- 1The Second Medical Center & National Clinical Research Center for Geriatric Diseases, Chinese PLA General Hospital, Beijing, China
- 2Department of Cardiology, Cangzhou Central Hospital, Hebei Medical University, Cangzhou, China
- 3Department of Computer Science, Tsinghua University, Beijing, China
- 4Artificial Intelligence Lab, Global Health Drug Discovery Institute, Beijing, China
Background: The residual SYNTAX score (RSS) is considered a powerful prognostic indicator for determining a reasonable revascularization strategy in patients undergoing percutaneous coronary intervention (PCI), but the absence of clinical parameters is one of the limitations of RSS, especially in the chronic renal insufficiency (CRI) comorbidity setting. The present work aimed to investigate the incremental prognostic value of clinical residual SYNTAX score (CRSS) compared with RSS in CRI cases after PCI.
Methods: Totally 2,468 consecutive CRI cases who underwent PCI from January 2014 to September 2017 were included in this retrospective analysis. CRSS was obtained by multiplying RSS by the modified ACEF score. Individuals with CRSS >0 were considered to have incomplete revascularization and stratified by CRSS tertiles, the remaining cases constituted the complete revascularization (CR) group. The outcomes between these groups were compared.
Results: At a median follow-up of 3 years, compared with CR group, individuals with CRSS >12 showed elevated rates of all clinical outcomes, and those with CRSS ≤ 12 showed similar all-cause and cardiac mortality rates. In multivariable analysis, CRSS was a powerful independent predictive factor of all clinical outcomes. The net reclassification improvement levels of CRSS over RSS for all-cause and cardiac mortality rates were 10.3% (p = 0.007) and 16.4% (p < 0.001), respectively. Compared with RSS, CRSS markedly ameliorated all-cause and cardiac mortality risk stratification.
Conclusions: Compared with RSS, CRSS has incremental predictability for long-term all-cause and cardiac mortality in CRI cases following PCI.
Introduction
The residual SYNTAX score (RSS) is considered an independent predictive factor of adverse outcomes among individuals undergoing percutaneous coronary intervention (PCI), and might aid in assessing a rational degree of revascularization (1–7). Our recent study demonstrated that RSS has stronger predictability than baseline SYNTAX score (SS) for unplanned revascularization (UR) and stroke, as well as major adverse cardiovascular and cerebrovascular events (MACCEs) in chronic renal insufficiency (CRI) cases undergoing PCI at the 3-year follow-up (8). However, the absence of clinical parameters in RSS represents one of the limitations in its ability to precisely risk stratify individuals with complex coronary artery disease (CAD). Previous studies have shown the prognostic value of clinical residual SYNTAX score (CRSS), which is derived as a product of RSS and modified ACEF (ACEFCRCL) score (3, 9). However, no previous studies have assessed the predictive potential of CRSS in CRI cases. CRI is a traditional risk factor for cardiovascular morbidity and mortality. It is associated with poor procedural success rate, increased complications and worse clinical outcomes, such as restenosis and stent thrombosis, after PCI (10, 11). Therefore, the goal of the current work was to determine the prognostic ability of CRSS comparatively to RSS in CRI cases.
Methods
Study Population
A total of 14,174 consecutive patients were administered PCI between January 2014 and September 2017 in Cangzhou Central Hospital, Hebei Medical University. Among them, 2529 cases with an estimated glomerular filtration rate (EGFR) <90 mL/min per 1.73 m2 were consecutively enrolled. The simplified Modification of Diet in Renal Disease (MDRD) formula was used for EGFR assessment (12). Considering the SS can be used only in individuals with native CAD, nine patients with prior coronary artery bypass grafting (CABG), 28 with staged PCI and 24 with unplanned PCI for the second hospitalization were excluded. Finally, 2,468 individuals were assessed in this retrospective study (Figure 1). Ethical approval was obtained from the ethics committee of Cangzhou Central Hospital, Hebei Medical University. Each patient was asked to provide signed informed consent.
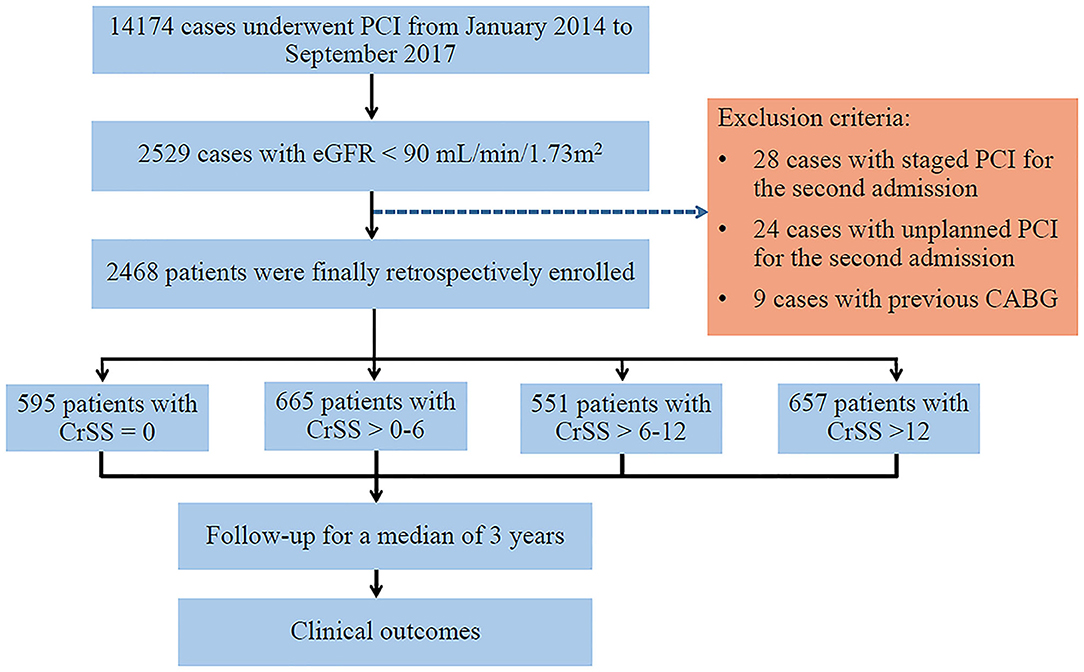
Figure 1. Study Flow Chart. CABG, coronary artery bypass graft; CrSS, clinical residual SYNTAX score; eGFR, estimated glomerular filtration rate; PCI, percutaneous coronary intervention.
Clinical Residual SYNTAX Score
CRSS was derived as follows: CRSS = (RSS) × (ACEFCRCL score) (13). Baseline SS was calculated by visualization by two of three experienced interventionists who were well-trained in SS evaluation and blinded to patient grouping and outcomes. In case of disagreement, the third cardiologist provided an opinion, and a consensual decision was made after discussion (14). Subsequently, RSS was determined according to the remaining obstructive coronary disease treated by PCI (1). The ACEFCRCL score was obtained as age/ejection fraction +1 point for every 10 mL/min decrease in CRCL below 60 mL/min per 1.73 m2 (maximum of six points).
Study Endpoints
Complete revascularization (CR) was reflected by a post-PCI CRSS = 0. Individuals with incomplete revascularization (IR) were stratified according to CRSS tertiles. The primary endpoints included cardiac death (CD) and all-cause death (ACD). The secondary endpoints were myocardial infarction (MI), UR, stroke, and MACCEs (combining ACD, MI, stroke and UR). Revascularization was defined as UR for ischemic symptoms and events driven by CABG or PCI. The above endpoints were examined separately by 2 cardiologists, and any disagreement was solved by consensual discussion.
Statistical Analysis
Continuous data were presented as mean ± SD, and compared by one-way ANOVA. Categorical data were expressed as n (%), and compared by the chi-square or Fisher's exact test. The Kaplan-Meier method was utilized for assessing clinical outcomes, with the log-rank test for comparison. The patients were considered to be at risk up to the last follow-up. Multivariable analysis was conducted by a Cox regression model utilizing the enter method. In addition to CRSS, variables related to adverse events were incorporated in the model for analysis. The Supremum test was employed to verify the proportional hazards assumption for various endpoints. By combining the ACEFCRCL score with RSS, improvement in model performance, discrimination and risk classification was examined, by (a) comparatively evaluating the areas under the curves (AUCs) for the two nested models using the nonparametric method and (b) calculating net reclassification improvement (NRI) and integrated discrimination improvement (IDI) indices (15). Two-sided p < 0.05 was regarded as statistically significant. SPSS 24.0 (IBM Corp., Armonk, NY, USA) and R 3.6.0 were utilized for data analysis.
Results
Baseline Characteristics and Procedural Results
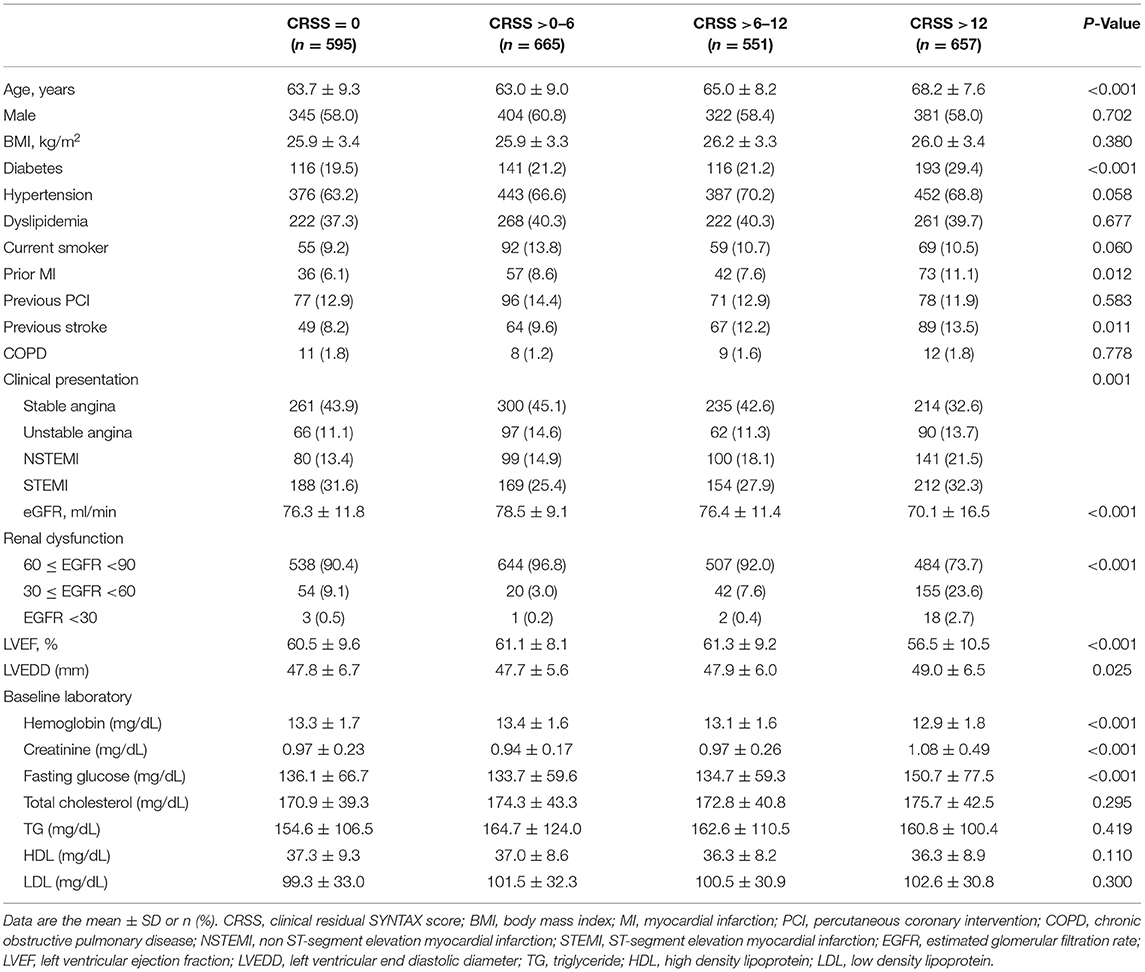
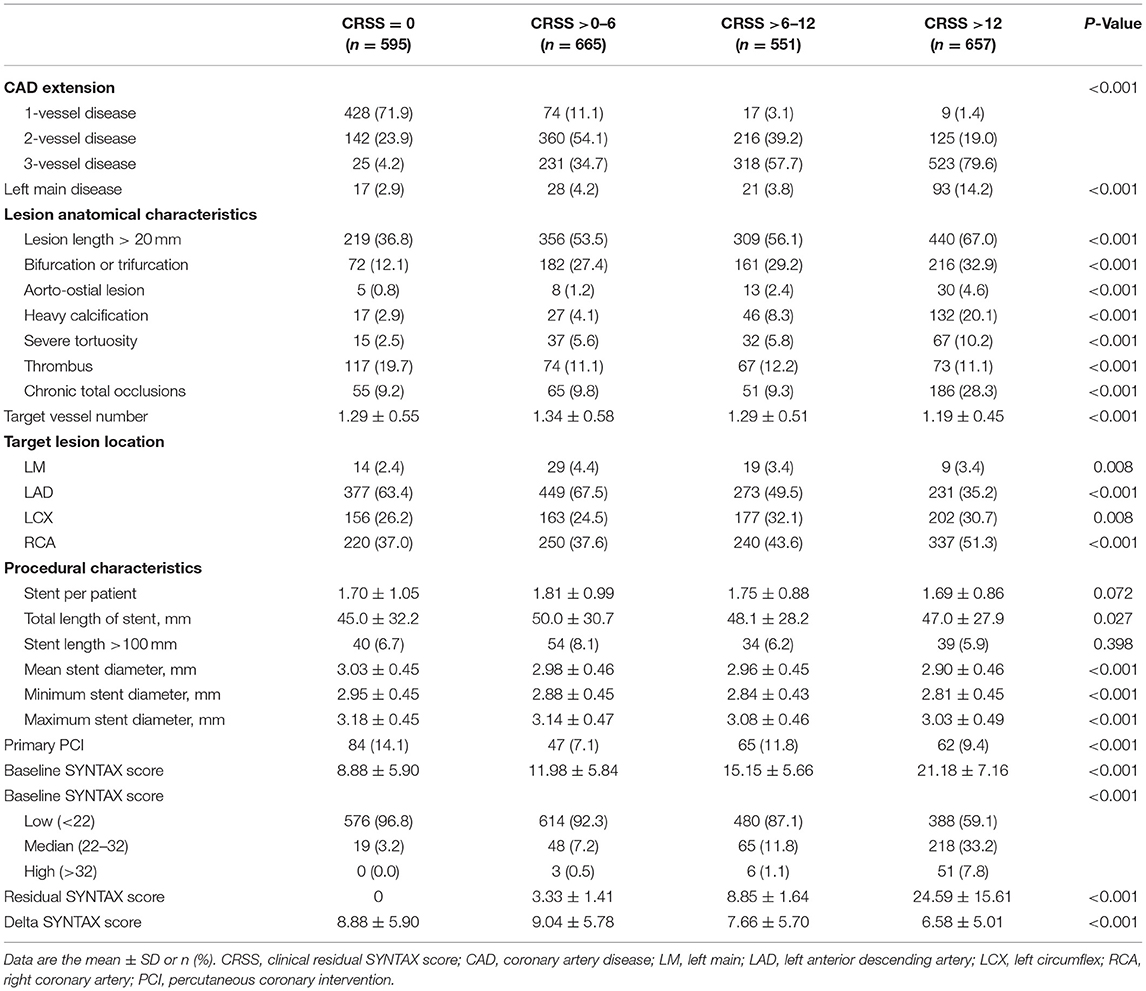
The values of RSS ranged from 0 to 44.5 (6.4 ± 6.6), and CRSS ranged from 0 to 130.2 (9.4 ± 12.6). CR was achieved in 595 patients (24.1%). The clinical and angiographic features of all cases after stratification by CRSS are summarized in Tables 1, 2. In comparison with individuals with CR, those with IR had increased rates of clinical comorbidities, including older age, diabetes, clinical presentation of MI, old MI, prior stroke, reduced EGFR, lower left ventricular ejection fraction, lower hemoglobin and higher fasting glucose (p < 0.05 or p < 0.001). Patients with IR had anatomically complex coronary disease, including higher baseline SS, three-vessel and left main disease, long lesions, bifurcations or trifurcations, aorto-ostial lesions, severe calcification and tortuosity, thrombus and chronic total occlusion lesions (all p < 0.001). Patients with IR had longer total length of implanted stents (p = 0.027) and increased target vessel number (p < 0.001).
Clinical Outcomes
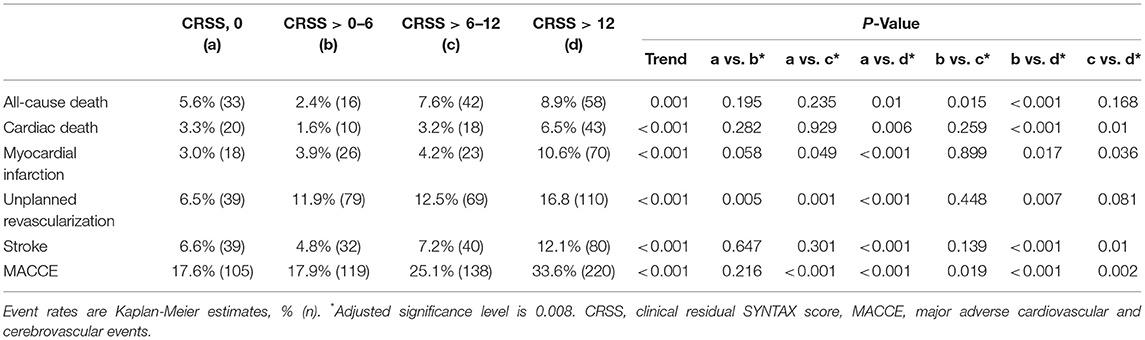
There were 2,425 patients (98.3%) who completed the median 3-year (1.5~5 years) follow-up. Clinical outcomes stratified based on CRSS are depicted in Table 3 and Figure 2. Patients with CRSS >12 had increased 5-year cumulative incidence rates of adverse events, including ACD (8.9%), CD (6.5%), MI (10.6%), UR (16.8%), stroke (12.1%) and MACCEs (33.6%) (all p ≤ 0.001). Subjects with CRSS ≤ 12 had ACD, CD, MI, and stroke rates comparable to those with CR. Multivariable Cox regression analysis demonstrated that CRSS independently predicted all clinical outcomes at a follow-up of 3 years (Figure 3).
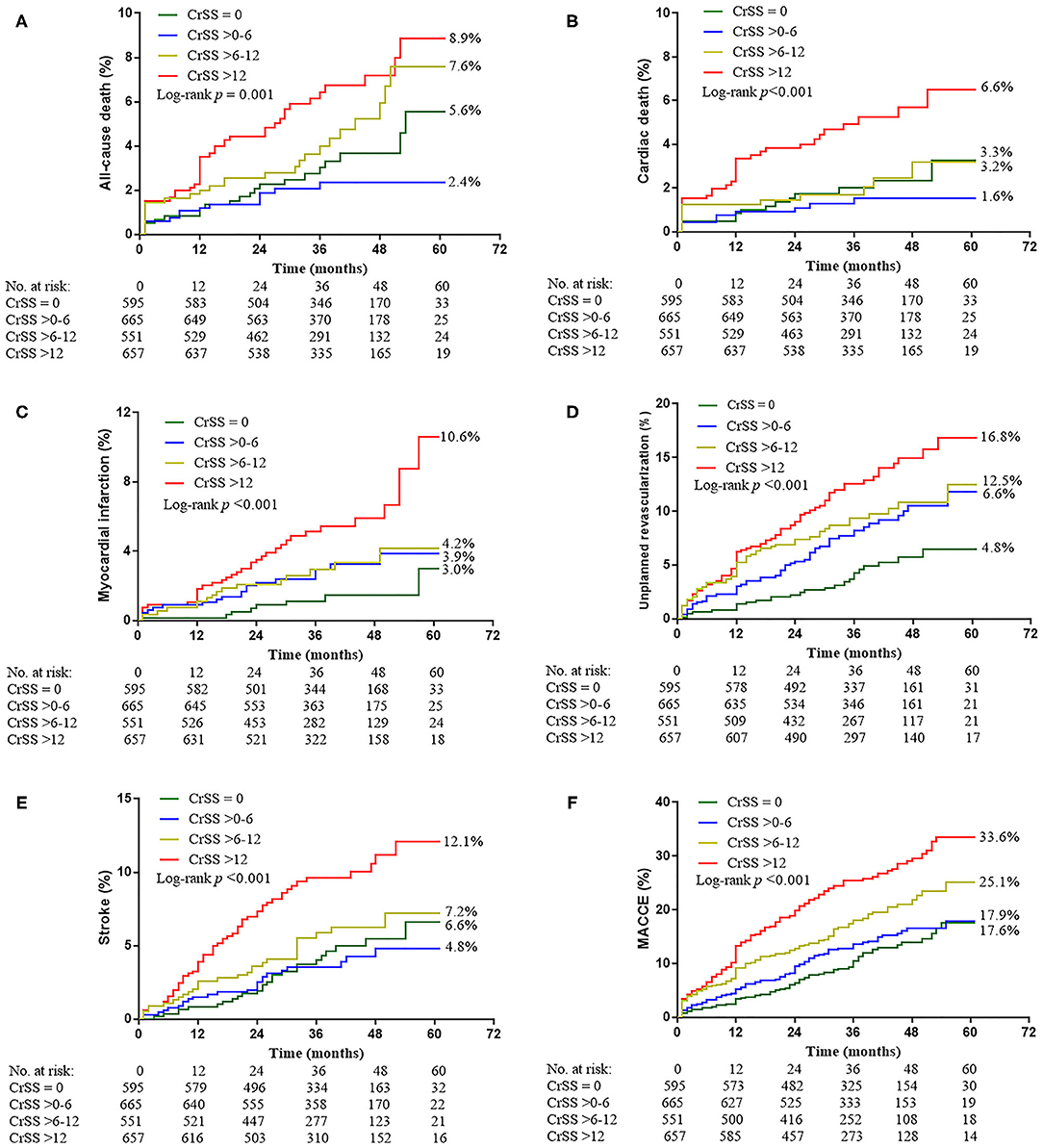
Figure 2. Kaplan-Meier Curves Showing Event Rates Stratified by the CRSS Through 5 Years. (A) All-cause death. (B) Cardiac death. (C) Myocardial infarction. (D) Unplanned revascularization. (E) Stroke. (F) Major adverse cardiovascular and cerebrovascular events (MACCE).
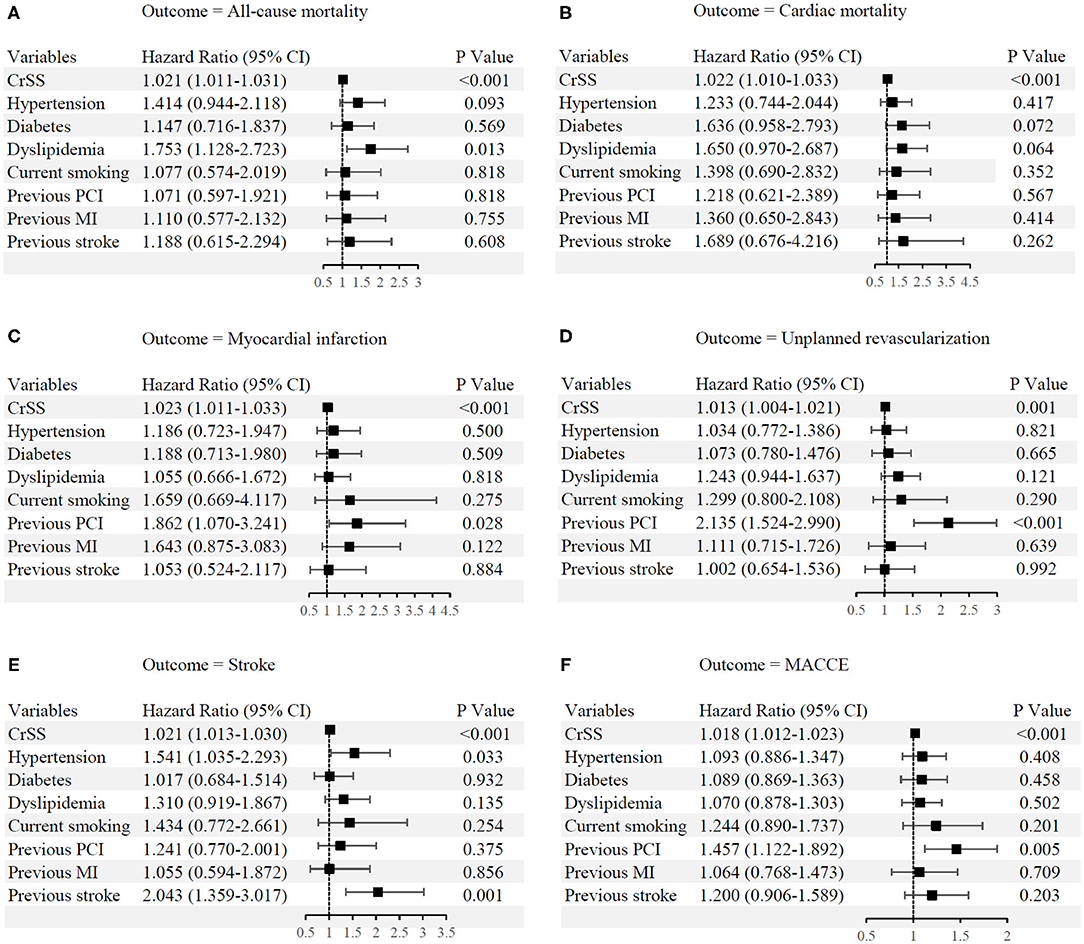
Figure 3. Independent predictors of long-term clinical outcomes. (A) All-cause mortality. (B) Cardiac mortality. (C) Myocardial infarction. (D) Unplanned revascularization. (E) Stroke. (F) Major adverse cardiovascular and cerebrovascular events. CI, confidence interval; CRSS, clinical residual SYNTAX score; MACCE, major adverse cardiovascular and cerebrovascular events; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Discriminative and Predictive Capability of CRSS and RSS
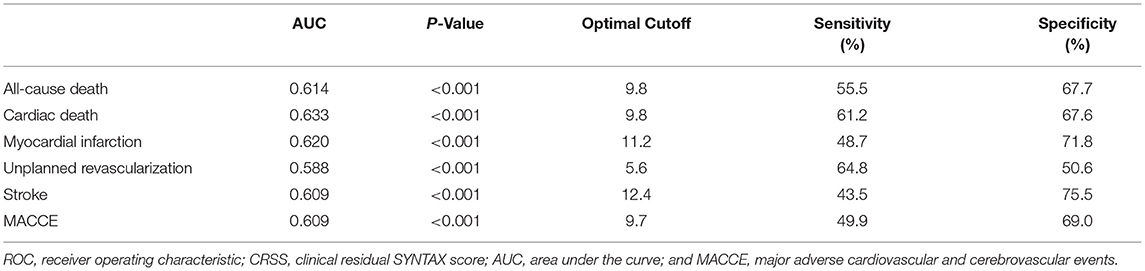
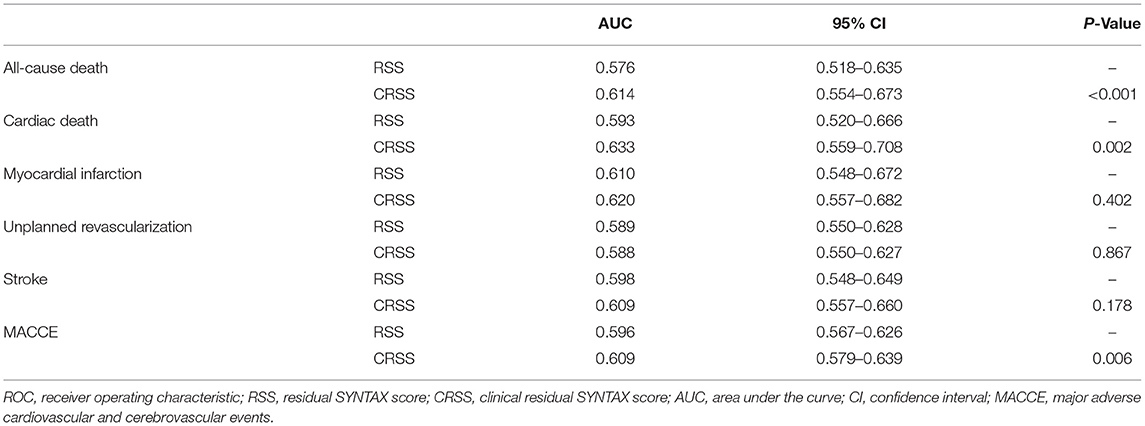
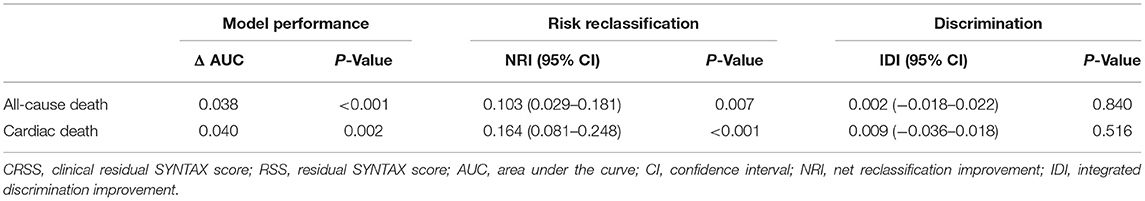
Receiver operating characteristic (ROC) curve analysis revealed CRSS was significantly associated with 3-year all-cause and cardiac mortality rates, MI, UR, stroke and MACCEs (all p < 0.001). A CRSS cutoff of 9.8 had a predictive value for all-cause and cardiac mortality (Table 4). CRSS demonstrated greater performance for all-cause and cardiac mortality as well as MACCEs in comparison with RSS (Table 5, Figure 4).
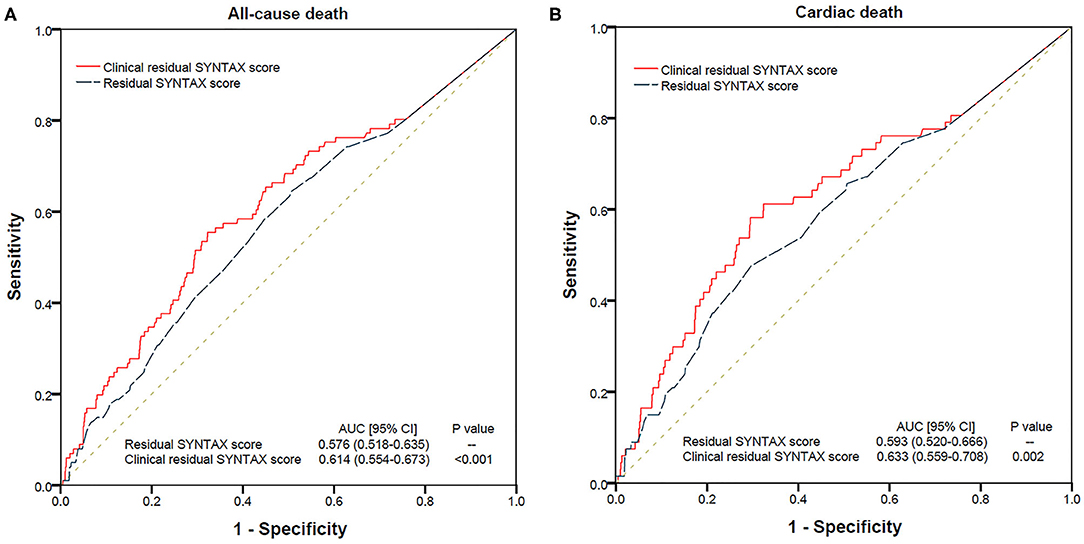
Figure 4. Comparison of ROC Curves between RSS and CRSS for Predicting Long-term All-cause (A) and Cardiac (B) mortality. AUC, area under the curve; CRSS, clinical residual SYNTAX score; ROC, receiver operating characteristic; RSS, residual SYNTAX score.
Furthermore, CRSS markedly ameliorated risk stratification for all-cause and cardiac mortality. The NRI of CRSS vs. RSS for all-cause and cardiac mortality were 10.3% (p = 0.007) and 16.4% (p < 0.001), respectively. However, the IDI indices of CRSS vs. RSS for all-cause (p = 0.840) and cardiac mortality (p = 0.516) were not statistically significant (Table 6).
Discussion
We comprehensively investigated the predictive value of CRSS for long-term patient outcomes in CRI cases after PCI. Our findings indicate that elevated CRSS is a representative marker of increased cardiac-kidney comorbidities and more anatomically complex disease. CRSS is a strong independent predictor of long-term adverse events such as all-cause and cardiac mortality. Furthermore, CRSS is superior to RSS in predicting long-term all-cause and cardiac mortality in CRI cases following PCI.
In this study, CR was achieved in only 24.1% of patients, which was obviously lower than previously reports (1–4, 16) but corroborating a recent study in which CR was achieved in 20.8% and 28.2% of CKD and non-CKD patients, respectively (17). CRI cases show higher rates of cardiovascular risk factors and comorbidities, anatomically complex disease, and complications associated with invasive procedures, as well as lower procedural success rates, and worse outcomes (10, 11). CRI cases have elevated risk of developing contrast-related acute kidney injury following PCI (18). Therefore, it is difficult for cardiologists to treat individuals with highly complex CAD and CRI. Furthermore, the current study demonstrated that patients with older age, increased clinical cardiac-kidney comorbidities and more anatomically complex disease, as quantified by CRSS, tended to have IR, corroborating previous reports (3, 9).
The RSS, which was first developed by Stone in a large cohort of acute coronary syndrome (ACS) cases, is considered an important tool for quantifying and risk-stratifying the degree and complexity of residual stenosis following PCI, with a strong independent predictive value for clinical outcomes (1). Its prognostic value has been fully validated in multivessel CAD cases (7, 16), individuals with unprotected left main disease (19), primary PCI cases (6, 20, 21), complex CAD after treatment with second-generation drug-eluting stents (4) and all-comers (3, 5). Our recent study also demonstrated that RSS can help assess reasonable levels of revascularization and ameliorate predictability accuracy in comparison with baseline SS for UR, stroke, and MACCEs for CRI cases after PCI (8). However, the absence of relevant clinical parameters is the main limitation of RSS. Previous studies have demonstrated the incremental prognostic value of scoring systems simultaneously including anatomic and clinical features in comparison with strictly anatomic SS (22). The clinical SS, which combines clinical variables (ACEFCRCL score) with SS, showed superiority over SS or the ACEFSCR score alone in predicting 5-year death and MACCEs in complex CAD after PCI (13).
Park and colleagues firstly described CRSS in patients included in a large, multicenter and all-comer PCI registry, and demonstrated that it has better predictive value for 1-year ACD and target lesion failure after PCI compared with RSS (3). Recently, Song and co-workers assessed the prognostic value of CRSS in a large-sample study examining real-world patients, and the results showed that CRSS has improved predictability of 2-year mortality than the anatomic RSS and SYNTAX revascularization index (9). However, few reports have investigated the predictive value of CRSS in CRI cases.
We first examined the predictive value of CRSS in CRI cases after PCI. In comparison with individuals with CR, those with CRSS >12 had progressively increasing adverse long-term outcomes such as all-cause and cardiac mortality; those with CRSS ≤ 12 had comparable long-term ACD, CD, MI and stroke rates. In multivariable analysis, CRSS was a strong independent predictive factor of all long-term outcomes. Furthermore, CRSS remarkably ameliorated all-cause and cardiac mortality risk stratification, suggesting that compared with RSS, CRSS has greater performance and risk classification ability for long-term all-cause and cardiac mortality in CRI cases. At the same time, this study showed RSS had better predictability accuracy for UR than CRSS, indicating the progression of residual coronary lesions is the main cause of UR. These findings suggest that clinicians should strengthen clinical management, follow-up and secondary prevention for high-risk patients with high CRSS to improve clinical outcomes.
Limitations
Although this study was the first report to validate CRSS in CRI cases undergoing PCI, it had multiple limitations. First, participants were enrolled in a single center, which may lead to selection bias. Secondly, kidney function was examined by serum creatinine-derived EGFR rather than directly measuring kidney function, including iothalamate clearance. Furthermore, patients with CRI have a high risk of developing contrast-induced nephropathy (CIN), which is a strong predictor of poor clinical outcomes post-PCI. We did not evaluate the prognostic effect of CIN in this study. Finally, the functional assessment is paramount in guiding the clinical practice and improving clinical outcomes in patients undergoing PCI (23). However, we did not utilize fractional flow reserve to physiologically evaluate ischemia in vessels with residual disease because of the invasive nature and elevated cost of the procedure, and CR definition was only based on RSS. Further prospective multiple-center randomized studies are warranted for improved evaluation.
Conclusions
In a large-size study including real-world CRI cases following PCI, CRSS independently predicted long-term all-cause and cardiac mortality, MI, UR, stroke and MACCEs, and had improved predictive value for long-term all-cause and cardiac mortality compared with RSS.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committee of Cangzhou Central Hospital, Hebei Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author Contributions
LY, X-FC, and FC provided the conception of the idea for the study. LY, YW, DH, and FC contributed to the development of the methodology and wrote the manuscript. LY and PL analyzed the acquired data. SL and MJ were responsible for the interpretation of statistical results. FC revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the National Key R&D Program of China (2018YFC0116305) and the National Nature Science Foundation of China (91939303, 81820108019).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Mr Zhao Wang at the Medical School of Chinese PLA and Miss Xiaoli Liu at Beihang University for help with data management.
References
1. Genereux P, Palmerini T, Caixeta A, Rosner G, Green P, Dressler O, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol. (2012) 59:2165–74. doi: 10.1016/j.jacc.2012.03.010
2. Farooq V, Serruys PW, Bourantas CV, Zhang Y, Muramatsu T, Feldman T, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. (2013) 128:141–51. doi: 10.1161/CIRCULATIONAHA.113.001803
3. Park KW, Kang J, Kang SH, Ahn HS, Kang HJ, Koo BK, et al. The impact of residual coronary lesions on clinical outcomes after percutaneous coronary intervention: residual SYNTAX score after percutaneous coronary intervention in patients from the efficacy of xience/promus versus cypher in rEducing late loss after stENTing (EXCELLENT) registry. Am Heart J. (2014) 167:384–92. doi: 10.1016/j.ahj.2013.09.015
4. Xu B, Yang YJ, Han YL, Lu SZ, Li B, Liu Q, et al. Validation of residual SYNTAX score with second-generation drug-eluting stents: one-year results from the prospective multicentre SEEDS study. EuroIntervention. (2014) 10:65–73. doi: 10.4244/EIJV10I1A12
5. Song Y, Gao Z, Tang X, Jiang P, Xu J, Yao Y, et al. Impact of residual SYNTAX score on clinical outcomes after incomplete revascularisation percutaneous coronary intervention: a large single-centre study. EuroIntervention. (2017) 13:1185–93. doi: 10.4244/EIJ-D-17-00132
6. Singbal Y, Fryer M, Garrahy P, Lim R. Baseline and residual SYNTAX score in predicting outcomes after acute infarct angioplasty. EuroIntervention. (2017) 12:1995–2000. doi: 10.4244/EIJ-D-15-00269
7. Malkin CJ, George V, Ghobrial MS, Krishnan A, Siotia A, Raina T, et al. Residual SYNTAX score after PCI for triple vessel coronary artery disease: quantifying the adverse effect of incomplete revascularisation. EuroIntervention. (2013) 8:1286–95. doi: 10.4244/EIJV8I11A197
8. Yan L, Li P, Wang Y, Han D, Li S, Zhang J, et al. Impact of the residual SYNTAX score on clinical outcomes after percutaneous coronary intervention for patients with chronic renal insufficiency. Catheter Cardiovasc Interv. (2020) 95(Suppl. 1):606–15. doi: 10.1002/ccd.28652
9. Song Y, Gao Z, Tang XF, Jiang P, Xu JJ, Yao Y, et al. Impact of residual SYNTAX score and its derived indexes on clinical outcomes after percutaneous coronary intervention: data from a large single center. Chin Med J. (2018) 131:1390–6. doi: 10.4103/0366-6999.233958
10. Tsai TT, Messenger JC, Brennan JM, Patel UD, Dai D, Piana RN, et al. Safety and efficacy of drug-eluting stents in older patients with chronic kidney disease: a report from the linked CathPCI registry-CMS claims database. J Am Coll Cardiol. (2011) 58:1859–69. doi: 10.1016/j.jacc.2011.06.056
11. Sarnak MJ, Amann K, Bangalore S, Cavalcante JL, Charytan DM, Craig JC, et al. Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. (2019) 74:1823–38. doi: 10.1016/j.jacc.2019.08.1017
12. Roth D, Bloom RD, Molnar MZ, Reese PP, Sawinski D, Sise ME, et al. KDOQI US commentary on the 2018 KDIGO clinical practice guideline for the prevention, diagnosis, evaluation, and treatment of hepatitis C. Am J Kidney Dis. (2020) 75:665–83. doi: 10.1053/j.ajkd.2019.12.016
13. Garg S, Sarno G, Garcia-Garcia HM, Girasis C, Wykrzykowska J, Dawkins KD, et al. A new tool for the risk stratification of patients with complex coronary artery disease: the clinical SYNTAX Score. Circ Cardiovasc Interv. (2010) 3:317–26. doi: 10.1161/CIRCINTERVENTIONS.109.914051
14. Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. (2009) 5:50–6. doi: 10.4244/EIJV5I1A9
15. Pencina MJ, D'Agostino RB Sr, D'Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. (2008) 27:157–72; discussion 207–12. doi: 10.1002/sim.2929
16. Witberg G, Lavi I, Assali A, Vaknin-Assa H, Lev E, Kornowski R. The incremental impact of residual SYNTAX score on long-term clinical outcomes in patients with multivessel coronary artery disease treated by percutaneous coronary interventions. Catheter Cardiovasc Interv. (2015) 86:3–10. doi: 10.1002/ccd.25753
17. Kim J, Lee JM, Choi KH, Rhee TM, Hwang D, Park J, et al. Differential clinical outcomes between angiographic complete versus incomplete coronary revascularization, according to the presence of chronic kidney disease in the drug-eluting stent era. J Am Heart Assoc. (2018) 7:e007962. doi: 10.1161/JAHA.117.007962
18. Solomon RJ, Natarajan MK, Doucet S, Sharma SK, Staniloae CS, Katholi RE, et al. Cardiac angiography in renally impaired patients (CARE) study: a randomized double-blind trial of contrast-induced nephropathy in patients with chronic kidney disease. Circulation. (2007) 115:3189–96. doi: 10.1161/CIRCULATIONAHA.106.671644
19. Malkin CJ, Ghobrial MS, Raina T, Siotia A, Morton AC, Gunn J. Impact of incomplete revascularization in patients undergoing PCI for unprotected left main stem stenosis. Catheter Cardiovasc Interv. (2013) 81:939–46. doi: 10.1002/ccd.24695
20. Khan R, Al-Hawwas M, Hatem R, Azzalini L, Fortier A, Joliecoeur EM, et al. Prognostic impact of the residual SYNTAX score on in-hospital outcomes in patients undergoing primary percutaneous coronary intervention. Catheter Cardiovasc Interv. (2016) 88:740–7. doi: 10.1002/ccd.26413
21. Altekin RE, Kilinc AY, Onac M, Cicekcibasi O. Prognostic value of the residual SYNTAX score on in-hospital and follow-up clinical outcomes in ST elevation myocardial infarction patients undergoing percutaneous coronary interventions. Cardiol Res Pract. (2020) 2020:9245431. doi: 10.1155/2020/9245431
22. Kashiwagi D, Ebisawa S, Yui H, Maruyama S, Nagae A, Sakai T, et al. Prognostic usefulness of residual SYNTAX score combined with clinical factors for patients with acute coronary syndrome who underwent percutaneous coronary intervention from the SHINANO Registry. Heart Vessels. (2021) 36:170–9. doi: 10.1007/s00380-020-01680-3
Keywords: residual SYNTAX score, clinical residual SYNTAX score, coronary artery disease, percutaneous coronary intervention, chronic renal insufficiency
Citation: Yan L, Li P, Wang Y, Han D, Li S, Jiang M, Cao X and Cao F (2021) The Incremental Prognostic Value of the Clinical Residual SYNTAX Score for Patients With Chronic Renal Insufficiency Undergoing Percutaneous Coronary Intervention. Front. Cardiovasc. Med. 8:647720. doi: 10.3389/fcvm.2021.647720
Received: 24 January 2021; Accepted: 16 March 2021;
Published: 15 April 2021.
Edited by:
Jean Jacques Goy, Fribourg Cantonal Hospital, SwitzerlandReviewed by:
Philippe Commeau, Polyclinique les fleurs Groupe ELSAN, FranceMariama Akodad, Centre Hospitalier Universitaire de Montpellier, France
Copyright © 2021 Yan, Li, Wang, Han, Li, Jiang, Cao and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Cao, ZmVuZ2Nhbzg4MjgmI3gwMDA0MDsxNjMuY29t
†These authors have contributed equally to this work
 Liqiu Yan
Liqiu Yan Peiyao Li3,4†
Peiyao Li3,4† Yabin Wang
Yabin Wang Dong Han
Dong Han Feng Cao
Feng Cao