- 1Department of Orthopedics, First Affiliated Hospital of Dalian Medical University, Dalian, China
- 2Graduate School of Dalian Medical University, Dalian Medical University, Dalian, China
Purpose: To compare biomechanical and clinical properties of the novel internal fixation Interlocking Hip Screw (IHS) and conventional inverted triangle cannulated screws (ITCS) for treatment of Pauwels Ⅲ femoral neck fractures.
Methods: Twenty synthetic femurs were osteotomized to simulate 70° Pauwels Ⅲ femoral neck fractures and randomly divided into two groups: Group IHS and Group ITCS. Specimens were loaded in quasi-static ramped and cyclical compression testing in 25° adduction to analyze for axial stiffness, failure load, and interfragmentary displacement. 21 matched patients with Pauwels Ⅲ femoral neck fracture who received closed reduction and internal fixation from January 2020 to January 2021 in both Group IHS and Group ITCS. Demographic data, time to surgery, operating duration, intraoperative blood loss, number of fluoroscopies, length of hospital stay, fracture healing time, Harris Hip Score (HHS), the score of Visual Analogue Scale (VAS) and complications such as nonunion, avascular necrosis, and femoral neck shortening were compared.
Results: All specimens in the two groups survived in the axial and cyclical compression test. The axial stiffness was significantly higher for Group IHS (277.80 ± 26.58 N/mm) versus Group ITCS (205.33 ± 10.46 N/mm), p < 0.05. The maximum failure loading in Group IHS performed significantly higher than in Group ITCS (1,400.48 ± 71.60 N versus 996.76 ± 49.73 N, p < 0.05). The interfragmentary displacement of the cyclic loading test for Groups IHS and Group ITCS was 1.15 ± 0.11 mm and 1.89 ± 0.14 mm, respectively, p < 0.05. No significant difference was found in terms of demographic data, time to surgery, intraoperative blood loss, length of hospital stay and the occurrence of nonunion and avascular necrosis between groups. Shorter operating duration and fewer intraoperative fluoroscopic views were noticed using IHS compare to ITCS, p < 0.05. The HHS was 72.14 ± 5.76 and 86.62 ± 5.01 in Group IHS, and was 67.29 ± 5.27 and 81.76 ± 5.13 in Group ITCS at 3-month and 6-month follow-up, respectively, p < 0.05. The magnitude of femoral neck shortening was significantly lower in Group IHS compared to Group ITCS (4.80 ± 1.03 mm versus 5.56 ± 1.21 mm, p < 0.05).
Conclusion: Our study demonstrated that IHS provided better biomechanical and clinical performance due to its unique biological and biomechanical mechanisms, compared with ITCS. Thus, IHS is a feasible alternative to ITCS for the fixation of Pauwels Ⅲ femoral neck fractures.
1 Introduction
Hip fractures cripple 4.5 million individuals worldwide each year, of which femoral neck fractures account for about 53%. More than half of hip fractures will occur in Asia by 2040, accompanied by an enormous socioeconomic burden and medical challenge (Bhandari and Swiontkowski, 2017). Most femoral neck fractures in young adults are Pauwels Ⅲ femoral neck fractures caused by high energy trauma with a high risk of complications such as nonunion, avascular necrosis, and femoral neck shortening (Jiang et al., 2021). A series of implants have been proposed for superior prognosis of Pauwels Ⅲ femoral neck fractures (Stoffel et al., 2017; Chan, 2019; Duffin and Pilson, 2019), however, the optimal choice of internal fixation is still controversial and no consensus has been established (Florschutz et al., 2015). Inverted triangle cannulated screws (ITCS) were widely used for Pauwels Ⅲ femoral neck fractures in China (Slobogean et al., 2017). Nowadays, the novel minimally invasive implant Interlocking Hip Screw (IHS) consisted of a small side plate and the dynamic combined interlocking screws had made preliminary progress in the clinical application for the Pauwels Ⅲ femoral neck fractures. To the authors’ knowledge, limited biomechanical and clinical outcomes data exist on this new device. Therefore, the goal of our study is to compare both the biomechanical and clinical properties of IHS and ITCS in the fixation of Pauwels Ⅲ femoral neck fractures.
2 Materials and methods
2.1 Biomechanical analysis
2.1.1 Specimens preparation
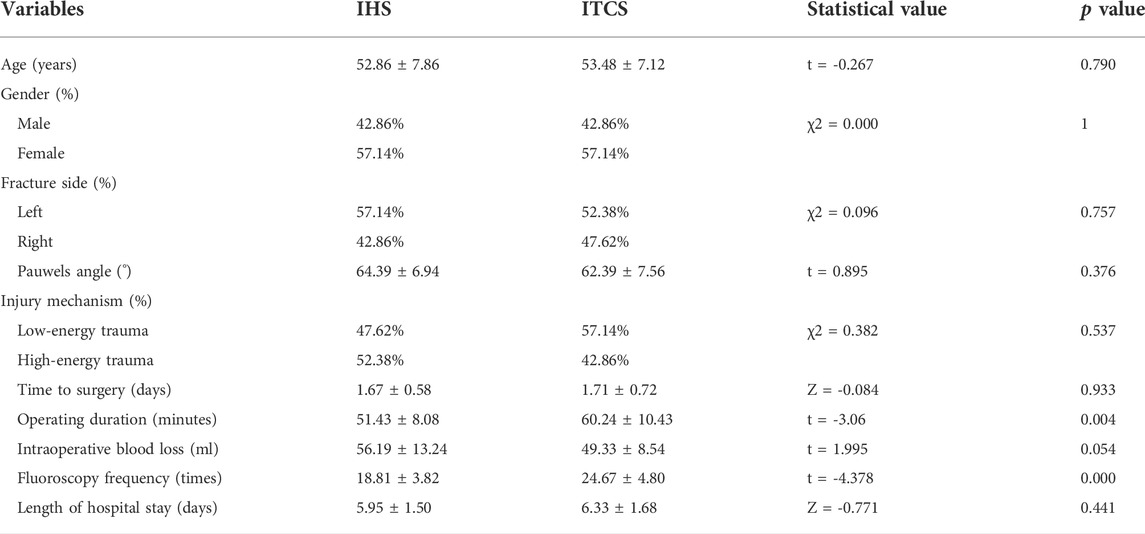
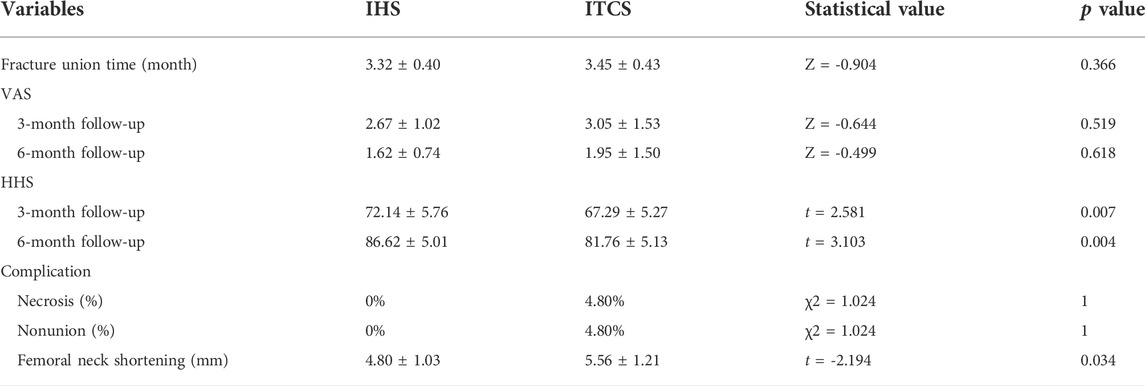
Twenty composite femurs (Kim et al., 2022) (#1005117, ORTHObones, 3B Scientific, Hamburg, Germany) were randomly assigned to two groups: Group IHS (n = 10) fixed with IHS (Waston Medical, Changzhou, Jiangsu, China) and Group ITCS (n = 10) fixed with ITCS (Waston Medical, Changzhou, Jiangsu, China). Before osteotomy, all specimens were predrilled for subsequent anatomical reduction. The osteotomy line passed through the midpoint of the femoral neck axis formed a 70° angle with the horizontal line and removed a 30° distal wedge fragment to eliminate medial support (Stoffel et al., 2017; Knobe et al., 2018). We perform the osteotomy line in computer-aided design (CAD) Unigraphics NX 12.0 software beforehand and 3D printed custom cutting jig accordingly (Wang et al., 2022). Subsequently, a handsaw was used for osteotomy according to the custom-designed cutting jig (Figure 1). In Group IHS, the dynamic combined interlocking screws were inserted center–center in both anteroposterior and lateral views over one guidewire by using a set of dedicated instruments, and the two-hole 127° side plate was fixed to the femoral shaft by two 5.0 mm locking screws (Figure 2). In Group ITCS, three 7.3 mm partial thread cannulated screws were inserted into the femoral head in a standard inverted triangular configuration through cannulated screws guiding jig, resting the inferior screw on the calcar, and the anterosuperior and posterosuperior screws were close to the femoral neck cortex (Figure 3). Surgical simulations were carried out in Unigraphics NX 12.0 software to determine the appropriate length and position of the internal fixation, prior to fracture creation. All fixation procedures were performed by an experienced orthopedic trauma surgeon under the guidance of C-arm fluoroscopy according to the manufacturer’s guidelines. Each specimen was cut to a length of 25 cm, measured from the most superior point of the femur, and placed in a self-made metal cylinder tube potted with anchoring cement polymethylmethacrylate (PMMA) to satisfy the strength requirement of the biomechanical experiment (Bliven et al., 2020).
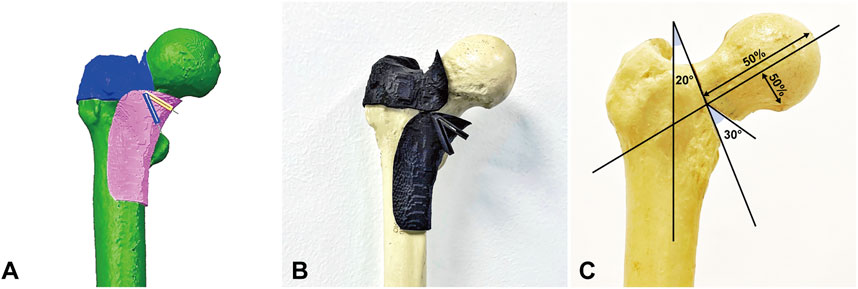
FIGURE 1. Creation of Pauwels Ⅲ femoral neck fracture. (A) Simulation of comminution 70° Pauwels Ⅲ femoral neck fractures with 30° distal wedge via Unigraphics NX 12.0 software. (B) Osteotomy jig made by 3D printing technology. (C) The osteotomy line passed through the midpoint of the femoral neck axis formed a 70° angle with the horizontal line and removed a 30° wedge fragment to eliminate medial support.
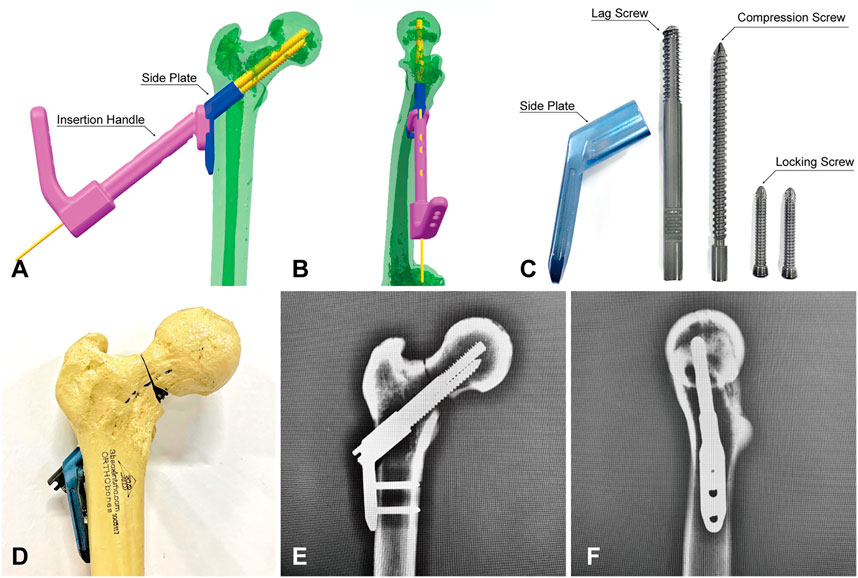
FIGURE 2. Fixation of Pauwels Ⅲ femoral neck fractures with IHS. (A,B) Simulation of IHS implantation in Unigraphics NX 12.0 software. (C) Components of IHS internal fixation. (D) Fixation with IHS. (E,F) anteroposterior and lateral fluoroscopic views after IHS fixation.

FIGURE 3. Fixation of Pauwels Ⅲ femoral neck fractures with ITCS. (A,B) Simulation of ITCS implantation in Unigraphics NX 12.0 software. (C) Components of ITCS internal fixation. (D) Fixation with ITCS. (E,F) anteroposterior and lateral fluoroscopic views after ITCS fixation.
2.1.2 Biomechanical protocol
Biomechanical testing was performed on a servo-hydraulic material testing system (Instron10000, Norwood, MA, United States). All specimens were installed in 25° adduction of the femoral shaft (Figure 4) and loaded along the machine axis to simulate a single-leg stance (Schaefer et al., 2015; Kuan et al., 2016). A spherically shaped PMMA shell cup was attached to the machine actuator as a load mediator to transmit the pressure on the femoral head.
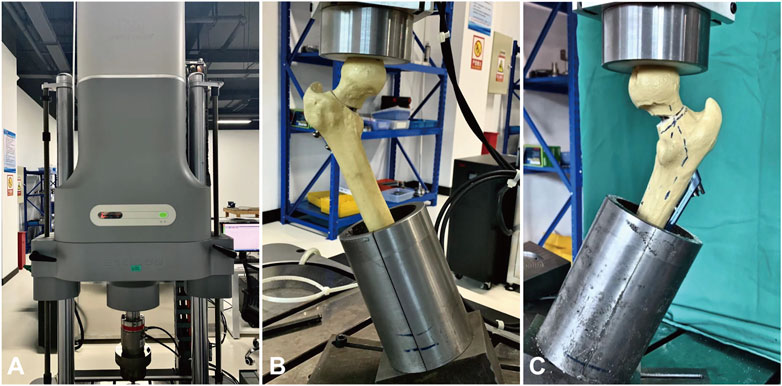
FIGURE 4. During the axial and cyclical compression tests, the specimen was installed in 25° adduction to simulate single leg stance. (A) Biomechanical testing was performed on a servo-hydraulic material testing system (Instron10000, Norwood, MA, United States). (B) Biomechanical test of Group IHS. (C) Biomechanical test of Group ITCS.
In the axial compression test, five synthetic femurs of Group IHS and five synthetic femurs of Group ITCS were tested for quasi-static ramped compression loading at the loading rate of 2 mm/min (Zhang et al., 2018). Machine data in terms of axial load and displacement were recorded via the servo-hydraulic material testing system. The failure of the specimen was defined as loosening, cutout, or breaking of internal fixation, fracture of synthetic femurs, the recorded displacement of 5 mm, and a sudden decrease in the recorded axial load (Zhang et al., 2018; Zhang et al., 2020).
In the cyclical compression test, the other five synthetic femurs of Group A and Group B were tested for double-peaked physiological compression cyclical loading (Bergmann et al., 2001)at 2 Hz for 10,000 cycles. The 10,000 loading cycles correspond to the number of steps walked at 4–6 weeks postoperatively, which is the expected period for preliminary fracture healing (Nuchtern et al., 2014; Steffensmeier et al., 2022). Keeping the valley load of each cycle at a constant level of 200 N and the peak load at 700 N to simulate partial weight-bearing after internal fixation of femoral neck fractures (Nowotarski et al., 2012). The ascending linear slope of the load-displacement curve in the axial compression test was defined as the axial stiffness of the bone–implant construct. The maximum failure load in the axial compression test and the max interfragmentary displacement during cyclic loading were recorded.
2.2 Clinical evaluation
2.2.1 Inclusion and exclusion criteria
After obtaining the Institutional Review Board approval, we performed a retrospective study that enrolled 53 patients with Pauwels Ⅲ femoral neck fractures who underwent closed reduction and internal fixation with the IHS or ITCS in our trauma center from January 2020 to January 2021. Inclusion criteria were: the time interval from injury to operation < 3 weeks, Age > 18 years and <65 years, isolated Pauwels Ⅲ femoral neck fractures, and adequate radiographic and clinical follow-up. Exclusion criteria included: pathological femoral neck fractures, patients with previous hip fractures, and open fractures. There were 21 patients with Pauwels Ⅲ femoral neck fractures treated with IHS and made up Group IHS. Of 32 patients treated with ITCS, 21 patients were matched for age and sex with adequate radiographic and clinical follow-up, comprising Group ITCS.
2.2.2 Surgical method
All patients with femoral neck fractures were evaluated preoperatively by an anesthesiologist. After medical contraindications were eliminated, the surgery was performed immediately by a senior trauma orthopedic surgeon. After general anesthesia, closed reduction was performed on the fracture traction table in the supine position. The C-arm is routinely placed between the legs to observe the quality of the fracture reduction and the position of the implant (Zhang and Tang, 2022). If anatomical position is difficult to obtain after three attempts, the Gotfried positive buttress reduction (Huang et al., 2020) would be adopted for some patients. In Group IHS, a straight lateral incision of approximately 4 cm was made in the proximal femur, directly across the fascia to the bone. In both AP and lateral views, a 3.0 mm guidewire was inserted along the center of the femoral neck to a depth of 5 mm beneath the surface of the femoral head cartilage. After reaming along the guidewire, a two-hole 127 degrees side plate and the dynamic combined interlocking screws were inserted into the femoral neck. The fracture gap was eliminated by the IHS unique combination compression mechanism that drove the semi-threaded lag screw when twisting the full-threaded compression screw in. Subsequently, the side plate was fixed to the femoral shaft by two 5.0 mm locking screws. In Group ITCS, three guide wires forming an inverted triangle configuration were inserted into the femoral head approximately 5 mm from the subchondral bone in both AP and lateral views (Tang et al., 2021). After ensuring the proper position, three 7.5 mm semi-threaded lag cannulated screws were inserted along the guide wires. Dissipation of the fracture gap during twisting of the cannulated screws.
2.2.3 Perioperative management
Intravenous antibiotics were administered within 24 h after surgery to prevent infection. Oral rivaroxaban for 35 days postoperatively to prevent lower extremity deep vein thrombosis (Falck-Ytter et al., 2012). All patients were required to follow-up at 6 weeks, 3 months, and 6 months postoperative in the outpatient clinic for review, and every 6 months afterward. Patients in both groups were instructed to be non-weight bearing with crutches until 6 weeks postoperatively when partial weight bearing was started. Gradually increase the frequency and weight of partial weight-bearing exercises to full weight-bearing 3 months postoperatively (Dong et al., 2019).
2.2.4 Data collection
Demographic, clinical, and radiographic data were obtained from the patient medical record. Demographic data included age, gender, and side of injury. Clinical information included mechanism of injury, time to surgery, implants used, operating duration, intra-operative blood loss, number of intra-operative fluoroscopies, length of hospital stay, fracture union time, Harris Hip Score (HHS), and the scores of Visual Analogue Scale (VAS) at 3-month and 6-month follow-up. Admission radiographs were analyzed for the Pauwels angle. Intra-operative and post-operative radiographs were analyzed to assess the quality of fracture reduction, implant placement, and complications such as nonunion, avascular necrosis, and femoral neck shortening at 12-month follow-up.
2.3 Statistical analysis
SPSS 25.0 (IBM, Armonk, NY, United States) was utilized for data analysis. Data were expressed as mean ± standard deviation or number (%). The count data were compared by a chi-squared test. Kolmogorov Smirnov test was used to analyze the normality of the distribution of continuous variables. Continuous variables of a normal distribution with homogeneous variance were compared between groups by t-test. Mann Whitney U test was used to compare continuous variables of a normal distribution with inhomogeneous variance and continuous variables not in line with normal distribution. All tests were two-tailed and assessed at the 5% significance level.
3 Results
3.1 Biomechanical analysis
All specimens in the two groups survived in the axial compression and cyclical compression test without evidence of failure. The biomechanical data in terms of axial stiffness, failure load during the quasi-static loading test, and interfragmentary displacement during the double-peaked physiological compression cyclic loading test were shown in Figure 5. The mean axial stiffness was significantly higher for Group IHS (277.80 ± 26.58 N/mm) versus Group ITCS (205.33 ± 10.46 N/mm), p < 0.05. The mean maximum loading failure in Group IHS performed significantly better than that in Group ITCS (1,400.48 ± 71.60 N versus 996.76 ± 49.73 N, p < 0.05). The interfragmentary displacement of the cyclic loading test for Groups IHS and Group ITCS was 1.15 ± 0.11 mm and 1.89 ± 0.14 mm, respectively, p < 0.05.
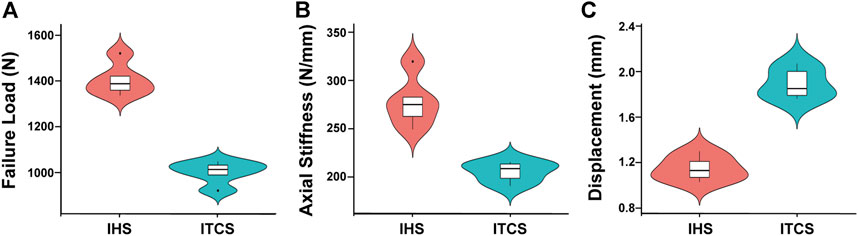
FIGURE 5. Biomechanical experimental data in Group IHS and Group ITCS. (A) Failure load during the quasi-static loading test of each group. (B) Axial stiffness during the quasi-static loading test of each group. (C) Interfragmentary displacement during the double-peaked physiological compression cyclic loading test of each group.
3.2 Clinical analysis
There were 21 matched patients (9 males and 12 females) in both Group IHS and Group ITCS. All patients in both groups received at least 1 year of clinical follow-up and typical caseswere shown in Figure 6. No significant difference was found between the two groups in terms of age, gender, side of injury, mechanism of injury, Pauwels angle, time to surgery, intraoperative blood loss, and length of hospital stay between the two groups, p > 0.05. Patients who underwent IHS treatment had shorter operating duration (51.43 ± 8.08 min versus 60.24 ± 10.43 min, p < 0.05) and fewer intraoperative fluoroscopic views (18.81 ± 3.82 times versus 24.67 ± 4.80 times, p < 0.05), as illustrated in Table 1.
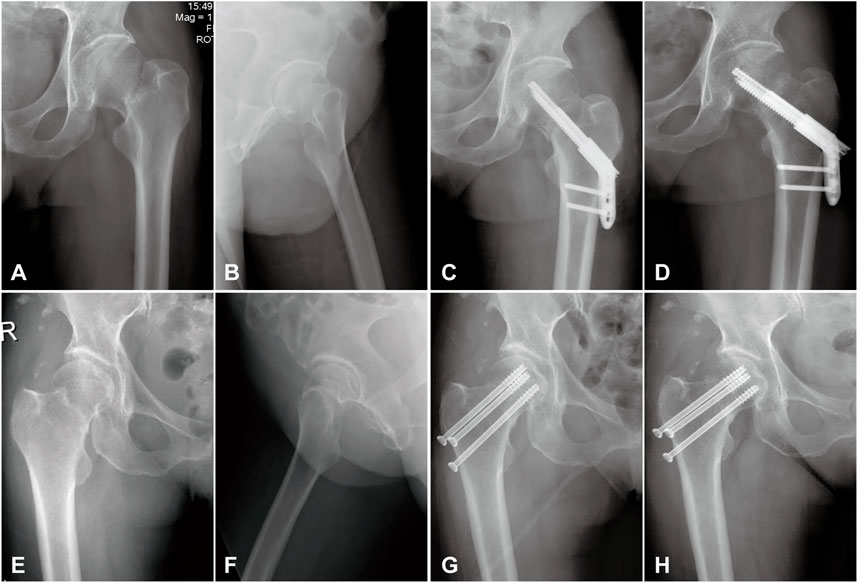
FIGURE 6. Radiographs of group IHS and group ITCS. (A,B): Preoperative anteroposterior and lateral radiographs of a 44-year-old male with Pauwels Ⅲ femoral neck fracture. (C): Anteroposterior radiographs of this patient fixed with the IHS technique at 1 day after operation. (D): Anteroposterior radiographs of this patient fixed with the IHS technique at 3-month follow-up. (E,F): Preoperative anteroposterior and lateral radiographs of a 56-year-old female with Pauwels Ⅲ femoral neck fracture. (G): Anteroposterior radiographs of this patient fixed with the ITCS technique at 1 day after operation. (H): Anteroposterior radiographs of this patient fixed with the ITCS technique at 3-month follow-up.
There were no significant differences between the two groups in terms of fracture union time and the scores of VAS at 3-month and 6-month follow-up. The HHS was 72.14 ± 5.76 and 86.62 ± 5.01 in Group HIS, and was 67.29 ± 5.27 and 81.76 ± 5.13 in Group ITCS at 3-month and 6-month follow-up, respectively, p < 0.05, indicating that IHS fixation facilitated the recovery of postoperative hip function. Concerning postoperative complications, there was no significant difference in the occurrence of nonunion and avascular necrosis between the two groups. Nevertheless, femoral neck shortening was observed in both groups. The magnitude of femoral neck shortening was significantly lower in Group IHS than in Group ITCS (4.80 ± 1.03 mm versus 5.56 ± 1.21 mm, p < 0.05), as illustrated in Table 2.
4 Discussion
With the increase of high-energy trauma such as traffic accidents and high-fall injuries, the incidence of femoral neck fractures in young adults has increased significantly, predominantly vertical Pauwels Ⅲ femoral neck fractures. The optimal selection of internal fixation for Pauwels Ⅲ femoral neck fractures remains controversial due to the high probability of femoral head necrosis, fracture nonunion, and femoral neck shortening. A previous expert opinion survey of the Orthopaedic Trauma Association’s (OTA) membership on the treatment of high-angle vertical femoral neck fractures in young adult patients showed that 46% of experts were unconvinced that their implant was supported by the literature (Luttrell et al., 2014). A 17-item survey completed by 540 surgeons from the Canadian Orthopaedic Association, the Orthopaedic Trauma Association, and attendees at an international fracture course revealed the lack of consensus on femoral neck fracture fixation in young people and there is an equal divide in preference between multiple cannulated screws and angular stable construct such as IHS(Slobogean et al., 2015).
To the best of our knowledge, the present study was the first study to evaluate the biomechanical and clinical evaluation of IHS and ITCS fixation on Pauwels Ⅲ femoral neck fractures. In our biomechanical experiment, we demonstrated that IHS had a significant benefit in terms of construct stiffness and protection from fracture displacement, compared with ITCS. Generally, the femoral neck fracture is fixed with ITCS according to the three-point principle (Bout et al., 1997). However, in the article by Collinge CA et al. (Collinge et al., 2014), major femoral neck comminution (>1.5 cm in any dimension) was identified in 96% of Pauwels Ⅲ femoral neck fractures cases, the same as in our chosen osteotomy model, resulting in insufficient stability of the second point in the three-point support for cannulated screws fixation.
Severe shortening of the femoral neck is associated with decreased gait velocity, impaired physical function, and the incidence of reoperation (Felton et al., 2019). IHS had better resistance to fracture micromotion and provided marked clinical benefit in terms of maintaining reduction, and femoral neck shortening in this small clinical series, which may be the reason for the significant difference in postoperative hip function between the two groups. As the successful initiation of fracture healing requires appropriate reduction and stabilization, the solid mechanical environment in the initial stages is one of the most important factors in achieving successful patient outcomes (Dong et al., 2019).
The combined interlocking screws of IHS are compressed immediately to reduce the fracture gap during operation and limited dynamic sliding compression after the operation following the mechanism of fracture healing (Einhorn and Gerstenfeld, 2015). The particular compression mechanism of the combined interlocking screws avoids the Z-effect phenomenon of two lag screws and the weak anti-rotation ability of a single screw (Strauss et al., 2007). The lateral locking compression plate of IHS fixed to the femoral shaft provided angular stability and resistance to shear force. The low radius of curvature of the lateral plate forms double line contact, reducing the contact area and decreasing compression of the periosteum as well as disrupting of the local blood supply. However, significant differences were unable to be demonstrated for nonunion and avascular necrosis of the femoral head, possibly due to the small sample size and inadequate follow-up duration.
In addition, our study found that the operative time was significantly shorter in the IHS group due to the relative manipulation simplicity. The IHS device is convenient to operate and inserted over one guide wire via a set of dedicated instruments. Operative time was generally considered as an influential factor associated with higher blood loss, longer anesthesia, higher infection rates, and overall higher postoperative complication rates (Cheng et al., 2018; Vazquez et al., 2021). The number of intraoperative fluoroscopies was fewer in patients who underwent IHS fixation. Mastrangelo et al. reported a significantly increased risk of cancer among orthopaedic surgeons exposed to long-term occupational radiation, with a cancer incidence rate of 29%, seven times higher than unexposed workers (Mastrangelo et al., 2005). Thus, it is essential to reduce the risk of radiation during surgical procedures (Yamashita et al., 2016; van Rappard et al., 2019).
However, there are several limitations in our biomechanical experiment and clinical research. To ensure the consistency of neck-shaft angle and bone density, we selected synthetic composite femurs as specimens rather than fresh-frozen human cadaveric femurs which are the gold standard for biomechanical experiment specimens (Windolf et al., 2009), and that may have a slight impact on the experimental results. We did not simulate the soft tissues surrounding the hip joint, such as muscles, joint capsules, and ligaments in the biomechanical experiment, which are important for stabilizing the structure and function of the hip joint (Fu et al., 2022). Our biomechanical experiments could not simulate the hip joint loading in all directions, such as A-P bending test which simulates the physiologic stress on the femoral head when rising from a seated position. Our clinical study was retrospective and observational design, and all data analyzed is subject to the quality of the data originally imported into the medical record, which might have resulted in methodological bias. Moreover, the relatively small patient size and short follow-up may result in the underestimation of the complication rate and prognosis.
5 Conclusion
In summary, our biomechanical experiment and the clinical study demonstrated IHS achieves better biomechanical support, shorter operative time, fewer intraoperative fluoroscopies, higher Harris hip score, and less femoral neck shortening due to its unique biological and biomechanical mechanisms, compared with inverted triangle cannulated screws. Thus, IHS is a feasible alternative to inverted triangle cannulated screws for the fixation of Pauwels Ⅲ femoral neck fractures. However, a long-term follow-up multicentre prospective controlled trial will be necessary to demonstrate the effectiveness of IHS in the fixation of Pauwels Ⅲ femoral neck fractures in the future.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Dalian Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JZ, HJ, WD and KT contributed to the conception of the study and wrote the manuscript; ZC, ZL, DZ and CL designed the manuscript outline; XT and KT critically reviewed the manuscript; all authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation (No.81601901) and the Natural Science Foundation of Liaoning (No.2019-MS- 079).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bergmann, G., Deuretzbacher, G., Heller, M., Graichen, F., Rohlmann, A., Strauss, J., et al. (2001). Hip contact forces and gait patterns from routine activities. J. Biomech. 34 (7), 859–871. doi:10.1016/s0021-9290(01)00040-9
Bhandari, M., and Swiontkowski, M. (2017). Management of acute hip fracture. N. Engl. J. Med. Overseas. Ed. 377 (21), 2053–2062. doi:10.1056/NEJMcp1611090
Bliven, E., Sandriesser, S., Augat, P., von Ruden, C., and Hackl, S. (2020). Biomechanical evaluation of locked plating fixation for unstable femoral neck fractures. Bone Jt. Res. 9 (6), 314–321. doi:10.1302/2046-3758.96.BJR-2019-0331.R1
Bout, C. A., Cannegieter, D. M., and Juttmann, J. W. (1997). Percutaneous cannulated screw fixation of femoral neck fractures: The three point principle. Injury 28 (2), 135–139. doi:10.1016/s0020-1383(96)00161-1
Chan, D. S. (2019). Femoral neck fractures in young patients: State of the art. J. Orthop. Trauma 33 (1), S7–S11. doi:10.1097/BOT.0000000000001366
Cheng, H., Clymer, J. W., Po-Han Chen, B., Sadeghirad, B., Ferko, N. C., Cameron, C. G., et al. (2018). Prolonged operative duration is associated with complications: A systematic review and meta-analysis. J. Surg. Res. 229, 134–144. doi:10.1016/j.jss.2018.03.022
Collinge, C. A., Mir, H., and Reddix, R. (2014). Fracture morphology of high shear angle "vertical" femoral neck fractures in young adult patients. J. Orthop. Trauma 28 (5), 270–275. doi:10.1097/BOT.0000000000000014
Dong, Q., Han, Z., Zhang, Y. G., Sun, X., and Ma, X. L. (2019). Comparison of transverse cancellous lag screw and ordinary cannulated screw fixations in treatment of vertical femoral neck fractures. Orthop. Surg. 11 (4), 595–603. doi:10.1111/os.12503
Duffin, M., and Pilson, H. T. (2019). Technologies for young femoral neck fracture fixation. J. Orthop. Trauma 33 (1), S20–S26. doi:10.1097/BOT.0000000000001367
Einhorn, T. A., and Gerstenfeld, L. C. (2015). Fracture healing: Mechanisms and interventions. Nat. Rev. Rheumatol. 11 (1), 45–54. doi:10.1038/nrrheum.2014.164
Falck-Ytter, Y., Francis, C. W., Johanson, N. A., Curley, C., Dahl, O. E., Schulman, S., et al. (2012). Prevention of VTE in orthopedic surgery patients: Antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 141, e278S–e325S. doi:10.1378/chest.11-2404
Felton, J., Slobogean, G. P., Jackson, S. S., Della Rocca, G. J., Liew, S., Haverlag, R., et al. (2019). Femoral neck shortening after hip fracture fixation is associated with inferior hip function: Results from the FAITH trial. J. Orthop. Trauma 33, 487–496. doi:10.1097/BOT.0000000000001551
Florschutz, A. V., Langford, J. R., Haidukewych, G. J., and Koval, K. J. (2015). Femoral neck fractures: Current management. J. Orthop. Trauma 29 (3), 121–129. doi:10.1097/BOT.0000000000000291
Fu, G., Zhong, G., Yang, Z., Cheng, S., Ma, L., and Zhang, Y. (2022). Two cannulated screws provide sufficient biomechanical strength for prophylactic fixation in adult patients with an aggressive benign femoral neck lesion. Front. Bioeng. Biotechnol. 10, 891338. doi:10.3389/fbioe.2022.891338
Huang, K., Fang, X., Li, G., and Yue, J. (2020). Assessing the effect of Gotfried reduction with positive buttress pattern in the young femoral neck fracture. J. Orthop. Surg. Res. 15 (1), 511. doi:10.1186/s13018-020-02039-0
Jiang, D., Zhan, S., Hu, H., Zhu, H., Zhang, C., and Jia, W. (2021). The effect of vertical and oblique inclinations on fracture stability and reoperation risks in femoral-neck fractures of nongeriatric patient. Front. Bioeng. Biotechnol. 9, 782001. doi:10.3389/fbioe.2021.782001
Kim, M. S., Yoon, D. K., Shin, S. H., Choe, B. Y., Rhie, J. W., Chung, Y. G., et al. (2022). Quantitative assessment of the restoration of original anatomy after 3D virtual reduction of long bone fractures. Diagn. (Basel) 12 (6), 1372. doi:10.3390/diagnostics12061372
Knobe, M., Altgassen, S., Maier, K. J., Gradl-Dietsch, G., Kaczmarek, C., Nebelung, S., et al. (2018). Screw-blade fixation systems in Pauwels three femoral neck fractures: A biomechanical evaluation. Int. Orthop. 42 (2), 409–418. doi:10.1007/s00264-017-3587-y
Kuan, F. C., Yeh, M. L., Hong, C. K., Chiang, F. L., Jou, I. M., Wang, P. H., et al. (2016). Augmentation by cerclage wire improves fixation of vertical shear femoral neck fractures-A biomechanical analysis. Injury 47 (10), 2081–2086. doi:10.1016/j.injury.2016.07.030
Luttrell, K., Beltran, M., and Collinge, C. A. (2014). Preoperative decision making in the treatment of high-angle "vertical" femoral neck fractures in young adult patients. An expert opinion survey of the Orthopaedic Trauma Association's (OTA) membership. J. Orthop. Trauma 28 (9), e221–e225. doi:10.1097/BOT.0000000000000080
Mastrangelo, G., Fedeli, U., Fadda, E., Giovanazzi, A., Scoizzato, L., and Saia, B. (2005). Increased cancer risk among surgeons in an orthopaedic hospital. Occup. Med. (Lond). 55 (6), 498–500. doi:10.1093/occmed/kqi048
Nowotarski, P. J., Ervin, B., Weatherby, B., Pettit, J., Goulet, R., and Norris, B. (2012). Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel's type C femoral neck fractures. Injury 43 (6), 802–806. doi:10.1016/j.injury.2011.09.012
Nuchtern, J. V., Ruecker, A. H., Sellenschloh, K., Rupprecht, M., Puschel, K., Rueger, J. M., et al. (2014). Malpositioning of the lag screws by 1- or 2-screw nailing systems for pertrochanteric femoral fractures: A biomechanical comparison of gamma 3 and intertan. J. Orthop. Trauma 28 (5), 276–282. doi:10.1097/BOT.0000000000000008
Schaefer, T. K., Spross, C., Stoffel, K. K., and Yates, P. J. (2015). Biomechanical properties of a posterior fully threaded positioning screw for cannulated screw fixation of displaced neck of femur fractures. Injury 46 (11), 2130–2133. doi:10.1016/j.injury.2015.07.021
Slobogean, G. P., Sprague, S. A., Scott, T., McKee, M., and Bhandari, M. (2015). Management of young femoral neck fractures: Is there a consensus? Injury 46 (3), 435–440. doi:10.1016/j.injury.2014.11.028
Slobogean, G. P., Stockton, D. J., Zeng, B., Wang, D., Ma, B. T., and Pollak, A. N. (2017). Femoral neck fractures in adults treated with internal fixation: A prospective multicenter Chinese cohort. J. Am. Acad. Orthop. Surg. 25 (4), 297–303. doi:10.5435/JAAOS-D-15-00661
Steffensmeier, A., Shah, N., Archdeacon, M., Watson, D., Sanders, R. W., and Sagi, H. C. (2022). Clinical and biomechanical effects of femoral neck buttress plate used for vertical femoral neck fractures. Injury 53 (3), 1137–1143. doi:10.1016/j.injury.2021.12.004
Stoffel, K., Zderic, I., Gras, F., Sommer, C., Eberli, U., Mueller, D., et al. (2017). Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws. J. Orthop. Trauma 31 (3), 131–137. doi:10.1097/BOT.0000000000000739
Strauss, E. J., Kummer, F. J., Koval, K. J., and Egol, K. A. (2007). The "Z-effect" phenomenon defined: A laboratory study. J. Orthop. Res. 25 (12), 1568–1573. doi:10.1002/jor.20457
Tang, Y., Zhang, Z., Wang, L., Xiong, W., Fang, Q., and Wang, G. (2021). Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: A preliminary comparative study. J. Orthop. Surg. Res. 16 (1), 504. doi:10.1186/s13018-021-02659-0
van Rappard, J. R. M., de Jong, T., Hummel, W. A., Ritt, M., and Moues, C. M. (2019). Radiation exposure to surgeon and assistant during flat panel mini C-arm fluoroscopy in hand and wrist surgical procedures. J. Hand Surg. Br. 44 (1), 68.e1–68.e5. doi:10.1016/j.jhsa.2018.05.010
Vazquez, O., Gamulin, A., Hannouche, D., and Belaieff, W. (2021). Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): Short-term clinical and radiological outcomes. J. Orthop. Surg. Res. 16 (1), 477. doi:10.1186/s13018-021-02622-z
Wang, Y., Chen, W., Zhang, L., Xiong, C., Zhang, X., Yu, K., et al. (2022). Finite element analysis of proximal femur bionic nail (PFBN) compared with proximal femoral nail antirotation and InterTan in treatment of intertrochanteric fractures. Orthop. Surg. 14, 2245–2255. doi:10.1111/os.13247
Windolf, M., Braunstein, V., Dutoit, C., and Schwieger, K. (2009). Is a helical shaped implant a superior alternative to the dynamic hip screw for unstable femoral neck fractures? A biomechanical investigation. Clin. Biomech. (Bristol, Avon. 24 (1), 59–64. doi:10.1016/j.clinbiomech.2008.07.004
Yamashita, K., Higashino, K., Wada, K., Morimoto, M., Abe, M., Takata, Y., et al. (2016). Radiation exposure to the surgeon and patient during a fluoroscopic procedure: How high is the exposure dose? A cadaveric study. Spine (Phila Pa 1976) 41 (15), 1254–1260. doi:10.1097/BRS.0000000000001542
Zhang, B., Liu, J., and Zhang, W. (2018). Ordinary cannulated compression screws or headless cannulated compression screws? A synthetic bone biomechanical research in the internal fixation of vertical femoral neck fracture. Biomed. Res. Int. 2018, 4898301–4898305. doi:10.1155/2018/4898301
Zhang, J., and Tang, X. (2022). The application of the 150° oblique tangential fluoroscopic view to detect the posterosuperior femoral neck screw in–out–in intraoperatively. Sci. Rep. 12 (1), 12790. doi:10.1038/s41598-022-17221-z
Keywords: biomechanics, osteotomy, osteosynthesis, internal fixation, femoral neck fracture, cannulated screws
Citation: Zhang J, Jiang H, Dai W, Hersi SA, Chun tien chui wan Cheong J, Chu Z, Lou Z, Zhang D, Liu C, Tian K and Tang X (2022) Biomechanical and clinical evaluation of interlocking hip screw in Pauwels Ⅲ femoral neck fractures: A comparison with inverted triangle cannulated screws. Front. Bioeng. Biotechnol. 10:1047902. doi: 10.3389/fbioe.2022.1047902
Received: 19 September 2022; Accepted: 17 October 2022;
Published: 31 October 2022.
Edited by:
Changjiang Pan, Huaiyin Institute of Technology, ChinaReviewed by:
Feng Wu, Xuzhou University of Technology, ChinaChao Han, Tianjin Hospital, China
Yapeng Zhou, The University of Hong Kong, China
Copyright © 2022 Zhang, Jiang, Dai, Hersi, Chun tien chui wan Cheong, Chu, Lou, Zhang, Liu, Tian and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kang Tian, ZG11LXRpYW5rYW5nQG91dGxvb2suY29t; Xin Tang, c3VyZ2VvbnRhbmd4aW5AMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Jian Zhang
Jian Zhang Haozheng Jiang
Haozheng Jiang Wei Dai1†
Wei Dai1† Zhenchen Chu
Zhenchen Chu Kang Tian
Kang Tian Xin Tang
Xin Tang