- 1School of Chinese Medicine, China Medical University, Taichung, Taiwan
- 2Department of Chinese Medicine, China Medical University Hospital, Taichung, Taiwan
- 3Department of Traditional Chinese Medicine, Changhua Christian Hospital, Changhua, Taiwan
- 4Graduate Institute of Chinese Medicine, China Medical University, Taichung, Taiwan
- 5Division of Nephrology, Department of Internal Medicine, Kuang Tien General Hospital, Taichung, Taiwan
- 6Big Data Center, Epidemiology and Biostatistics Center, Changhua Christian Hospital, Changhua, Taiwan
- 7Nephrology Division, Department of Internal Medicine, Changhua Christian Hospital, Changhua, Taiwan
- 8Department of Computer Science and Engineering, National Sun Yat-Sen University, Kaohsiung, Taiwan
- 9Department of Healthcare Administration and Medical Informatics, Kaohsiung Medical University, Kaohsiung, Taiwan
Introduction: Chronic kidney disease (CKD) is a significant global health problem associated with high morbidity and mortality rates. Traditional Chinese Medicine (TCM) utilizes tongue diagnosis to differentiate symptoms and predict prognosis. This study examines the relationship between tongue characteristics and CKD severity using an automatic tongue diagnosis system (ATDS), which captures tongue images non-invasively to provide objective diagnostic information.
Methods: This cross-sectional, case-control study was conducted from July 1, 2019, to December 31, 2021. Participants were divided into three groups based on estimated glomerular filtration rate (eGFR): control (eGFR > 60 ml/min/1.732), CKD stage 3 (30 ≤ eGFR < 60 ml/min/1.732), and CKD stage 4–5 (eGFR < 30 ml/min/1.732). Tongue images were analyzed using ATDS to extract nine primary features: tongue shape, color, fur, saliva, fissures, ecchymosis, tooth marks, and red dots. Statistical analyses included non-parametric methods and ordinal logistic regression.
Results: This study revealed that significant differences in the fur thickness, tongue color, amount of ecchymosis, and saliva among three groups. Ordinal logistic regression indicated that pale tongue color (OR: 2.107, P < 0.001), bluish tongue color (OR: 2.743, P = 0.001), yellow fur (OR: 3.195, P < 0.001), wet saliva (OR: 2.536, P < 0.001), and ecchymoses (OR: 1.031, P = 0.012) were significantly associated with increased CKD severity. Additionally, each red dot and tooth mark decreased the odds of severe CKD.
Conclusion: Tongue features such as paleness, wet saliva, yellow fur, and ecchymosis are prevalent in CKD patients and can serve as early clinical indicators of the disease. This study demonstrates that TCM tongue diagnosis, facilitated by ATDS, is a valuable, non-invasive method for identifying CKD and distinguishing its stages.
1 Introduction
Chronic kidney disease (CKD) is a progressive condition affecting more than 10% of the global population, making it a significant public health concern (Kovesdy, 2022). CKD is characterized by a glomerular filtration rate (GFR) of <60 mL/min/1.73 m2 or the presence of other indicators of kidney damage, such as imaging abnormalities or albuminuria, particularly comorbidity with hypertension and diabetes (Webster et al., 2017; Matsushita et al., 2015). CKD progresses from an asymptomatic early stage to debilitating later stages, characterized by symptoms such as fatigue, nausea, and swelling, primarily due to complications like anemia and chronic inflammation (Evans et al., 2022; Charles and Ferris, 2020). As CKD progresses to end-stage renal disease (ESRD), life-sustaining treatments such as dialysis or kidney transplantation become necessary (KDIGO Group, 2020).
The growing prevalence of CKD raises concerns about the cost and health-related quality of life (HRQoL) burden of patients (Honeycutt et al., 2013; Pergola et al., 2019). There is a significant disparity in the evidence about direct and indirect costs attributed to CKD and ESRD, with the most complete evidence concentrated on direct health care costs of patients with advanced to the later stages of CKD (Nichols et al., 2020; Wang et al., 2016). Therefore, it is essential to find effective and conservative treatment methods to slow progression and reduce complications of CKD.
The diagnosis in TCM is based on four main approaches, including inspection, auscultation and olfaction, inquiry, and pulse diagnosis (Tian et al., 2023). Tongue diagnosis, serving as a vital non-invasive tool to provide useful clinical information, plays a crucial role in TCM. The tongue is considered to reflect the physiological and pathological condition of the body, as well as the degree and progression of the disease, through the meridians that connect the tongue to the internal organs (Jiang et al., 2012). By observing tongue features, TCM practitioners can probe qi-blood, yin-yang disorders which are important in treatment selection and prognosis (Feng et al., 2023). Clinically, doctors observe tongue features, such as tongue color and shape, fur color and thickness, and the amount of saliva, to help deduce the primary pattern of a patient (Lo et al., 2012). However, tongue inspection is often biased by subjective judgment, which originates from personal experience, knowledge, diagnostic skills, thinking patterns, and color perception. The inconsistency of subjective diagnosis can be improved by using the development of validated instruments.
The automatic tongue diagnosis system (ATDS) has shown high consistency and can provide objective and reliable information and analysis of tongue characteristics, facilitating doctors to make effective observations and diagnoses of specific diseases (Lo et al., 2012). In recent years, several researches have applied case-control methodology to explore the association between tongue characteristics and specific diseases, including breast cancer (Hsu et al., 2021), type 2 diabetes (Hsu et al., 2016), ischemic stroke (Huang et al., 2022), metabolic syndrome (Lee et al., 2016), and CKD (Chung et al., 2023), in the hope of deriving discriminating tongue features to distinguish individuals with/without the specific disease through a non-invasive means in the early stage. This research aims to identify distinctive tongue features associated with CKD, offering a non-invasive diagnostic tool for early detection and management.
2 Methods
2.1 Study design
We conducted a cross-section, case-control, and observational study from July 1, 2019 to December 31, 2021. Participants were divided into the following three groups according to the status of their renal function: control group (eGFR > 60 ml/min/1.732), CKD stage 3 group (30 ml/min/1.732 < eGFR < 60 ml/min/1.732) and CKD stage 4–5 group without dialysis (eGFR < 30 ml/min/1.732). Participants were enrolled in the control group without evidence of kidney damage, such as albuminuria or abnormal findings on renal imaging. Subjects with any of the following conditions will be excluded: cancer; acute infection; unable to protrude the tongue stably; risk of temporomandibular joint dislocation (Chen et al., 2021). This study has been reviewed and approved by the Institutional Review Board (IRB) of Changhua Christian Hospital (CCH), Taiwan (IRB Nos. 190404 and 140704). This trial was registered with the National Institute of Health Clinical Trial Registry (clinicaltrials.gov; NCT04708743).
2.2 Participants
In this case-control study, we utilized data from a previous study to identify 340 healthy participants, excluding 22 subjects due to insufficient data, spanning from January 1, 2012, to December 31, 2016 (Hsu et al., 2019). We initially identified 370 patients with CKD stage 3 and 111 patients with CKD stage 4–5. Tongue images for all participants, including the control group, CKD stage 3 group, and CKD stage 4–5 group, were collected using the validated Automatic Tongue Diagnosis System (ATDS), which automatically extracted the corresponding tongue features.
2.3 Data collection
Information including demography, body mass index (BMI, kg/m2), CKD staging, estimated glomerular filtration rate (eGFR) and blood urea nitrogen (BUN) were collected for each subject. The duration of CKD history, comorbidity and complication in patient with CKD were also collected. Tongue images were collected for each subject to further derive the relevant tongue features of every participant. All personal details and photographs of subjects recruited were encrypted to ensure confidentiality.
2.4 Automatic tongue diagnosis system
We analyzed the data from the subjects and the tongue features using the ATDS. The ATDS was specifically developed to capture tongue images and automatically extract features reliably, aiding TCM practitioners in diagnosis. The effectiveness of the ATDS lies in its ability to segment the tongue region and extract tongue features automatically. This ensured that all tongue images were captured using the same hardware and software configuration, providing a consistent foundation for the data collection process. The ATDS performs three major functions: image capturing and color calibration, tongue area segmentation, and tongue feature extraction. These processes are seamlessly integrated within the system.
2.5 Outcome measures
Nine primary tongue features were extracted using the ATDS: tongue color, tongue shape, saliva, tongue fur, fur thickness, tongue fissure, ecchymosis, tooth marks, and red dots. The extracted features are detailed as follows:
1. Tongue color: includes slightly white, slightly red, red, dark red, and dark purple.
2. Tongue shape: includes shape (thin and small, moderate, fat and large) and tongue body position (normal, tilted to the left, tilted to the right).
3. Saliva: total area and amount of saliva categorized as none, little, normal, or excessive.
4. Tongue fur: includes fur color (white, yellow, dyed), amount, average covering area, maximum covering area, minimum covering area, and degree of thickness (none, thin, thick).
5. Fur thickness: degree of thickness (thin or thick) and the percentage of thick tongue fur.
6. Tongue fissure: includes the number of fissures, average covering area, shortest length, and longest length.
7. Ecchymosis: includes the number of ecchymoses, average covering area, maximum covering area, and minimum covering area.
8. Tooth marks: includes the number of tooth marks, average covering area, maximum covering area, and minimum covering area.
9. Red dots: includes the number of red dots, average covering area, maximum covering area, and minimum covering area.
2.6 Data analysis
The tongue features of the participants were extracted using ATDS, and cross compared with the kidney injury severity groups to see if there was a linear correlation between them. A trend analysis was categorized by their eGFR into three groups: eGFR ≥ 60 ml/min/1.732 (control group), 30 ≤ eGFR < 60 ml/min/1.732 (CKD stage 3), and eGFR < 30 ml/min/1.732 (CKD stage 4–5). Data are expressed as number, percentage, median, or interquartile range (IQR, 25th−75th percentile) where appropriate. Since the distribution of tongue features was non-normal, non-parametric statistics were employed for univariate analysis. The Jonckheere-Terpstra test was used for continuous variables, and the chi-square test for trend was used for categorical variables to examine the association between tongue features and kidney injury severity. To identify tongue features predictive of renal impairment, we performed an ordinal logistic regression analysis, adjusting for potential confounders. All potential predictors associated with renal impairment were assessed, and odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were calculated. All data were analyzed using the IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY). Statistical significance was set at p < 0.05.
3 Results
In this case-control study, we utilized data from a previous study to identify 340 healthy participants, excluding 22 subjects due to insufficient data. From July 1, 2019, to December 31, 2021, 481 patients with chronic kidney disease (CKD) underwent TCM tongue diagnosis. Thirty-three CKD patients were excluded due to unclear tongue images. The final study population consisted of 318 healthy participants (eGFR ≥ 60 ml/min/1.732), 345 patients of stage 3 CKD (30 ≤ eGFR < 60 ml/min/1.732), and 103 patients of stage 4–5 CKD (eGFR < 30 ml/min/1.732). As shown in Figure 1, the exploratory flow chart for CKD-associated tongue diagnosis variates.

Figure 1. Exploratory flow chart of participant selection for chronic kidney disease and associated tongue diagnosis study.
This study applied a non-parametric trend test and the demographic and clinical characteristics of the participants were summarized in Table 1. The median age increased with the severity of CKD, with median ages of 63, 65, and 65 years for the control, CKD stage 3, and CKD stage 4–5, respectively (p = 0.005). Hemoglobin levels decreased significantly with the severity of CKD (p < 0.001). Fasting glucose levels increased significantly with the severity of CKD (p < 0.001). Total cholesterol and triglyceride levels exhibited significant variations across the groups, with total cholesterol generally decreasing and triglycerides increasing as renal function worsened (p < 0.001 and p = 0.030, respectively). Levels of uric acid, blood urea nitrogen (BUN), and creatinine increased significantly with worsening renal function (p < 0.001). The proportion of participants with thick tongue fur increased significantly as eGFR level worsened (p < 0.001). The numbers of ecchymoses, teeth marks, and red dots decreased significantly with the severity of CKD (p < 0.001).
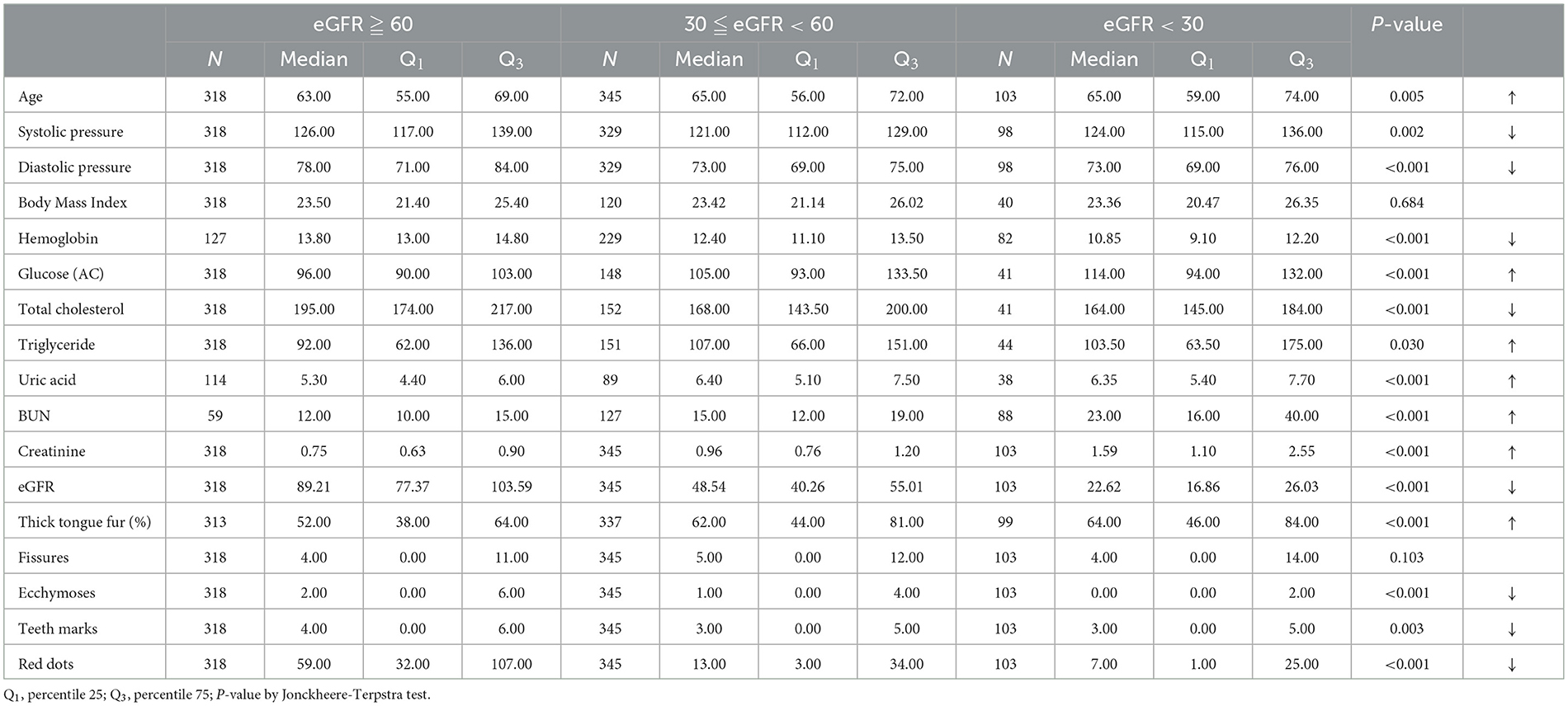
Table 1. Demographic and clinical characteristics of study participants with statistical comparison across CKD stages.
Table 2 presented the demographic and tongue features of the study participants. The prevalence of comorbidities increased significantly with worsening renal, whereas 27.0% of the CKD stage 3 group and 31.1% of the CKD stage 4–5 group were comorbidities with diabetes (p < 0.001). Besides, 19.1% of the CKD stage 3 group and 17.5% of the CKD stage 4–5 group were companied with hypertension (p < 0.001). Participants with wet saliva were significantly more likely to exhibit decreased eGFR, with an increasing trend observed as renal function decreased (p < 0.001). The color and thickness of tongue fur showed significant correlations with CKD severity. Yellow fur and thick fur were more prevalent in participants with lower eGFR (p < 0.001). Pale tongue color was associated with poorer renal function, being more common in CKD stage 3 and stage 4–5 groups (p < 0.001).
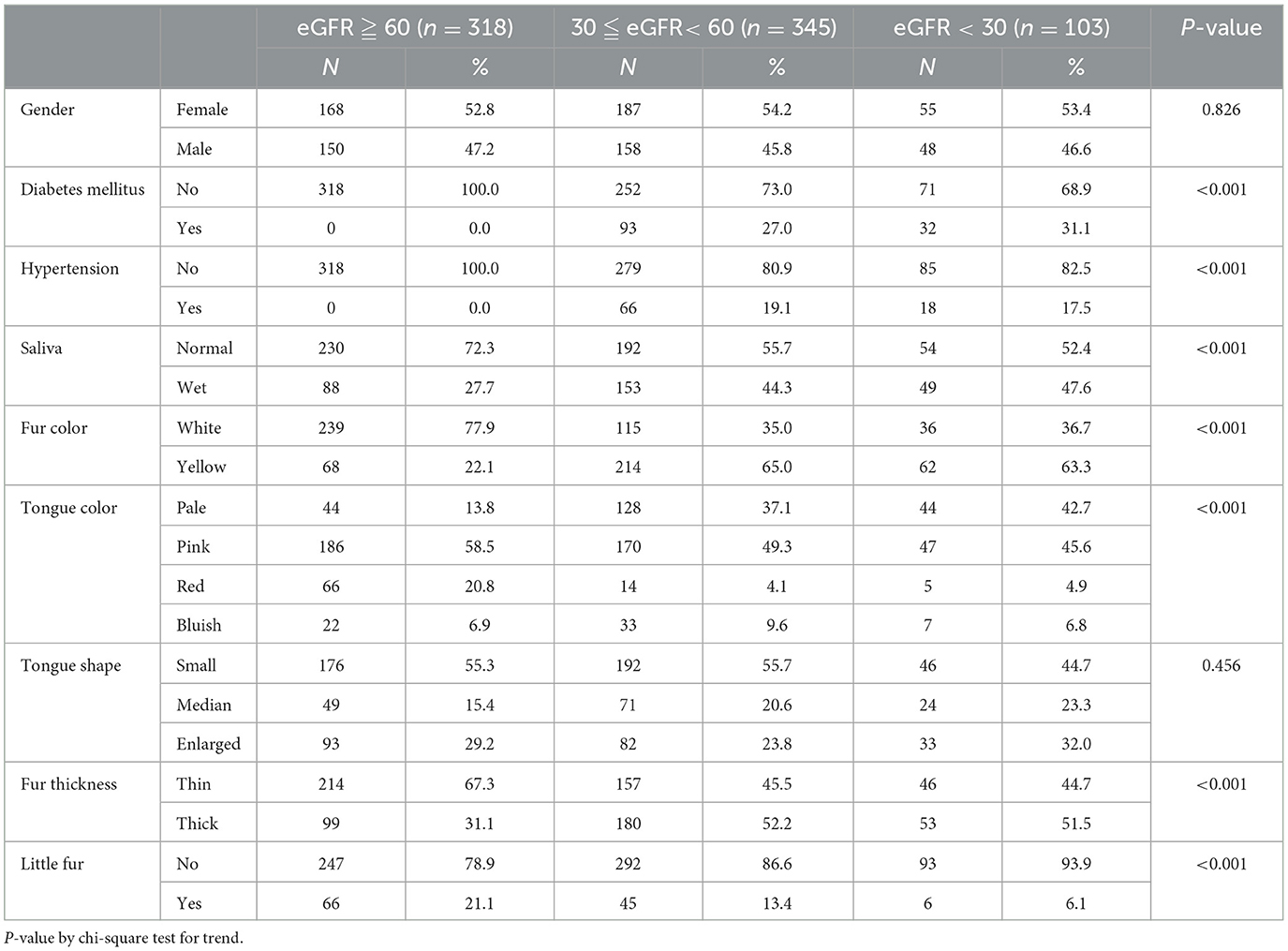
Table 2. Demographic and tongue diagnosis features of study participants with statistical comparisons across CKD stages.
Table 3 shows the results of the ordinal logistic regression analysis, which was conducted to identify factors associated with the stage of CKD. Each additional red dot on the tongue was associated with a decrease in the severity of CKD, with an ordinal odds ratio (OR) of 0.972 (95% CI: 0.965–0.979, p < 0.001), while each additional tooth mark was associated with a reduction in the severity of CKD, with an OR of 0.938 (95% CI: 0.884–0.995, p = 0.032). The presence of ecchymoses on the tongue was positively associated with the stage of CKD, with an OR of 1.031 (95% CI: 1.007–1.056, p = 0.012). Participants with wet saliva had a significantly higher likelihood of severe CKD, with an OR of 2.536 (95% CI: 1.805–3.564, p < 0.001). Yellow tongue fur was strongly associated with increased stage of CKD, with an OR of 3.195 (95% CI: 2.281–4.477, p < 0.001). Pale tongue color was associated with increased severity of CKD, with an OR of 2.107 (95% CI: 1.445–3.072, p < 0.001). Bluish tongue color was also associated with increased severity, with an OR of 2.743 (95% CI: 1.516–4.962, p = 0.001). Red tongue color was not significantly associated with CKD severity (p = 0.542).
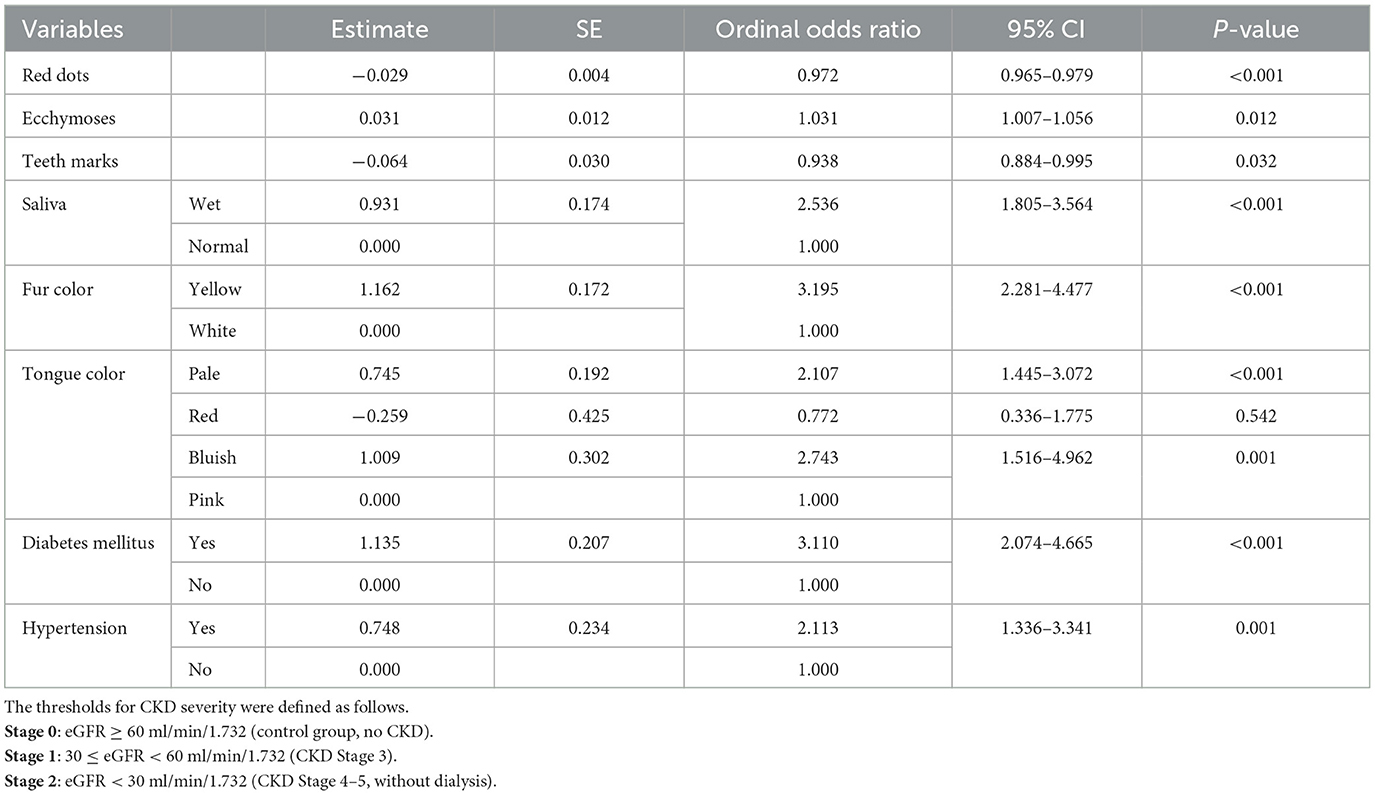
Table 3. Ordinal logistic regression analysis of tongue diagnosis features and clinical factors associated with eGFR severity.
4 Discussion
In this study, we employed an ATDS, which provides an objective and standardized method to capture and analyze tongue features. This minimizes the subjectivity and variability found in traditional tongue diagnosis. Previous research on tongue diagnosis in TCM has laid a solid foundation by exploring associations between tongue features and various diseases, including metabolic syndrome, type 2 diabetes, ischemic stroke, and breast cancer. For example, Chung et al. (2023) identified several tongue characteristics, including fur thickness, color, ecchymosis, teeth marks, and red dots, as potential markers of renal function in CKD patients (Chung et al., 2023). However, the study was limited by a small sample size. In this case-control study, we utilized data from a previous study to identify 340 healthy participants and enrolled 481 patients with chronic kidney disease (CKD) who underwent TCM tongue diagnosis. The use of ATDS minimized the subjective assessments typically made by practitioners, thereby reducing inconsistencies in diagnosis.
Statistical analyses revealed that specific tongue features were significantly associated with renal function severity. Hemoglobin, ecchymoses, teeth marks, and red dots were inversely related to renal function, decreasing as renal function worsened. Conversely, thick tongue fur and wet saliva increased with worsening renal function. The ordinal logistic regression analysis identifies several significant predictors of CKD severity as measured by eGFR. Tongue features such as red dots, ecchymoses, teeth marks, fur color, and tongue color are significantly associated with eGFR severity, demonstrating the diagnostic potential of these non-invasive markers. Additionally, clinical conditions such as diabetes mellitus and hypertension are confirmed as significant predictors of severe CKD. These findings suggest that the ATDS can provide valuable, objective data for the early detection and monitoring of CKD, aligning TCM practices with modern diagnostic methodologies.
According to the TCM theory, tongue diagnosis involves diagnosing a disease by observing changes in the tongue body and tongue fur of a patient. In clinical practice, tongue diagnosis is a highly valuable method for determining the strength of vital force (i.e., qi), the depth of the disease location, the nature of pathogens, and the changes in symptoms. In TCM, a pale tongue is equivalent to anemia in Western medicine. Anemia occurs in 34–94.3% CKD patients, mainly due to decreased renal erythropoietin, iron, folic acid, or vitamin B12 deficiency, poor erythrocyte survival, and blood loss during dialysis (Tajbakhsh et al., 2013; Tajalli et al., 2021; Gluba-Brzozka et al., 2020). Wet saliva in TCM corresponds to abnormal water metabolism in the body in Western medicine. Wet saliva also indicates spleen deficiency syndrome in TCM, which hinders thorough blood filtration and transpiration of excess water, causing edema in patients with kidney disease (Wu et al., 2020). According to TCM theory, the spleen plays an important role in various physiological functions, including regulating the transport and metabolism of water and nutrients in the body (Wu, 1998). When the spleen is incapable of transporting body fluids, it leads to an accumulation of moisture within the body, a condition referred to as water dampness, which signifies spleen-deficiency syndrome in TCM (Yang and Jia, 2013).
When the tongue appears to be yellow and heavily coated, this indicates damp-heat syndrome in TCM, which is caused by a combination of dampness and heat (Yuan et al., 2021). According to TCM theory, excess saliva is caused by spleen-deficiency syndrome; yellow thick tongue coating is often related to damp-heat syndrome (Zhou et al., 2022; Kang et al., 2022). Yellow fur color usually results from poor oral hygiene as food and bacteria can collect on the filiform papillae on the surface. In TCM theory, a yellow tongue fur indicates an interior heat pattern. In CKD patients, yellow fur may correspond to the accumulation of uremic toxins and metabolic waste products that the kidneys are unable to filter out, such as BUN and creatinine. Several studies have discussed the relationship between CKD and tongue characteristics such as tongue-coating thickness, tongue-coating microbiota, and metabolic markers (Guo et al., 2022; Chung et al., 2023).
TCM classifies these vascular complications as blood stasis. Tongue diagnosis plays a key role in TCM, where ecchymosis and engorged sublingual collateral vessels are manifestations of blood stasis. Numerous diseases can cause blood stasis, including cardiovascular disease, cerebral vascular accidents, and CKD (Park et al., 2015; Kouri and Rheault, 2021). Patients with CKD are at high risk of developing ESRD, cardiovascular disease (associated with arterial hypertension), and cardiovascular mortality (Sun et al., 2014).
One study reported that patients with CKD commonly exhibited features such as blood deficiency and stasis with qi deficiency (Wang et al., 2022). Our study indicated that patients with the later stages of CKD had more yellow thick fur compared to the control group. This suggested that damp-heat syndrome may also be a clinical characteristic of CKD in the context of TCM. In modern medicine, renal failure results from kidney injury, leading to reduced renal function, which causes electrolyte dysregulation and the accumulation of fluids, body waste, and toxins. Severe kidney dysfunction can lead to uremic syndrome (Makris and Spanou, 2016). According to TCM theory, uremic syndrome is related to asthenia and excess superficiality. Excess syndrome is characterized by ecchymoses, red dots, and thick white or yellow fur, while deficiency syndrome is characterized by teeth marks, pale tongue, and excess saliva. In general, TCM generally believes that spleen-kidney deficiency is an internal condition where blood deficiency, blood stasis, dampness, and heat are interconnected with the patient's viscera. Although no significant differences in teeth marks were observed, there was a trends toward disease progression, and teeth marks are often seen in dialysis patients (Rashpa et al., 2018).
This study has certain limitations. First, this was a cross-sectional study. The cross-sectional nature of this study captures data at a single point in time, which limits the ability to establish causality between tongue features and the progression of CKD. Secondly, underlying conditions or medication use might influence tongue features independently of CKD. Although we adjusted for key comorbidities like diabetes and hypertension in our statistical models, we recognize that other factors, including medication use, might introduce bias. Third, this study excluded patients undergoing dialysis, who often present with distinct tongue features due to their advanced disease state and treatment effects. The longitudinal study designs and more diverse and broader patient population would provide a more robust understanding of how tongue features change over time and in relation to CKD progression. Fourth, we did not analyze sublingual collateral vessels, which might offer additional insights into vascular complications related to CKD. Future studies should consider including these features for a more thorough assessment.
5 Conclusion
In conclusion, tongue features such as paleness, wet saliva, yellow fur, and ecchymosis were prevalent in CKD patients and may serve as early clinical indicators of the CKD. This study demonstrates that TCM tongue diagnosis, facilitated by ATDS, is a valuable, non-invasive method for identifying CKD and distinguishing its stages.
Data availability statement
The data supporting the findings of this study are available from the corresponding author on request.
Ethics statement
This study involving humans has been reviewed and approved by the Institutional Review Board of Changhua Christian Hospital, Taiwan (IRB no. 190404). This trial was registered with the National Institute of Health clinical trial registry (http://clinicaltrials.gov/; NCT04708743). The participants provided their written informed consent to participate in this study.
Author contributions
P-CH: Writing – original draft, Writing – review & editing. J-MC: Writing – original draft, Writing – review & editing. C-CC: Investigation, Supervision, Writing – review & editing. Y-JC: Writing – original draft, Formal analysis. P-FC: Investigation, Supervision, Writing – review & editing. JC: Writing – review & editing. L-CL: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by program grants from Ministry of Science and Technology, Taiwan (MOST 110-2314-B-039-023) and China Medical University Hospital, Taiwan (DMR-109-006, DMR-111-197, DMR-HHC-111-1, and DMR-112-003).
Acknowledgments
The authors would like to thank the Changhua Christian Hospital, Taiwan for the grant support. The authors acknowledge the use of artificial intelligence (ChatGPT) in English language editing for this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Charles, C., and Ferris, A. H. (2020). Chronic kidney disease. Prim. Care. 47, 585–595. doi: 10.1016/j.pop.2020.08.001
Chen, J. M., Chiu, P. F., Wu, F. M., Hsu, P. C., Deng, L. J., Chang, C. C., et al. (2021). The tongue features associated with chronic kidney disease. Medicine 100:e25037. doi: 10.1097/MD.0000000000025037
Chung, C. J., Wu, C. H., Hu, W. L., Shih, C. H., Liao, Y. N., Hung, Y. C., et al. (2023). Tongue diagnosis index of chronic kidney disease. Biomed. J. 46, 170–178. doi: 10.1016/j.bj.2022.02.001
Evans, M., Lewis, R. D., Morgan, A. R., Whyte, M. B., Hanif, W., Bain, S. C., et al. (2022). A Narrative review of chronic kidney disease in clinical practice: current challenges and future perspectives. Adv. Ther. 39, 33–43. doi: 10.1007/s12325-021-01927-z
Feng, L., Xiao, W., Wen, C., Deng, Q., Guo, J., and Song, H. (2023). Objectification of tongue diagnosis in traditional medicine, data analysis, and study application. J. Vis. Exp. e65140. doi: 10.3791/65140
Gluba-Brzozka, A., Franczyk, B., Olszewski, R., and Rysz, J. (2020). The influence of inflammation on anemia in CKD patients. Int. J. Mol. Sci. 21:725. doi: 10.3390/ijms21030725
Guo, S., Wu, G., Liu, W., Fan, Y., Song, W., Wu, J., et al. (2022). Characteristics of human oral microbiome and its non-invasive diagnostic value in chronic kidney disease. Biosci. Rep. 42:BSR20210694. doi: 10.1042/BSR20210694
Honeycutt, A. A., Segel, J. E., Zhuo, X., Hoerger, T. J., Imai, K., Williams, D., et al. (2013). Medical costs of CKD in the Medicare population. J. Am. Soc. Nephrol. 24, 1478–1483. doi: 10.1681/ASN.2012040392
Hsu, P. C., Huang, Y. C., Chiang, J. Y., Chang, H. H., Liao, P. Y., Lo, L. C., et al. (2016). The association between arterial stiffness and tongue manifestations of blood stasis in patients with type 2 diabetes. BMC Comp. Altern. Med. 16:324. doi: 10.1186/s12906-016-1308-5
Hsu, P. C., Wu, H. K., Chang, H. H., Chen, J. M., Chiang, J. Y., Lo, L. C. A., et al. (2021). Perspective on tongue diagnosis in patients with breast cancer. Evid. Based Comp. Alternat. Med. 2021:4441192. doi: 10.1155/2021/4441192
Hsu, P. C., Wu, H. K., Huang, Y. C., Chang, H. H., Chen, Y. P., Chiang, J. Y., et al. (2019). Gender- and age-dependent tongue features in a community-based population. Medicine 98:e18350. doi: 10.1097/MD.0000000000018350
Huang, Y. S., Wu, H. K., Chang, H. H., Lee, T. C., Huang, S. Y., Chiang, J. Y., et al. (2022). Exploring the pivotal variables of tongue diagnosis between patients with acute ischemic stroke and health participants. J. Tradit. Comp. Med. 12, 505–510. doi: 10.1016/j.jtcme.2022.04.001
Jiang, B., Liang, X., Chen, Y., Ma, T., Liu, L., Li, J., et al. (2012). Integrating next-generation sequencing and traditional tongue diagnosis to determine tongue coating microbiome. Sci. Rep. 2:936. doi: 10.1038/srep00936
Kang, X., Lu, B., Xiao, P., Hua, Z., Shen, R., Wu, J., et al. (2022). Microbial characteristics of common tongue coatings in patients with precancerous lesions of the upper gastrointestinal tract. J. Healthc. Eng. 2022:7598427. doi: 10.1155/2022/7598427
KDIGO Group (2020). KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 98, S1–S115. doi: 10.1016/j.kint.2020.06.019
Kouri, A. M., and Rheault, M. N. (2021). Cardiovascular disease in children with chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 30, 231–236. doi: 10.1097/MNH.0000000000000684
Kovesdy, C. P. (2022). Epidemiology of chronic kidney disease: an update 2022. Kidney Int. Suppl. 12, 7–11. doi: 10.1016/j.kisu.2021.11.003
Lee, T. C., Lo, L. C., and Wu, F. C. (2016). Traditional chinese medicine for metabolic syndrome via TCM pattern differentiation: tongue diagnosis for predictor. Evid. Based Comp. Alternat. Med. 2016:1971295. doi: 10.1155/2016/1971295
Lo, L. C., Chen, Y. F., Chen, W. J., Cheng, T. L., and Chiang, J. Y. (2012). The study on the agreement between automatic tongue diagnosis system and traditional chinese medicine practitioners. Evid. Based Comp. Alternat. Med. 2012:505063. doi: 10.1155/2012/505063
Makris, K., and Spanou, L. (2016). Acute kidney injury: definition, pathophysiology and clinical phenotypes. Clin. Biochem. Rev. 37, 85–98.
Matsushita, K., Coresh, J., Sang, Y., Chalmers, J., Fox, C., Guallar, E., et al. (2015). Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol. 3, 514–525. doi: 10.1016/S2213-8587(15)00040-6
Nichols, G. A., Ustyugova, A., Déruaz-Luyet, A., O'Keeffe-Rosetti, M., and Brodovicz, K. G. (2020). Health care costs by type of expenditure across eGFR stages among patients with and without diabetes, cardiovascular disease, and heart failure. J. Am. Soc. Nephrol. 31, 1594–1601. doi: 10.1681/ASN.2019121308
Park, B., You, S., Jung, J., Lee, J. A., Yun, K. J., Lee, M. S., et al. (2015). Korean studies on blood stasis: an overview. Evid. Based Comp. Alternat. Med. 2015:316872. doi: 10.1155/2015/316872
Pergola, P. E., Pecoits-Filho, R., Winkelmayer, W. C., Spinowitz, B., Rochette, S., Thompson-Leduc, P., et al. (2019). Economic burden and health-related quality of life associated with current treatments for anaemia in patients with CKD not on dialysis: a systematic review. Pharmacoecon. Open 3, 463–478. doi: 10.1007/s41669-019-0132-5
Rashpa, R. S., Mahajan, V. K., Kumar, P., Mehta, K. S., Chauhan, P. S., Rawat, R., et al. (2018). Mucocutaneous manifestations in patients with chronic kidney disease: a cross-sectional study. Indian Dermatol. Online J. 9, 20–26. doi: 10.4103/idoj.IDOJ_160_17
Sun, W., Liu, D., Gong, P., Shi, X., Wang, Y., Wang, P., et al. (2014). Predicting cardiovascular mortality in chronic kidney disease (CKD) patients. Ann. Transplant. 19, 513–518. doi: 10.12659/AOT.891207
Tajalli, F., Mirahmadi, S. M., Mozafarpoor, S., Goodarzi, A., Nasiri Partovi, M., Lakestani, D., et al. (2021). Mucocutaneous manifestations of patients with chronic kidney disease under hemodialysis: a cross-sectional study of 49 patients. Dermatol. Ther. 34:e15015. doi: 10.1111/dth.15015
Tajbakhsh, R., Dehghan, M., Azarhoosh, R., Haghighi, A. N., Sadani, S., Zadeh, S. S., et al. (2013). Mucocutaneous manifestations and nail changes in patients with end-stage renal disease on hemodialysis. Saudi J. Kidney Dis. Transpl. 24, 36–40. doi: 10.4103/1319-2442.106236
Tian, Z., Wang, D., Sun, X., Fan, Y., Guan, Y., Zhang, N., et al. (2023). Current status and trends of artificial intelligence research on the four traditional Chinese medicine diagnostic methods: a scientometric study. Ann. Transl. Med. 11:145. doi: 10.21037/atm-22-6431
Wang, V., Vilme, H., Maciejewski, M. L., and Boulware, L. E. (2016). The economic burden of chronic kidney disease and end-stage renal disease. Semin. Nephrol. 36, 319–330. doi: 10.1016/j.semnephrol.2016.05.008
Wang, Y., Feng, Y., Li, M., Yang, M., Shi, G., Xuan, Z., et al. (2022). Traditional Chinese medicine in the treatment of chronic kidney diseases: theories, applications, and mechanisms. Front. Pharmacol. 13:917975. doi: 10.3389/fphar.2022.917975
Webster, A. C., Nagler, E. V., Morton, R. L., and Masson, P. (2017). Chronic kidney disease. Lancet 389, 1238–1252. doi: 10.1016/S0140-6736(16)32064-5
Wu, T. C., Lu, C. N., Hu, W. L., Wu, K. L., Chiang, J. Y., Sheen, J. M., et al. (2020). Tongue diagnosis indices for gastroesophageal reflux disease: a cross-sectional, case-controlled observational study. Medicine 99:e20471. doi: 10.1097/MD.0000000000020471
Wu, X. N. (1998). Current concept of spleen-stomach theory and spleen deficiency syndrome in TCM. World J. Gastroenterol. 4, 2–6. doi: 10.3748/wjg.v4.i1.2
Yang, X., and Jia, C. (2013). Understanding association of spleen system with earth on traditional Chinese medicine theory. J. Tradit. Chin. Med. 33, 134–136. doi: 10.1016/S0254-6272(13)60115-6
Yuan, S., Wang, N., Wang, J. L., Pan, J., Xue, X. Y., Zhang, Y. N., et al. (2021). Gender differences in Damp-Heat Syndrome: a review. Biomed. Pharmacother. 143:112128. doi: 10.1016/j.biopha.2021.112128
Keywords: Traditional Chinese Medicine (TCM), tongue diagnosis, automatic tongue diagnosis system (ATDS), chronic kidney disease (CKD), renal function
Citation: Hsu P-C, Chen J-M, Chang C-C, Chang Y-J, Chiu P-F, Chiang JY and Lo L-C (2025) Exploring the pivotal variables of tongue diagnosis between patients with chronic kidney disease and health participants. Front. Big Data 7:1443646. doi: 10.3389/fdata.2024.1443646
Received: 04 June 2024; Accepted: 25 November 2024;
Published: 03 January 2025.
Edited by:
Serestina Viriri, University of KwaZulu-Natal, South AfricaReviewed by:
Balu Bhasuran, Florida State University, United StatesSid Ahmed Benabderrahmane, New York University, United States
Copyright © 2025 Hsu, Chen, Chang, Chang, Chiu, Chiang and Lo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lun-Chien Lo, bGNsb0BtYWlsLmNtdS5lZHUudHc=
 Po-Chi Hsu
Po-Chi Hsu Jia-Ming Chen
Jia-Ming Chen Chia-Chu Chang5
Chia-Chu Chang5 Yu-Jun Chang
Yu-Jun Chang Ping-Fang Chiu
Ping-Fang Chiu John Y. Chiang
John Y. Chiang Lun-Chien Lo
Lun-Chien Lo