- Department of Cardiac Surgery, Beijing Anzhen Hospital, Capital Medical University, Beijing, China
Background and Aims: The impact of obstructive sleep apnea (OSA) on perioperative myocardial infarction (PMI) following coronary artery bypass grafting (CABG) remains unclear. Off-pump CABG (OPCABG) has become a common practice for CABG in China. The present study investigated mainly the correlation between OSA and PMI following OPCABG.
Methods: In this prospective observational single-center study, consecutive eligible patients listed for elective OPCABG underwent cardiorespiratory polygraphy before surgery between January 2019 and June 2020. OSA was defined as an apnea-hypopnea index (AHI) ≥15 events/h. The primary end point was perioperative myocardial infarction (PMI) following OPCABG (type 5 MI).
Results: Patients with OSA accounted for 42.2% (62/147) of the cohort. Twenty-four patients (16.3%) met the protocol criteria for PMI: 17 (27.4%) in the OSA group and 7 (8.2%) in the non-OSA group (P = 0.002). Multivariate logistic regression analysis revealed that AHI (OR = 1.115, 95% CI 1.066 to 1.166, P < 0.001), high-sensitivity c-reactive protein (hs-CRP) (OR = 1.080, 95% CI 1.025 to 1.138, P = 0.004), and SYNTAX score (OR = 1.098, 95% CI 1.056 to 1.141, P < 0.001) were associated with PMI incidence. Furthermore, ROC analysis revealed that the AHI (AUC = 0.766, 95% CI 0.689 to 0.832, P < 0.001) and SYNTAX score (AUC = 0.789, 95% CI 0.715 to 0.852, P < 0.001) had predictive value for PMI. In addition, multiple linear regression analysis showed that the AHI was an independent influencing factor of hs-CRP (B = 0.176, 95% CI 0.090 to 0.263, P < 0.001) and the SYNTAX score (B = 0.553, 95% CI 0.397 to 0.709, P < 0.001).
Conclusions: OSA was independently associated with a higher incidence of PMI following OPCABG, and the formation of severe coronary atherosclerotic lesions aggravated by an enhanced inflammatory response might be the potential mechanism. The efficacy of CPAP treatment for improving prognosis after CABG remains to be further investigated.
Introduction
Coronary artery bypass grafting (CABG) is the standard of care for patients with extensive coronary artery disease (CAD). Techniques to perform CABG without cardiopulmonary bypass (off-pump CABG, OPCABG) have emerged to reduce complications associated with cardiopulmonary bypass and manipulation of the aorta, especially for higher-risk patients who could benefit from short-term prognosis improvement (1). Despite decades of refinement, perioperative myocardial infarction (PMI) following CABG, with an incidence of 1.9–30%, remains a major predictor of increased cardiovascular mortality and healthcare resource utilization (2–4). Therefore, it is necessary to identify high-risk patients with PMI and initiate targeted treatment in advance.
Obstructive sleep apnea (OSA), characterized by recurrent episodes of partial or complete collapse of the upper airway during sleep, is highly prevalent in patients with CAD (5). OSA has been proven to be closely related to the degree of coronary atherosclerosis and myocardial infarction through activation of proinflammatory responses, oxidative stress, sympathetic excitation, platelets, or metabolic dysregulation (6). Compared with the general population, OSA, diagnosed by an apnea-hypopnea index (AHI) ≥15, has a significantly higher prevalence of ~50% in CABG patients (7). Considerable evidence has confirmed that OSA is strongly correlated with increased risks of new revascularization, typical angina, atrial fibrillation and prolonged length of hospital stay after CABG (7, 8); however, the impact of OSA on PMI following CABG is still unclear. Therefore, we investigated mainly the correlation between OSA and PMI following OPCABG (type 5 MI), which was defined by the fourth universal definition of MI (9).
Materials and Methods
Study Design
This prospective observational single-center study was conducted in Beijing Anzhen Hospital, Capital Medical University. We enrolled consecutive patients with coronary artery disease who were scheduled to undergo elective OPCABG and had not been diagnosed with OSA from January 2019 to June 2020. The study protocol, which was approved by the institutional review board (Approval No.: 2013025), was explained to all patients, all of whom signed informed consent.
Patients
All participating patients, who were between 40 and 75 years old, underwent an overnight sleep study before OPCABG. The exclusion criteria were as follows: preoperative treatment with an intra-aortic balloon pump (IABP), pulmonary insufficiency (e.g., chronic obstructive pulmonary disease), central sleep apnea (≥50% central events or central AHI ≥10/h), body temperature >37.5°C, combination with other surgeries, on-pump CABG, and sleep study failure (patients without adequate signal recording).
Overnight Sleep Study
Overnight sleep studies were performed after clinical stabilization (within 1 week after admission) by portable cardiorespiratory polygraphy (ApneaLink, Resmed, Australia), which might provide high diagnostic accuracy and offer an accessible alternative to full polysomnography. The reported sensitivity and specificity were 0.88 and 0.84, respectively (10). Nasal airflow, arterial oxygen saturation, thoracoabdominal movements, and snoring episodes were recorded. Sleep studies were scored according to the American Academy of Sleep Medicine 2007 guidelines (11). Apnea was defined as an absence of airflow lasting ≥10 s (obstructive if thoracoabdominal movement was present and central if thoracoabdominal movement was absent). Hypopnea was defined as a reduction in airflow of >30% for ≥10 s and associated with a decrease in arterial oxygen saturation >4%. AHI was defined as the number of apneas and hypopneas per hour of total recording time. The oxygen desaturation index (ODI) was the number of times that oxygen saturation decreased by >3% per hour. Recruited patients were categorized into OSA (AHI ≥ 15 events/h) and non-OSA (AHI <15 events/h) groups. A satisfactory polygraphy signal recorded for a minimum of 3 h was considered a valid test. All studies were double-scored manually by independent sleep technologists. Further, scoring was performed in cases of discrepancy by a senior consultant in sleep medicine. All OSA patients were recommended for further evaluation and consideration of continuous positive airway pressure (CPAP) therapy after discharge.
OPCABG
Surgical indications were in accordance with the guidelines (12). The same experienced cardiac surgeon (Y.Y.) performed all surgeries. The quality of graft anastomosis met the criteria recommended by the Operation Quality Committee of Beijing Anzhen Hospital. Measurement of graft flow and pulsatility index (PI) was performed by placing a handheld flow probe (MediStim, Oslo, Norway) around the graft. After surgery, the patients were monitored in the intensive care unit (ICU) until ventilator removal, and vital signs were stable. Perioperative management was conducted according to the guidelines (13). Within 48 h after OPCABG, myocardial markers were routinely tested every 6 h, and electrocardiogram (ECG) and echocardiography were performed every 12 h.
Outcome
The primary end point was CABG-related MI ≦48 h after the operation (type 5 MI), also known as perioperative myocardial infarction (PMI), defined by the fourth universal definition of MI [cardiac troponin (cTn) >10 times the 99th percentile upper reference limit or a rise of cTn values >20% if the baseline values were elevated or falling, in addition to ECG changes, angiographic findings or new regional wall motion abnormalities] (9). All relevant data were independently judged by two experienced doctors (L.H. L, D.X.H.), who were blinded to sleep study results.
Statistical Analyses
For continuous variables, a normal distribution was assessed using the Kolmogorov-Smirnov test. Continuous variables are shown as the mean ± SD or median (first and third quartiles) and were compared by using Student's t-test or the Mann-Whitney U-test. Categorical variables are presented as percentages and were compared using the chi-square test. To analyze the association between PMI and other variables, multivariate logistic regression analysis was implemented (demographic characteristics, cardiovascular risk factors and variables with p < 0.1 in the univariate logistic regression were included in the model). Additionally, we assessed the predictive value of AHI, SYNTAX score and high-sensitivity c-reactive protein (hs-CRP) for PMI through receiver operating characteristic (ROC) curve analysis. The predictive values were evaluated with the area under the curve (AUC), and the difference in the AUC with statistical significance was assessed with the DeLong test. Furthermore, the correlation between AHI and hs-CRP or SYNTAX score was determined by multivariate linear regression analysis (the model included demographic characteristics, cardiovascular risk factors and variables with p < 0.1 in the univariate linear regression). All analyses were conducted with SPSS 24.0 (SPSS., Chicago, IL, USA) and MedCalc V.11.4 (MedCalc, Inc., Ostend, Belgium) assuming a 2-sided test with a 5% level of significance.
Results
Basic Characteristics and Overnight Sleep Study Results
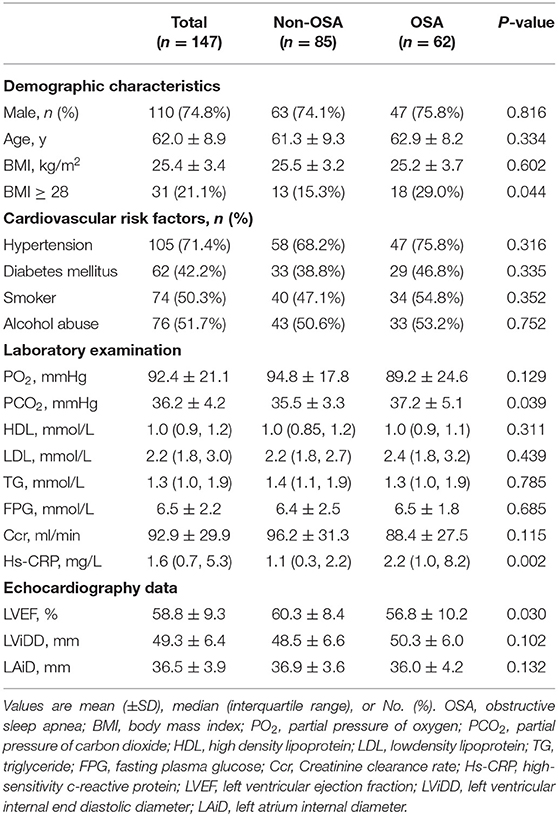
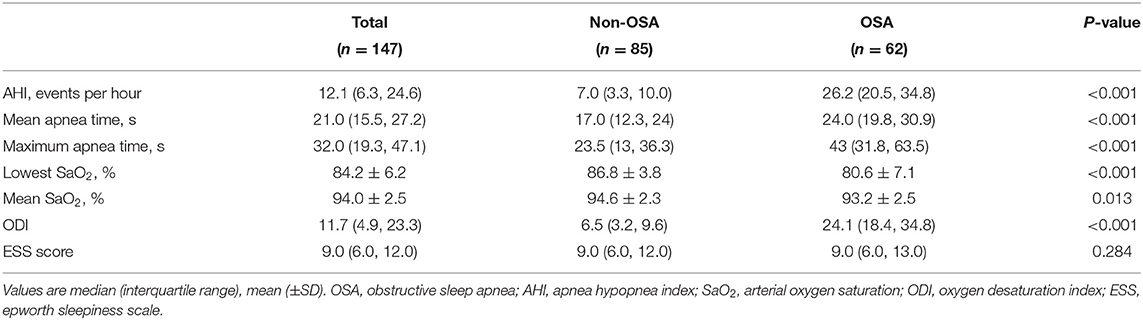
A total of 215 consecutive eligible patients scheduled for OPCABG were prospectively enrolled. After exclusion of 68 patients, 147 patients were included (Figure 1). The mean age of the patients recruited was 62.0 ± 8.9 years, and 74.8% were male. Patients with OSA accounted for 42.2% of the cohort and exhibited higher PCO2, percentage of BMI ≥ 28, hs-CRP levels and lower LVEF than the non-OSA group (Table 1). The median AHI level of patients with OSA was 26.2 (interquartile range, 14.3), and they had longer mean and maximum apnea times, higher oxygen desaturation indices, and lower lowest and mean arterial oxygen saturations than those without OSA (Table 2).
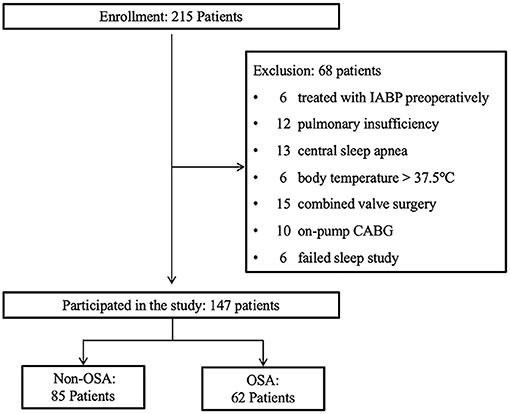
Figure 1. Study design flowchart. IABP, intra-aortic ballon pump; CABG, coronary artery bypass grafting; OSA, obstructive sleep apnea.
Angiographic and Surgical Characteristics
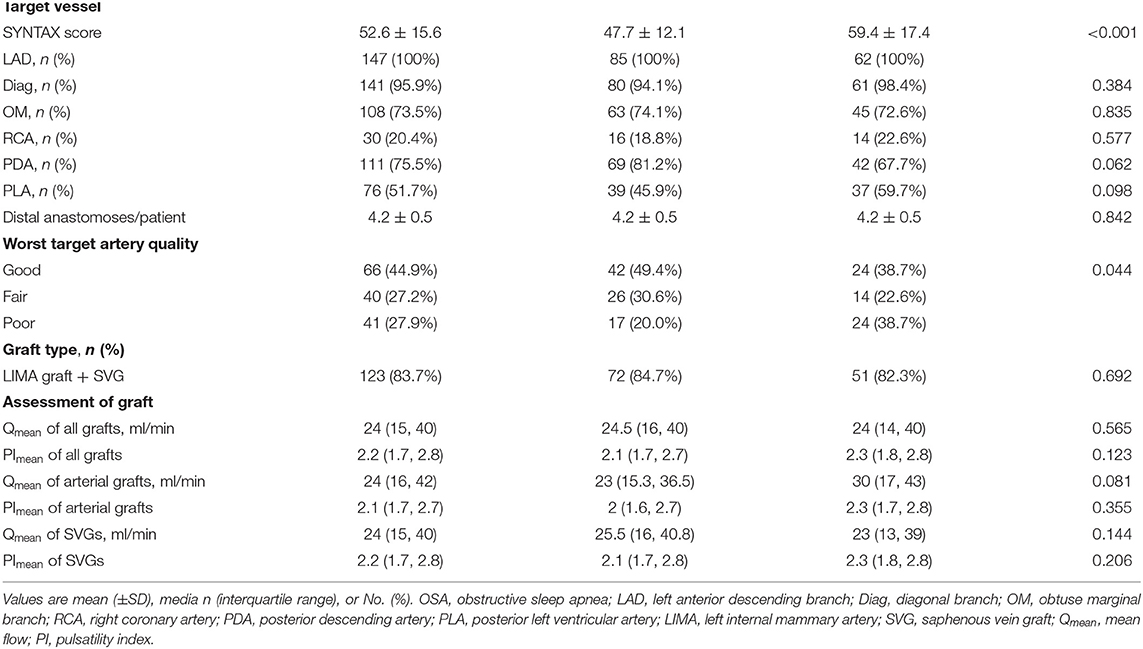
Angiographic and OPCABG surgical characteristics are shown in Table 3. The mean SYNTAX score of all patients was 52.6 ± 15.6, and in the OSA group, it was significantly higher than that in the non-OSA group (P < 0.001). The number of target vessels, distal anastomoses/patient, graft type, and assessment of grafts did not differ between the OSA and non-OSA groups.
Primary End Point
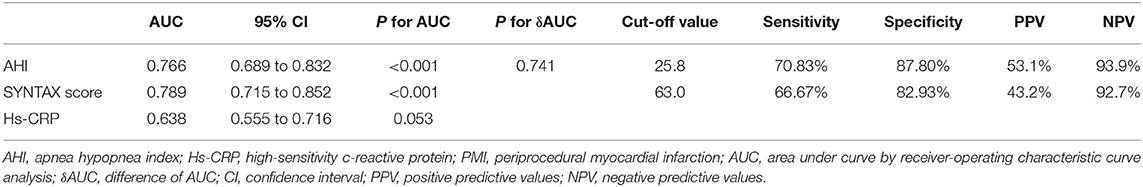
Twenty-four patients (16.3%) met the protocol criteria for PMI: 17 (27.4%) in the OSA group and 7 (8.2%) in the non-OSA group (P = 0.002) (Figure 2). Among the 24 cases, there were 6, 6 and 12 cases of PMI of the anterior, lateral and inferior wall, respectively, and there was no significant difference between the OSA group and non-OSA group. Extracorporeal membrane oxygenation (ECMO) and IABP were used in 1 and 6 patients, respectively; two cases died of PMI. Univariate logistic regression analysis revealed that AHI (OR = 1.088, 95% CI 1.050 to 1.127, P < 0.001), hs-CRP (OR = 1.075; 95% CI 1.027 to 1.125, P = 0.002) and SYNTAX score (OR = 1.086, 95% CI 1.049 to 1.123, P < 0.001) were strongly associated with an increased risk of developing PMI (Table 4). After adjustments for sex, age, BMI, hypertension, diabetes mellitus, smoking status, alcohol abuse, and left atrial internal diameter through multivariate logistic regression analysis, the correlation persisted (OR = 1.115, 95% CI 1.066 to 1.166, P < 0.001; OR = 1.080, 95% CI 1.025 to 1.138, P = 0.004; OR = 1.098, 95% CI 1.056 to 1.141, P < 0.001, respectively) (Table 5). As the ROC analysis revealed, the AHI (AUC = 0.766, 95% CI 0.689 to 0.832, P < 0.001) and SYNTAX score (AUC = 0.789, 95% CI 0.715 to 0.852, P < 0.001) had predictive value for PMI (Table 6).
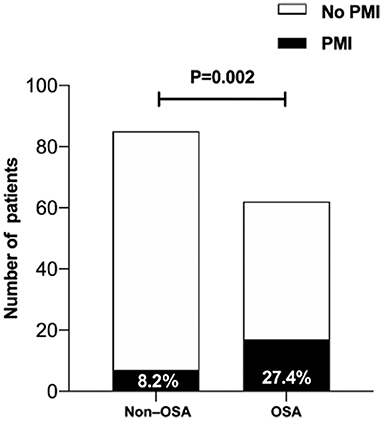
Figure 2. The proportion of patients with PMI in the moderate-severe OSA group was significantly higher than in the non-OSA group. PMI, periprocedural myocardial infarction; OSA, obstructive sleep apnea.
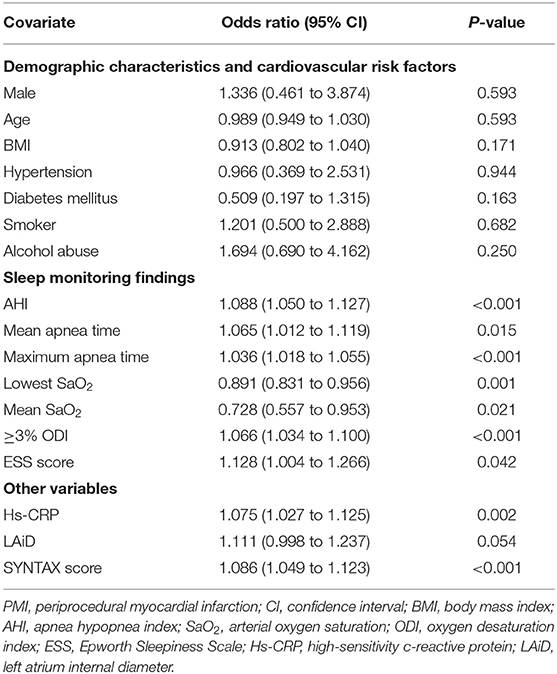
Table 4. Univariate logistic regression analysis for the correlation between various indicators and PMI.
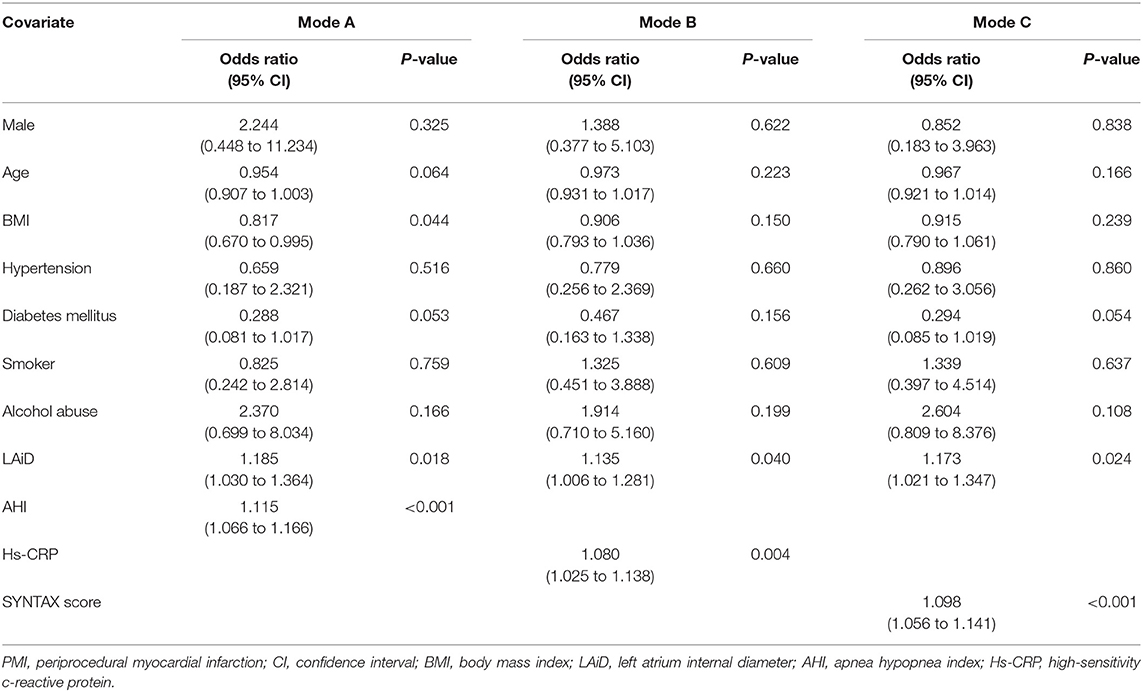
Table 5. Multivariate logistic regression analysis for the correlation between various indicators and PMI.
AHI Was Strongly Correlated With hs-CRP and SYNTAX Score
As demonstrated in Table 7, multiple linear regression analysis showed that AHI was independently associated with hs-CRP (B = 0.176, 95% CI 0.090 to 0.263, P < 0.001) and SYNTAX score (B = 0.553, 95% CI 0.397 to 0.709, P < 0.001).
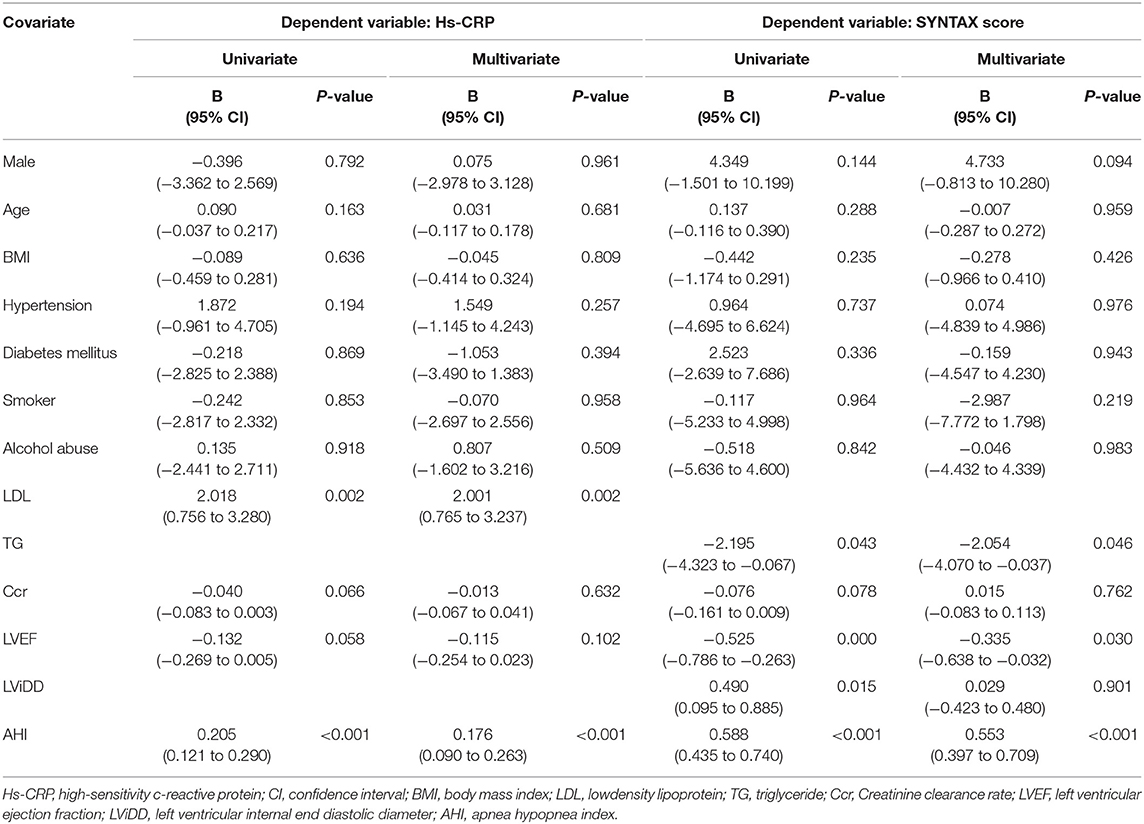
Table 7. Univariate and multivariate linear regression analysis for the independent influencing factors of hs-CRP level and SYNTAX score.
Discussion
To the best of our knowledge, this is the first study to evaluate the impact of OSA on PMI following OPCABG. In this prospective cohort of 147 patients who underwent OPCABG, the prevalence of OSA was 42.2%, and compared with in non-OSA patients, PMI was more likely to occur in patients with OSA. AHI, hs-CRP, and SYNTAX score were independent risk factors for PMI. In regard to identifying patients at high risk of having PMI, the AHI, and SYNTAX score could provide a superior discriminatory ability to that of hs-CRP. In addition, AHI was associated with changes in hs-CRP and SYNTAX score.
Along with the in-depth understanding of the pathogenesis and prognostic significance of PMI following CABG, different definitions have emerged, and the incidence of PMI ranges from 1.9 to 30% depending on different diagnostic criteria and patient populations (2, 3). The Fourth Universal Definition of Myocardial Infarction (2018) (9), applied in this study, remains the accepted standard in contemporary clinical practice. In addition, the diagnosis of PMI in several large randomized controlled trials was based on the creatine kinase-myocardial band (CK-MB) (14), but recently, the ESC Study Group on Cardiac Biomarkers of the Association for Acute Cardiovascular Care suggested that CK-MB be eliminated from the menu of biomarkers available since it was less sensitive and clinically instructive than cTn (15). We diagnosed patients based on cTn combined with other presentations and found that PMI following OPCABG occurred in 16.3% of patients with severe coronary lesions (mean SYNTAX score was 52.6).
An analysis from the EXCEL (Evaluation of XIENCE vs. Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial showed that PMI was associated with cardiovascular death and all-cause death at 3 years (16). In a Korean registry of 3,183 patients who underwent CABG, the presence of PMI was associated with increased risks of major cardiovascular events at the 5-year follow-up regardless of the PMI definition (2). PMI can be ascribed to multiple causes. In the EXCEL trial, age, chronic obstructive pulmonary disease, and aortic cross-clamp duration were independent predictors of PMI following CABG (16). Other well-established risk factors for PMI include left main coronary artery disease, recent MI, unstable angina, emergent operations, poor target-artery quality, inadequate revascularization, and prolonged bypass duration (17). However, few studies have focused on OPCABG. Our findings extend those of previous studies by proposing that OSA increases the risk of PMI in patients who underwent OPCABG. Of note, we found no significant correlation between the incidence of PMI and the measurement index of graft (flow and PI), the reason for this result might be that all indices met the quality control standard (flow>15/min and PI < 5.0) (18).
OSA has been advocated as a new emerging contributor to the development of CAD by guidelines and expert consensus (19, 20), and intravascular ultrasound has indicated that patients with OSA present a larger total atheroma volume in the coronary artery (21). The SYNTAX (SYNergy between PCI with TAXUS and Cardiac Surgery) score was created, more than a decade ago, to provide an angiographic tool grading the complexity of coronary artery disease in patient with left main or multivessel disease, and it relates to CAD outcomes (22). Evidence has revealed that OSA significantly correlates with the SYNTAX score (23). Our study supported this finding and further demonstrated that both the AHI and SYNTAX score could identify patients at high risk for developing PMI following OPCABG; however, the accuracy is still moderate, and their performance should be further explored.
Intermittent hypoxia (IH), sleep fragmentation, and intrathoracic pressure swings in OSA appear to promote the development of cardiovascular disease, and inflammation is proposed as an intermediate mechanism linking OSA with the severity of coronary lesions (6). IH appears to facilitate atheromatous lesion formation by promoting systemic inflammation, partially via activation of the transcription factor NF-κB (24). The most studied biomarker in this context is hs-CRP, which has been demonstrated to participate actively in atherosclerosis via the induction and enhanced expression of adhesion molecules (25). Our findings were consistent with previous literature: hs-CRP levels were strongly associated with the severity of OSA. We added further evidence that the hs-CRP level was an independent risk factor for PMI following OPCABG; however, its limited predictive value for PMI might be due to its susceptibility to multiple interference factors.
In addition, evidence has confirmed that patients with OSA show reduced fibrinolytic capacity (26) and increased platelet activation and aggregation (27), all of which may contribute to PMI via thrombotic events of grafts or native vessels after CABG.
CPAP remains the standard of care for patients with OSA, and evidence has revealed that it is correlated with a reduced inflammatory response (28) and coagulability (29), as well as improvement in early signs of atherosclerosis (30), suggesting that CPAP may improve the prognosis of coronary revascularization. Wu et al. (31) reported that untreated moderate-to-severe OSA was independently correlated with a significantly increased risk of repeat revascularization after percutaneous coronary intervention (PCI). Cassar et al. (32) found that screening for and treating OSA (CPAP) in patients who underwent PCI might result in decreased cardiac death. However, we know little about the role of CPAP in reducing the incidence of complications after CABG. In consideration of our previous clinical practice, we speculate that patient compliance and timing of CPAP treatment after CABG may be the key to curative effects. Additional trials evaluating the effects of CPAP in patients with OSA who underwent CABG are warranted.
This study has several limitations. First, this was a single-center study with a limited sample size, and the results need to be validated through multicenter, large-sample studies. Follow-up of the cohort is needed. Second, compared with polysomnography, portable cardiorespiratory polygraphy may underestimate the severity of OSA, but it is safe and simple to identify OSA in a high-risk patient population (11). Finally, mechanical ventilation treatment after surgery might weaken the short-term effect of OSA to a certain extent.
Conclusions
This prospective cohort study demonstrated for the first time that OSA was independently associated with a higher incidence of PMI following OPCABG, and the formation of severe coronary atherosclerotic lesions aggravated by an enhanced inflammatory response might be the potential mechanism. The efficacy of CPAP treatment for improving prognosis after CABG remains to be further explored.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study was approved by the Institutional Review Board of Beijing Anzhen Hospital of Capital Medical University (Approval No: 2013025). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KF, MG, and YY: study concept and design. KF, MG, WY, HL, LC, and XD: acquisition, analysis, or interpretation of data. KF and MG: drafting of the manuscript. WY and YY: obtained funding. All authors: critical revision of the manuscript for important intellectual content, read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (81770343). The funds were used to acquire portable sleep monitors for the study. The sponsor had no role in the design or conduct of this research.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors of this study would like to thank all the study participants.
References
1. Chikwe J, Lee T, Itagaki S, Adams DH, Egorova NN. Long-term outcomes after. off-pump versus on-pump coronary artery bypass grafting by experienced surgeons. J Am Coll Cardiol. (2018) 72:1478–86. doi: 10.1016/j.jacc.2018.07.029
2. Cho MS, Ahn JM, Lee CH, Kang DY, Lee JB, Lee PH, et al. Differential rates and clinical significance of periprocedural myocardial infarction after stenting or bypass surgery for multivessel coronary disease according to various definitions. JACC Cardiovasc Interv. (2017) 10:1498–507. doi: 10.1016/j.jcin.2017.05.051
3. Thielmann M, Sharma V, Al-Attar N, Bulluck H, Bisleri G, Bunge JJH, et al. ESC joint working groups on cardiovascular surgery and the cellular biology of the heart position paper: perioperative myocardial injury and infarction in patients undergoing coronary artery bypass graft surgery. Eur Heart J. (2017) 38:2392–407. doi: 10.1093/eurheartj/ehx383
4. Chen JC, Kaul P, Levy JH, Haverich A, Menasché P, Smith PK, et al. Myocardial infarction following coronary artery bypass graft surgery increases healthcare resource utilization. Crit Care Med. (2007) 35:1296–301. doi: 10.1097/01.CCM.0000262403.08546.A2
5. Mandal S, Kent BD. Obstructive sleep apnoea and coronary artery disease. J Thorac Dis. (2018) 10:S4212–20. doi: 10.21037/jtd.2018.12.75
6. Ryan S. Mechanisms of cardiovascular disease in obstructive sleep apnoea. J Thorac Dis. (2018) 10:S4201–11. doi: 10.21037/jtd.2018.08.56
7. Uchôa CHG, Danzi-Soares NJ, Nunes FS, de Souza AAL, Nerbass FB, Pedrosa RP, et al. Impact of OSA on cardiovascular events after coronary artery bypass surgery. Chest. (2015) 147:1352–60. doi: 10.1378/chest.14-2152
8. Tafelmeier M, Weizenegger T, Ripfel S, Fauser M, Floerchinger B, Camboni D, et al. Postoperative complications after elective coronary artery bypass grafting surgery in patients with sleep-disordered breathing. Clin Res Cardiol. (2018) 107:1148–59. doi: 10.1007/s00392-018-1289-0
9. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction 2018. J Am Coll Cardiol. (2018) 72:2231–64. doi: 10.1016/j.jacc.2018.08.1038
10. Gantner D, Ge JY, Li LH, Antic N, Windler S, Wong K, et al. Diagnostic accuracy of a questionnaire and simple home monitoring device in detecting obstructive sleep apnoea in a Chinese population at high cardiovascular risk. Respirology. (2010) 15:952–60. doi: 10.1111/j.1440-1843.2010.01797.x
11. Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable monitoring task force of the American Academy of sleep medicine. J Clin Sleep Med. (2007) 3:737–47. doi: 10.5664/jcsm.27032
12. Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. (2019) 40:87–165. doi: 10.1093/eurheartj/ehy855
13. Hillis LD, Smith PK, Anderson JL, Bittl JA, Bridges CR, Byrne JG, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. (2011) 124:e652–735. doi: 10.1161/CIR.0b013e31823b5fee
14. Hara H, Serruys PW, Takahashi K, Kawashima H, Ono M, Gao C, et al. Impact of peri-procedural myocardial infarction on outcomes after revascularization. J Am Coll Cardiol. (2020) 76:1622–39. doi: 10.1016/j.jacc.2020.08.009
15. Jaffe AS, Lindahl B, Giannitsis E, Mueller C, Cullen L, Hammarsten O, et al. ESC study group on cardiac biomarkers of the Association for acute cardiovascular care: a fond farewell at the retirement of CKMB. Eur Heart J. (2021) 42:2260–64. doi: 10.1093/eurheartj/ehaa1079
16. Ben-Yehuda O, Chen S, Redfors B, McAndrew T, Crowley A, Kosmidou I, et al. Impact of large periprocedural myocardial infarction on mortality after percutaneous coronary intervention and coronary artery bypass grafting for left main disease: an analysis from the EXCEL trial. Eur Heart J. (2019) 40:1930–41. doi: 10.1093/eurheartj/ehz113
17. Yau JM, Alexander JH, Hafley G, Mahaffey KW, Mack MJ, Kouchoukos N, et al. Impact of perioperative myocardial infarction on angiographic and clinical outcomes following coronary artery bypass grafting (from PRoject of Ex-vivo Vein graft ENgineering via Transfection [PREVENT] IV). Am J Cardiol. (2008) 102:546–51. doi: 10.1016/j.amjcard.2008.04.069
18. Kieser TM, Taggart DP. The use of intraoperative graft assessment in guiding graft revision. Ann Cardiothorac Surg. (2018) 7:652–62. doi: 10.21037/acs.2018.07.06
19. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. (2012) 33:1635–701. doi: 10.1093/eurheartj/ehs092
20. Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation. (2008) 118:1080–111. doi: 10.1161/CIRCULATIONAHA.107.189420
21. Tan A, Hau W, Ho HH, Ghaem Maralani H, Loo G, Khoo SM, et al. OSA and coronary plaque characteristics. Chest. (2014) 145:322–30. doi: 10.1378/chest.13-1163
22. Farooq V, Girasis C, Magro M, Onuma Y, Morel MA, Heo JH, et al. The CABG SYNTAX score - an angiographic tool to grade the complexity of coronary disease following coronary artery bypass graft surgery: from the SYNTAX Left Main Angiographic (SYNTAX-LE MANS) substudy. EuroIntervention. (2013) 8:1277–85. doi: 10.4244/EIJV8I11A196
23. Ishiwata S, Tomita Y, Ishiwata S, Narui K, Daida H, Kasai T. Association between obstructive sleep apnea and SYNTAX score. J Clin Med. (2020) 9:3314. doi: 10.3390/jcm9103314
24. Ryan S, Taylor CT, McNicholas WT. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation. (2005) 112:2660–7. doi: 10.1161/CIRCULATIONAHA.105.556746
25. Pasceri V, Cheng JS, Willerson JT, Yeh ET. Modulation of C-reactive protein-mediated monocyte chemoattractant protein-1 induction in human endothelial cells by anti-atherosclerosis drugs. Circulation. (2001) 103:2531–4. doi: 10.1161/01.CIR.103.21.2531
26. Rångemark C, Hedner JA, Carlson JT, Gleerup G, Winther K. Platelet function and fibrinolytic activity in hypertensive and normotensive sleep apnea patients. Sleep. (1995) 18:188–94. doi: 10.1093/sleep/18.3.188
27. Bokinsky G, Miller M, Ault K, Husband P, Mitchell J. Spontaneous platelet activation and aggregation during obstructive sleep apnea and its response to therapy with nasal continuous positive airway pressure. A preliminary investigation. Chest. (1995) 108:625–30. doi: 10.1378/chest.108.3.625
28. Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, et al. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation. (2003) 107:1129–34. doi: 10.1161/01.CIR.0000052627.99976.18
29. Phillips CL, McEwen BJ, Morel-Kopp MC, Yee BJ, Sullivan DR, Ward CM, et al. Effects of continuous positive airway pressure on coagulability in obstructive sleep apnoea: a randomised, placebo-controlled crossover study. Thorax. (2012) 67:639–44. doi: 10.1136/thoraxjnl-2011-200874
30. Drager LF, Bortolotto LA, Figueiredo AC, Krieger EM, Lorenzi GF. Effects of continuous positive airway pressure on early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med. (2007) 176:706–12. doi: 10.1164/rccm.200703-500OC
31. Wu X, Lv S, Yu X, Yao L, Mokhlesi B, Wei Y. Treatment of OSA reduces the risk of repeat revascularization after percutaneous coronary intervention. Chest. (2015) 147:708–18. doi: 10.1378/chest.14-1634
Keywords: obstructive sleep apnea, perioperative myocardial infarction, off-pump coronary artery bypass grafting, syntax score, high-sensitivity c-reactive protein
Citation: Fan K, Gao M, Yu W, Liu H, Chen L, Ding X and Yu Y (2021) Obstructive Sleep Apnea Increases the Risk of Perioperative Myocardial Infarction Following Off-Pump Coronary Artery Bypass Grafting. Front. Cardiovasc. Med. 8:689795. doi: 10.3389/fcvm.2021.689795
Received: 11 April 2021; Accepted: 09 June 2021;
Published: 08 July 2021.
Edited by:
Takatoshi Kasai, Juntendo University, JapanCopyright © 2021 Fan, Gao, Yu, Liu, Chen, Ding and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Yu, aGVhcnR5dXlhbmdAaG90bWFpbC5jb20=
†These authors have contributed equally to this work
 Kangjun Fan†
Kangjun Fan† Mingxin Gao
Mingxin Gao Liang Chen
Liang Chen Yang Yu
Yang Yu