- 1Division of Cardiovascular Medicine, Department of Internal Medicine, Kurume University School of Medicine, Kurume, Japan
- 2Department of Community Medicine, Kurume University School of Medicine, Kurume, Japan
Accumulation of visceral fat leads to metabolic syndrome and increases risks of cerebro-cardiovascular diseases, which should be recognized and improved at the early stage in general population. Accurate measurement of visceral fat area (VFA) is commonly performed by the abdominal cross-sectional image measured by computed tomography scan, which is, however, limited due to the radiation exposure. The bioelectrical impedance analysis (OMRON, HDS-2000 DUALSCANR) has been recently developed to measure VFA, which is more easily accessible modality. In the present study, we investigated the clinical usefulness of DUALSCANR in 226 subjects who received health examination, including blood chemistries, electrocardiography, cardio, and carotid ultrasonography. VFA was measured within only just 5 min. Average of VFA was 83.5 ± 36.3 cm2 in men, and 64.8 ± 28.0 cm2 in women, which was correlated to weight (r = 0.7404, p < 0.0001), body mass index (BMI) (r = 0.7320, p < 0.0001), and waist circumstance (r = 0.7393, p < 0.0001). In multivariate analyses, VFA was significantly associated with weight (p < 0.0001), BMI (p < 0.0001), and waist circumstance (p < 0.0001). Compared to the group of smaller waist and normal BMI, VFA was significantly increased (p < 0.0001) in the group of larger waist and obese subjects. In conclusion, these results indicated that DUALSCANR is useful to measure VFA easily in general population, even in a large number of subjects.
Introduction
Obesity has been rapidly increasing over the last decades all over the world (1), which is a serious concern and should be recognized and improved at the early stage in general population, especially in the aspects of the increased risk of cardiovascular diseases as primary prevention (2). It is simple for obesity assessment to measure body mass index (BMI), waist circumference, or waist-to-hip ratio. However, it is clinically important to distinguish visceral from subcutaneous adipose tissues by using imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT) scan (3, 4), because visceral fat accumulation was found to be specifically associated with the metabolic alterations of obesity, both in men and women (5). Serial-slice CT is able to evaluate the visceral adipose tissue (VAT) in detail (6). Dual-energy X-ray absorptiometry (DEXA) is usually used to measure total body fat, which has been also used to measure central abdominal fat (7). It has been reported that visceral fat measured by CT scan has a strong correlation with central abdominal fat measured by DEXA (7–14).
However, these methods are limited in the clinical use, due to the radiation exposure and the cost of techniques, which is not suitable to general health checkup examination. Where more easily accessible modality at lower cost should be developed, the bioelectrical impedance analysis (BIA) has been recently developed, which is used in population and clinical studies as a technique to estimate body composition (15–19). Unno and colleagues (15) found that VFA estimated by BIA is useful for detection of metabolic syndrome (MetS), as consistently reported by other studies (16–20).
Therefore, in the present study, we aimed to examine whether the new method of BIA is useful to measure VFA in Japanese general population.
Subjects and Methods
Study Population
A total of 226 subjects (87 males and 139 females: aged 40–90 years) received a population-based health examination in Uku town, a fishing community in southwestern Japan in 2011. This town is an isolated island in Sasebo city, located in Nagasaki prefecture, and the total population is about 3,700. A detailed content of the recent survey in the same district was previously described (21, 22).
Data Collection
Height and weight were measured, and BMI was calculated as weight (kilograms) divided by the square of height (square meters) as an index of the presence or absence of obesity. Waist circumference was measured at the level of the umbilicus in a standing position. Blood pressure (BP) was measured twice with the subjects in the sitting (first) and supine (second) position. Vigorous physical activity and smoking were avoided for at least 30 min before BP measurements. The second BP with the fifth phase diastolic pressure was used for analysis.
Blood was drawn from the antecubital vein for determinations of lipids profiles [total cholesterol, high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), and triglycerides], creatinine, uric acid (UA), fasting plasma glucose (FPG), glycated hemoglobin A1c [HbA1c(NGSP)], and high-sensitivity C-reactive protein (hs-CRP) in the morning after a 12-h fast. Fasting blood samples were centrifuged within 1 h after the collection. Estimated glomerular filtration rate (eGFR) was calculated using the modification of diet in renal disease (MDRD) study equation modified with a Japanese coefficient (23).
All subjects underwent the new abdominal BIA method (OMRON, HDS-2000 DUALSCANR) to estimate VFA in the morning after a 12-h fast. The voltage occurring at the flank to the flow of current between the umbilicus and the back correlates significantly with VFA and is unaffected by subcutaneous fat area. The voltage becomes larger as VFA even in the subjects with the same waist circumference because the electric resistance of intra-abdominal fat is greater than that of fat-free mass, and the density of the equipotential lines between two electrodes becomes denser. Using this method, we measured VFA of individuals within 5 min.
C-IMT of the common carotid artery was determined by using duplex ultrasonography (Sonosite “TITAN,” ALOKA) with a 10-MHz transducer in the supine position. Longitudinal B-mode images at the diastolic phase of the cardiac cycle were recorded by a single trained technician who was blinded to the subjects’ background. We measured the only far site of the wall of c-IMT. The images were magnified and measured on the screen and printed with a high-resolution line recorder (LSR-100A, Toshiba). We measured c-IMT according to the originally described method published in Circulation (24). Briefly, the c-IMT defined by Pignoli et al. (24) was measured as the distance from the leading edge of the first echogenic line to the leading edge of the second echogenic line. The first line represented the lumen–intimal interface; the collagen-containing upper layer of the tunica adventitia formed the second line. At each longitudinal projection, the site of the greatest thickness, including plaque, was sought along the arterial walls nearest and farthest from the skin from the common carotid artery to the internal carotid artery. Three determinations of c-IMT of one artery were conducted at the site of the greatest thickness and at two other points, 1 cm upstream and 1 cm downstream from this site. The averaged value among the six IMTs (three from the left and three from the right) was used as the representative value for each individual.
This study was approved by the mayor, by the welfare department of Uku town, and by the Research Ethics Committee of the Kurume University School of Medicine (Process numbers 2284), approved the study in conformity with the principles embodied in the declaration of Helsinki. All participants were informed about research procedures and risks before signing an informed consent.
Statistical Analysis
Results were presented as means ± SDs. Because of skewed distributions, natural logarithmic (ln) transformations were performed for triglycerides and hs-CRP. Log-transformed values were reconverted to antilogarithm forms in the tables. The medications for hypertension, dyslipidemia, and diabetes mellitus were coded as dummy variables. Gender, smoking habits, and alcohol intake were also coded as dummy variables. First, we performed univariate analysis for VFA levels as dependent variable. Second, multivariate analysis after adjustments for age and sex was performed for correlates of VFA levels. Finally, comparisons of various parameters between VFA levels (VFA < 100 cm2 vs. VFA ≥ 100 cm2) was performed. Statistical significance was defined as p < 0.05. All statistical analyses were performed using the SAS system (Release 9.3, SAS Institute, Cary, NC, USA).
Results
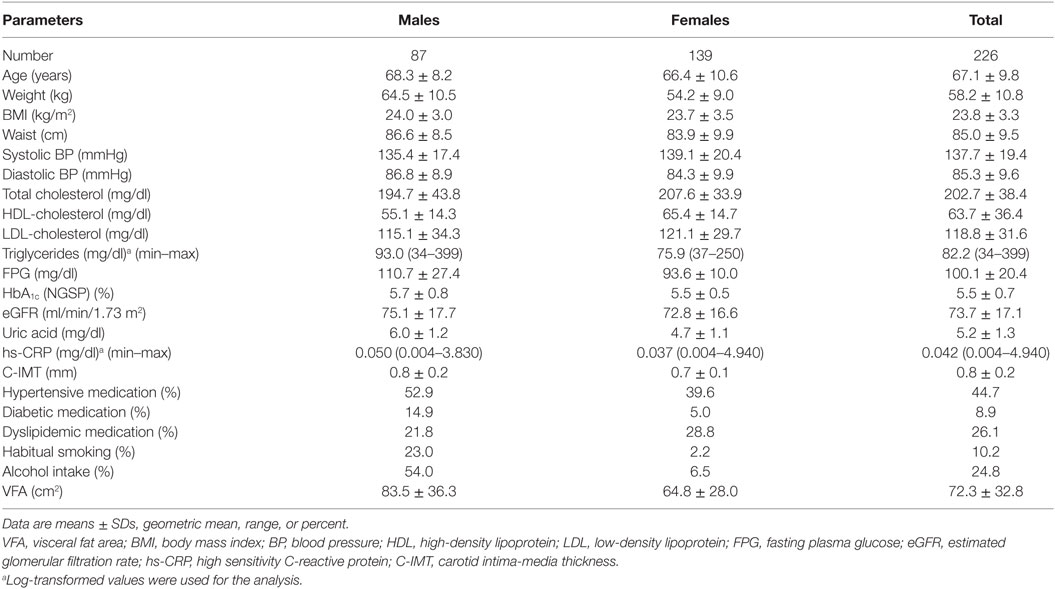
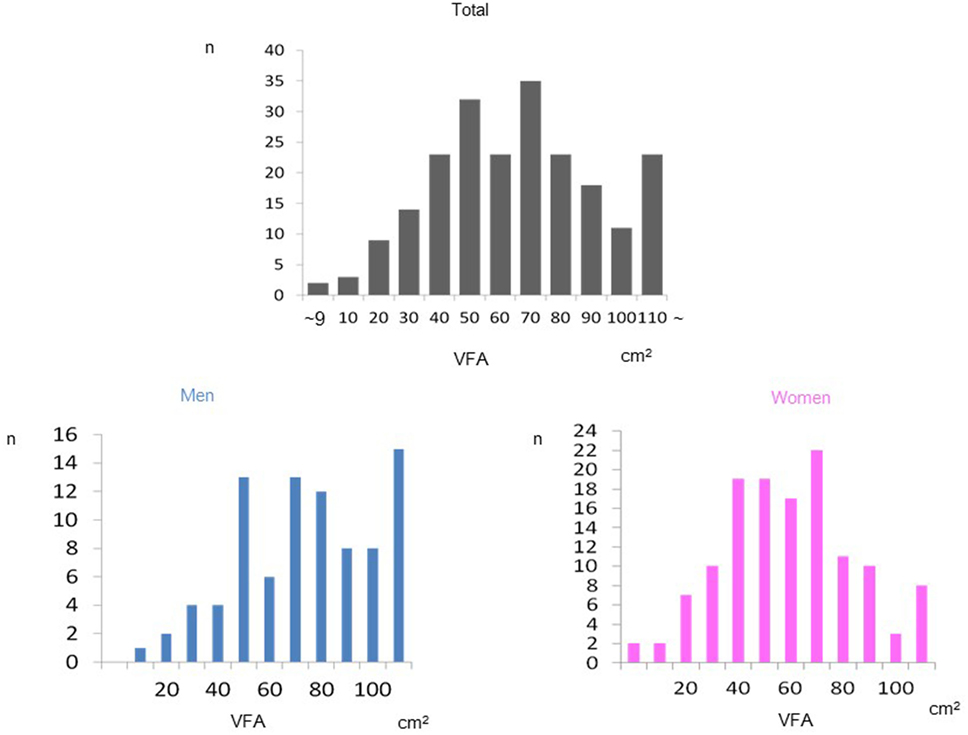
Demographic and clinical characteristics of the enrolled study subjects are presented in Table 1. Mean values of VFA were 83.5 cm2 in men and 64.8 cm2 in women, respectively, indicating that most of the subjects were non-obese. Mean VFA values of most subjects were within normal range. The prevalence of VFA in total and both genders was shown in Figure 1. VFA levels had a normal distribution in both genders. The association between VFA values and waist, weight, and BMI were demonstrated in Figure 2. Strong association between VFA and waist (r = 0.739, p < 0.0001), VFA and weight (r = 0.740, p < 0.0001), and VFA and BMI (r = 0.732, p < 0.0001) were observed.
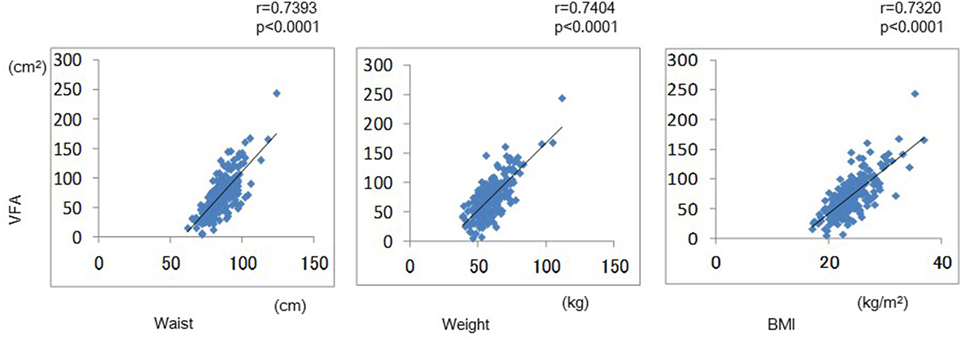
Figure 2. The correlation between VFA values and waist, weight, and body mass index were demonstrated.
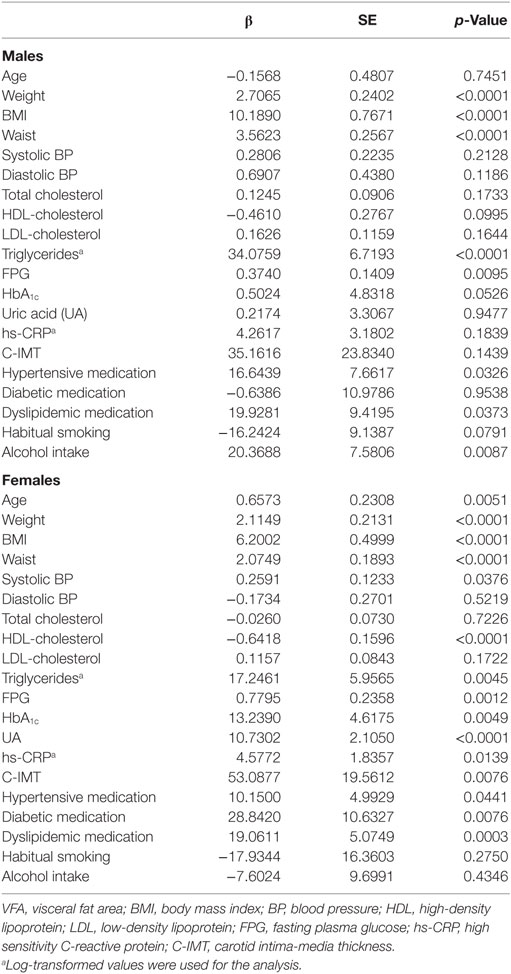
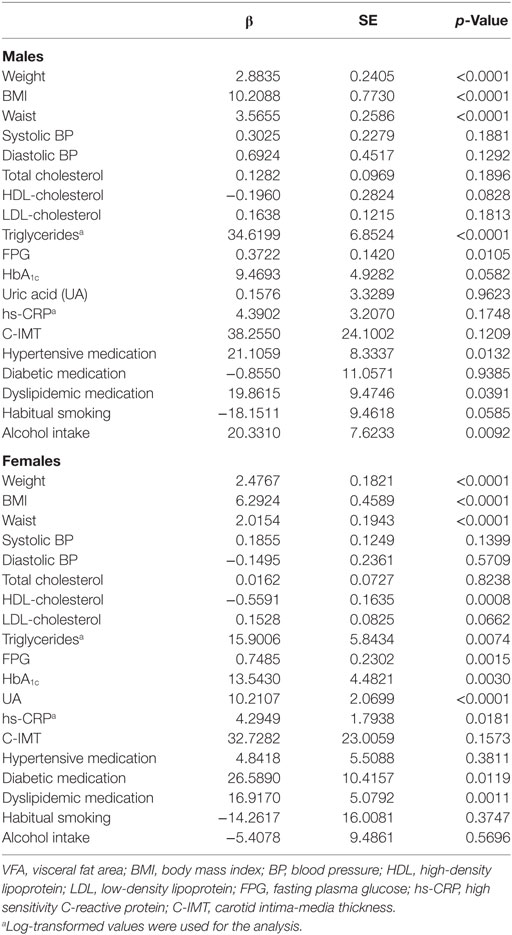
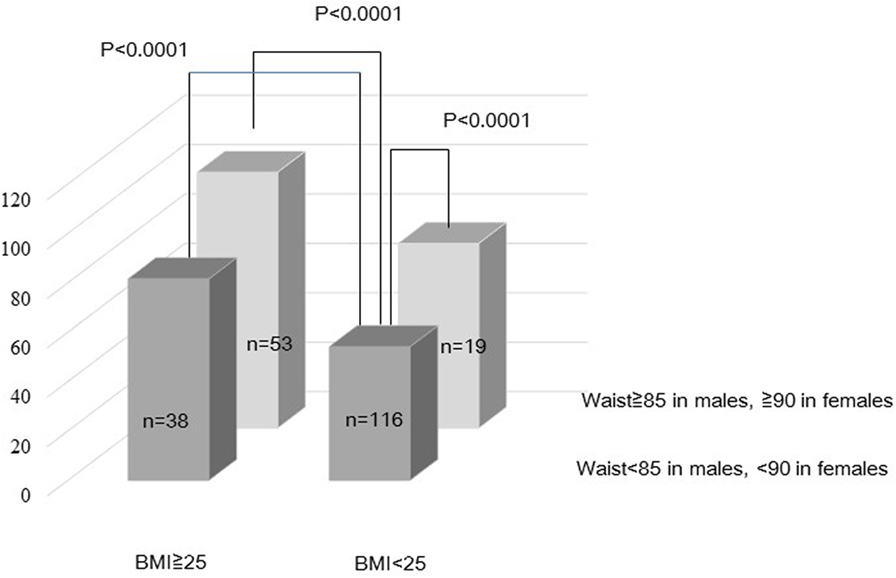
Univariate analysis for VFA levels as dependent variable stratified by gender was shown in Table 2. Weight (p < 0.0001), BMI (p < 0.0001), waist (p < 0.0001), triglycerides (p < 0.0001), FPG (p < 0.01), hypertensive medication (p < 0.05), dyslipidemic medication (p < 0.05), and alcohol intake (p < 0.01) were significantly associated with VFA areas in males. Age (p < 0.01), weight (p < 0.0001), BMI (p < 0.0001), waist (p < 0.0001), systolic BP (p < 0.05), HDL-c (p < 0.0001; inversely), triglycerides (p < 0.01), FPG (p < 0.01), HbA1c (p < 0.01), UA (p < 0.0001), hs-CRP (p < 0.05), c-IMT (p < 0.01), hypertensive medication (p < 0.05), diabetic medication (p < 0.01), and dyslipidemic medication (p < 0.001) were significantly associated with VFA areas in females. Table 3 shows the multivariate analysis adjusted for age for VFA levels as dependent variable. Weight (p < 0.0001), BMI (p < 0.0001), waist (p < 0.0001), triglycerides (p < 0.0001), FPG (p < 0.05), hypertensive medication (p < 0.05), dyslipidemic medication (p < 0.05), and alcohol intake (p < 0.01) in males. Weight (p < 0.0001), BMI (p < 0.0001), waist (p < 0.0001), HDL-c (p < 0.001; inversely), triglycerides (p < 0.01), FPG (p < 0.01), HbA1c (p < 0.01), UA (p < 0.0001), hs-CRP (p < 0.05), diabetic medication (p < 0.05), and dyslipidemic medication (p < 0.01) were significantly associated with VFA areas in females. In multivariate analysis for VFA levels after adjustment for age, sex, and medications for hypertension, diabetes, and dyslipidemia, the significance of weight (p < 0.0001), BMI (p < 0.0001), and waist (p < 0.0001) in both genders were still remained. In order to investigate the impacts of waist and BMI on VFA, we create the hierarchical model stratified two groups of waist and BMI adjustment for age and sex (Figure 3). Compared to the group of smaller waist and normal BMI, VFA was significantly increased (p < 0.0001) in the group of larger waist and obese subjects.
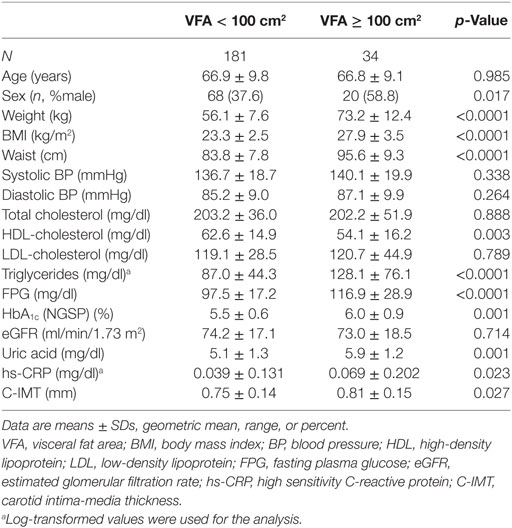
Comparison between various parameters stratified by VFA (<100 vs. ≧100 cm2) was demonstrated in Table 4. Male gender (p < 0.05), weight (p < 0.0001), BMI (p < 0.0001), waist (p < 0.0001), HDL-c (p < 0.05; inversely), triglycerides (p < 0.0001), FPG (p < 0.0001), HbA1c (p < 0.01), UA (p < 0.01), hs-CRP (p < 0.05), and c-IMT (p < 0.05) were significantly associated with elevated VFA areas (≧100 cm2).
To compare the usefulness between VFA and BMI, we performed the multiple stepwise regression analysis. Then, we found that triglycerides (p < 0.0001), FPG (p = 0.0002), and HDL-c (p = 0.0144; inversely) were independently related to VFA (R2 = 0.2698), whereas; FPG (p = 0.0001), HDL-c (p < 0.0049; inversely), and age (p = 0.0262) were independently related to BMI (R2 = 0.1375), suggesting that VFA is stronger statistical power to find out not only obese subjects but also subjects with accumulation of visceral fat than BMI.
Discussion
The adipocytokines secreted by excessive VFA are closely linked with metabolic disorders, such as type 2 diabetes, hypertension, and dyslipidemia, which develop various metabolic and cardiovascular disorders during several decades (25). Therefore, it is important for each individual in general population to recognize VFA for the primary prevention of cerebro-cardiovascular diseases in health checkup examinations, which should be simple and at low cost. In the present study, we have indicated that the VFA measurement by a new BIA method is useful and suitable to general population in the evaluation of adiposity of individuals. Conventional BIA approaches have estimated total fat content but not regional fat distribution (26, 27). Compared to the new method, waist circumference underestimates visceral fat amount because of the accumulation of abdominal subcutaneous fat (28–30). From the results of hierarchical multiple regression, our data may propose that the usefulness of VFA by DUALSCAN shows its superiority over waist and BMI in this study setting. In the multiple stepwise regression analysis, VFA is stronger statistical power to find out not only obese subjects but also subjects with accumulation of visceral fat than BMI. The abdominal dual BIA method of the DUALACAN seemed to measure VFA more precisely with less influence of subcutaneous fat area compared with the conventional whole-body BIA method (31). Because VSA measurement using the DUALSCAN showed a closer correlation with metabolic variables than whole-body BIA method in a health checkup examination, the device was approved as medical device by Health, Labour, and Welfare Ministry since 2011 in Japan (32). Moreover, the evaluation of VFA by the BIA is really a simple and easily accessible device even in a health checkup examination in Japanese general population.
Comparisons between DEXA or abdominal CT and BIA have been already performed in healthy adults (33, 34) and overweight individuals (35). Estimated VFA by BIA was accurate and accessible device is also admitted in obese patients (36, 37). On the contrary, some reports have indicated that the validity, reliability, and accuracy of BIA were not satisfied (38, 39). Although we did not examine the validity and accuracy of BIA, Japanese investigators (40, 41) reported the strong correlations between VFA by abdominal CT and VFA by BIA (r = 0.88, p < 0.001), between VFA by X-ray CT and VFA by BIA (r = 0.89, p < 0.001). BIA also has favorable effects on evaluation of skeletal muscle mass (42) and on assessing fat-free mass (43). We consider that VFA measurement by this technique can be enough as a screening to recognize the accumulation of visceral fat, which leads to MetS and increases risks of cerebro-cardiovascular diseases.
VFA levels are significantly associated with metabolic factors such as waist circumference FPG, and triglycerides. These significant associations are remained after adjustment for age and sex. The significance of hs-CRP with VFA deserves consideration. Report from Turkey (44) is consistent with ours. One mechanism for the elevation of hs-CRP in obese individuals might be associated with a high production of cytokines such as IL-6 and TNF-α by the excess adipose tissue, which would induce higher hs-CRP production by the liver (45).
The present study has several limitations. First, this study was cross-sectional with comparatively a small number of subjects. Prospective studies with a large number are needed to investigate the evaluation of role of BIA. Second, our population was relatively healthy, and most of them had BMI within normal limits. Thus, it is necessary to investigate the role of BIA in heterogeneous populations. Third, we do not have the data on the potential bias caused by metabolic factors such as medication and possibility of having edematous diseases. Fourth, although this study was performed in the typical fishing area in Japan, the background of these subjects may be a little different from those of other Japanese people. Fifth, we did not distinguish a clinical importance of VSA from SFA and also did not append the relationship between the SFA and other variables because we did not have data on SFA levels. Finally, we were not able to compare DUALSCAN and CT in the enrolled subjects, because we have no CT scan data.
In conclusion, our results may suggest that a new simple measurement system of visceral fat accumulation by BIA is useful to measure VFA even in a health checkup examination in a general population.
Author Contributions
ME: conception and design of the study, drafting of the article, and critical revision of the article for important intellectual content. HA: conception and design of the study, drafting of the article. AF: analysis and interpretation of data, EK: analysis and interpretation of data, SN, YN, SK, EN, NM, TT, and AS: collection and assembly of data. YF: final approval of the article.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was supported in part by the Kimura Memorial Heart Foundation, Fukuoka, and by a Grant-in-Aid for Scientific Research (C), from the Ministry of Education, Culture, Sports, Science and Technology, Japan. We are grateful to the elected officials and residents of Uku town, and the team of physicians in Department of Internal Medicine, Division of Cardiovascular Medicine, Kurume University School of Medicine for their help in performing the health examinations.
References
1. Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet (2011) 377:557–67. doi:10.1016/S0140-6736(10)62037-5
2. Aune D, Sen A, Norat T, Janszky I, Romundstad P, Tonstad S, et al. Body mass index, abdominal fatness, and heart failure incidence and mortality: a systematic review and dose-response meta-analysis of prospective studies. Circulation (2016) 133:639–49. doi:10.1161/CIRCULATIONAHA.115.016801
3. Kodama N, Tahara N, Tahara A, Honda A, Nitta Y, Mizoguchi M, et al. Effects of pioglitazone on visceral fat metabolic activity in impaired glucose tolerance or type 2 diabetes mellitus. J Clin Endocrinol Metab (2013) 98:4438–45. doi:10.1210/jc.2013-2920
4. Tahara N, Yamagishi S, Kodama N, Tahara A, Honda A, Nitta Y, et al. Clinical and biochemical factors associated with area and metabolic activity in the visceral and subcutaneous adipose tissues by FDG-PET/CT. J Clin Endocrinol Metab (2015) 100:E739–47. doi:10.1210/jc.2014-3896
5. Albu JB, Kovera AJ, Johnson JA. Fat distribution and health in obesity. Ann N Y Acad Sci (2000) 904:491–501. doi:10.1111/j.1749-6632.2000.tb06505.x
6. Sumner AE, Farmer NM, Tulloch-Reid MK, Sebring NG, Yanovski JA, Reynolds JC, et al. Sex differences in visceral adipose tissue volume among African Americans. Am J Clin Nutr (2002) 76:975–9.
7. Anjana M, Sandeep S, Deepa R, Vimaleswaran KS, Farooq S, Mohan V. Visceral and central abdominal fat and anthropometry in relation to diabetes in Asian Indians. Diabetes Care (2004) 27:2948–53. doi:10.2337/diacare.27.12.2948
8. Hill AM, LaForgia J, Coates AM, Buckley JD, Howe PR. Estimating abdominal adipose tissue with DXA and anthropometry. Obesity (2007) 15:504–10. doi:10.1038/oby.2007.629
9. Tchoukalova YD, Koutsari C, Karpyak MV, Votruba SB, Wendland E, Jensen MD. Subcutaneous adipocyte size and body fat distribution. Am J Clin Nutr (2008) 87:56–63.
10. Goel K, Gupta N, Misra A, Poddar P, Pandey RM, Vikram NK, et al. Predictive equations for body fat and abdominal fat with DXA and MRI as reference in Asian Indians. Obesity (2008) 16:451–6. doi:10.1038/oby.2007.55
11. Lee K, Lee S, Kim YJ, Kim YJ. Waist circumference, dual-energy X-ray absortiometrically measured abdominal adiposity, and computed tomographically derived intra-abdominal fat area on detecting metabolic risk factors in obese women. Nutrition (2008) 24:625–31. doi:10.1016/j.nut.2008.03.004
12. Micklesfield LK, Evans J, Norris SA, Lambert EV, Jennings C, Joffe Y, et al. Dual-energy X-ray absorptiometry and anthropometric estimates of visceral fat in Black and White South African Women. Obesity (2010) 18:619–24. doi:10.1038/oby.2009.292
13. Gradmark AM, Rydh A, Renström F, De Lucia-Rolfe E, Sleigh A, Nordström P, et al. Computed tomography-based validation of abdominal adiposity measurements from ultrasonography, dual-energy X-ray absorptiometry and anthropometry. Br J Nutr (2010) 104:582–8. doi:10.1017/S0007114510000796
14. Micklesfield LK, Goedecke JH, Punyanitya M, Wilson KE, Kelly TL. Dual-energy X-ray performs as well as clinical computed tomography for the measurement of visceral fat. Obesity (2012) 20:1109–14. doi:10.1038/oby.2011.367
15. Unno M, Furusyo N, Mukae H, Koga T, Eiraku K, Hayashi J. The utility of visceral fat level by bioelectrical impedance analysis in the screening of metabolic syndrome – the results of the Kyushu and Okinawa Population Study (KOPS). J Atheroscler Thromb (2012) 19:462–70. doi:10.5551/jat.11528
16. Ranasinghe C, Gamage P, Katulanda P, Andraweera N, Thilakarathne S, Tharanga P. Relationship between body mass index (BMI) and body fat percentage, estimated by bioelectrical impedance, in a group of Sri Lankan adults: a cross sectional study. BMC Public Health (2013) 13:797. doi:10.1186/1471-2458-13-797
17. Luke A, Bovet P, Forrester TE, Lambert EV, Plange-Rhule J, Dugas LR, et al. Prediction of fat-free mass using bioelectrical impedance analysis in young adults from five populations of African origin. Eur J Clin Nutr (2013) 67:956–60. doi:10.1038/ejcn.2013.123
18. Lewin A, Pannier B, Méline J, Karusisi N, Thomas F, Chaix B. Residential neighborhood, geographic work environment, and work economic sector: associations with body fat measured by bioelectrical impedance in the RECORD Study. Ann Epidemiol (2014) 24:180–6. doi:10.1016/j.annepidem.2013.12.001
19. Saragat B, Buffa R, Mereu E, De Rui M, Coin A, Sergi G, et al. Specific bioelectrical impedance vector reference values for assessing body composition in the Italian elderly. Exp Gerontol (2014) 50:52–6. doi:10.1016/j.exger.2013.11.016
20. Sakamaki K, Maejima Y, Tokita Y, Masamura Y, Akuzawa M, Nagano M, et al. Impact of the visceral fat area measured by dual impedance method on the diagnostic components of metabolic diseases in the middle-aged Japanese population. Intern Med (2016) 55:1691–6. doi:10.2169/internalmedicine.55.6088
21. Obuchi A, Adachi H, Enomoto M, Fukami A, Kumagai E, Nakamura S, et al. High plasma fetuin-A levels are associated with metabolic syndrome among males but not females in a Japanese general population. Diabetes Res Clin Pract (2014) 106:128–35. doi:10.1016/j.diabres.2014.07.002
22. Fukami A, Adachi H, Hirai Y, Enomoto M, Otsuka M, Kumagai E, et al. Association of serum eicosapentaenoic acid to arachidonic acid ratio with microalbuminuria in a population of community-dwelling Japanese. Atherosclerosis (2015) 239:577–82. doi:10.1016/j.atherosclerosis.2015.02.033
23. Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis (2009) 53:982–92. doi:10.1053/j.ajkd.2008.12.034
24. Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurements with ultrasound imaging. Circulation (1986) 74:1399–406. doi:10.1161/01.CIR.74.6.1399
25. Ouchi N. Adipocytokines in cardiovascular and metabolic diseases. J Atheroscler Thromb (2016) 23:645–54. doi:10.5551/jat.34918
26. Chien MY, Huang TY, Wu YT. Prevalence of sarcopenia estimated using a bioelectrical impedance analysis prediction equation in community-dwelling elderly people in Taiwan. J Am Geriatr Soc (2008) 56:1710–5. doi:10.1111/j.1532-5415.2008.01854.x
27. Piccoli A, Crosignani P, Nappi C, Ronsini S, Bruni V, Marelli S, et al. Effect of the ethinylestradiol/norelgestromin contraceptive patch on body composition. Results of bioelectrical impedance analysis in a population of Italian women. Nutr J (2008) 26:21. doi:10.1186/1475-2891-7-21
28. Okauchi Y, Kishida K, Funahashi T, Noguchi M, Ogawa T, Ryo M, et al. Absolute value of bioelectrical impedance analysis-measured visceral fat area with obesity-related cardiovascular risk factors in Japanese workers. J Atheroscler Thromb (2010) 26:1237–45. doi:10.5551/jat.5694
29. Medoua GN, Nana ES, Essa’a VJ, Ntsama PM, Matchawe C, Rikong HA, et al. Body composition of Cameroonian lactating women determined by anthropometry, bioelectrical impedance, and deuterium dilution. Nutrition (2011) 27:414–9. doi:10.1016/j.nut.2010.09.008
30. Mally K, Trentmann J, Heller M, Dittmar M. Reliability and accuracy of segmental bioelectrical impedance analysis for assessing muscle and fat mass in older Europeans: a comparison with dual-energy X-ray absorptiometry. Eur J Appl Physiol (2011) 111:1879–87. doi:10.1007/s00421-010-1795-x
31. Park KS, Lee DH, Lee J, Kim YJ, Jung KY, Kim KM, et al. Comparison between two methods of bioelectrical impedance analyses for accuracy in measuring abdominal visceral fat area. J Diabetes Complications (2016) 30:343–9. doi:10.1016/j.jdiacomp.2015.10.014
32. Health and Welfare Statistics Association 2010/2011. Annual health, labour and welfare report. J Health Labour Welfare Minist (2010) 57:87–8. (in Japanese).
33. Velazquez-Alva Mdel C, Irigoyen-Camacho ME, Huerta-Huerta R, Delgadillo-Velazquez J. A comparison of dual energy X-ray absorptiometry and two bioelectrical impedance analyzers to measure body fat percentage and fat-free mass index in a group of Mexican young women. Nutr Hosp (2014) 29:1038–46. doi:10.3305/nh.2014.29.5.7254
34. Verney J, Schwartz C, Amiche S, Pereira B, Thivel D. Comparisons of a multi-frequency bioelectrical impedance analysis to the dual-energy X-ray absorptiometry scan in healthy young adults depending on their physical activity level. J Hum Kinet (2015) 47:73–80. doi:10.1515/hukin-2015-0063
35. Lamb MJ, Byrne CD, Wilson JF, Wild SH. Evaluation of bioelectrical impedance analysis for identifying overweight individuals at increased cardio-metabolic risk: a cross-sectional study. PLoS One (2014) 9:e106134. doi:10.1371/journal.pone.0106134
36. Yamakage H, Ito R, Tochiya M, Muranaka K, Tanaka M, Matsuo Y, et al. The utility of dual bioelectrical impedance analysis in detecting intra-abdominal fat area in obese patients during weight reduction therapy in comparison with waist circumference and abdominal CT. Endocr J (2014) 61:807–19. doi:10.1507/endocrj.EJ14-0092
37. Faria SL, Faria OP, Cardeal MD, Ito MK. Validation study of multi-frequency bioelectrical impedance with dual-energy X-ray absorptiometry among obese patients. Obes Surg (2014) 24:1476–80. doi:10.1007/s11695-014-1190-5
38. Talma H, Chinapaw MJ, Bakker B, HiraSing RA, Terwee CB, Altenburg TM. Bioelectrical impedance analysis to estimate body composition in children and adolescents: a systematic review and evidence appraisal of validity, responsiveness, reliability and measurement error. Obes Rev (2013) 14:895–905. doi:10.1111/obr.12061
39. Bosaeus M, Karlsson T, Holmäng A, Ellegård L. Accuracy of quantitative magnetic resonance and eight-electrode bioelectrical impedance analysis in normal weight and obese women. Clin Nutr (2014) 33:471–7. doi:10.1016/j.clnu.2013.06.017
40. Ryo M, Maeda K, Onda T, Katashima M, Okumiya A, Nishida M, et al. A new simple method for the measurement of visceral fat accumulation by bioelectrical impedance. Diabetes Care (2005) 28:451–3. doi:10.2337/diacare.28.2.451
41. Shiga T, Hamaguchi T, Oshima Y, Kanai H, Hosoda K, Nakao K. A new simple measurement system of visceral fat accumulation by bioelectrical impedance analysis. In: Dössel O, Schlegel WC, editors. IFMBE Proceedings 25/VII. Munich (2009). p. 338–41.
42. Yamada M, Moriguch Y, Mitani T, Aoyama T, Arai H. Age-dependent changes in skeletal muscle mass and visceral fat area in Japanese adults from 40 to 79 years-of-age. Geriatr Gerontol Int (2014) 14(Suppl 1):8–14. doi:10.1111/ggi.12209
43. Huang AC, Chen YY, Chuang CL, Chiang LM, Lu HK, Lin HC, et al. Cross-mode bioelectrical impedance analysis in a standing position for estimating fat-free mass validated against dual-energy X-ray absorptiometry. Nutr Res (2015) 35:982–9. doi:10.1016/j.nutres.2015.08.005
44. Aydin M, Dumlu T, Alemdar R, Kayapinar O, Celbek G, Karabacak A, et al. Correlation between the body fat composition and high sensitive C-reactive protein in Turkish adults. Endocr Regul (2012) 46:147–52. doi:10.4149/endo_2012_03_147
Keywords: visceral fat area, metabolic syndrome, health examination, general population, epidemiological study
Citation: Enomoto M, Adachi H, Fukami A, Kumagai E, Nakamura S, Nohara Y, Kono S, Nakao E, Morikawa N, Tsuru T, Sakaue A and Fukumoto Y (2017) A Useful Tool As a Medical Checkup in a General Population—Bioelectrical Impedance Analysis. Front. Cardiovasc. Med. 4:3. doi: 10.3389/fcvm.2017.00003
Received: 05 October 2016; Accepted: 16 January 2017;
Published: 02 February 2017
Edited by:
Ichiro Sakuma, Hokko Memorial Hospital, JapanReviewed by:
Toshio Hayashi, Nagoya University Hospital, JapanIzuru Masuda, Takeda Hospital, Japan
Koichi Okita, Hokusho University, Japan
Copyright: © 2017 Enomoto, Adachi, Fukami, Kumagai, Nakamura, Nohara, Kono, Nakao, Morikawa, Tsuru, Sakaue and Fukumoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mika Enomoto, ZW1pa2FAbWVkLmt1cnVtZS11LmFjLmpw
 Mika Enomoto
Mika Enomoto Hisashi Adachi1,2
Hisashi Adachi1,2 Yoshihiro Fukumoto
Yoshihiro Fukumoto