- 1Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, United States
- 2Department of Medicine, Indiana University School of Medicine, Indianapolis, IN, United States
- 3Division of Pediatric Cardiology, Department of Pediatric and Adolescent Medicine, Mayo Clinic, Rochester, MN, United States
- 4Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN, United States
Introduction: Cardiac papillary fibroelastomas (PFEs) are the most common primary benign cardiac tumors, although they are somewhat unusual in children and typically seen on the left-sided cardiac valves.
Case summary: A 10-week-old patient was found to have a partial atrioventricular canal defect, with associated tricuspid and mitral regurgitation. He was medically managed until 1 year of age, when surgical correction was done. During the procedure, a PFE was found incidentally on the TV.
Conclusion: This is one of the youngest patients to be reported with PFE, thus adding to the literature of these unusual cases in children.
Introduction
Cardiac papillary fibroelastomas (PFEs) are the most common primary benign tumors of the heart (1). Histologically, they consist of avascular fibroelastic tissue surrounded by endocardium (1). While not malignant in the classical sense, they have a clinical importance since they may be a source of systemic embolization due to embolization of either the tumor or adherent surface thrombus (2, 3). Symptoms are frequently the sequelae of embolization and can include angina, shortness of breath, and symptoms of stroke/transient ischemic attack (1–3).
Their etiology is still unknown, though several theories were proposed. Given their propensity to arise on damaged endocardium, it is possible that this injury can result in their formation. In this report, we describe a case of a PFE arising on the tricuspid valve (TV) in a 1-year-old born with congenital heart disease.
Case Report
A previously healthy prematurely-born (36 4/7 weeks) male presented to his pediatrician at 1-week of age for regular follow up. The pediatrician realized a soft 2/6 systolic murmur with a fixed split. An echocardiogram showed both a partial atrioventricular (AV) canal defect, consisting of a primum atrial septal defect (ASD), and cleft mitral valve (MV). The patient was maintained on medical management (diuretics) and supplemental oxygen for episodic cyanotic spells. At 13 months of age, episodes of persistent cyanosis and respiratory distress occurred, which on work-up revealed pulmonary hypertension. He was then transferred to our institution for definitive surgical correction of his congenital disease.
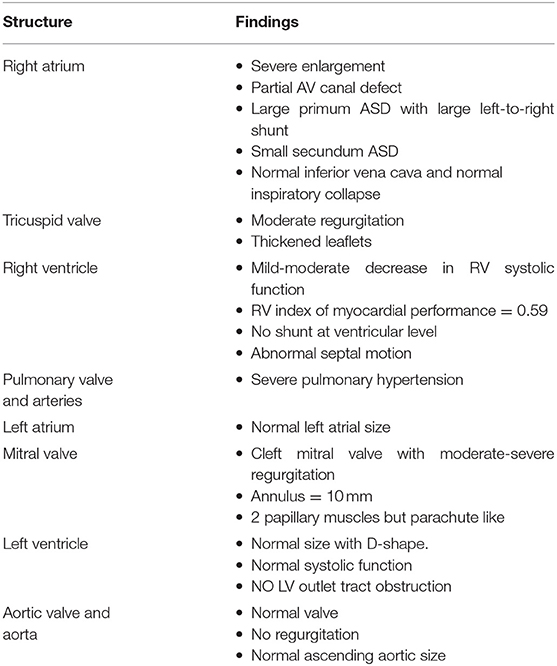
On admission, the patient was fussy and diaphoretic. Physical exam revealed a grade 3/6 systolic ejection murmur at the upper left sternal border and grade 3/6 diastolic rumble at the left lower sternal border. Chest Xray revealed cardiomegaly, prominent aortic nob and increased pulmonary vascular markings. A detailed preoperative congenital transthoracic echocardiogram reported, in addition to the partial AV canal defect, a thickened MV with moderate-severe regurgitation (Figure 1A, Supplementary Videos 1, 2). Further examination of the MV revealed mild mitral hypoplasia. Left ventricular size and function (ejection fraction = 77%) were normal. The aortic valve was normal. In addition, severe pulmonary hypertension (systolic pulmonary artery pressure = 72 mm Hg) with severe right ventricular and right atrial enlargement with subsequent decrease in right systolic function were noted. Furthermore, thickened TV leaflets with moderate regurgitation was seen, especially during the Intra-Op transesophageal echocardiography (Figure 1B). Detailed findings of the echocardiogram can be found in Table 1. During surgery, a large primum defect and a small secundum defect separated by a muscle bar were noted. The anterior mitral leaflet appeared dysplastic on either side of the cleft with a parachute configuration. The surgeon then partially sutured the mitral cleft and performed commissuroplasty. There was residual mild mitral regurgitation after repair and surgeon could not further intervene on the valve because of concerns that it would make it stenotic. The tricuspid valve was dilated, and a mass was noted. Tricuspid annuloplasty and excision of the mass was done. Finally, the surgeon was able to patch the atrial septal defect (Supplementary Video 3). A 3-mm punch was places in the atrial septal patch given the pulmonary hypertension.
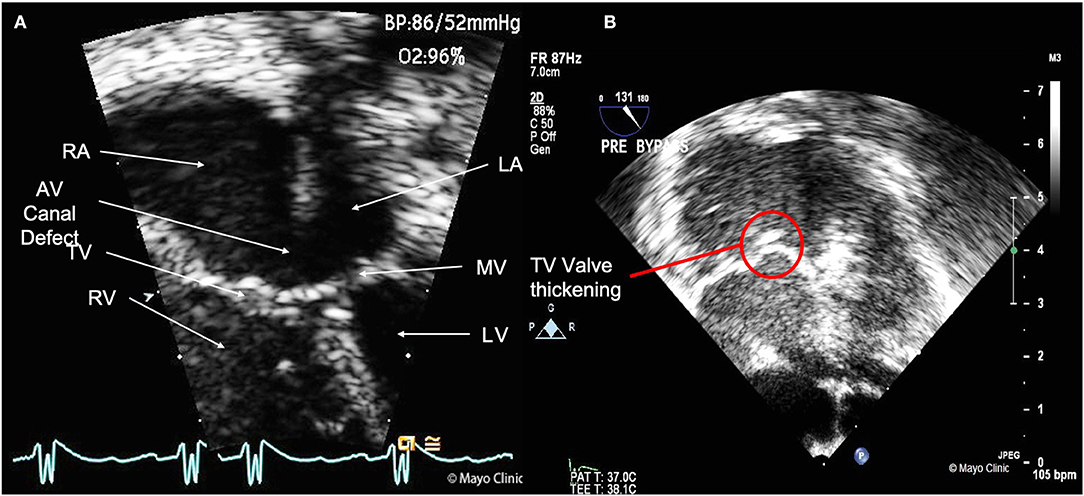
Figure 1. (A) Transthoracic echocardiography image showing the 4 cardiac chambers (RA, Right atrium; RV, Right ventricle; LA, left atrium; LV, Left ventricle), mitral valve (MV), tricuspid valve (TV), and the partial AV canal defect. (B) Intra-Op transesophageal echocardiography image, with view of the thickened TV.
Gross inspection of the TV tissue revealed a 0.7 × 0.2 × 0.2 cm mass that appeared as a portion of pedunculated tan tissue with minute papillary projects. Gross and light microscopic examination confirmed the diagnosis of PFE (Figure 2). Molecular analysis of the specimen did not reveal a KRAS mutation on targeted amplification.
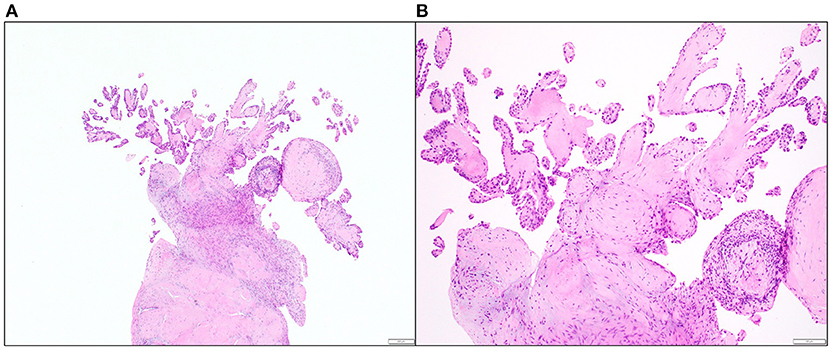
Figure 2. Excised papillary fibroelastoma of a TV leaflet on light microscopic examination (A) 40x original magnification, and (B) 100x magnification (hematoxylin and eosin stain).
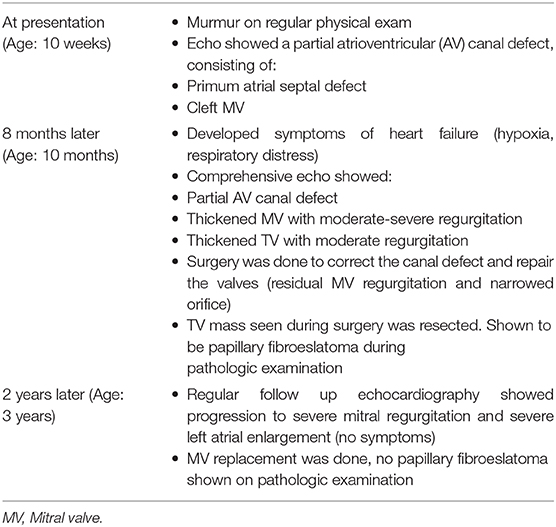
The patient had close follow up with regular echocardiograms until 3 years of age. The patient reported no symptoms other than occasional fatigue. Due to severe residual mitral regurgitation, with severe left atrial enlargement (Left atrial volume index = 90 ml/m2), he then underwent MV replacement with a mechanical valve. The MV salvaged was found to be dysplastic on pathologic examination, however no PFE was found. Table 2 summarizes the clinical presentation, management and follow up of the patient.
Discussion
PFEs are now considered the most common primary cardiac tumor found in the general population (3). The etiology of PFE is not well-established. Multiple theories exist, including the acquired and congenital theories. Not uncommonly, PFEs arising on damaged endocardial surfaces. This postulate is strengthened by multiple observations of PFEs arising on damaged valve. It is also not uncommon in adults for the PFE to be identified in the OR by the surgeon or by intraoperative echocardiography (20%) (3). This highlights the necessity of surgeons and echocardiographers to have a high level of vigilance in patients with underlying endocardial pathology for the possibility of PFE.
Furthermore, most reports in children are in association with congenital heart disease, in which there is abnormal flow and, hence, endocardial injury (4, 5). Two prior cases reported PFE in trisomic patients with cardiac anomalies, although our patient did not have a known chromosomal abnormality (4, 5). More recently, cases of PFE that harbor mutations in the oncogenic driver gene KRAS raise the possibility of a subset of these being truly neoplastic – possibly resulting from clonal expansion (possibly after injury) (6). This would essentially suggest the possibility of a complex interplay between environmental factors that potentially result in a genetically driven process.
Conclusion
This is one of the youngest patients reported in the literature to have a papillary fibroelastoma confirmed by pathology, thus expanding the descriptive spectrum of patients affected by this condition.
Data Availability Statement
The original contributions generated for the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
All authors contributed to the writing and revision of the manuscript.
Funding
This work was supported by the Mayo Foundation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2020.624219/full#supplementary-material
Supplementary Video 1. Transthoracic echocardiography view of the AV canal defect area. The tricuspid and mitral valves are also visible.
Supplementary Video 2. Transthoracic echocardiography (with Doppler) showing communication through the canal defect and severe mitral and tricuspid regurgitation.
Supplementary Video 3. Post repair transesophageal view of the repaired septal defect.
Abbreviations
ASD, Atrial septal defect; AV, Atrio-ventricular; AV, Aortic valve; MV, Mitral valve; PFE, Papillary fibroelastoma; TV, Tricuspid valve.
References
1. Maleszewski JJ, Bois MC, Bois JP, Young PM, Stulak JM, Klarich KW. Neoplasia and the heart: pathological review of effects with clinical and radiological correlation. J Am Coll Cardiol. (2018) 72:202–27. doi: 10.1016/j.jacc.2018.05026
2. Sun JP, Asher CR, Yang XS, Cheng GG, Scalia GM, Massed AG, et al. Clinical and echocardiographic characteristics of papillary fibroelastomas: a retrospective and prospective study in 162 patients. Circulation. (2001) 103:2687–93. doi: 10.1161/01.CIR.103.222687
3. Tamin SS, Maleszewski JJ, Scott CG, Khan SK, Edwards WD, Bruce CJ, et al. Prognostic and bioepidemiologic implications of papillary fibroelastomas. J Am Coll Cardiol. (2015) 65:2420–9. doi: 10.1016/j.jacc.2015.03569
4. Anderson KR, Fiddler GI, Lie JT. Congenital papillary tumor of the tricuspid valve. An unusual cause of right ventricular outflow obstruction in a neonate with trisomy E. Mayo Clin Proc. (1977) 52:665–9.
5. Okada K, Masuoka A, Hotoda K, Uno Y, Suzuki T. A rare case of pediatric primary cardiac tumor in a patient with Down syndrome. Asian Cardiovasc Thorac Ann. (2017) 25:630–2. doi: 10.1177/0218492317721788
Keywords: papillary fibroelastoma, cardiac tumor, congenital heart disease, pediatrics, case report
Citation: Ahmad A, El-Am EA, Kurmann RD, Hagler DJ, Bois MC, Maleszewski JJ and Klarich KW (2021) Case Report: A Rare Case of Right-Sided Papillary Fibroelastoma in a 1-Year-Old With Congenital Heart Disease. Front. Cardiovasc. Med. 7:624219. doi: 10.3389/fcvm.2020.624219
Received: 30 October 2020; Accepted: 31 December 2020;
Published: 27 January 2021.
Edited by:
Giovanni Battista Luciani, University of Verona, ItalyReviewed by:
Jochen Grohmann, University of Freiburg Medical Center, GermanyMadhusudan Ganigara, Donald and Barbara Zucker School of Medicine at Hofstra-Northwell, United States
Stiljan Hoxha, University of Verona, Italy
Copyright © 2021 Ahmad, El-Am, Kurmann, Hagler, Bois, Maleszewski and Klarich. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kyle W. Klarich, a2xhcmljaC5reWxlQG1heW8uZWR1
 Ali Ahmad
Ali Ahmad Edward A. El-Am
Edward A. El-Am Reto D. Kurmann1
Reto D. Kurmann1