- 1Arrhythmia Unit, Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China
- 2Department of Hepatobiliary Surgery, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China
- 3East Unit, Department of Cardiovascular Medicine, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China
- 4Department of Cardiology, Cedars-Sinai Medical Center, Smidt Heart Institute, Los Angeles, CA, United States
- 5Department of Cardiovascular Surgery, The First Affiliated Hospital of Xi'an Jiaotong University, Xi'an, China
Rationale: Chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA) have been identified as independent risk factors for cardiovascular diseases. However, the impact of COPD and OSA overlap syndrome (OS) on cardiovascular outcomes remains to be elucidated.
Objective: To determine the prevalence of cardiovascular events and their risk factors in OS patients.
Methods: Seventy-four patients who had OS between January 2015 and July 2020 were retrospectively enrolled, and 222 COPD-only patients and 222 OSA-only patients were pair-matched for age and sex from the same period and served as the OS-free control group. The prevalence rates of coronary heart disease (CHD), arrhythmia, heart failure, and pulmonary arterial hypertension (PAH) were compared among the three groups, and multivariable logistic regression models were used to screen the risk factors for specific cardiovascular events.
Results: OS patients had higher prevalence rates of heart failure (10.8 vs. 0.5 and 1.4%, respectively) and PAH (31.1 vs. 4.5 and 17.1%, respectively) than those with OSA alone or COPD alone (all P < 0.01). The CHD prevalence was also significantly higher in the OS group than in the COPD-alone group (25.7 vs. 11.7%, P < 0.01). There was no significant difference in the prevalence of arrhythmia among the three groups (20.3, 22.5, and 13.1%, respectively, P > 0.05). In OS patients, risk factors for CHD included hypertension, diabetes, body mass index, lactate dehydrogenase level, and tidal volume; risk factors for heart failure included diabetes, partial pressure of oxygen, partial pressure of carbon dioxide, maximum ventilatory volume, and neutrophilic granulocyte percentage; and risk factors for PAH included minimum nocturnal oxygen saturation, partial pressure of carbon dioxide, and brain natriuretic peptide and lactate dehydrogenase levels.
Conclusions: OS patients have a higher prevalence of cardiovascular events, which is associated with hypoxemia, hypercapnia, and impaired lung function in these patients.
Introduction
Chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea (OSA) are among the most prevalent chronic diseases and represent a major reason for health-care utilization, imposing a heavy health burden worldwide (1–3). The prevalence of COPD in American adults is estimated to be 13.9% (4, 5) compared with 13.7% in Chinese adults aged 40 years or older (6), and the incidence of OSA in adults is close to 9–26% (7). Existing epidemiological data suggest that overlap syndrome (OS), which refers to the coincidence of both COPD and OSA (8), is not a common disease in the general population (incidence ranges from 1 to 3.6%), but patients who already have COPD or OSA exhibit a significant increase in the incidence of overlap syndrome (2.9–65.9%) (9).
COPD is characterized by incomplete reversible airflow obstruction that increases the risk of cardiovascular disease through increased sympathetic nervous activity and persistent low-grade systemic inflammation (10, 11). Obstruction of the upper airway during sleep causes OSA, which leads to periodic apnea and hypopnea, resulting in nocturnal hypoxemia. Patients with OSA usually complain of severe snoring, problems with being awakened by wheezing or suffocation, and daytime sleepiness (12, 13). OSA has also been recognized as a risk factor for cardiovascular diseases. Possible pathophysiological mechanisms include transient and repeated oxygen desaturation, which could induce oxidative stress, systemic inflammation, endothelial dysfunction, and autonomic dysfunction (14).
Under the synergistic effect of COPD and OSA, patients with OS have lower nocturnal oxygen saturation, more profound oxidative stress, more serious systemic inflammation, more severe vascular endothelial dysfunction, and accelerated atherosclerosis (15–17), all of which are believed to be strong risk factors for cardiovascular disease. It is well known that COPD and OSA are independent risk factors for cardiovascular events. However, real-world evidence concerning the prevalence and related risk factors for cardiovascular diseases in patients with COPD and OSA overlap syndrome has rarely been reported. Therefore, this study aimed to evaluate the prevalence of specific cardiovascular events and their risk factors in patients with COPD and OSA overlap syndrome to help improve the management of these patients.
Methods
Study Design
This is a cross-sectional study, and anonymized clinical data were collected from the Biobank of the First Affiliated Hospital of Xi'an Jiaotong University from January 2015 to July 2020. The Ethics Committee of the First Affiliated Hospital of Xi'an Jiaotong University approved this study (no. XJTU1AF2020LSK-187), and informed consent was obtained. All methods were carried out in accordance with the relevant guidelines and regulations according to the principles expressed in the Declaration of Helsinki.
Subjects
The medical records of all patients who were diagnosed with COPD or OSA were retrospectively analyzed. The diagnoses were based on clinical expert consensus documents. COPD should have been considered in any patient with dyspnea, chronic cough or sputum production, a history of exposure to risk factors for the disease, and a post-bronchodilator forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) <0.70 as measured by spirometry. OSA was defined as symptoms such as excessive daytime sleepiness, recurrent awakenings from sleep, daytime fatigue, and impaired concentration, as well as overnight monitoring demonstrating five or more obstructed breathing events per hour during sleep (apnea/hypopnea index > 5). OS was defined as the simultaneous occurrence of COPD and OSA in the same patient (8, 18, 19). The exclusion criteria were as follows: (1) age > 80 or <18 years old; (2) lack of clinical data; (3) life expectancy less than 1 year; (4) severe COPD patients with noninvasive or invasive respiratory ventilators; (5) severe renal insufficiency (glomerular filtration rate <30 ml/min); (6) previous upper airway surgery for OSA; (7) a history of arrhythmias with a definitive cause (unrelated to the disease under study); and (8) unwillingness to participate in the study. The enrolled cohort was then divided into three groups: (1) OS group, (2) OSA-alone group, and (3) COPD-alone group. The two control groups were pair-matched with the OS group with respect to age and sex at a ratio of 1:3 (Figure 1).
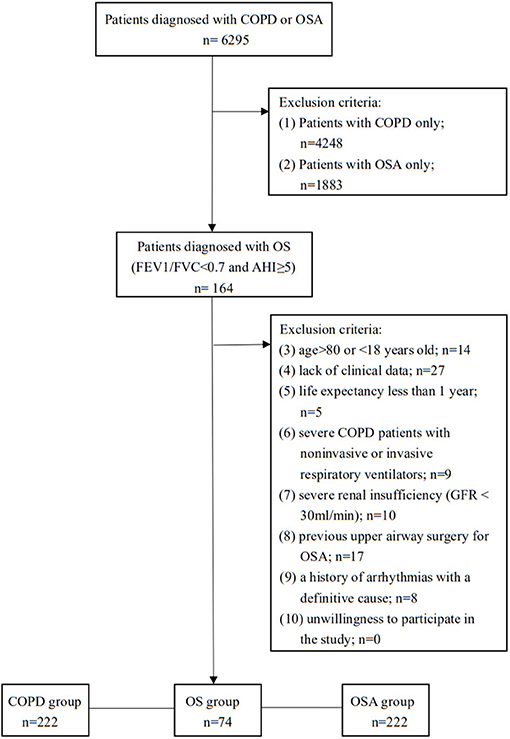
Figure 1. Study protocol. OS, overlap syndrome; OSA, obstructive sleep apnea; COPD, chronic obstructive pulmonary disease; AHI, apnea-hypopnea index; FEV1/FVC, forced expiratory volume in 1 s/forced vital capacity.
Data Collection
All data, including medical history, personal history, and laboratory examination, were obtained from the electronic medical record system of the hospital and recorded using a standardized protocol. Pulmonary function tests were performed according to the guidelines of the American Thoracic Society (20), and full-night polysomnography was performed in accordance with those of the American Academy of Sleep Medicine (21). All clinical diagnoses were made by professional staff according to standardized criteria.
Outcomes Measures
The primary endpoint in this study was to explore the prevalence rates of four specific types of cardiovascular diseases—coronary heart disease (CHD), heart failure, arrhythmia, and pulmonary arterial hypertension (PAH)—and whether there was any difference in prevalence between patients with OS and those with OSA alone or COPD alone. The secondary endpoint was to screen the risk factors for these diseases.
Statistical Analysis
The Kolmogorov–Smirnov test was used to test the normality of each data distribution. Categorical variables are reported as counts and percentages, whereas continuous variables are reported as the mean (X) and standard deviation. When comparing groups, the Kruskal–Wallis test was used if the data were not normally distributed, and analysis of variance with a post-hoc test was used if the data were normally distributed for continuous variables. The chi-squared test was used for categorical variables. When the ratio of variables to missing values was less than 5, the median of quantitative variables or the most common attribute values of qualitative data were used as simple assignments. Univariable logistic regression models were used to characterize OS compared with COPD alone or OSA alone, and multivariable logistic regression was used to explore the risk factors for cardiovascular diseases. Statistical analyses were conducted with SPSS v18.0.0. P < 0.05 were considered statistically significant.
Results
Characteristics of Study Participants
Of the 6,295 patients initially recruited to the study, 4,412 had COPD as the main diagnosis, and 2047 had OSA. Through a detailed screening, 74 consecutive patients identified to have overlap syndrome were enrolled in the OS group; 222 patients paired-matched for age and sex were enrolled in the OSA-alone group, and the same method was used to form the COPD-alone group (Figure 1).
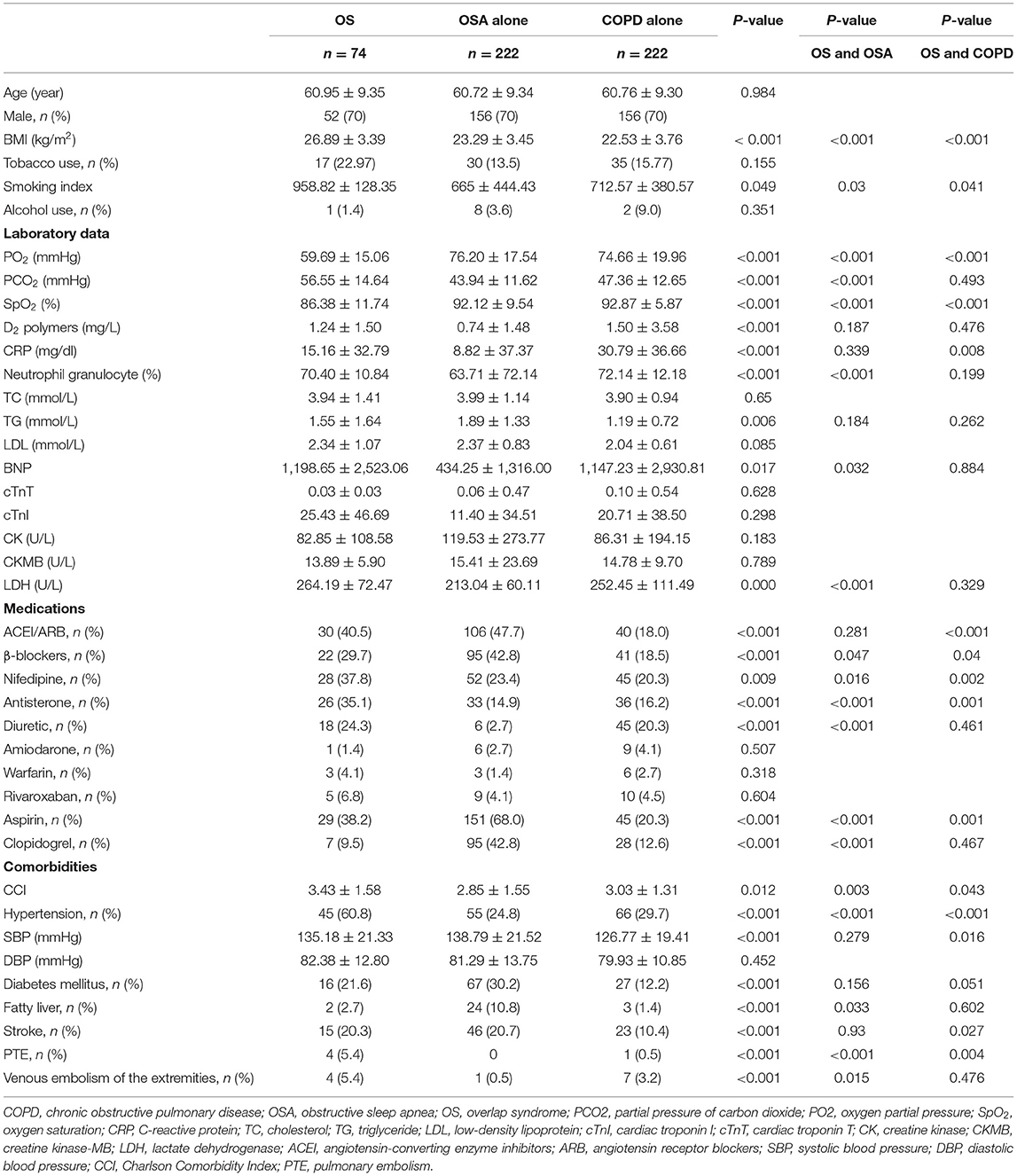
In this study, the prevalence rate of COPD in OSA patients was 8.01% (164/2047), and the prevalence rate of OSA in COPD patients was 3.72% (164/4412). The clinical characteristics of the study subjects with OS, OSA alone, and COPD alone are described in Table 1. The study cohort was predominantly composed of men (70%), with a mean age of 60.95 ± 9.35 years. The smoking index (P < 0.05), body mass index (BMI) (P < 0.01), and partial pressure of carbon dioxide (PCO2) (P < 0.01) were higher, and the partial pressure of oxygen (PO2) (P < 0.01) and oxygen saturation (SaO2) (P < 0.01) were lower in subjects with overlap syndrome than in those from the other two groups. The patients with OS had higher serum levels of brain natriuretic peptide (BNP), lactate dehydrogenase (LDH), and neutrophil granulocytes than the patients with OSA alone (all P < 0.05). However, the serum troponin levels and the number of patients who smoked or drank alcohol were similar between the three groups (Table 1).
Regarding medications, the number of patients using nifedipine and spironolactone in the OS group was significantly higher than that in the other two groups (P < 0.01), and the number of patients using angiotensin-converting enzyme inhibitors/angiotensin receptor blockers and beta-blockers in the OS group was significantly higher than that in the COPD-alone group (P < 0.01). The use of medications such as amiodarone, warfarin, or rivaroxaban was not significantly different among the three groups (Table 1).
For comorbidities, the Charlson comorbidity index was significantly higher in the OS group than in the COPD-alone group or OSA-alone group (P < 0.05). Six common comorbidities in these cohorts were evaluated: the prevalence of hypertension and pulmonary thromboembolism (PTE) in the OS group was significantly higher than that in the other two groups (P < 0.01); the prevalence of stroke in the OS group was higher than that in the COPD-alone group (P < 0.05); and the prevalence of venous embolism of the extremities in the OS group was higher than that in the OSA-alone group (P < 0.05). However, no significant difference was observed in the prevalence of diabetes among the three groups (Table 2).
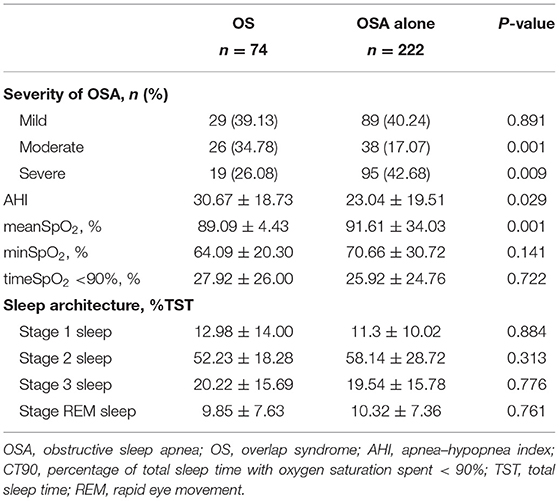
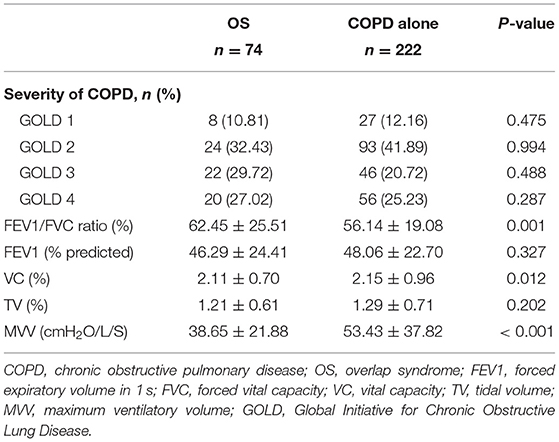
Polysomnography
In the overlap syndrome population, most patients were categorized as having mild/moderate OSA (mild = 39.13%, moderate = 34.78%), whereas, in the OSA-alone group, nearly half of the patients (42.68%) had severe OSA (Table 2). In the sleep testing study, the apnea/hypopnea index was much higher (30.67 ± 18.73 vs. 23.04 ± 19.51, P < 0.05), and the mean oxygen saturation (mean SpO2; 89.09 ± 4.43 vs. 91.61 ± 34.03, P < 0.01) was much lower in the OS group than in the OSA-alone group, whereas the minimum SpO2 and sleep architecture were not different between the two groups.
Pulmonary Function Test
There was no significant difference in the distribution of COPD severity between the OS group and COPD-alone group (P > 0.05), and FEV1% predicted was also comparable in both groups (P > 0.05). However, the FEV1/FVC ratio was significantly lower in the OS group than in the COPD alone group. Vital capacity and maximum ventilatory volume (MVV), which represent lung volume and pulmonary ventilation function, were lower in patients with overlap syndrome than in those with COPD alone (Table 3).
Prevalence of Cardiovascular Events
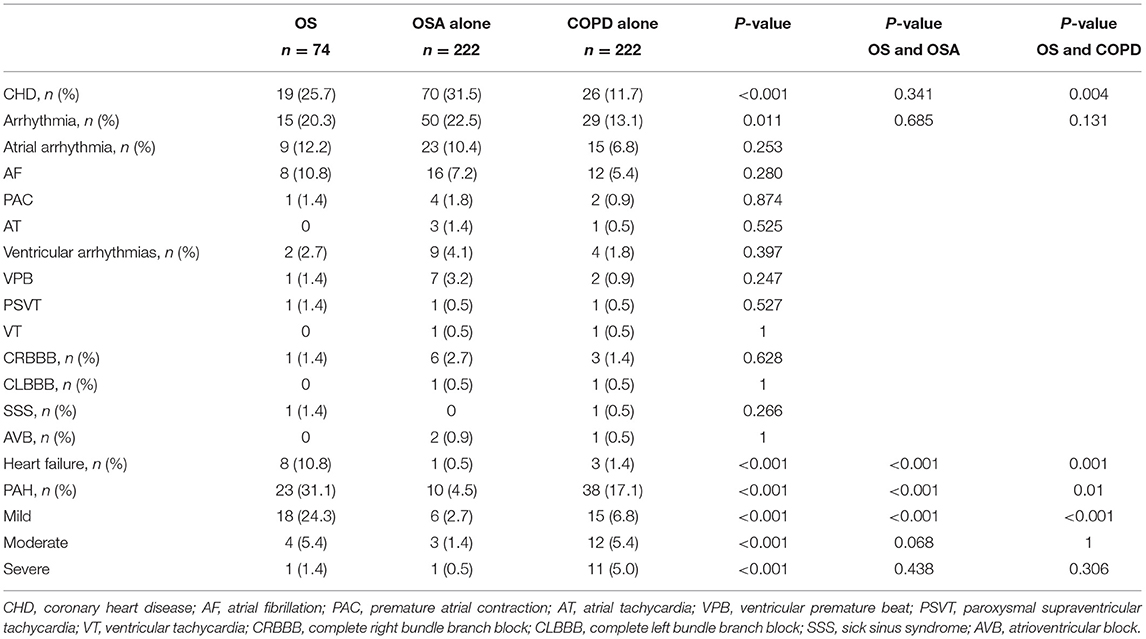
The prevalence rates of four cardiovascular events in the OS, OSA, and COPD groups were 25.7, 31.5, and 11.7% for CHD, 20.3, 22.5, and 13.1% for arrhythmias, 10.8, 0.5, and 1.4% for heart failure, and 31.1, 4.5, and 17.1% for PAH, respectively. The prevalence of heart failure and PAH in subjects with OS was significantly higher than in those with OSA or COPD alone (P < 0.01), and the prevalence of CHD in subjects with OS was higher than in those with COPD alone (P < 0.01). However, the prevalence of arrhythmias (such as atrial fibrillation, premature atrial contraction, ventricular premature contraction, and atrioventricular or ventricular tachycardia) was not significantly different between the OS group and OSA or COPD groups (Figure 2 and Table 4).
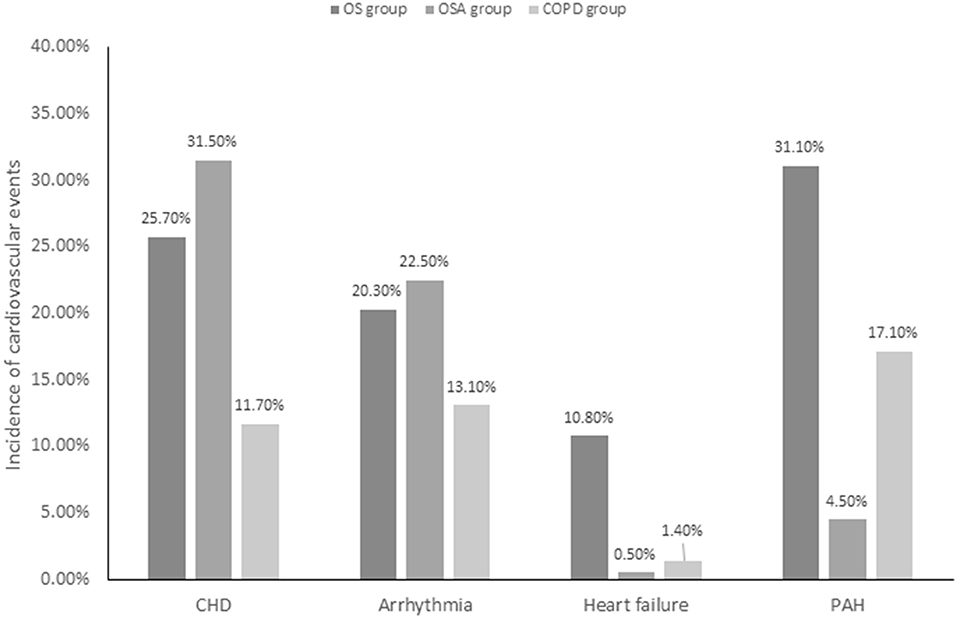
Figure 2. Incidence of cardiovascular events in study patients. OS, overlap syndrome; OSA, obstructive sleep apnea; COPD, chronic obstructive pulmonary disease; CHD, coronary heart disease; PAH, pulmonary arterial hypertension; PTE, pulmonary embolism.
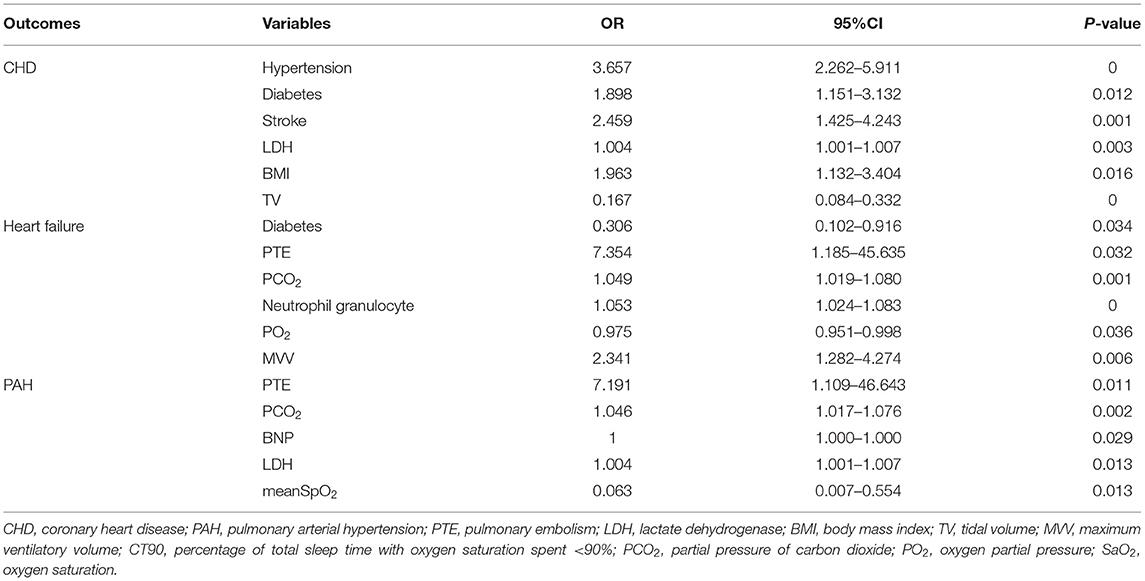
Risk Factors for Cardiovascular Events
Regarding the risk factors for cardiovascular diseases, multivariate logistic regression showed that hypertension, diabetes, stroke, LDH level, BMI, and tidal volume were positively correlated with CHD prevalence; diabetes, PTE, PCO2, PO2, MVV, and neutrophil granulocyte percentage were correlated with heart failure prevalence; and PTE, PCO2, BNP and LDH levels, and mean SpO2 were correlated with PAH prevalence (Table 5).
Discussion
In this study, a significant increase in the prevalence of cardiovascular events was observed in the OS population. Patients with OS had a higher prevalence of heart failure and PAH than those with COPD alone or OSA alone (P < 0.01), and the prevalence of CHD was also higher in the OS group than in the COPD-alone group (P < 0.01). In patients with OS, risk factors for CHD included hypertension, diabetes, stroke, BMI, LDH level, and tidal volume; risk factors for heart failure included diabetes, PTE, PO2, PCO2, MVV, and neutrophilic granulocyte percentage; and risk factors for PAH included PTE, PCO2, minSpO2, PCO2, and BNP and LDH levels. To the best of our knowledge, this study initially identifies the prevalence and risk factors for cardiovascular events in OS patients in an Asian population compared with both OSA-alone patients and COPD-alone patients.
Although the underlying mechanisms of exactly how OS contributes to cardiovascular events have not been fully elucidated, there are many pathways by which cardiovascular events occur in the presence of OS. The association between the burden of nocturnal hypoxemia, inflammation, and cardiovascular disease in our study is consistent with that found in other clinical investigations in this field (15, 22). In addition, we found that daytime hypoxemia and hypercapnia also contribute to the development of cardiovascular disease.
Hypoxemia is thought to act as a cardiovascular risk factor by increasing cardiac load, inducing oxidative stress by concomitant reactive oxygen species release, impairing vascular endothelial function (23), causing electrophysiological instability in the cardiac conduction system (24), and leading to severe metabolic disorder. Chronic hypoxia and hypercapnia caused by COPD and intermittent nocturnal hypoxia and sleep deprivation caused by OSA can lead to a decrease in the sensitivity of the respiratory center to both hypoxemia and hypercapnia stimulation in patients with OS, leading to further aggravated hypoxemia and hypercapnia. Previous studies confirmed that OS patients have more serious nocturnal hypoxemia, which has been considered a risk factor for cardiovascular diseases (22). However, our study evaluated not only nocturnal hypoxemia but also daytime hypoxemia and hypercapnia, and we found that patients with OS also had higher levels of daytime hypoxemia and hypercapnia than the COPD group or OSA group. Therefore, together with nocturnal hypoxemia, daytime hypoxemia and hypercapnia may have a synergistic effect on promoting cardiovascular diseases. This finding may have clinical implications for developing a better strategy for oxygen therapy in patients with OS.
Hypoxia can upregulate the expression of systemic inflammatory mediators (23, 24) and cause systemic inflammation, which is considered to be another important factor in cardiovascular diseases. There are many common molecular signaling pathways between COPD and OSA, such as C-reactive protein, interleukin 6, and nuclear factor kappa B. Their interaction can cause a systemic inflammatory response and increase body oxidative stress, leading to cardiovascular diseases. Baseline sustained hypoxemia in patients with OS predisposes them to other molecular responses relevant to the mechanisms of cardiovascular disease, especially via activation of the transcription factor pathway mediated by hypoxia-inducible factor-1 alpha (25) and related downstream products such as vascular endothelial growth factor. In this study, the level of serum C-reactive protein, a marker of inflammation, was higher in patients with overlap syndrome than in patients with COPD alone, indicating that OSA increased body's inflammatory stress in patients with COPD. There was no significant difference in serum C-reactive protein levels between the OS and OSA-alone groups. One plausible reason is that, in this study, the vast majority of patients in the OSA-alone group were admitted to the hospital for arrhythmias, and these patients already have a higher level of inflammation.
The prevalence of heart failure and PAH in subjects with OS in this study was significantly higher than in those with OSA or COPD alone, and the prevalence of CHD in subjects with OS was higher than in those with COPD alone, which has rarely been reported in real-world studies. No statistically significant difference in the prevalence of arrhythmia between the three groups was found in this study, although there have been studies confirming that patients with OS are at greater risk of AF than those with either COPD or OSA alone (26).
Multivariate logistic regression analysis showed that the prevalence rate of cardiovascular events in this study was correlated with hypertension, diabetes, stroke, PTE, BMI, BNP level, decreased pulmonary function, and nocturnal hypoxemia, which were already believed to be risk factors for cardiovascular diseases (22, 27). In logistic regression analysis, the risk factors for cardiovascular events included daytime hypoxemia and hypercapnia. Therefore, the high incidence of cardiovascular events in patients with OS was speculated to be ultimately caused by hypoxia, hypercapnia, and systemic inflammation. In our study, arterial blood gas analysis was performed in all patients to assess daytime hypoxemia and hypercapnia and is essential in identifying the promoting effect of daytime hypoxemia and hypercapnia on cardiovascular diseases. The benefits of continuous positive airway pressure (CPAP) are now clearly established in patients with OS. Marin and coauthors reported improved long-term survival and a lower rate of hospitalizations in over 200 OS patients treated with CPAP compared with those who were not treated, and the outcomes of those OS patients treated with CPAP were similar to those of patients with COPD alone over a median follow-up period of 9.4 years (28). So, it is reasonable to hypothesize that a more stringent treatment of hypoxia and hypercapnia may be beneficial for patients with overlap syndrome. A prospective, multicenter trial should be carried out to research the effect of improvement of daytime hypoxemia and hypercapnia on cardiovascular outcomes of patients with OS.
We acknowledge certain limitations in this study that should be highlighted when interpreting the findings. First, given the retrospective nature of the study, clinical information on every aspect of cardiovascular events and their risk factors in the cohort was not available; for example, data by Holter, or telemetry monitoring were missing, and therefore, the prevalence of paroxysmal arrhythmias could not be evaluated. Second, this is a single-center retrospective study with a small population. Third, the low incidence of overlap syndrome may lead to an analysis bias, although we enlarged the sample size of the control groups to increase the credibility of the data.
Conclusion
Patients with OS are at greater risk of cardiovascular events than patients with either COPD or OSA alone, which is related to their impaired pulmonary function, severe hypoxemia, and hypercapnia. It is of great importance for clinical physicians to diagnose and treat patients with OS, promote the management of these patients and improve their quality of life.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Xi'an Jiaotong University (No. XJTU1AF2020LSK-187). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MT and YL: methodology, writing, and original draft preparation. MT, SL, and XY: data curation and investigation. TS: supervision, writing, reviewing, and editing the manuscript. All authors provided critical review of the manuscript and approved the final draft for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful to Dr. Guoliang Li for his valuable comments on this manuscript and the Biobank of the First Affiliated Hospital of Xi'an Jiaotong University for providing clinical data.
References
1. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Arch Bronconeumol. (2017) 53:128–49. doi: 10.1016/j.arbr.2017.02.001
2. Malhotra A, Orr JE, Owens RL. On the cutting edge of obstructive sleep apnoea: where next? Lancet Respir Med. (2015) 3:397–403. doi: 10.1016/S2213-2600(15)00051-X
3. Lévy P, Kohler M, McNicholas WT, Barbé F, McEvoy RDVKS, et al. Obstructive sleep apnoea syndrome. Nat Rev Dis Primers. (2015) 1:15015. doi: 10.1038/nrdp.2015.24
4. Jemal A, Ward E, Hao Y, Thun M. Trends in the leading causes of death in the United States, 1970–2002. JAMA. (2005) 294:1255–9. doi: 10.1001/jama.294.10.1255
5. Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. (2000) 160:1683–9. doi: 10.1001/archinte.160.11.1683
6. Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China. (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. (2018) 391:1706–17. doi: 10.1016/S0140-6736(18)30841-9
7. Young T, Palta M, Dempsey J, Skatrud J, Webe S, Bad S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. (1993) 32:1230–5:1230–5. doi: 10.1056/NEJM199304293281704
8. McNicholas WT. Chronic obstructive pulmonary disease and obstructive sleep apnea: overlaps in pathophysiology, systemic inflammation, and cardiovascular disease. Am J Respir Crit Care Med. (2009) 180:692–700. doi: 10.1164/rccm.200903-0347PP
9. Shawon MS, Perret JL, Senaratna CV, Lodge C, Hamilton GS, Dharmage SC. Current evidence on prevalence and clinical outcomes of co-morbid obstructive sleep apnea and chronic obstructive pulmonary disease: a systematic review. Sleep Med Rev. (2017) 32:58–68. doi: 10.1016/j.smrv.2016.02.007
10. Sin DD, Man SF. Chronic obstructive pulmonary disease: a novel risk factor for cardiovascular disease. Can J Physiol Pharmacol. (2005) 83:8–13. doi: 10.1139/y04-116
11. Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease. (COPD). Lancet. (2004) 364:613–20. doi: 10.1016/S0140-6736(04)16855-4
12. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. (2011) 86:549–54. doi: 10.4065/mcp.2010.0810
13. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. (2009) 5:263–76. doi: 10.5664/jcsm.27497
14. Parish JM, Somers VK. Obstructive sleep apnea and cardiovascular disease. Mayo Clin Proc. (2004) 79:1036–46. doi: 10.4065/79.8.1036
15. Shiina K, Tomiyama H, Takata Y, Yoshida M, Kato K, Nishihata Y, et al. Overlap syndrome: additive effects of COPD on the cardiovascular damages in patients with OSA. Respir Med. (2012) 106:1335–41. doi: 10.1016/j.rmed.2012.05.006
16. McNicholas WT. Diagnosis of obstructive sleep apnea in adults. Proc Am Thorac Soc. (2008) 5:154–60. doi: 10.1513/pats.200708-118MG
17. Chaouat A, Weitzenblum E, Krieger J, Ifoundza T, Oswald M, Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am J Respir Crit Care Med. (1995) 151:82–6. doi: 10.1164/ajrccm.151.1.7812577
18. Culver BH, Graham BL, Coates AL, Wanger J, Berry CE, Clarke PK, et al. Recommendations for a standardized pulmonary function report. An official american thoracic society technical statement. Am J Respir Crit Care Med. (2017) 196:1463–72. doi: 10.1164/rccm.201710-1981ST
19. Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of sleep medicine. J Clin Sleep Med. (2012) 8:597–619. doi: 10.5664/jcsm.2172
20. MacNee W. Oxidants/antioxidants and COPD. Chest. (2000) 117(5 Suppl 1):303S–17S. doi: 10.1378/chest.117.5_suppl_1.303S-a
21. Cortassa S, Aon MA, Marban E, Winslow RL, O'Rourke B. An integrated model of cardiac mitochondrial energy metabolism and calcium dynamics. Biophys J. (2003) 84:2734–55. doi: 10.1016/S0006-3495(03)75079-6
22. Kendzerska T, Leung RS, Aaron SD, Ayas N, Sandoz JS, Gershon AS, et al. Cardiovascular outcomes and all-cause mortality in patients with obstructive sleep apnea and chronic obstructive pulmonary disease (Overlap Syndrome). Annals Am Thoracic Soc. (2019) 16:71–81. doi: 10.1513/AnnalsATS.201802-136OC
23. Takabatake N, Nakamura H, Abe S, Inoue S, Hino T, Saito H, et al. The relationship between chronic hypoxemia and activation of the tumor necrosis factor-alpha system in patients with chronic obstructive pulmonary disease. Am J Resp Crit Care. (2000) 161:1179–84. doi: 10.1164/ajrccm.161.4.9903022
24. Zamarron C, Garcia Paz V, Morete E, del Campo Matias F. Association of chronic obstructive pulmonary disease and obstructive sleep apnea consequences. Int J Chron Obstruct Pulmon Dis. (2008) 3:671–82. doi: 10.2147/COPD.S4950
25. Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. (2005) 112:2660–7. doi: 10.1161/CIRCULATIONAHA.105.556746
26. Akinnusi M, El-Masri AR, Lawson Y, El-Solh AA. Association of overlap syndrome with incident atrial fibrillation. Intern Emerg Med. (2021) 16:633–42. doi: 10.1007/s11739-020-02469-y
27. Hu W, Zhao Z, Wu B, Shi Z, Dong M, Xiong M, et al. Obstructive sleep apnea increases the prevalence of hypertension in patients with chronic obstructive disease. COPD. (2020) 17:523–32. doi: 10.1080/15412555.2020.1815688
Keywords: chronic obstructive pulmonary disease, risk stratification, cardiac rhythm abnormalities, obstructive sleep apnea, overlap syndrome, cardiovascular events
Citation: Tang M, Long Y, Liu S, Yue X and Shi T (2021) Prevalence of Cardiovascular Events and Their Risk Factors in Patients With Chronic Obstructive Pulmonary Disease and Obstructive Sleep Apnea Overlap Syndrome. Front. Cardiovasc. Med. 8:694806. doi: 10.3389/fcvm.2021.694806
Received: 13 April 2021; Accepted: 21 June 2021;
Published: 14 July 2021.
Edited by:
Tong Liu, Tianjin Medical University, ChinaReviewed by:
Alexandru Corlateanu, Nicolae Testemitanu State University of Medicine and Pharmacy, MoldovaLigang Ding, Chinese Academy of Medical Sciences, China
Datun Qi, Fuwai Central China Cardiovascular Hospital, China
Radostina Cherneva, Medical University, Sofia, Bulgaria
Copyright © 2021 Tang, Long, Liu, Yue and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Shi, c2hpdGFvMDY4QHhqdHUuZWR1LmNu
 Manyun Tang
Manyun Tang Yunxiang Long2
Yunxiang Long2 Tao Shi
Tao Shi