- 1Faculty of Architecture, Chiang Mai University, Chiang Mai, Thailand
- 2Department of Pediatrics, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 3Faculty of Architecture, Walailak University, Nakhon Si Thammarat, Thailand
Physical environment factors in healthcare facilities play an important role in user health and wellbeing, especially among healthcare workers. This research studies the problems, prioritization, and in-depth details of each physical environment factor that affects the stress levels of medical staff. It also seeks to involve medical staff in identifying the built environment factors that influence their stress levels. An examination and comparison of the physical environment factors that affect the mental health and stress of out-patient and pediatric ward staff will also be presented. A three-step data collection process was used: physical environment observation using a checklist, a survey using an analytic hierarchy process (AHP) questionnaire, and individual interviews. Data were collected from 16 medical staff in the pediatric out-patient ward and 17 medical staff in medicine out-patient ward. The observational findings showed that the two out-patient wards had similar environmental problems. AHP ranking findings illustrate that acoustics, privacy, and accessibility were issues of concern for both out-patient ward medical staff. Four different themes emerged from the analysis of the medical staff interviews. Two design recommendations are made to reduce medical staff stress: improving the working environment to decrease stress and improving space management.
1 Introduction
Designing a workplace environment that is comfortable for medical staff can help reduce occupational burnout and increase efficiency in health service provision (Montgomery et al., 2022). This requires evidence-based design in conjunction with field study to identify the physical factors that affect the efficiency and stress levels of medical staff, who have a high risk of mental health problems due to work loads and demands. For example, stress, burnout, anxiety, or depression could affect the health service efficiency of medical staff, with the workplace environment being an important factor (Gray, P. et al., 2019). After the COVID-19 pandemic, there has been more responsiveness between mental health and architecture, especially in healthcare facilities and with medical staff (Goulart F.M. and Ono R., 2022).
In addition to work-related issues encountered on a day-to-day basis, the physical environments of clinics or workplaces also impact these stress levels and efficiency, potentially affecting health services (Favrod, C. et al., 2018). The present case study concerns Maharaj Nakorn Chiang Mai Hospital, which serves as a tertiary care university hospital for patients who suffer from severe illnesses and are at high risk. The study was conducted in two distinct out-patient clinics with different functions: the general internal medicine out-patient located in the Chaloem Phrabarami Building, and the general pediatric out-patient clinic in the Sriphat Medical Center (Figure 1).
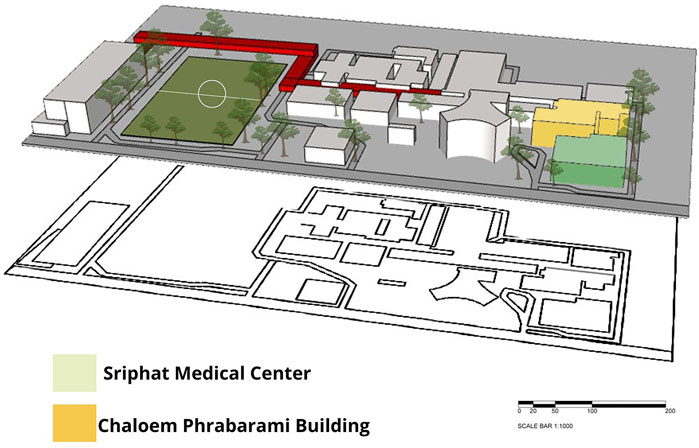
Figure 1. Study area: Sriphat Medical Center and Chaloem Phrabarami buildings, location of general medicine ward and pediatric medical ward.
This research studies and compares the physical environment problems between outpatient departments and pediatric wards. The two research questions are framed as follows:
(1) What are the current environmental conditions of the internal medicine clinic and the pediatric clinic, and how do they affect the stress levels of medical staff working in each?
(2) Which environmental factor(s) affect(s) the stress levels of the medical staff working in the internal medicine and pediatric clinics?
2 Literature review
The physical environment is a factor that can cause stress arising from humans interacting with their sensory environments. Out-patient clinics should facilitate basic examinations and ensure flexible, comprehensive, and adequate services to patients and their families. Total Alliance Health Partners International (TAHPI) (2017) categorize space design in out-patient clinics into five areas: patient, support, staff, non-overnight treatment, and public areas.
Evidence-based design refers a design approach that incorporates scientific analysis and research to create designs that are suitable for users, particularly in the case of healthcare facility design, which is characterized by complexity, in order to enhance a building’s efficiency (Lawson, 2010). Hamilton (2003) describes the four levels of evidence-based practice. The first involves conducting literature review, and the second level involves readings and hypothesizing expected outcomes to minimize irrelevant design tasks. The third level requires the dissemination of findings through academic conferences or publications in order to encourage accessibility and discussion, while the fourth level includes the validation of evidence by qualified experts. The Center for Health Design (CHD) introduced a precise guideline for using post-occupancy evaluation (POE) to evaluate hospital buildings: “Clinic Design for POE”. This entails an assessment to be conducted after occupancy to evaluate clinical areas, focusing on spatial and physical environmental factors (The Center for Health Design, 2015).
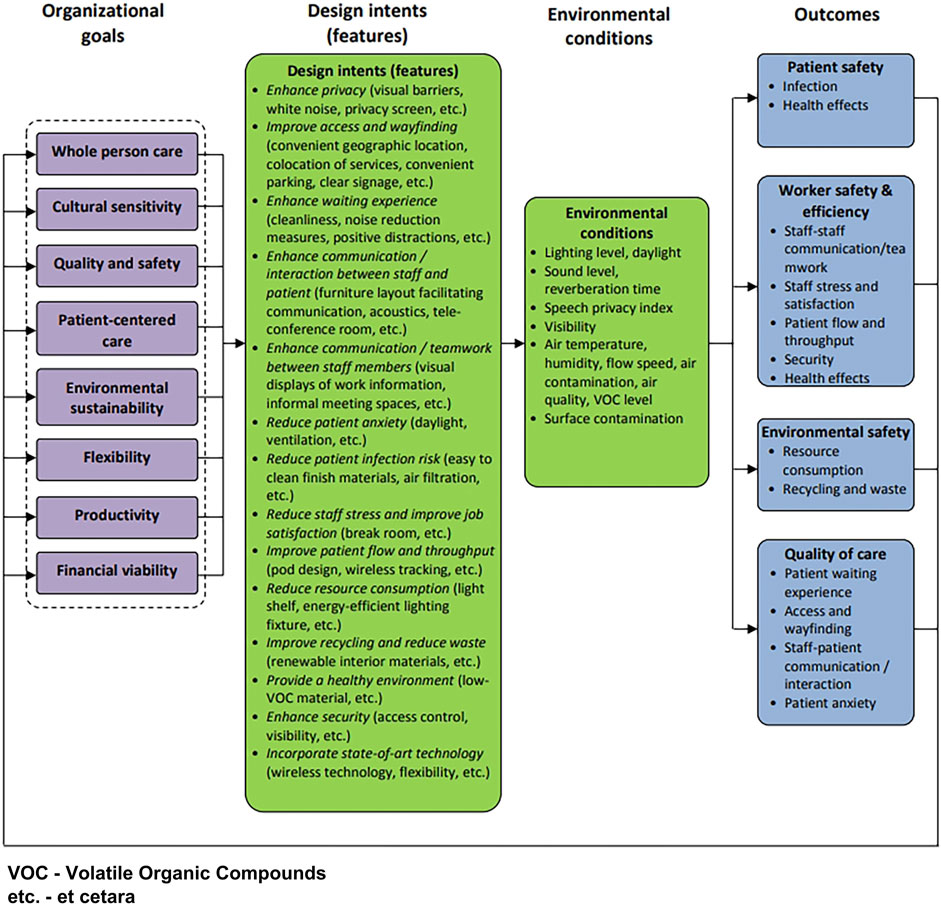
According to the design intention in Figure 2 illustrating the conceptual framework of clinic design POE, there are seven features relevant to this study: enhancing privacy, improving access and wayfinding, enhancing waiting experience, improving communication/interaction between staff and patients, enhancing communication/interaction between staff members, reducing patient infection risk, and reducing staff stress and improving job satisfaction. The framework also specifies five environmental conditions that cover lighting and sound levels, privacy, visibility, and contamination. This served as a basis for designing the data collection process, which includes a survey, questionnaire, and interview.
Stress reduction design in hospitals involves designing a physical environment that helps reduce stress and fatigue, while increasing the efficiency of medical staff. The physical environment factors relevant to healing environment design are as follows.
• Lighting: this should be adequate and appropriate for the respective tasks in each area, at 100–500 LUX (Pan American Health Organization: PAHO, 2020).
• Acoustics: noise levels within the building should not exceed 40–45 dB (World Health Organization (WHO), 2010; U.S. Environmental Protection Agency (US EPA), 1978).
• Accessibility: access should be easy and quick from outside the building, with clear directional signs and no obstruction (Department of Health, 2014).
• Privacy: ensuring both audio and visual privacy in functional areas and private areas for staff (Ulrich et al., 2004).
• Interior decor: providing windows or openings that afford views of green spaces and nature, and using bright colors or decorative paintings (Ulrich et al., 2004; Department of Health, 2014).
• Sufficient space both in functional and support areas (Total Alliance Health Partners International (TAHPI)., 2017).
• Relaxation areas: hospital non-clinical areas should provide relaxation space and greenery areas to help reduce stress (Ulrich et al., 2004).
• Positive distraction: objects or areas that can reduce stress, such as televisions, decorative paintings, and natural or biomimetic materials (Ulrich et al., 2004; Department of Health, 2014).
• Queues: hospital should be able to provide information the number of patients waiting for medical services and the waiting times (Department of Health, 2014).
• Air quality: specific management regarding thermal conditions (for Thailand, comfort zone ranges 18–25°C) (ERDI-CMU, 2024); clinical and non-clinical areas should implement ventilation machines, including air filtration (ASHRAE, 2019).
POE and prioritizing clinical design POE are evaluations of the physical environment after a certain period of use.
Physical environment factors can impact the stress levels of medical staff, as humans interact with the physical environment through their sensory systems. Thus, out-patient clinic design should facilitate basic examinations and ensure flexible, comprehensive, and adequate services to patients and their families. This study focused on areas for medical staff, which could be divided into four zones: support, staff, clinical, and other. Only support and staff areas were investigated in this research. There are a variety of factors that affect the stress levels and mental health of medical staff, particularly registered nurses and nurse assistants with their extensive working hours in out-patient clinics. This research aimed to identify the physical environment factors that affect the stress levels of medical staff working in Medical Maharaj Nakorn Chiang Mai Hospital.
3 Methodology
3.1 Research design
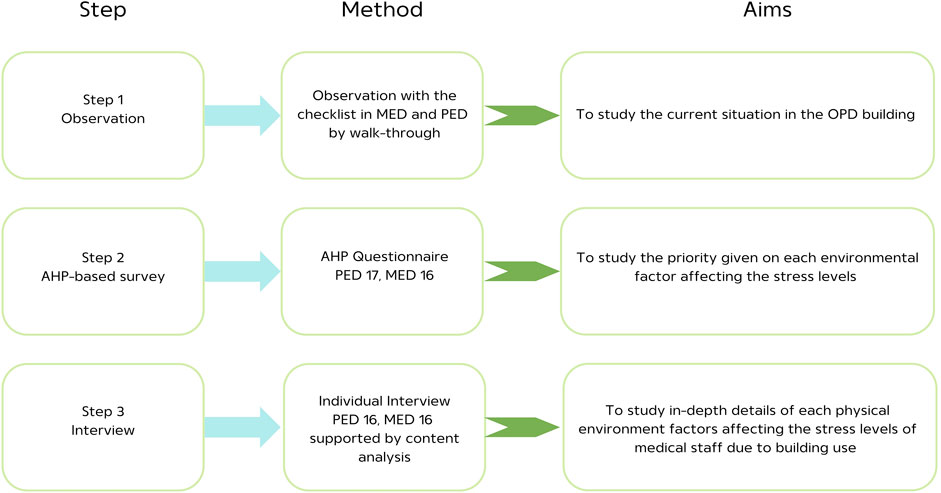
A three-step data collection process was used in this study: observation of the physical environment, a questionnaire survey, and individual interviews. We first gathered the physical environment information by using a checklist and then converting it into a questionnaire before obtaining further details from individual interviews. Figure 3 presents a flow chart demonstrating the research process.
Step 1: Physical environment observation. This step of data collection is known as “walk-through observation” (Fronczek-Munter, 2016). Data were collected through a checklist, photographs, and architectural building plans.
Step 2: AHP-based survey. An analytic hierarchy process (AHP) questionnaire was used.
Step 3: Interviews. Data were collected through individual interviews with medical staff in the two wards which was supported by content analysis.
3.2 Case study
The first step of this study was built-environment observation, in which the data were collected through walk-through observation. It was conducted in two wards: the medicine and pediatric out-patient wards. They were selected due to their similarity in not requiring overnight stays with a difference in terms of patients’ age. Both clinics were situated in Maharaj Nakorn Chiang Mai Hospital, which is a tertiary hospital with over 30 years of operation and a capacity of 1,400 beds.
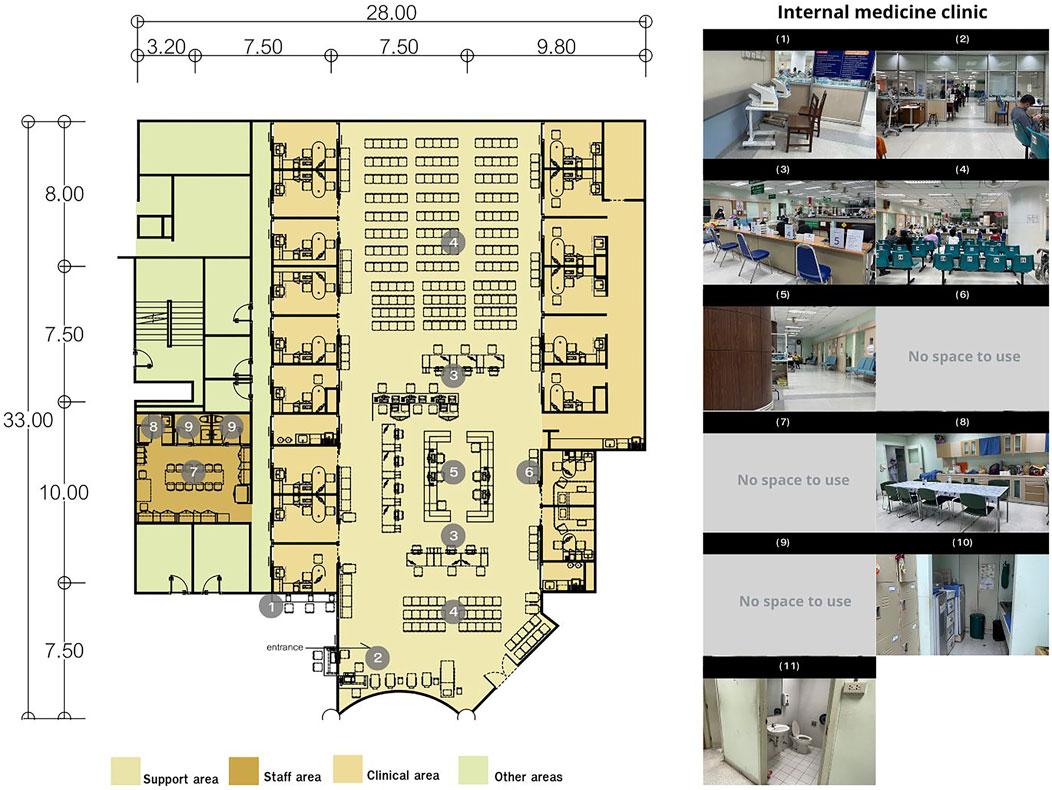
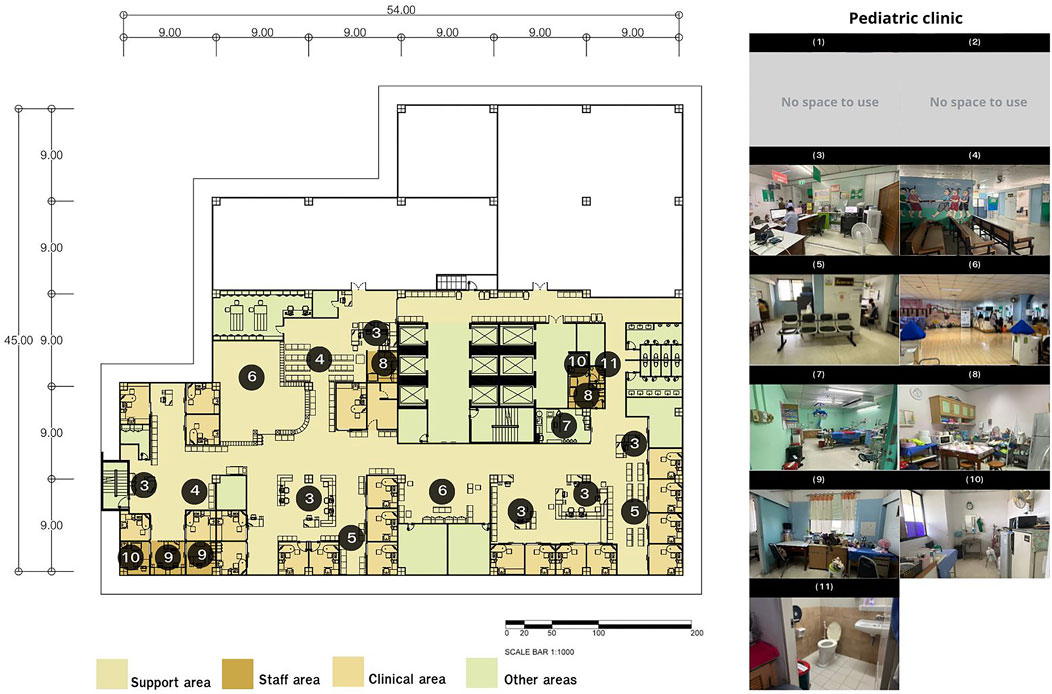
Both out-patient ward layouts can be classified into four main areas. Figures 4 and 5 illustrate the overall areas of both wards.
(1) Support area (light yellow) includes the history-taking areas, waiting areas, and nurses’ stations.
(2) Staff area (brown) includes staff lounges.
(3) Clinical area (dark yellow) includes the examination rooms.
(4) Other areas (green).
The data were collected only in areas frequently used by registered nurses and nursing assistants, which were the support and staff areas. Clinical and other areas were excluded.
3.3 Participants
This study aimed to compare two out-patient wards regarding which physical environment factors in each could cause stress, focusing on the differences in patients’ age and other contexts. Hence, the pediatric and medicine out-patient wards were chosen. A group of medical staff (registered nurse and nurse assistant) from two out-patient wards in the Maharaj Nakorn Chiang Mai Hospital were surveyed about their workplace physical environments through an AHP questionnaire and interviews. Data were collected from 16 medical staff in the pediatric out-patient ward and 17 in the medicine out-patient ward. Participants were first informed about the purpose of the study. A set of questionnaires was provided and then an individual interview was conducted to gather more information on each factor. Ethical approval was obtained from the Research Ethics Committee Panel 5 Faculty of Medicine, Chiang Mai University (NONE-2566–0585).
3.4 Data collection and analysis
The study data collection was divided into three steps. The first step was physical environment observations, the second was an AHP-based survey, and the last step was individual interviews.
Step 1: Physical environment observation
A physical environment observational study was conducted using a checklist (lighting, acoustics, accessibility, privacy, interior, working environment, sufficient space, relaxation space, queues, and positive distraction) and photographs of walk-throughs. The same checklist, consisting of physical environment factors associated with stress, was employed to compare the two out-patient wards regarding each factor. The data were analyzed using the observation results as recorded in the checklist in conjunction with photographs and architectural building plans to compare the two wards factor by factor.
Step 2: AHP-based survey
We applied a quantitative method called “analytical hierarchy process” (AHP), used for quantitative decision-making. This method is used to solve complex problems that involve selecting or making decisions from multiple alternatives. It consists of breaking down a problem into a series of steps or layers, such as goals, criteria, and decision options (Saaty, T., 1990). This method includes the following.
Consistency Index (CI):
The CI measures the degree of consistency in the pairwise comparison matrix. It indicates how much the judgments deviate from perfect consistency. Mathematically, it is calculated using the following formula:
where
• λmax is the largest eigenvalue of the pairwise comparison matrix.
• n is the number of items being compared.
Consistency ratio (CR):
The CR evaluates how much the consistency of the judgments deviates from a random set of judgments. It compares the CI to an average random consistency index (RI), which is a value based on the size of the matrix.
The formula for the CR is
where
• RI is the random index, depending on the number of elements (n) and derived from a randomly generated matrix. For instance, for three items, the RI is 0.58, and for four items it is 0.9.
• If the CR is less than 0.10 (10%), the consistency is acceptable. If it is above 0.10, the judgments may need to be revised because they are considered too inconsistent.
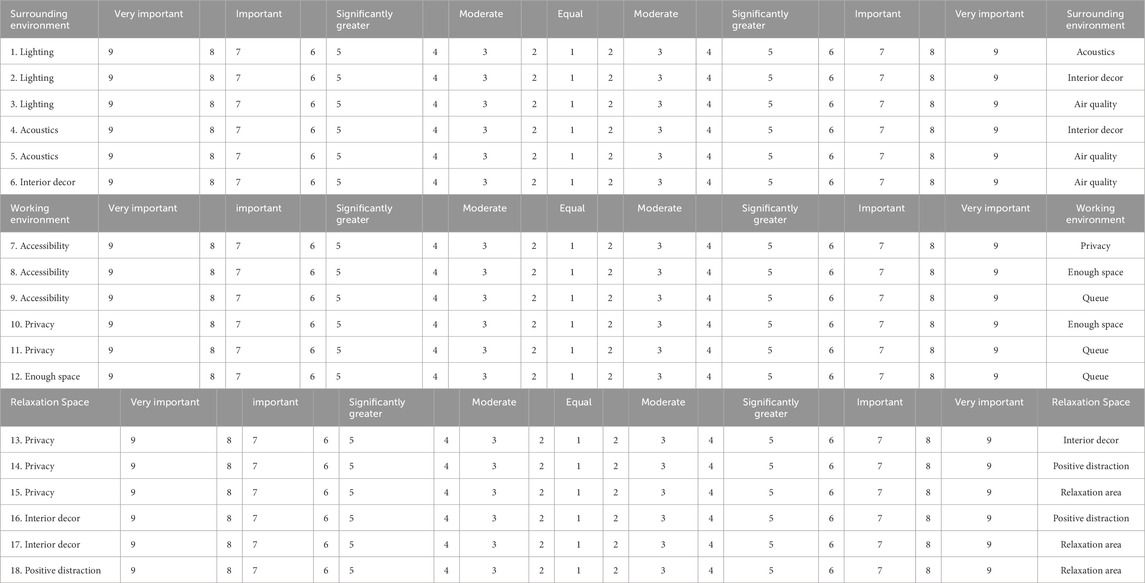
A questionnaire was designed to record the priority given to each environmental factor. The questionnaire items were derived from the factors in the checklist to compare the prioritization of factors. The 18-item questionnaire was designed to compare each pair of factors. Participants were medical staff recruited to answer the AHP questionnaire, and later the same group of medical staff were interviewed. The interviews took about 10–15 min by completing the questionnaire and giving ratings by marking numbers ranging from 1 to 9. A rating of 1 indicated equal importance of both factors, while 9 indicated that the factor in questions was significantly more important than the other. The factors obtained from physical environment observation were categorized into three main factors, each containing minor factors that were paired for comparison (Table 1, which illustrates the comparison of environment factors used in the AHP method).
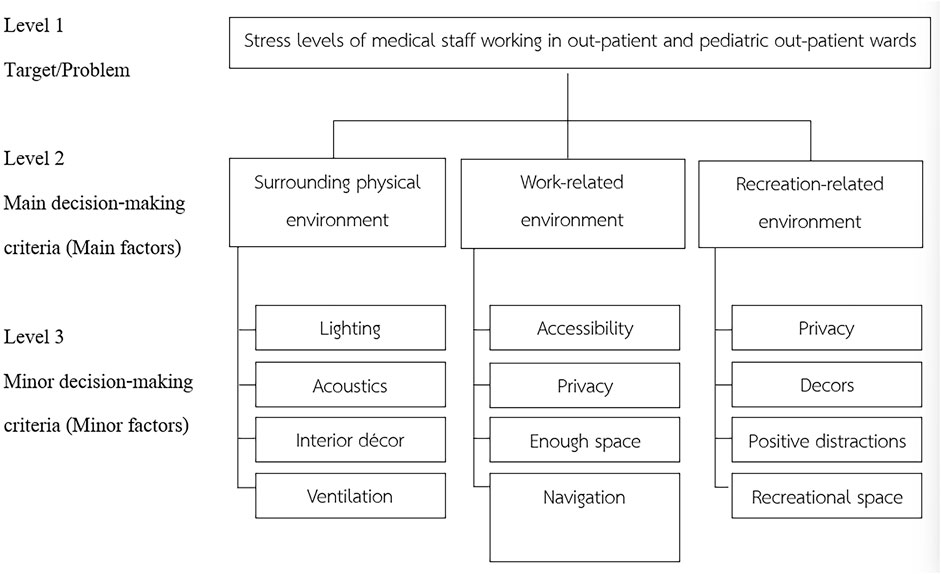
For data analysis, AHP was employed to arrange the factors in the hierarchy structure (Saaty, T., 1990). This illustrates each factor’s priority in hierarchical order in each ward. Figure 6 shows the chart of the AHP hierarchical order, where level 1 refers to this research problem statement, level 2 to the main environmental factors that have a strong effect on medical staff stress, and level 3 relates to minor environmental factors that have an effect on medical staff stress levels.
Step 3: Individual interview
The results obtained from the questionnaire were then utilized in designing interview questions. The interview was conducted individually for approximately 15–20 min per person. The interview questions were:
- What is the current situation in the Out-Patient Department (OPD) building?
- Do you think that physical environment factors could affect your stress rate or job performance?
- Which factors are the most important to and impact your stress or job performance?
- Do you think that the OPD’s current condition promotes or negatively impacts your stress and performance?
The individual interviews were analyzed as follows.
Individual interviews were supported by content analysis (Corbin and Strauss, 2015; Waroonkun and Prugsiganont, 2022). The researcher transcribed the interviews from the audio recordings and divided the transcriptions into meaning units. These units were then abbreviated into condensed meaning units and coded by searching for key phrases related to the physical problems of the OPD buildings. The codes were grouped into categories, sub-categories, and themes (Erlingsson and Brysiewicz, 2018). How the content analysis was applied is explained below.
• Condensed meaning units: a process of shortening the text while still preserving the core meaning.
• Code: a label; a name that most exactly describes what this particular condensed meaning unit is focused on.
• Category: formed by grouping related codes through their content or context. Codes were organized into categories when they described different or similar aspects of the text’s content that belong together.
• Sub-categories: categories related to each other through their content can then be grouped into categories.
• Theme: expressing an underlying meaning; latent content, found in two or more categories. Themes express data on an interpretation (latent).
4 Result
4.1 Area observation
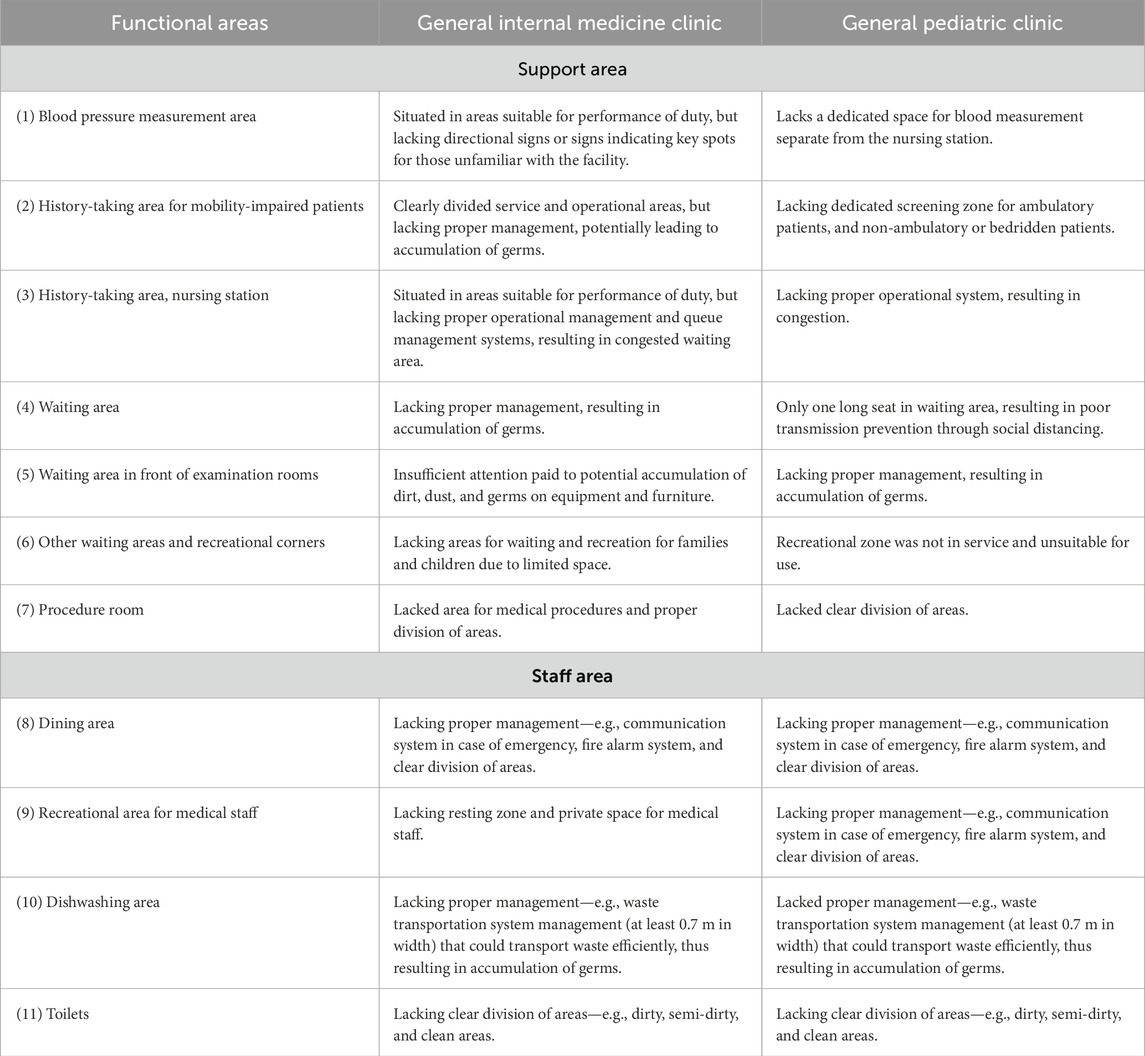
The walk-through observations and photographs present the current physical state of the two out-patient wards. Figures 5 and 6 show the layout and use of the General Internal Medicine Clinic at Chaloem Phrabarami Building and the General Pediatric Clinic at Sriphat Medical Centre, respectively. The support and staff areas of both clinics served as the areas of study. Both Figures 5, 6 compared architectural plans and walk-through observations. However, Figures 5, 6 revealed different building plans. Due to the difference in location, there were some similarities and differences in terms of their physical environments, particularly in the recreational areas. The clinic designed for adult patients had a dedicated recreational space which was separate from areas accessible by patients, making it more private than the clinic designed for pediatric patients. Table 2 shows a comparison between the two clinics by area with clear descriptions provided.
4.2 AHP ranking findings
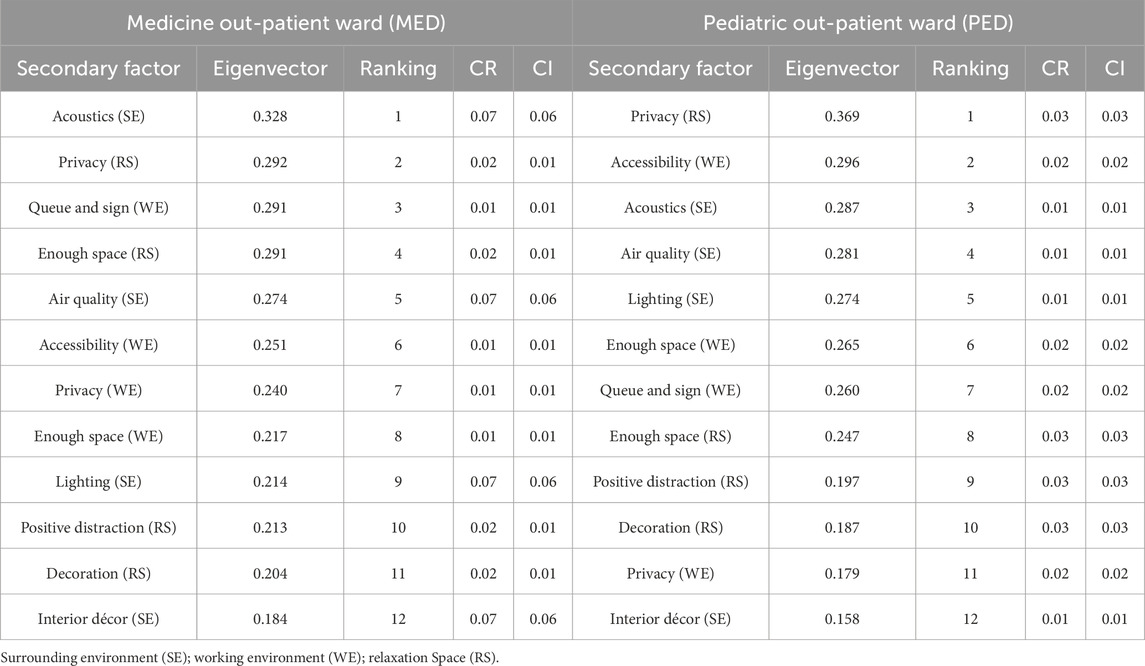
This study employed a questionnaire to conduct pairwise comparisons to assess the relative importance of factors in both clinics. The results were analyzed using the analytic hierarchy process (AHP), and then physical environment factors were ranked. The Consistency Ratio (CR) and index (CI) were calculated, whereby the CR had to be less than 0.1 to be considered consistent (Saaty, 1990). The results, showing ranking factors, are as follows. Surrounding environment (SE) CR (MED = 0.07, PED = 0.01); CI (MED = 0.06, PED = 0.01). Working environment (WE) CR (MED = 0.01, PED = 0.02); CI (MED = 0.01, PED = 0.02). Relaxation space (RS) CR (MED = 0.02, PED = 0.03); CI (MED = 0.01, PED = 0.03). PED refers to “pediatric out-patient ward” and MED refers to “medicine out-patient ward”. Table 3 provides AHP analysis results, where the table also compares and ranks the most important physical environment factors between the general medical and pediatric clinics.
Acoustics was the most important factor for staff working in the General Internal Medicine Clinic at 0.312, followed by privacy in the recreational space (0.293) and indications of service (0.202). For the General Pediatric Clinic, the staff rated privacy in the recreational space (0.355) as the most important factor, followed by accessibility (0.290) and acoustics (0.288). The use of interior decor was regarded as the least important factor in both clinics at 0.157 and 0.162.
4.3 Interviewresults
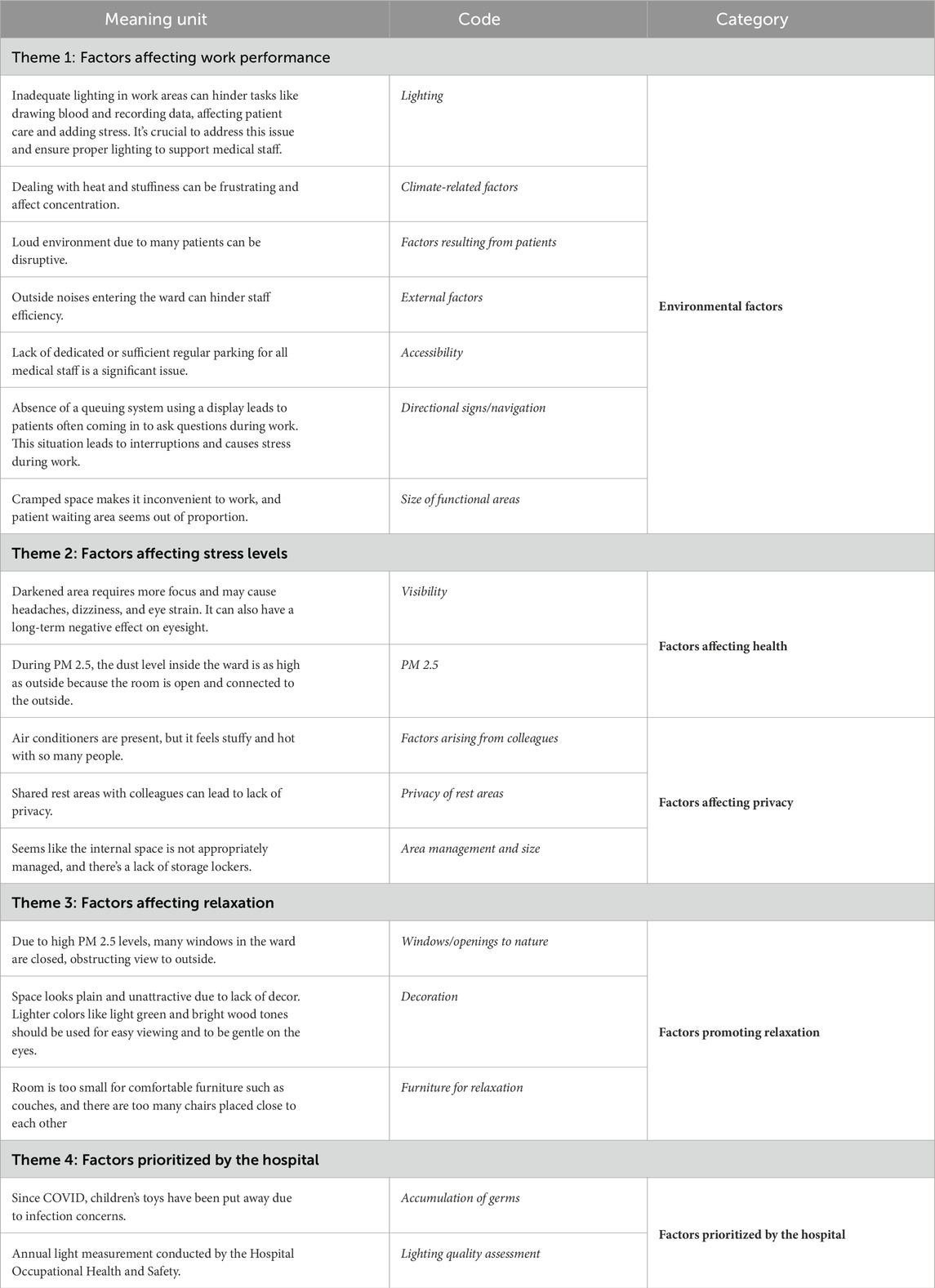
Interviews on physical environment factors were conducted individually, taking 15–20 min per person. Using content analysis, the data were analyzed and categorized into four themes: factors affecting work performance, factors affecting stress levels, factors affecting relaxation, and factors prioritized by the hospital. Table 4 provides the examples of medical staff interview analysis. Details are discussed below.
Theme 1. Factors affecting work performance refer to environmental factors in the areas under study that have direct and indirect impacts on the work performance of the medical staff. Such factors result from patients, external factors, lighting, weather conditions, area accessibility, directional signs, navigation, and sizes of functional areas.
o Lighting: Staff in both clinics agreed that there was insufficient lighting, which affected their work performance and concentration (Medicine Out-Patient Ward (MED) 43.75%) and (Pediatric Out-Patient Ward (PED) 62.50%). Interviews with staff in the General Internal Medicine Clinic revealed that insufficient lighting disrupted their efficiency. Similarly, staff in the General Pediatric Clinic stated that the functional areas did not have enough lighting, causing inconvenience during tasks such as blood drawing, result reading, and data recording.
o Climate-related factors: The temperature and internal climate in both clinics impeded work performance and space usage (MED 43.75% and PED 43.75%). The interviews with staff in both clinics showed that these factors obstructed work performance and space usage, such as by causing a reduction in concentration. The temperature measured during data collection (6 April 2024) was 39–43 °C (Thai Meteorological Department, 2024)—10°C higher than the Thai comfort zone. This condition resulted from air conditioning being available only in certain areas.
o Factors resulting from patients: Due to the nature of their work, medical staff, especially nurses, had to be in contact with patients and families, which could cause noise disturbance (MED 87.50% and PED 50%). The staff in both clinics reported that a large number of patients generated noise (e.g., talking and shouting), disrupting their concentration and impairing their ability to focus on their work.
o External factors: These included noise disturbance from external sources, repair work within the buildings, calls and notifications, and traffic (MED 37.50% and PED 37.50%). Both groups of staff stated that noise from outside sources, such as announcements, ambulances, and repair work, affected their performance.
o Accessibility: The lack of a clear division between areas for staff and patients within the hospital resulted in work-related issues, such as with clocking in and out due to limited parking spaces. The interviews with staff in both clinics showed that insufficient parking spaces for medical staff was an ongoing problem affecting their timekeeping (MED 43.75% and PED 75%).
o Directional signs/navigation: These signs and indications could enhance the staff’s convenience and mobility. The staff of both clinics reported a lack of proper area management, thus increasing burdens on them (MED 75% and PED 68.75%), such as the lack of an electronic queue management system and signs for key spots for those who might be unfamiliar with the location.
o Size of functional areas: Both clinics lacked enough space to accommodate their operations (MED 31.25% and PED 62.50%). The interviews revealed that both clinics had limited space, resulting in congestion during staff use and operations.
Theme 2. Factors affecting stress levels refer to physical environment factors affecting stress levels, which divide into two categories—those affecting health and those affecting privacy.
• Factors affecting health consist of visibility and PM 2.5 ventilation.
o Visibility: Lighting could affect visibility for medical staff. Based on the interviews with staff in both clinics, insufficient lighting caused visual difficulties and disrupted their work performance.
o PM 2.5: Chiang Mai faces annual air quality issues, causing it to be one of the world’s most affected cities by PM 2.5; due to the open-air structures, pollutants could enter the clinics. Interviews with staff in both clinics showed that PM 2.5 levels inside the clinics were as high as outside due to the lack of PM 2.5 prevention measures (no internal ventilation system within the buildings). The PM 2.5 level measured during data collection (6 April 2024) was 231 μg/m³ (parts per million) (Iqualityair, 2024).
• Factors affecting privacy arise from colleagues, privacy in the resting zones, and area organization and size.
o Factors arising from colleagues: There was no private space for staff within the recreational space. Both groups of staff stated that the lack of private space within recreational space affected their resting and sense of privacy. Personal lockers and recreational zones should be provided for staff.
o Privacy of resting areas: Resting areas should be conveniently located near the clinics’ functional areas. Interviews with staff from both clinics reported that there was no clear division of areas within the resting areas due to limited space, making them less desirable for use.
o Area management and size: Area management within the resting areas could increase privacy. However, it must be proportionate to the size, as narrow or insufficient space could negatively impact privacy within the resting areas. The staff from both clinics stated that the areas were crowded and insufficient.
Theme 3. Factors affecting relaxation refer to physical environment factors that impact both the physical and psychological relaxation of the medical staff. Factors promoting relaxation include windows/openings to nature, decor, and furniture for relaxation.
o Windows/openings to nature: A limited number of windows at the clinics reduced natural views from working areas. The interviews showed that the lack of openings to nature in both clinics resulted in stress at work due to the lack of visual relaxation.
o Decor: Currently, both clinics had very little decor; only vibrant pastel colors and biomimetic materials were used. Interview data indicated that both groups of staff preferred to have more decor within the clinics, such as paintings of nature and beautiful scenery.
o Furniture for relaxation: The use of furniture in both clinics did not take into account functionality. Interview data showed that the amount of furniture was insufficient for use and impractical for users, and that there was a lack of furniture for relaxation, such as resting sofas.
Theme 4. Factors prioritized by the hospital refer to factors to which the hospital gave priority through prescribed policies and guidelines. Factors prioritized by the hospital consisted of the accumulation of germs and lighting quality assessment.
o Accumulation of germs: Hospitals are sources of germs. The interviews with the General Internal Medicine Clinic showed that plant pots were prohibited inside the building, as they could be sources of dust, dirt, or germs, while the staff at the General Pediatric Clinic mentioned that toys in the recreational area were removed to prevent infection and the transmission and accumulation of pathogens.
o Lighting quality assessment: Since lighting is important to visibility and work performance, the hospital assigned officers to assess lighting quality and fix any related issues. Staff at the General Internal Medicine Clinic reported that occupational health officers had been brought in for annual assessments of the lighting.
5 Discussion
In this study, we aimed to gain insights into the problems and in-dept details regarding physical environmental factors that affect the stress levels of medical staff in the General Internal Medicine Clinic and the General Pediatric Clinic. The answers to the established research questions are as follows.
(1) How do the current environmental conditions of the two clinics affect the stress levels of the medical staff working in each? Observational surveys and interviews revealed major issues regarding built environment and the clear division of zones. In the General Internal Medicine Clinic, the blood pressure measurement area, the procedure room, the resting areas for staff, and the restrooms are not clearly divided, which can cause congestion during use, particularly in resting areas and restrooms. Both clinics did not have clear zonings, making the spaces inadequate for use and lacking in both audio and visual privacy (Ulrich et al., 2004). Areas can be zoned by three key functional areas for clearly divided spaces. The first would be the entrance zone, comprising the reception area, waiting area, and patient accommodation areas such as restrooms and play areas. The second zone would be for history-taking, comprising areas for initial assessment and history-taking, blood pressure measurement, blood drawing, and temperature measurement, as well as areas for staff use, both for professional and recreational purposes (Total Alliance Health Partners International (Total Alliance Health Partners International (TAHPI)., 2017).
In terms of management and space design, both the General Internal Medicine and General Pediatric Clinics lack several aspects of proper internal building management. First, the areas designated for non-ambulatory patients’ history-taking lack an effective patient screening management system, resulting in insufficient functional space (Total Alliance Health Partners International (TAHPI)., 2017) and the capacity to accommodate patients receiving health services, leading to congestion, especially in the entrance–exit areas. Such a crowded working environment may impact the efficiency and mental health of medical staff, as well as pose potential risks regarding the accumulation of germs in areas heavily frequented by patients with respiratory diseases (Rao, 2004; Cubukcuoglu C. et al., 2022). The second issue is inadequate operational management systems. In the history-taking areas and the nursing stations, the queue system is not properly managed, and waiting times and queue number are not displayed in the waiting areas, hindering patients’ access to relevant information (Department of Health, 2014). Third, there is no communication system connecting the operational area with the resting area in case of emergency, thus raising the need for an internal telephone line (Han, J. et al., 2018). Lastly, the lack of proper space management and furniture placement causes difficulties in hygiene maintenance, potentially leading to the accumulation of germs. Moreover, the furniture is unsuitable for use as it does not conform to ergonomic principles (Total Alliance Health Partners International (TAHPI)., 2017; Lehane, E. et al., 2019).
(2) There are two design recommendations that can be followed to provide an improved environment for medical staff and help reduce their stress levels.
5.1 Environmental improvement to reduce stress
• Consider adding windows or openings that afford views of green spaces and nature, or increasing the amount of lighting to 500 LUX in the operational areas, 50 LUX in the corridor, and 100 LUX in the waiting hall (Pan American Health Organization: PAHO, 2020; Ulrich et al., 2004; Department of Health, 2014).
• Improve the air-conditioning and ventilation systems by adopting heating, ventilation, and air conditioning (HVAC) systems, high-efficiency particulate air (HEPA) filter ventilation, and UV light (ASHRAE, 2019) to optimize working conditions for the medical staff.
• Consider adding interior decor, such as a television in the waiting hall or paintings to enhance the aesthetics of the rest areas for staff, and decorating the clinics using natural or biomimetic materials, as well as adjusting the furniture placement according to ergonomic principles. Uses of benches and furniture articles with hard-to-reach corners or made from materials that are difficult to clean should be discouraged (Ulrich et al., 2004; Department of Health, 2014).
5.2 Improvement in space management
• Space should be managed in a practical manner with clear divisions, particularly in the nursing stations and the waiting and reception areas to improve service provision and access to relevant information, as well as to facilitate operations and maximize efficiency for medical staff (Department of Health, 2014). Improvements should also be made in the private areas reserved for staff by providing personal lockers and recreational zones for use during breaks (Ulrich et al., 2004; Department of Health, 2014).
• Technology should be adopted to assist queue management by incorporating an online patient registration system to reduce the number of patients in the waiting areas. This will help reduce infection rates and noises that can disturb the practitioners. The AHP ranking results confirm that acoustics is the most prominent factor to impact stress levels (World Health Organization (WHO), 2010; U.S. Environmental Protection Agency (US EPA), 1978).
• Establish cleaning procedures that are in line with WHO COVID-19 prevention protocols (WHO, 2022), which require areas to be cleaned regularly, at least two to three times daily, and sufficient wash basins to be provided in different areas.
6 Conclusion
This study was conducted to obtain insights into problems regarding the factors that affect the stress levels of medical staff working in the General Internal Medicine Clinic and the General Pediatric Clinic, as well as to examine and compare the physical environment factors affecting their mental health and stress levels. The problems are categorized into two aspects: issues regarding the clear division of areas which contribute to congestion, operational area management, and resting areas for staff, and issues regarding area management and design whereby the hospital had not incorporated a screening system in the history-taking areas and nursing stations, and queue management technology that would help systematize the operation. Moreover, the furniture was not suitable and there was a lack of cleaning procedures to reduce the accumulation of germs. To reduce stress caused by the workplace, lighting sources and green spaces should be added, as well as an appropriate HVAC system. An assessment of factors affecting staff mental health and stress levels shows that acoustics and privacy are regarded as the most important factors across both clinics, followed by accessibility and navigation.
7 Implications
This research enables a better understanding of the problems and physical environment factors that affect the stress levels of medical staff working in the General Internal Medicine and the General Pediatric Clinics, and its findings can also be applied to reduce stress among medical practitioners in public hospitals. It highlights the importance of the involvement of medical staff in identifying environmental factors in detail. Guidelines on environmental improvement to reduce stress among medical staff include improving the workplace environment by adding windows or openings that afford views of nature and green spaces, upgrading air-conditioning and ventilation systems, improving clinics decors, changing furniture placement following ergonomic principles, and avoiding furniture with hard-to-reach corners or made from materials that are difficult to clean.
• Space management must be optimized to suit staff operations with a clear division of areas. Technology should be incorporated for managing the queue system. In terms of hygiene maintenance, cleaning procedures must be established, which would include regular cleaning at least two to three times daily, and wash basins should be readily available in various locations.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee Faculty of Medicine Chiang Mai University. This research received ethical number: MRCMU2566R_022 with research ID: NONE-2566-0585. The studies were conducted in accordance with local legislation and institutional requirements. Participants provided their written informed consent to participate in this study.
Author contributions
TW: conceptualization, formal analysis, investigation, methodology, resources, supervision, validation, writing–original draft, and writing–review and editing. SP: conceptualization, formal analysis, supervision, writing–original draft and writing–review and editing. KW: conceptualization, resources, and writing–original draft. JC: data curation, formal analysis, methodology, resources, software, visualization, and writing–review and editing. NP: data curation, formal analysis, investigation, methodology, visualization, and writing–review and editing.
Funding
The authors declare that financial support was received for the research, authorship, and/or publication of this article. The research was funded by Chiang Mai University Mid-Career Research Fellowship Program grant number: MRCMU2566R_022.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
ASHRAE. (2019). Ventilation for acceptable indoor air quality. Available at: https://ashrae.iwrapper.com/ASHRAE_PREVIEW_ONLY_STANDARDS/STD_62.1_2019 [Accessed March 15, 2024].
Corbin, J. M., and Strauss, A. L. (2015). Basics of qualitative research: techniques and procedures for developing grounded theory. 4th ed. CA: Sage publications.
Cubukcuoglu, C., Nourian, P., Sariyildiz, I. S., and Tasgetiren, M. F. (2022). Optimal design of new hospitals: a computational workflow for stacking zoning and routing. Automation Constr. 134, 104102. doi:10.1016/j.autcon.2021.104102
Department of Health (2014). Departmental improvement plan. Available at: https://assets.publishing.service.gov.uk/media/5a7ee45440f0b62305b83d67/DIP_April_2014 (Accessed March 10, 2024).
ERDI-CMU (2024). Thailand comfort zone. Available at: https://erdi.cmu.ac.th/website_new/ (Accessed October 9, 2024).
Erlingsson, C., and Brysiewicz, P. (2018). A hands-on guide to doing content analysis. Afr. J. Emerg. Med. 7, 93–99. doi:10.1016/j.afjem.2017.08.001
Favrod, C., Jan du Chêne, L., Martin Soelch, C., Garthus-Niegel, S., Tolsa, J. F., Legault, F., et al. (2018). Mental health symptoms and work-related stressors in hospital midwives and NICU nurses: a mixed methods study. Front. Psychiatry 9, 364. doi:10.3389/fpsyt.2018.00364
Fronczek-Munter, A. (2016). Usability briefing for hospital design: exploring user needs and experiences to improve complex buildings. Lyngby, Copenhagen, Denmark: Technical University of Denmark. [PhD thesis].
Goulart, F. M., and Ono, R. (2022). Post-occupancy evaluation and codesign in mental healthcare buildings: user’s input as a driver for functional and technical adaptations in post COVID-19 reality. Front. Built Environ. 8. doi:10.3389/fbuil.2022.962940
Gray, P., Senabe, S., Naicker, N., Kgalamono, S., Yassi, A., and Spiegel, J. M. (2019). Workplace-based organizational. Int. J. Environ. Res. public health 16, 22. doi:10.3390/ijerph16224396
Han, J., Kang, H. J., and Kwon, G. H. (2018). A measurement for evaluating the environmental quality of advanced healthcare facilities: intelligent healthscape quality for medical staff. Build. Environ. 144, 532–541. doi:10.1016/j.buildenv.2018.08.023
Iqualityair (2024). The Reality of air pollution in Chiang mai. Available at: https://www.iqair.com/th/thailand (Accessed September 9, 2024).
Lawson, B. (2010). Healing architecture, Arts and Health, 2 (2), 95–108. doi:10.1080/17533010903488517
Lehane, E., Leahy-Warren, P., O'Riordan, C., Savage, E., Drennan, J., O'Tuathaigh, C., et al. (2019). Evidence-based practice education for healthcare professions: an expert view. BMJ evidence-based Med. 24 (3), 103–108. doi:10.1136/bmjebm-2018-111019
Montgomery, A., Lainidi, O., Johnson, J., Creese, J., Baathe, F., Baban, A., et al. (2022). Employee silence in health care: charting new avenues for leadership and management. Health Care Manag. Rev. 48, 52–60. Publish Ahead of Print. doi:10.1097/hmr.0000000000000349
Pan American Health Organization (2020). PAHO. Available at: https://www.paho.org/en/documents/smart-hospital-save-energy-lighting-flyer (Accessed October 20, 2023).
Rao, S. K. M. (2004). Designing hospital for better infection control: an experience. Med. J. Armed Forces India 60, 63–66. doi:10.1016/s0377-1237(04)80163-1
Saaty, T. L. (1990). How to make a decision: the analytic hierarchy process. Eur. J. Operational Res. 48, 9–26. doi:10.1016/0377-2217(90)90057-i
Thai Meteorological Department (2024). Thailand temperature forecast. Available at: https://www.tmd.go.th/forecast/daily/070420240000 (Accessed April 6, 2024).
The Center for Health Design (2015). Clinic design post-occupancy evaluation toolkit. Available at: https://www.healthdesign.org/insights-solutions/clinic-design-post-occupancy-evaluation-toolkit-pdf-version (Accessed May 10, 2024).
Total Alliance Health Partners International (TAHPI) (2017). International health facility guidelines. Available at: https://www.healthfacilityguidelines.com/ViewPDF/ViewIndexPDF/iHFG_part_b_complete (Accessed June 9, 2024).
Ulrich, R. S., Zimring, C., Quan, X., Joseph, A., and Choudhary, R. (2004) The role of the physical environment in the hospital of the 21st century: a once-in-a-lifetime opportunity, 5. Concord, California, USA: The Center for Health Design, 1–69.
U.S. EPA (U.S. Environmental Protection Agency) (1978). Information on levels of environmental noise requisite to protect public health and welfare with an adequate margin of safety. Available at: http://www.nonoise.org/library/levels74/levels74.htm (Accessed September 11, 2023).
Waroonkun, T., and Prugsiganont, S. (2022). Preventing the spread of COVID-19 through environmental design in Thai community hospitals. Front. Built Environ. 8. doi:10.3389/fbuil.2022.947211
World Health Organization (WHO). (2010). Noise. Available at: https://www.who.int/europe/news-room/fact-sheets/item/noise (Accessed September 9, 2023).
World Health Organization (WHO). (2022). Cleaning and disinfection of environmental surfaces in the context of COVID-19. Available at: https://www.who.int/publications/i/item/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19 (Accessed May 15, 2024).
Keywords: medical staff, environment, involvement, stress reduction, outpatient clinic
Citation: Waroonkun T, Wejaphikul K, van der Hoeven S, Chotirat J and Pittayaporn N (2025) Identifying stress reduction factors in built environment through medical staff involvement . Front. Built Environ. 10:1473560. doi: 10.3389/fbuil.2024.1473560
Received: 31 July 2024; Accepted: 30 October 2024;
Published: 07 January 2025.
Edited by:
Ilaria Pigliautile, Università degli Studi di Perugia, ItalyReviewed by:
Hasim Altan, Prince Mohammad bin Fahd University, Saudi ArabiaVeronica Martins Gnecco, University of Perugia, Italy
Copyright © 2025 Waroonkun, Prugsiganont van der Hoeven, Wejaphikul, Chotirat and Pittayaporn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Supuck Prugsiganont van der Hoeven, c3VwdWNrLnBAY211LmFjLnRo
 Tanut Waroonkun
Tanut Waroonkun Karn Wejaphikul
Karn Wejaphikul Supuck van der Hoeven
Supuck van der Hoeven Jutamat Chotirat
Jutamat Chotirat Nitchakarn Pittayaporn
Nitchakarn Pittayaporn