
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Cardiovasc. Med. , 11 March 2021
Sec. General Cardiovascular Medicine
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.648725
This article is part of the Research Topic Clinical Cases in Cardiovascular Medicine: 2021 View all 10 articles
Background: Pheochromocytoma patients who present with shock are extremely rare. Here, we report a patient who presented with shock and was diagnosed with pheochromocytoma.
Case Summary: A 59-year-old woman with a history of hypertension without any treatment for 5 years presented with chest tightness. Vital signs on arrival indicated blood pressure of 78/50 mmHg. Twelve-lead electrocardiogram indicated ST-segment depression in leads II, III, aVF, and V3–V6 and QT prolongation. Coronary angiogram revealed no evidence of coronary artery disease. Contrast-enhanced computed tomography demonstrated an inhomogeneous right adrenal mass (2.5 × 3.0 cm). Her 24-h urinary norepinephrine and catecholamine levels were elevated. The patient underwent laparoscopic right adrenalectomy. Histopathology confirmed adrenal pheochromocytoma with residual necrosis. The patient was diagnosed with pheochromocytoma. During the 2-year follow-up, the patient was asymptomatic, and her blood pressure remained normal without medication. ECG showed that the ST-segment depression in leads II, III, aVF, and V3–V6 and the QT prolongation had disappeared. The patient showed no signs of recurrence, with normal urine norepinephrine and catecholamine levels.
Conclusion: Patients with pheochromocytoma can present with hypotension or even shock. Clinicians should suspect pheochromocytoma when a patient with a history of hypertension has sudden hypotension or even shock.
Pheochromocytoma is a rare neuroendocrine tumor that originates from the adrenal medulla or extra-adrenal paraganglion chromaffin tissue and secretes catecholamines (1). The clinical manifestations of patients with pheochromocytoma are diverse, ranging from asymptomatic to cardiac arrest. The typical triad, including episodic headache, palpitations and sweating, only occurs in 24% of pheochromocytoma patients (2, 3). This often misleads clinicians to make a wrong diagnosis. Hypertension is one of the most common manifestations of pheochromocytoma and can be persistent or paroxysmal.
Shock is defined as insufficient perfusion of organs and peripheral tissues, and is classified as hypovolemic, cardiogenic, or restrictive (vasodilatation/distribution) according to its etiology. However, pheochromocytoma patients who present with shock are extremely rare. The pathophysiological factors of hypotension or shock include tumor necrosis leading to a sudden decrease in continuous catecholamine secretion, adrenergic receptor desensitization, and decreased vascular volume. Here, we report a case of a patient with pheochromocytoma characterized by shock.
A 59-year-old woman presented with chest tightness for 2 h. 2 h before admission, the patient experienced chest tightness accompanied by palpitations, dizziness, vomiting and sweating.
The patient had a history of hypertension for 5 years without any treatment or etiological diagnosis. The patient denied a family history of premature coronary artery disease and special personal history, such as smoking and drinking.
Vital signs on arrival indicated blood pressure 78/50 mmHg, heart rate 102 beats per min and a respiratory rate of 26 beats per minute. The patient was conscious, but her lips were cyanotic. Her face was pale, and her extremities were wet and cold. There was no obvious abnormality in the heart or lung examination. Jugular vein engorgement and peripheral edema were not found.
The troponin I level was 1.16 ng/mL (reference interval <0.04). Hemoglobin, leukocytes, electrolytes, B-type natriuretic peptide, liver function, renal function, and D-dimer were not significantly abnormal. Twelve-lead electrocardiogram (ECG) indicated a sinus rhythm with ST-segment depression in leads II, III, aVF, and V3–V6 and QT prolongation (QTc 529 ms) (Figure 1). Coronary angiogram revealed no evidence of coronary artery disease (Figure 2). Echocardiography showed a thickened ventricular septum (12 mm) and normal left ventricular function without abnormal wall motion (left ventricular ejection fraction of 55%). Chest computed tomography showed no obvious abnormality, but abdominal computed tomography showed an adrenal mass. Contrast-enhanced computed tomography demonstrated an inhomogeneous right adrenal mass (2.5 × 3.0 cm, Figure 3). The urinary norepinephrine level was 288.8 nmol/24 h (reference interval 80.3–164.0), and the urinary catecholamine level was 307.4 nmol/24 h (reference interval 94.5–238.3). 24 h urinary epinephrine level was normal.
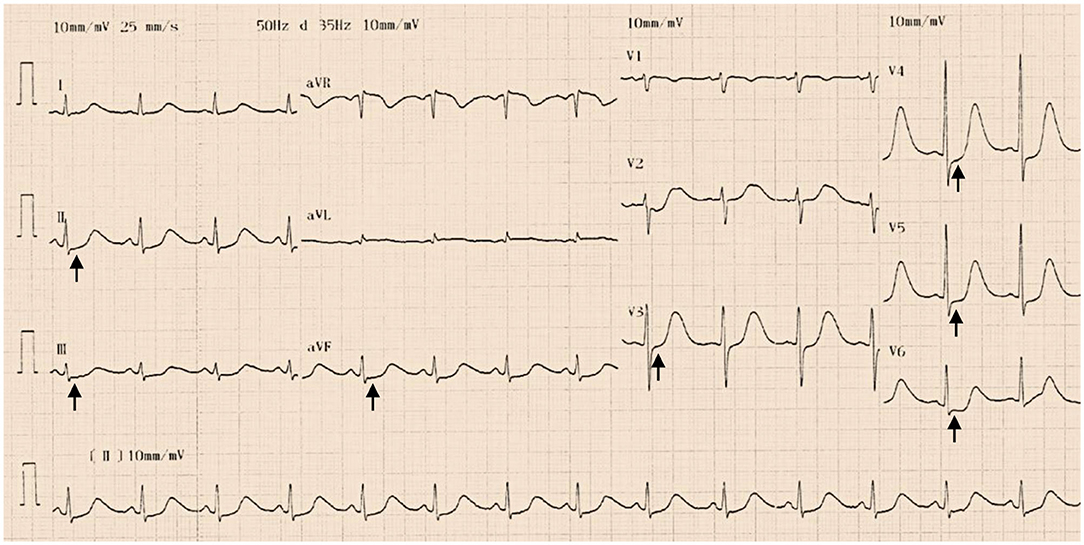
Figure 1. Twelve-lead electrocardiogram indicated a sinus rhythm with ST-segment depression in leads II, III, aVF, and V3–V6 (black arrows) and QT prolongation (QTc 529 ms) at admission.
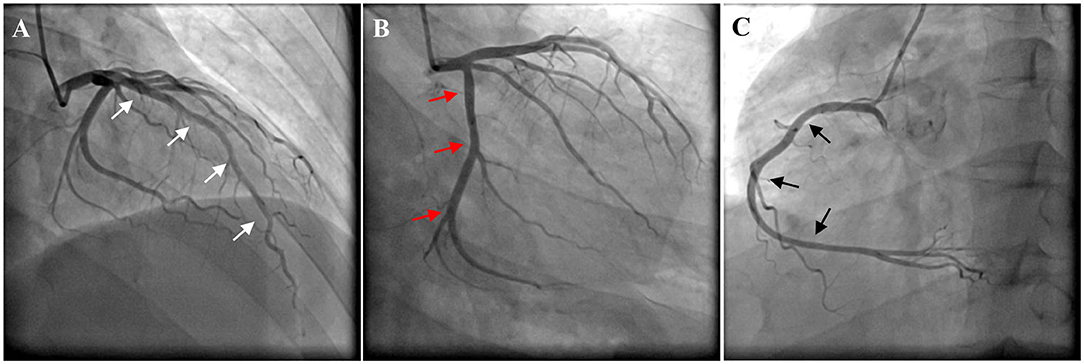
Figure 2. Coronary angiogram revealed no evidence of coronary artery disease. (A) Left anterior descending artery (white arrows). (B) Left circumflex artery (red arrows). (C) Right coronary artery (black arrows).
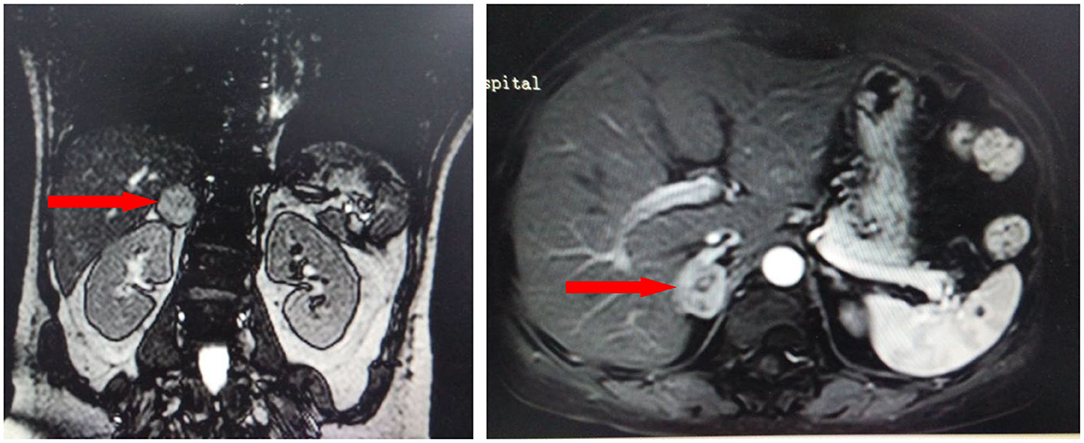
Figure 3. Contrast-enhanced computed tomography demonstrated an inhomogeneous right adrenal mass (2.5 × 3.0 cm, red arrows).
Saline solution and dopamine injection were administered to maintain blood pressure. The patient's condition gradually improved, and her blood pressure gradually stabilized. 7 days later, the patient was transferred to the urology department and successfully underwent laparoscopic right adrenalectomy. Histopathology confirmed adrenal pheochromocytoma with residual necrosis. Immunohistochemistry confirmed that chromogranin A, neuron-specific enolase and synaptophysin were positive. The patient was diagnosed with pheochromocytoma.
The patient was free of complications during hospitalization. During the 2-year follow-up, the patient was asymptomatic, and her blood pressure remained normal without medication. ECG showed that the ST-segment depression in leads II, III, aVF, and V3–V6 and the QT prolongation had disappeared (Figure 4). The patient showed no signs of recurrence, with normal urine norepinephrine and catecholamine levels (Table 1).
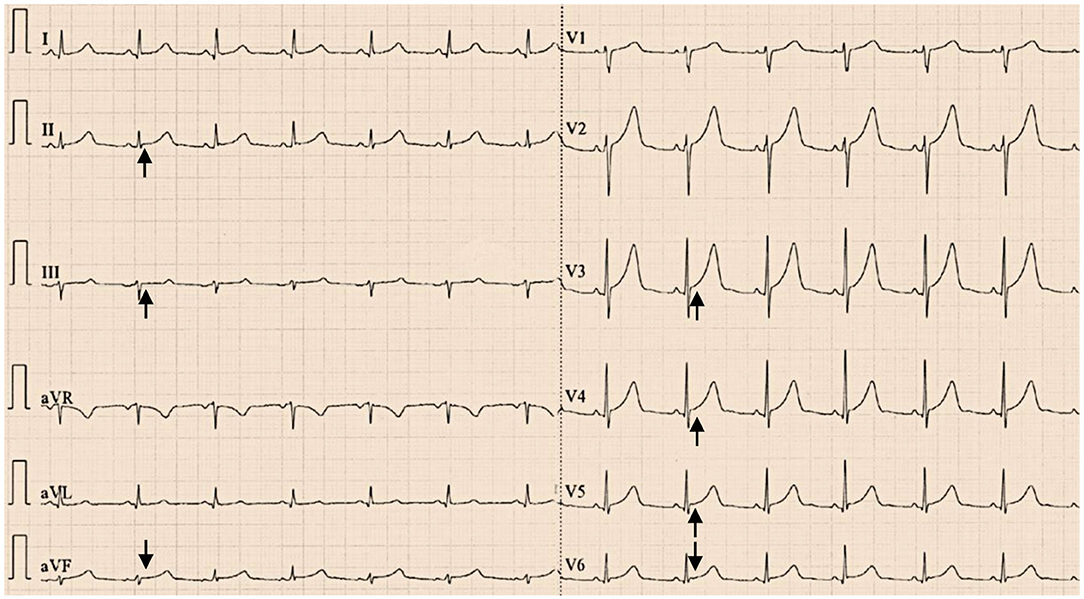
Figure 4. Twelve-lead electrocardiograms showed that the ST-segment depression in leads II, III, aVF, and V3–V6 had disappeared (black arrows) with normal QT interval (QTc 424 ms) at the 2-year follow-up after resection of the pheochromocytoma.
Pheochromocytoma can produce excessive amounts of catecholamines, especially epinephrine and norepinephrine, and release them continuously or intermittently (4, 5). Pheochromocytoma has various clinical manifestations. The typical triad of pheochromocytoma, including episodical headache, palpitations and sweating, lasts from a few minutes to a few hours as a direct consequence of excessive catecholamine secretion and is often accompanied by hypertension (6). Approximately 90% of patients with pheochromocytoma present with sustained or paroxysmal hypertension (7, 8). Hypertension in pheochromocytoma usually manifests as high peripheral resistance and low heart index. Norepinephrine secreted by pheochromocytoma increases peripheral vascular resistance, leading to increased systolic and diastolic blood pressure (9). Epinephrine-secreting pheochromocytoma usually causes patients to experience paroxysmal symptoms, such as headaches, palpitations, sweating and anxiety, while patients with norepinephrine-secreting tumors usually have persistent symptoms (such as persistent hypertension) related to the continuous catecholamine overdose (10). In our case, the patient's norepinephrine level was elevated, but the epinephrine level was normal. The patient did not present with the typical triad of pheochromocytoma, which may be because the tumor secreted norepinephrine rather than epinephrine. The patient had a history of hypertension for 5 years, and persistent hypertension is related to the continuous catecholamine overdose produced by norepinephrine-secreting tumors.
Occasionally, patients with pheochromocytoma experience hypotension or even shock. The pathophysiological factors of hypotension and shock include tumor necrosis leading to a sudden decrease in continuous catecholamine secretion, adrenergic receptor desensitization, and decreased vascular volume (11). Some cardiovascular events, such as myocardial infarction and arrhythmia, can also cause shock (12). In our case, the pheochromocytoma concomitant with circulatory shock may have been related to the sudden decrease in catecholamine secretion caused by tumor necrosis, and histopathology confirmed an adrenal pheochromocytoma with residual necrosis.
Pheochromocytoma can also cause other cardiovascular complications, including cardiac hypertrophy, heart failure, arrhythmias, ischemic heart disease and even acute myocardial infarction, which are due to the effects of secreted catecholamines (3, 13). Norepinephrine secreted by pheochromocytoma can cause structural and functional remodeling of the heart, such as left ventricular hypertrophy. Catecholamines, especially norepinephrine, can cause myocardial damage by increasing the oxygen consumption and apoptosis of cardiomyocytes and can further lead to left ventricular systolic dysfunction and dilated cardiomyopathy (14, 15). Some factors can lead to an imbalance of the oxygen supply and demand, such as cardiotoxicity of catecholamines, increased muscle mass and coronary artery spasm, causing myocardial ischemic necrosis (16, 17). Patients may have chest pain and tightness, and ECG may manifest as ST-segment elevation or depression. Myocardial enzymes may be elevated (18, 19). In some cases, pheochromocytoma is associated with Takotsubo cardiomyopathy, characterized by reversible left ventricular apical ballooning (20–22). The level of B-type natriuretic peptide is generally significantly elevated in these patients (23). In our case, the typical wall motion abnormalities of Takotsubo cardiomyopathy were not reflected in echocardiography, and the B-type natriuretic peptide level was normal. Therefore, the suspicion of Takotsubo cardiomyopathy caused by pheochromocytoma was not confirmed. The ECG of patients with pheochromocytoma may also show a variety of abnormalities in the heart rhythm, conduction, and repolarization, including a significantly prolonged QT interval and deep and wide, symmetrical, inverted T waves. A prolonged QT interval may induce the risk of torsade de pointes ventricular tachycardia (24). In our case, preoperative ECG showed ST-segment depression in leads II, III, aVF and V3–V6 and QT prolongation, and follow-up ECG showed that these changes had disappeared after laparoscopic adrenalectomy.
The patient did not undergo echocardiography again to determine whether the ventricular septum returned to normal thickness during the 2-year follow-up.
Occasionally, patients with pheochromocytoma can present with hypotension or even shock. Pheochromocytoma should be suspected when a patient with a history of hypertension has sudden hypotension or even shock.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
All authors contributed in this patient care, diagnosis and treatment, and in writing this article, contributed to the article, and approved the submitted version.
This study was funded by Natural Science Basic Research Program of Shaanxi Province: No. 2020JQ-939; Science and Technology Development Incubation Fund Project of Shaanxi Provincial People's Hospital: No. 2019YXQ-08.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to acknowledge all who contributed in this case diagnosis, therapy, and decision-making.
1. Farrugia FA, Martikos G, Tzanetis P, Charalampopoulos A, Misiakos E, Zavras N, et al. Pheochromocytoma, diagnosis and treatment: review of the literature. Endocr Regul. (2017) 51:168–81. doi: 10.1515/enr-2017-0018
2. Rupala K, Mittal V, Gupta R, Yadav R. Atypical presentation of pheochromocytoma: central nervous system pseudovasculitis. Indian J Urol. (2017) 33:82–4. doi: 10.4103/0970-1591.195760
3. Gu YW, Poste J, Kunal M, Schwarcz M, Weiss I. Cardiovascular manifestations of pheochromocytoma. Cardiol Rev. (2017) 25:215–22. doi: 10.1097/CRD.0000000000000141
4. Berends AMA, Eisenhofer G, Fishbein L, Horst-Schrivers ANAVD, Kema IP, Links TP, et al. Intricacies of the molecular machinery of catecholamine biosynthesis and secretion by chromaffin cells of the normal adrenal medulla and in pheochromocytoma and paraganglioma. Cancers (Basel). (2019) 11:1121. doi: 10.3390/cancers11081121
5. Farrugia FA, Charalampopoulos A. Pheochromocytoma. Endocr Regul. (2019) 53:191–212. doi: 10.2478/enr-2019-0020
6. Garg SK, Garg P, Urumdas M. An interesting presentation of pheochromocytoma. Indian J Crit Care Med. (2018) 22:40–2. doi: 10.4103/ijccm.IJCCM_407_17
7. Mañas-Martínez AB, Medrano-Navarro AL, Aguillo-Gutiérrez E. Hemorrhagic pheochromocytoma presenting as severe hypertension with myocardial infarction. Ann Endocrinol (Paris). (2017) 78:54–6. doi: 10.1016/j.ando.2016.10.004
8. Manger WM. The protean manifestations of pheochromocytoma. Horm Metab Res. (2009) 41:658–63. doi: 10.1055/s-0028-1128139
9. Prejbisz A, Lenders JW, Eisenhofer G, Januszewicz A. Cardiovascular manifestations of phaeochromocytoma. J Hypertens. (2011) 29:2049–60. doi: 10.1097/HJH.0b013e32834a4ce9
10. Reisch N, Peczkowska M, Januszewicz A, Neumann HP. Pheochromocytoma: presentation, diagnosis and treatment. J Hypertens. (2006) 24:2331–9. doi: 10.1097/01.hjh.0000251887.01885.54
11. Galetta F, Franzoni F, Bernini G, Poupak F, Carpi A, Cini G, et al. Cardiovascular complications in patients with pheochromocytoma: a mini-review. Biomed Pharmacother. (2010) 64:505–9. doi: 10.1016/j.biopha.2009.09.014
12. Zhang Q, Zhao R. Risk factors analysis of prognosis of adult acute severe myocarditis. World J Clin Cases. (2020) 8:5547–54. doi: 10.12998/wjcc.v8.i22.5547
13. Nazari MA, Rosenblum JS, Haigney MC, Rosing DR, Pacak K. Pathophysiology and acute management of tachyarrhythmias in pheochromocytoma: JACC review topic of the week. J Am Coll Cardiol. (2020) 76:451–64. doi: 10.1016/j.jacc.2020.04.080
14. Gupta MK, Neelakantan TV, Sanghamitra M, Tyagi RK, Dinda A, Maulik S, et al. An assessment of the role of reactive oxygen species and redox signaling in norepinephrine-induced apoptosis and hypertrophy of H9c2 cardiac myoblasts. Antioxid Redox Signal. (2006) 8:1081–93. doi: 10.1089/ars.2006.8.1081
15. Y-Hassan S, Falhammar H. Cardiovascular manifestations and complications of pheochromocytomas and paragangliomas. J Clin Med. (2020) 9:2435. doi: 10.3390/jcm9082435
16. Naranjo J, Dodd S, Martin YN. Perioperative management of pheochromocytoma. J Cardiothorac Vasc Anesth. (2017) 31:1427–39. doi: 10.1053/j.jvca.2017.02.023
17. Ramachandran R, Rewari V. Current perioperative management of pheochromocytomas. Indian J Urol. (2017) 33:19–25. doi: 10.4103/0970-1591.194781
18. Vilcant V. Pheochromocytoma-induced cardiomyopathy mimicking acute coronary syndrome. J Am Osteopath Assoc. (2017) 117:537–40. doi: 10.7556/jaoa.2017.104
19. Khattak S, Sim I, Dancy L, Whitelaw B, Sado D. Phaeochromocytoma found on cardiovascular magnetic resonance in a patient presenting with acute myocarditis: an unusual association. BMJ Case Rep. (2018) 2018:bcr2017222621. doi: 10.1136/bcr-2017-222621
20. Afana M, Panchal RJ, Simon RM, Hejab A, Lahiri SW, Khandelwal AK, et al. Pheochromocytoma-induced Takotsubo cardiomyopathy. Tex Heart Inst J. (2019) 46:124–7. doi: 10.14503/THIJ-17-6407
21. Zhang R, Gupta D, Albert SG. Pheochromocytoma as a reversible cause of cardiomyopathy: analysis and review of the literature. Int J Cardiol. (2017) 249:319–23. doi: 10.1016/j.ijcard.2017.07.014
22. Su Z, Wang Y, Fei H. Takotsubo-like cardiomyopathy in pheochromocytoma. CASE (Phila). (2019) 3:157–61. doi: 10.1016/j.case.2019.04.006
23. Ahmed KA, Madhavan M, Prasad A. Brain natriuretic peptide in apical ballooning syndrome (Takotsubo/stress cardiomyopathy): comparison with acute myocardial infarction. Coron Artery Dis. (2012) 23:259–64. doi: 10.1097/MCA.0b013e3283526a57
Keywords: pheochromocytoma, hypotension, shock, electrocardiogram, cardiovascular complication
Citation: Wu H-Y, Gao T-J, Cao Y-W and Liang L (2021) Case Report: Pheochromocytoma in a 59-Year-Old Woman Presenting With Hypotension. Front. Cardiovasc. Med. 8:648725. doi: 10.3389/fcvm.2021.648725
Received: 01 January 2021; Accepted: 22 February 2021;
Published: 11 March 2021.
Edited by:
Leonardo Roever, Federal University of Uberlandia, BrazilReviewed by:
Owais Bhat, Virginia Commonwealth University, United StatesCopyright © 2021 Wu, Gao, Cao and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi-Wei Cao, Y3l3MDgxMEAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.