- 1School of Athletic Performance, Shanghai University of Sport, Shanghai, China
- 2Sports Nutrition Center, National Institute of Sports Medicine, Beijing, China
- 3College of Sports and Health, Shandong Sport University, Jinan, China
- 4Sports Science Research Institute of the State Sports General Administration, Beijing, China
Objectives: To explore the acute intervention effects of tissue flossing on chronic knee pain (CKP) in boxers.
Methods: Eighteen boxers with CKP (12 male/6 female) were randomly divided into an experimental group (EG) with tissue flossing (n = 9) and a control group (CG) (n = 9). The visual analog scale (VAS), Lysholm knee function score, flexion range of motion (ROM), maximal isometric extensor muscle strength, and stability of the knee were measured pre- and post-intervention (EG: 3-minute tissue flossing, CG: rest).
Results: VAS (F = 15.849, p = 0.001, η2p = 0.498) and Lysholm knee function (F = 9.327, p = 0.008, η2p = 0.357) significantly improved more in the EG than in the CG. There was a significant difference for maximal isometric extensor muscle strength (F = 17.769, p = 0.001, η2p = 0.542) and knee stability (F = 13.844, p = 0.002, η2p = 0.464) but no significant difference for ROM (F = 1.218, p = 0.287, η2p = 0.075) between the EG and CG.
Conclusion: Tissue flossing can reduce knee pain, improve knee function, increase knee extensor strength, and improve knee stability in boxers with CKP.
1 Introduction
Boxing is an activity prone to injury. During boxing competitions, the incidence rate of lower extremity injuries among boxers is 1,220 per 1,000 h (Zhou et al., 2022). Boxers may also suffer such injuries due to overuse, amounting to 21.6% of total injuries (Zhou et al., 2022). A study by the British boxing team showed that knee injuries (any musculoskeletal condition that prevented the boxer from participating in either training or competition for >24 h) accounted for 25% of all injuries in boxers (Loosemore et al., 2015). Therefore, knee injuries are quite common in boxers and thus require attention from researchers.
The main factor associated with knee injuries in boxers is incorrect knee movement patterns (Wilczyński et al., 2020), including technical movements specific to boxing and incorrect squat techniques (Duong et al., 2023). For example, jabs and crosses are two scoring techniques that require a boxer’s knee to be in an internal rotation position, adding an additional load to the knee. Repeated practice in this specific position leads to an increased risk of injury to the knee joint (Duong et al., 2023). Specifically, the knee abduction moment increases with greater knee internal rotation (Wang et al., 2022). An elevated knee abduction moment is associated with a higher risk of anterior cruciate ligament injury (Ekdahl et al., 2024) and increased tibiofemoral cartilage contact pressure (Erbulut et al., 2021), which can contribute to the development of overuse injuries such as early osteoarthritis (Pache et al., 2018). Squats are commonly employed to enhance lower extremity strength in boxers (Escamilla, 2001), which can increase the power of their punches through kinetic chains (Zhou et al., 2022). A correlation between the maximal isometric strength in half-squat position and the effectiveness of jabs (r = 0.68) and the crosses (r = 0.83) was reported in boxing (Zhou et al., 2022). However, athletes often exhibit incorrect techniques when performing squats, such as the knee in an internal rotation position or knee-dominated squats, which increase the risk of knee injuries (Duong et al., 2023). The average recovery time that can attend training after knee damage in boxers was reported to be 21 days (Loosemore et al., 2015). Due to the continuous and long-term nature of training, athletes frequently do not receive adequate rest and treatment following injuries, leading to the development of chronic knee pain (CKP).
CKP refers to knee pain lasting more than 3 months (Zhang et al., 2017). This pain is primarily a manifestation of damage to the structures within the knee, usually accompanied by decreases in the level of knee function (Ventura et al., 2018), such as limited range of motion (ROM), reduced muscle strength around the knee, and decreased joint stability. Tissue flossing—otherwise known as voodoo band or floss band—is a natural rubber tape strip with a certain thickness and excellent elasticity (Wu et al., 2022). It features low allergic reactions and ultra-strong elasticity characteristics. Currently, it is commonly used in the field of rehabilitation and is considered a novel tool for treatment (Driller and Overmayer, 2017b; Driller et al., 2017a; Marco A. et al., 2020; Wienke et al., 2020; Wu et al., 2022). Tissue flossing applies pressure to joints and muscles, which enhances joint function (e.g., ROM) (Wu et al., 2022), improves muscle function (e.g., muscle strength) (Kaneda et al., 2019), and promotes recovery (e.g., relieving knee pain) (Marco A. et al., 2020). The only existing study on the therapeutic effects of tissue flossing found that an acute intervention significantly improved knee pain in individuals with patellofemoral pain syndrome (Marco A. et al., 2020). However, this was a pilot study involving only five amateur athletes and utilized a crossover study design (Marco A. et al., 2020). The effect produced by tissue flossing can last at least 20 min (Wu et al., 2022). For boxers engaged in 3-round, 3-minute competitions with 1-minute breaks in between, totaling 11 min, tissue flossing might help alleviate pain during competition or training and potentially enhance performance. Therefore, we decided to implement tissue flossing for boxers with CKP. The main mechanisms include fascial shear (Stecco et al., 2013), pain gate control (Moayedi and Davis, 2013), and blood flow restriction and reperfusion (Reeves et al., 2006; Hughes et al., 2017). The pressure exerted by tissue flossing on joints and muscles is in the form of shear forces (Stecco et al., 2013), which can loosen adhesion in muscle tissues and reduce the viscosity of hyaluronic acid to restore lubricating effects, thereby increasing joint mobility (Stecco et al., 2013). It also stimulates large myelinated nerve fibers (type Ⅰ afferent neurons), which generate nerve impulses that inhibit the transmission of pain signals, thereby reducing the sensation of pain (Moayedi and Davis, 2013). Simultaneously, the pressure generated by the tissue flossing restricts the blood flow to the joint, muscles, and tissue, causing muscles to temporarily enter an anaerobic state and altering the metabolic type of the muscle (Reeves et al., 2006; Hughes et al., 2017). Upon the removal of the fascial compression band, there is a substantial influx of blood, which creates a reperfusion effect. This enhances vasodilation, eliminates muscle tissue waste, and nourishes the muscles, thereby improving muscle contraction efficiency (Reeves et al., 2006; Hughes et al., 2017).
At present, few studies have explored the effect of tissue flossing at different pressure values on warm-up or treatment. Galis et al. applied 150 mmHg as the low pressure and 200 mmHg as the high pressure during a tissue flossing intervention, finding significant improvement in ankle dorsiflexion only at the lower pressure (Galis and Cooper, 2022). Therefore, controlling the pressure value of the tissue flossing at 150 mmHg may produce a positive treatment effect. The recommended duration for tissue flossing is 1–3 min (Konrad et al., 2021). One-minute tissue flossing has been proven to improve countermovement jump and relieve pain (Marco A. et al., 2020). However, this research was conducted among amateur athletes (Marco A. et al., 2020), and a 1-minute intervention may not yield the same effect on professional athletes. Two minutes of tissue flossing have been shown to significantly improve hamstring flexibility without notably enhancing jump power (Maust et al., 2021). In contrast, 3 minutes of tissue flossing not only improves hamstring flexibility, but also enhances landing stabilization (Wu et al., 2022). More importantly, this study found that the effects (improved hamstring flexibility and landing stabilization) of a 3-minute tissue flossing last for at least 20 min (Wu et al., 2022), well exceeding the 11-minute duration of a boxing competition. Therefore, a 3- minute tissue flossing intervention was selected for the present study.
As a rehabilitation approach to improve CKP symptoms, the tissue flossing may provide an efficient therapeutic method for boxers with CKP, as well as other athletes who engaged in lower-extremity-demanding sports. Currently, there has been no research examining the immediate effects of applying tissue flossing in boxers with CKP. Therefore, this study aims to investigate the acute effects of tissue flossing on boxers suffering from CKP. It is hypothesized that immediately following a 3-minute tissue flossing intervention, boxers with CKP can exhibit significant improvements in knee pain, function, ROM, muscle strength, and stability.
2 Materials and methods
2.1 Participants
2.1.1 Sample size calculation
G*Power was designed as a general stand-alone power analysis program for statistical tests commonly used in social and behavioral research (Faul et al., 2007). It provides improved effect size calculators and graphic options, supports both distribution-based and design-based input modes, and offers all types of power analyses (Faul et al., 2007). G*Power 3.1 was utilized for the sample size calculation with a repeated measures ANOVA (within–between interaction). The primary outcome VAS score (the mean ± standard deviation of the VAS score: pre-intervention for experimental group (EG) and control group (CG) - 3.4 ± 1.3 vs. 4.5 ± 2.6; post-intervention for EG, and CG- 2.1 ± 0.8 vs. 4.6 ± 3.0) in the pilot study was utilized for the effect size calculation in SPSS 26.0 (IBM, United States) with two-way repeated-measures ANOVAs, and the result showed that the effect size η2p was 0.435. A minimal sample size of seven participants per group was calculated based on this effect size and a power of 0.8. Considering a 20% attrition rate (Regnaux et al., 2015; Ventura et al., 2018), nine participants for each group were required.
2.1.2 Randomization
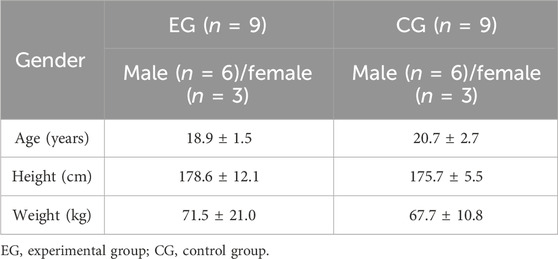
Participant recruitment was completed by the enrollment of 18 boxers with CKP from provincial boxing teams. Participants were assigned numbers: female boxers drew numbers 1 to 6, while male boxers drew numbers 7 to 18. Odd-numbered participants were assigned to the tissue flossing group (EG; n = 9), and even-numbered participants were assigned to the control group (CG; n = 9). The intervention and testing were conducted separated for each participant to ensure single blinding. The demographic information of the participants is shown in Table 1.
2.1.3 Inclusion and exclusion criteria
The inclusion criteria of the participants were as follows: (1) CKP patients: a visual analog scale (VAS) score of 3 points or greater experienced during training in the past month, and knee pain that has persisted for more than 3 months (Hott et al., 2015; Zhang et al., 2017; Ventura et al., 2018); (2) active professional boxers of grade II (based on the Chinese National Athletes Grading System) or above, regardless of gender; (3) aged between 18 and 24 years; and (4) no intake of medications affecting muscle performance (e.g., muscle relaxants) within the past 3 months. Inclusion criteria were designed to limit the participants to a typical boxing population in China who often suffer CKP.
Participants who (1) had experienced new injuries within the past 3 months; (2) had a history of ligament rupture, fracture, or surgery related to the knee joint or who had prosthetic devices implanted or replaced; (3) had chronic diseases may impact overall health and quality of life, such as peripheral joint disease or heart disease; and (4) had latex allergy were excluded. The exclusion criteria were to further eliminate patients with injuries other than CKP or conditions deemed unsuitable for this study, ensuring data reliability and participants safety throughout the study.
All participants signed an informed consent form. The ethical committee of the Shanghai University of Sport approved the study prior to the initiation of testing (102772024RT045). This study was conducted in accordance with the principles of the Declaration of Helsinki.
2.2 Intervention
A blue, medium-weight version of a 2 m × 5 cm floss band (Sanctband, Perak Darul Ridzuan, Malaysia) was used for the intervention. The pressure value of the floss band was set at 150 mmHg ± 10 mmHg (Galis and Cooper, 2022), measured using a Kikuhime pressure monitoring device (HPM-KH-01, Horsens, Denmark) (Driller et al., 2017a). The device has proven to have high reliability (ICC = 0.99, CV = 1.1%) and validity (CV = 4.9%) (Mills et al., 2020).
Each participant in the EG stood with their affected knee slightly bent, and a pressure monitor was placed on the lateral condyle of the femur (Marco A. et al., 2020). The floss band was then wrapped from their tibial tuberosity upward to 5 cm above the patella on the femur, ensuring that the patella was exposed when passing over. The first wrap was applied without tension for fixation, while subsequent wraps required 50% tension, with each successive wrap overlapping the previous one by half to ensure continuity between the layers of the floss band. Participants in the EG sat quietly for 3 min with tissue flossing (Wu et al., 2022), while the participants in the CG sat quietly for 3 min without any intervention.
2.3 Measurements
The VAS score of knee pain and the Lysholm knee scoring scale were measured first. Afterwards, all the participants engaged in a 5-minute jog, followed by another 5 min of dynamic stretching (DeVita et al., 2018) for warm-up. The dynamic stretching routine included lunges (15 repetitions, 2 s per repetition, 30s/side, total 1min), lateral squats (15 repetitions, 2 s per repetition, 30 s/side, total 1 min), hamstring stretches (15 repetitions, 2 s per repetition, 30 s/side, total 1 min), butt kicks (30 s), and stationary running (30 s) (Su et al., 2017). The ROM of the knee, maximal isometric strength of the knee extensor muscles, and single-leg stance with eyes closed were evaluated (Figure 1).
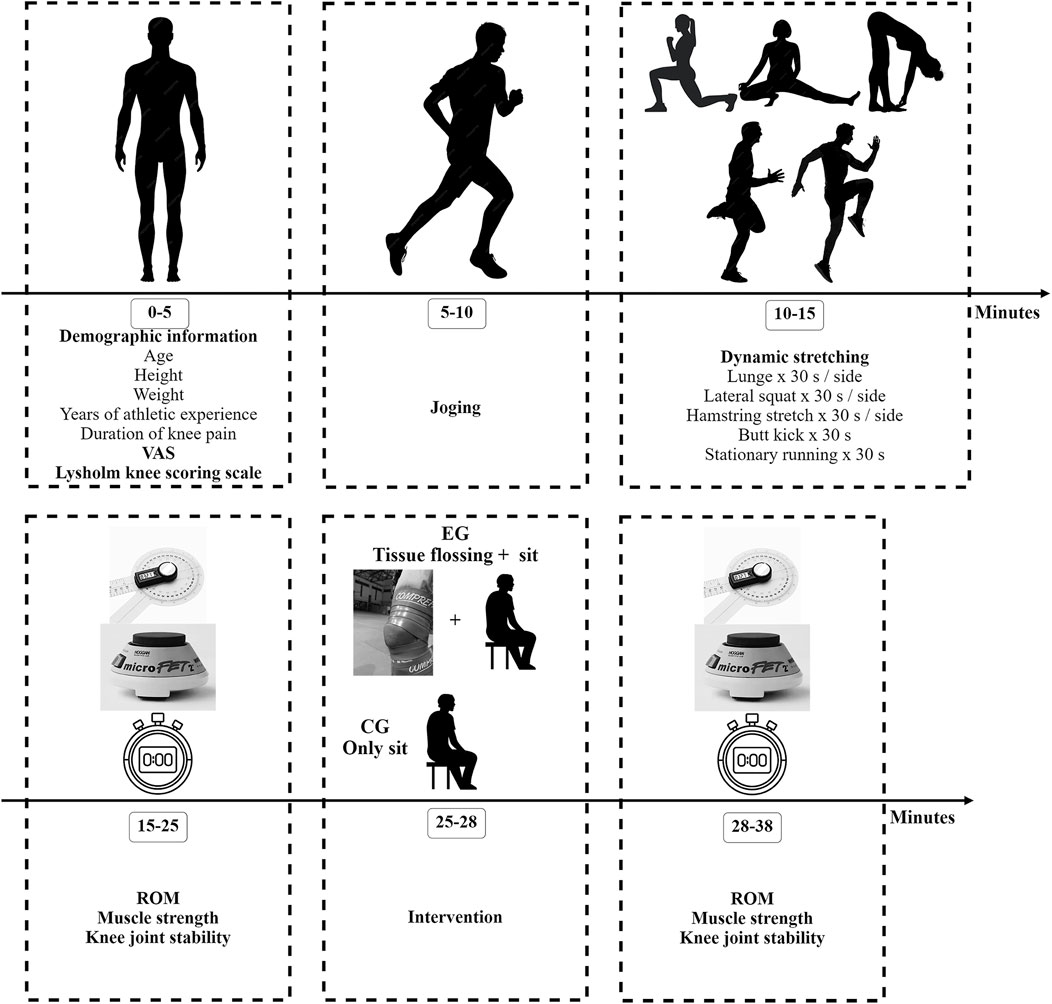
Figure 1. Study flowchart VAS, visual analogue scale; ROM, range of motion; EG, experiment group; CG, control group.
2.4 VAS score of knee pain
The VAS was used to subjectively assess the degree of knee pain. This ranged from “no pain” to “the worst imaginable pain” at the respective ends (Heller et al., 2016). Each participant marked a vertical line on the scale, and the length from the leftmost end to the mark was measured to the nearest millimeter to represent the level of pain (Heller et al., 2016). The scale has been shown to have high reliability (ICC = 0.90) and validity (CV = 7.29%) (Paungmali et al., 2012).
2.5 Lysholm knee scoring scale
The Lysholm knee scoring scale was utilized to evaluate the impact of CKP on the daily activities of the participants, who filled in the questionnaire based on their experiences. The scale consists of eight items: pain, instability, locking sensation, swelling, limping, climbing stairs, squatting, and the use of walking aids. The total score ranges from 0 to 100 points, with higher scores indicating better knee function. Scores above 95 are considered excellent, 85–94 are good, 65–84 are fair, and below 65 are poor (Briggs et al., 2009; Collins et al., 2011). The scale has demonstrated high reliability (ICC = 0.935) and acceptable internal consistency (Cronbach’s alpha = 0.726) (Wang et al., 2016).
2.6 ROM
Each participant lay prone on the examining table. The researcher placed the center of the electronic goniometer (GemRed, Guangxi Crystal Sensor Technology Co., Ltd., Guangxi, China) on the lateral condyle of the knee joint. The fixed arm was aligned parallel to the longitudinal axis of the femur, while the moving arm was aligned parallel to the line between the lateral malleolus and the head of the fibula. Upon the researcher’s command, the participant slowly flexed their knee to its maximum, at which point the researcher recorded the angle. To avoid compensatory movements, such as hip rotation, flexion, or abduction, verbal reminders were provided throughout the measurement process. Three measurements were taken with a 30-second interval between each, and the average was utilized for further analysis (Dos Santos et al., 2017).
2.7 Maximal isometric strength of the knee extensor muscles
The researcher used a hand-held dynamometer (Micro FET2, Hoggan Health Industries, Draper, USA) to measure the maximal isometric strength of the knee extensor muscles (Stark et al., 2011). The reliability of this device in strength measurement has proven to be high (ICC = 0.90) (Mentiplay et al., 2015).
Each participant sat at the edge of an examining table with both legs dangling freely, and it was ensured that the hips and knees were positioned at a 90° angle. They were required to maintain an upright torso and hold onto the edge of the examining table with both hands. The researcher stood against a wall, aligning their back with it, and placed the hand-held dynamometer on the front part of the participant’s shin near the proximal ankle joint. Upon the researcher’s command, the participant exerted maximum force against the dynamometer for 5 s. This measurement was repeated three times, with 30 s between each measurement (Martin et al., 2006). The highest value was recorded for further analysis. Throughout the testing process, the researcher provided ongoing verbal encouragement to ensure that the participants continuously maintained maximum effort (Martin et al., 2006).
2.8 Single-leg stance with eyes closed
Knee pain can change proprioceptive information (Bennell et al., 2008) and reduce proprioception (Kavchak et al., 2012), and thus impair knee stability (Bennell et al., 2008). The single-leg stance with eyes closed can reflect knee stability and proprioception without visual input (Baumann et al., 2017; Wu et al., 2022). Therefore, it was used as the measurement of knee joint stability. Each participant stood naturally with their eyes closed. Upon the researcher’s command, they lifted the unaffected leg and started being timed for the duration of their stance. The timer stopped when the supporting foot moved or the lifting foot touched the ground. The measurement was performed twice, and the better result was utilized for further analysis.
2.9 Statistical analysis
Data analysis was conducted using SPSS 26.0 (IBM, United States). The normality of the data distribution was tested using the Shapiro–Wilk test. For data meeting the normal distribution, means ± standard deviations (M ± SD) were used to present the data, while median and interquartile range M (P25, P75) were used for data that did not follow a normal distribution. The baselines were analyzed using an independent-samples t-test. If there were no significant differences at the baseline, two-way repeated-measures ANOVAs were utilized for the data analysis, which considered time (pre-intervention vs. post-intervention) and group (EG vs. CG) as factors affecting related variables (knee VAS score, Lysholm knee function score, ROM of knee, maximum isometric muscle strength of the knee extensors, and single-leg stance time with eyes closed). If there was an interaction effect between time and group, a simple effects analysis was performed. If data at the baseline were significantly different, the data were analyzed using an analysis of covariance to compare differences between the EG and CG (Hara et al., 2020). The aligned rank transform (ART) was used by ARTool 2.2.2 to transform the nonparametric data, and then two-way ANOVA was used to analyze the transformed data (Leys and Schumann, 2010; Wobbrock et al., 2011). If there was an interaction effect between time (pre-intervention vs. post-intervention) and group (EG vs. CG), a simple effects analysis was performed (Leys and Schumann, 2010; Wobbrock et al., 2011). Effect size was categorized as follows: 0 ≤ η2p < 0.05 (no effect), 0.05 ≤ η2p < 0.26 (small effect), 0.26 ≤ η2p < 0.64 (medium effect), and η2p ≥ 0.64 (large effect). Statistical significance for all data was set at a p-value of less than 0.05.
3 Results
All data fit normal distribution except single-leg stance with eyes closed. Apart from ROM and maximal isometric strength of the knee extensor muscle, the rest of the data at baseline were not significantly different (Table 2).
3.1 VAS score of knee pain
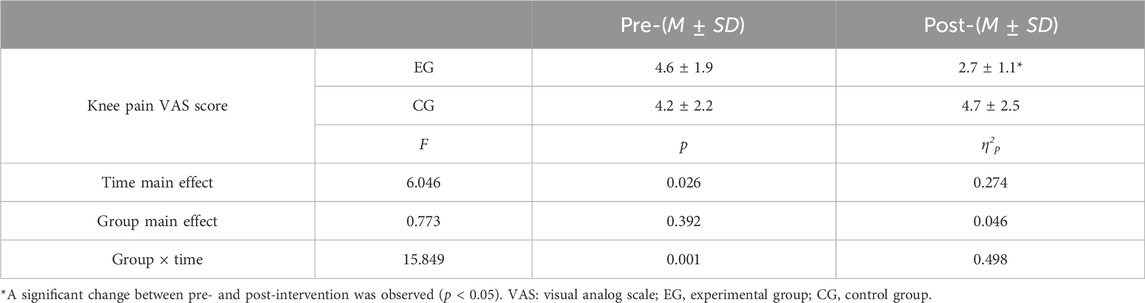
The results of the two-way repeated measures ANOVA (Table 3) indicated that there was a significant interaction between time and group for the VAS score of knee pain (F = 15.849, p = 0.001, η2p = 0.498).
The results of the simple main effect of time (F = 6.046, p = 0.026, η2p = 0.274) showed a significant decrease in VAS score of knee pain in the EG (F = 20.737, p < 0.001, η2p = 0.564) and no significant change in the VAS score of knee pain in the CG (F = 1.159, p = 0.298, η2p = 0.068) post-intervention.
3.2 Lysholm knee function score
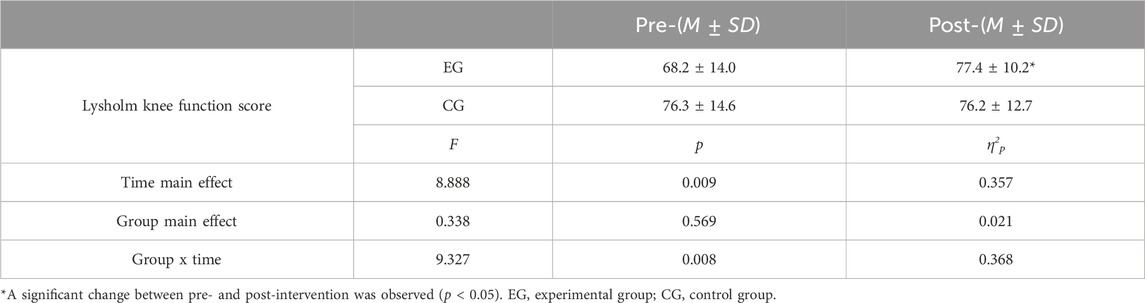
The results of the two-way repeated measures ANOVA (Table 4) indicated a significant interaction effect between time and group on the Lysholm knee function scores (F = 9.327, p = 0.008, η2p = 0.357).
The simple main effect of time (F = 8.888, p = 0.009, η2p = 0.357) revealed that the Lysholm knee function scores significantly increased following the intervention in the EG (F = 18.213, p = 0.001, η2p = 0.532), but there was no significant change in the CG (F = 0.003, p = 0.960, η2p < 0.001).
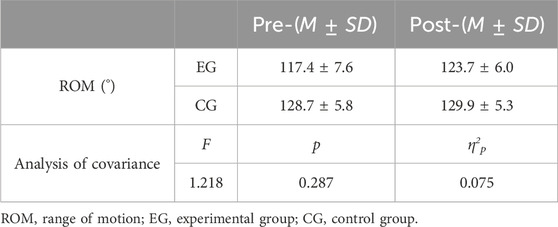
3.3 ROM
The results of the analysis of covariance showed no significant differences between the EG and CG post-intervention (F = 1.218, p = 0.287, η2p = 0.075). However, the ROM of knee flexion increased by 6.32° in the EG post-intervention (Table 5).
3.4 Maximal isometric strength of the knee extensor muscles
The results of the analysis of covariance showed a significant difference between the EG and CG post-intervention (F = 17.769, p = 0.001, η2p = 0.542) (Table 6).
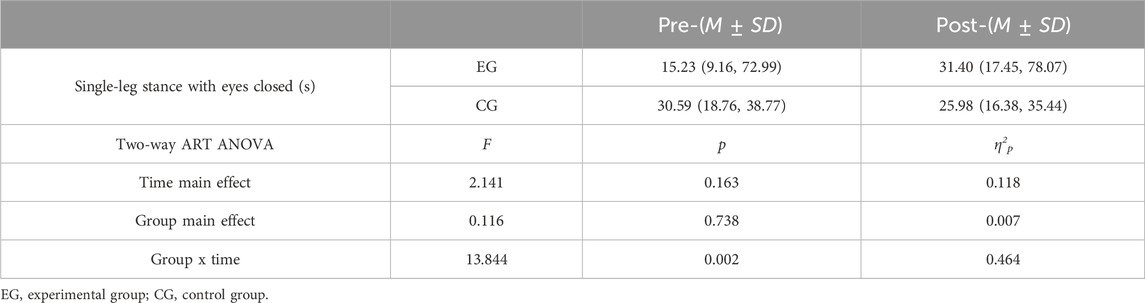
3.5 Single-leg stance with eyes closed
The results of the two-way ANOVA after ART (Table 7) indicated that there was a significant interaction between time and group for the duration of the single-leg stance with eyes closed (F = 13.844, p = 0.002, η2p = 0.464).
The results of the simple main effect of time (F = 2.141, p = 0.163, η2p = 0.118) and group (F = 0.116, p = 0.738, η2p = 0.007) both showed no significant change in the duration of the single-leg stance with eyes closed.
4 Discussion
This study investigated the acute effects of tissue flossing on boxers with CKP. Our findings indicated that, after a 3-minute tissue flossing intervention, the VAS scores for knee pain, Lysholm knee scale scores, and the maximum isometric strength of the knee extensors in EG improved significantly compared to those in CG. However, there were no significant changes in knee ROM or single-leg stance duration with eyes closed. This indicates that tissue flossing can be used as a short term and highly effective method for relieving knee pain and increasing muscle strength for CKP boxers before competitions or training.
Immediately following the tissue flossing intervention, the boxers in the EG experienced a significant improvement in knee pain compared to those in the CG. Pain is the primary symptom of CKP (Hinman et al., 2015; Terry et al., 2022), and a reduction in knee muscle strength (Cheatham, 2020) and joint ROM is also associated with pain (Yoshizuka et al., 2022). In 2020, Marco A et al. conducted a study on five male athletes with patellofemoral pain syndrome, who performed three countermovement jumps with a 15-s interval between jumps while wearing tissue flossing (Marco A. et al., 2020). Their results indicated that the athletes had a significant reduction in knee pain post-intervention, consistent with the findings of this experiment (Marco A. et al., 2020). León-Morillas et al. showed that tissue flossing combined with physiotherapy for 8 weeks can significantly decrease anterior knee pain (León-Morillas et al., 2024). A case study indicated that 9 weeks of tissue flossing intervention could significantly improve knee pain (Weber, 2018). Although the two studies did not report on acute interventions for knee pain, they can prove that tissue flossing is beneficial for knee pain (Weber, 2018). There are several possible reasons why tissue flossing significantly improves knee pain. First, according to the gate control theory of pain, the mechanical pressure exerted by tissue flossing stimulates large myelinated nerve fibers (type I afferent neurons), and generates neural impulses (Moayedi and Davis, 2013; Wu et al., 2022). These large nerve fibers inhibit the activity of the small nerve fibers responsible for transmitting pain and thus suppress pain transmission and result in pain relief (Moayedi and Davis, 2013; Wu et al., 2022). Second, local mechanical pressure may reduce the influx of inflammatory mediators, leading to a decrease in intracellular osmotic pressure and consequently reducing the inflammatory response and sensitivity of pain receptors (Prill et al., 2019; Konrad et al., 2021).
Boxers in the EG showed a significant increase in the Lysholm knee scoring scale compared to those in the CG. One study indicated that the subjects showed a significant improvement in the Lysholm knee scoring scale after both an acute and 4 weeks of instrument-assisted soft tissue mobilization therapy combined with blood flow restriction training, consistent with the results of this experiment (Liu and Wu, 2023). Although this study did not utilize tissue flossing, the working mechanism of blood flow restriction was similar to tissue flossing. The difference between the studies was the accuracy of quantification of the pressure. The significant improvement in the Lysholm knee scoring scale due to tissue flossing may have been related to pain relief. The EG had an average increase of 9.22 points on the Lysholm knee scoring scale, which was primarily due to improvement in the following three sections: pain, squatting, and climbing stairs. This suggests that the tissue flossing intervention had an immediate positive effect on improving knee function and that its mechanism of action may be through pain relief to enhance the function scores of squats and climbing stairs.
The knee extensor muscle strength of the EG significantly improved when compared to that of the CG. Kaneda et al. found that immediately after a 2-minute tissue flossing intervention, there was a significant increase in the maximum eccentric contraction strength of the knee extensors (p = 0.02) (Kaneda et al., 2019). The results of this study were consistent with ours. Similarly, Marco A et al. demonstrated that a tissue flossing intervention could immediately significantly enhance the jump height, jump power, and jump force of the subjects (Marco A. et al., 2020). Although their study did not directly measure knee muscle strength, it indirectly reflected that the muscle strength and explosive power of the lower extremities significantly increased after a tissue flossing intervention through jumping. There are also studies that have presented opposite results. Paravlic et al. found that after three consecutive 2-minute tissue flossing interventions, there were significant decreases in jump height and the contractile characteristics of the vastus lateralis muscle (muscle contraction speed, maximum displacement amplitude) of the subjects (Paravlic et al., 2022). The authors believed that the reason for this phenomenon was related to the pressure, location, duration of the tissue flossing intervention, and different combined exercises (Paravlic et al., 2022). Besides pain relief, there may be three other reasons for the significant enhancement of knee muscle strength. First, the pressure exerted by tissue flossing on the joint is similar to blood flow restriction, which reduces blood flow and causes local muscles and joints to be in a state of hypoxia and ischemia (Reeves et al., 2006; Hughes et al., 2017). In this state, type II muscle fibers are recruited more quickly, thereby increasing muscle strength (Schiaffino and Reggiani, 2011). Second, after the removal of the tissue flossing, blood will be re-perfused into the muscle tissue (Hughes et al., 2017). At this moment, nitric oxide synthase is activated, leading to an increase in nitric oxide levels (Hughes et al., 2017). Nitric oxide causes vasodilation, temporarily increases blood flow, nourishes the muscles, improves muscle contraction efficiency, and ultimately leads to an increase in muscle strength (Maiorana et al., 2003). Third, pain has an inhibitory effect on muscles, causing a decrease in knee extensor muscle strength. The degree of muscle inhibition is proportional to the level of pain (Henriksen et al., 2011). Research has shown that for every 1-mm increase in pain using VAS to evaluate pain, there is an approximately 0.4% decrease in muscle strength (Henriksen et al., 2011). The results of this study indicate that after a 3-minute tissue flossing intervention, the pain in the knee joints of boxers decreased immediately. Therefore, the degree of muscle inhibition was reduced, and knee extensor muscle strength increased accordingly.
There was no significant change in knee flexion ROM between the EG and CG post-intervention. The results of studies by Wu et al. and Cheatham et al. were not consistent with those of the current study (Wu et al., 2022; Cheatham, 2020). Wu et al. found that flossing bands combined with movements (walking knee hugs, side squats, and forward lunges; each movement repeated 10 times within 3 min) could significantly increase the ROM of the knee. Cheatham et al. conducted an intervention with tissue flossing on the thighs of healthy individuals for 2-minute active movements (standing hip flexion for 30 s, seated knee extension and flexion for 30 s, and bodyweight squats for 1 min) and found that a 2-minute application of tissue flossing could immediately significantly enhance the ROM of the knee (an average improvement of 4°) (Cheatham, 2020). The results of the differences between the current study and the other two studies may mainly have been caused by the combined movements and the duration of the interventions. However, the current study demonstrated that ROM increased by 6.32° after the tissue flossing intervention. There were two possible reasons why the ROM of the knee was increased. First, it may be related to the relief of pain (Yoshizuka et al., 2022). Patients often adopt a strategy of immobilization to recover when they experience knee pain, and prolonged immobilization can lead to tissue adhesions around the knee joint, resulting in decreased joint ROM. Additionally, the enhancement of joint ROM may be related to the shear forces generated by tissue flossing. The mechanical pressure applied by tissue flossing creates significant shear forces between different tissues, such as the epimysium, perimysium, and endomysium (Stecco et al., 2013). These shear forces facilitate the loosening of adhesive points and restore the lubricating action of hyaluronic acid, thereby contributing to an increase in joint ROM (Stecco et al., 2013).
EG exhibited better knee stability when compared to CG after the intervention. This suggests that acute tissue flossing can markedly improve proprioception and knee stability. Wu et al. (2022) reported no significant differences in single-leg standing (with eyes open or closed) or landing stability among participants immediately following an intervention using tissue flossing, a result that contrasts with the findings of this study. The main reason for the opposing results is that Wu et al. limited the maximum measurement time for single-leg standing time with eyes closed or open to 30 s, whereas the present study imposed no such restriction. The findings of the present study suggest two key factors contributing to the significant improvement in knee stability. First, the reduction in knee pain can directly enhance knee stability. One study indicates that pain triggers the release of inflammatory chemicals that sensitize nerve terminals, leading to abnormal firing of afferent nerve impulses, particularly from small-diameter pain-related nerves and large-diameter proprioceptive nerves (Prabhakar et al., 2023). This abnormal firing compromises knee stability. However, as pain decreases, this process is mitigated, thereby enhancing knee stability (Prabhakar et al., 2023). Second, the quadriceps muscles serve as dynamic stabilizer of the knee joint (Chang et al., 2021), and increased quadriceps muscle strength contributes to enhanced knee stability. Thus, the observed improvement in knee stability could be explained by the enhanced relative strength of the knee extensor muscles following the tissue flossing intervention.
In practice, the tissue flossing provides boxers with CKP a short-term, highly effective method for relieving knee pain, improving knee function, enhancing muscle strength and knee stability. Moreover, since this intervention does not require combination with other exercises, boxers with CKP can use it as an acute treatment before training or competitions.
5 Conclusion
Apart from ROM, applying tissue flossing for 3 min to boxers with CKP significantly alleviated knee pain and improved knee function scores, muscular strength and knee stability. The findings of this study can be applied to immediately relieve CKP symptoms in boxers and to offer an additional treatment option for athletes with CKP.
6 Limitation
In this study, we did not investigate the duration of the intervention effects or the trend of changes in various variables following immediate intervention. This can be explored further in future research.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Jie, Chen; Wang, Dan (2024), “Acute Effects of Tissue Flossing on Boxers with Chronic Knee”, Mendeley Data, V1, doi: 10.17632/n46pws4vnb.1.
Ethics statement
The studies involving humans were approved by The ethical committee of the Shanghai University of Sport. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing–original draft, Writing–review and editing. QW: Visualization, Writing–review and editing. ZZ: Validation, Writing–review and editing. QS: Supervision, Writing–review and editing. PZ: Writing–review and editing. DW: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the program for Overseas High-Level Talents at Shanghai Institutions of Higher Learning [grant numbers TP2019072]; the China National Sports General Administration’s Weightlifting, Wrestling, and Judo Management Center [grant number 2023AY012 and 2022AY009], and the Shanghai Key Lab of Human Performance (Shanghai University of sport) [grant number 11DZ2261100].
Acknowledgments
A profound note of gratitude to DW, whose invaluable guidance and support were instrumental in the success of this research endeavor.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Baumann, F., Bahadin, Ö., Krutsch, W., Zellner, J., Nerlich, M., Angele, P., et al. (2017). Proprioception after bicruciate-retaining total knee arthroplasty is comparable to unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 25, 1697–1704. doi:10.1007/s00167-016-4121-2
Bennell, K. L., Hunt, M. A., Wrigley, T. V., Lim, B.-W., and Hinman, R. S. (2008). Role of muscle in the genesis and management of knee osteoarthritis. Rheum. Dis. Clin. North Am. 34 (3), 731–754. doi:10.1016/j.rdc.2008.05.005
Briggs, K. K., Steadman, J. R., Hay, C. J., and Hines, S. L. (2009). Lysholm score and tegner activity level in individuals with normal knees. Am. J. Sports Med. 37, 898–901. doi:10.1177/0363546508330149
Chang, N.-J., Hung, W.-C., Lee, C.-L., Chang, W.-D., and Wu, B.-H. (2021). Effects of a single session of floss band intervention on flexibility of thigh, knee joint proprioception, muscle force output, and dynamic balance in young adults. Appl. Sci. 11, 12052. doi:10.3390/app112412052
Cheatham, S. (2020). Myofascial compression interventions: comparison of roller massage, instrument assisted soft-tissue mobilization, and floss band on passive knee motion among inexperienced individuals. Clin. Prac. Athl. Train. 3. doi:10.31622/2020/0003.3.5
Collins, N. J., Misra, D., Felson, D. T., Crossley, K. M., and Roos, E. M. (2011). Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-ps), knee outcome survey activities of daily living scale (KOS-adl), lysholm knee scoring scale, oxford knee score (OKS), western ontario and McMaster universities osteoarthritis index (WOMAC), activity rating scale (ARS), and tegner activity score (TAS). Arthritis Care Res. 63, S208–S228. doi:10.1002/acr.20632
DeVita, P., Aaboe, J., Bartholdy, C., Leonardis, J. M., Bliddal, H., and Henriksen, M. (2018). Quadriceps-strengthening exercise and quadriceps and knee biomechanics during walking in knee osteoarthritis: a two-centre randomized controlled trial. Clin. Biomech. 59, 199–206. doi:10.1016/j.clinbiomech.2018.09.016
Dos Santos, R. A., Derhon, V., Brandalize, M., Brandalize, D., and Rossi, L. P. (2017). Evaluation of knee range of motion: correlation between measurements using a universal goniometer and a smartphone goniometric application. J. Bodyw. Mov. Ther. 21, 699–703. doi:10.1016/j.jbmt.2016.11.008
Driller, M., Mackay, K., Mills, B., and Tavares, F. (2017a). Tissue flossing on ankle range of motion, jump and sprint performance: a follow-up study. Phys. Ther. Sport 28, 29–33. doi:10.1016/j.ptsp.2017.08.081
Driller, M. W., and Overmayer, R. G. (2017b). The effects of tissue flossing on ankle range of motion and jump performance. Phys. Ther. Sport 25, 20–24. doi:10.1016/j.ptsp.2016.12.004
Duong, V., Oo, W. M., Ding, C., Culvenor, A. G., and Hunter, D. J. (2023). Evaluation and treatment of knee pain: a review. JAMA 330, 1568. doi:10.1001/jama.2023.19675
Ekdahl, M., Ulman, S., and Butler, L. (2024). Relationship of knee abduction moment to trunk and lower extremity segment acceleration during sport-specific movements. Sensors 24 (5), 1454. doi:10.3390/s24051454
Erbulut, D. U., Sadeqi, S., Summers, R., and Goel, V. K. (2021). Tibiofemoral cartilage contact pressures in athletes during landing: a dynamic finite element study. Journal of Biomechanical Engineering. J. Biomech. Eng. 143 (10), 101006. doi:10.1115/1.4051231
Escamilla, R. F. (2001). Knee biomechanics of the dynamic squat exercise. Med. Sci. Sports Exerc 33, 127–141. doi:10.1097/00005768-200101000-00020
Faul, F., Erdfelder, E., Lang, A.-G., and Buchner, A. (2007). G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39 (2), 175–191. doi:10.3758/bf03193146
Galis, J., and Cooper, D. J. (2022). Application of a floss band at differing pressure levels: effects at the ankle joint. J. Strength Cond. Res. 36, 2454–2460. doi:10.1519/JSC.0000000000003833
Hara, E. S., Witzel, A. L., Minakuchi, H., De Pitta, C. E., Gallo, R. T., Okada, M., et al. (2020). Vibratory splint therapy for decreasing sleep clenching: a pilot study. CRANIO® 38, 15–21. doi:10.1080/08869634.2018.1488652
Heller, G. Z., Manuguerra, M., and Chow, R. (2016). How to analyze the visual analogue scale: myths, truths and clinical relevance. Scand. J. Pain 13, 67–75. doi:10.1016/j.sjpain.2016.06.012
Henriksen, M., Rosager, S., Aaboe, J., Graven-Nielsen, T., and Bliddal, H. (2011). Experimental knee pain reduces muscle strength. J. Pain 12, 460–467. doi:10.1016/j.jpain.2010.10.004
Hinman, R., McCrory, P., Pirotta, M., Relf, I., Forbes, A., Crossley, K., et al. (2015). Acupuncture for chronic knee pain: a randomized clinical trial. JAMA 58, 27–29. doi:10.1016/S0415-6412(15)30009-6
Hott, A., Liavaag, S., Juel, N. G., and Brox, J. I. (2015). Study protocol: a randomised controlled trial comparing the long term effects of isolated hip strengthening, quadriceps-based training and free physical activity for patellofemoral pain syndrome (anterior knee pain). BMC Musculoskelet. Disord. 16, 40. doi:10.1186/s12891-015-0493-6
Hughes, L., Paton, B., Rosenblatt, B., Gissane, C., and Patterson, S. D. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br. J. Sports Med. 51, 1003–1011. doi:10.1136/bjsports-2016-097071
Kaneda, H., Takahira, N., Tsuda, K., Tozaki, K., Kudo, S., Sasaki, S., et al. (2019). Effects of tissue flossing and dynamic stretching on hamstring muscles function. J. Sports Sci. Med. 19, 681–689. Available at: https://pubmed.ncbi.nlm.nih.gov/33239941.
Kavchak, A. J. E., Fernández-de-las-Peñas, C., Rubin, L. H., Arendt-Nielsen, L., Chmell, S. J., Durr, R. K., et al. (2012). Association between altered somatosensation, pain, and knee stability in patients with severe knee osteoarthrosis. Clin. J. Pain 28, 589–594. doi:10.1097/AJP.0b013e31823ae18f
Konrad, A., Močnik, R., and Nakamura, M. (2021). Effects of tissue flossing on the healthy and impaired musculoskeletal system: a scoping review. Front. Physiol. 12, 666129. doi:10.3389/fphys.2021.666129
León-Morillas, F., García-Marín, M., Corujo-Hernández, C., Martín Alemán, M., Castellote-Caballero, Y., Cahalin, L. P., et al. (2024). Evaluating the impact of flossing band integration in conventional physiotherapy for patellofemoral pain syndrome. JCM 13, 2958. doi:10.3390/jcm13102958
Leys, C., and Schumann, S. (2010). A nonparametric method to analyze interactions: the adjusted rank transform test. J. Exp. Soc. Psychol. 46, 684–688. doi:10.1016/j.jesp.2010.02.007
Liu, Y., and Wu, L. (2023). Effect of instrument-assisted soft tissue mobilization combined with blood flow restriction training on function, pain and strength of patients with patellofemoral joint pain. BMC Musculoskelet. Disord. 24, 698. doi:10.1186/s12891-023-06701-6
Loosemore, M., Lightfoot, J., Palmer-Green, D., Gatt, I., Bilzon, J., and Beardsley, C. (2015). Boxing injury epidemiology in the Great Britain team: a 5-year surveillance study of medically diagnosed injury incidence and outcome. Br. J. Sports Med. 49, 1100–1107. doi:10.1136/bjsports-2015-094755
Maiorana, A., O'Driscoll, G., Taylor, R., and Green, D. (2003). Exercise and the nitric oxide vasodilator system. Sports Med. 33, 1013–1035. doi:10.2165/00007256-200333140-00001
Marco, A. G.-L., Juan, M. C.-T., Julián, G.-M., and Miguel, G.-J. (2020). The effects of tissue flossing on perceived knee pain and jump performance: a pilot study. Int J Hum Mov Sports Sci 8, 63–68. doi:10.13189/saj.2020.080203
Martin, H. J., Yule, V., Syddall, H. E., Dennison, E. M., Cooper, C., and Aihie Sayer, A. (2006). Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? a comparison with the gold standard biodex dynamometry. Gerontology 52, 154–159. doi:10.1159/000091824
Maust, Z., Bradney, D., Collins, S. M., Wesley, C., and Bowman, T. G. (2021). The effects of soft tissue flossing on hamstring range of motion and lower extremity power. Int. J. Sports Phys. Ther. 16, 689–694. doi:10.26603/001c.24144
Mentiplay, B. F., Perraton, L. G., Bower, K. J., Adair, B., Pua, Y.-H., Williams, G. P., et al. (2015). Assessment of lower limb muscle strength and power using hand-held and fixed dynamometry: a reliability and validity study. PLoS One 10, e0140822. doi:10.1371/journal.pone.0140822
Mills, B., Mayo, B., Tavares, F., and Driller, M. (2020). The effect of tissue flossing on ankle range of motion, jump, and sprint performance in elite rugby union athletes. J. Sport Rehabil. 29, 282–286. doi:10.1123/jsr.2018-0302
Moayedi, M., and Davis, K. D. (2013). Theories of pain: from specificity to gate control. J. Neurophysiol. 109, 5–12. doi:10.1152/jn.00457.2012
Pache, S., Aman, Z. S., Kennedy, M., Nakama, G. Y., Moatshe, G., Ziegler, C., et al. (2018). Meniscal root tears: current concepts review. Arch. Bone Jt. Surg. 6 (4), 250–259.
Paravlic, A. H., Segula, J., Drole, K., Hadzic, V., Pajek, M., and Vodicar, J. (2022). Tissue flossing around the thigh does not provide acute enhancement of neuromuscular function. Front. Physiol. 13, 870498. doi:10.3389/fphys.2022.870498
Paungmali, A., Sitilertpisan, P., Taneyhill, K., Pirunsan, U., and Uthaikhup, S. (2012). Intrarater reliability of pain intensity, tissue blood flow, thermal pain threshold, pressure pain threshold and lumbo-pelvic stability tests in subjects with low back pain. Asian J. Sports Med. 3, 8–14. doi:10.5812/asjsm.34718
Prabhakar, A. J., Joshua, A. M., Prabhu, S., and Kamat, Y. D. (2023). Effectiveness of balance training on pain and functional outcomes in knee osteoarthritis: a systematic review and meta-analysis. F1000Res 13 (11)–598. doi:10.12688/f1000research.111998.2
Prill, R., Schulz, R., and Michel, S. (2019). Tissue flossing: a new short-term compression therapy for reducing exercise-induced delayed-onset muscle soreness. a randomized, controlled and double-blind pilot crossover trial. J. Sports Med. Phys. Fit. 59, 861–867. doi:10.23736/S0022-4707.18.08701-7
Reeves, G. V., Kraemer, R. R., Hollander, D. B., Clavier, J., Thomas, C., Francois, M., et al. (2006). Comparison of hormone responses following light resistance exercise with partial vascular occlusion and moderately difficult resistance exercise without occlusion. J. Appl. Physiol. 101, 1616–1622. doi:10.1152/japplphysiol.00440.2006
Regnaux, J., Lefevre-Colau, M., Trinquart, L., Nguyen, C., Boutron, I., Brosseau, L., et al. (2015). High-intensity versus low-intensity physical activity or exercise in people with hip or knee osteoarthritis. Cochrane Database Syst. Rev. 29 (10), 2015. doi:10.1002/14651858.CD010203.pub2
Schiaffino, S., and Reggiani, C. (2011). Fiber types in mammalian skeletal muscles. Physiol. Rev. 91, 1447–1531. doi:10.1152/physrev.00031.2010
Stark, T., Walker, B., Phillips, J. K., Fejer, R., and Beck, R. (2011). Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM&R 3, 472–479. doi:10.1016/j.pmrj.2010.10.025
Stecco, A., Gesi, M., Stecco, C., and Stern, R. (2013). Fascial components of the myofascial pain syndrome. Curr. Pain Headache Rep. 17, 352. doi:10.1007/s11916-013-0352-9
Su, H., Chang, N.-J., Wu, W.-L., Guo, L.-Y., and Chu, I.-H. (2017). Acute effects of foam rolling, static stretching, and dynamic stretching during warm-ups on muscular flexibility and strength in young adults. J. Sport Rehabil. 26, 469–477. doi:10.1123/jsr.2016-0102
Terry, E. L., Tanner, J. J., Cardoso, J. S., Sibille, K. T., Lai, S., Deshpande, H., et al. (2022). Associations between pain catastrophizing and resting-state functional brain connectivity: ethnic/race group differences in persons with chronic knee pain. J Neurosci. Res. 100, 1047–1062. doi:10.1002/jnr.25018
Ventura, J., Sobczak, J., and Chung, J. (2018). The chronic knee pain program: a self-management model. Int. J. Orthop. Trauma Nurs. 29, 10–15. doi:10.1016/j.ijotn.2018.01.001
Wang, C., Yang, G., Yang, H., Chen, C., Zhang, H., Wang, K., et al. (2022). Research on knee joint load and influencing factors of typical tai chi movements. Appl. Bionics Biomech. 8, 1–11. doi:10.1155/2022/6774980
Wang, W., Liu, L., Chang, X., Jia, Z. Y., Zhao, J. Z., and Xu, W. D. (2016). Cross-cultural translation of the lysholm knee score in Chinese and its validation in patients with anterior cruciate ligament injury. BMC Musculoskelet. Disord. 17, 436. doi:10.1186/s12891-016-1283-5
Weber, P. (2018). Flossing: an alternative treatment approach to Osgood-Schlatter’s disease: case report of an adolescent soccer player. J. Bodyw. Mov. Ther. 22, 860–861. doi:10.1016/j.jbmt.2018.09.043
Wienke, A. K., Thiel, C., and Kopkow, C. (2020). Effekte von medical flossing bei patienten mit schulterbeschwerden – randomisierte kontrollierte pilotstudie. physioscience 16, 5–15. (In German: English abstract). doi:10.1055/a-1078-6882
Wilczyński, B., Zorena, K., and Ślęzak, D. (2020). Dynamic knee valgus in single-leg movement tasks. Potentially modifiable factors and exercise training options. a literature review. IJERPH 17, 8208. doi:10.3390/ijerph17218208
Wobbrock, J. O., Findlater, L., Gergle, D., and Higgins, J. J. (2011). The aligned rank transform for nonparametric factorial analyses using only anova procedures. ACM, 143–146. doi:10.1145/1978942.1978963
Wu, S.-Y., Tsai, Y.-H., Wang, Y.-T., Chang, W.-D., Lee, C.-L., Kuo, C.-E. A., et al. (2022). Acute effects of tissue flossing coupled with functional movements on knee range of motion, static balance, in single-leg hop distance, and landing stabilization performance in female college students. IJERPH 19, 1427. doi:10.3390/ijerph19031427
Yoshizuka, H., Taniguchi, T., Fukuta, K., Mitsutake, T., and Honda, S. (2022). Decrease in medial meniscal extrusion after physical therapy to improve knee pain and range of motion in patients with knee osteoarthritis: a retrospective study. PLoS One 17, e0277628. doi:10.1371/journal.pone.0277628
Zhang, Q., Yue, J., Golianu, B., Sun, Z., and Lu, Y. (2017). Updated systematic review and meta-analysis of acupuncture for chronic knee pain. Acupunct. Med. 35, 392–403. doi:10.1136/acupmed-2016-011306
Keywords: voodoo flossband, blood flow restriction, knee joint, pain, muscle strength
Citation: Chen J, Wang Q, Zhao Z, Song Q, Zhao P and Wang D (2025) Acute effects of tissue flossing on boxers with chronic knee pain. Front. Bioeng. Biotechnol. 12:1508054. doi: 10.3389/fbioe.2024.1508054
Received: 08 October 2024; Accepted: 17 December 2024;
Published: 14 January 2025.
Edited by:
Houyi Sun, Shandong University, ChinaReviewed by:
Chi-Wen Lung, University of Illinois at Urbana-Champaign, United StatesAllan Fu, The University of Sydney, Australia
Copyright © 2025 Chen, Wang, Zhao, Song, Zhao and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Wang, d2FuZ2RhbkBzdXMuZWR1LmNu
 Jie Chen
Jie Chen Qirong Wang
Qirong Wang Zhiguang Zhao
Zhiguang Zhao Qipeng Song
Qipeng Song Peng Zhao
Peng Zhao Dan Wang
Dan Wang