
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Cardiovasc. Med. , 07 May 2021
Sec. Cardiovascular Epidemiology and Prevention
Volume 8 - 2021 | https://doi.org/10.3389/fcvm.2021.621626
Tooth loss reflects the endpoint of two major dental diseases: dental caries and periodontitis. These comprise 2% of the global burden of human diseases. A lower number of teeth has been associated with various systemic diseases, in particular, atherosclerotic cardiovascular diseases (ACVD). The aim was to summarize the evidence of tooth loss related to the risk for ACVD or death. Cohort studies with prospective follow-up data were retrieved from Medline-PubMed and EMBASE. Following the PRISMA guidelines, two reviewers independently selected articles, assessed the risk of bias, and extracted data on the number of teeth (tooth loss; exposure) and ACVD-related events and all-cause mortality (ACM) (outcome). A total of 75 articles were included of which 44 were qualified for meta-analysis. A lower number of teeth was related to a higher outcome risk; the pooled risk ratio (RR) for the cumulative incidence of ACVD ranged from 1.69 to 2.93, and for the cumulative incidence of ACM, the RR ranged from 1.76 to 2.27. The pooled multiple adjusted hazard ratio (HR) for the incidence density of ACVD ranged from 1.02 to 1.21, and for the incidence density of ACM, the HR ranged from 1.02 to 1.30. This systematic review and meta-analyses of survival data show that a lower number of teeth is a risk factor for both ACVD and death. Health care professionals should use this information to inform their patients and increase awareness on the importance of good dental health and increase efforts to prevent tooth loss.
In general, a lower number than 32 natural teeth in adults reflects the endpoint of dental caries and periodontitis. Tooth loss at a younger age is mainly due to caries, and in older ages, it is due to periodontitis. The cumulative incidence for caries peaks before the age of 30, while for periodontitis, it peaks between 20 and 40 years of age. The worldwide prevalence of severe tooth loss ( ≤9 remaining teeth) is 2.4% (1, 2). Tooth loss leads to reduced masticatory function, poorer nutritional status and unhealthy dietary changes, low self-esteem and quality of life, and negative general health (3–5). The burden of disease of severe caries, severe periodontitis, and the consequent tooth loss comprises 2% of the global burden of human diseases (6).
Apart from genetic and biological determinants, caries and periodontitis (and subsequent tooth loss) share several risk factors. In particular, hyposalivation, smoking, dysbiotic oral biofilms, and dietary fermentable carbohydrates contribute to their occurrence, while diabetes, obesity, and rheumatoid arthritis have been shown to be associated with both oral diseases (3, 4).
While material, behavioral, cultural, and psychosocial factors have been shown to contribute to the risk of both oral diseases and atherosclerotic cardiovascular diseases (ACVD) (7, 8), a biomedical connection between tooth loss and ACVD has also been investigated (9, 10). Shared pathways for oral diseases and ACVD have been proposed and studied; notably, short-lived bacteremias in periodontitis give rise to low-grade systemic inflammation and pro-inflammatory action and may contribute to the onset of atherosclerosis (11, 12). The atherosclerotic process may eventually lead to the occurrence of ACVD events (morbidity or mortality), like coronary heart diseases (CHD), cerebrovascular accidents, and peripheral arterial disease (13, 14). ACVD is responsible for up to 54% of deaths in the United States and 45% of deaths in Europe (15, 16).
Although the relationship between tooth loss and ACVD-related events and all-cause mortality (ACM) has been studied often, conflicting results have been reported, and solid evidence is lacking (17–20). Previously published systematic reviews did not allow for solid conclusions about the relationship between the number of teeth and ACVD, as they include a small number of studies (20) or restricted the outcome to ACM only (19). This systematic review and meta-analysis reports up-to-date evidence about the relationship between tooth loss, ACVD-related events, and ACM.
This systematic review and meta-analyses were conducted in accordance with the guidelines of Preferred Reporting Items of Systematic Reviews and Meta-analyses (PRISMA Statement) and the guidelines for Meta-analysis Of Observational Studies in Epidemiology (MOOSE Guidelines) (Supplementary Files 1, 2) (21, 22).
Is tooth loss, particularly a lower number of present teeth, more related to an increased risk for ACVD-related events (morbidity or mortality) and ACM?
Any study that evaluated the relationship between the number of teeth and ACVD-related morbidity, ACVD-related mortality, or ACM was retrieved from PubMed-Medline (National Library of Medicine, Washington, D.C.) and EMBASE (Excerpta Medical Database by Elsevier). We reported on studies included in these databases before June 17, 2020. The search was conducted by NB (for detail on the used search terms, see Supplementary File 3). There were no additional records identified through other sources, all studies were available, and, therefore, it was decided that there was no need to contact the authors of identified publications.
We included cohort studies reported in the English language that evaluated a prospective relationship between the number of teeth and ACVD events or ACM at any follow-up time. Study participants, regardless of age, with a known (categorical or linear scaled) number of teeth at study inclusion were followed longitudinally to assess for the occurrence of ACVD events or ACM. Cumulative incidences and incidence densities were calculated. Events were based on information from hospital admissions (ICD codes, medical records), death certificates, self-report, or questionnaires. Cross-sectional studies, case-control studies, review articles, letters, personal opinions, book chapters, conference abstracts, patents, and articles written in a language other than English were excluded.
Two reviewers (NB and NS) independently screened titles of the retrieved studies based on the eligibility criteria mentioned above. The studies were categorized as definitely not eligible (notably, to be excluded), definitely eligible, or to be decided. Next, the reviewers screened abstracts for records, which were judged as to be decided. Subsequently, the same approach was followed for screening based on abstract. Thereafter, full texts were obtained for studies that met the inclusion criteria during screening based on the abstract or which then remained to be decided. Eligibility for final inclusion of publications was based on full text reading. Reviewers resolved initial disagreements by consensus discussion. For the reference list of the included studies, see Supplementary File 4.
Two reviewers (NB and NS) used the ROBINS-E Tool (Risk Of Bias In Non-Randomized Studies—of Exposures) to assess the methodological quality and potential risk of bias of the included studies. The ROBINS-E tool comprises seven domains of bias: confounding, selection of participants into the study, classification of exposures, departures from intended exposures, missing data, measurement of outcomes, and selection of the reported result. Each domain was categorized into a low, moderate, or serious risk of bias. Judgments within each domain were summarized into an overall risk of bias assessment for each study (23). If one domain was judged as a serious risk of bias, the overall risk of bias of that study was assessed as a serious risk of bias. If all the domains were judged as low risk of bias, the overall risk of bias of that study was assessed as low risk of bias. Otherwise, the study was judged as a moderate risk of bias.
The following study data reported in the articles that met the selection criteria were extracted: author names, country, study design (inception or non-inception cohorts), the total number of participants and their demographic characteristics (age and sex), number of remaining teeth, number of participants with incident ACVD-related events or ACM, and follow-up time. Based on this information, it was possible to calculate the crude risk ratio (RR) with a 95% confidence interval (95% CI) for the cumulative incidence of ACVD-related events and ACM. Next to this, the crude and adjusted hazard ratio (HR) with 95% CI for the incidence density of ACVD-related events and ACM in different categories of the remaining number of teeth, if reported, were also obtained from the articles. The crude RR and HR were defined as the RR or HR of the number of teeth for ACVD-related events and ACM, not adjusted for other variables available in the included studies. The adjusted HR was defined as the HR adjusted for age and sex only or by multiple variables, such as education level, socioeconomic status, lifestyle habits or general health, etc., available in the included studies (see Supplementary Tables 1, 2).
The indicators for the potential risk of bias of the included studies contained the approaches to count the number of remaining teeth, patients' ACVD status at baseline, and follow-up rate. In the review, the approaches to counting the remaining number of teeth were classified into two categories: (1) based on clinical examination and (2) based on patients' self-reporting. Patients' ACVD status at baseline was classified into two categories: (1) ACVD status was presented and adjusted/excluded at baseline, and (2) ACVD status was presented without adjustment/exclusion at baseline or no information. The follow-up rate was classified into two categories: (1) low follow-up rate (<80%) and (2) high follow-up rate (≥80%). All the data were independently extracted by NB and NS, crossed-checked, and discussed to resolve possible disagreements.
Cumulative incidence is the measure of the occurrence of new ACVD-related events or ACM during the follow-up period. To assess the cumulative incidence of ACVD-related events and ACM between different groups of the number of remaining teeth, network meta-analyses with random effect models were carried out using the total number of study participants and the number of ACVD-related events or ACM.
Most of the included studies compared exposures (notably, the number of remaining teeth) using four common exposure categories:
• 0 teeth vs. 1–32 teeth,
• 0–19 teeth vs. 20–32 teeth,
• 0 teeth vs. 1–19 teeth vs. 20–32 teeth,
• 0–10 teeth vs. 11–16 teeth vs. 17–24 teeth vs. 25–32 teeth.
Some studies, using other than these four common categories, allowed transformation into the above, whereas the studies in which this was not possible were excluded for meta-analysis.
Two of the four common exposure categories included more than two groups. Therefore, network meta-analyses with random effect models were carried out (24). Network meta-analysis is defined as a meta-analysis comprising direct exposure comparisons within trials and indirect exposure comparisons across trials for a common comparator against at least two exposure groups (24). Because all the included studies in the present review reported data for all the exposure groups, the comparisons between any two groups in the network meta-analyses can be made directly. Therefore, the evidence from the indirect comparisons can be ignorable, and the assessment of ranking probabilities of each group and of the inconsistency between direct and indirect evidence was not necessary. The other two common exposure categories included two groups only, and, therefore, pair-wise meta-analyses were performed. Cumulative meta-analyses were used to assess the change in the aggregate estimate by adding study data in the order of the time of their publication (25). The results for studies reporting cumulative incidence data for ACVD-related events or ACM by common exposure category were statistically pooled and expressed as risk ratio (RR) and 95% confidence intervals (95% CI).
Incidence density (or hazard) is the measure for the rate of occurrence of new ACVD-related events or ACM per unit of time, the person-time of follow-up. It allows for pooling studies with different durations of follow-up. To compare the incidence density of ACVD-related events or ACM between different groups of the number of remaining teeth, generic inverse variance meta-analyses with random effect models were carried out to pool the hazard ratio (HR) of ACVD-related events or ACM of the individual studies. The HR was pooled separately based on two out of the four common categories in which the number of remaining teeth was classified only into two groups:
• 0 teeth vs. 1–32 teeth,
• 0–19 teeth vs. 20–32 teeth.
The other two common categories, in which the number of teeth was classified into more than two groups, were not included in the assessment of incidence density because the generic inverse variance meta-analysis only allows for the HR between two groups. Besides, the HR was pooled per number of lost teeth when the number of remaining teeth was regarded as a continuous variable. The HR was also pooled separately for different types of HR (crude HR, HR adjusted by age/sex, and HR adjusted by multiple variables). Cumulative meta-analyses were used to assess the change in the aggregate estimate by adding study data in the order of the time of their publication (25). The HR and standard errors (SE) of individual studies were log-transformed based on the formulas provided by Woods et al. (26). The pooled results were expressed as HR and 95% CI. The statistical heterogeneity of each meta-analysis was explored by the I2 test. The heterogeneity was considered substantial to considerable if I2 > 50% (27).
Funnel plots were used to assess the publication bias for the meta-analyses, which included at least 10 studies. A funnel plot for a meta-analysis including fewer than 10 studies is not recommended because of its insufficient statistical power (28).
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) system was used to appraise the strength of the evidence emerging from this review. Two reviewers (NB and NS) rated the strength of the evidence according to the factors that can reduce the quality of evidence (risk of bias, inconsistency of results, indirectness of evidence, imprecision, and publication bias) and the factors that can increase the quality of evidence (large magnitude of the effect, dose-response gradient, and effect of plausible residual confounding) (29). Any disagreement between the two reviewers was resolved by discussion.
All analyses were performed with the R software 3.3 (R Development Core Team, Vienna, Austria) and Review Manager 5.4 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Figure 1 shows a flowchart of the study selection. The database search revealed 3,857 potential articles, of which 1,386 articles were removed for being duplicates. In the first screening based on title, 1,998 articles were excluded, leaving 473 articles for screening on the abstract; based on this, 289 articles were excluded, leaving 184 articles for full-text reading. Based on the full-text reading, another 109 articles were excluded, leaving 75 articles included for further analysis (for the reference list, see Supplementary File 3). The agreements between the two reviewers (NB and NS) based on the screening of titles, abstracts, and full-text reading were 92, 78, and 90%, respectively. Because the categories of the number of teeth in these 75 studies were too heterogeneous to allow for all to undergo transformation into any of the four common categories of the number of teeth, 44 articles were qualified for meta-analysis.
Table 1 shows the main characteristics of the 75 included articles for the qualitative synthesis. The articles were derived from all continents with the number of participants ranging from 173 to 4,440,970 [median: 5,688 and interquartile range (IQR): 718–41,000]. The majority of the studies included both males and females, whereas eight studies only included men, three studies only women, and, for one study, the male/female ratio was unknown. Only in 25 out of the 75 studies was the age of the study participants ≥60 years of age, whereas the other studies included participants from a wider age range. The maximum follow-up time ranged from 1 to 57 years. Most studies used clinical examination to assess the number of teeth (51 studies). For reporting of the outcome, 26 studies reported both ACVD-related events and ACM, 24 studies only reported ACM, and 25 studies only reported ACVD-related events. This information was mostly retrieved from medical records, death certificates, and death registers. All studies were prospective observational cohort studies, 67 studies reported findings from Cox proportional hazard analysis, five studies used logistic regression models, two studies used Poisson regression models, and one study applied a linear regression model. Exclusion of participants with prevalent ACVD at baseline was performed in 30 studies, and therefore, these studies could be defined as inception cohorts. In 21 studies, adjustment for prevalent ACVD at baseline was performed, whereas in 24 studies, no adjustment was performed, or no information for ACVD at baseline was available. The follow-up rate was high (≥80%) in 68 studies, low (<80%) in six studies, and unknown in one study (Table 1).
Supplementary Tables 1, 2 show the descriptive information and summary results of the studies regarding tooth loss and ACVD-related events (Supplementary Table 1) and regarding tooth loss and ACM (Supplementary Table 2).
To estimate the potential risk of bias, the methodological qualities of the included studies were assessed. Overall, out of the 44 studies, the potential risk of bias was estimated to be “low” for 28 studies, “moderate” for three studies, and “serious” for 13 studies. This overall risk of bias assessment was estimated based on the risk of bias assessment within the seven domains. Within the domain confounding, there were 11 studies estimated as “serious,” and two studies were estimated as “moderate” risk of bias. Within the domain classification of exposures, there was only one study that was estimated as “moderate” risk of bias; within the domain measurement of the outcomes, there was only one study that was estimated as “serious” risk of bias; and within the domain missing data, two studies were estimated as “serious” risk of bias and two studies as “moderate” risk of bias. All the other studies within these domains were assessed as “low” risk of bias. Within the domain selection of participants into the study, departures from intended exposures, and selection of the reported result, all studies were estimated as “low” risk of bias (Supplementary File 5).
Using pairwise meta-analysis, 10 studies were pooled, including the number of remaining teeth classified into 0 and 1–32 teeth, and four studies with the number of remaining teeth were classified into 0–19 and 20–32 teeth. Using network meta-analysis, two studies with the number of remaining teeth were classified into 0, 1–19, and 20–32 teeth, and four studies with the number of teeth were classified into 0–10, 11–16, 17–24, and 25–32 teeth. The results showed that the categories with a lower number of remaining teeth always had a significantly higher risk of ACVD-related events than the categories with a higher number of remaining teeth (Figure 2A and Supplementary Table 3). The highest RR was found in the comparison of 0 teeth vs. 1–32 remaining teeth [RR: 2.93 (1.92–4.50)], 0 teeth vs. 20–32 remaining teeth [RR: 2.65 (1.77–3.98)], and 0–10 remaining teeth vs. 25–32 remaining teeth [RR: 2.65 (1.84–3.81)] (Figure 2A and Supplementary Table 3). The heterogeneity of those meta-analyses ranged from 0 to 99%.
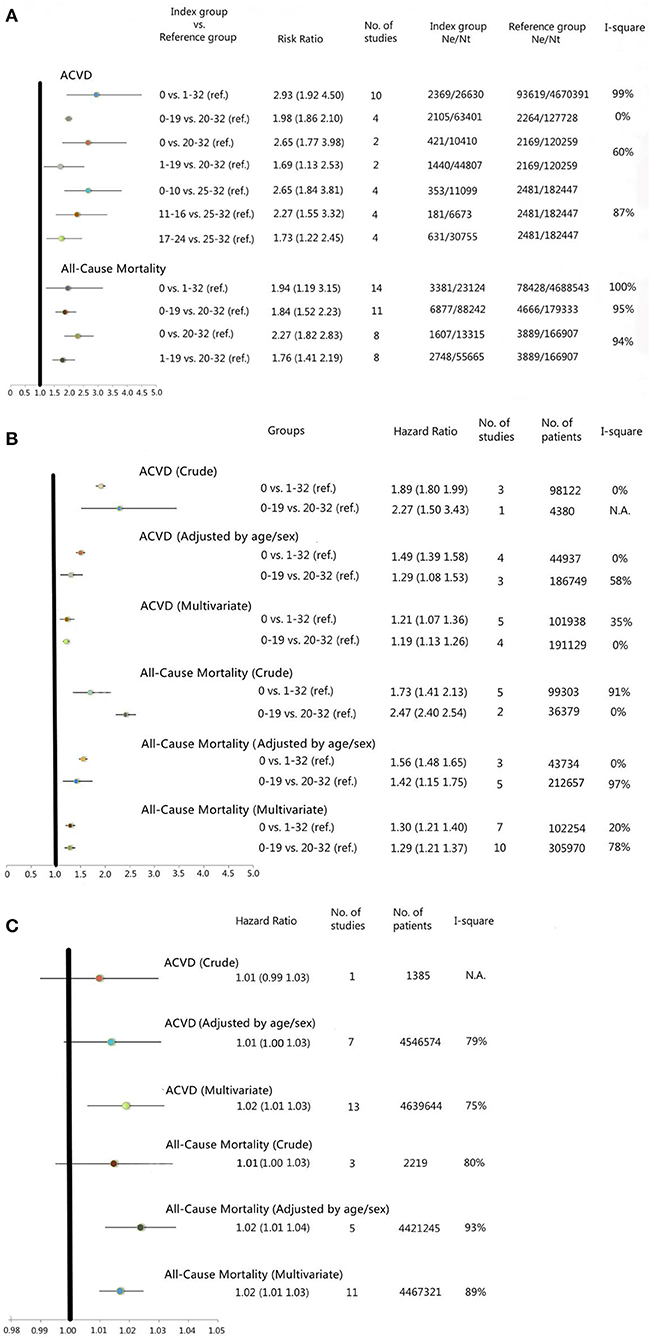
Figure 2. (A) Forest plots for meta-analysis of cumulative incidence for categorical data of the number of teeth, ACVD, and all-cause mortality. (B) Forest plots for meta-analysis of incidence density for categorical data of the number of teeth, atherosclerotic cardiovascular disease (ACVD) and all-cause mortality. (C) Forest plots for meta-analysis of incidence density for continuous data of the number of teeth, ACVD, and all-cause mortality. ACVD, Atherosclerotic Cardiovascular Disease; vs., versus; ref., reference group; Ne, number of events; Nt, number of total included study participants; N.A., Not Applicable. The Hazard Ratio (HR) in the Forest Plot which was based only on one study, was obtained directly from the included study.
Using generic inverse variance meta-analysis for calculation of HR, five studies were included with the number of remaining teeth classified into 0 and 1–32 teeth, and four studies were included with the number of remaining teeth classified into 0–19 and 20–32 teeth. The results showed that the categories with a lower number of remaining teeth had significantly higher HR of ACVD-related events than the categories with a higher number of remaining teeth in both the crude and adjusted (for age/sex and for multiple variables) models (Figure 2B and Supplementary Table 4). The categories edentulous vs. 1–32 teeth and 0–19 teeth vs. 20–32, showed an increased hazard for ACVD in the lowest category of teeth [multiple adjusted model; 0 vs. 1–32, HR: 1.21 (1.07–1.36), 0–19 vs. 20–32, HR: 1.19 (1.13–1.26)] (Figure 2B and Supplementary Table 4). The heterogeneity of those meta-analyses ranged from 0 to 58%.
Using generic inverse variance meta-analysis for calculation of HR, 13 studies were included with the number of remaining teeth regarded as a continuous variable. The results showed an increased hazard for ACVD with an increased number of lost teeth in the multiple adjusted model [HR: 1.02 (1.01–1.03)] (Figure 2C and Supplementary Table 4). The heterogeneity of those meta-analyses ranged from 75 to 79%.
Most of the subgroup analyses, based on the approaches to count the remaining number of teeth, patients' ACVD status at baseline, and follow-up rate of the included studies, showed no statistically significant changes in the outcome (Supplementary Tables 3, 4). The heterogeneity was not reduced significantly in the subgroup analyses. This indicated that the three indicators may not significantly influence the outcomes and may not be the important reason to cause heterogeneity of the pooled results.
Using pairwise meta-analysis, 14 studies were included with the number of remaining teeth classified into 0 and 1–32 teeth, and 11 studies with the number of remaining teeth classified into 0–19 and 20–32 teeth. Using network meta-analysis, eight studies were included with the number of remaining teeth classified into 0, 1–19, and 20–32 teeth. None classified the number of remaining teeth into four categories. The results showed that the categories with a lower number of remaining teeth had a significantly higher risk of ACM than the categories with a higher number of remaining teeth (Figure 2A and Supplementary Table 3). The highest RR was found in the comparison of 0 teeth vs. 20–32 remaining teeth [RR: 2.27 (1.82–2.83)] (Figure 2A and Supplementary Table 3). The heterogeneity of those meta-analyses ranged from 94 to 100%.
Using generic inverse variance meta-analysis, seven studies were included with the number of remaining teeth classified into 0 and 1–32 teeth, and 10 studies were included with the number of remaining teeth classified into 0–19 and 20–32 teeth. The results showed that the categories with a lower number of remaining teeth had significantly higher HR of ACM than the categories with a higher number of remaining teeth in both the crude and adjusted (for age/sex and for multiple variables) models (Figure 2B and Supplementary Table 4). The categories edentulous vs. 1–32 teeth and 0–19 teeth vs. 20–32 showed an increased hazard for ACM in the lowest category of teeth [multiple adjusted model; 0 vs. 1–32, HR: 1.30 (1.21–1.40), 0–19 vs. 20–32, HR: 1.29 (1.21–1.37)] (Figure 2B and Supplementary Table 4). The heterogeneity of those meta-analyses ranged from 0 to 97%.
Using generic inverse variance meta-analysis, 11 studies were included with the number of remaining teeth regarded as a continuous variable. The results showed an increased hazard for ACM with an increased number of lost teeth in the multiple adjusted model [HR: 1.02 (1.01–1.03)] (Figure 2C and Supplementary Table 4). The heterogeneity of those meta-analyses ranged from 80 to 93%.
Most of the subgroup analyses, based on the approaches to count the remaining number of teeth, patients' ACVD status at baseline, and follow-up rate of the included studies, showed no statistically significant changes in the outcome (Supplementary Tables 3, 4). The heterogeneity was not reduced significantly in all subgroup analyses, except in the subgroup analysis for crude HR of 0 vs. 1–32 remaining teeth. This indicated that the three indicators may not significantly influence the outcomes and may not be the important reason to cause heterogeneity of the pooled results.
The cumulative meta-analyses showed a rather limited overtime drift for the pooled RR and pooled HR and their confidence intervals (Supplementary Tables 5, 6). With some exemptions, the pooled RR and HR ranged between 1 and 2. Hence, there is a fairly stable overtime relationship between the number of teeth and ACVD or ACM-related outcomes, but the width of the confidence intervals did not narrow in a constant manner.
To estimate the level of publication bias, funnel plots were created for six meta-analyses with at least 10 studies. The results showed that there was no to minor publication bias for these meta-analyses (Supplementary File 6).
Supplementary File 7 presents a summary of the various factors used to rate the strength of the evidence according to GRADE. The rating was assessed for all the separate meta-analyses. The cumulative incidence for categorical data of the number of teeth and ACVD showed two meta-analyses having moderate strength of evidence and two meta-analyses having high strength of evidence. The cumulative incidence for categorical data of the number of teeth and ACM showed two meta-analyses having low strength of evidence and one meta-analysis having high strength of evidence. The multivariable incidence density for categorical and continuous data of the number of teeth and ACVD showed one meta-analysis having low strength of evidence and two meta-analyses having moderate strength of evidence. The multivariable incidence density for categorical and continuous data of the number of teeth and ACM showed two meta-analyses having low strength of evidence and one meta-analysis having moderate strength of evidence (Supplementary File 7).
To our knowledge, this systematic review and meta-analyses containing 75 prospective cohort studies from all over the world, including a diversity of populations of both men and women of all ages, is the largest to date providing evidence that tooth loss is related to an increased risk for ACVD-related events and ACM. The crude analyses showed that tooth loss is related to ACVD morbidity, ACVD mortality, and ACM: the lower the number of remaining teeth, the higher the risk of an ACVD event or death. These effects remained after adjusting for methodological weaknesses of the analyzed studies.
To interpret and explain the risk of tooth loss for ACVD, several plausible (biological) mechanisms need to be taken into consideration.
• Tooth loss and ACVD share risk factors, such as age, sex, SEP, obesity, and smoking (105). As a consequence, their subsequent occurrence during the life course reveals to be associated. While earlier research has shown a dose-response relationship (20), the direction, size, and precision of association estimates we reported here are consistent throughout all analyses. Hence, it is unlikely that this association is coincidental.
• Tooth loss is the ultimate event representing two major dental pathologies. (i) Dental caries is a lifelong disease and traditionally considered an important cause of tooth loss. Dental caries has a multifactorial etiology, but the consumption of dietary carbohydrates is the main factor (1, 2). This corresponds to a risk factor for ACVD, namely, overconsumption of carbohydrates leads to overweight and obesity, metabolic syndrome, and diabetes; these are obvious risk factors for ACVD (3–6). (ii) At older ages, periodontitis is the main cause of tooth loss. Periodontitis is a chronic multi-causal inflammatory disease of the supportive tissues of the teeth with progressive loss of attachment and alveolar bone, finally leading to tooth loss (1, 2). Ample research has been performed to identify pathophysiological mechanisms to explain the association between periodontitis and ACVD (11, 12). Thus, since periodontitis is associated with ACVD, the ultimate endpoint is also associated. A low-grade systemic inflammation in periodontitis and daily short-lived bacteremias in relation to atherosclerosis have been investigated (106–108). Low-grade chronic systemic inflammatory stress in periodontitis is considered to contribute to increased inflammation around atherosclerotic plaques at predilection places and vulnerable arteries; circulating bacteremia contribute to a pro-inflammatory and pro-thrombotic state, may induce autoimmunity, as well as dyslipidemia (11, 12). Increased adjusted RR for the relationship between periodontitis and ACVD from 1.50 up to 3.20 has been reported (14, 109).
• Masticatory dysfunction and related dietary changes have been proposed (5, 110, 111). An impaired masticatory function may lead to inadequate food choices and, therefore, reduced amounts of nutrients. This may include increases in intake of industrially processed rather than natural foods, avoiding hard-to-chew food, and home processing their foods into softer foods. In turn, this leads to increased intake of fermentable carbohydrates, saturated fatty acids, and reduction of the sources of dietary fiber and essential vitamins and minerals, consequently contributing to systemic diseases (3, 5, 110–113). A study reporting about the link between tooth loss, nutritional status, and stroke outcomes showed in the multivariable analysis that tooth loss and a worse nutritional status were independently associated with poor stroke outcomes (OR: 1.33) (114).
• Socioeconomic position (SEP) is an explanatory variable for a lower number of teeth for which strong and consistent evidence is available. SEP is defined mainly based on income, education, and employment status. Several studies show that low SEP is associated with significant tooth loss (7, 8). SEP influences lifestyle habits like smoking and performing good oral hygiene. Also, access to healthcare centers and periodic dental examination is more limited for people with a low SEP (7, 115, 116). SEP also plays a role in the development of ACVD. In people with low SEP, biological, behavioral, material, and psychosocial risk factors (like health insurance and financial difficulties, obesity, smoking, physical inactivity, life events, educational inequalities), lower health literacy, and inequalities in access to care and medical treatment, accentuate the link between SEP, ACVD, and mortality (8, 117). For low adulthood SEP, multiple adjusted increased risks for ACVD up to 1.84 were reported (8).
Despite a large number of studies and the state-of-art methodologies applied, within the findings of this systematic review and meta-analyses, the following aspects observed in the study methods need attention.
• The risk of bias assessment in the individual studies, by using the ROBINS-E tool, showed a low risk of bias for 28 studies, a moderate risk of bias for 3 studies, and a serious risk of bias for 13 studies. For the studies with moderate and serious risk of bias, the main issue was the bias due to confounding, where important covariables for the relation between the number of teeth and ACVD or ACM were not available in the multivariable analyses. It is difficult to predict the direction of bias for the outcome, but we can assume that a suboptimal multivariable analysis causes an overestimation of the effect. Funnel plots were made to assess the publication bias for the larger meta-analyses and showed none to a minor level of publication bias.
• Some studies defined the determinant (number of remaining or missing teeth) based on patients' self-reported information. This may be less accurate than the number of teeth based on clinical examination and may bias the results of the review. In addition, most included studies use categories containing up to 32 remaining teeth. Whether third molars should be incorporated in defining a full dentition remains controversial. This aspect could introduce bias, but considering the fact that the used categories contain groups of 1–32, 20–32, or 25–32 teeth, the introduced bias is negligible considering a full dentition containing only 28 teeth (excluding third molars) is also incorporated in those categories. Also, a large number of the currently included studies used two groups of present teeth in their statistical analysis: groups 0–19 teeth vs. 20–32 teeth. Most likely, this is based on the fact that in dentistry, 20 teeth present is considered as the minimal number of teeth needed for sufficient chewing ability (118).
• Only 15 studies included in the meta-analyses are inception cohort studies, which only included participants without ACVD at baseline. In another 14 studies, a part of the participants had ACVD at baseline, but this was adjusted for in the analysis. However, in the remaining 15 studies, some participants had ACVD at baseline without adjustment in the analysis or the information on participants' ACVD status at baseline, and the adjustment was not reported. For those 15 studies, the association between the number of teeth and the outcomes may be overestimated if the prevalent ACVD at baseline was included without adjustment. This may bias the pooled results of the meta-analyses.
• The follow-up rate differed between studies and was classified into <80% and ≥80% follow-up rates. Loss to follow-up may severely compromise the validity of a study and bias the results if the patients who drop out are different from those who do not drop out (119). Based on the rule of thumb, a dropout rate >20% may cause serious bias (120). In the present study, we assumed that the patients who experienced the events at follow-up may be more likely to drop out than those without events, and this may lead to the underestimation of the results. However, the subgroup analyses using the three indicators for risk of bias, i.e., the approaches to count the number of remaining teeth, patients' ACVD status at baseline, and follow-up rate, showed a very minor effect on the heterogeneity of the meta-analyses. This indicated that the level of risk of bias across the included studies was not the main reason for the heterogeneity of the meta-analyses (Supplementary Tables 3, 4).
• The harmonization of the number of teeth varied across studies. Some studies reported the number of remaining or missing teeth as a continuous variable, while other studies used different categories for the number of remaining or missing teeth, and these categories were not always comparable and transferrable across included studies. Also, probably in most of these studies, the categories were post-hoc defined. Therefore, 44 studies using the four predefined common categories of exposure comparisons qualified for meta-analyses. Due to the exclusion of 31 studies, an overestimation of effect cannot completely be ruled out. However, by using this predefined approach to meta-analysis, we have found a consistent effect across the reported separate meta-analyses. Moreover, none of the overall estimates of the cumulative meta-analyses showed meaningful changes over time (Supplementary Tables 5, 6).
• The heterogeneity in the meta-analyses was high. The I2 for some of the meta-analyses was larger than 75% (Figures 2A–C and Supplementary Tables 3, 4), which indicated considerable heterogeneity. So perhaps, conventionally, one would refrain from pooling, as a random-effects model will not allow remediation of this situation (27). Moreover, the sensitivity analyses did not provide clues for sources of heterogeneity. Therefore, the remaining uncertainty is whether this unexplained heterogeneity due to the residual variation results in either an overestimation or an underestimation of the estimates of effect (so bias in the estimates). The high heterogeneity may be caused by differences in follow-up periods and multivariate adjustments across included studies, but also by their variated study populations, notably patients' age and countries of origin. For example, there were quite some studies only including participants at older ages (≥60 years of age) who are known, on the one hand, to carry a higher risk for ACVD events or ACM (121), while the peak incidence of severe tooth loss is at 65 years of age (4). The follow-up time of the included studies was quite diverse. With a longer follow-up period, more study participants may experience an ACVD event or die. Also, the exposure, tooth loss, is a time-dependent variable, while in most studies, it is reported as the number of teeth at baseline, which is seen as time independent. This may have resulted in an underestimation of the effect. In addition, the covariates in the multivariate models are diverse across studies. The multivariate HR values adjusted for various covariates were directly pooled in the meta-analysis. Besides, the rationale for selection of the covariates in most studies was not reported. It is not known whether the covariates were determined a priori or simply based on the availability of potential confounding data at hand. If the latter is the case, this may have biased the findings of the meta-analyses.
• Across studies, the evidence emerging from the separate meta-analysis, assessed by the use of GRADE, varies. For the meta-analyses with ACVD as the outcome, the strength of the evidence was mainly moderate. For the meta-analyses with ACM as the outcome, the strength of the evidence was mainly low. Therefore, our conclusion based on the outcome ACVD is more valid than our conclusion based on the outcome ACM.
In conclusion, this large systematic review and meta-analysis of survival data shows that a lower number of teeth increases the risk of ACVD-related morbidity or mortality, and ACM. Dental professionals should use this knowledge to inform their patients and the public at large to be aware of their general health and visit their general physician to discuss this aspect; and, vice versa, medical specialists should motivate their patients to visit the dentist regularly and to encourage them to maintain their own teeth as much as possible.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
NB and NS contributed to the conception, design, data acquisition, analysis, interpretation, and drafted and critically revised the manuscript. BL and GH contributed to the conception, design, analysis, interpretation, and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work ensuring integrity and accuracy.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank Dr. E. P. Jansma, Medical Information Specialist, for the contribution to the design and implementation of the search strategy.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.621626/full#supplementary-material
1. Kassebaum NJ, Bernabe E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res. (2014) 93(7 Suppl.):20S–8S. doi: 10.1177/0022034514537828
2. Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. (2019) 394:249–60. doi: 10.1016/S0140-6736(19)31146-8
3. Chapple IL, Bouchard P, Cagetti MG, Campus G, Carra MC, Cocco F, et al. Interaction of lifestyle, behaviour or systemic diseases with dental caries and periodontal diseases: consensus report of group 2 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. (2017) 44(Suppl.18):S39–51. doi: 10.1111/jcpe.12685
4. Tonetti MS, Bottenberg P, Conrads G, Eickholz P, Heasman P, Huysmans MC, et al. Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well-being as an essential component of healthy ageing - Consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. (2017) 44(Suppl.18):S135–44. doi: 10.1111/jcpe.12681
5. Ervin RB, Dye BA. Number of natural and prosthetic teeth impact nutrient intakes of older adults in the United States. Gerodontology. (2012) 29:e693–702. doi: 10.1111/j.1741-2358.2011.00546.x
6. DALYs GBD, Collaborators H. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. (2016) 388:1603–58. doi: 10.1016/S0140-6736(16)31460-X
7. Duijster D, Oude Groeniger J, van der Heijden G, van Lenthe FJ. Material, behavioural, cultural and psychosocial factors in the explanation of socioeconomic inequalities in oral health. Eur J Public Health. (2018) 28:590–7. doi: 10.1093/eurpub/ckx209
8. Kamphuis CB, Turrell G, Giskes K, Mackenbach JP, van Lenthe FJ. Socioeconomic inequalities in cardiovascular mortality and the role of childhood socioeconomic conditions and adulthood risk factors: a prospective cohort study with 17-years of follow up. BMC Public Health. (2012) 12:1045. doi: 10.1186/1471-2458-12-1045
9. Offenbacher S, Barros SP, Altarawneh S, Beck JD, Loewy ZG. Impact of tooth loss on oral and systemic health. Gen Dent. (2012) 60:494–500.
10. Joshipura K. The relationship between oral conditions and ischemic stroke and peripheral vascular disease. J Am Dent Assoc. (2002) 133(Suppl.):23S–30S. doi: 10.14219/jada.archive.2002.0373
11. Schenkein HA, Loos BG. Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases. J Clin Periodontol. (2013) 40(Suppl.14):S51–69. doi: 10.1111/jcpe.12060
12. Sanz M, Marco Del Castillo A, Jepsen S, Gonzalez-Juanatey JR, D'Aiuto F, Bouchard P, et al. Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol. (2020) 47:268–88. doi: 10.1111/jcpe.13189
13. Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res. (2016) 118:535–46. doi: 10.1161/CIRCRESAHA.115.307611
14. Lockhart PB, Bolger AF, Papapanou PN, Osinbowale O, Trevisan M, Levison ME, et al. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association?: a scientific statement from the American Heart Association. Circulation. (2012) 125:2520–44. doi: 10.1161/CIR.0b013e31825719f3
15. Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. (2016) 37:3232–45. doi: 10.1093/eurheartj/ehw334
16. Writing Group M, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. (2016) 133:e38–360. doi: 10.1161/CIR.0000000000000350
17. Pussinen PJ, Kononen E. Oral health: a modifiable risk factor for cardiovascular diseases or a confounded association? Eur J Prev Cardiol. (2016) 23:834–8. doi: 10.1177/2047487316636506
18. Bauersachs J, Berliner D. Poor oral health and coronary artery disease: association or causality? Eur J Prev Cardiol. (2018) 25:596–7. doi: 10.1177/2047487318761053
19. Koka S, Gupta A. Association between missing tooth count and mortality: a systematic review. J Prosthodont Res. (2018) 62:134–51. doi: 10.1016/j.jpor.2017.08.003
20. Peng J, Song J, Han J, Chen Z, Yin X, Zhu J, et al. The relationship between tooth loss and mortality from all causes, cardiovascular diseases, and coronary heart disease in the general population: systematic review and dose-response meta-analysis of prospective cohort studies. Biosci Rep. (2019) 39:1773. doi: 10.1042/BSR20181773
21. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. (2009) 62:1006–12. doi: 10.1016/j.jclinepi.2009.06.005
22. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
23. The ROBINS-E tool. Risk Of Bias In Non-randomized Studies - of Exposures. Available online at: https://www.bristol.ac.uk/population-health-sciences/centres/cresyda/barr/riskofbias/robins-e/ (accessed March 12, 2021).
24. Li T, Puhan MA, Vedula SS, Singh S, Dickersin K, Ad Hoc Network Meta-analysis Methods Meeting Working G. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. (2011) 9:79. doi: 10.1186/1741-7015-9-79
25. Leimu R, Koricheva J. Cumulative meta-analysis: a new tool for detection of temporal trends and publication bias in ecology. Proc Biol Sci. (2004) 271:1961–6. doi: 10.1098/rspb.2004.2828
26. Woods BS, Hawkins N, Scott DA. Network meta-analysis on the log-hazard scale, combining count and hazard ratio statistics accounting for multi-arm trials: a tutorial. BMC Med Res Methodol. (2010) 10:54. doi: 10.1186/1471-2288-10-54
27. Deeks JH, Altman DG. Chapter 10: analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors, Cochrane Handbook for Systematic Reviews of Interventions version 60 2nd ed. Oxford: John Wiley & Sons Ltd. (2019).
28. Cochrane Handbook. Cochrane Handbook for Systematic Reviews of Interventions. Available online at: https://handbook/5/1.cochrane.org/chapter_10/10_4_3_1_recommendations_on_testing_for_funnel_plot_asymmetry.htm(accessed March 12, 2021).
29. GRADE. Grading of Recommendations Assessment, Development and Evaluation (Short GRADE) Working Group. (2000). Available online at: https://gdt.gradepro.org/app/handbook/handbook.html (accessed March 12, 2021).
30. Abnet CC, Qiao YL, Dawsey SM, Dong ZW, Taylor PR, Mark SD. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int J Epidemiol. (2005) 34:467–74. doi: 10.1093/ije/dyh375
31. Adolph M, Darnaud C, Thomas F, Pannier B, Danchin N, Batty GD, et al. Oral health in relation to all-cause mortality: the IPC cohort study. Sci Rep. (2017) 7:44604. doi: 10.1038/srep44604
32. Aida J, Kondo K, Yamamoto T, Hirai H, Nakade M, Osaka K, et al. Oral health and cancer, cardiovascular, and respiratory mortality of Japanese. J Dental Res. (2011) 90:1129–35. doi: 10.1177/0022034511414423
33. Ajwani S, Mattila KJ, Narhi TO, Tilvis RS, Ainamo A. Oral health status, C-reactive protein and mortality–a 10 year follow-up study. Gerodontology. (2003) 20:32–40. doi: 10.1111/j.1741-2358.2003.00032.x
34. Ajwani S, Mattila KJ, Tilvis RS, Ainamo A. Periodontal disease and mortality in an aged population. Spec Care Dentist. (2003) 23:125–30. doi: 10.1111/j.1754-4505.2003.tb00297.x
35. Ando A, Tanno K, Ohsawa M, Onoda T, Sakata K, Tanaka F, et al. Associations of number of teeth with risks for all-cause mortality and cause-specific mortality in middle-aged and elderly men in the northern part of Japan: the Iwate-KENCO study. Community Dent Oral Epidemiol. (2014) 42:358–65. doi: 10.1111/cdoe.12095
36. Ansai T, Takata Y, Soh I, Awano S, Yoshida A, Sonoki K, et al. Relationship between tooth loss and mortality in 80-year-old Japanese community-dwelling subjects. BMC Public Health. (2010) 10:386. doi: 10.1186/1471-2458-10-386
37. Batty GD, Jung KJ, Mok Y, Lee SJ, Back JH, Lee S, et al. Oral health and later coronary heart disease: cohort study of one million people. Eur J Prev Cardiol. (2018) 25:598–605. doi: 10.1177/2047487318759112
38. Brown DW. Complete edentulism prior to the age of 65 years is associated with all-cause mortality. J Public Health Dentistry. (2009) 69:260–6. doi: 10.1111/j.1752-7325.2009.00132.x
39. Cabrera C, Hakeberg M, Ahlqwist M, Wedel H, Bjorkelund C, Bengtsson C, et al. Can the relation between tooth loss and chronic disease be explained by socio-economic status? A 24-year follow-up from the population study of women in Gothenburg, Sweden. Eur J Epidemiol. (2005) 20:229–36. doi: 10.1007/s10654-004-5961-5
40. Caplan DJ, Ghazal TS, Cowen HJ, Oliveira DC. Dental status as a predictor of mortality among nursing facility residents in eastern Iowa. Gerodontology. (2017) 34:257–63. doi: 10.1111/ger.12260
41. Chang Y, Woo HG, Lee JS, Song TJ. Better oral hygiene is associated with lower risk of stroke. J Periodontol. (2020) 92:87–94. doi: 10.1002/JPER.20-0053
42. Chang Y, Woo HG, Park J, Lee JS, Song TJ. Improved oral hygiene care is associated with decreased risk of occurrence for atrial fibrillation and heart failure: a nationwide population-based cohort study. Eur J Prev Cardiol. 27:1835–45. doi: 10.1177/2047487319886018
43. Choe H, Kim YH, Park JW, Kim SY, Lee SY, Jee SH. Tooth loss, hypertension and risk for stroke in a Korean population. Atherosclerosis. (2009) 203:550–6. doi: 10.1016/j.atherosclerosis.2008.07.017
44. Darnaud C, Thomas F, Danchin N, Boutouyrie P, Bouchard P. Masticatory capacity and mortality: the preventive and clinical investigation center (IPC) cohort study. J Dental Res. (2020) 99:152–8. doi: 10.1177/0022034519889021
45. Del Brutto OH, Mera RM, Zambrano M, Del Brutto VJ. Severe edentulism is a major risk factor influencing stroke incidence in rural Ecuador (The Atahualpa Project). Int J Stroke. (2017) 12:201–4. doi: 10.1177/1747493016676621
46. Dewake N, Hashimoto H, Nonoyama T, Nonoyama K, Shimazaki Y. Posterior occluding pairs of teeth or dentures and 1-year mortality in nursing home residents in Japan. J Oral Rehabil. (2020) 47:204–11. doi: 10.1111/joor.12883
47. Dietrich T, Jimenez M, Krall Kaye EA, Vokonas PS, Garcia RI. Age-dependent associations between chronic periodontitis/edentulism and risk of coronary heart disease. Circulation. (2008) 117:1668–74. doi: 10.1161/CIRCULATIONAHA.107.711507
48. Fukai K, Takiguchi T, Ando Y, Aoyama H, Miyakawa Y, Ito G, et al. Mortality rates of community-residing adults with and without dentures. Geriatr Gerontol Int. (2008) 8:152–9. doi: 10.1111/j.1447-0594.2008.00464.x
49. Furuta M, Takeuchi K, Adachi M, Kinoshita T, Eshima N, Akifusa S, et al. Tooth loss, swallowing dysfunction and mortality in Japanese older adults receiving home care services. Geriatr Gerontol Int. (2018) 18:873–80. doi: 10.1111/ggi.13271
50. Garcia RI, Krall EA, Vokonas PS. Periodontal disease and mortality from all causes in the VA Dental Longitudinal Study. Ann Periodontol. (1998) 3:339–49. doi: 10.1902/annals.1998.3.1.339
51. Goto Y, Wada K, Uji T, Koda S, Mizuta F, Yamakawa M, et al. Number of teeth and all-cause and cancer mortality in a Japanese community: the takayama study. J Epidemiol. (2020) 30:213–8. doi: 10.2188/jea.JE20180243
52. Hamalainen P, Meurman JH, Keskinen M, Heikkinen E. Relationship between dental health and 10-year mortality in a cohort of community-dwelling elderly people. Eur J Oral Sci. (2003) 111:291–6. doi: 10.1034/j.1600-0722.2003.00055.x
53. Hayasaka K, Tomata Y, Aida J, Watanabe T, Kakizaki M, Tsuji I. Tooth loss and mortality in elderly Japanese adults: effect of oral care. J Am Geriatr Soc. (2013) 61:815–20. doi: 10.1111/jgs.12225
54. Heitmann BL, Gamborg M. Remaining teeth, cardiovascular morbidity and death among adult Danes. Prev Med. (2008) 47:156–60. doi: 10.1016/j.ypmed.2008.04.007
55. Hiratsuka T, Komiyama T, Ohi T, Tanji F, Tomata Y, Tsuji I, et al. Contribution of systemic inflammation and nutritional status to the relationship between tooth loss and mortality in a community-dwelling older Japanese population: a mediation analysis of data from the Tsurugaya project. Clin Oral Investig. (2020) 24:2071–7. doi: 10.1007/s00784-019-03072-y
56. Hirotomi T, Yoshihara A, Ogawa H, Miyazaki H. Number of teeth and 5-year mortality in an elderly population. Community Dent Oral Epidemiol. (2015) 43:226–31. doi: 10.1111/cdoe.12146
57. Hoke M, Schillinger T, Mlekusch W, Wagner O, Minar E, Schillinger M. The impact of dental disease on mortality in patients with asymptomatic carotid atherosclerosis. Swiss Med Wkly. (2011) 141:w13236. doi: 10.4414/smw.2011.13236
58. Holmlund A, Holm G, Lind L. Number of teeth as a predictor of cardiovascular mortality in a cohort of 7,674 subjects followed for 12 years. J Periodontol. (2010) 81:870–6. doi: 10.1902/jop.2010.090680
59. Holmlund A, Lampa E, Lind L. Oral health and cardiovascular disease risk in a cohort of periodontitis patients. Atherosclerosis. (2017) 262:101–6. doi: 10.1016/j.atherosclerosis.2017.05.009
60. Holm-Pedersen P, Schultz-Larsen K, Christiansen N, Avlund K. Tooth loss and subsequent disability and mortality in old age. J Am Geriatr Soc. (2008) 56:429–35. doi: 10.1111/j.1532-5415.2007.01602.x
61. Hu HY, Lee YL, Lin SY, Chou YC, Chung D, Huang N, et al. Association between tooth loss, body mass index, and all-cause mortality among elderly patients in Taiwan. Medicine. (2015) 94:e1543. doi: 10.1097/MD.0000000000001543
62. Hung HC, Joshipura KJ, Colditz G, Manson JE, Rimm EB, Speizer FE, et al. The association between tooth loss and coronary heart disease in men and women. J Public Health Dentistry. (2004) 64:209–15. doi: 10.1111/j.1752-7325.2004.tb02755.x
63. Hung HC, Willett W, Merchant A, Rosner BA, Ascherio A, Joshipura KJ. Oral health and peripheral arterial disease. Circulation. (2003) 107:1152–7. doi: 10.1161/01.CIR.0000051456.68470.C8
64. Iwasaki M, Sato M, Yoshihara A, Ansai T, Miyazaki H. Association between tooth loss and medical costs related to stroke in healthy older adults aged over 75 years in Japan. Geriatr Gerontol Int. (2017) 17:202–10. doi: 10.1111/ggi.12687
65. Janket SJ, Baird AE, Jones JA, Jackson EA, Surakka M, Tao W, et al. Number of teeth, C-reactive protein, fibrinogen and cardiovascular mortality: a 15-year follow-up study in a Finnish cohort. J Clin Periodontol. (2014) 41:131–40. doi: 10.1111/jcpe.12192
66. Janket SJ, Surakka M, Jones JA, Lam A, Schnell RA, Rose LM, et al. Removable dental prostheses and cardiovascular survival: a 15-year follow-up study. J Dent. (2013) 41:740–6. doi: 10.1016/j.jdent.2013.05.009
67. Joshipura KJ, Hung HC, Rimm EB, Willett WC, Ascherio A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke. (2003) 34:47–52. doi: 10.1161/01.STR.0000052974.79428.0C
68. Joshipura KJ, Rimm EB, Douglass CW, Trichopoulos D, Ascherio A, Willett WC. Poor oral health and coronary heart disease. J Dental Res. (1996) 75:1631–6. doi: 10.1177/00220345960750090301
69. Joshy G, Arora M, Korda RJ, Chalmers J, Banks E. Is poor oral health a risk marker for incident cardiovascular disease hospitalisation and all-cause mortality? Findings from 172 630 participants from the prospective 45 and Up Study. BMJ Open. (2016) 6:e012386. doi: 10.1136/bmjopen-2016-012386
70. Kebede TG, Holtfreter B, Kocher T, Meisel P, Dietrich T, Biffar R, et al. Association of periodontal destruction and diabetes with mortality. J Dental Res. (2017) 96:56–63. doi: 10.1177/0022034516668839
71. Kim JK, Baker LA, Davarian S, Crimmins E. Oral health problems and mortality. J Dent Sci. (2013) 8:11. doi: 10.1016/j.jds.2012.12.011
72. LaMonte MJ, Genco RJ, Hovey KM, Wallace RB, Freudenheim JL, Michaud DS, et al. History of periodontitis diagnosis and edentulism as predictors of cardiovascular disease, stroke, and mortality in postmenopausal women. J Am Heart Assoc. (2017) 6:4518. doi: 10.1161/JAHA.116.004518
73. Lee HJ, Choi EK, Park JB, Han KD, Oh S. Tooth loss predicts myocardial infarction, heart failure, stroke, and death. J Dental Res. (2019) 98:164–70. doi: 10.1177/0022034518814829
74. Li Q, Chalmers J, Czernichow S, Neal B, Taylor BA, Zoungas S, et al. Oral disease and subsequent cardiovascular disease in people with type 2 diabetes: a prospective cohort study based on the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified-Release Controlled Evaluation (ADVANCE) trial. Diabetologia. (2010) 53:2320–7. doi: 10.1007/s00125-010-1862-1
75. Liljestrand JM, Havulinna AS, Paju S, Mannisto S, Salomaa V, Pussinen PJ. Missing teeth predict incident cardiovascular events, diabetes, and death. J Dental Res. (2015) 94:1055–62. doi: 10.1177/0022034515586352
76. Matsuyama Y, Aida J, Watt RG, Tsuboya T, Koyama S, Sato Y, et al. Dental status and compression of life expectancy with disability. J Dental Res. (2017) 96:1006–13. doi: 10.1177/0022034517713166
77. Morita I, Nakagaki H, Kato K, Murakami T, Tsuboi S, Hayashizaki J, et al. Relationship between survival rates and numbers of natural teeth in an elderly Japanese population. Gerodontology. (2006) 23:214–8. doi: 10.1111/j.1741-2358.2006.00134.x
78. Morrison HI, Ellison LF, Taylor GW. Periodontal disease and risk of fatal coronary heart and cerebrovascular diseases. J Cardiovasc Risk. (1999) 6:7–11. doi: 10.1177/204748739900600102
79. Mucci LA, Hsieh CC, Williams PL, Arora M, Adami HO, de Faire U, et al. Do genetic factors explain the association between poor oral health and cardiovascular disease? A prospective study among Swedish twins. Am J Epidemiol. (2009) 170:615–21. doi: 10.1093/aje/kwp177
80. Munoz-Torres FJ, Mukamal KJ, Pai JK, Willett W, Joshipura KJ. Relationship between tooth loss and peripheral arterial disease among women. J Clin Periodontol. (2017) 44:989–95. doi: 10.1111/jcpe.12787
81. Noguchi S, Toyokawa S, Miyoshi Y, Suyama Y, Inoue K, Kobayashi Y. Five-year follow-up study of the association between periodontal disease and myocardial infarction among Japanese male workers: MY Health Up Study. J Public Health. (2015) 37:605–11. doi: 10.1093/pubmed/fdu076
82. Nomura Y, Kakuta E, Okada A, Otsuka R, Shimada M, Tomizawa Y, et al. Effects of self-assessed chewing ability, tooth loss and serum albumin on mortality in 80-year-old individuals: a 20-year follow-up study. BMC Oral Health. (2020) 20:122. doi: 10.1186/s12903-020-01113-7
83. Oluwagbemigun K, Dietrich T, Pischon N, Bergmann M, Boeing H. Association between number of teeth and chronic systemic diseases: a cohort study followed for 13 years. PLoS ONE. (2015) 10:e0123879. doi: 10.1371/journal.pone.0123879
84. Osterberg T, Carlsson GE, Sundh V, Mellstrom D. Number of teeth–a predictor of mortality in 70-year-old subjects. Community Dent Oral Epidemiol. (2008) 36:258–68. doi: 10.1111/j.1600-0528.2007.00413.x
85. Osterberg T, Carlsson GE, Sundh V, Steen B. Number of teeth–a predictor of mortality in the elderly? A population study in three Nordic localities. Acta Odontol Scand. (2007) 65:335–40. doi: 10.1080/00016350701739519
86. Padilha DM, Hilgert JB, Hugo FN, Bos AJ, Ferrucci L. Number of teeth and mortality risk in the Baltimore Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. (2008) 63:739–44. doi: 10.1093/gerona/63.7.739
87. Paganini-Hill A, White SC, Atchison KA. Dental health behaviors, dentition, and mortality in the elderly: the leisure world cohort study. J Aging Res. (2011) 2011:156061. doi: 10.4061/2011/156061
88. Park SY, Kim SH, Kang SH, Yoon CH, Lee HJ, Yun PY, et al. Improved oral hygiene care attenuates the cardiovascular risk of oral health disease: a population-based study from Korea. Eur Heart J. (2019) 40:1138–45. doi: 10.1093/eurheartj/ehy836
89. Qi L, Qian Y, Zhu F, Cao N, Lu H, Zhang L. Association between periodontal disease and tooth loss and mortality in an elderly Chinese population. Aging Clin Exp Res. (2020) 32:2375–82. doi: 10.1007/s40520-019-01446-6
90. Ragnarsson E, Eliasson ST, Gudnason V. Loss of teeth and coronary heart disease. Int J Prosthodont. (2004) 17:441–6.
91. Reichert S, Schlitt A, Beschow V, Lutze A, Lischewski S, Seifert T, et al. Use of floss/interdental brushes is associated with lower risk for new cardiovascular events among patients with coronary heart disease. J Periodontal Res. (2015) 50:180–8. doi: 10.1111/jre.12191
92. Reichert S, Schulz S, Benten AC, Lutze A, Seifert T, Schlitt M, et al. Periodontal conditions and incidence of new cardiovascular events among patients with coronary vascular disease. J Clin Periodontol. (2016) 43:918–25. doi: 10.1111/jcpe.12611
93. Saito M, Shimazaki Y, Nonoyama T, Tadokoro Y. Associations of number of teeth with medical costs and hospitalization duration in an older Japanese population. Geriatr Gerontol Int. (2019) 19:335–41. doi: 10.1111/ggi.13622
94. Schwahn C, Polzer I, Haring R, Dorr M, Wallaschofski H, Kocher T, et al. Missing, unreplaced teeth and risk of all-cause and cardiovascular mortality. Int J Cardiol. (2013) 167:1430–7. doi: 10.1016/j.ijcard.2012.04.061
95. Shimazaki Y, Soh I, Saito T, Yamashita Y, Koga T, Miyazaki H, et al. Influence of dentition status on physical disability, mental impairment, and mortality in institutionalized elderly people. J Dental Res. (2001) 80:340–5. doi: 10.1177/00220345010800010801
96. Soikkonen K, Wolf J, Salo T, Tilvis R. Radiographic periodontal attachment loss as an indicator of death risk in the elderly. J Clin Periodontol. (2000) 27:87–92. doi: 10.1034/j.1600-051x.2000.027002087.x
97. Tu YK, Galobardes B, Smith GD, McCarron P, Jeffreys M, Gilthorpe MS. Associations between tooth loss and mortality patterns in the Glasgow Alumni Cohort. Heart. (2007) 93:1098–103. doi: 10.1136/hrt.2006.097410
98. Tuominen R, Reunanen A, Paunio M, Paunio I, Aromaa A. Oral health indicators poorly predict coronary heart disease deaths. J Dental Res. (2003) 82:713–8. doi: 10.1177/154405910308200911
99. Vedin O, Hagstrom E, Ostlund O, Avezum A, Budaj A, Flather MD, et al. Associations between tooth loss and prognostic biomarkers and the risk for cardiovascular events in patients with stable coronary heart disease. Int J Cardiol. (2017) 245:271–6. doi: 10.1016/j.ijcard.2017.07.036
100. Vedin O, Hagstrom E, Budaj A, Denchev S, Harrington RA, Koenig W, et al. Tooth loss is independently associated with poor outcomes in stable coronary heart disease. Eur J Prev Cardiol. (2016) 23:839–46. doi: 10.1177/2047487315621978
101. Vogtmann E, Etemadi A, Kamangar F, Islami F, Roshandel G, Poustchi H, et al. Oral health and mortality in the Golestan Cohort Study. Int J Epidemiol. (2017) 46:2028–35. doi: 10.1093/ije/dyx056
102. Watt RG, Tsakos G, de Oliveira C, Hamer M. Tooth loss and cardiovascular disease mortality risk–results from the Scottish Health Survey. PLoS ONE. (2012) 7:e30797. doi: 10.1371/journal.pone.0030797
103. Wu T, Trevisan M, Genco RJ, Dorn JP, Falkner KL, Sempos CT. Periodontal disease and risk of cerebrovascular disease: the first national health and nutrition examination survey and its follow-up study. Arch Intern Med. (2000) 160:2749–55. doi: 10.1001/archinte.160.18.2749
104. Yuan JQ, Lv YB, Kraus VB, Gao X, Yin ZX, Chen HS, et al. Number of natural teeth, denture use and mortality in Chinese elderly: a population-based prospective cohort study. BMC Oral Health. (2020) 20:100. doi: 10.1186/s12903-020-01084-9
105. World Heart Federation. Cardiovascular Risk Factors. Available online at: https://www.world-heart-federation.org/resources/risk-factors (accessed March 12, 2021).
106. Everett BM, Pradhan AD, Solomon DH, Paynter N, MacFadyen J, Zaharris E, et al. Rationale and design of the Cardiovascular Inflammation Reduction Trial: a test of the inflammatory hypothesis of atherothrombosis. Am Heart J. (2013) 166:199–207.e15. doi: 10.1016/j.ahj.2013.03.018
107. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. (2017) 377:1119–31. doi: 10.1056/NEJMoa1707914
108. Teeuw WJ, Slot DE, Susanto H, Gerdes VE, Abbas F, D'Aiuto F, et al. Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J Clin Periodontol. (2014) 41:70–9. doi: 10.1111/jcpe.12171
109. Humphrey LL, Fu R, Buckley DI, Freeman M, Helfand M. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med. (2008) 23:2079–86. doi: 10.1007/s11606-008-0787-6
110. Hung HC, Colditz G, Joshipura KJ. The association between tooth loss and the self-reported intake of selected CVD-related nutrients and foods among US women. Community Dent Oral Epidemiol. (2005) 33:167–73. doi: 10.1111/j.1600-0528.2005.00200.x
111. Wakai K, Naito M, Naito T, Kojima M, Nakagaki H, Umemura O, et al. Tooth loss and intakes of nutrients and foods: a nationwide survey of Japanese dentists. Community Dent Oral Epidemiol. (2010) 38:43–9. doi: 10.1111/j.1600-0528.2009.00512.x
112. Anand SS, Hawkes C, de Souza RJ, Mente A, Dehghan M, Nugent R, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system: a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. (2015) 66:1590–614. doi: 10.1016/j.jacc.2015.07.050
113. Hujoel PP, Lingstrom P. Nutrition, dental caries and periodontal disease: a narrative review. J Clin Periodontol. (2017) 44(Suppl.18):S79–84. doi: 10.1111/jcpe.12672
114. Shiga Y, Nezu T, Hosomi N, Aoki S, Nishi H, Naito H, et al. Effect of tooth loss and nutritional status on outcomes after ischemic stroke. Nutrition. (2020) 71:110606. doi: 10.1016/j.nut.2019.110606
115. Nakahori N, Sekine M, Yamada M, Tatsuse T, Kido H, Suzuki M. Socioeconomic status and remaining teeth in Japan: results from the Toyama dementia survey. BMC Public Health. (2019) 19:691. doi: 10.1186/s12889-019-7068-7
116. Wennstrom A, Ahlqwist M, Stenman U, Bjorkelund C, Hakeberg M. Trends in tooth loss in relation to socio-economic status among Swedish women, aged 38 and 50 years: repeated cross-sectional surveys 1968–2004. BMC Oral Health. (2013) 13:63. doi: 10.1186/1472-6831-13-63
117. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. (2018) 137:2166–78. doi: 10.1161/CIRCULATIONAHA.117.029652
118. Ueno M, Yanagisawa T, Shinada K, Ohara S, Kawaguchi Y. Masticatory ability and functional tooth units in Japanese adults. J Oral Rehabil. (2008) 35:337–44. doi: 10.1111/j.1365-2842.2008.01847.x
119. Dettori JR. Loss to follow-up. Evid Based Spine Care J. (2011) 2:7–10. doi: 10.1055/s-0030-1267080
120. Sackett DL. Evidence-based medicine. Semin Perinatol. (1997) 21:3–5. doi: 10.1016/S0146-0005(97)80013-4
Keywords: systematic review, meta-analysis, number of teeth, tooth loss, atherosclerosis, cardiovascular disease, mortality, risk
Citation: Beukers NGFM, Su N, Loos BG and van der Heijden GJMG (2021) Lower Number of Teeth Is Related to Higher Risks for ACVD and Death—Systematic Review and Meta-Analyses of Survival Data. Front. Cardiovasc. Med. 8:621626. doi: 10.3389/fcvm.2021.621626
Received: 26 October 2020; Accepted: 22 March 2021;
Published: 07 May 2021.
Edited by:
Hack-Lyoung Kim, Seoul Metropolitan Government - Seoul National University Boramae Medical Center, South KoreaReviewed by:
Takamasa Komiyama, Tohoku University, JapanCopyright © 2021 Beukers, Su, Loos and van der Heijden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicky G. F. M. Beukers, bi5nLmYubS5iZXVrZXJzQGFjdGEubmw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.