- Department of Orthopedics, Peking University First Hospital, Beijing, China
Introduction: Polyetheretherketone (PEEK) lumbar fusion rods have been successfully used in short-segment posterior instrumentation to prevent adjacent segment degeneration. However, limited studies have reported their application in lumbar long-segment instrumentation. This study aimed to compare the biomechanical performances of PEEK rods and titanium rods in lumbar long-segment instrumentation using finite element (FE) models, with the expectation of providing clinical guidance.
Methods: A lumbar FE model (A) and four lumbar fixation FE models (BI, CI, BII, CII) of the L1–S1 vertebral body were developed using CT image segmentation (A: intact model; BI: intact model with L2–S1 PEEK rod internal fixation; CI: intact model with L2–S1 titanium rod internal fixation; BII: intact model with L3–S1 PEEK rod internal fixation; CII: intact model with L3–S1 titanium rod internal fixation). A 150-N preload was applied to the top surface of L1, similar to the intact model. The stresses on the lumbar intervertebral disc, facet joint, pedicle screws, and rods were calculated to evaluate the biomechanical effect of the different fixation procedures in lumbar long-segment instrumented surgery.
Results: Under the four physiological motion states, the average stresses on the adjacent segment intervertebral disc and facet joint in all fixation models were greater than those in the intact model. Furthermore, the average stresses on the adjacent segment intervertebral disc and facet joint were greater in models CI and CII than in models BI and BII, respectively. The average stresses on the pedicle screws and rods were decreased in models BI and BII compared with models CI and CII under the four physiological motion states, respectively.
Discussion: The PEEK rod internal fixation system may have better biomechanical properties than the titanium rod internal fixation system in delaying adjacent segment degeneration, improving the lumbar function of postoperative patients, and reducing the risk of screw loosening and breakage in lumbar long-segment instrumentation.
1 Introduction
Posterior lumbar fusion and internal fixation is a classic surgical method for treatment of lumbar degenerative diseases (Li et al., 2013; Du et al., 2020; Pei et al., 2023; Zhang et al., 2023). Titanium alloy rods have been widely used in lumbar fusion internal fixation systems because of their close biomechanical properties to bone, excellent biocompatibility, and provision of sufficient strength under physiological loads (Kurtz and Devine, 2007; Wedemeyer et al., 2007; Ponnappan et al., 2009). However, the titanium alloys used in screw-rod fixation systems have a much higher elastic modulus than bone tissue (110 GPa vs. 0.1–20 GPa), and this can lead to stress concentration in posterior lumbar screw-rod fixation systems and stress shielding of intervertebral bone grafts, thereby increasing the risk of long-term complications such as pseudarthrosis, adjacent segment degeneration (ASD), and screw loosening or breakage (De Iure et al., 2012; Wu et al., 2020; Fan et al., 2021).
In recent years, the latest advancements in posterior spinal fixation have focused on the concept of dynamic stabilization (Khoueir et al., 2007; Greiner-Perth et al., 2016). Dynamic stabilization, which is often used as a non-fusion fixation alternative, is theoretically superior to traditional stiff fixation and can minimize ASD. When applied to fusion methods, enhanced dynamic stabilization provides additional load sharing to the anterior column and reduces stress at the bone-screw interface. However, decreased stability of internal fixation is an inherent risk factor for pseudarthrosis. The ideal fixation system would maximize the fusion rate by providing sufficient stability without excessive rigidity to minimize stress on the adjacent segment.
Polyetheretherketone (PEEK) is a fully biocompatible biomaterial that is increasingly being used for spinal implants. Its elastic modulus (3.6 GPa) is much lower than that of titanium alloys and closer to that of bone, and thus PEEK can better balance the load distribution between the anterior and posterior columns (Kurtz and Devine, 2007; Ponnappan et al., 2009; Ma and Tang, 2014; Li et al., 2018; Laubach et al., 2022; Wu et al., 2023). In previous studies, PEEK rods were successfully used for short-segment lumbar internal fixation with good clinical outcomes (Zhao et al., 2022; Li et al., 2023a). However, limited studies have reported their application in long-segment lumbar internal fixation. The present study aimed to compare the biomechanical performances of PEEK rods and titanium rods in lumbar long-segment instrumentation surgery using finite element (FE) models, with the expectation of providing clinical guidance.
2 Materials and methods
2.1 Development of an FE model of the intact lumbar-sacral spine
To establish an FE model of the intact lumbar-sacral spine, 0.5-mm thick CT images of the L1–S1 vertebral body in a healthy male subject were obtained from Peking University First Hospital. Mimics 11 (Materialise, Belgium), a medical image processing software program, was used to reconstruct the surface geometries of the vertebrae and sacrum. The models were then exported to Geomagics Studio 13.0 (Raindrop Geomagics, United States) and converted to WRP files. The separate vertebrae and sacrum models were integrated with origin alignment in SolidWorks 2020 (Dassault Systems, France) and the intervertebral discs and posterior elements were created based on the reconstructed vertebrae. The thicknesses of the cortical bones and endplates were set at 2 mm and 0.5 mm, respectively. The material properties of the FE model were derived from previous studies (Ambati et al., 2015; Zhang et al., 2022; Li et al., 2023b) and are detailed in Table 1. The final FE model of the lumbar-sacral spine was composed of L1–L5, sacrum, coccyx, and five intervertebral discs (Figure 1).
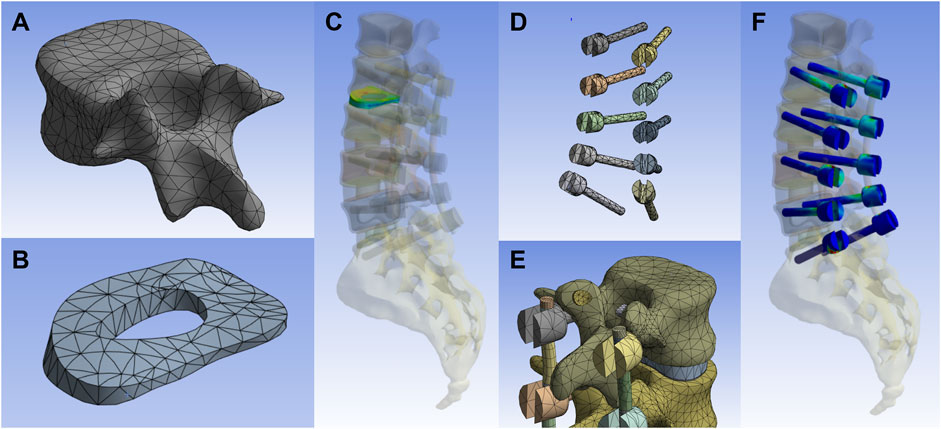
Figure 1. Development of an FE model. (A) The vertebral body after dividing the grid. (B,C) The Annulus fibrosus and its combination relationship in the whole model. (D) Model of pedicle screw. (E) Assembly relationship of pedicle screw, rods, facet joints and vertebrae. (F) Assembly relationship of pedicle screws in the overall model.
2.2 Development of FE models of the implanted lumbar-sacral spine
To simulate implantation and fixation, four FE models were established by modifying the intact model based on posterior spinal surgery. Briefly, we modeled implantation of internal fixation at L2–S1 and L3–S1 using rod fixation systems over the length of five segments and four segments, respectively. We then assigned the materials in each section as whole PEEK or whole titanium, generating the four implanted FE models. The titanium pedicle screws had a diameter of 6.5 mm. The PEEK rods and titanium rods had a diameter of 5.5 mm. All of the implants were meshed as three-dimensional solid elements.
As shown in Figure 2, the FE models of the implanted lumbar-sacral spine were established for the study. Model A was the intact model, model BI was the intact model with L2–S1 PEEK rod internal fixation, model CI was the intact model with L2–S1 titanium rod internal fixation, model BII was the intact model with L3–S1 PEEK rod internal fixation, and model CII intact model with L3–S1 titanium rod internal fixation. The surgical operation was simulated in the models with internal fixation, and comparative analysis of the mechanical properties was performed. The models provided a realistic reproduction of the surgical operation and enabled analysis of the mechanical properties.
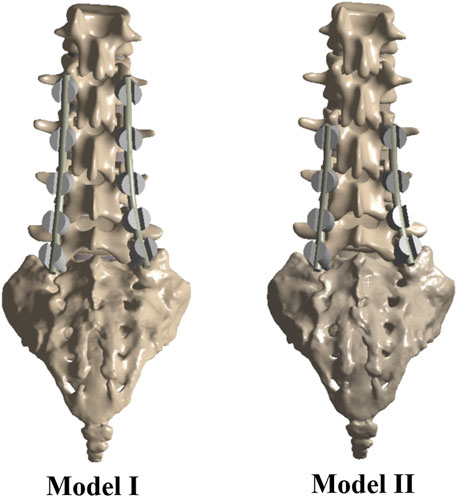
Figure 2. The FE models of the implanted lumbar-sacral spine constructed for the present study. Model I: intact model with L2–S1 internal fixation; Model II: intact model with L3–S1 internal fixation.
2.3 FE analysis of the implanted lumbar-sacral spine
The interactions between the pedicle screws and vertebrae and between the pedicle screws and rods were defined as bonded. The facet joints were assigned no separation with two adjacent vertebrae. All faces of the sacrum and coccyx were fixed in all directions. A 150-N preload and a 10-Nm moment were applied to the top surface of L1 to validate the loading conditions in the intact model, based on a previous in vitro study (Yamamoto et al., 1989). For the implanted models, a displacement-controlled FE analysis was used and the loads were applied in two steps. First, a 150-N preload was applied to the top surface of L1, similar to the intact model. Second, to determine the equivalent moment, an iterative process of moment increasing from 10 Nm was used and the approximated moment was applied to the top surface of L1, reaching the same range of motion (ROM) as the intact model. The accuracy of the ROM was 0.01 degrees. The two-step load procedure was based on several works in accordance with a hybrid testing protocol (Zhong et al., 2009; Zhang et al., 2022).
2.4 Data analyses
The stresses on the lumbar intervertebral disc and facet joint were used to evaluate the biomechanical effects on these areas after the different internal fixation procedures (titanium or PEEK rods) under the conditions of flexion, extension, lateral bending, and axial rotation, which are related to the risk of ASD. The stresses on the screws and rods were calculated to evaluate the risk of instrument failure.
3 Results
In this study, an L1–S1 vertebral body model was reconstructed and implanted with internal fixation systems for FE analysis. The biomechanical properties under four physiological motion states were evaluated.
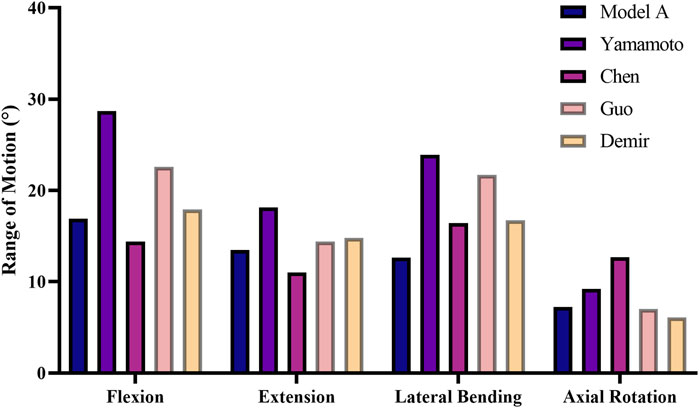
3.1 Verification of model validity
To validate the L1–S1 intact lumbar spine FE model, the ROM was calculated for model A and compared with the ROMs in previous in vitro studies and FE studies under the same loads (Yamamoto et al., 1989; Chen et al., 2001; Guo and Yin, 2019; Demir et al., 2020). As shown in Figure 3, excellent agreement was noted between the experimental results and the calculated results. The ROM in model A was concluded to be in good agreement with the results of the other studies, thus confirming the validity of the experimental FE model.
3.2 Stresses on the intervertebral discs
The average stresses on the L1–L2 and L2–L3 intervertebral discs in the five models are shown in Figure 4. Compared with model A, the average stresses on the L1–L2 intervertebral disc in model BI and model CI and the average stresses on the L2–L3 intervertebral disc in model BII and model CII were increased under the four physiological motion states. In addition, the average stress on the L1–L2 intervertebral disc in model CI was greater than that in model BI under the four physiological motion states; similarly, the average stress on the L2–L3 intervertebral disc in model CII was greater than that in model BII under the four physiological motion states. The average stress on the L1–L2 intervertebral disc was increased by an average of 167.0% for model BI and 283.8% for model CI compared with model A under the four physiological motion states. The average stress on the L2–L3 intervertebral disc was increased by an average of 95.1% for model BII and 135.6% for model CII compared with model A under the four physiological motion states. These findings may be used to solve the problem of disc degeneration on the adjacent segment in patients after lumbar long-segment instrumented surgery.
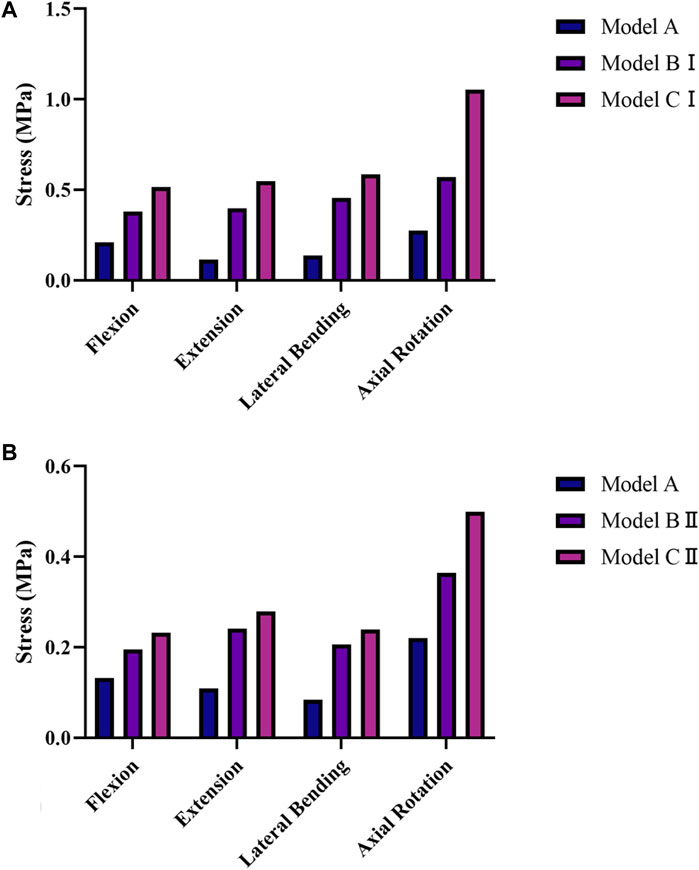
Figure 4. Average von Mises stresses on the intervertebral discs in the five models under the four physiological motion states. (A) Average von Mises stresses on the L1–L2 intervertebral disc in models A, BI, and CI under the four physiological motion states. (B) Average von Mises stresses on the L2–L3 intervertebral disc in models A, BII, and CII under the four physiological motion states.
3.3 Stresses on the facet joints
The average stresses on the L1–L2 and L2–L3 facet joints in the five models are shown in Figure 5. Compared with model A, the average stresses on the L1–L2 facet joint in model BI and model CI and the L2–L3 facet joint in model BII and model CII were increased under the four physiological motion states. In addition, the average stress on the L1–L2 facet joint in model CI was greater than that in model BI under the four physiological motion states; similarly, the average stress on the L2–L3 facet joint in model CII was greater than that in model BII under the four physiological motion states. The average stress on the L1–L2 facet joint was increased by an average of 162.8% for model BI and 269.5% for model CI compared with model A under the four physiological motion states. The average stress on the L2–L3 facet joint was increased by an average of 86.7% for model BII and 121.9% for model CII compared with model A under the four physiological motion states. These findings may be used to solve the problem of facet joint degeneration on the adjacent segment in patients after lumbar long-segment instrumented surgery.
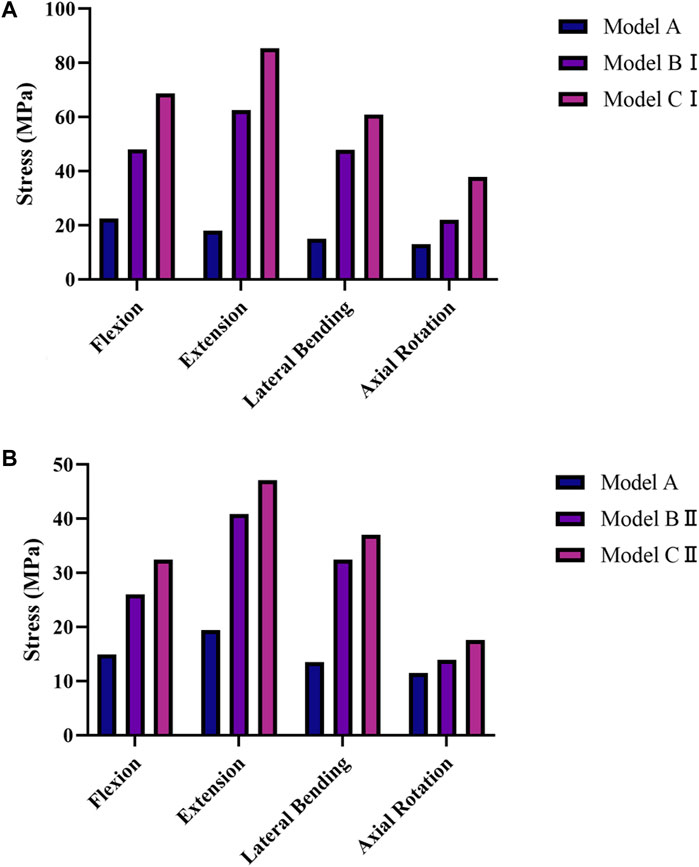
Figure 5. Average von Mises stresses on the facet joints in the five models under the four physiological motion states. (A) Average von Mises stresses on the L1–L2 facet joint in models A, BI, and CI under the four physiological motion states. (B) Average von Mises stresses on the L2–L3 facet joint in models A, BII, and CII under the four physiological motion states.
3.4 Stresses on the screws and rods
The average stresses on the screws and rods in the four implanted models with the internal fixation systems are shown in Figures 6, 7, respectively. The average stresses on the screws and rods in models CI and CII were greater than those in models BI and BII under the four physiological motion states, respectively. Compared with model BI, the average stresses on the screws and rods in model CI were increased by an average of 150.0% and 940.8% under the four physiological motion states, respectively. Compared with model BII, the average stresses on the screws and rods in model CII were increased by an average of 129.3% and 903.6% under the four physiological motion states, respectively. These findings may be used to solve the problem of internal fixation system failure and screw-rod fracture in patients after lumbar long-segment instrumented surgery. Additionally, the comparison of the nephogram of von Mises stress on the intervertebral discs, facet joints, pedicle screws, and rods in flexion and extension condition on different models are shown in Figures 8–11, respectively.
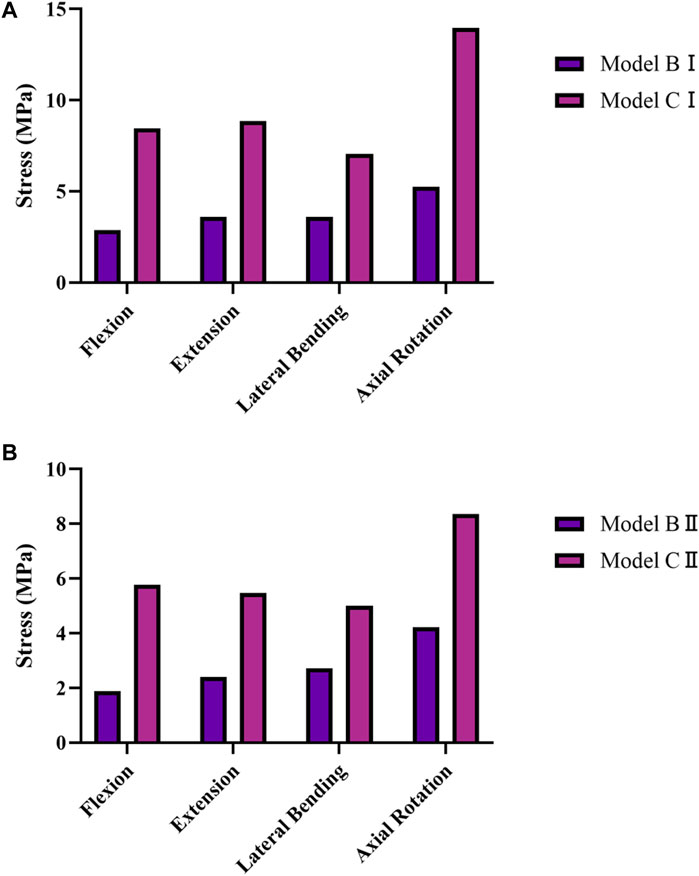
Figure 6. Average von Mises Stress on the pedicle screws in models BI, BII, CI, and CII under the four physiological motion states. (A) Average von Mises stresses on the pedicle screws in models BI and CI under the four physiological motion states. (B) Average von Mises stresses on the pedicle screws in models BII and CII under the four physiological motion states.
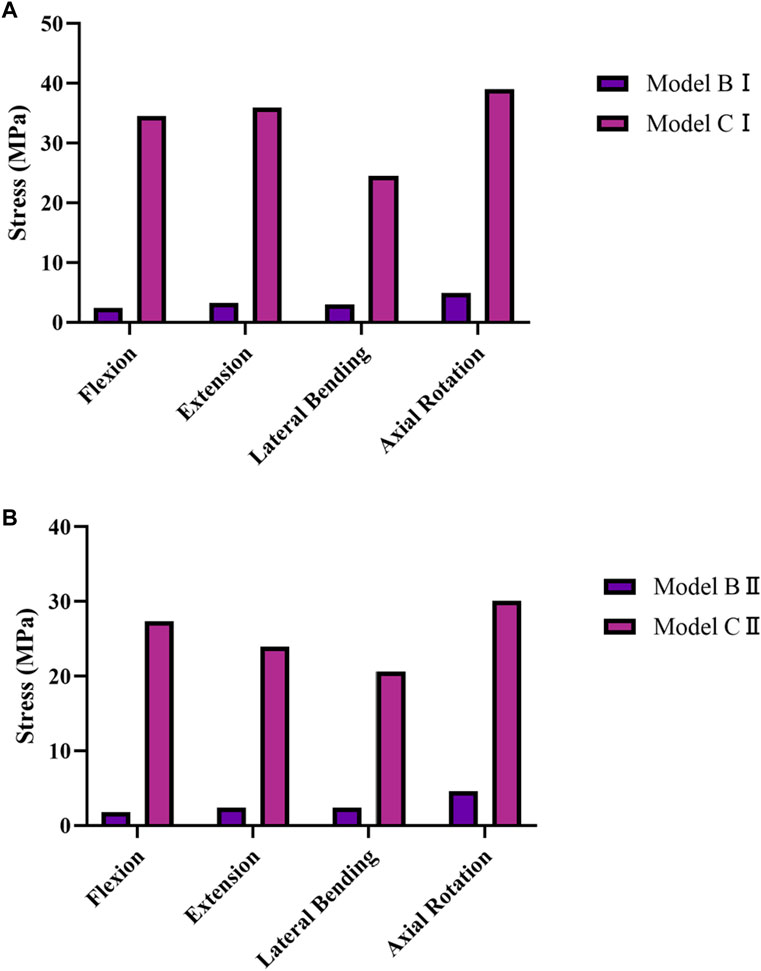
Figure 7. Average von Mises stresses on the rods in models BI, BII, CI, and CII under the four physiological motion states. (A) Average von Mises stresses on the rods in models BI and CI under the four physiological motion states. (B) Average von Mises stresses on the rods in models BII and CII under the four physiological motion states.
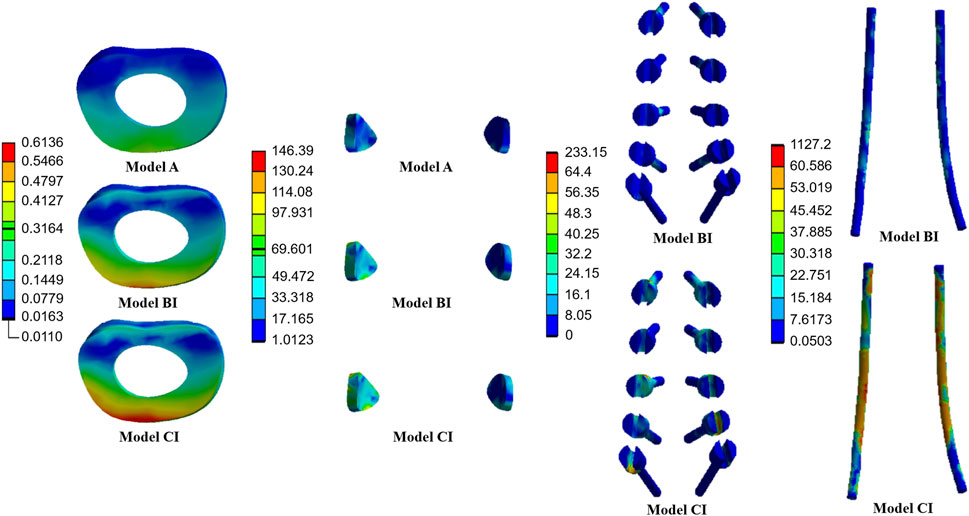
Figure 8. Nephogram of von Mises stress (MPa) on the L1/2 intervertebral discs, L1/2 facet joints, pedicle screws, and rods in flexion condition on Models A, BI, and CI.
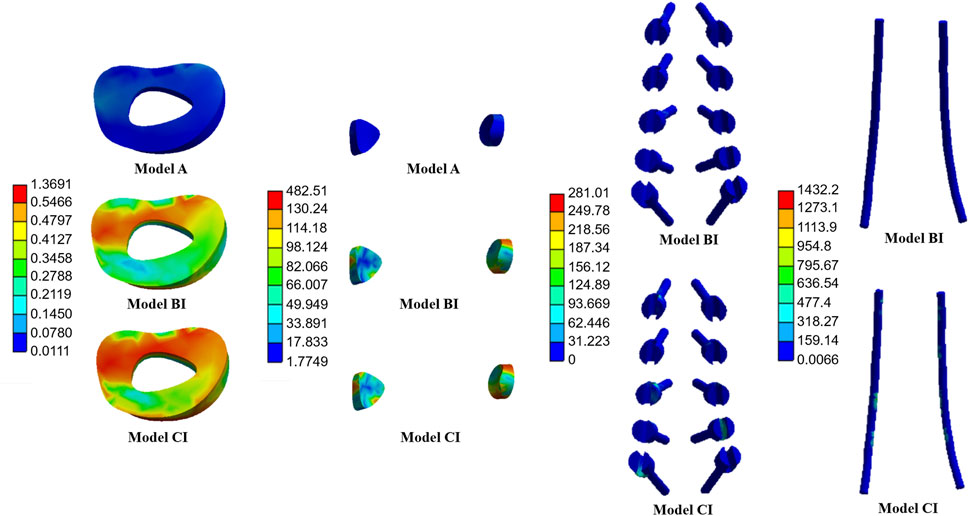
Figure 9. Nephogram of von Mises stress (MPa) on the L1/2 intervertebral discs, L1/2 facet joints, pedicle screws, and rods in extension condition on Models A, BI, and CI.
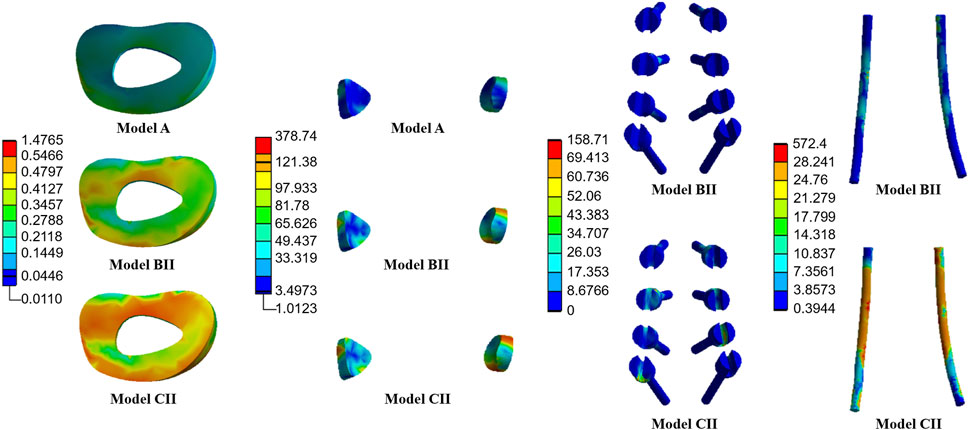
Figure 10. Nephogram of von Mises stress (MPa) on the L2/3 intervertebral discs, L2/3 facet joints, pedicle screws, and rods in flexion condition on Models A, BII, and CII.
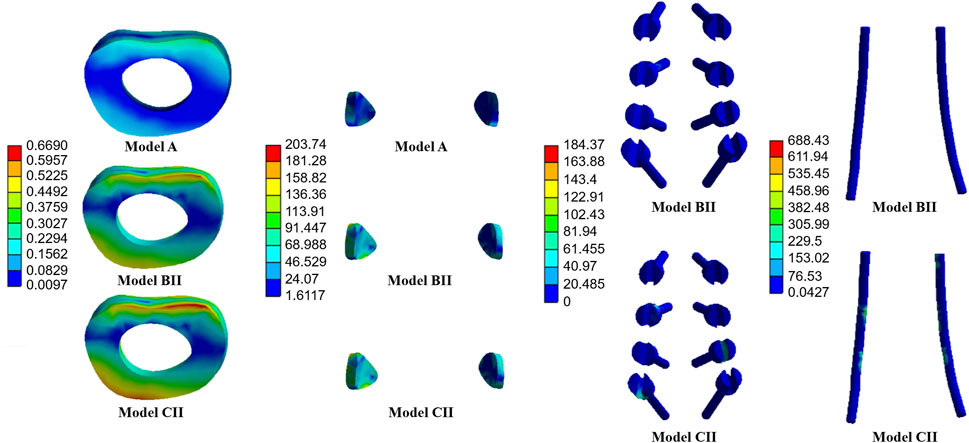
Figure 11. Nephogram of von Mises stress (MPa) on the L2/3 intervertebral discs, L2/3 facet joints, pedicle screws, and rods in extension condition on Models A, BII, and CII.
4 Discussion
Currently, titanium pedicle screw rods (rigid fixation) and PEEK cages have been widely used in posterior lumbar fusion surgery to stabilize the surgical segment and restore the spinal column sequence (Li et al., 2020; Laubach et al., 2022). However, the complications caused by rigid fixation, such as ASD, pseudarthrosis, screw loosening, loss of motion, and back pain, significantly reduce the quality of life of patients, and thus the concept of semi-rigid fixation has been applied in recent years (Khoueir et al., 2007; Greiner-Perth et al., 2016; Nikkhoo et al., 2021). The core point for semi-rigid fixation is that the low-strength material still limits the ROM of the fixed segment, but tends to also reduce the overall structural stiffness of the system, leading to more even distribution of the spinal load between the anterior and posterior columns and preventing various complications caused by the unbalanced load distribution associated with rigid fixation. A less rigid stabilization system can also theoretically preserve part of the rotational motion at the instrumented level and unload any extra stress exposure on adjacent levels (Maragkos et al., 2020; Nikkhoo et al., 2021).
As a representative component for semi-rigid fixation systems, PEEK rods have been highly anticipated by scholars and gradually introduced into posterior spinal fusion since 2007 (Huang et al., 2016). Although previous studies showed that PEEK rods had better load distribution performance than titanium rods and were successfully used for short-segment lumbar internal fixation with good clinical outcomes, doctors remain very cautious about their clinical application in long-segment lumbar internal fixation. One important reason for this is that the biomechanical performance of PEEK rods has not been comprehensively evaluated in long-segment lumbar internal fixation. Moreover, it is difficult to evaluate the biomechanical effects of lumbar fixation in clinical studies. Therefore, the present study was conducted to compare the biomechanical performances of PEEK rods and titanium rods in lumbar long-segment instrumentation surgery using FE models, with the expectation of providing clinical guidance. As the spinal fixation construct is the most essential component of lumbar fusion surgery, this study aimed to investigate the fixation itself. Thus, posterolateral fixation was utilized when simulating the postoperative models with titanium rods and PEEK rods, and bone graft fusion between the transverse processes was neglected, as a common simplification in the literature (Jahng et al., 2013; Jin et al., 2013).
ASD is a common complication after lumbar fusion surgery, because the decrease in ROM of the fixed segment requires compensation by the adjacent segment, and the internal fixation changes the normal mechanical transmission process in the spine. In a previous FE study, Jin et al. (Jin et al., 2013) demonstrated that PEEK rods significantly decreased the stresses on the intervertebral disc and facet joint in the upper adjacent segment compared with titanium rod internal fixation in short-segment lumbar internal fixation surgery. In the present study, the average stresses on the intervertebral disc and facet joint in the upper adjacent segment in all internal fixation models were greater than those in the intact model under all four physiological motion states. Meanwhile, the average stresses on the intervertebral disc and facet joint on the upper adjacent segment in the titanium rod models (CI and CII) were greater than those in the PEEK rod models (BI and BII) under the four physiological motion states, respectively, showing that the use of PEEK rods in lumbar long-segment instrumentation surgery confers the advantage of reduced ASD. However, it is not sufficient to solely evaluate ASD based on the stresses on the intervertebral disc and facet joint in lumbar long-segment instrumentation surgery, and other factors such as intervertebral disc height and sagittal balance should also be taken into account.
The stability of pedicle screw rod internal fixation systems has always been a concern of spine surgeons. In the present study, use of PEEK rods led to lower screw stress than use of titanium rods, leading to a lower risk of screw breakage with PEEK rods in lumbar long-segment instrumentation surgery. This effect may also be attributed to the reduced stress shielding with PEEK rods, which would reduce the load through the posterior hardware. A related study found that PEEK rods have the potential biomechanical advantages of better anterior column load sharing and reduced stress at the bone-to-screw interface (Ponnappan et al., 2009), consistent with the findings in the present study.
A recent study tested the biomechanical properties of PEEK rods and titanium rods in vitro using human lumbar spine specimens, and the results indicated that there were no significant differences in the stability provided by PEEK rods and titanium rods under any of the loading modes examined (Yeager et al., 2015). In addition to limiting abnormal segmental motion, maintenance of good anterior and posterior column load distribution in the spine is essential to alleviate various complications. While titanium rods are uniquely suited to provide postoperative stability, they also dramatically alter the physiological loading characteristics of the spine (Ponnappan et al., 2009; Yeager et al., 2015). A titanium pedicle screw rod system was shown to transmit approximately 67% of the axial compressive load during posterior lumbar internal fixation surgery, whereas the posterior column in the natural upright position carries only approximately 20% of the load (Cunningham and Polly, 2002; Ahn et al., 2008). An FE study revealed that PEEK rods carry at least 6% less load than titanium rods (Gornet et al., 2011). In the present study, the results demonstrated the average stresses on the rods were increased in the titanium rod models (CI and CII) under the four physiological motion states compared with the PEEK rod models (BI and BII), respectively. It is speculated that the advantage of the load distribution performance of PEEK rods is mainly due to the reduction in stress concentration in the posterior pedicle screw rod system. However, the stress data indicated that although the stresses on PEEK rods were lower than those on titanium rods, the yield stress was significantly lower on PEEK rods (100 MPa) than on titanium rods (750 MPa), resulting a higher ratio of stress on the rod to yield stress on the rod material for the PEEK rods. Consequently, the PEEK rod system may face a higher risk of rod breakage. In summary, just as there are two sides to a coin, PEEK rods have both advantages and disadvantages. Therefore, further studies are warranted to validate the clinical outcomes for use of PEEK rods in lumbar long-segment instrumentation surgery in clinical practice.
The present experimental study inevitably has some limitations. First, the geometry of the human lumbar spine varies from individual to individual, but the FE model built in this study was based on a single patient. Therefore, additional samples are needed for future validation. Second, the theoretical numerical model based on the FE method simplifies the highly complex spinal system to a large extent, and factors such as the fibbers in the discs, muscle, and cyclic load are not considered. Third, due to the limitations of the available experimental data, only the intact model was validated, and the surgical models were developed using the intact model. In general, the biomechanical data obtained in the present study should be viewed as comparative data between different surgical cases due to the limitations of the model itself.
5 Conclusion
The PEEK rod internal fixation system may have better biomechanical properties than the titanium rod internal fixation system in delaying ASD, improving lumbar function in postoperative patients, and reducing the risk of screw loosening and breakage in lumbar long-segment instrumentation. Further studies are warranted to comprehensively validate the clinical outcomes for use of PEEK rods in lumbar long-segment instrumentation surgery in clinical practice.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of Peking University First Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CL: Conceptualization, Writing–original draft, Writing–review and editing. YZ: Methodology, Resources, Writing–original draft, Writing–review and editing. LQ: Formal Analysis, Methodology, Software, Writing–review and editing. BX: Formal Analysis, Writing–review and editing. LY: Investigation, Writing–review and editing. RZ: Visualization, Writing–review and editing. CL: Funding acquisition, Supervision, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study is supported by the Capital Health Research and Development of Special Fund (2022-2Z-40713), National High Level Hospital Clinical Research Funding (Youth Clinical Research Project of Peking University First Hospital, 2023YC22), and National Natural Science Foundation of China (No. U20A20390, 12332019).
Acknowledgments
The authors thank Alison Sherwin, PhD, from Liwen Bianji (Edanz) (www.liwenbianji.cn/) for editing the English text of a draft of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahn, Y.-H., Chen, W.-M., Lee, K.-Y., Park, K.-W., and Lee, S.-J. (2008). Comparison of the load-sharing characteristics between pedicle-based dynamic and rigid rod devices. Biomed. Mater. Bristol, Engl. 3 (4), 044101. doi:10.1088/1748-6041/3/4/044101
Ambati, D. V., Wright, E. K., Lehman, R. A., Kang, D. G., Wagner, S. C., and Dmitriev, A. E. (2015). Bilateral pedicle screw fixation provides superior biomechanical stability in transforaminal lumbar interbody fusion: a finite element study. Spine J. Official J. North Am. Spine Soc. 15 (8), 1812–1822. doi:10.1016/j.spinee.2014.06.015
Chen, C. S., Cheng, C. K., Liu, C. L., and Lo, W. H. (2001). Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med. Eng. Phys. 23 (7), 485–493. doi:10.1016/s1350-4533(01)00076-5
Cunningham, B. W., and Polly, D. W. (2002). The use of interbody cage devices for spinal deformity: a biomechanical perspective. Clin. Orthop. Relat. Res. 394, 73–83. doi:10.1097/00003086-200201000-00009
De Iure, F., Bosco, G., Cappuccio, M., Paderni, S., and Amendola, L. (2012). Posterior lumbar fusion by peek rods in degenerative spine: preliminary report on 30 cases. Eur. Spine J. Official Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 21 (Suppl. 1), S50–S54. doi:10.1007/s00586-012-2219-x
Demir, E., Eltes, P., Castro, A. P., Lacroix, D., and Toktaş, İ. (2020). Finite element modelling of hybrid stabilization systems for the human lumbar spine. Proc. Institution Mech. Eng. Part H, J. Eng. Med. 234 (12), 1409–1420. doi:10.1177/0954411920946636
Du, X., Ou, Y.-S., Zhu, Y., Luo, W., Jiang, G.-Y., and Jiang, D.-M. (2020). Oblique lateral interbody fusion combined percutaneous pedicle screw fixation in the surgical treatment of single-segment lumbar tuberculosis: a single-center retrospective comparative study. Int. J. Surg. Lond. Engl. 83, 39–46. doi:10.1016/j.ijsu.2020.09.012
Fan, W., Guo, L.-X., and Zhang, M. (2021). Biomechanical analysis of lumbar interbody fusion supplemented with various posterior stabilization systems. Eur. Spine J. Official Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 30 (8), 2342–2350. doi:10.1007/s00586-021-06856-7
Gornet, M. F., Chan, F. W., Coleman, J. C., Murrell, B., Nockels, R. P., Taylor, B. A., et al. (2011). Biomechanical assessment of a PEEK rod system for semi-rigid fixation of lumbar fusion constructs. J. Biomechanical Eng. 133 (8), 081009. doi:10.1115/1.4004862
Greiner-Perth, R., Sellhast, N., Perler, G., Dietrich, D., Staub, L. P., and Röder, C. (2016). Dynamic posterior stabilization for degenerative lumbar spine disease: a large consecutive case series with long-term follow-up by additional postal survey. Eur. Spine J. Official Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 25 (8), 2563–2570. doi:10.1007/s00586-016-4532-2
Guo, L.-X., and Yin, J.-Y. (2019). Finite element analysis and design of an interspinous device using topology optimization. Med. Biol. Eng. Comput. 57 (1), 89–98. doi:10.1007/s11517-018-1838-8
Huang, W., Chang, Z., Song, R., Zhou, K., and Yu, X. (2016). Non-fusion procedure using PEEK rod systems for lumbar degenerative diseases: clinical experience with a 2-year follow-up. BMC Musculoskelet. Disord. 17, 53. doi:10.1186/s12891-016-0913-2
Jahng, T.-A., Kim, Y. E., and Moon, K. Y. (2013). Comparison of the biomechanical effect of pedicle-based dynamic stabilization: a study using finite element analysis. Spine J. Official J. North Am. Spine Soc. 13 (1), 85–94. doi:10.1016/j.spinee.2012.11.014
Jin, Y. J., Kim, Y. E., Seo, J. H., Choi, H. W., and Jahng, T.-A. (2013). Effects of rod stiffness and fusion mass on the adjacent segments after floating mono-segmental fusion: a study using finite element analysis. Eur. Spine J. Official Publ. Eur. Spine Soc. Eur. Spinal Deformity Soc. Eur. Sect. Cerv. Spine Res. Soc. 22 (5), 1066–1077. doi:10.1007/s00586-012-2611-6
Khoueir, P., Kim, K. A., and Wang, M. Y. (2007). Classification of posterior dynamic stabilization devices. Neurosurg. Focus 22 (1), 1–8. doi:10.3171/foc.2007.22.1.3
Kurtz, S. M., and Devine, J. N. (2007). PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 28 (32), 4845–4869. doi:10.1016/j.biomaterials.2007.07.013
Laubach, M., Kobbe, P., and Hutmacher, D. W. (2022). Biodegradable interbody cages for lumbar spine fusion: current concepts and future directions. Biomaterials 288, 121699. doi:10.1016/j.biomaterials.2022.121699
Li, C., Liu, L., Shi, J.-Y., Yan, K.-Z., Shen, W.-Z., and Yang, Z.-R. (2018). Clinical and biomechanical researches of polyetheretherketone (PEEK) rods for semi-rigid lumbar fusion: a systematic review. Neurosurg. Rev. 41 (2), 375–389. doi:10.1007/s10143-016-0763-2
Li, C.-d., Sun, H.-l., and Lu, H.-z. (2013). Comparison of the effect of posterior lumbar interbody fusion with pedicle screw fixation and interspinous fixation on the stiffness of adjacent segments. Chin. Med. J. 126 (9), 1732–1737. doi:10.3760/cma.j.issn.0366-6999.20112393
Li, J., Qin, L., Yang, K., Ma, Z., Wang, Y., Cheng, L., et al. (2020). Materials evolution of bone plates for internal fixation of bone fractures: a review. J. Mater. Sci. Technol. 36, 190–208. doi:10.1016/j.jmst.2019.07.024
Li, W., Han, J., Xin, Q., Liu, Q., Feng, C., Liu, Y., et al. (2023b). Finite element mechanical analysis of ipsilateral approach and contralateral approach in unilateral bilateral endoscopic spine surgery. J. Orthop. Surg. Res. 18 (1), 979. doi:10.1186/s13018-023-04476-z
Li, W., Zhao, H., Li, C., Liu, T., Guan, J., Yang, Y., et al. (2023a). Polyetheretherketone (PEEK) rods versus titanium rods for posterior lumbar fusion surgery: a systematic review and meta-analysis. J. Orthop. Surg. Res. 18 (1), 348. doi:10.1186/s13018-023-03817-2
Ma, R., and Tang, T. (2014). Current strategies to improve the bioactivity of PEEK. Int. J. Mol. Sci. 15 (4), 5426–5445. doi:10.3390/ijms15045426
Maragkos, G. A., Atesok, K., and Papavassiliou, E. (2020). Prognostic factors for adjacent segment disease after L4-L5 lumbar fusion. Neurosurgery 86 (6), 835–842. doi:10.1093/neuros/nyz241
Nikkhoo, M., Lu, M.-L., Chen, W.-C., Fu, C.-J., Niu, C.-C., Lin, Y.-H., et al. (2021). Biomechanical investigation between rigid and semirigid posterolateral fixation during daily activities: geometrically parametric poroelastic finite element analyses. Front. Bioeng. Biotechnol. 9, 646079. doi:10.3389/fbioe.2021.646079
Pei, B., Xu, Y., Zhao, Y., Wu, X., Lu, D., Wang, H., et al. (2023). Biomechanical comparative analysis of conventional pedicle screws and cortical bone trajectory fixation in the lumbar spine: an in vitro and finite element study. Front. Bioeng. Biotechnol. 11, 1060059. doi:10.3389/fbioe.2023.1060059
Ponnappan, R. K., Serhan, H., Zarda, B., Patel, R., Albert, T., and Vaccaro, A. R. (2009). Biomechanical evaluation and comparison of polyetheretherketone rod system to traditional titanium rod fixation. Spine J. Official J. North Am. Spine Soc. 9 (3), 263–267. doi:10.1016/j.spinee.2008.08.002
Wedemeyer, M., Parent, S., Mahar, A., Odell, T., Swimmer, T., and Newton, P. (2007). Titanium versus stainless steel for anterior spinal fusions: an analysis of rod stress as a predictor of rod breakage during physiologic loading in a bovine model. Spine 32 (1), 42–48. doi:10.1097/01.brs.0000251036.99413.20
Wu, J., Shi, L., Liu, D., Wu, Z., Gao, P., Liu, W., et al. (2023). Evaluating screw stability after pedicle screw fixation with PEEK rods. Glob. Spine J. 13 (2), 393–399. doi:10.1177/2192568221996692
Wu, J., Shi, L., Pei, Y., Yang, D., Gao, P., Xiao, X., et al. (2020). Comparative effectiveness of PEEK rods versus titanium alloy rods in cervical fusion in a new sheep model. Eur. Spine J. 29 (5), 1159–1166. doi:10.1007/s00586-020-06307-9
Yamamoto, I., Panjabi, M. M., Crisco, T., and Oxland, T. (1989). Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine 14 (11), 1256–1260. doi:10.1097/00007632-198911000-00020
Yeager, M. S., Cook, D. J., and Cheng, B. C. (2015). In vitro comparison of dynesys, PEEK, and titanium constructs in the lumbar spine. Adv. Orthop. 2015, 895931–895938. doi:10.1155/2015/895931
Zhang, M., Ren, W., Mo, Z., Li, J., Pu, F., and Fan, Y. (2022). Biomechanics of adjacent segment after three-level lumbar fusion, hybrid single-level semi-rigid fixation with two-level lumbar fusion. Comput. Methods Biomechanics Biomed. Eng. 25 (4), 455–463. doi:10.1080/10255842.2021.1959557
Zhang, X., Wang, Y., Zhang, W., Liu, S., Liu, Z., Wang, K., et al. (2023). Perioperative clinical features and long-term prognosis after oblique lateral interbody fusion (olif), olif with anterolateral screw fixation, or olif with percutaneous pedicle fixation: a comprehensive treatment strategy for patients with lumbar degenerative disease. Neurospine 20 (2), 536–549. doi:10.14245/ns.2244954.477
Zhao, Y., Xu, B., Qi, L., Li, C., Yue, L., Yu, Z., et al. (2022). Hybrid surgery with PEEK rods for lumbar degenerative diseases: a 2-year follow-up study. BMC Musculoskelet. Disord. 23 (1), 4. doi:10.1186/s12891-021-04895-1
Keywords: lumbar degenerative disease, posterior lumbar instrumentation, PEEK, dynamic stabilization, adjacent segment degeneration, finite element analysis
Citation: Li C, Zhao Y, Qi L, Xu B, Yue L, Zhu R and Li C (2024) Comparison of biomechanical effects of polyetheretherketone (PEEK) rods and titanium rods in lumbar long-segment instrumentation: a finite element study. Front. Bioeng. Biotechnol. 12:1416046. doi: 10.3389/fbioe.2024.1416046
Received: 11 April 2024; Accepted: 24 June 2024;
Published: 11 July 2024.
Edited by:
Jingwei Zhang, Shanghai Jiao Tong University, ChinaReviewed by:
Marco Parente, University of Porto, PortugalMaria Ludovica Pallotta, IRCCS Ospedale Galeazzi Sant’Ambrogio, Italy
Copyright © 2024 Li, Zhao, Qi, Xu, Yue, Zhu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chunde Li, bGljaHVuZGVAdmlwLnNpbmEuY29t
†These authors have contributed equally to this work
 Chao Li
Chao Li Yao Zhao†
Yao Zhao† Longtao Qi
Longtao Qi Beiyu Xu
Beiyu Xu Lei Yue
Lei Yue