- 1School of Nursing, Capital Medical University, Beijing, China
- 2College of Nursing and Rehabilitation, North China University of Science and Technology, Hebei, China
Purpose: The study aims to develop a finite element model of the pelvic floor and thighs of elderly men to quantitatively assess the impact of different pelvic floor muscle trainings and the urinary and defecation control ability.
Methods: A finite element model of the pelvic floor and thighs of elderly men was constructed based on MRI and CT. Material properties of pelvic floor tissues were assigned through literature review, and the relative changes in waistline, retrovesical angle (RVA) and anorectad angulation (ARA) to quantitatively verify the effectiveness of the model. By changing the material properties of muscles, the study analyzed the muscle strengthening or impairment effects of the five types of rehabilitation training for four types of urination and defecation dysfunction. The changes in four outcome indicators, including the retrovesical angle, anorectad angulation, stress, and strain, were compared.
Results: This study indicates that ARA and RVA approached their normal ranges as material properties changed, indicating an enhancement in the urinary and defecation control ability, particularly through targeted exercises for the levator ani muscle, external anal sphincter, and pelvic floor muscles. This study also emphasizes the effectiveness of personalized rehabilitation programs including biofeedback, exercise training, electrical stimulation, magnetic stimulation, and vibration training and advocates for providing optimized rehabilitation training methods for elderly patients.
Discussion: Based on the results of computational biomechanics, this study provides foundational scientific insights and practical recommendations for rehabilitation training of the elderly’s urinary and defecation control ability, thereby improving their quality of life. In addition, this study also provides new perspectives and potential applications of finite element analysis in elderly men, particularly in evaluating and designing targeted rehabilitation training.
1 Introduction
In contemporary society, the aging of the population continues to intensify, and the health problems of the elderly have received increasing attention. The decline in muscle strength and diminished neurological control often experienced with age and frailty lead to conditions such as urinary incontinence, urinary retention, fecal incontinence and constipation (Talasz et al., 2018; Ma and Chen, 2020; Levaillant et al., 2023; Salari et al., 2023), significantly affecting life quality. The resultant emotional distress and increased dependency on caregivers (Bektas et al., 2023), which plays a vital role in determining the care dependence of the elderly and has an impact on social and economic development. It is becoming more and more prominent that how to effectively improve the urinary and defecation control ability of the elderly in the field of rehabilitation medicine.
For the elderly retaining partial urinary and defecation control ability, the five rehabilitation training methods of exercise training, magnetic stimulation, electrical stimulation, vibration stimulation and biofeedback, which are validated for enhancing the muscles strength in the pelvic floor, abdomen, back, and hips, thereby improving control bowel movements (Mazur-Bialy et al., 2020; Alouini et al., 2022). However, different rehabilitation training methods may have different effects on the urinary and defecation control ability, it is necessary to delineate the quantitative relationship between different rehabilitation training methods and urinary and defecation control ability and to understand the underlying mechanism to provide guidance for clinical rehabilitation practices. Finite element analysis (FEA), a critical computational tool, is considered a technique for simulating the mechanical properties of an object by dividing it into discrete elements and creating a numerical calculation model to represent its behavior (Chen et al., 2010). In recent years, it is widely used in the urethral support function (Peng et al., 2016), the occurrence of levator ani muscle injury and pelvic floor disease during vaginal delivery (Zhou et al., 2020), and the mechanical mechanism of posterior vaginal prolapse (Qiu, 2017). By establishing finite element models, it can simulate the biomechanical behavior of human tissues and organs and analyze the biomechanics of complex systems quantitatively. It is a method that provides a new idea for the evaluation of the effects of rehabilitation training (Yang et al., 2024). This approach underpins the development of models to simulate elderly men’s pelvic floor structures, enhancing our understanding of urinary and defecation control ability mechanisms (Zhang and Yao, 2015).
This study aims to develop a finite element model to simulate five distinct rehabilitation training methods. By changing the values of material properties proportionally, the strengthening and impairment of muscle capacity are simulated. Meanwhile, the defecation ability of the elderly is reflected through the retrovesical angle (RVA) and anorectad angulation (ARA). By comparing the changes in defecation outcome indicators under various parameter settings, the mechanism and relationship between the rehabilitation training methods and urinary and defecation control ability is quantified. This provides precise and effective guidance for the rehabilitation training of the elderly, thereby improving their quality of life.
2 Methods
2.1 Participant
The implementation of this study complied with relevant ethical requirements (ethical approval number: Linyanshen [2023] No.079 and Z2024SY007). Our study has been registered in the Chinese Clinical Trial Registry Center (ChiCTR2400080749) and our research protocol has been published online (Wang et al., 2024). The pelvic floor medical imaging data collection participant is a 61-year-old Chinese old adult with a body mass index (BMI) of 25.4 kg/m2, good physical health, normal daily living ability, normal cognitive ability, normal communication ability, and normal pelvic floor medical imaging data. The participant’s bowel function was normal, and there was no history of defecation dysfunction or surgery. Participant signed informed consent forms before scanning medical images. During the scan, participant was placed in a supine position with his hands on top of head and legs together and straightened. Scanning started from the highest point of the participant’s iliac crest, CT scan to the knee joint, and MRI scan to 1 cm of the perineum. Radiologists used a 64-slice spiral scanning dual-source CT machine produced by Siemens of Germany and a 3.0T magnetic resonance scanner produced by Philips of the Netherlands to scan, obtain pelvic floor scan data and store it in DICOM format. Among them, CT was scanned with a slice thickness of 0.5 mm and a resolution of 512 × 512, with a total of 598 images, as shown in Figure 1. Static MRI was scanned with 3D-PelvicVIEW-T2, TR 1250 ms, TE 151 ms, field of view 400 cm, continuous 1.0 mm slices Thickness-free volumetric scanning, a total of 400 images, as shown in Figure 2. After the static MRI scan, the participant was asked to perform resting maneuvers, Kegel maneuvers, relaxation maneuvers, and Valsalva maneuvers in order, and at the same time, dynamic MRI scans were performed. Dynamic MRI used the BTFE_Sag_Dyn sequence along the sagittal plane, with a slice thickness of 8 mm and a frame rate of 9–10 frames/s, with a total of 150 images, as shown in Figure 3. For inclusion and exclusion criteria for the participant and the specific data collection methods, please refer to our previous research protocol (Wang et al., 2024).
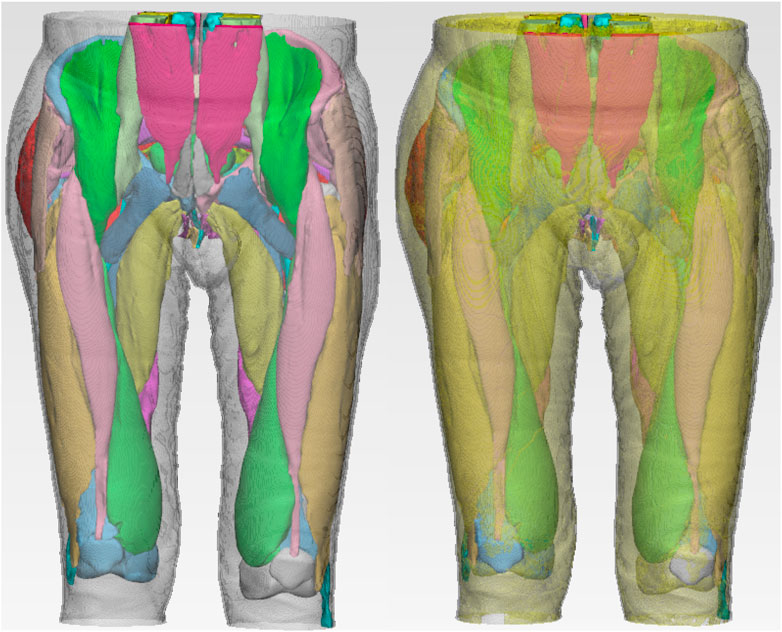
A composite finite element model of the participant’s pelvic floor, abdomen, back and hip was established through medical imaging data, in which the bone geometry model was through CT images and the soft tissue geometry model was through MRI images. First, the segmentation was performed under the guidance of experienced pelvic floor radiologists. We used the medical modeling software Mimics to reconstruct a relatively rough model, and then used the smoothing function in the Mimics software to beautify it, reduce the angle of points or edges, make the edges smoother, smooth the 3D image, and then the accurate model is imported into Ansys software for numerical simulation calculations.
2.2 Material properties
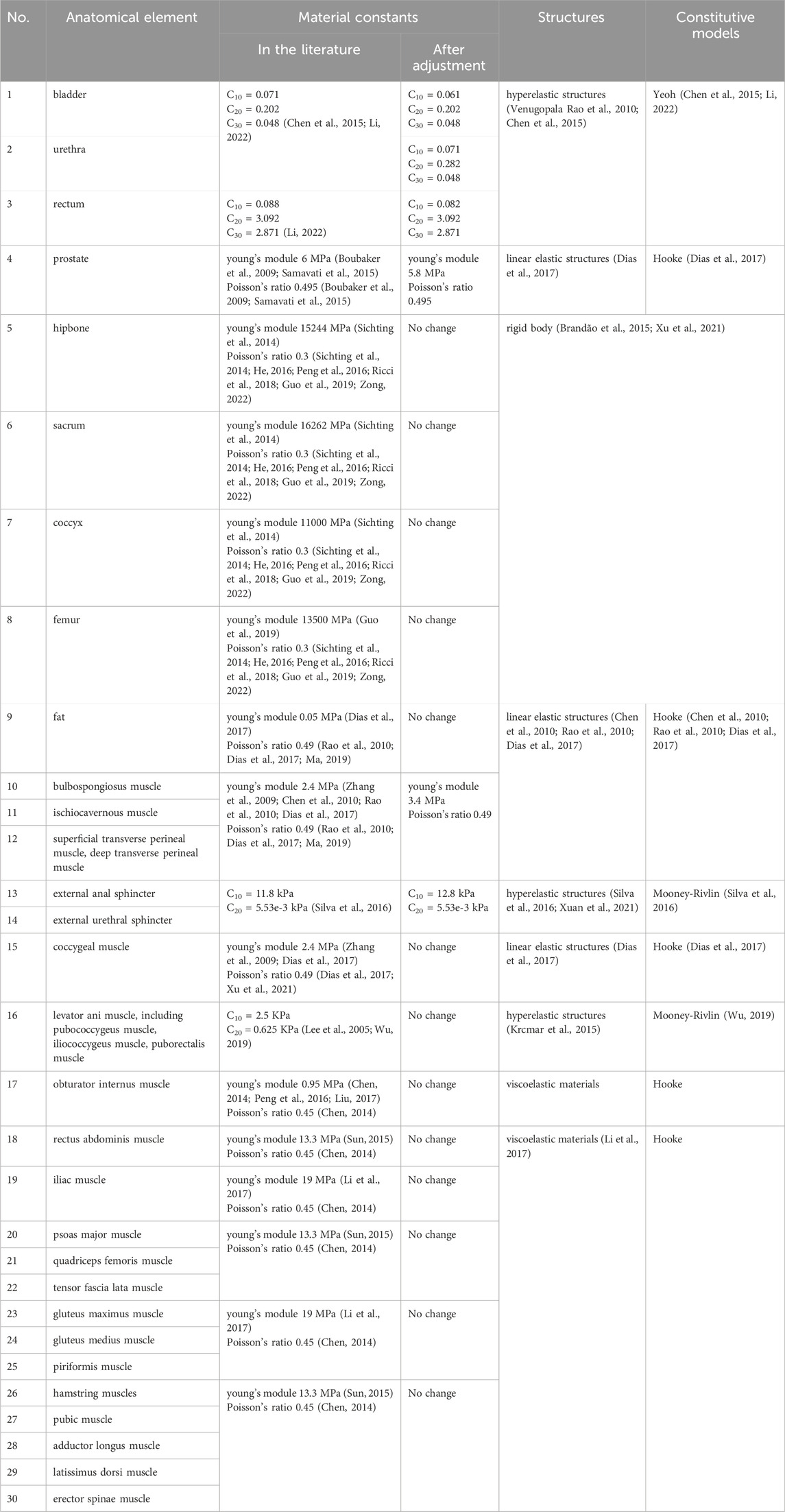
Since this study focuses on the mechanical analysis results of muscles related to urination and defecation, the material properties of the bladder, urethra, rectum, external anal sphincter, external urethral sphincter, and levator ani muscle were analyzed using Yeoh and Mooney-Rivlin hyperelastic structures. For simulation, Hooke linear elastic structures were used for other organs, muscles and fat of the pelvic floor, and viscoelastic structures of the standard linear solid model and hooke were used for the abdominal, back and hip muscles. The pelvis was modeled as a rigid body and fixed structure, considering that its stiffness is much higher than that of soft tissue and therefore its deformation is negligible under normal pelvic function. The finite element type is mainly tetrahedron, supplemented by hexahedron. When setting the material properties in the model, we retrieved existing material data in previous studies (Lee et al., 2005; Boubaker et al., 2009; Zhang et al., 2009; Rao et al., 2010; Venugopala Rao et al., 2010; Wein, 2011; Larson et al., 2012; Chen, 2014; Sichting et al., 2014; Brandão et al., 2015; Chen et al., 2015; Krcmar et al., 2015; Samavati et al., 2015; Sun, 2015; He, 2016; Ma et al., 2016; Peng et al., 2016; Silva et al., 2016; Dias et al., 2017; Li et al., 2017; Liu, 2017; Ricci et al., 2018; Guo et al., 2019; Li et al., 2019; Ma, 2019; Wu, 2019; Zhou et al., 2020; Xu et al., 2021; Xuan et al., 2021; Li, 2022; Yao et al., 2022; Zong, 2022), summarized the mechanical parameters recognized in the literature, and obtained the material properties of the research object in this study. Because the literature shows that there are differences in the mechanical performance characteristics of old and young pelvic soft tissues, and the material properties may change (Chantereau et al., 2014), we made appropriate adjustments on the of material properties, and we verified whether the data conditioning is appropriate by completing the verification steps of the finite element model, the specific parameters are shown in Table 1.
2.3 Constraint boundaries
The coordinates of the three-dimensional finite element model are set as follows: the x-axis is perpendicular to the sagittal plane of the human body, and the positive direction points to the left; the y-axis is perpendicular to the coronal plane of the human body, and the positive direction points backward; the z-axis is the longitudinal axis of the human body, and the positive direction points to the head. In the analysis of static structural mechanics, in order to simulate the in-body state of human defecation-related muscles as closely as possible, the bone is set as a rigid body and all nodes are fully constrained. We limited the translation and rotation of bones in the three axes of x, y and z. The tops of the rectus abdominis muscle, psoas major muscle, and erector spinae muscle are fixed. The contact condition between bones and muscles, bladder and prostate, prostate and colon were set to bind.
2.4 Model validity verification
In the finite element modeling process, it is very necessary to verify the validity of the finite element model. The methods of finite element model validation usually include geometric shape validation, literature result validation, and experimental result validation (Peng et al., 2023). Peng et al. (2016) conducted a validation study by comparing pelvic floor configurations achieved in computer simulation results with dynamic MRI observations along the midsagittal plane at both rest and maximal Valsalva maneuvers, and we highly recognize this geometric form validation method. Due to the lack of literature results and experimental results of elderly pelvic floor, It is very difficult to verify using methods such as literature results verification and experimental results verification. Therefore, We will compare the Valsalva maneuvers of the elderly during dynamic MRI scanning with the Valsalva maneuvers of the pelvic floor simulated by the finite element model, and compare whether the variety of the three anatomical landmark points of the two are consistent.
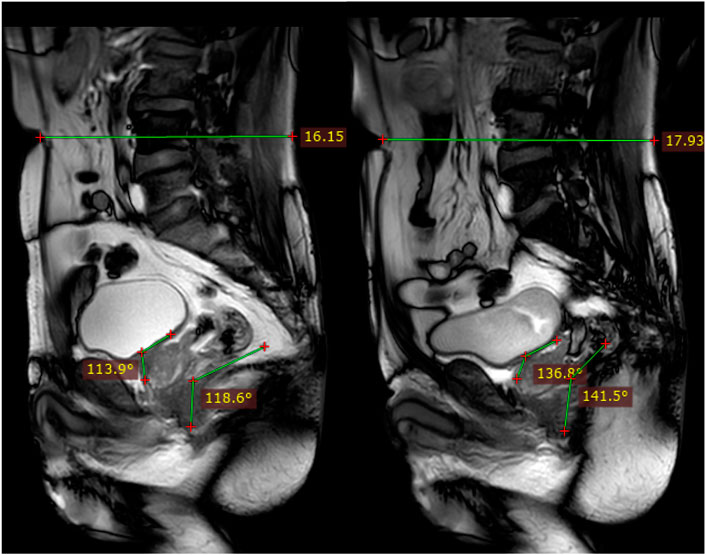
The specific process of dynamic MRI scanning is detailed in our previous research protocol (Wang et al., 2024) and we completed the Valsalva maneuvers through simulation of the finite element model. The Valsalva simulation plan’s loading site is the anterior abdominal wall, and in the resting state, E = 0.019 and the load is 0.5 kPa. At moderate tension, E = 0.241 and the load is 4.5 kPa. Under severe tension, E = 0.947 and the load is 5.0 kPa (Wu, 2019), and the direction of application is from the top of the anterior abdominal wall to the direction of the coccyx (Qiu, 2017). During model verification, the three anatomical landmarks include relative changes in waistline, changes in retrovesical angle (RVA) and changes in anorectad angulation (ARA). Among them, the RVA is the angle formed by the median sagittal plane of the bladder floor and the long axis of the urethra, and the ARA is the angle between the longitudinal axis of the anal canal and the posterior wall of the rectum above the levator ani muscle. These two angles are often measured in imaging data of the pelvic floor. Due to the lack of relevant research and guidelines specifying the scope of differences, we consulted relevant biomechanical experts and combined them with clinical situations. If the differences are within 10%, it will be considered that the model construction is more accurate.
2.5 Applied loads and simulation plans analysis
After completing the construction and verification of the finite element model, we will conduct specific finite element analysis under different simulation plans. Muscle elastic modulus refers to the ratio of deformation to the force applied on muscles and is a critical parameter for assessing muscle stiffness. Research has shown that rehabilitation exercises such as muscle contraction training and resistance movements can indirectly affect this modulus, resulting in decreased passive stiffness and increased muscle softness and flexibility (de Sousa et al., 2023). Since finite element analysis does not directly simulate rehabilitation training, we adapted simulation to reflect muscle capacity changes after rehabilitation training. So, we simulated a 25%, 50%, 75%, 100% strengthening in muscle capacity, a normal muscle capacity, a 25%, 50%, 75%, 95% impairment in muscle capacity. These adjustments were achieved by varying the material properties’ correlation properties to 1.25x, 1.5x, 1.75x, 2x (for increases), 1x (for baseline), 0.75x, 0.5x, 0.25x, and 0.05x (for decreases), respectively.
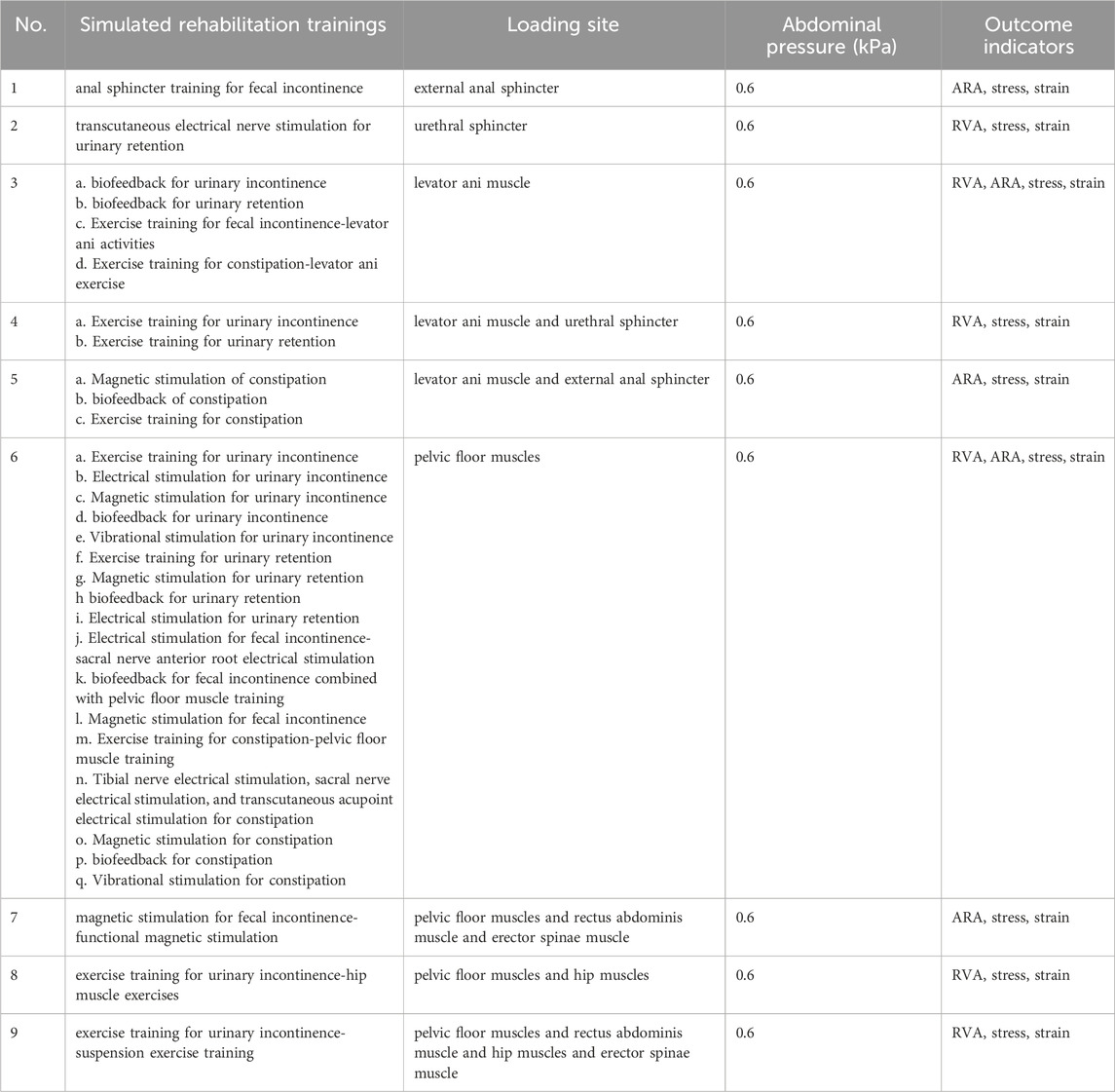
Currently, there are five known rehabilitation training methods for improving bowel function including exercise training, biofeedback, electrical stimulation, magnetic stimulation, and vibrational stimulation. Table 2 lists the muscles based on the literature content corresponding to the five types of rehabilitation training for the four types of urination and defecation dysfunction. We found that the five rehabilitation training methods mainly enhance the elderly’s urination and defecation abilities through muscle training, such as external anal sphincter, urethral sphincter, levator ani muscle, pelvic floor muscles, rectus abdominis muscle, hip muscles and erector spinae muscle. When performing finite element analysis, delete tissues and muscles that are weakly related to urination and defecation from the established finite element model, such as obturator internus muscle, skin, fat, pyramidal muscle, tensor fascia lata muscle, pubic muscle and latissimus dorsi muscle.
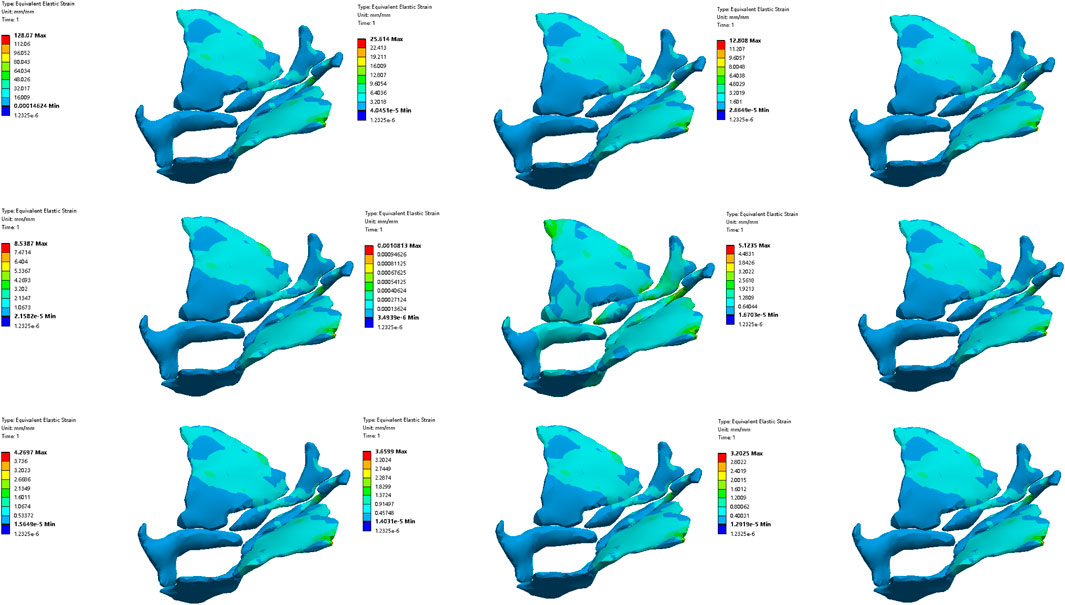
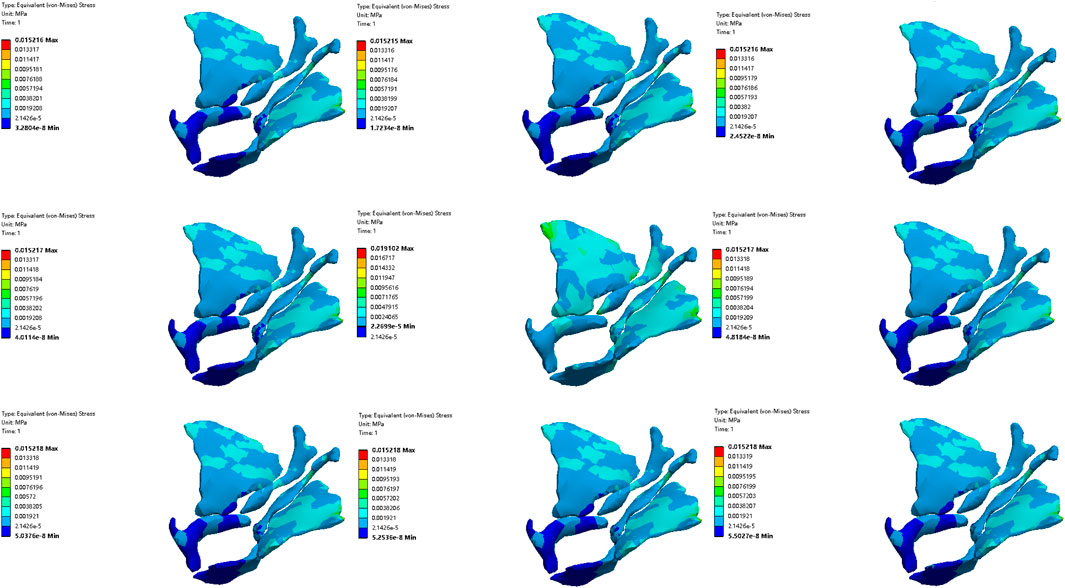
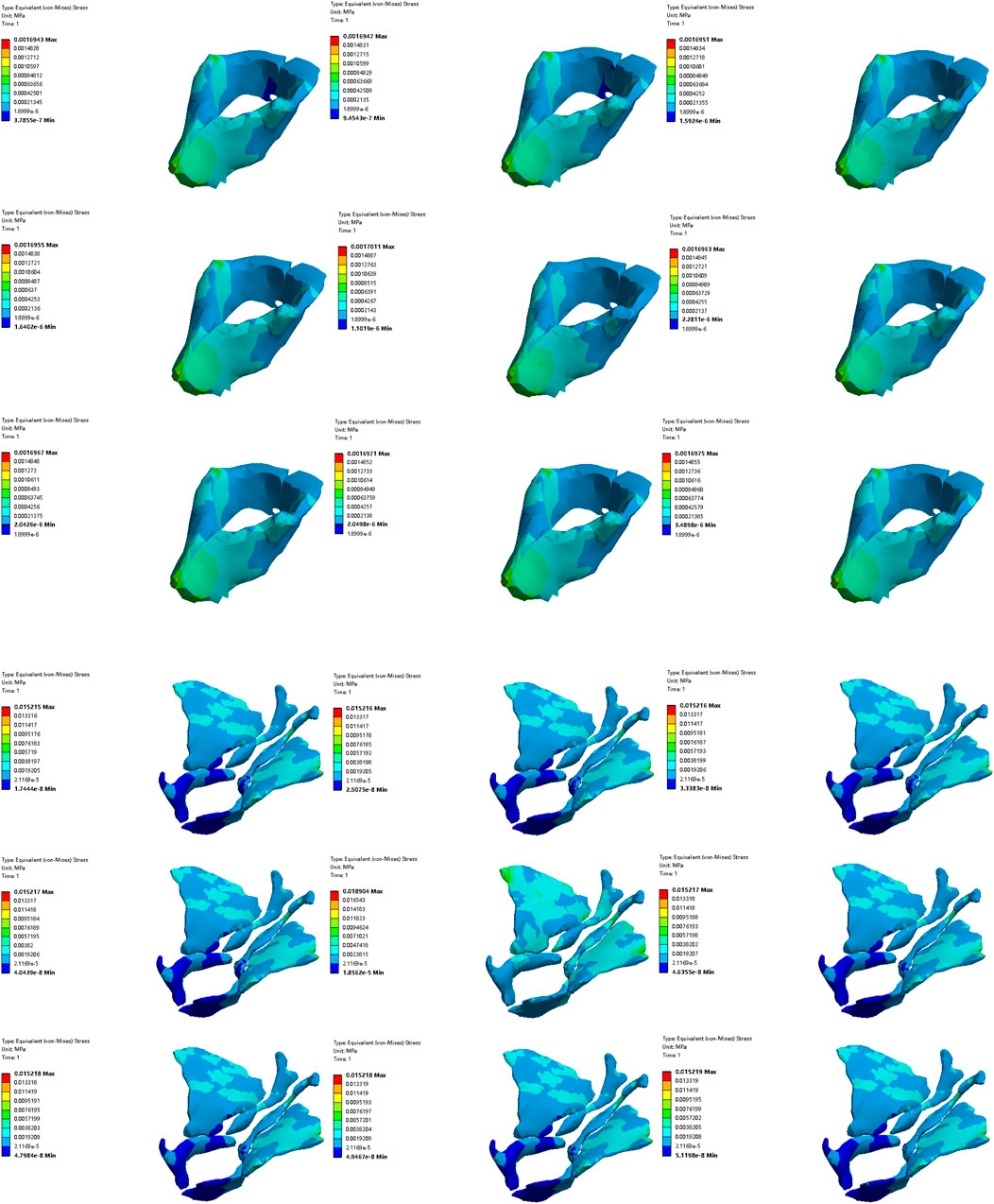
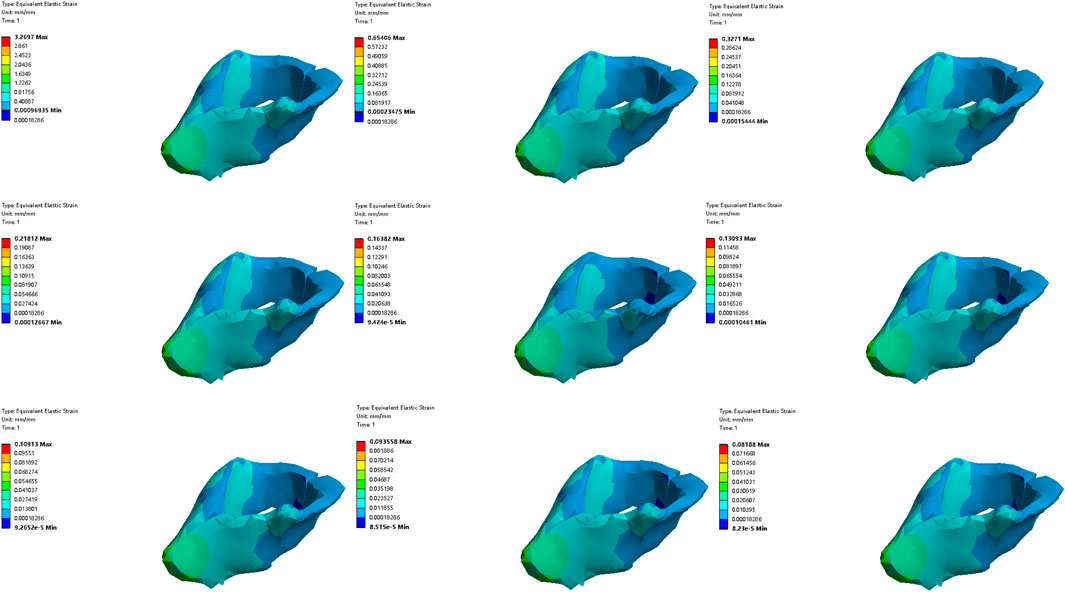
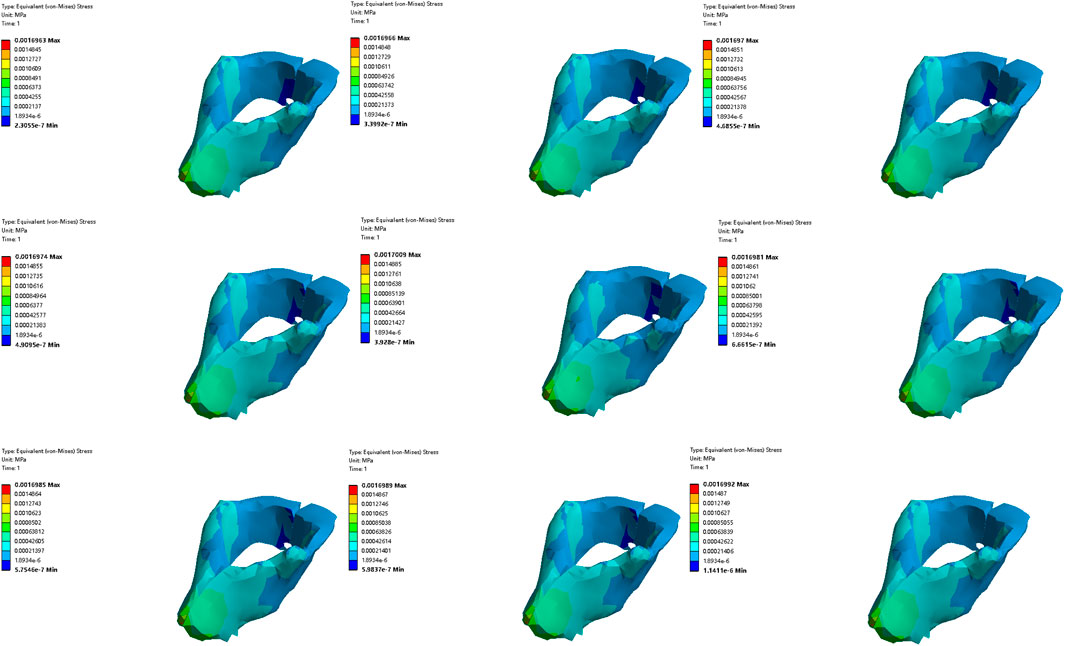
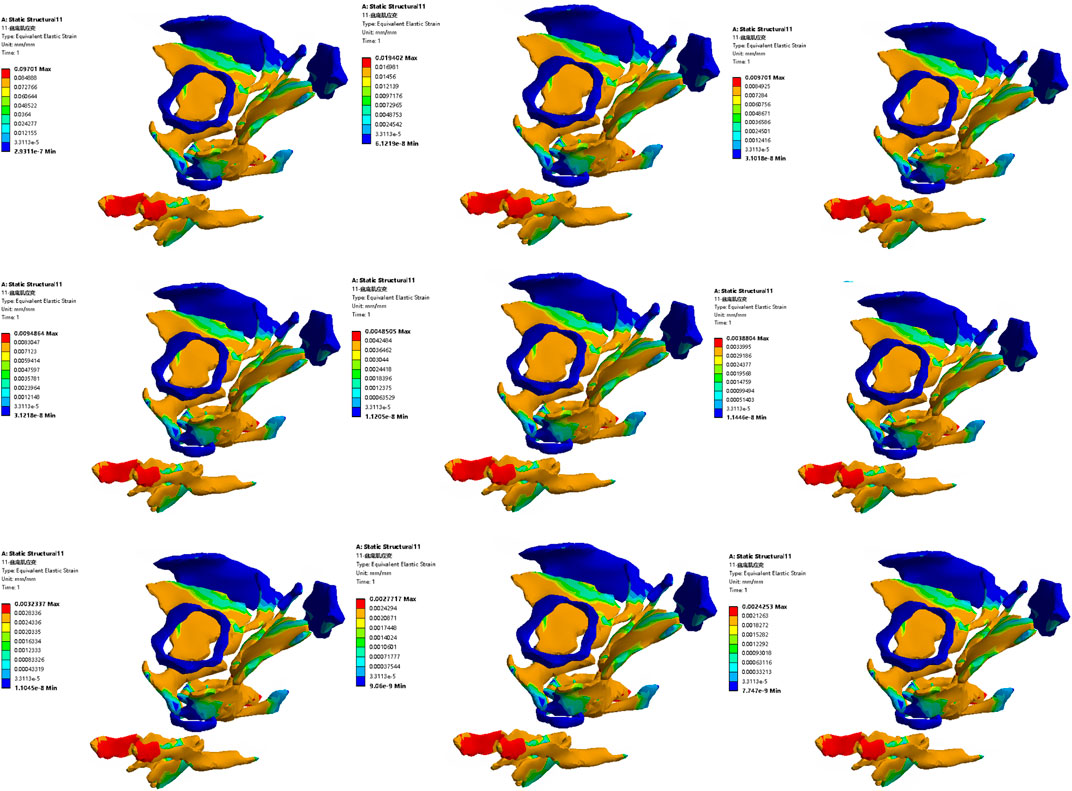
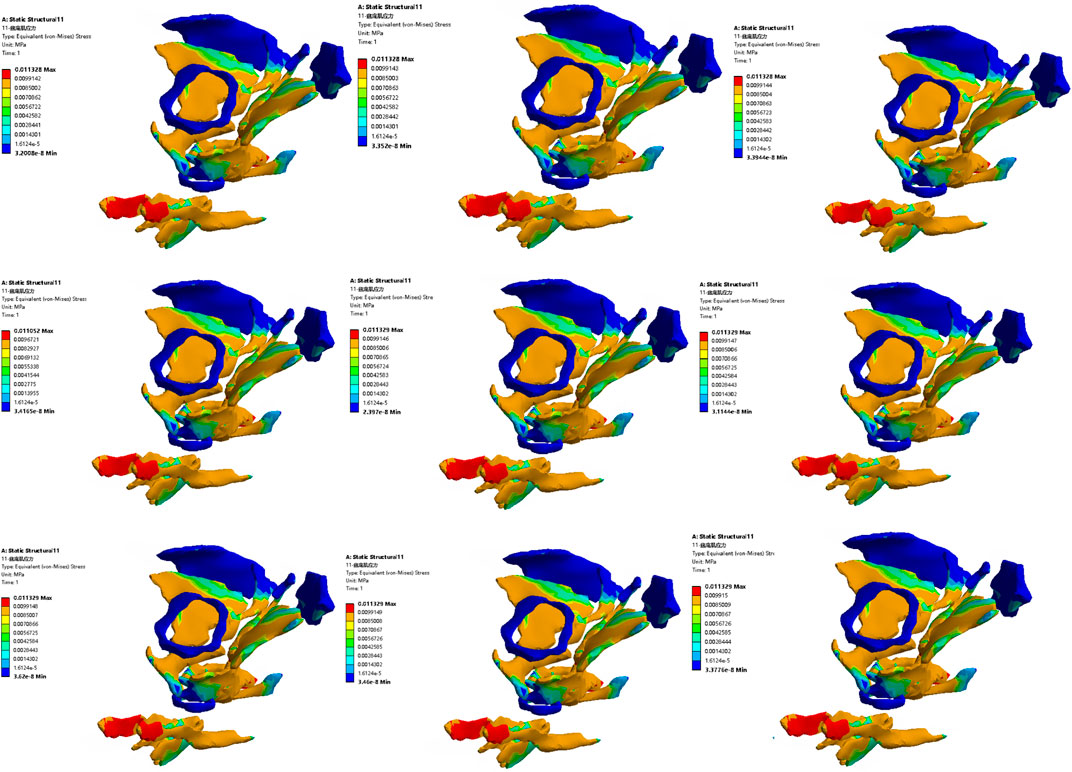
Regarding intra-abdominal pressure, a search of the literature shows that the resting intra-abdominal pressure is 0.4–0.64 kPa (Song et al., 2012), and the abdominal pressure in another literature was 0.665 kPa (Korkmaz and Rogg, 2007), so the abdominal pressure was selected as 0.6 kPa in our study. The main outcome measure of the study are RVA and ARA, which are well-known parameters for evaluating the control ablity of urination and defecation dysfunction (Guo et al., 2015; Zhou and Lai, 2021). The second outcome measure of the study are the von Mises stress cloud map and strain region of the area in the finite element model of elderly men under different simulation plans. The simulation plans table is listed in Table 2. The first two columns list the test number and the simulated rehabilitation trainings, and the third column lists the loading site. The first to ninth simulation plans simulate the muscle strengthening or impairment effects of the five types of rehabilitation training for the four types of urination and defecation dysfunction.
3 Results
3.1 Finite element model establishment
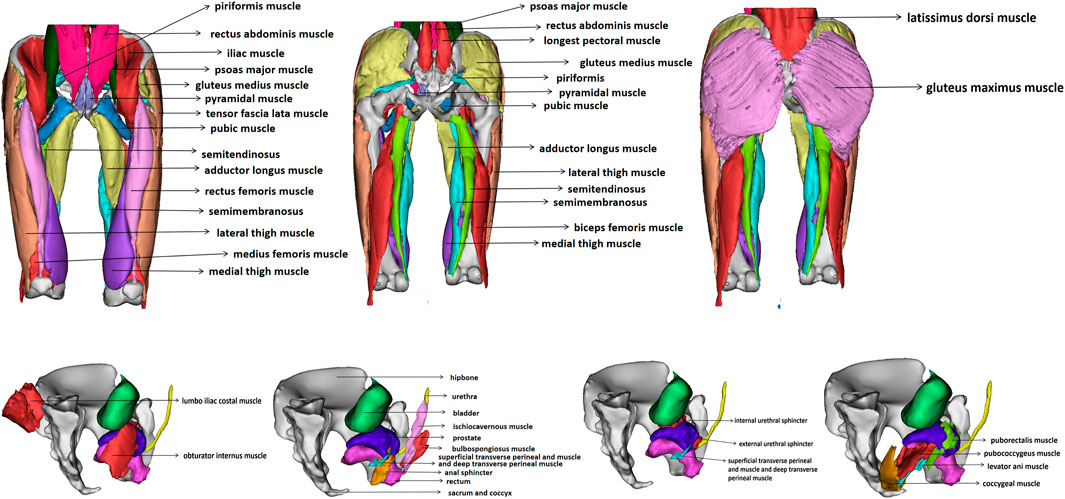
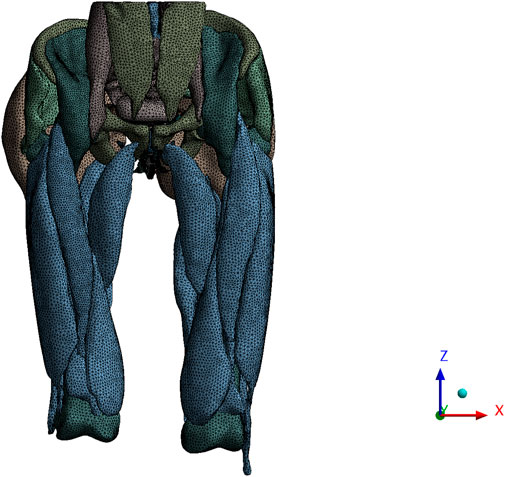
The finite element model includes the final three-dimensional pelvic floor model including organs including bladder, urethra, rectum and prostate, bones including hipbone, sacrum, coccyx and femur, pelvic floor muscles including bulbocavernosus muscle, ischiocavernosus muscle, superficial transverse perineal muscle, deep transverse perineal muscle, external anal sphincter, external urethral sphincter, coccygeal muscle, pubococcygeus muscle, iliococcygeus muscle, puborectalis muscle and obturator internal muscle, abdominal muscles including rectus abdominis muscle and pyramidal muscle, hip muscles including iliacus muscle, psoas major muscle, rectus femoris muscle, vastus lateralis muscle, vastus intermedius muscle, vastus medialis muscle, tensor fascia lata muscle, gluteus maximus muscle, gluteus medius muscle, piriformis muscle, semitendinosus muscle, semimembranosus muscle, biceps femoris muscle, pubic muscle and adductor longus muscle, back muscles including latissimus dorsi muscle, iliocostalis muscle, longissimus thoracis muscle, skin, fat, a total of 41 structures, 1188,251 nodes and 251,290 elements. Figure 4 shows the finite element model of old adult. Figure 5 is an annotation diagram of different muscle positions of the finite element model. Figure 6 shows the mesh division of the finite element model.
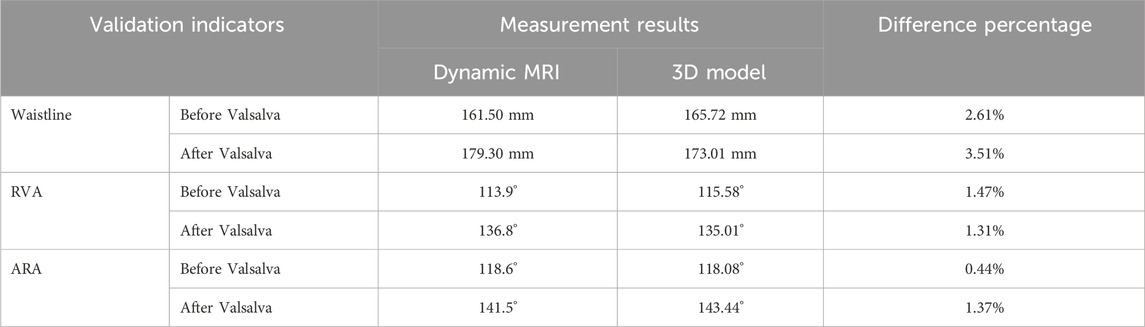
3.2 Verification of finite element model
We compared pelvic floor changes achieved along the midsagittal plane in computer simulations with imaging observations of Valsalva maneuvers in dynamic MRI. The results showed that the relative changes in waistline, RVA and ARA are within 3.51%, indicating a high consistency between the simulated situation constructed in the study and the actual pelvic floor situation of the elderly, as shown in Figure 7. The comparison of dynamic MRI and 3D model measurement results are shown in Table 3.
3.3 Finite element simulation plans analysis results
3.3.1 Results of changes in ARA and RVA with material properties
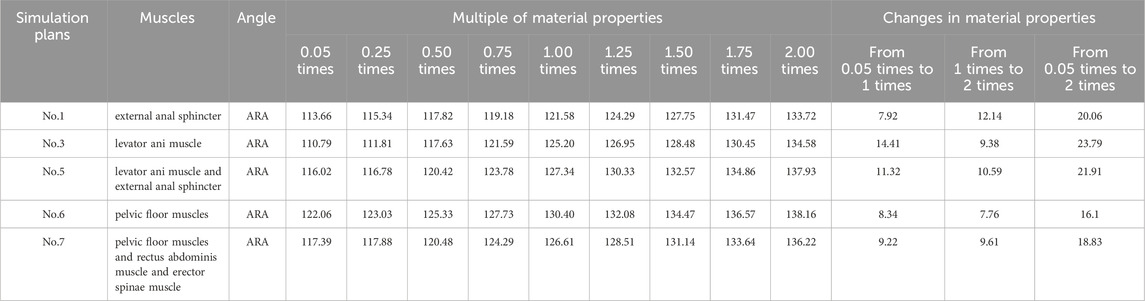
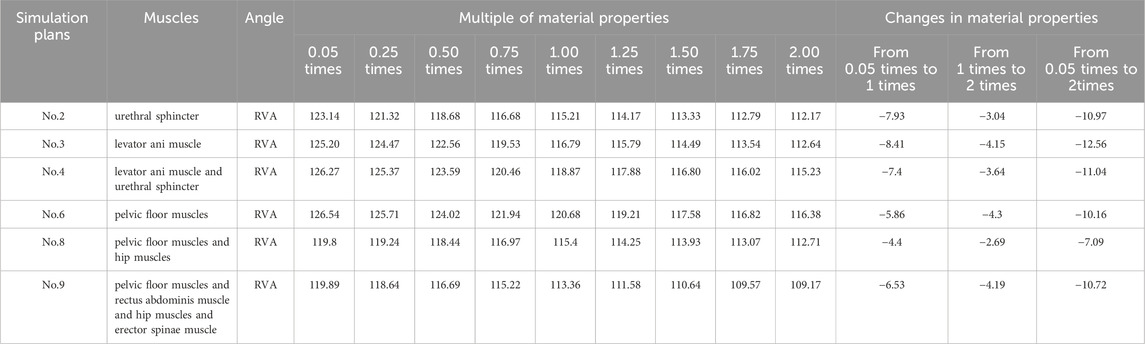
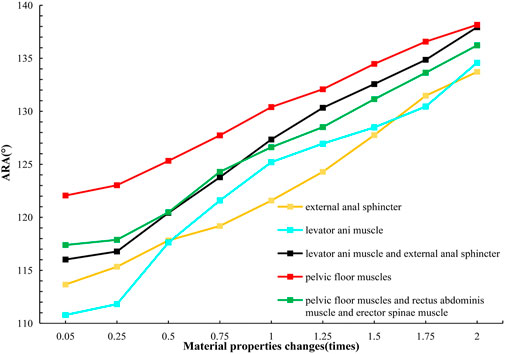
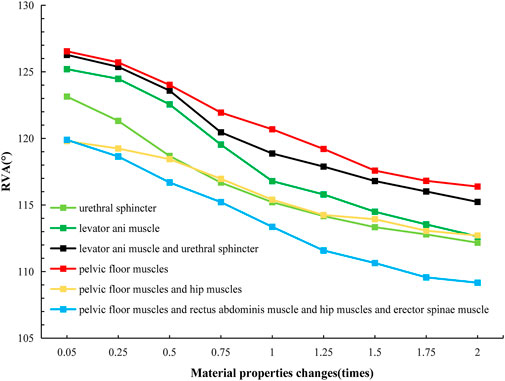
We analyzed the numerical changes of ARA and RVA in response to varying material properties respectively, illustrating how these changes correlate with the urinary and defecation abilities of elderly individuals. These relationships are depicted through changes in muscle strength associated with specific defecation and urinary rehabilitation training methods, as shown in Table 4 and 5. Figures 8, 9 present line graphs illustrating the angular responses (ARA and RVA) of five distinct muscle or muscle group combinations to variations in material properties. The x-axis quantifies the changes in material properties as multiplicative factors ranging from 0.05 to 2 times, while the y-axis displays the angular response values, with AVA ranging from 110° to 140°and RVA from 105° to 135°. Figure 8 illustrates that with the increase of material properties, the ARA consistently rises under simulation plans 1, 3, 5, 6, and 7. Conversely, as shown in Figure 9, the RVA diminishes with increasing in material properties under simulation plans 2, 3, 4, 6, 8, and 9. The variation in the slope of each line demonstrates the sensitivity of different muscle groups to changes in material properties.
3.3.2 Comparative analysis of simulated rehabilitation muscles for constipation and fecal incontinence
Simulation plans 3, 5, and 6 were designed to simulate the muscles strengthening and impairment effects on muscles implicated in constipation rehabilitation training. The muscles examined include levator ani muscle, levator ani muscle and external anal sphincter, and pelvic floor muscles. Comparative analysis of improvement of ARA across different simulations, if rehabilitation training gradually changes the material properties of muscles in elderly people from below normal to normal, the training effect of levator ani muscle is better than that of levator ani muscle, external anal sphincter, and pelvic floor muscles in sequence (Figures 10, 11). When the material properties of muscles gradually changes from greater than the normal value to the normal value, the training effect of levator ani muscle and external anal sphincter is better than levator ani muscle and pelvic floor muscles in sequence (Figures 12, 13).
Simulation plans 1, 3, 6, and 7 were designed to simulate the muscles strengthening and impairment effects of fecal incontinence rehabilitation training, among which the muscles included external anal sphincter, levator ani muscle, pelvic floor muscles, pelvic floor muscles and rectus abdominis muscle and erector spinae muscle. By comparing the improvement degree of ARA under different simulations, when rehabilitation training gradually changes the material properties of muscles in elderly people from less than normal to normal the training effect of levator ani muscle is better than that of pelvic floor muscles and rectus abdominis muscle and erector spinae muscle, pelvic floor muscles, and external anal sphincter, sequentially (Figures 10, 11). As the material properties of muscles gradually changes from approach normalcy from above-normal levels, the training effect of external anal sphincter is better than that of pelvic floor muscles and rectus abdominis muscle and erector spinae muscle, levator ani muscle, and pelvic floor muscles, respectively (Figures 14, 15).
It is noteworthy that regardless of muscle material properties in elderly people, training the levator ani muscle alone yields better outcomes than training it as part of the pelvic floor group for managing constipation and fecal incontinence in the elderly. Furthermore, regardless of the state of muscle material properties in the elderly, a comprehensive training approach that includes pelvic floor muscles, rectus abdominis, and erector spinae muscles proves more effective than focusing solely on the pelvic floor muscles in constipation and fecal incontinence rehabilitation trainings.
3.3.3 Comparative analysis of simulated rehabilitation muscles for urinary incontinence and urinary retention
Simulation plans 3, 4, 6, 8, and 9 were designed to simulate the muscles enhancement and impairment effects of urinary incontinence rehabilitation training. The targeted muscle groups included levator ani muscle, levator ani muscle and urethral sphincter, pelvic floor muscles, pelvic floor muscles and hip muscles, pelvic floor muscles and rectus abdominis muscle and hip muscles and erector spinae muscle. By comparing the degree of improvement in RVA under different simulations, it can be indicated that rehabilitation training progressively changes the material properties of muscles in elderly people from less than normal to normal, the efficacy of training the levator ani muscle alone surpassed that of combined training with the urethral sphincter, and also outperformed the broader group training involving pelvic floor muscles and rectus abdominis muscle and hip muscles and erector spinae muscle, pelvic floor muscles, pelvic floor muscles and hip muscles, sequentially (Figures 10, 11). Furthermore, when the material properties of the muscles from greater than the normal value to the normal value, the training effectiveness of the pelvic floor muscles excelled over that of the pelvic floor muscles and rectus abdominis muscle and hip muscles and erector spinae muscls, levator ani muscles, levator ani muscles and urethral sphincter, and pelvic floor muscles and hip muscles in sequence (Figures 16, 17).
Simulation plans 2, 3, 4, and 6 were designed to simulate the muscles strengthening and impairment effects of urinary retention rehabilitation training. The muscles include urethral sphincter, levator ani muscle, levator ani muscle and urethral sphincter, and pelvic floor muscles. By comparing the degree of improvement in RVA under different simulations, it can be concluded that rehabilitation training gradually changes the material of muscles in elderly people from less than normal to normal, and the training’s efficacy on levator ani muscle surpassed urethral sphincter alone and levator ani muscle combined with the urethral sphincter (Figures 10, 11). The training’s efficacy on levator ani muscle and also exceeded training effects on pelvic floor muscles. In addition, when the material properties of the muscles gradually changes from greater than the normal value to the normal value, the effect of pelvic floor muscles is superior to those involving levator ani muscle alone, or levator ani muscle in combination with urethral sphincter, and urethral sphincter alone respectively (Figures 16, 17).
It should be noted that irrespective of the muscle material properties in the elderly, the training of the levator ani muscle alone demonstrates superior effectiveness over combined training with the urethral sphincter in managing urinary incontinence and retention. Furthermore, both individual and combined training of pelvic floor muscles with rectus abdominis muscles, hip muscles, erector spinae muscles provide more significant benefits compared to training that combines only the pelvic floor muscles with hip muscles.
Moreover, it was observed that alterations in the material properties of muscles from 0.05 to 0.25 times did not significantly impact the ARA. Similarly, when the muscle material properties ranged from 1.50 to 2.00 times, there was no significant change in the RVA.
4 Discussion
This study gathered muscles medical imaging from a elderly male to develop and verified a finite element model. This study explored the quantitative relationship between rehabilitation training methods on muscles and urinary and defecation dysfunction, ultimately elucidating the mechanism of improving urinary and defecation dysfunction. One of the advantages of finite element models is that they provide a cost-effective solution for studying complex biomechanical processes, such as rehabilitation training for bowel and bladder functions, without the need for extensive resources, specialists, or equipment. Additionally, these models enhance safety by eliminating the potential risks associated with human trials. Due to the consistent reproducibility of computations, finite element models are able to deliver highly repeatable results. Previous studies have developed some pelvic floor finite element models for the treatment of urinary incontinence, however that predominantly focused on young postpartum women (Hu and Pierre, 2019), leading to a gap in models suited for older men. Male and female pelvic floor anatomy are different, and aging individuals experience physiological changes including decreased muscle strength and changes in pelvic floor tissue relaxation and elasticity. Currently, there is a lack of finite element model of the pelvic floor for analyzing fecal incontinence, constipation, urinary incontinence and urinary retention in elderly men, therefore it is very necessary to construct a finite element model of the pelvic floor of elderly men to guide rehabilitation and treatment. In addition, our model also integrates additional muscular systems, such as those of the back, hip, and abdomen, which play significant roles in urination and defecation rehabilitation training and are often overlooked in existing models. This innovative approach is more conducive to simulating the rehabilitation training methods and measuring the quantitative relationship between five rehabilitation training methods and the urinary and defecation control ability of elderly men, which is also one of the innovative points of this study.
The primary structures that affect the ability to control bowel movements are mainly divided into three parts including pelvic floor muscles, core muscles and sacral nerves. Pelvic floor muscles are crucial for regulating urination, defecation, and maintaining vaginal contractions. Core muscles, encompassing the waist, abdomen, hips, and legs, serve as pivotal points for trunk movements, enhancing stability for the spine and pelvis, and increasing abdominal pressure. Sacral nerves play a vital role in managing the reflexes of the bladder, sphincters, and pelvic floor. In this study, we systematically investigatesd the impact of rehabilitation training on the urinary and defecation abilities of elderly by analyzing the angular changes of ARA and RVA in response to alterations in the material properties of involved muscles.
Regarding the changes in material properties of pelvic floor muscles in the elderly, it is observed that these tissues physiologically lose some elasticity due to aging, potentially reducing the Young’s module of soft tissues (Bhattarai and Staat, 2018). Regular muscle training or other healthy habits in some elderly individuals may increase the Young’s module, potentially reversing some age-related degenerative changes. It is important to note that changes in the Young’s module of pelvic floor muscles in the elderly are not absolute. These changes depend on individual characteristics, natural aging, disease types, and cannot be universally generalized. Hence, our study simulated a range of material properties from 0.05 to 2 times to accommodate various simulation scenarios.
The normal range of ARA and RVA vary, and the variability in results could be attributed to the individual differences among assessors or the participants. According to literature (Xue, 1996; Mortele and Fairhurst, 2007; Colaiacomo et al., 2009; Bitti et al., 2014; Kobi et al., 2018; Zhou and Lai, 2021; The MR Group of the Radiology Branch of the Chinese Medical Association, 2022), the typical resting range of ARA is between 90° and 127°, while during defecation, it extends from 120° to 152.4°. The resting RVA spans from 90° to 120° (Liu et al., 2013). In cases of anterior pelvic dysfunction, RVA values can expand from the normal range of 90°–120°–160°–180°during the tension phases (Fielding et al., 2000). Some research also suggests that RVA for individuals with stress urinary incontinence may exceed 140° (Li and Yan, 2015). The results indicate that as the material properties of muscles or muscle groups change, ARA and RVA are gradually approaching the normal range. Therefore, theoretically, it can be posited that rehabilitation training methodologies including biofeedback, exercise training, electrical stimulation, magnetic stimulation, and vibration training may enhance the ability of elderly men to control bowel movements.
The responsiveness of different muscles to changes in ARA and RVA angles can be evaluated by comparing the slopes of each line in Tables 8 and 9. A higher slope indicates a greater responsiveness of that muscle or muscle combination to changes in ARA and RVA angles. Research findings indicate that individual training of specific muscle groups, particularly the levator ani muscle, proves more effective in treating disorders of both urination and defecation in the elderly compared to combined training with pelvic floor and urethral sphincter muscles. This could be due to the specific role that the levator ani muscle plays in supporting the pelvic organs and controlling the functions closely related to the bowel movements. While the specific research studies that the comparative effectiveness of isolated levator ani muscle training versus comprehensive pelvic floor muscle training might not be directly available, general principles of physical therapy and muscle rehabilitation suggest that targeted exercises can indeed improve the functionality of specific muscles more effectively than generalized training. A study reached a similar conclusion to ours, the study pointed out that with the increase of external load, the training effect on certain muscles significantly increases, while the training effect on other muscles is much smaller. The simulation results show that compared with pure weightlifting training, training based on optimal load orientation concept (OLOC) can significantly improve the training effect of specific muscles, and training methods targeting specific muscles maximize the training effect of target muscles (Song et al., 2018).
In addition, research findings indicate that targeted muscle rehabilitation training for the levator ani muscle and anal external anal sphincter in cases of fecal dysfunction, and for the levator ani muscle and pelvic floor muscles in cases of urinary dysfunction, theoretically holds the greatest potential for significant improvement in the urinary and defecation control ability of the elderly. Previous studies (Zhou and Lai, 2021) have highlighted that the key factors influencing individual urinary and defecation control ability include the levator ani muscle, puborectalis muscle, and external anal sphincter, all of which are closely associated with fecal dysfunction. Abnormalities in the structure or function of these muscles lead to bowel control problems. This aligns with the conclusions of our research, which suggests that optimizing the function of the peri-anal muscle group is essential for improving urinary and defecation control ability. Furthermore, for urinary function, the pelvic floor muscles are the most critical source of support (Li and Lu, 2023), with the levator ani muscle playing a significant supportive role (Ashton-Miller and DeLancey, 2007). The literature (Zhou et al., 2020) pointed out that pelvic floor muscle exercise, mainly involving the levator ani muscle, is a method for treating pelvic floor dysfunction diseases. Pelvic floor muscles rehabilitation training, including Kegel exercises, pelvic floor muscle training, biofeedback training, electrical stimulation, and acupuncture, is commonly used in elderly males post-laparoscopic radical prostatectomy (Feng, 2022) and for managing lower urinary tract symptoms post-stroke (Tibaek et al., 2017).
In conclusion, these results are significant for understanding and treating muscle-related urination and defecation dysfunction. The findings emphasize the importance of personalized and targeted rehabilitation approaches in effectively addressing pelvic floor dysfunctions. Some studies (Okada et al., 2001; Tang et al., 2020) have employed shear wave elastography (SWE) to assess the biomechanical properties of pelvic floor muscles. Future research should further explore how specific rehabilitation training methods practically affect muscle material properties, aiming to adjust these properties through tailored exercises to improve bowel disorders in the elderly. When designing and implementing targeted rehabilitation training, it is recommended to advocate for personalized and dynamic treatment plans. Specifically, the response characteristics of different muscles under varying stress conditions should be considered, and training intensity and muscle group rehabilitation strategies should be adjusted based on the changes in muscle material properties to enhance the effectiveness of rehabilitation training for the elderly.
The study acknowledges several limitations. Firstly, due to constraints, this study was conducted on a single elderly male subject, and the results may not fully represent all elderly men. Secondly, the complexity of the human body necessitated the simplification of certain biomechanical processes. This includes a focus on specific muscle groups, such as the abdominal muscles specifically refer to the rectus abdominis, and the hip muscles specifically refer to the iliopsoas, quadriceps, gluteus maximus, hamstrings, gluteus medius, and adductor longus The back muscles were specifically the erector spinae, without incorporating ligament roles or all muscle combinations. Third, while the study provides insights into muscle functionality and its effects on rehabilitation outcomes, the results of this study are based on the relationship between muscles and ARA, RVA, and it does not a direct relationship between rehabilitation training methods and urinary and defecation control ability. This possibly leading to over-idealized conclusions. In actual rehabilitation training, it may not be possible to train a single muscle alone, and it is also difficult to achieve proportional changes in muscles. However, this research offers a methodological approach to explain the mechanism of urinary and defecation control ability and elucidates the potential mechanisms linking rehabilitation training methods with the urinary and defecation control ability in the elderly.
5 Conclusion
In conclusion, by constructing and verificating a finite element model the study demonstrates that rehabilitation training, including exercise training, electrical stimulation, magnetic stimulation, biofeedback, and vibration stimulation, can improve the urinary and defecation control ability of elderly men. Crucially, the research results highlights the pivotal role of the levator ani muscle, external anal sphincter, and pelvic floor muscles in the managing of urination and defecation dysfunction. Moreover, this study emphasizes the effectiveness of targeted rehabilitation training in restoring urinary and defecation control among the elderly, emphasizing the need to adjust muscle training intensity and method based on the individual’s muscle material properties to optimize therapeutic outcomes.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Xuanwu Hospital, Capital Medical University and Ethics Committee of Capital Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
RW: Data curation, Formal Analysis, Investigation, Methodology, Software, Validation, Writing–original draft, Writing–review and editing. GL: Formal Analysis, Methodology, Supervision, Validation, Writing–review and editing. LJ: Formal Analysis, Funding acquisition, Resources, Supervision, Writing–review and editing. JZ: Formal Analysis, Methodology, Supervision, Writing–review and editing. YY: Data curation, Writing–review and editing. HZ: Data curation, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study is supported by the National Key R&D (research and development) Program of China (grant 2022YFB4703300). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of National Key R&D Program of China.
Acknowledgments
Thanks to Zhu Ying from Peking University First Hospital, Wu Chunxue from Xuanwu Hospital of Capital Medical University, professor Qian Xiuqing from Biomedical Engineering College of Capital Medical University, Zhang Zhiyong from North China University of Science and Technology for their guidance and help in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alouini, S., Memic, S., and Couillandre, A. (2022). Pelvic floor muscle training for urinary incontinence with or without biofeedback or electrostimulation in women: a systematic review. Int. J. Environ. Res. Public Health 19 (5), 2789. doi:10.3390/ijerph19052789
Ashton-Miller, J. A., and DeLancey, J. O. (2007). Functional anatomy of the female pelvic floor. Ann. N. Y. Acad. Sci. 1101, 266–296. doi:10.1196/annals.1389.034
Bektas, A. N., Unal, N., and Akpinar, C. (2023). Urinary incontinence in older adults: impact on caregiver burden. J. Gerontol. Nurs. 49 (4), 39–46. doi:10.3928/00989134-20230310-01
Bhattarai, A., and Staat, M. (2018). Modelling of soft connective tissues to investigate female pelvic floor dysfunctions. Comput. Math. Methods Med. 2018, 1–16. doi:10.1155/2018/9518076
Bitti, G. T., Argiolas, G. M., Ballicu, N., Caddeo, E., Cecconi, M., Demurtas, G., et al. (2014). Pelvic floor failure: MR imaging evaluation of anatomic and functional abnormalities. Radiographics 34 (2), 429–448. doi:10.1148/rg.342125050
Boubaker, M. B., Haboussi, M., Ganghoffer, J. F., and Aletti, P. (2009). Finite element simulation of interactions between pelvic organs: predictive model of the prostate motion in the context of radiotherapy. J. Biomech. 42 (12), 1862–1868. doi:10.1016/j.jbiomech.2009.05.022
Brandão, S., Parente, M., Mascarenhas, T., da Silva, A. R. G., Ramos, I., and Jorge, R. N. (2015). Biomechanical study on the bladder neck and urethral positions: simulation of impairment of the pelvic ligaments. J. Biomech. 48 (2), 217–223. doi:10.1016/j.jbiomech.2014.11.045
Chantereau, P., Brieu, M., Kammal, M., Farthmann, J., Gabriel, B., and Cosson, M. (2014). Mechanical properties of pelvic soft tissue of young women and impact of aging. Int. Urogynecol J. 25 (11), 1547–1553. doi:10.1007/s00192-014-2439-1
Chen, W., Yan, Z. H., and Wu, L. J. (2010). Finite element analysis of female pelvic floor anal elevator muscle. Chin. J. Tissue Eng. Res. Clin. Rehabilitation 14 (43), 8125–8128. doi:10.3969/j.issn.1673-8225.2010.43.036
Chen, Z. W., Joli, P., Feng, Z. Q., Rahim, M., Pirró, N., and Bellemare, M. E. (2015). Female patient-specific finite element modeling of pelvic organ prolapse (POP). J. Biomech. 48 (2), 238–245. doi:10.1016/j.jbiomech.2014.11.039
Colaiacomo, M. C., Masselli, G., Polettini, E., Lanciotti, S., Casciani, E., Bertini, L., et al. (2009). Dynamic MR imaging of the pelvic floor: a pictorial review. Radiographics 29 (3), e35. doi:10.1148/rg.e35
Chen, Q. Q. (2014). A finite element studies of the different functions for the ligaments of the uterus in maintaining uterine in the normal position[D]. Shanghai: Fudan University.
de Sousa, A. M. M., Cavalcante, J. G. T., Bottaro, M., Vieira, D. C. L., Babault, N., Geremia, J. M., et al. (2023). The influence of hip and knee joint angles on quadriceps muscle-tendon unit properties during maximal voluntary isometric contraction. Int. J. Environ. Res. Public Health 20 (5), 3947. Published 2023 Feb 23. doi:10.3390/ijerph20053947
Dias, N., Peng, Y., Khavari, R., Nakib, N. A., Sweet, R. M., Timm, G. W., et al. (2017). Pelvic floor dynamics during high-impact athletic activities: a computational modeling study. Clin. Biomech. (Bristol, Avon) 41, 20–27. doi:10.1016/j.clinbiomech.2016.11.003
Feng, Y. Y. (2022). Application study of pelvic floor rehabilitation plan based on Cox health behavior interaction model in patients with urinary incontinence after laparoscopic radical prostatectomy[D]. Jiangnan University. doi:10.27169/d.cnki.gwqgu.2022.002315
Fielding, J. R., Dumanli, H., Schreyer, A. G., et al. (2000). MR-based threedimentional modeling of the normal pelvic floor. AJR 174 (3), 567–660. doi:10.2214/ajr.174.3.1740657
Guo, E. F., Ma, L., Kan, Y. M., Zhang, S. H., Sun, M., Liu, Y., et al. (2015). The application value of transperineal ultrasound in female stress urinary incontinence. Chin. J. Clin. Med. Imaging 26 (03), 197–199.
Guo, P. N., Zhang, Z. Y., and Gao, Y. (2019). Design and Finite element analysis of customized pelvic prosthesis. China J. Orthop. traumatology 32 (06), 564–568. doi:10.3969/j.issn.1003-0034.2019.06.016
He, J. L. (2016). Anatomy studies and finite element analysis for unstable posterior pelvic ring di sruptions treated with tension band pIate[D]. Shandong University. doi:10.7666/d.Y3037037
Hu, J. S., and Pierre, E. F. (2019). Urinary incontinence in women: evaluation and management. Am. Fam. Physician 100 (6), 339–348.
Kobi, M., Flusberg, M., Paroder, V., and Chernyak, V. (2018). Practical guide to dynamic pelvic floor MRI. J. Magn. Reson Imaging 47 (5), 1155–1170. doi:10.1002/jmri.25998
Korkmaz, I., and Rogg, B. (2007). A simple fluid-mechanical model for the prediction of the stress-strain relation of the male urinary bladder. J. Biomech. 40 (3), 663–668. doi:10.1016/j.jbiomech.2006.02.014
Krcmar, M., Krofta, L., Urbankova, I., Reisl, J. F., Havelkova, L., and Hyncik, L. (2015). “Biomechanical properties of levator ani muscle used for virtual model of pelvic floor,”. International Urogynecology Journal, S163–S164. SPRINGER LONDON LTD 236 GRAYS INN RD, 6TH FLOOR, LONDON WC1X 8HL, ENGLAND.
Larson, K. A., Luo, J., Guire, K. E., Chen, L., Ashton-Miller, J. A., and DeLancey, J. O. L. (2012). 3D analysis of cystoceles using magnetic resonanceimaging assessing midline, paravaginal, and apical defects. Int. urogynecolog J. 23 (3), 285–293. doi:10.1007/s00192-011-1586-x
Lee, S. L., Darzi, A., and Yang, G. Z. (2005). Subject specific finite element modelling of the levator ani. Med. Image Comput. Assist. Interv. 8 (Ptl), 360–367. doi:10.1007/11566465_45
Levaillant, M., Venara, A., Damon, H., Siproudhis, L., Brochard, C., and Hamel, J. F. (2023). Young women and elderly men at risk of severe faecal incontinence: results of a French nationwide database analysis: faecal incontinence in France. Int. J. Colorectal Dis. 38 (1), 131. doi:10.1007/s00384-023-04431-8
Li, D., and Lu, R. (2023). Research progress in pelvic floor ultrasound for assessing the morphology and function of levator ani muscle in women. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 48 (8), 1267–1273. doi:10.11817/j.issn.1672-7347.2023.220577
Li, G., Tan, Z., Lv, X., and Ren, L. (2019). A computationally efficient finite element pedestrian model for head safety: development and validation. Appl. Bionics Biomech. 2019, 1–13. doi:10.1155/2019/4930803
Li, H. Y., Cui, Z. Y., Cui, S. H., Ruan, S. J., and He, L. J. (2017). Development and validation of a finite element model for a 6-year-old child pelvis. Chin. J. Automot. Eng. 7 (2), 100–105. doi:10.3969/j.issn.2095-1469.2017.02.04
Li, J. Q., and Yan, H. F. (2015). Clinical exploration of ultrasound measurement of bladder neck mobility and posterior angle of bladder urethra in the diagnosis of stress urinary incontinence in middle-aged and elderly women. J. Changzhi Med. Coll. 29 (04), 287–289. doi:10.3969/j.issn.1006-0588.2015.04.018
Li, S. (2022). Computer simulation biomechanical research based on magnetic resonance imaging of female pelvic organ prolapse[D]. Kunming Medical University. doi:10.27202/d.cnki.gkmyc.2022.000772
Liu, F. F., Xu, L., Ying, T., Tao, J. J., and Hu, B. (2013). The value of perineal ultrasound in the diagnosis of anterior pelvic dysfunction in women. Chin. J. Ultrasound Imaging 22 (12), 1063–1066. doi:10.3760/cma.j.issn.1004-4477.2013.12.016
Liu, X. (2017). Finite element modeling of pelvic floor muscles in female patients with moderate to severe stress urinary incontinence and simulation stress analysis of storage and leakage state[D]. Shanxi Medical University.
Ma, X. B., and Chen, C. X. (2020). The defecation status and its impact on physical and mental health of elderly people. Chin. J. Gerontology 40 (18), 3983–3986. doi:10.3969/j.issn.1005-9202.2020.18.053
Ma, X. X., Shi, S. Y., Xi, B., Chan, Y., Sun, X. L., Yang, X., et al. (2016). Stress distribution and deformation of uterosacral ligament and cardinal ligament under different working conditions simulated by the finite element model. Chin. J. Obstet. Gynecol. 51 (2), 14–19. doi:10.3760/cma.j.issn.0529-567X.2016.02.007
Ma, Z. J. (2019). Study on the mechanism of pelvic vascular injury by lateral impact[D]. Nanjing Medical University. doi:10.27249/d.cnki.gnjyu.2019.000006
Mazur-Bialy, A. I., Kołomańska-Bogucka, D., Nowakowski, C., and Tim, S. (2020). Urinary incontinence in women: modern methods of physiotherapy as a support for surgical treatment or independent therapy. J. Clin. Med. 9 (4), 1211. doi:10.3390/jcm9041211
Mortele, K. J., and Fairhurst, J. (2007). Dynamic MR defecography of the posterior compartment: indications, techniques and MRI features. Eur. J. Radiol. 61, 462–472. doi:10.1016/j.ejrad.2006.11.020
Okada, Y., Nakagawa, C., Shigeta, M., Nomura, Y., Inoue, E., Ichizuka, K., et al. (2001)2024). Evaluation of levator ani muscle elasticity after vaginal delivery and cesarean section using shear wave elastography. J. Med. Ultrason. 51 (1), 95–101. doi:10.1007/s10396-023-01369-w
Peng, L., Duan, Z. L., Li, Z. Y., Li, J. H., Li, Y. H., Wang, S., et al. (2023). Research status and progress on the establishment and validation of finite element models for adolescent idiopathic scoliosis. Chin. J. Tissue Eng. Res. 27 (27), 4393–4400. doi:10.12307/2023.388
Peng, Y., Khavari, R., Nakib, N. A., Boone, T. B., and Zhang, Y. (2016). Assessment of urethral support using MRI-derived computational modeling of the female pelvis. Int. Urogynecol J. 27 (2), 205–212. doi:10.1007/s00192-015-2804-8
Qiu, Z. Y. (2017). Finite element analysis and mechanical mechanism of posterior vaginal prolapsed based on MR imaging[D]. Fujian Medical University. doi:10.27020/d.cnki.gfjyu.2017.000067
Rao, G. V., Rubod, C., Brieu, M., Bhatnagar, N., and Cosson, M. (2010). Experiments and FE modeling for the study of prolapsed in the pelvic system. Comp. Meth Biomech. Biomed. Eng. 13 (3), 349–357. doi:10.1080/10255840903251270
Ricci, P. L., Maas, S., Kelm, J., and Gerich, T. (2018). Finite element analysis of the pelvis including gait muscle forces: an investigation into the effect of rami fractures on load transmission. J. Exp. Orthop. 5 (1), 33. doi:10.1186/s40634-018-0151-7
Salari, N., Ghasemianrad, M., Ammari-Allahyari, M., Rasoulpoor, S., Shohaimi, S., and Mohammadi, M. (2023). Global prevalence of constipation in older adults: a systematic review and meta-analysis. Wien Klin. Wochenschr 135 (15-16), 389–398. doi:10.1007/s00508-023-02156-w
Samavati, N., Mcgrath, D. M., Jewett, M. A., van der Kwast, T., Ménard, C., and Brock, K. K. (2015). Effect of material property heterogeneity on biomechanical modeling of prostate under deformation. Phys. Med. Biol. 60 (1), 195–209. doi:10.1088/0031-9155/60/1/195
Sichting, F., Rossol, J., Soisson, O., Stefan Klima, S., Milani, T., and Hammer, N. (2014). Pelvic belt effects on sacroiliac joint ligaments: a computational approach to understand therapeutic effects of pelvic belts. Pain Physician 17 (1), 43–51. doi:10.36076/ppj.2014/17/43
Silva, M., Brandão, S., Parente, M., Mascarenhas, T., and Natal Jorge, R. (2016). Establishing the biomechanical properties of the pelvic soft tissues through an inverse finite element analysis using magnetic resonance imaging. Proc. Institution Mech. Eng. Part H J. Eng. Med. 230 (4), 298–309. doi:10.1177/0954411916630571
Song, H. F., Huang, Y., Ni, C. X., Lei, L. L., Wang, X. Y., Liu, Z. C., et al. (2012). A finite element method for the simulation of levator ani muscle stress under different conditions. Chin. J. Tissue Eng. Res. 16 (26), 4852–4856. doi:10.3969/j.issn.1673-8225.2012.26.020
Song, Z., Nie, C., Li, S., Dario, P., and Dai, J. S. (2018). A muscle-specific rehabilitation training method based on muscle activation and the optimal load orientation concept. Appl. Bionics Biomech. 2018, 1–13. doi:10.1155/2018/2365983
Sun, T. J. (2015). Abdominal impact and injury mechanism analysis of a six-year-old occupant based on finite element methods[D]. Tianjin University of Science and Technology.
Talasz, H., Gosch, M., Kofler, M., and Lechleitner, M. (2018). Voiding disorders in geriatric patients: correlation with agerelated functional impairments. Z Gerontol. Geriatr. 51 (1), 67–73. doi:10.1007/s00391-016-1097-y
Tang, J. H., Zhong, C., Wen, W., Wu, R., Liu, Y., and Du, L. (2020). Quantifying levator ani muscle elasticity under normal and prolapse conditions by shear wave elastography: a preliminary study. J. Ultrasound Med. 39 (7), 1379–1388. doi:10.1002/jum.15232
The MR Group of the Radiology Branch of the Chinese Medical Association (2022). The MR Group of the Radiology Branch of the Chinese Medical Association MRI techniques and reporting standards for female pelvic floor functional disorders Chinese. J. Radiology 56 (1), 16–24. doi:10.3760/cma.j.cn112149-20210426-00412
Tibaek, S., Gard, G., Dehlendorff, C., Iversen, H. K., Biering-Soerensen, F., and Jensen, R. (2017). Is pelvic floor muscle training effective for men with poststroke lower urinary tract symptoms? A single-blinded randomized, controlled trial. Am. J. Mens. Health 11 (5), 1460–1471. doi:10.1177/1557988315610816
Venugopala Rao, G., Rubod, C., Brieu, M., Bhatnagar, N., and Cosson, M. (2010). Experiments and finite element modelling for the study of prolapse in the pelvic floor system. Comput. Methods Biomech. Biomed. Engin 13 (3), 349–357. doi:10.1080/10255840903251270
Wang, R., Liu, G., Jing, L., Zhang, J., Li, C., and Gong, L. (2024). Finite element analysis of pelvic floor biomechanical models to elucidate the mechanism for improving urination and defecation dysfunction in older adults: protocol for a model development and validation study. JMIR Res. Protoc. 13, e56333. doi:10.2196/56333
Wein, A. J. (2011). Re: FDA safety communication: update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. J. Urology 186 (6), 2328–2330. doi:10.1016/j.juro.2011.08.047
Wu, X. L. (2019). Finite element analysis of biomechanics of injured levator ani muscle in female patients with moderate to severe SUI[D]. Shanxi Medical University.
Xu, Z., Wu, Y., and Zhang, X. Q. (2021). Finite element modeling method of female pelvic floor structure with mechanical simulation function. China Patent: CN 113570723A 10.29.
Xuan, R., Yang, M., Gao, Y., Ren, S., Li, J., Yang, Z., et al. (2021). A simulation analysis of maternal pelvic floor muscle. Int. J. Environ. Res. Public Health 18 (20), 10821. doi:10.3390/ijerph182010821
Xue, J. L. (1996). Evaluation of anorectal angle in self-made and clinical application of the anus. J. Pract. Med. Technol. (05), 379–380.
Yang, M., Chen, C., Wang, Z., Long, J., Huang, R., Qi, W., et al. (2024). Finite element analysis of female pelvic organ prolapse mechanism: current landscape and future opportunities. Front. Med. (Lausanne) 11, 1342645. doi:10.3389/fmed.2024.1342645
Yao, T. Q., Qian, J. W., and Shen, J. H. (2022). Refined reconstruction modeling and mechanical analysis method of female pelvic floor system under sagittal plane[P]. China Patent: CN 114121290A, 2022.03.01.
Zhang, H., and Yao, L. Q. (2015). Research progress on the application of the finite element method in female pelvic floor functional disorders. J. Chronic Dis. 16 (01), 57–60. doi:10.16440/j.cnki.1674-8166.2015.01.018
Zhang, Y., Kim, S., Erdman, A. G., Roberts, K. P., and Timm, G. W. (2009). Feasibility of using a computer modeling approach to study SUI Induced by landing a jump. Ann. Biomed. Eng. 37 (7), 1425–1433. doi:10.1007/s10439-009-9705-2
Zhou, C. J., and Lai, S. L. (2021). Research progress on MRI evaluation of abnormal defecation control function. Magn. Reson. Imaging 12 (8), 114–117124. doi:10.12015/issn.1674-8034.2021.08.027
Zhou, L. X., Gu, X. L., and Du, H. L. (2020). Injury of levator ani muscles and occurrence of pelvic floor diseases during vaginal delivery based on finite element method. J. Med. Biomechanic 35 (06), 732–738. doi:10.16156/j.1004-7220.2020.06.013
Keywords: elderly men, rehabilitation training, muscles, quantification, urinary and defecation control ability, finite element analysis
Citation: Wang R, Liu G, Jing L, Zhang J, Ye Y and Zhu H (2024) Quantifying the effects of five rehabilitation training methods on the ability of elderly men to control bowel movements: a finite element analysis study. Front. Bioeng. Biotechnol. 12:1392448. doi: 10.3389/fbioe.2024.1392448
Received: 27 February 2024; Accepted: 04 June 2024;
Published: 26 June 2024.
Edited by:
Wujing Cao, Chinese Academy of Sciences (CAS), ChinaReviewed by:
Marco Parente, University of Porto, PortugalYadong Mo, Beijing University of Posts and Telecommunications (BUPT), China
Zw Z., University of Shanghai for Science and Technology, China
Copyright © 2024 Wang, Liu, Jing, Zhang, Ye and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liwei Jing, bHdqaW5nMjAwNEBjY211LmVkdS5jbg==
 Rui Wang
Rui Wang Guangtian Liu
Guangtian Liu Liwei Jing1*
Liwei Jing1* Jing Zhang
Jing Zhang