammation (8–10).
Here, we present a case of a previously healthy patient positive for SARS-CoV-2 who died of cardiac complications consisting of necrotizing myocarditis and extensive microthrombosis within 48 h after initial cardiac symptoms.
Case
A 47-year-old female suffered from oligosymptomatic flu-like disease for a week before she was found unconscious and apneic at home. Advanced cardiac life support was promptly administered by paramedics. Upon hospital admission, electrocardiography (ECG) showed ST-segment depression in all the leads and elevations in augmented vector right (aVR). Subsequently performed coronary angiography revealed no relevant coronary stenosis. Echocardiography detected moderately reduced left ventricular function (left ventricular ejection fraction (LVEF) 30%) and normal right ventricular size and function. There was no evidence of left ventricular hypertrophy or dilatation. Computerized tomography excluded pulmonary thromboembolism but showed bilateral lower-lobe consolidations. High-sensitivity troponin T (hsTropT) was elevated (272 ng/l at admission; peak of 507 ng/l 10 h after admission), as were brain natriuretic peptide (>70,000 ng/l) and C-reactive protein (282 mg/l). The leucocyte count was within normal range. A nasopharyngeal swab was positive for SARS-CoV-2. Apart from mild thrombocytopenia (140 G/L) and mildly prolonged activated partial thromboplastin time (aPTT) (39 s) at the time of admission, all other coagulation parameters were within normal ranges. Despite exhaustive invasive intensive care interventions including continuous adrenalin/noradrenaline infusion, prophylactic antibiotic therapy (piperacillin/tazobactam), and two further attempts of cardiac resuscitation, the patient died of cardio-respiratory failure within 48 h of admission. Her detailed clinical course is shown in the timeline section. Previous clinical history included episodes of depression, which had been treated with venlafaxine, and a cholecystectomy.
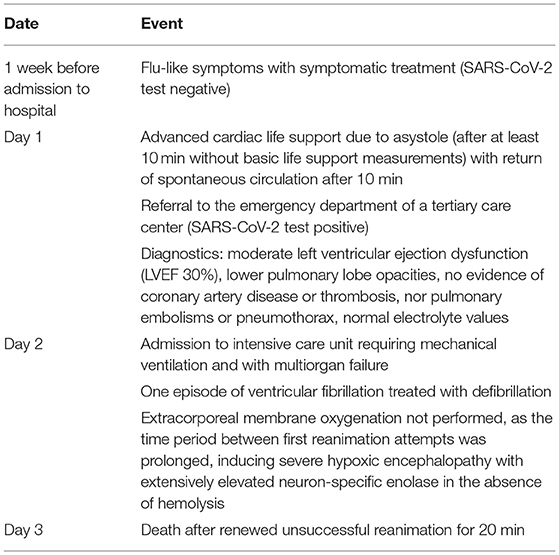
An autopsy was performed. No relevant comorbidities apart from obesity [body mass index (BMI) 31.6] were noticed. Major findings included moderate bilateral suppurative pneumonia with COVID-19-characteristic capillary stasis, yet without diffuse alveolar damage. Most notably, the heart presented as normotrophic and irregularly perfused with mild diffuse necrotizing myocarditis (Figure 1A) accompanied by extensive thrombotic microangiopathy of cardiac capillaries (Figures 1B,C; microthrombi in cardiac capillaries immunohistochemically stained for fibrin), which was determined as the cause of death. RT-qPCR of heart tissue was positive for SARS-CoV-2-N-gene (Ct 35.7). Immunohistochemistry for adenovirus was negative.
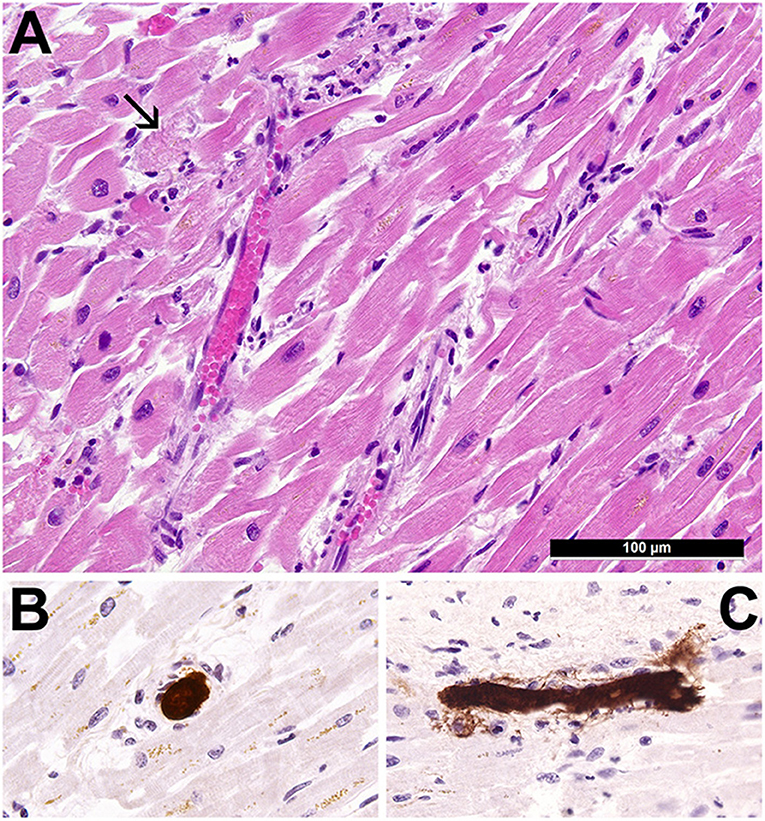
Figure 1. Cardiopathological findings. (A) Morphology of the heart showing multifocal inflammatory infiltrates consisting of neutrophilic granulocytes, lymphocytes and histiocytes, capillarostasis, and perifocal single-cell necroses of cardiomyocytes (arrow) (H&E, ×400). (B,C) Immunohistochemical staining for fibrin demonstrating cross section and longitudinal section of capillaries with prominent microthrombi occluding the lumens (immunohistochemistry for fibrin, ×400).
Timeline
Discussion
The interesting feature of this COVID-19 case study is the combination of both myocarditis and extensive microthrombosis of cardiac capillaries.
Our group, amongst others, has previously presented comprehensive autopsy cohorts of patients succumbing to COVID-19 describing microthrombosis predominantly in the lungs and further organs (2, 11, 12). Microthrombi in the pulmonary capillary bed and subsequently increased intravascular pressure in the pulmonary circulation have been attributed to heart failure in several studies. A recent report focusing on heart pathology described microthrombi in 12/15 COVID-19 cases (13); thrombi were also found in some control cases with influenza infection, metastatic carcinoma, or advanced severe bacterial pneumonia. In line with this case, we have previously investigated cardiopathological characteristics of patients succumbing to COVID-19 associated respiratory failure, similarly demonstrating a high incidence of capillary dilatation, stasis, and microthrombosis, especially in cases with detectable SARS-CoV-2 cardiac viral load (14).
It is well-acknowledged that COVID-19 predisposes to a procoagulatory state. The underlying pathophysiology for thromboinflammation is likely multifaceted, involving direct endothelial damage by SARS-CoV-2, secondary inflammatory endothelial damage, an overexpression of procoagulatory genes (e.g., SERPINE genes) in target organs, and generation of neutrophilic extracellular traps, and immunological, particularly antiphospholipid-mediated processes [rev. in (15)].
Myocarditis, in particular borderline myocarditis, in COVID-19 patients has been described (7). In a systematic review of 41 studies compiling 316 cases of COVID-19 autopsies, Roshdy et al. identified five cases (i.e., 1.5%) with inflammatory infiltrates fulfilling the Dallas criteria of myocarditis (8). In ≈10% of cases, mild focal inflammatory infiltrates in the myocardial interstitium had been noticed. In one study on endomyocardial biopsies taken for elucidating the cause of acute heart failure or in suspicion of myocarditis (16), isolated cases showed both presence of SARS-CoV-2 genomes and inflammatory infiltrates also affecting small vessels, while thrombi had not been described in this series.
In our case, the patient exclusively presented with localized cardiac microthrombi; other organs were not affected (also confirmed by immunohistochemistry). Microthrombi were partially associated with inflammatory infiltrates and single-cell cardiomyocyte necrosis, which we interpret as a sequela of the thrombotic microangiopathy. Acute heart failure, which is the non-disputable cause of death, can be attributed to both features—myocarditis and microthrombi—and our findings strongly support that both morphological features can be collectively interpreted as a rare but severe COVID-19-related thromboinflammatory cardiac complication. There was no evidence of a preexisting heart condition based on imaging and autopsy findings as well as the clinical history of the patient. Admittedly, it has to be considered that her intake of antidepressant (venlafaxine) might have contributed to cardiac pathology, yet the features described in single case reports and a review article of individuals treated with venlafaxine and cardiac problems were not evident in this case (17–19). Furthermore, there was no evidence of serotonin syndrome, mydriasis, or seizures.
Taken together, our morphologic findings and the preexisting literature illustrate that COVID-19 is an angiocentric, particularly microangiopathic, thromboinflammatory disease with significant thrombotic diathesis, in all likelihood warranting thromboprophylaxis even in oligosymptomatic circumstances. This case also delineates several potential etiologies for microthrombi: inflammatory reaction and primary hypercoagulative state. Further systematic analyses on risk stratification for receipt of prophylactic anticoagulation in COVID-19 are urgently required.
Patient Perspective
Heart failure is a severe complication of COVID-19. As illustrated in this case, it can also arise in previously healthy patients and might develop independently of pulmonary findings. Myocarditis and microthrombosis of the cardiac capillaries are potentially treatable etiologies of heart failure in such instances, yet their diagnosis may be difficult without histological examination. Thorough investigation of both coagulation parameters and the myocardium might be therefore required in patients with unexplained or rapidly deteriorating heart failure in the setting of COVID-19. It remains to be determined if prophylactic anticoagulation even in oligosymptomatic COVID-19 patients is feasible.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AT performed the autopsy. AT and TM designed the study and wrote the manuscript. NC and EG took care of the patient and provided clinical data. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Botnar Research Centre for Child Health, BRCCH.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Dr. med. J. D. Haslbauer for critically proofreading the manuscript.
References
1. Wichmann D, Sperhake JP, Lutgehetmann M, Steurer S, Edler C, Heinemann A, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. (2020) 173:268–77. doi: 10.7326/M20-2003
2. Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, et al. Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology. (2020) 77:198–209. doi: 10.1111/his.14134
3. Lax SF, Skok K, Zechner P, Kessler HH, Kaufmann N, Koelblinger C, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome : results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. (2020) 173:350–61. doi: 10.7326/M20-2566
4. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. (2020) 75:2950–73. doi: 10.1016/j.jacc.2020.04.031
5. Rentsch CT, Beckman JA, Tomlinson L, Gellad WF, Alcorn C, Kidwai-Khan F, et al. Early initiation of prophylactic anticoagulation for prevention of coronavirus disease 2019 mortality in patients admitted to hospital in the United States: cohort study. BMJ. (2021) 372:n311. doi: 10.1136/bmj.n311
6. Giannis D, Allen S, Tsang J, Flint S, Pinhasov T, Williams S, et al. Post-Discharge thromboembolic outcomes and mortality of hospitalized COVID-19 patients: the CORE-19 registry. Blood. (2021) 137:2838–47. doi: 10.1182/blood.2020010529
7. Mele D, Flamigni F, Rapezzi C, Ferrari R. Myocarditis in COVID-19 patients: current problems. Intern Emerg Med. (2021) 23:1–7. doi: 10.1007/s11739-021-02635-w
8. Roshdy A, Zaher S, Fayed H, Coghlan JG. COVID-19 and the heart: a systematic review of cardiac autopsies. Front Cardiovasc Med. (2020) 7:626975. doi: 10.3389/fcvm.2020.626975
9. Craver R, Huber S, Sandomirsky M, McKenna D, Schieffelin J, Finger L. Fatal eosinophilic myocarditis in a healthy 17-year-old male with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2c). Fetal Pediatr Pathol. (2020) 39:263–8. doi: 10.1080/15513815.2020.1761491
10. Basso C, Leone O, Rizzo S, De Gaspari M, van der Wal AC, Aubry MC, et al. Pathological features of COVID-19-associated myocardial injury: a multicentre cardiovascular pathology study. Eur Heart J. (2020) 41:3827–35. doi: 10.1093/eurheartj/ehaa664
11. Duarte-Neto AN, Monteiro RAA, da Silva LFF, Malheiros D, de Oliveira EP, Theodoro-Filho J, et al. Pulmonary and systemic involvement in COVID-19 patients assessed with ultrasound-guided minimally invasive autopsy. Histopathology. (2020) 77:186–97. doi: 10.1111/his.14160
12. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. (2020) 395:1417–8. doi: 10.1016/S0140-6736(20)30937-5
13. Bois MC, Boire NA, Layman AJ, Aubry MC, Alexander MP, Roden AC, et al. COVID-19-associated nonocclusive fibrin microthrombi in the heart. Circulation. (2021) 143:230–43. doi: 10.1161/CIRCULATIONAHA.120.050754
14. Haslbauer JD, Tzankov A, Mertz KD, Schwab N, Nienhold R, Twerenbold R, et al. Characterisation of cardiac pathology in 23 autopsies of lethal COVID-19. J Pathol Clin Res. (2021) 7:326–37. doi: 10.1002/cjp2.212
15. Bosmuller H, Matter M, Fend F, Tzankov A. The pulmonary pathology of COVID-19. Virchows Arch. (2021) 478:137–50. doi: 10.1007/s00428-021-03053-1
16. Escher F, Pietsch H, Aleshcheva G, Bock T, Baumeier C, Elsaesser A, et al. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail. (2020) 7:2440–7. doi: 10.1002/ehf2.12805
17. Vinetti M, Haufroid V, Capron A, Classen JF, Marchandise S, Hantson P. Severe acute cardiomyopathy associated with venlafaxine overdose and possible role of CYP2D6 and CYP2C19 polymorphisms. Clin Toxicol. (2011) 49:865–9. doi: 10.3109/15563650.2011.626421
18. Elikowski W, Malek-Elikowska M, Ganowicz-Kaatz T, Fertala N, Zawodna M, Baszko A, et al. Transient left ventricular hypertrophy in a 30-year-old female with chronic emotional stress and depression treated with venlafaxine. Pol Merkur Lekarski. (2019) 47:144–9.
Keywords: COVID-19, heart, myocarditis acute and fulminant, thrombus, thromboinflammation
Citation: Menter T, Cueni N, Gebhard EC and Tzankov A (2021) Case Report: Co-occurrence of Myocarditis and Thrombotic Microangiopathy Limited to the Heart in a COVID-19 Patient. Front. Cardiovasc. Med. 8:695010. doi: 10.3389/fcvm.2021.695010
Received: 14 April 2021; Accepted: 30 June 2021;
Published: 29 July 2021.
Edited by:
Marijana Tadic, Universität Ulm, GermanyReviewed by:
Evgeny Belyavskiy, Charité – Universitätsmedizin Berlin, GermanyJelena Suzic Lazic, University Hospital Center Dr Dragiša Mišović, Serbia
Copyright © 2021 Menter, Cueni, Gebhard and Tzankov. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandar Tzankov, YWxleGFuZGFyLnR6YW5rb3ZAdXNiLmNo
 Thomas Menter
Thomas Menter Nadine Cueni2
Nadine Cueni2 Eva Caroline Gebhard
Eva Caroline Gebhard