
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Behav. Neurosci., 14 March 2024
Sec. Learning and Memory
Volume 18 - 2024 | https://doi.org/10.3389/fnbeh.2024.1349672
Background: Severe traumatic brain injuries (TBIs) are an important health issue worldwide, which are associated with harmful side effects. This meta-analysis investigates the cognitive and functional outcomes in severe brain trauma cases. It assesses the impact on memory, verbal and visual abilities, attention, learning, and the presence of depression. The study provides a comprehensive overview of the consequences of severe brain trauma injury on cognitive and functional domains.
Objective: The main objective of the current comprehensive meta-analysis study is to assess and analyze the impact of severe TBI on functional and cognitive outcomes, including verbal, visual, attention, learning, memory, and emotional stability.
Methods: We collected data from three online databases, including PubMed, Cochrane Library, and Embase. Case–control trials related to severe TBI association with cognitive and functional outcomes were included. Verbal strength, visual functions, learning abilities, attention, memory, and depression were considered primary outcomes.
Results: We have included 13 case–control studies with 1,442 subjects in this meta-analysis, which provide adequate data to determine the pooled effect size for targeted outcomes. The effect of severe TBI on the inducement of depression and impairment of memory, verbal, visual, attention, and learning abilities compared to the control group showed statistically significant outcomes (p < 0.05).
Conclusion: Severe TBI is strongly associated with impaired cognitive and functional abilities, including visual and verbal disabilities, impaired memory, depression inducement, attention deficits, and learning disabilities.
Severe traumatic brain injury (TBI) represents a major global health concern, with profound implications for individuals, families, and healthcare systems. Survivors of severe brain trauma often face long and arduous journeys toward recovery, marked by a spectrum of cognitive and functional challenges. Understanding the factors that influence cognitive and functional outcomes in this population is not only crucial for optimizing patient care but also for informing healthcare policies and interventions (Robinson, 2021).
The pathophysiology of severe brain trauma is complex and multifaceted. The initial mechanical insult, often resulting from accidents, falls, or violence, sets in motion a cascade of events, including primary and secondary injury mechanisms that can lead to structural damage, inflammation, and neurochemical imbalances (Orr and Gensel, 2017; Ng and Lee, 2019). These processes, occurring within the highly delicate and intricately interconnected neural networks of the brain, can result in a wide range of neurological deficits (Ng and Lee, 2019). While advances in neuroimaging and neurocritical care have expanded our understanding of TBI, there remains a pressing need to comprehensively assess the cognitive and functional consequences of severe brain trauma (Pavlovic et al., 2019; Olsen et al., 2021; Howlett et al., 2022). Various case–control research studies have concluded that the incidence of severe TBI is strongly linked to altered cognitive functionality. As a consequence of the brain injury, TBI patients experienced impaired memory and altered verbal, visual, and learning functions. Moreover, the prevalence of depression is significantly higher in severe TBI cases (Hellawell et al., 1999; Ashman et al., 2008).
Our objective is to provide a comprehensive and evidence-based understanding of the cognitive and functional outcomes in severe TBI cases. This study represents an extensive exploration of cognitive and functional outcomes in severe brain trauma cases through a comprehensive meta-analysis. Our analysis synthesizes data on a range of cognitive domains, including memory, attention, vision, language, and executive functions. By synthesizing data on functional outcomes, we aim to highlight the challenges faced by TBI survivors and the target areas where intervention strategies may be most effective.
Various search engines were employed to gather data, including the Cochrane Library,1 PubMed,2 and Embase3 databases. We used Medical Subject Headings (MeSH) terms as keywords, including “traumatic brain injury,” “severe TBI,” “cognitive impairments associated with TBI,” “severe TBI related physical impairments,” and “TBI induced depression.” Moreover, aside from conducting a methodical search on PubMed, we expanded our search scope by utilizing the “related articles” feature to precisely evaluate the abstracts, studies, and citations. Our database search was confined to records available exclusively in the English language.
This comprehensive meta-analysis has included case–control studies aimed at assessing the association between severe TBI and the development of cognitive disorders and physical impairment. The study included published data spanning various time periods from 1997 to the present, to ensure thorough coverage of the existing literature. In order to maintain the integrity of the exclusion criteria, the following aspects were considered in study selection: (1) the exclusion of animal studies, (2) only limited to studies with published data, (3) the exclusion of articles with inappropriate methodology, data collection, statistical analysis, and overall outcome quality, (4) avoidance of derivative data sources, such as review articles, (5) the exclusion of participants with severe TBI who also had concurrent life-threatening conditions such as cancer, cardiac disorders, neurodegenerative disorders, and other neurological conditions., which ensured a focused analysis of the specific impact of TBI on health outcomes, and (6) the exclusion of participants with mild and moderate TBI.
The characteristics of all included studies are concisely summarized in Table 1. For data retrieval and inclusion, the following parameters were taken into account: (1) case–control studies were selected to gather data on the association between severe TBI and cognitive disorders and physical impairments, (2) the focus was exclusively on patients with severe TBI, (3) studies with sufficient sample size, (4) inclusion of studies with verified measurement methods and appropriate statistical analyses, (5) population inclusion of both males and females, and (6) the inclusion of research studies with well-conducted analyses and outcomes.
Two investigators independently conducted data extraction. Data from the studies included in the analysis were systematically collected and organized within a standardized Excel spreadsheet. The collected data from these studies have included various information, including author names, study locations, publication years, sample sizes, sex distribution, age demographics, follow-up periods, outcome measurements, and research findings. The study selection process is shown in Figure 1, using the PRISMA flow chart. We extracted mean values, standard deviations, and sample sizes from the research studies to evaluate the potential risk of cognitive disorders and physical impairments associated with severe TBI.
To create a comprehensive database for our meta-analysis, a Microsoft Excel spreadsheet was established, including all the pertinent data for the analysis, and was thoroughly reviewed by the third author to resolve any inconsistencies. The third author precisely addressed discrepancies through comprehensive data examination, consultations with co-authors, and utilization of statistical methodologies, ensuring a robust and reliable meta-analysis outcome.
We have included 13 case–control studies in this meta-analysis. In total, 6 studies out of 13 have a population age of ≥45 years and 7 studies include patient populations of age ≥ 25 years. In all included studies, the risk of cognitive disorders, including depression, impaired memory, and poor attention, was assessed along with the physical impairments such as visual disabilities and impaired verbal and learning functions in severely traumatic brain-injured patients. In Table 1, the characteristics and findings of the included studies are summarized.
Following outcome measures from the case–control studies were involved in the pooled estimation of the analysis, such as CVLT, WMS-III, WMS-LM, ES, WMS-VR, COWAT (FAS), WCST CS, MMSE, PSQI, BAI, BDI, GOS, NART, TMT, HISC, GOSE, EOWPVT, NMI, and WMS-R (Table 2). The current comprehensive meta-analysis was performed, involving a meticulous literature search that identified and included 13 research studies. In the first step, a total of 962 studies were identified via database search. After removing duplicates and conducting a preliminary screening of full-text articles, a total of 84 articles were assessed for eligibility. Out of these, 71 studies were excluded based on criteria such as duplicate data, limited sample size, unreliable and complex data, poor assessment methodology, and sub-optimal outcomes. The study selection is illustrated in a PRISMA flow diagram (Figure 1).
In this meta-analysis, all statistical analyses were performed using Review Manager, Version 5.3 (Cochrane Collaboration in Oxford, England). The study adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The means and standard deviations of included research studies were extracted to determine the association between severe TBI and the risk of cognitive disorders and physical impairments by a random-effects model. The estimated pooled mean difference and the corresponding 95% confidence interval (CI) were calculated to estimate the incidence of cognitive disorders in severe TBI patients. We assessed heterogeneity among the studies via the chi-square (χ2) test and the I2 statistics. Cochran’s Q-test yielded a p-value below 0.10, indicating significant statistical heterogeneity.
To assess the association between severe TBI and verbal functionality, a total of 6 case–control studies with a sample size of 568 have generated a pooled estimate of the study’s effect size (Figure 2). The outcomes have reported an SMD of −0.48, which suggests a substantial effect size, indicating that individuals with severe TBI possess lower verbal performance compared to healthy individuals. For visual quality, a total of 6 studies (507 participants) have produced a pooled SMD of −0.26 using a random-effect model, showing a strong association of severe TBI with poor visual outcomes (Figure 3). Moreover, 5 case–control trials with 418 subjects have produced a pooled SMD of −0.27, indicating altered learning abilities in severe TBI patients (Figure 4).
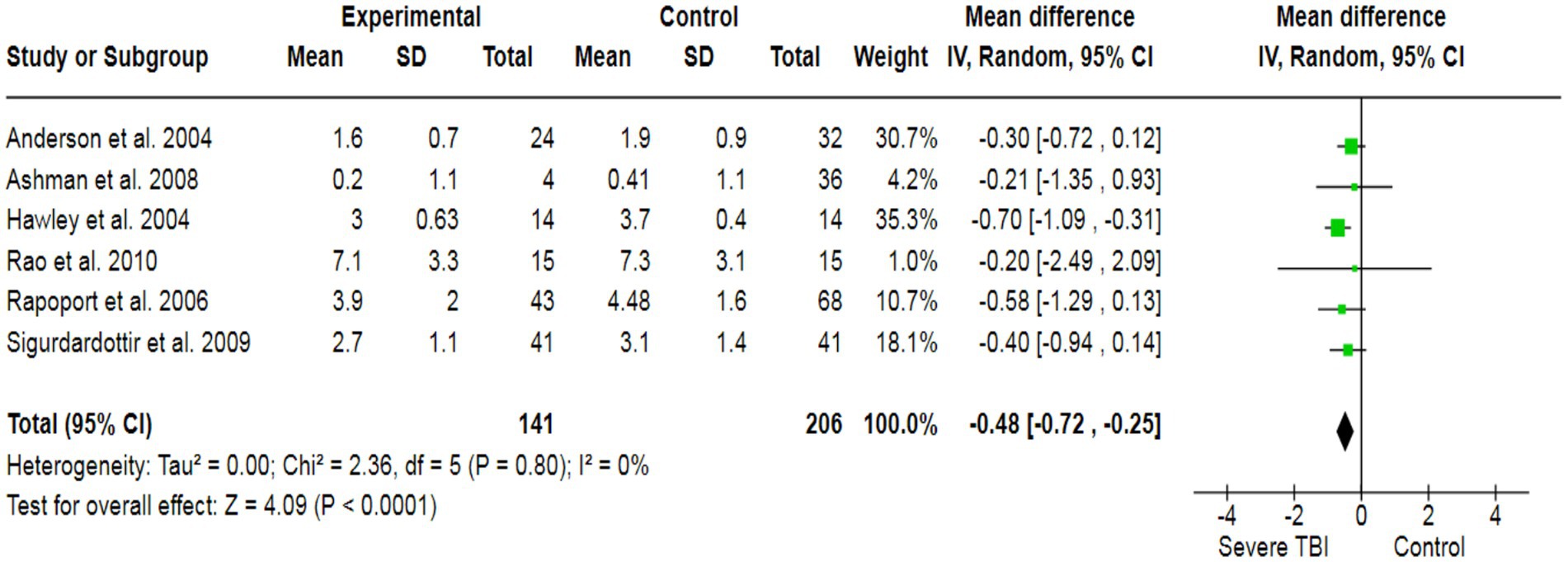
Figure 2. The forest plot of severe TBI and the risk of verbal impairment; diamond (pooled estimate), squares (individual study effects), and horizontal lines (confidence intervals).
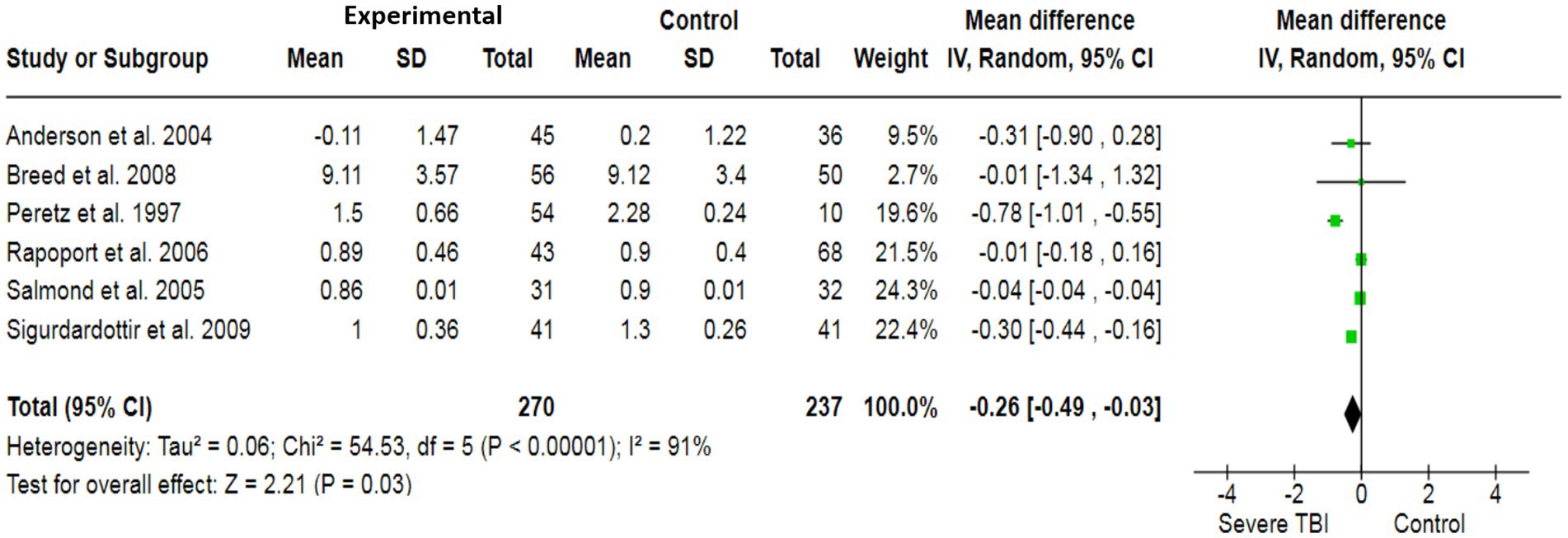
Figure 3. The forest plot of severe TBI and visual impairment risk; diamond (pooled estimate), squares (individual study effects), and horizontal lines (confidence intervals).
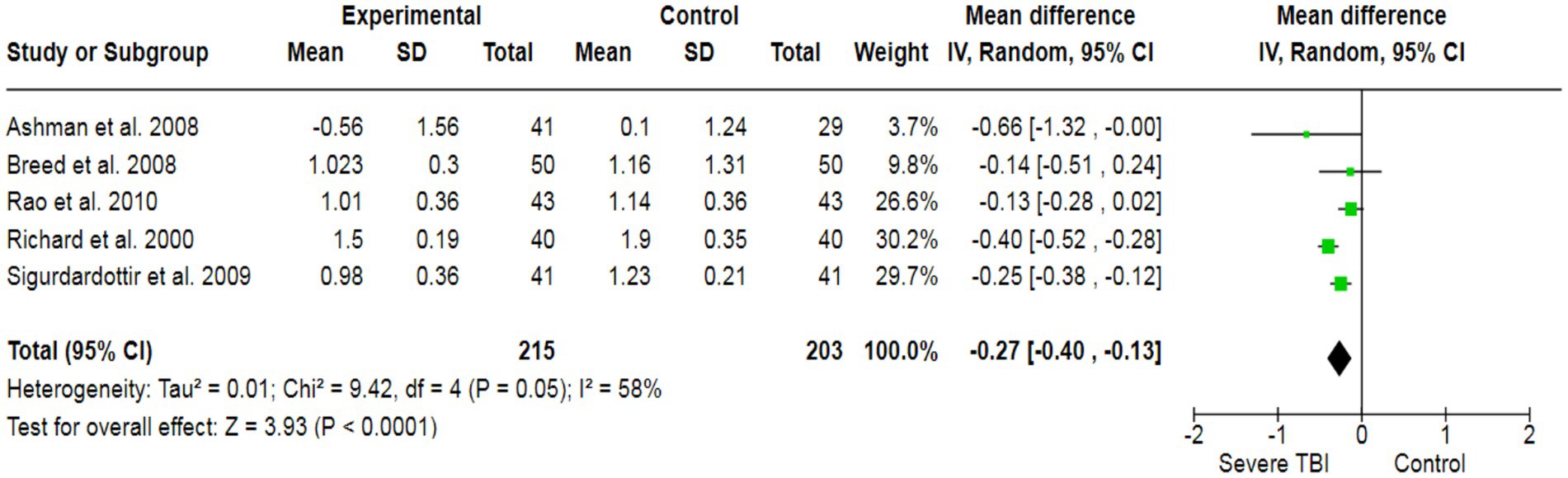
Figure 4. The forest plot of severe TBI and the risk of impairment of learning abilities; diamond (pooled estimate), squares (individual study effects), and horizontal lines (confidence intervals).
To assess the potential inducement of depression in severe TBI patients, we analyzed data from three studies (213 participants), which collectively yielded a pooled effect size of SMD = 3.74 (Figure 5). This indicated a significant association between severe TBI and an increased likelihood of experiencing depression compared to healthy individuals. Additionally, our analysis revealed a strong association between severe TBI and the risk of altered memory (pooled SMD: −0.36) (Figure 6), as well as a significant association between severe TBI and impaired attention (pooled SMD: −0.18) (Figure 7).
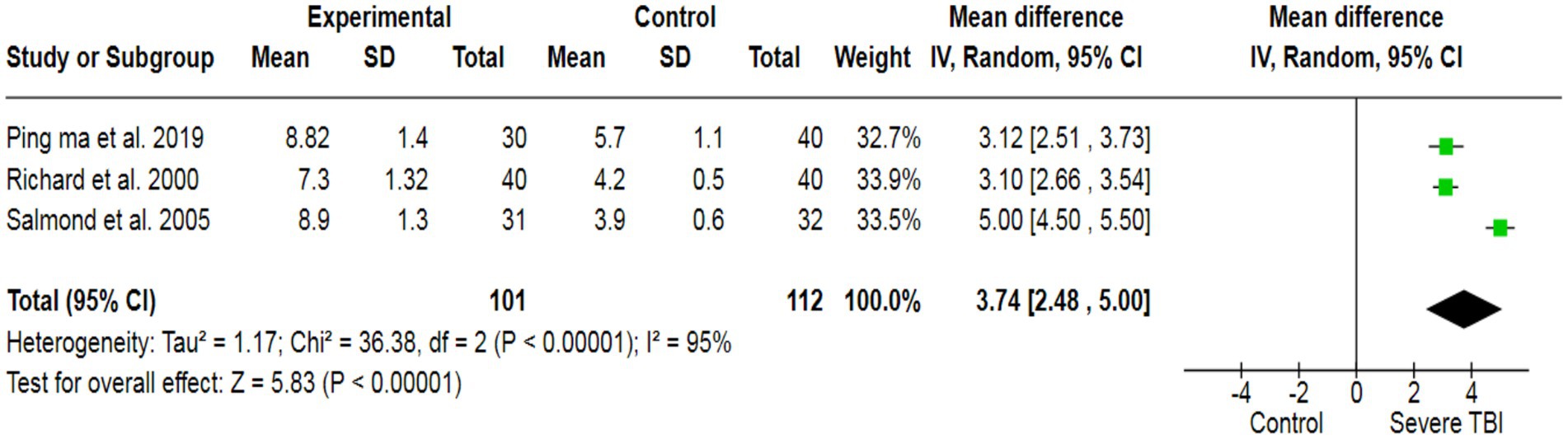
Figure 5. The forest plot of severe TBI and depression risk; diamond (pooled estimate), squares (individual study effects), and horizontal lines (confidence intervals).
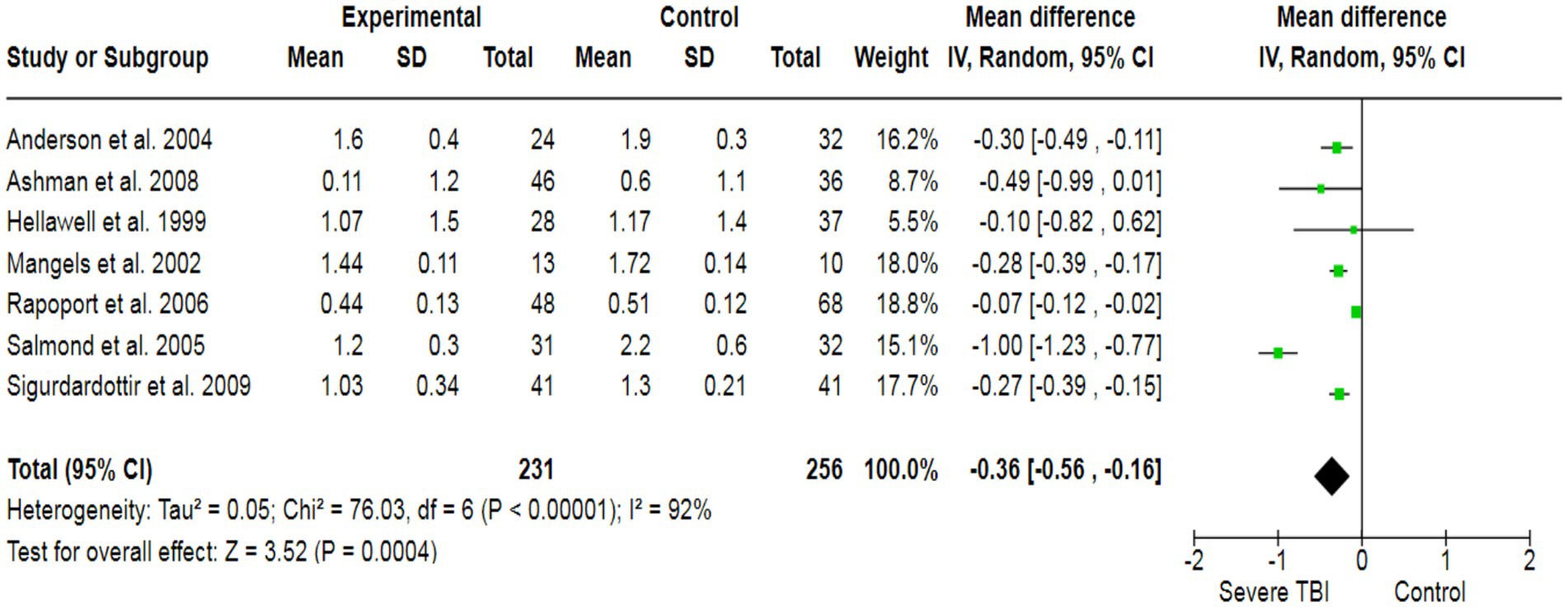
Figure 6. The forest plot of severe TBI and the risk of altered memory; diamond (pooled estimate), squares (individual study effects), and horizontal lines (confidence intervals).
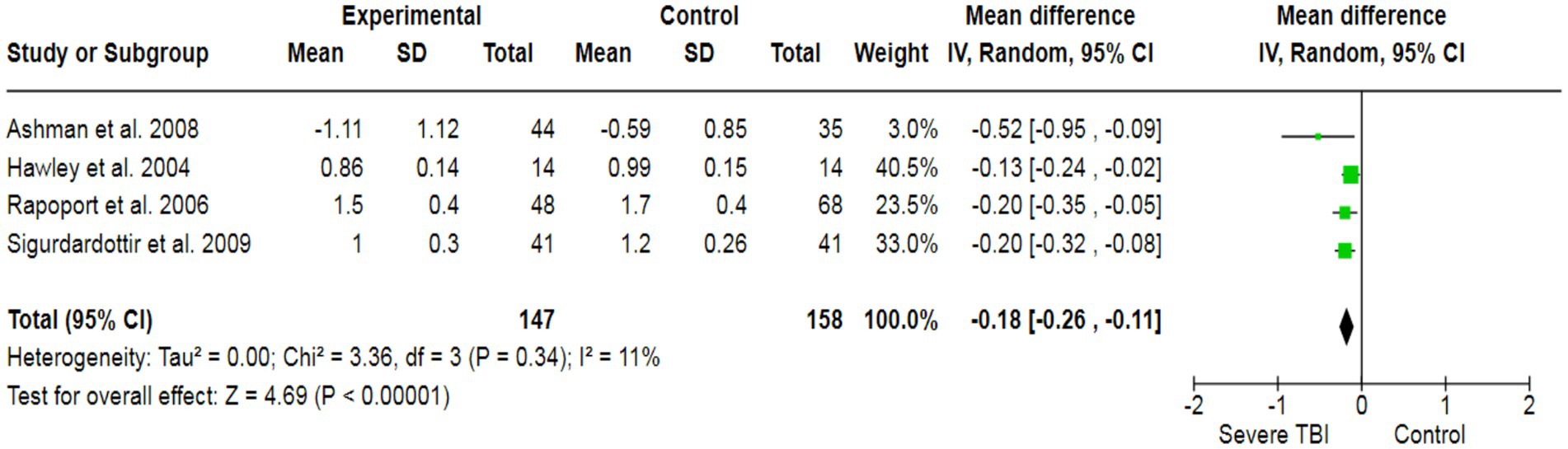
Figure 7. The forest plot of severe TBI and the risk of altered attention; diamond (pooled estimate), squares (individual study effects), and horizontal lines (confidence intervals).
The heterogeneity test was statistically analyzed via the Cochran Q-test. A large heterogeneity was found among studies concerning the relationship between severe TBI and the risk of visual impairment (I2 = 91%), learning abilities (I2 = 58%), the risk of depression (I2 = 95%), altered memory (I2 = 92%), and impaired attention (I2 = 58%), which may have influenced the validity and generalizability of the results.
The potential risk of bias for each included study was independently evaluated by the Cochrane Collaboration to assess methodological quality (Figure 8). Several research trials showed high risk, with major sources of bias associated with performance bias, allocation concealment, self-reporting outcomes, random sequence generation, and protection from other potential biases. Due to the challenge of unsegregated participants and the age factor, along with multiple outcome measures, the majority of RCTs included here are at greater risk of bias.
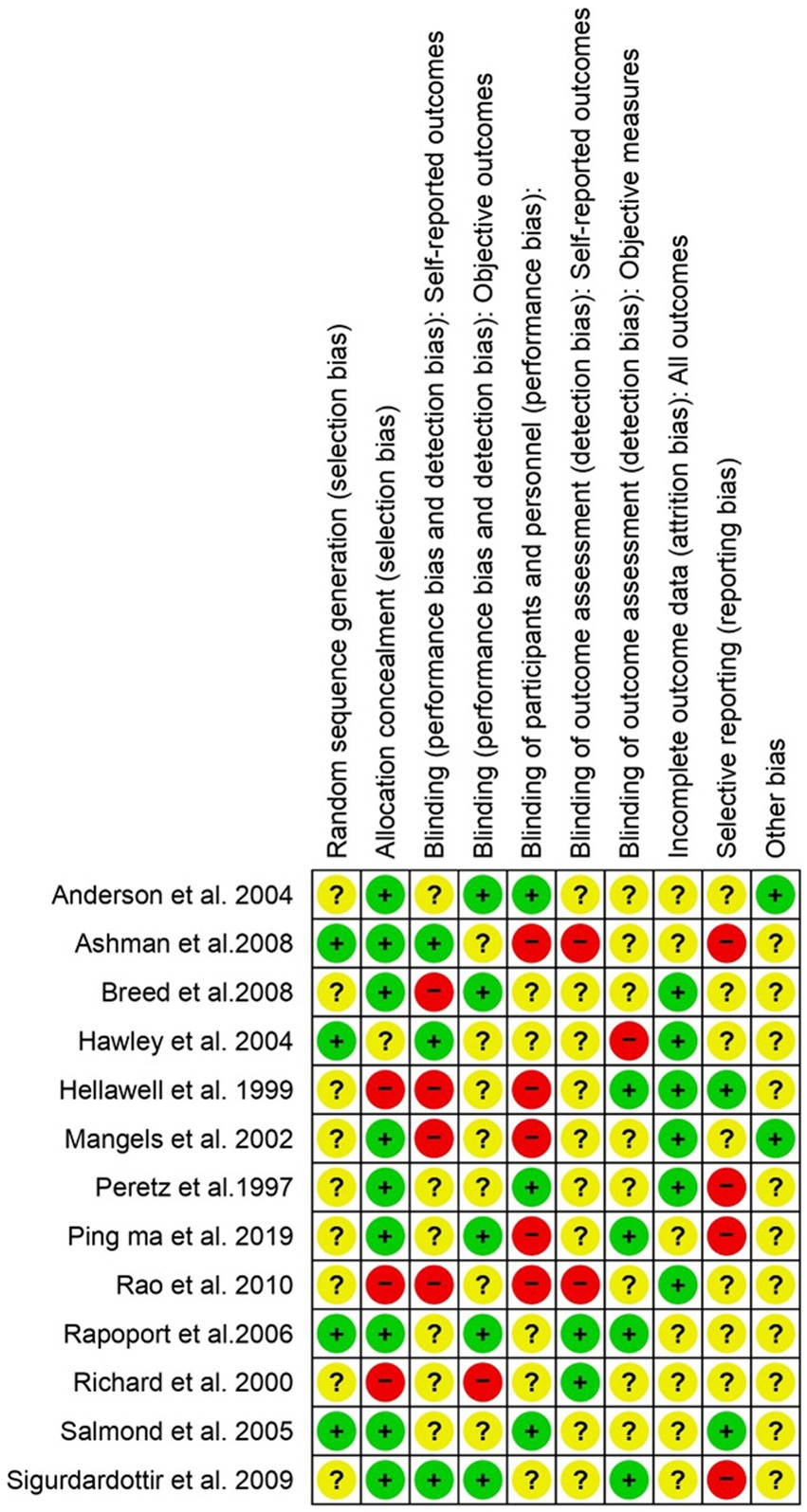
Figure 8. The risk of bias assessment for each included study in accordance with “Cochrane RoB 2”. Low risk (+), unclear (?), and high risk (−).
Severe TBI significantly affects various dimensions, including cognitive functions, emotional wellbeing, and physical abilities. The complex interplay of neural damage, disrupted neurochemical balance, and associated complications often leads to critical challenges in memory and executive functions, emotional regulation, and motor skills. Additionally, it can lead to behavioral changes and impaired learning abilities. These alterations disturb a person’s social and psychological wellbeing (Arciniegas et al., 2002). The primary aim of this comprehensive meta-analysis is to determine the altered functional cognitive impairments, including verbal, visual, learning, attention, and memory disabilities, and the inducement of depression in severe traumatic brain-injured patients. This comprehensive meta-analysis review included 13 studies with 1,442 study participants, which provided data for analysis. The estimated pooled analysis outcomes of our study revealed that severe traumatic brain injuries have a significantly strong association with impaired memory, visual functionality, learning abilities, verbal functions, attention deficits, and the inducement of depression.
Numerous research studies corroborate our findings. An investigative study has shown that patients who have experienced severe TBI exhibit highly significant alterations in verbal and visual functionalities, as well as impaired attention and memory. This study was conducted by measuring various outcome measures, including CVLT, COWAT, WMS-LM, and WMS-VR (Ashman et al., 2008). In this comprehensive meta-analysis, 13 case–control studies were included with 1,442 participants to determine the association between severe TBI and cognitive and functional disabilities, including memory, depression, attention deficit, learning disabilities, and verbal and visual impairments. The pooled outcomes of the current analysis revealed that severe TBI has a significant association with altered cognitive and functional abilities. The outcome measuring instruments for the analysis are good in construct validity and reliability, elaborating that these are high-quality measures of primary and secondary outcomes, including depression, verbal, visual, learning, memory, and attention.
A case–control study involving TBI patients has demonstrated that several cognitive dysfunctions were highly significant in patients over the age of 65 years who had experienced severe TBI. This study assessed learning and visual abilities using outcome measures such as WMS-VR and WMS-LM. Outcomes from the study revealed that in older adult patients, significant alterations in visual and learning abilities were found (Breed et al., 2008). Similarly, in younger severe TBI patients aged 6 to 40 years, statistically significant alterations in intellectual, verbal, and memory strengths were found, which were measured using MS-III and WMS-R outcome measures (Mangels et al., 2002; Hawley, 2004). Similarly, a case–control study was conducted in 2004, including 117 participants, consisting of 33 control subjects and 84 severe TBI patients aged 2–7 years. The outcomes revealed that severe TBI patients in this group exhibited impaired learning and memory functionality, which was assessed using the EOWPVT and NMI outcome measures (Anderson et al., 2004).
To prevent cognitive and functional disabilities in severe TBI patients, it is important to get immediate and specialized medical care, with a focus on reducing injury and alleviating cognitive dysfunctionalities. Offering cognitive therapy and emotional support can help to improve their long-term recovery. Further advanced research studies are required in this field to provide a more comprehensive understanding of the association between severe TBI and functional and cognitive disabilities, including depression, attention deficit, verbal and visual impairment, and learning abilities. Novel research studies are needed to explore the intricate mechanisms underlying the association between severe TBI and cognitive disabilities, utilizing sophisticated neuroimaging techniques, longitudinal assessments, and detailed neurobehavioral analyses. Moreover, intervention-focused studies aimed at evaluating personalized therapeutic approaches and their impact on long-term functional outcomes will significantly contribute to improving patient care.
Our findings indicated a strong association between severe TBI and the risk of cognitive and functional disabilities. However, there are some study limitations in this meta-analysis, including randomized controlled studies that are not evaluated with reference to some essential factors, including patients’ age, body mass index, ethnicity, social and demographic statuses, sample size, and co-morbidities.
Our findings demonstrate a strong association between severe TBI and impaired cognitive and functional abilities. The results indicate significant impairments in memory, verbal and visual disabilities, depression inducement, attention deficits, and learning disabilities among individuals with severe TBI compared to the control group. These outcomes highlight the importance of understanding the long-term effects of TBI on various cognitive and functional domains.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
ZS: Conceptualization, Methodology, Writing – original draft. YJ: Software, Writing – original draft. NM: Software, Writing – original draft. WZ: Formal analysis, Writing – original draft. ZY: Formal analysis, Writing – original draft. SW: Data curation, Writing – original draft. QL: Data curation, Writing – original draft. JR: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Aharon-Peretz, J., Kliot, D., Amyel-Zvi, E., Tomer, R., Rakier, A., and Feinsod, M. (1997). Neurobehavioral consequences of closed head injury in the elderly. Brain Inj. 11, 871–876. doi: 10.1080/026990597122945
Anderson, V. A., Morse, S. A., Catroppa, C., Haritou, F., and Rosenfeld, J. V. (2004). Thirty month outcome from early childhood head injury: a prospective analysis of neurobehavioural recovery. Brain 127, 2608–2620. doi: 10.1093/brain/awh320
Arciniegas, D. B., Held, K., and Wagner, P. (2002). Cognitive impairment following traumatic brain injury. Curr. Treat. Options Neurol. 4, 43–57. doi: 10.1007/s11940-002-0004-6
Ashman, T. A., Cantor, J. B., Gordon, W. A., Sacks, A., Spielman, L., Egan, M., et al. (2008). A comparison of cognitive functioning in older adults with and without traumatic brain injury. J. Head Trauma Rehabil. 23, 139–148. doi: 10.1097/01.HTR.0000319930.69343.64
Breed, S., Sacks, A., Ashman, T. A., Gordon, W. A., Dahlman, K., and Spielman, L. (2008). Cognitive functioning among individuals with traumatic brain injury, Alzheimer's disease, and no cognitive impairments. J. Head Trauma Rehabil. 23, 149–157. doi: 10.1097/01.HTR.0000319931.76966.ff
Hawley, C. A. (2004). Behaviour and school performance after brain injury. Brain Inj. 18, 645–659. doi: 10.1080/02699050310001646189
Hellawell, D. J., Taylor, R. T., and Pentland, B. (1999). Cognitive and psychosocial outcome following moderate or severe traumatic brain injury. Brain Inj. 13, 489–504. doi: 10.1080/026990599121403
Howlett, J. R., Nelson, L. D., and Stein, M. B. (2022). Mental health consequences of traumatic brain injury. Biol. Psychiatry 91, 413–420. doi: 10.1016/j.biopsych.2021.09.024
Ma, H. P., Chen, P. S., Wong, C. S., Chang, C. F., Ou, J. C., Tsai, Y. R., et al. (2019). Psychometric evaluation of anxiety, Depression, and Sleep Quality after a Mild Traumatic Brain Injury: a Longitudinal Study. Behav. Neurol. 2019:4364592. doi: 10.1155/2019/4364592
Mangels, J. A., Craik, F. I., Levine, B., Schwartz, M. L., and Stuss, D. T. (2002). Effects of divided attention on episodic memory in chronic traumatic brain injury: a function of severity and strategy. Neuropsychologia 40, 2369–2385. doi: 10.1016/S0028-3932(02)00084-2
Ng, S. Y., and Lee, A. Y. W. (2019). Traumatic brain injuries: pathophysiology and potential therapeutic targets. Front. Cell. Neurosci. 13:528. doi: 10.3389/fncel.2019.00528
Olsen, A., Babikian, T., Bigler, E. D., Caeyenberghs, K., Conde, V., Dams-O’Connor, K., et al. (2021). Toward a global and reproducible science for brain imaging in neurotrauma: the ENIGMA adult moderate/severe traumatic brain injury working group. Brain Imaging Behav. 15, 526–554. doi: 10.1007/s11682-020-00313-7
Orr, M. B., and Gensel, J. C. (2017). Interactions of primary insult biomechanics and secondary cascades in spinal cord injury: implications for therapy. Neural Regen. Res. 12, 1618–1619. doi: 10.4103/1673-5374.217332
Pavlovic, D., Pekic, S., Stojanovic, M., and Popovic, V. (2019). Traumatic brain injury: neuropathological, neurocognitive and neurobehavioral sequelae. Pituitary 22, 270–282. doi: 10.1007/s11102-019-00957-9
Rao, V., Bertrand, M., Rosenberg, P., Makley, M., Schretlen, D. J., Brandt, J., et al. (2010). Predictors of new-onset depression after mild traumatic brain injury. J. Neuropsychiatry Clin. Neurosci. 22, 100–104. doi: 10.1176/jnp.2010.22.1.100
Rapoport, M. J., Herrmann, N., Shammi, P., Kiss, A., Phillips, A., and Feinstein, A. (2006). Outcome after traumatic brain injury sustained in older adulthood: a one-year longitudinal study. Am. J. Geriatr. Psychiatry 14, 456–465. doi: 10.1097/01.JGP.0000199339.79689.8a
Richards, B. (2000). The effects of aging and mild traumatic brain injury on neuropsychological performance. York University, Ontario. Canada: Citeseer.
Robinson, C. P. (2021). Moderate and severe traumatic brain injury. Continuum (Minneap Minn) 27, 1278–1300. doi: 10.1212/CON.0000000000001036
Salmond, C. H., Chatfield, D. A., Menon, D. K., Pickard, J. D., and Sahakian, B. J. (2005). Cognitive sequelae of head injury: involvement of basal forebrain and associated structures. Brain 128, 189–200. doi: 10.1093/brain/awh352
Keywords: brain trauma, severe TBI, depression, verbal and visual disabilities, learning and memory impairment, cognitive disabilities
Citation: Shuanglong Z, Jiangyuan Y, Meng N, Zheng W, Yunshui Z, Wei S, Li Q and Rongcai J (2024) A meta-analysis of cognitive and functional outcomes in severe brain trauma cases. Front. Behav. Neurosci. 18:1349672. doi: 10.3389/fnbeh.2024.1349672
Received: 05 December 2023; Accepted: 26 February 2024;
Published: 14 March 2024.
Edited by:
Kevin D. Beck, The State University of New Jersey, United StatesReviewed by:
Zhuofan Lei, University of Maryland, United StatesCopyright © 2024 Shuanglong, Jiangyuan, Meng, Zheng, Yunshui, Wei, Li and Rongcai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiang Rongcai, emhhbmdzaHVhbmdsb25nMjA2QG91dGxvb2suY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.