
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Audiol. Otol., 17 April 2025
Sec. Clinical Research in Auditory Implants and Hearing Aids
Volume 3 - 2025 | https://doi.org/10.3389/fauot.2025.1583242
Introduction: Bilateral cochlear implantation is the typical intervention for children with severe-to-profound sensorineural hearing loss, but speech perception and hearing outcomes remain variable. This scoping review explores which contextual factors relate to speech perception and hearing outcomes following pediatric bilateral cochlear implantation based on themes aligned with Bronfenbrenner's bioecological systems theory: (1) individual; (2) microsystem; (3) mesosytem; (4) exosystem; (5) macrosystem; and (6) chronosystem.
Method: PRISMA-ScR guidelines were followed to systematically search nine electronic databases with a keyword strategy. Eligible studies were published in English and included an analysis of contextual factors in relation to a behavioral speech perception or hearing outcome measure. Study quality was assessed using Quality Assessment with Diverse Studies (QuADS) criteria and the role of contextual factors in outcomes was explored with a narrative synthesis approach.
Results: Twenty-three research articles met the criteria for inclusion. Contextual factors identified ranged from the proximal to distal context. Contextual factors such as non-verbal cognitive ability, social skills, cochlear implant usage, positive parent-child interactions, educational placement, auditory or oral therapy, ethnicity and prematurity were related to cochlear implant outcomes.
Discussion: Relationships between contextual factors and outcomes were not consistent across developmental time or studies. Study quality and methodological limitations are discussed. Research on outcomes related to bilateral cochlear implantation should actively integrate and examine contextual factors in prospective, longitudinal designs. This approach will facilitate the development of interventions to target specific levels of the bioecological system, thereby improving outcomes for the pediatric bilateral cochlear implant recipient.
A cochlear implant (CI) converts sound signals into electrical impulses for transmission to the auditory cortex via an electrode array implanted in the cochlea, providing access to environmental sounds including speech and music (Deep et al., 2019; Macherey and Carlyon, 2014). Since the first UK CI in 1989, the number of implantations has surged. In the UK, over 4,900 children with severe-to-profound sensorineural hearing loss have at least one CI (CRIDE, 2023). Advances in electrode design and preservation methods have improved the likelihood of preserving residual hearing post-implantation (Deep et al., 2019; NICE., 2009; van der Straaten et al., 2021). Candidacy guidelines have also relaxed with evidence that individuals with better pre-implant hearing benefit from CIs (Lovett et al., 2015; Vickers et al., 2015), allowing individuals with some residual hearing to qualify for implantation. Simultaneous bilateral cochlear implantation is now the recommended standard of care in the UK for children with sensorineural hearing loss where bilateral hearing aids do not provide adequate benefit (NICE., 2009).
Despite providing degraded auditory signal representation, including amplitude, temporal, and frequency distortions with inter-electrode variability (Macherey and Carlyon, 2014), CIs produce several beneficial outcomes. Early cochlear implantation for children born with severe-to-profound hearing loss provides access to audition for language development during a critical period of cortical plasticity, especially before 3.5 years of age (Kral and Sharma, 2012; Persic et al., 2020; Sharma et al., 2005, 2002). The efficacy and success of pediatric cochlear implantation is typically measured by speech perception, speech production and language acquisition abilities in children, or functional evaluations of listening in infants. In addition to improved aural/oral language skills, early cochlear implantation supports recipients to develop reading and cognitive skills, as well as social, behavioral and academic skills comparable to hearing typically developing children (Barker et al., 2009; Cejas et al., 2023; Geers et al., 2013; Hoffman et al., 2015; McSweeny et al., 2021; Scherf et al., 2009; Wang et al., 2021).
Despite similar pre-implant factors, there remains considerable unexplained variation in outcomes for CI recipients (Driver and Jiang, 2017; Pisoni et al., 2017). Not all children who receive CIs achieve typical age-appropriate hearing or speaking skills (Litovsky and Gordon, 2016; van Wieringen and Wouters, 2015). In addition, pediatric CI recipients may have comorbid or additional difficulties or diagnoses that negatively impact implantation outcomes (Cejas et al., 2015). Though sensorineural hearing loss has been linked to poorer quality of life (Ronner et al., 2020; Umansky et al., 2011), better audiological and language skills, maternal educational level, and familial support of pediatric CI recipients have all been associated with improved life quality (Silva et al., 2020). Despite the wealth of research on a variety of predictive factors for CI outcomes (Boons et al., 2012; Cejas et al., 2023; Davidson et al., 2019; Geers and Nicholas, 2013; Glaubitz et al., 2021; Ruben, 2018; Tobey et al., 2013), such as age at implantation and inter-implant delay (Sharma et al., 2020), electrode array positioning (Aschendorff et al., 2007), the importance of long-term post-implantation follow-ups (Wie et al., 2020), and unilateral or bilateral implantation (Eskridge et al., 2021), the impact of the child's developmental context on their cochlear implant-related outcomes has been far less explored.
Whether retrospective chart reviews or experimental work, research has often grouped patients by surgical or implant factors, such as age at implant, inter-implant interval, and whether implants were sequentially or simultaneously implanted. Group averages have been compared to determine which factors confer benefit or risk for speech perception and audiological outcomes post-implantation (Boons et al., 2012; Holt et al., 2020). This approach ignores the intra-individual heterogeneity inherent between as well as within patient groups, even when matched for gender, age, hearing and language experience. Individuals are situated within their specific developmental context, encompassing all external factors that are not directly related to the intervention itself, which may contribute directly or indirectly to the intervention outcomes. It remains unclear which contextual factors are developmentally relevant for speech perception or audiological outcomes for the pediatric bilateral CI recipient. The revised Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) guidelines advocate reporting of context for healthcare interventions (Goodman et al., 2016), to aid with understanding what influences success in healthcare interventions. However, a theoretical framework grounded in developmental context is crucial to assess how various contextual factors shape developmental trajectories and interact over time.
There is good reason to consider the ecology of the individual, as CI outcomes will be influenced by the environment in which an individual is situated and the interactions the individual has with others (Bronfenbrenner, 1977). Bronfenbrenner's ecological and bioecological theories emphasize the interdependence of the developing person and the context in which they are developing (Bronfenbrenner, 1977; Bronfenbrenner and Evans, 2000). These theories acknowledge a multitude of factors that interact dynamically and reciprocally to influence the outcomes of the developing person, including process, person, context and time (Bronfenbrenner and Morris, 2006). Since its inception, the bioecological theory and its subsequent iterations have provided a holistic framework for considering how interconnected systems impact on an individual's development. As such, the theory is valuable for considering the range and level at which biopsychosocial contextual factors exert an influence on developmental outcomes for pediatric CI recipients in relation to both within-patient and external environmental factors.
Across various re-iterations of this influential theory (Rosa and Tudge, 2013), Bronfenbrenner described the levels at which the developing individual could be influenced by the context in which they are situated (illustrated in Figure 1): individual (concerning within-person variation), microsystem (most proximal — e.g., family, school or neighborhood), mesosystem (two or more interacting microsystems — e.g., relationships between school and home; how education or healthcare providers interact with the family), exosystem (outside of the direct physical proximity to the developing person — e.g., parental workplace or access to audiology services), macrosystem (most distal — e.g., societal, socioeconomic or cultural influences), and chronosystem (events over the individual's developmental phase; sociohistorical context that the individual develops in). Whilst a bioecological systems approach has been recommended to establish the ecology most conducive to development across cognitive, social and linguistic domains for deaf children (Clark et al., 2019), to our knowledge, Bronfenbrenner's framework has not been actively adopted for the study of post-implant speech perception and audiological outcomes across CI recipients.
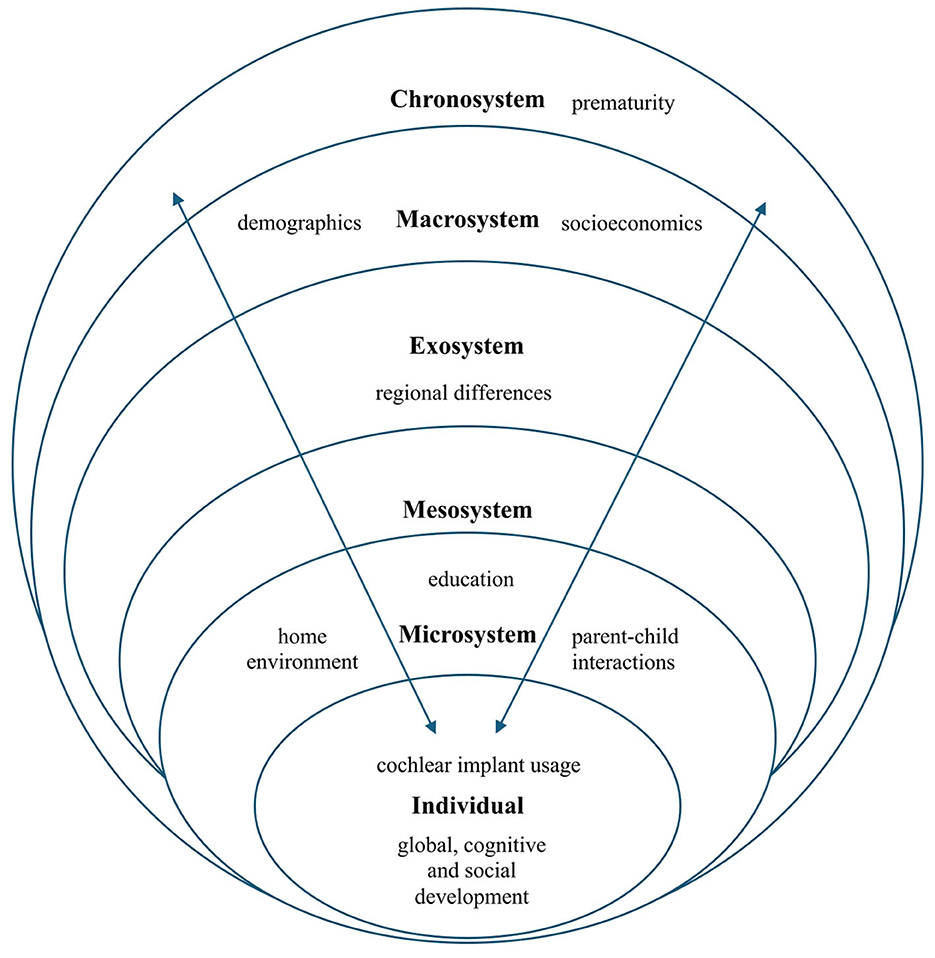
Figure 1. Illustration of Bronfenbrenner's Bioecological Systems Theory with the contextual factors identified in this scoping review (adapted from Rosa and Tudge, 2013).
This framework allows us to conceptualize the systems influencing pediatric outcomes following implantation. Though previous research has not directly adopted this framework, the importance of within-patient variability (individual differences), due to factors like additional diagnoses or neurocognitive functioning (Fortnum and Davis, 1997; Kennedy et al., 2006), has been explored. External or environmental factors have also been associated with CI outcomes, though not necessarily analyzed as part of a holistic developmental framework. Social determinants of health, such as socioeconomic status, home environment and parental education level have been shown to influence language outcomes in previous reviews (Holzinger et al., 2020; Sharma et al., 2020). Beyond the home environment, early educational placements in preschools with an intervention program to support the language development of children with CIs led to improved later language outcomes (Moog and Geers, 2010). These examples indicate that developmental context plays an important role in cochlear implantation outcomes, but no structured framework per se was adopted to systematically analyze the results.
To the best of our knowledge, Bronfenbrenner's framework has been referenced in a limited number of studies investigating the microsystem of family ecology (influence of family composition, functioning, and environment) in relation to language outcomes following cochlear implantation (Davenport and Holt, 2019; Holt et al., 2020). For instance, familial interactions and support are associated with psychosocial and neurocognitive outcomes for children who use hearing aids or CIs, and the authors suggest a bidirectional relationship between the family microsystem and language outcomes (Holt et al., 2020). Despite these indications of the importance of external developmental factors, a lack of developmental theoretical framework has resulted in an absence of consensus on predictive or prognostic factors and mechanisms or their relative importance across development for pediatric CI recipients. Placing the individual in its larger ecology to explore developmental factors related to post-implantation outcomes can yield useful information to optimize support and outcomes for CI recipients. Additionally, it fosters a multidisciplinary approach by incorporating insights from audiology, psychology, education, and social sciences to identify both clinical benefits and social challenges that may influence implantation success.
With the dearth of research examining developmentally relevant predictive factors for CI outcomes, this scoping review aims to explore the impact of contextual factors associated with speech perception and hearing outcomes following pediatric bilateral cochlear implantation as part of a wider novel auditory intervention project (Vickers et al., 2021). First, using Bronfenbrenner's ecological systems theory as a framework, we aimed to identify which contextual factors have been studied in relation to speech perception or hearing outcomes in pediatric CI recipients. We focused on speech perception and hearing outcomes rather than language outcomes which relate to comprehension, as it has been argued that these should be differentiated in evaluations (Coene and Govaerts, 2014). Our second aim was to explore the predictive value of identified contextual factors on cochlear implant-related outcomes across development.
We followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Review (PRISMA-ScR) guidelines (Page et al., 2021; Tricco et al., 2018) to conduct the review.
Inclusion criteria included: (1) studies published in the English language; (2) a minimum of one participant implanted under the age of 18 years old in studies where both children and adults were included; (3) a minimum of one participant implanted bilaterally in studies where both unilaterally and bilaterally implanted participants were included, and (4) analysis of the effect of a contextual factor in relation to a behavioral speech perception or hearing outcome measure. Age-at-implantation and inter-implant interval are considered important individual predictive contextual factors for CI outcomes but were not included herein as these have been reviewed extensively elsewhere (Sharma et al., 2020).
Studies excluded from the review comprised review articles, conference abstracts and unpublished studies. Studies focusing only on neuroatypical populations (e.g., Goldenhar, Pendred syndrome, Down's syndrome, Autism, intellectual disability, Auditory Neuropathy Spectrum Disorder) without a typically developing implanted group were also excluded, as it is difficult to disentangle the effects of cochlear implantation and neuroatypicality on outcomes. Finally, studies reporting only pure-tone audiological measurements or event-related potentials, as opposed to behavioral hearing or speech perception outcomes, were excluded.
More recent studies tend to have a higher proportion of bilaterally implanted participants because of candidacy criteria changes (NICE., 2009). Better speech perception, sound localization and receptive vocabulary scores have been reported for children with bilateral implants compared to unilateral implants (Lovett et al., 2010; Sparreboom et al., 2015). It is thus possible that the effects observed in the reviewed studies would be attenuated by samples comprising only bilaterally implanted children, but these studies were included to ensure a comprehensive review of the literature. Where implantation type (bilateral or unilateral) was not specified, articles were excluded, as bilateral implantation is only a relatively recent recommendation by the UK's National Institute for Care and Excellence (NICE., 2009).
The following databases were searched for journal articles reporting retrospective or prospective studies published at any time before 25th January 2023: PubMed, WebofScience, Scopus, PsycInfo, PsycExtra, AMED, EMBASE, MEDLINE, and Cinahl.
A keyword strategy was used to search for articles reporting hearing and speech perception outcomes following pediatric bilateral cochlear implantation, using the National Library of Medicine's Medical Subject Headings (MeSH) database to refine search keywords. The search comprised the keywords: “cochlear implant” or “cochlear implantation” and “child” or “infant” or “pediatric” or “adolescent” or “adolescence” or “teenage” and “hearing outcome” and “speech perception”. We did not include the term “bilateral”, as it failed to consistently identify articles with pediatric bilateral cochlear implant users and would have excluded many studies including both bilateral and unilateral participants.
Search results were extracted from the data sources into an EndNote library for removal of duplicates and screening. Studies for inclusion were identified, screened, and reviewed by the first author, and verified by the second author. Study data were extracted, including participant details (N, type of implant, age, where available), the identified contextual factors, behavioral speech perception or hearing outcomes, statistical analyses and study characteristics (study design and country).
The quality of individual studies was assessed using the criteria detailed in the Quality Assessment with Diverse Studies (QuADS) appraisal tool (Harrison et al., 2021). This tool is used to assign each study a score between 0–3 on 13 study quality criteria, such as ‘description of data collection procedure' and ‘strengths and limitations critically discussed', resulting in a maximum score of 39.
The systematic search returned 6,549 publications after duplicate publications were removed. Following title and abstract screening, 162 publications were retrieved for full-text screening. Twenty-three of these publications met the eligibility criteria for inclusion in this review, with the PRISMA workflow outlined in Figure 2.
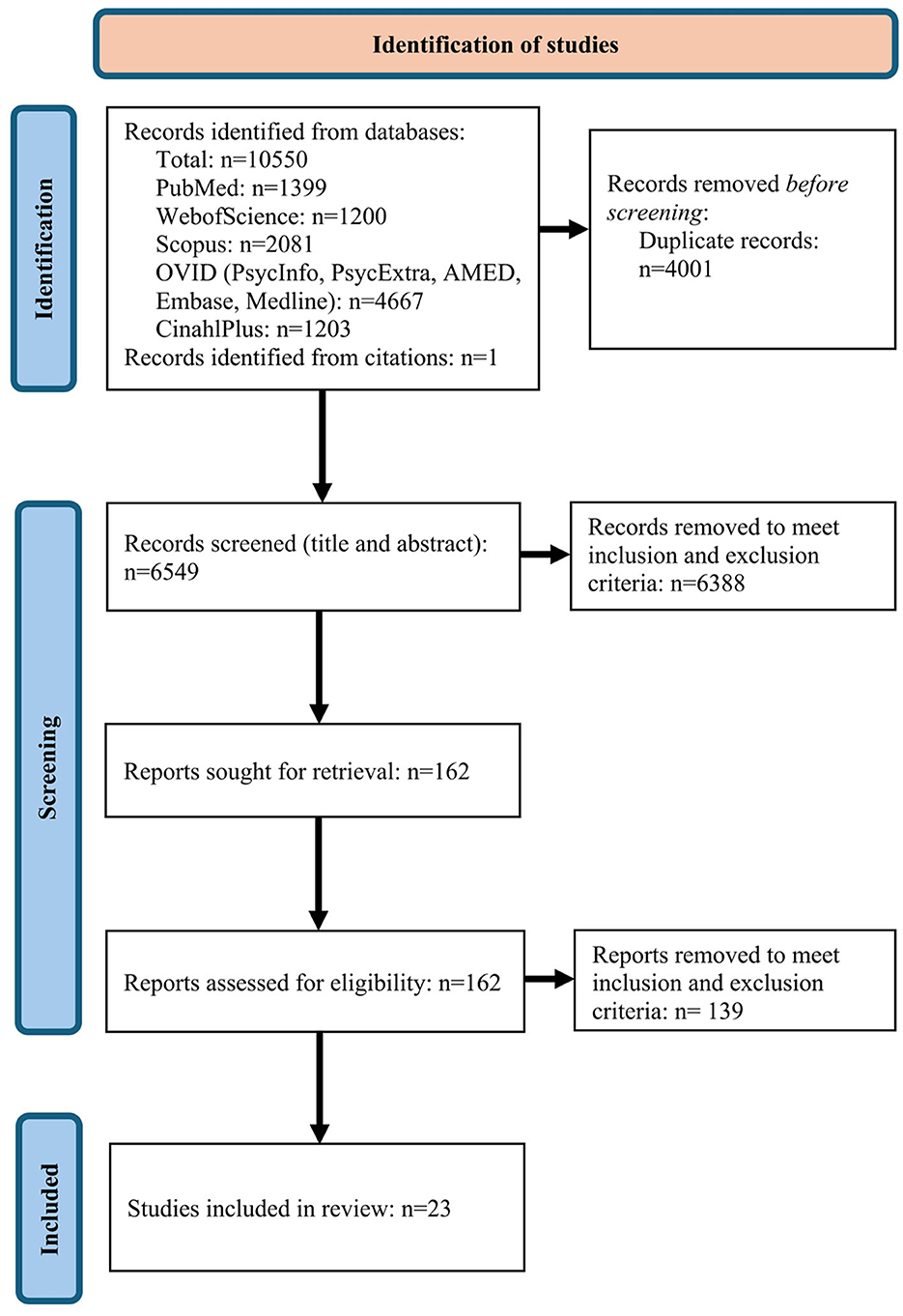
Figure 2. PRISMA flow chart illustrating identification of the studies for inclusion in the review (adapted from Page et al., 2021).
Table 1 outlines the contextual factors explored in relation to pediatric CI recipients' outcomes for each study included in the review. Contextual factors were grouped into themes aligned with Bronfenbrenner's bioecological systems theory: (1) individual (global, cognitive and social development and CI usage); (2) microsystem (parent-child interactions, home environment, education and communication mode); (3) exosystem (regional differences); (4) macrosystem (child and family demographics and socioeconomic factors), and (5) chronosystem (prematurity), as illustrated in Figure 1. Due to the heterogeneity of participant characteristics, outcome measures, and definitions of contextual factors in the studies included herein, a narrative synthesis approach was adopted. Studies were not pooled for effect size calculations and results are instead discussed qualitatively.
Our evaluation of study quality using the QuADS criteria (Harrison et al., 2021) is shown in Table 2. The QuADS tool has demonstrated good face and content validity in systematic reviews of health services research with a kappa of 0.66 for inter-rater reliability (Harrison et al., 2021). The quality of studies was rated by the first author and verified by the second author with discussion to agree all ratings. The two raters scored an average of 23.85 and 23.17 on the QuADS criteria, with the Mean Absolute Difference (MAD) at 0.68. The agreement percentage was thus approximately 97.11%, indicating a very high level of agreement between the two raters.
As Table 2 shows, the reviewed studies generally provided a clear description of the methods and research setting, with appropriate data collection tools and analytical methods. No study showed evidence that the research stakeholders (e.g., children with CIs, their caregivers, or educators) were involved in the research design. However, the requirement for patient and public involvement in research is still relatively new from research funders, so this is perhaps unsurprising. Additionally, most studies were retrospective, with limited evidence of sampling or power calculations across studies. Few studies reported explicit research questions or hypotheses. The reviewed studies generally scored low on reporting appropriate justification for selected analytic methods, providing full details about recruitment data (including discrepancies between target and recruitment numbers), or providing theoretical or conceptual underpinnings for the research over and above general reference to broad theories or key concepts in the Introduction to each study. In addition, the studies scored low on providing rationale for choice of data collection tools, and critical discussion of strengths and limitations. In sum, the studies included in this review received an average quality score of 62.53%.
Here, we discuss key findings from each theme in relation to speech perception or hearing outcomes and related research.
Individual factors concern within-person variation, and the individual factors identified herein encompassed global development, development in cognitive and social domains, and CI usage, with interactions changing over development and across domains. Better expressive vocabulary, non-verbal intelligence, and verbal intelligence were associated with better speech perception in some (Davidson et al., 2019; De Raeve et al., 2015; Niparko et al., 2010), but not all (e.g., Geers et al., 2013) studies. Cognitive skills were significantly associated with open-set phoneme, word and sentence scores at primary school entry (Dettman et al., 2016). However, this relationship changed over time, such that these cognitive skills were only significantly associated with open-set word and sentence scores by the end of primary school.
Less attention has been given to the relationship between global or social development and CI outcomes, but global development measured pre-implantation was not significantly related to auditory performance outcomes (Yang et al., 2020). Social development was specifically related to indexical speech perception (such as emotion identification and talker discrimination), but not linguistic speech perception (Geers et al., 2013). Better indexical speech perception was also associated with younger age at entering mainstream education placements, raising the possibility that age at mainstreaming mediates the association between social skills and speech perception, but these factors were not examined together.
The opportunity to extract data logs indicating granular CI use from individual devices has only emerged over the last two decades. Daily CI use was measured through device data logging or reports from patients, parents and clinicians. Increased CI usage was consistently related to better speech perception outcomes (Cesur et al., 2020; Easwar et al., 2018; Forli et al., 2023; Kleijbergen et al., 2022; Li et al., 2023; Sparreboom et al., 2012; Wiseman et al., 2021). Mean estimates of daily CI use varied from 11.59 ± 2.86 h per day (Easwar et al., 2018) to 12.56 ± 1.87 h per day (Cesur et al., 2020), with most children (85–87%) demonstrating regular daily CI use (Easwar et al., 2018; Friedmann et al., 2015; Marnane and Ching, 2015).
Risk factors associated with inconsistent device use include younger chronological age, presence of additional disabilities, signed language communication mode, lower levels of maternal education, lower socioeconomic status and use of state health insurance (Easwar et al., 2018). Interestingly, greater daily CI usage was a significant predictor of improved parent-reported aural/oral performance (Marnane and Ching, 2015), but the significance of maternal education, socioeconomic status, and communication mode as model predictors diminished when these additional contextual factors were considered.
Speech perception was significantly better for children with longer daily CI use, even when age and insurance status were accounted for (Wiseman et al., 2021). Speech recognition improved for children with regular daily use of their second CI compared to children without regular daily use (Kleijbergen et al., 2022; Li et al., 2023; Sparreboom et al., 2012). A one-hour increase in daily CI use was associated with a mean 2.56% increase in speech perception score (Easwar et al., 2018). Similarly, each hour of CI on-air time resulted in a 5% increase in word recognition score (Cesur et al., 2020). Relationships may be specific to usage of the second CI and age of receiving the second implant in sequential bilateral CI recipients, with second CI use, but not first CI use, significantly related to word recognition scores for the second implant alone (Forli et al., 2023).
The microsystem encompasses the most proximal elements of the individual's environment, such as family, school or neighborhood. The ecology of the microsystem is the level that has received the most attention in the studies reviewed, with contextual factors including parent-child interactions, maternal education, educational placement, and communication mode. Strong parent-child interactions were associated with better speech perception (Sininger et al., 2010). Communication mode was not significantly related to speech perception (Sparreboom et al., 2012), suggesting that access to language, whether oral or signed, may confer benefits for later speech perception.
Beyond the home environment, mainstream education placements were associated with better speech perception compared to special education placements (Sparreboom et al., 2015). Children in mainstream education attained significantly higher speech recognition scores than children in schools for the deaf (Sparreboom et al., 2015), with younger age at mainstreaming significantly associated with better indexical and linguistic speech perception (Geers et al., 2013). In addition to educational placement, two studies reported a weak effect of additional speech therapy or oral training on speech perception. The effect of speech therapy on a stimulus-repetition task only approached significance (Kleijbergen et al., 2022), and approximately 100 h of oral training was required to attain an age performance speech perception outcome 1 month older (Sininger et al., 2010). It is worth noting that speech therapy or oral training in this context includes interventions by various professionals, and the nature of these interventions can be highly variable.
Both the measurement of maternal or parental education, and speech perception or audiological outcomes, varied considerably across studies, with study-specific relationships reported. Maternal education was a significant predictor of segmental speech perception (Davidson et al., 2019), such as open set word tests in quiet/noise and speech pattern contrasts. However, this relationship was not evident across all tests of speech perception; maternal education did not predict suprasegmental speech perception, such as emotion identification and talker discrimination (Davidson et al., 2019). Furthermore, maternal education did not significantly predict speech discrimination performance (Peng et al., 2019), phoneme scoring in quiet (Kleijbergen et al., 2022), and speech perception in noise or quiet (Sparreboom et al., 2015). Maternal education was significantly associated with parent evaluations of aural/oral performance (Marnane and Ching, 2015), but auditory performance scores were not associated with maternal (le Roux et al., 2016) or parental education (Sharma et al., 2017).
The mesosystem comprises two or more interacting microsystems, such as relationships between home and clinic environments. Our systematic review did not identify any studies that examined mesosystem factors. This research gap highlights the necessity of future investigations into how interactions within immediate contexts, including family, school, and peer environments, collectively influence developmental trajectories.
The exosystem encompasses indirect environments or social systems that influence the individual, such as parental workplace or extended family. The influence of the exosystem was explored in only one study examining the wider regional context on outcomes in Denmark, where 96% of children in the East received bilateral CIs compared to 67% in the West (Percy-Smith et al., 2012). Auditory performance post-implant was comparable between East and West regions of Denmark (Percy-Smith et al., 2012), despite considerable regional differences in parent-reported self-esteem, communication mode, education placement and number implanted bilaterally.
The macrosystem is the most distal level, encompassing cultural or societal influences. Cultural, ethnicity and socioeconomic factors were explored at the macrosystem level in the reviewed studies. Poorer speech perception and auditory performance was found in minority ethnic groups in the reviewed studies (le Roux et al., 2016; Wu et al., 2015), though the effects of ethnicity were not disentangled from language spoken at home. In terms of socioeconomic status, this review found no evidence of a relationship with speech perception or auditory performance (Geers et al., 2013; Marnane and Ching, 2015; Sharma et al., 2017). However, speech perception scores of one sibling significantly predicted the second sibling's speech perception (Selleck et al., 2019), which may suggest a joint environmental influence, that could include socioeconomic status. Whilst UK cochlear implantation surgery is routinely performed via the NHS without direct cost to the recipient, healthcare is not equally or freely available in all countries. The relationship between health insurance status and speech perception was investigated in two studies. Notably, while no direct correlation between annual income and speech perception was observed in a pediatric Indian sample (Sharma et al., 2017), younger age at implantation was associated with higher socioeconomic status.
Finally, the chronosystem refers to events, changes and transitions over developmental time. Only one study was associated with chronosystem factors, specifically prematurity. Auditory performance scores for premature children were significantly lower than for children born >34 weeks' gestation, even with a minimum of 6 months implant use (le Roux et al., 2016).
To systematically identify contextual factors associated with outcomes following pediatric bilateral cochlear implantation, we sought to explore factors previously investigated in relation to speech perception or hearing outcomes in pediatric CI recipients. Additionally, we aimed to assess the predictive value of these identified contextual factors on CI outcomes, thereby elucidating the temporal and demographic contexts in which they exert significance.
Individual contextual factors significantly related to CI outcomes included non-verbal cognitive ability, social skills and CI usage. Nonetheless, these relationships were not consistently present across all measures in the identified studies and were found to change across development. Whilst this could suggest that there is a specific early developmental period where, for example, cognitive ability is a strong determinant of outcomes with additional contextual factors mediating the relationship later, the direction of influence was not systematically examined or specified. The impact of CI usage on various outcomes has received increased attention over the last two decades. Regular CI usage was associated with better speech perception and auditory outcomes. This aligns with previous findings from unilaterally implanted children (Fryauf-Bertschy et al., 1997) and from the speech production domain, where the relationship between word production and usage was related to exposure to speech in the listening environment (Glaubitz et al., 2021). However, when CI usage was modeled with additional contextual factors as predictors, this relationship was no longer significant across all studies. This emphasizes the significance of considering multiple contextual factors when assessing the impact of CIs. These contextual factors may interact to mediate irregular CI usage and subsequently influence outcomes.
Positive parent-child interactions, placement in a mainstream education setting, and auditory or oral therapy were the microsystem factors associated with better speech perception outcomes. The research demonstrating a correlation between robust parent-child interactions and enhanced speech perception (Sininger et al., 2010) aligns with findings establishing a link between increased parent-child interactions and improved language outcomes (Niparko et al., 2010). In addition, communication mode was not a significant predictor of speech perception. The disparity in outcomes may be attributed to variations in analysis and measurement techniques employed across studies. For example, while Geers et al. (2017) assessed both the quality and quantity of signed language input, the measurement of communication mode was frequently categorized as a binary or ternary variable (e.g., signed, spoken, or combination). There were also variations regarding which languages meet the criteria for signed language. Choice of communication mode may also reflect other contextual factors in the child's ecology, such as education setting or parental language.
Poorer speech perception was associated with special education placements. Placement in special education settings has similarly been associated with lower receptive vocabulary scores in bilateral CI recipients (Kleijbergen et al., 2022). Whilst studies exploring associations with educational placement were mostly prospective in design, small sample sizes limit the inferences that can be drawn. There may be further unspecified influences on the relationship between educational placement and speech perception, such as additional disabilities (Cejas et al., 2015; Cupples et al., 2018). The relationship between age at mainstreaming and speech perception could be explained by stronger speech perception skills permitting access to mainstream education or resulting from earlier access to mainstream education.
Recent reviews found that auditory verbal therapy related to better CI outcomes (Noel et al., 2023; Percy-Smith et al., 2018). However, the weak relationship between therapy and outcomes in this current review is unsurprising, given that the level of therapy or support offered routinely as part of usual care rehabilitation or through education settings varies considerably and is inconsistently reported or examined across studies. The effect of additional speech therapy or oral training may be small relative to standard rehabilitation therapy offered post-implantation. Additionally, auditory verbal training requires input from both clinicians and parents to be delivered effectively and it is not clear how this interaction within the microsystem may influence therapeutic outcomes.
Maternal education is often used as a proxy for socioeconomic status or familial resources (Hoff, 2003; Jackson et al., 2017). Nonetheless, while highest maternal education level was often reported descriptively, relatively few studies explored its relationship with functional outcomes. The lack of a relationship between CI outcomes and maternal education in most studies reviewed contrasts with findings indicating that maternal education significantly predicted language outcomes at 72 months post-implantation in Norwegian children with bilateral implants (Wie et al., 2020). However, maternal education may be a mediator whose effects on outcomes only become apparent in later development; for example, maternal education was not a significant predictor of language outcomes measured at 48 months post-implant (Wie et al., 2020). Whilst we have situated maternal education in the microsystem, it also exerts an influence on academic outcomes in hearing children (Harding et al., 2015), and there are multiple levels of Bronfenbrenner's framework at which maternal education could moderate or mediate CI outcomes.
No studies exploring contextual factors at the mesosystem level were identified in this review. This could include elements of clinician and educator support to foster a supportive environment for deaf children (Clark et al., 2019), and could indirectly influence CI outcomes. For example, differences in how clinicians interact with, or support, families could mediate later implantation ages for certain children. The family environment may also be shaped by parental self-efficacy and input from early interventionists (Davenport and Holt, 2019; Davenport et al., 2021; Roberts, 2018). Unlike hearing history, which cannot be changed, the family environment offers a unique opportunity for intervention outside of the clinic. For example, parents can be supported with strategies to enrich the home linguistic environment through leveraging parental self-efficacy to intervene, improving CI outcomes (Holt et al., 2020).
One study explored exosystem factors (Percy-Smith et al., 2012), in which regional differences were not significantly associated with auditory outcomes. It is plausible that multiple interacting factors in the microsystem may independently exert an effect but cumulatively cancel each other out. For example, more children in West than East Denmark received therapeutic support in the study. Whether auditory performance is comparable in the East and West because of the additional support received as a Western standard or because generally poorer attainment by Western children necessitated additional interventions is unclear. However, it should be noted that receptive vocabulary and language outcomes were significantly better in East than West Denmark (Percy-Smith et al., 2012), suggesting that relationships between contextual factors are outcome specific, and that exosystem factors may exert greater influence on more distal language outcomes than auditory performance. The paucity of research investigating these factors precludes the formulation of robust conclusions.
Ethnicity was the only macrosystem factor significantly associated with speech perception outcomes. Considering the reported heterogeneity among and within ethnic groups and the lack of focus on intersection with other factors such as socioeconomic status, it is difficult to draw conclusions about demographics per se. Mechanisms of action which could underlie this relationship include differences in culture shaping the linguistic home environment (Masek et al., 2021), bilingualism in the home environment (Dean et al., 2013; Glaubitz et al., 2021), and parental ethnicity (Wu et al., 2015). In a study of children with CIs and Auditory Neuropathy Spectrum Disorder excluded from this review, 10% of children with good speech perception had bilingual home environments, whereas >70% of children with poor speech perception had bilingual home environments (Dean et al., 2013). This could suggest that children with CIs in a bilingual home environment may be at greater risk of poor speech perception, although the sample size did not permit inferential statistical analyses.
Similar findings have been reported in a small study exploring language outcomes in bilingual children (two spoken languages, rather than a spoken and a signed language). Bilingual bilaterally implanted children also performed significantly worse than monolingual bilaterally implanted children in a composite German language measure (Glaubitz et al., 2021). Bilingualism was related to migration backgrounds for eight children in the bilingual group (Glaubitz et al., 2021). As these studies do not comment on the duration, quality or quantity of the language input that the children received in the language of testing, the nature of the relationship between bilingualism and speech perception requires further examination of effect strength, significance, and direction before conclusions can be drawn. Later age at implantation could also be one mechanism through which ethnicity influences CI outcomes. In a retrospective review of Norwegian children excluded from the current review, those with non-Nordic parents were implanted significantly later than children with Nordic parents (Amundsen et al., 2017). Overall, these findings underscore the need for more comprehensive, intersectional studies to clarify how ethnicity interacts with cultural and socioeconomic factors to shape speech perception outcomes.
There were also methodological limitations to testing in an additional language that need addressing. For example, one study in the United States reported that speech perception was significantly poorer for the test group where 58% of the participants were Hispanic, 17% were Caucasian, 17% were multi-ethnicity and 8% were Russian, compared to a control group where 71% of participants were White (Wu et al., 2015). In the test group (N = 12), four children did not speak English, five spoke English as a second language, and seven were bilingual. As all testing was conducted in English, these children would have been disadvantaged and group differences may have been exaggerated, limiting the conclusions that can be drawn.
There was no evidence of socioeconomic status directly influencing speech perception outcomes, although it may exert indirect effects in cases where CIs must be paid for, or through the home and social environment, as evidenced by the significant relationship between sibling's speech perception performance (Selleck et al., 2019). Beyond the reviewed speech perception and hearing outcomes, poorer language outcomes have also been associated with lower household incomes (Niparko et al., 2010). Type of healthcare insurance held was also the only significant predictor of receptive language outcomes for an American pediatric sample (Eskridge et al., 2021). In summary, while socioeconomic status does not appear to directly impact on speech perception outcomes, its indirect influence on language development and access to quality healthcare highlights the critical role of financial and social resources in pediatric auditory and language performance.
With respect to the chronosystem, the finding linking prematurity to poorer auditory performance is consistent with poorer neurodevelopmental outcomes across sensory modalities for premature children (Jarjour, 2015). This finding likely interacts with other levels of Bronfenbrenner's framework such as the microsystem, as non-oral communication mode and placement in non-mainstream education settings was also more likely with NICU admittance (le Roux et al., 2016). The role of social and cultural expectations in chronosystem factors is not fully understood; how individuals respond to life events and transitions is likely to depend on support from the wider ecological system. For example, prematurity may lead to developmental delays that can influence the support which a child is given or how they interact with the environment. Further research is required to understand how factors, such as prematurity, interact with the wider ecology to exert their influence on outcomes such as speech perception, sound localization and auditory performance for children and young people receiving bilateral CIs.
In this scoping review, we demonstrated that Bronfenbrenner's framework can be effectively used to conceptualize the individual CI recipient in their ecology. We have also highlighted the lack of research examining the relationships between an individual's outcomes and their context, leaving many questions unanswered about how, why and when contextual factors influence the benefit conferred by CIs for each individual. There has been insufficient consideration of the proximal or distal factors that influence development during various stages. The lack of follow-up in some retrospective reviews or prospective studies further exacerbates this issue.
The studies included in this review employed retrospective and prospective designs, including case-control and matched-case control methods. Retrospective studies or chart reviews are commonly employed in healthcare settings and entail the analysis of data primarily collected for clinical purposes rather than research objectives (Hess, 2004). These studies can serve as a means to refine the scope for future prospective investigations (Vassar and Holzmann, 2013), but they are frequently used in place of prospective studies in the field of cochlear implantation research. Thirteen of the 23 studies within this review utilized only retrospective chart reviews, without additional prospective measures. Whilst many of the studies pooled samples across cohorts and clinics, retrospective studies are inherently limited by their design, relying upon the use of medical information that has already been collected for a particular sample (Talari and Goyal, 2020; Vassar and Holzmann, 2013). Thus, these data might not be the most appropriate for examining the factors of interest and might not have been consistently collected across the sample. For example, Easwar et al. (2018) report that five different tests were used to measure speech perception across their sample, making it difficult to assess comparability. The assessment of speech perception and hearing outcomes may also be limited to functional listening in early infancy, with the risk that results cannot be disentangled from language acquisition. The risk of bias also increases with retrospective data, as information regarding clinician gatekeeping or additional variables that may have influenced CI outcomes may not have been recorded. Furthermore, not all studies explicitly describe exclusion and inclusion criteria or attrition from their studies. Additionally, few studies reported power calculations to determine the sample size required, which renders interpretation of the findings challenging, particularly with small sample sizes and in the absence of specific hypotheses and research questions.
The lack of longitudinal data to understand the distal effects of early contextual factor influences is a key limitation across the reviewed studies. Baseline measurements of contextual factors may not accurately reflect the contextual factor at the time of outcome measurement. This is acknowledged to some extent in studies examining the age of entering mainstream education, rather than just the type of education that a child receives at the time of outcome measurement. Although follow-up periods are conducted in numerous studies, the relationships between contextual factors are dynamic, and contextual factors can exert influence at various developmental stages. For example, Wie et al. (2020) emphasize the importance of long-term follow-ups of language outcomes. At a 4-year follow-up, age at implantation was a reliable predictor of language outcomes. However, children with CIs exhibited a relative decline in receptive vocabulary and expressive grammar at a 6-year follow-up compared to their hearing peers. This suggests a non-linear progression of development across language domains. Furthermore, bidirectional effects (where variables influence each other over time) are also rarely investigated but would be crucial to evaluate in relation to development.
Instead of treating contextual factors as variables to be controlled for, researchers must incorporate these factors into study designs to enhance the generalizability and validity of their research. Furthermore, comprehending the interaction between these variables can aid in establishing the mechanisms underlying the success of implants in improving speech perception and audiological outcomes. Studies employing longitudinal prospective designs with rolling enrolment would facilitate a more comprehensive understanding of the influence of each factor across development. For instance, to elucidate the impact of age at implantation on CI outcomes, researchers should examine the factors in a child's environment that make receiving a CI at a later age distinct from receiving one during an earlier developmental phase. Additionally, analyses of longitudinal prospective data would circumvent the current reliance on correlational methods, which lack the capability to analyse directionality or causality.
Whilst retrospective designs may be a pragmatic option when cost and clinician time are prohibitively high, the absence of randomized controlled trials and experimental studies to examine the influence of contextual factors is noteworthy. Randomized controlled trials have less bias than observational designs as differences in outcome can be attributed to the intervention if other variables are randomly distributed between comparison groups. However, whilst randomization ensures baseline characteristics are equally split between groups, contextual factors such as ethnicity cannot be practically manipulated and randomization itself does not preclude other sources of error, such as contextual factors that are not measured. Sullivan (2011) recommends cohort, case-control and matched designs instead. However, not all studies included in this review even included a control group, which precludes valid conclusions. Beyond quantitative studies, qualitative methods have also been successfully used to explore the perspective of the pediatric CI recipient, their parents and teachers with respect to hearing quality of life (Mather et al., 2013a,b). Qualitative research could help identify contextual factors that children, parents and teachers view as influencing their outcomes, especially in combination with quantitative data (i.e., a mixed methods approach).
Homogeneous outcomes should not be expected for CI recipients. The bilateral CI domain is dynamic, with evolving age and suitability criteria, and technological advancements that enhance sound access in noisy environments and optimize bilateral signal balance, all of which could impact reported outcomes. However, it is argued that assessment of the developmental context of CI candidates is necessary to ensure that each child has the requisite ecological support to achieve appropriate outcomes. The lack of research focusing on the mesosystem is a cause for concern. For instance, research has not examined the influence of a clinician's description of anticipated CI outcomes on a parent's decision regarding CI surgery or how a clinician's reference to infant-directed speech impacts the family dynamics. Whilst the clinic and clinician as contextual factors have received less attention, healthcare factors such as workplace culture and awareness can be measured in implementation research (Finch et al., 2024). By pooling data across multiple sites, the power to detect effects and generalize findings can be enhanced. It would be beneficial to investigate the influence of healthcare setting context, clinician's interest and attention, and rehabilitation methods or advice provided on CI outcomes. Although directly evaluating these healthcare settings as contextual factors may be challenging, it is crucial to do so to establish an evidence-based framework for intervening in the child's environment and ensuring the provision of adequate support.
Adopting Bronfenbrenner's bioecological theory presents challenges in understanding human development, due to the interconnections across various environmental layers, from immediate interactions to broader societal forces. This complexity necessitates sophisticated, multi-method research designs, such as hierarchical linear modeling and mixed-method approaches, to comprehensively capture both quantitative trends and qualitative nuances over times. Variations in cultural context and developmental stages further complicate these interactions, making it a challenging yet crucial endeavor to fully comprehend human development. Our review highlights the urgent need to delve into the interactions between developmental factors, which is currently lacking in existing research.
In conclusion, this scoping review aimed to identify the developmental contextual factors that significantly influence speech perception and hearing outcomes following pediatric bilateral cochlear implantation. While age at implantation and inter-implant interval have been previously examined, we identified proximal and distal contextual factors associated with CI outcomes. These factors were conceptualized using Bronfenbrenner's bioecological framework, which has demonstrated its utility in evaluating external influences and exploring the interplay of interacting factors to enhance support and outcomes after pediatric cochlear implantation. Although this review employed a narrative synthesis approach due to the heterogeneity of study designs and factors, prospective research should investigate the critical developmental windows within which contextual factors interact. The benefits of CIs are contingent upon multiple contextual factors that should be comprehensively analyzed rather than being selectively removed from prospective, longitudinal designs. This approach will facilitate the development of targeted interventions at various levels of the bioecological system, ultimately improving outcomes for pediatric bilateral CI recipients. Embedding this framework into clinical and research design for children with bilateral CI involves comprehensive evaluations that assess implant performance alongside the child's broader developmental context—including family dynamics, educational support, and community resources—while employing multi-level, longitudinal studies to capture the interplay between biological factors, implant efficacy, and psychosocial influences.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
FC: Conceptualization, Investigation, Project administration, Writing – original draft. NVZ: Conceptualization, Validation, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research (PGfAR) (NIHR201608). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
We thank Merle Mahon, Frances Early, Ruth Nightingale, Deborah Vickers and Dan Jiang for thoughtful comments. The content of this manuscript has been published as a PsyArXiv preprint: https://doi.org/10.31234/osf.io/vwtnc_v2.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Amundsen, V. V., Wie, O. B., Myhrum, M., and Bunne, M. (2017). The impact of ethnicity on cochlear implantation in Norwegian children. Int. J. Pediatr. Otorhinolaryngol. 93, 30–36. doi: 10.1016/j.ijporl.2016.12.002
Anderson, K. L. (2004). Auditory skills checklist. Available online at: https://successforkidswithhearingloss.com/wp-content/uploads/2011/12/Auditory-Skills-Checklist.doc (accessed July 25)
Archbold, S., Lutman, M. E., and Nikolopoulos, T. (1998). Categories of auditory performance: inter-user reliability. Br. J. Audiol. 32, 7–12. doi: 10.3109/03005364000000045
Aschendorff, A., Kromeier, J., Klenzer, T., and Laszig, R. (2007). Quality control after insertion of the nucleus contour and contour advance electrode in adults. Ear Hear. 28, 75S−79S. doi: 10.1097/AUD.0b013e318031542e
Barker, D. H., Quittner, A. L., Fink, N. E., Eisenberg, L. S., Tobey, E. A., Niparko, J. K., et al. (2009). Predicting behavior problems in deaf and hearing children: the influences of language, attention, and parent-child communication. Dev. Psychopathol. 21, 373–392. doi: 10.1017/S0954579409000212
Bench, J., and Bamford, J. (2002). Speech-Hearing Tests & the Spoken Language of Hearing-Impaired Children. London: Academic Press.
Boons, T., Brokx, J. P. L., Dhooge, I., Frijns, J. H. M., Peeraer, L., Vermeulen, A., et al. (2012). Predictors of spoken language development following paediatric cochlear implantation. Ear Hear. 33, 617–639. doi: 10.1097/AUD.0b013e3182503e47
Boothroyd, A., Eisenberg, L. S., and Martinez, A. S. (2010). An on-line imitative test of speech-pattern contrast perception (OlimSpac): developmental effects in normally hearing children. J. Speech Lang. Hear. Res. 53, 531–542. doi: 10.1044/1092-4388(2009/08-0260)
Bosman, A. J., and Smoorenburg, G. F. (1995). Intelligibility of Dutch CVC syllables and sentences for listeners with normal hearing and with three types of hearing impairment. Audiology 34, 260–284. doi: 10.3109/00206099509071918
Bradlow, A. R., Torretta, G. M., and Pisoni, D. B. (1996). Intelligibility of normal speech I: Global and fine-grained acoustic-phonetic talker characteristics. Speech Commun. 20, 255–272. doi: 10.1016/S0167-6393(96)00063-5
Bronfenbrenner, U. (1977). Toward an experimental ecology of human development. Am. Psychol. 32, 513–531. doi: 10.1037/0003-066X.32.7.513
Bronfenbrenner, U., and Evans, G. W. (2000). Developmental science in the 21st century: emerging questions, theoretical models, research designs and empirical findings. Soc. Dev. 9, 115–125. doi: 10.1111/1467-9507.00114
Bronfenbrenner, U., and Morris, P. A. (2006). “Handbook of child psychology,” in The Bioecological Model of Human Development, Theoretical models of Human Development Vol. 1 (Hoboken, NJ: John Wiley & Sons Inc), 793–828. doi: 10.1002/9780470147658.chpsy0114
Cejas, I., Barker, D. H., Petruzzello, E., Sarangoulis, C. M., and Quittner, A. L. (2023). Cochlear implantation and educational and quality-of-life outcomes in adolescence. JAMA Otolaryngol. Head Neck Surg. 149, 708–715. doi: 10.1001/jamaoto.2023.1327
Cejas, I., Hoffman, M. F., and Quittner, A. L. (2015). Outcomes and benefits of pediatric cochlear implantation in children with additional disabilities: a review and report of family influences on outcomes. Pediatric. Health Med. Ther. 6, 45–63. doi: 10.2147/PHMT.S65797
Cesur, S., Yuksel, M., and Ciprut, A. (2020). Data logging variables and speech perception in prelingually deafened pediatric cochlear implant users. Int. J. Pediatr. Otorhinolaryngol. 133:110003. doi: 10.1016/j.ijporl.2020.110003
Clark, M. D., Baker, S., and Simms, L. (2019). A culture of assessment: a bioecological systems approach for early and continuous assessment of deaf infants and children. Psychol. Sch. 57, 443–458. doi: 10.1002/pits.22313
Coene, M., and Govaerts, P. J. (2014). The development of oral language in children with bilateral hearing loss: from speech perception to morphosyntax. Lingua 139, 1–9. doi: 10.1016/j.lingua.2013.12.005
CRIDE (2023). CRIDE 2023 UK-wide summary: Education provision for deaf children in 2022/23. Available online at: https://www.ndcs.org.uk/media/9505/cride-2023-uk-wide-summary-final.pdf (accessed October 31, 2024).
Cupples, L., Ching, T. Y. C., Button, L., Leigh, G., Marnane, V., Whitfield, J., et al. (2018). Language and speech outcomes of children with hearing loss and additional disabilities: identifying the variables that influence performance at five years of age. Int. J. Audiol. 57, S93–S104. doi: 10.1080/14992027.2016.1228127
Davenport, B. C. A., and Holt, R. F. (2019). Influence of family environment on developmental outcomes in children with cochlear implants: a matched case study. Volta Rev. 119, 29–55. doi: 10.17955/tvr.119.1.808
Davenport, C. A., Houston, D. M., Bowdrie, K., and Holt, R. F. (2021). The role of early intervention in parental self-efficacy for families of children who are deaf or hard-of-hearing. J. Early Hear. Detect. Intervent. 6, 38–37.
Davidson, L. S., Geers, A. E., Uchanski, R. M., and Firszt, J. B. (2019). Effects of early acoustic hearing on speech perception and language for pediatric cochlear implant recipients. J. Speech Lang. Hear Res. 62, 3620–3637. doi: 10.1044/2019_JSLHR-H-18-0255
De Raeve, L., Vermeulen, A., and Snik, A. (2015). Verbal cognition in deaf children using cochlear implants: effect of unilateral and bilateral stimulation. Audiol. Neurootol. 20, 261–266. doi: 10.1159/000381003
Dean, C., Felder, G., and Kim, A. H. (2013). Analysis of speech perception outcomes among patients recieving cochlear implants with auditory neuropathy spectrum disorder. Otol. Neurol. 34, 1610–1614. doi: 10.1097/MAO.0b013e318299a950
Deep, N. L., Dowling, E. M., Jethanamest, D., and Carlson, M. L. (2019). Cochlear implantation: an overview. J. Neurol. Surg. B Skull Base 80, 169–177. doi: 10.1055/s-0038-1669411
Dettman, S. J., Dowell, R. C., Choo, D., Arnott, W., Abrahams, Y., Davis, A., et al. (2016). Long-term communication outcomes for children receiving cochlear implants younger than 12 months: a multicenter study. Otol. Neurotol. 37, e82–95. doi: 10.1097/MAO.0000000000000915
Dettman, S. J., Fiket, H., Dowell, R. C., Charlton, M., Williams, S. S., Tomov, A. M., et al. (2004). Speech perception results for children using cochlear implants who have additional special needs. Volta Rev. 104, 361–392.
Dillon, C. M., Burkholder, R. A., Cleary, M., and Pisoni, D. B. (2004). Nonword repetition by children with cochlear implants: accuracy ratings from normal-hearing listeners. J. Speech Lang. Hear. Res. 47, 1103–1116. doi: 10.1044/1092-4388(2004/082)
Driver, S., and Jiang, D. (2017). Paediatric cochlear implantation factors that affect outcomes. Eur. J. Paediatr. Neurol. 21, 104–108. doi: 10.1016/j.ejpn.2016.07.012
Easwar, V., Sanfilippo, J., Papsin, B., and Gordon, K. (2018). Impact of consistency in daily device use on speech perception abilities in children with cochlear implants: datalogging evidence. J. Am. Acad. Audiol. 29, 835–846. doi: 10.3766/jaaa.17051
Eisenberg, L. S., and Dirks, D. D. (1995). Reliability and sensitivity of paired comparisons and category rating in children. J. Speech Hear. Res. 38, 1157–1167. doi: 10.1044/jshr.3805.1157
Eisenberg, L. S., Johnson, K. C., Martinez, A. S., Cokely, C. G., Tobey, E. A., Quittner, A. L., et al. (2006). Speech recognition at 1-year follow-up in the childhood development after cochlear implantation study: Methods and preliminary findings. Audiol. Neuro-otol. 11, 259–268. doi: 10.1159/000093302
Eskridge, H. R., Park, L. R., and Brown, K. D. (2021). The impact of unilateral, simultaneous, or sequential cochlear implantation on pediatric language outcomes. Cochlear Implants Int. 22, 187–194. doi: 10.1080/14670100.2020.1871267
Finch, T. L., Bührmann, L., Potthoff, S., May, C. R., Gibson, B., Gumancik, J., et al. (2024). Systematic review of applications and properties of the NoMAD instrument for assessing implementation outcomes: study protocol. NIHR Open Res. 4:21. doi: 10.3310/nihropenres.13559.1
Forli, F., Bruschini, L., Franciosi, B., Berrettini, S., and Lazzerini, F. (2023). Sequential bilateral cochlear implant: long-term speech perception results in children first implanted at an early age. Eur. Arch. Otorhinol. 280, 1073–1080. doi: 10.1007/s00405-022-07568-4
Fortnum, H., and Davis, A. (1997). Epidemiology of permanent childhood hearing impairment in trent region, 1985–1993. Br. J. Audiol. 31, 409–446. doi: 10.3109/03005364000000037
Friedmann, D. R., Green, J., Fang, Y., Ensor, K., Roland, J. T., and Waltzman, S. B. (2015). Sequential bilateral cochlear implantation in the adolescent population. Laryngoscope 125, 1952–1958. doi: 10.1002/lary.25293
Fryauf-Bertschy, H., Tyler, R. S., Kelsay, D. M., Gantz, B. J., and Woodworth, G. G. (1997). Cochlear implant use by prelingually deafened children: the influences of age at implant and length of device use. J. Speech Lang. Hear. Res. 40, 183–199. doi: 10.1044/jslhr.4001.183
Galvin, K. L., Mok, M., and Dowell, R. C. (2007). Perceptual benefit and functional outcomes for children using sequential bilateral cochlear implants. Ear Hear. 28, 470–482. doi: 10.1097/AUD.0b013e31806dc194
Gathercole, S. E., and Baddeley, A. D. (1996). The Children's Test of Non-Word Repetition. London, Psychological Corporation.
Geers, A. E. (2002). Factors affecting the development of speech, language, and literacy in children with early cochlear implantation. Lang. Speech Hear. Ser. Sch. 33, 172–183. doi: 10.1044/0161-1461(2002/015)
Geers, A. E., Davidson, L. S., Uchanski, R. M., and Nicholas, J. G. (2013). Interdependence of linguistic and indexical speech perception skills in school-age children with early cochlear implantation. Ear Hear. 34, 562–574. doi: 10.1097/AUD.0b013e31828d2bd6
Geers, A. E., Mitchell, C. M., Warner-Czyz, A., Wang, N. Y., Eisenberg, L. S., and Team, C. D. I. (2017). Early sign language exposure and cochlear implantation benefits. Pediatrics, 140:e20163489. doi: 10.1542/peds.2016-3489
Geers, A. E., and Nicholas, J. G. (2013). Enduring advantages of early cochlear implantation for spoken language development. J. Speech Lang. Hear. Res. 56, 643–655. doi: 10.1044/1092-4388(2012/11-0347)
Glaubitz, C., Liebscher, T., and Hoppe, U. (2021). Age-related language performance and device use in children with very early bilateral cochlear implantation. Int. J. Pediatr. Otorhinolaryngol. 147:110780. doi: 10.1016/j.ijporl.2021.110780
Goodman, D., Ogrinc, G., Davies, L., Baker, G. R., Barnsteiner, J., Foster, T. C., et al. (2016). Explanation and elaboration of the SQUIRE (Standards for Quality Improvement Reporting Excellence) Guidelines, V.2.0: examples of SQUIRE elements in the healthcare improvement literature. BMJ Qual. Saf. 25:e7. doi: 10.1136/bmjqs-2015-004480
Gresham, F. M., and Elliott, S. N. (1990). The Social Skills Rating System. Circle Pines, MN: American Guidance Service. doi: 10.1037/t10269-000
Harding, J., and Morris, P. A.. (2015). The relationship between maternal education and children's academic outcomes: A theoretical framework. J. Marriage Fam. 77, 60–76. doi: 10.1111/jomf.12156
Harrison, R., Jones, B., Gardner, P., and Lawton, R. (2021). Quality assessment with diverse studies (QuADS): an appraisal tool for methodological and reporting quality in systematic reviews of mixed- or multi-method studies. BMC Health Serv. Res. 21:144. doi: 10.1186/s12913-021-06122-y
Hoff, E. (2003). The specificity of environmental influence: socioeconomic status affects early vocabulary development via maternal speech. Child. Dev. 74, 1368–1378. doi: 10.1111/1467-8624.00612
Hoffman, M. F., Quittner, A. L., and Cejas, I. (2015). Comparisons of social competence in young children with and without hearing loss: a dynamic systems framework. J. Deaf. Stud. Deaf. Educ. 20, 115–124. doi: 10.1093/deafed/enu040
Holt, R. F., Beer, J., Kronenberger, W. G., Pisoni, D. B., Lalonde, K., and Mulinaro, L. (2020). Family environment in children with hearing aids and cochlear implants: associations with spoken language, psychosocial functioning, and cognitive development. Ear. Hear. 41, 762–774. doi: 10.1097/AUD.0000000000000811
Holzinger, D., Dall, M., Sanduvete-Chaves, S., Saldana, D., Chacon-Moscoso, S., and Fellinger, J. (2020). The impact of family environment on language development of children with cochlear implants: a systematic review and meta-analysis. Ear. Hear. 41, 1077–1091. doi: 10.1097/AUD.0000000000000852
Jackson, M., Kiernan, K., and McLanahan, S. (2017). Maternal education, changing family circumstances, and children's skill development in the United States and UK. Ann. Am. Acad. Pol. Soc. Sci. 674, 59–84. doi: 10.1177/0002716217729471
Jarjour, I. T. (2015). Neurodevelopmental outcome after extreme prematurity: a review of the literature. Pediatr. Neurol. 52, 143–152. doi: 10.1016/j.pediatrneurol.2014.10.027
Kennedy, C. R., McCann, D. C., Campbell, M. J., Law, C. M., Mullee, M., Petrou, S., et al. (2006). Language ability after early detection of permanent childhood hearing impairment. N. Engl. J. Med. 354, 2131–2141. doi: 10.1056/NEJMoa054915
Killion, M. C., Niquette, P. A., Gudmundsen, G. I., Revit, L. J., and Banerjee, S. (2004). Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J. Acoust. Soc. Am. 116, 2395–2405. doi: 10.1121/1.1784440
Kirk, K. I., Pisoni, D. B., and Osberger, M. J. (1995). Lexical effects on spoken word recognition by pediatric cochlear implant users. Ear Hear. 16, 470–481. doi: 10.1097/00003446-199510000-00004
Kleijbergen, W. J., Sparreboom, M., Mylanus, E. A. M., de Koning, G., Helleman, H. W., Boermans, P., et al. (2022). Benefit of sequential bilateral cochlear implantation in children between 5 to 18 years old: A prospective cohort study. PLoS One 17:e0271497. doi: 10.1371/journal.pone.0271497
Kollmeier, B., Warzybok, A., Hochmuth, S., Zokoll, M. A., Uslar, V., Brand, T., et al. (2015). The multilingual matrix test: principles, applications, and comparison across languages: a review. Int. J. Audiol. 54, 3–16. doi: 10.3109/14992027.2015.1020971
Kral, A., and Sharma, A. (2012). Developmental neuroplasticity after cochlear implantation. Trends Neurosci. 35, 111–122. doi: 10.1016/j.tins.2011.09.004
le Roux, T., Vinck, B., Butler, I., Cass, N., Louw, L., Nauta, L., Schlesinger, D., Soer, M., Tshifularo, M., and Swanepoel de, W. (2016). Predictors of pediatric cochlear implantation outcomes in South Africa. Int. J. Pediatr. Otorhinolaryngol. 84, 61–70. doi: 10.1016/j.ijporl.2016.02.025
Li, Y. L., Chen, C. S., Yang, H. M., Chen, H. C., and Wu, J. L. (2023). Performance of sequentially bilateral cochlear implanted children who speak Mandarin. Audiol. Neurootol. 28, 106–115. doi: 10.1159/000526695
Litovsky, R. Y., and Gordon, K. (2016). Bilateral cochlear implants in children: effects of auditory experience and deprivation on auditory perception. Hear Res. 338, 76–87. doi: 10.1016/j.heares.2016.01.003
Lovett, R. E., Kitterick, P. T., Hewitt, C. E., and Summerfield, A. Q. (2010). Bilateral or unilateral cochlear implantation for deaf children: an observational study. Arch. Dis. Child. 95, 107–112. doi: 10.1136/adc.2009.160325
Lovett, R. E. S., Vickers, D. A., and Summerfield, A. Q. (2015). Bilateral cochlear implantation for hearing-impaired children: criterion of candidacy derived from an observational study. Ear Hear. 36, 14–23. doi: 10.1097/AUD.0000000000000087
Macherey, O., and Carlyon, R. P. (2014). Cochlear implants. Curr. Biol. 24, R878–R884. doi: 10.1016/j.cub.2014.06.053
Marnane, V., and Ching, T. Y. (2015). Hearing aid and cochlear implant use in children with hearing loss at three years of age: Predictors of use and predictors of changes in use. Int. J. Audiol. 54, 544–551. doi: 10.3109/14992027.2015.1017660
Masek, L. R., Ramirez, A. G., McMillan, B. T. M., Hirsh-Pasek, K., and Golinkoff, R. M. (2021). Beyond counting words: a paradigm shift for the study of language acquisition. Child Dev. Perspect. 15, 274–280. doi: 10.1111/cdep.12425
Mather, J., Archbold, S., and Gregory, S. (2013a). Deaf young people with sequential bilateral cochlear implants: the experience of parents and teachers. Deaf. Educ. In. 13, 173–198. doi: 10.1179/1557069X11Y.0000000009
Mather, J., Gregory, S., and Archbold, S. (2013b). The experiences of deaf young people with sequential bilateral cochlear implants. Deaf. Educ. Int. 13, 152–172. doi: 10.1179/1557069X11Y.0000000008
McSweeny, C., Cushing, S. L., Campos, J. L., Papsin, B. C., and Gordon, K. A. (2021). Functional consequences of poor binaural hearing in development: evidence from children with unilateral hearing loss and children receiving bilateral cochlear implants. Trends Hear. 25, 1–17. doi: 10.1177/23312165211051215
Moog, J. S., and Geers, A. E. (2010). Early educational placement and later language outcomes for children with cochlear implants. Otol. Neurol. 31, 1315–1319. doi: 10.1097/MAO.0b013e3181eb3226
NICE. (2009). Cochlear implants for children and adults with severe to profound deafness. Technology appraisal guidance TA166. NICE. Available online at: https://www.nice.org.uk/guidance/ta166 (accessed October 31, 2024).
Nikolopoulos, T. P., Lloyd, H., Archbold, S., and O'Donoghue, G. M. (2001). Pediatric cochlear implantation: the parents' perspective. Arch. Otolaryngol. Head Neck Surg. 127, 363–367. doi: 10.1001/archotol.127.4.363
Niparko, J. K., Tobey, E. A., Thal, D. J., Eisenberg, L. S., Wang, N. Y., Quittner, A. L., et al. (2010). Spoken language development in children following cochlear implantation. JAMA 303, 1498–1506. doi: 10.1001/jama.2010.451
Noel, A., Manikandan, M., and Kumar, P. (2023). Efficacy of auditory verbal therapy in children with cochlear implantation based on auditory performance - a systematic review. Cochlear Implants Int. 24, 43–53. doi: 10.1080/14670100.2022.2141418
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. doi: 10.1136/bmj.n71
Peng, Z. E., Hess, C., Saffran, J. R., Edwards, J. R., and Litovsky, R. Y. (2019). Assessing fine-grained speech discrimination in young children with bilateral cochlear implants. Otol. Neurotol. 40, e191–e197. doi: 10.1097/MAO.0000000000002115
Percy-Smith, L., Busch, G. W., Sandahl, M., Nissen, L., Josvassen, J. L., Bille, M., et al. (2012). Significant regional differences in Denmark in outcome after cochlear implants in children. Danish Med. J. 59:A4435.
Percy-Smith, L., Tønning, T. L., Josvassen, J. L., Mikkelsen, J. H., Nissen, L., Dieleman, E., et al. (2018). Auditory verbal habilitation is associated with improved outcome for children with cochlear implant. Cochlear Implants Int. 19, 38–45. doi: 10.1080/14670100.2017.1389020
Persic, D., Thomas, M. E., Pelekanos, V., Ryugo, D. K., Takesian, A. E., Krumbholz, K., et al. (2020). Regulation of auditory plasticity during critical periods and following hearing loss. Hear. Res. 397:107976. doi: 10.1016/j.heares.2020.107976
Peterson, G. E., and Lehiste, I. (1962). Revised CNC lists for auditory tests. J. Speech Hear. Disord. 27, 62–70. doi: 10.1044/jshd.2701.62
Pisoni, D. B., Kronenberger, W. G., Harris, M. S., and Moberly, A. C. (2017). Three challenges for future research on cochlear implants. World J. Otorhinolaryngol. Head Neck. Surg. 3, 240–254. doi: 10.1016/j.wjorl.2017.12.010
Robbins, A. M., Renshaw, J. J., and Berry, S. W. (1991). Evaluating meaningful auditory integration in profoundly hearing-impaired children. Am. J. Otol. 12, 144–150.
Roberts, M. Y. (2018). Parent-implemented communication treatment for infants and toddlers with hearing loss: a randomized pilot trial. J. Speech Lang. Hear. Res. 35, 1–10. doi: 10.1044/2018_JSLHR-L-18-0079
Ronner, E. A., Benchetrit, L., Levesque, P., Basonbul, R. A., and Cohen, M. S. (2020). Quality of life in children with sensorineural hearing loss. Otolaryngol. Head Neck. Surg. 162, 129–136. doi: 10.1177/0194599819886122
Rosa, E. M., and Tudge, J. (2013). Urie bronfenbrenner's theory of human development: its evolution from ecology to bioecology. J. Fam. Theory Rev. 5, 243–258. doi: 10.1111/jftr.12022
Ruben, R. J. (2018). Language development in the pediatric cochlear implant patient. Laryngosc. Investig. Otolaryngol. 3, 209–213. doi: 10.1002/lio2.156
Scherf, F. W., van Deun, L., van Wieringen, A., Wouters, J., Desloovere, C., Dhooge, I., et al. (2009). Functional outcome of sequential bilateral cochlear implantation in young children: 36 months postoperative results. Int. J. Pediatr. Otorhinolaryngol. 73, 723–730. doi: 10.1016/j.ijporl.2009.01.009
Selleck, A. M., Park, L. R., and Brown, K. D. (2019). Factors influencing pediatric cochlear implant outcomes: carolina sibling study. Otol. Neurotol. 40, 1148–1152. doi: 10.1097/MAO.0000000000002342
Sharma, A., Dorman, M. F., and Kral, A. (2005). The influence of a sensitive period on central auditory development in children with unilateral and bilateral cochlear implants. Hear. Res. 203, 134–143. doi: 10.1016/j.heares.2004.12.010
Sharma, A., Dorman, M. F., and Spahr, A. J. (2002). A sensitive period for the development of the central auditory system in children with cochlear implants: implications for age of implantation. Ear Hear. 23, 532–539. doi: 10.1097/01.AUD.0000042223.62381.01
Sharma, S., Bhatia, K., Singh, S., Lahiri, A. K., and Aggarwal, A. (2017). Impact of socioeconomic factors on paediatric cochlear implant outcomes. Int. J. Pediatr. Otorhinolaryngol. 102, 90–97. doi: 10.1016/j.ijporl.2017.09.010
Sharma, S. D., Cushing, S. L., Papsin, B. C., and Gordon, K. A. (2020). Hearing and speech benefits of cochlear implantation in children: a review of the literature. Int. J. Pediatr. Otorhinolaryngol. 133:109984. doi: 10.1016/j.ijporl.2020.109984
Silva, J. M., Yamada, M. O., Guedes, E. G., and Moret, A. L. M. (2020). Factors influencing the quality of life of children with cochlear implants. Braz. J. Otorhinolaryngol. 86, 411–418. doi: 10.1016/j.bjorl.2019.01.004
Sininger, Y. S., Grimes, A., and Christensen, E. (2010). Auditory development in early amplified children: factors influencing auditory-based communication outcomes in children with hearing loss. Ear Hear. 31, 166–185. doi: 10.1097/AUD.0b013e3181c8e7b6
Sparreboom, M., Langereis, M. C., Snik, A. F., and Mylanus, E. A. (2015). Long-term outcomes on spatial hearing, speech recognition and receptive vocabulary after sequential bilateral cochlear implantation in children. Res. Dev. Disabil. 36C, 328–337. doi: 10.1016/j.ridd.2014.10.030
Sparreboom, M., Leeuw, A. R., Snik, A. F., and Mylanus, E. A. (2012). Sequential bilateral cochlear implantation in children: parents' perspective and device use. Int. J. Pediatr. Otorhinolaryngol. 76, 339–344. doi: 10.1016/j.ijporl.2011.12.004
Sparreboom, M., Snik, A. F., and Mylanus, E. A. (2011). Sequential bilateral cochlear implantation in children: development of the primary auditory abilities of bilateral stimulation. Audiol. Neuro-otol. 16, 203–213. doi: 10.1159/000320270
Sullivan, G. M. (2011). Getting off the “gold standard”: randomized controlled trials and education research. J. Grad. Med. Educ. 3, 285–289. doi: 10.4300/JGME-D-11-00147.1
Sumner, G. A., and Spietz, A. (1995). NCAST Caregiver/Parent-Child Interaction Teaching Manual. Seattle, WA: NCAST Publications.
Talari, K., and Goyal, M. (2020). Retrospective studies - utility and caveats. J. R. Coll. Phys. Edinb. 50, 398–402. doi: 10.4997/jrcpe.2020.409
Thiessen, E. D., and Saffran, J. R. (2007). Learning to learn: infants' acquisition of stress-based strategies for word segmentation. Lang. Learn. Dev. 3, 73–100. doi: 10.1207/s15473341lld0301_3
Tobey, E. A., Thal, D., Niparko, J. K., Eisenberg, L. S., Quittner, A. L., Wang, N. Y., et al. (2013). Influence of implantation age on school-age language performance in pediatric cochlear implant users. Int. J. Audiol. 52, 219–229. doi: 10.3109/14992027.2012.759666
Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., et al. (2018). PRISMA Extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473. doi: 10.7326/M18-0850
Uchanski, R. M., Davidson, L. S., Quadrizius, S., Reeder, R., Cadieux, J., Kettel, J., et al. (2009). Two ears and two (or more?) devices: a pediatric case study of bilateral profound hearing loss. Trends Amplification 13, 107–123. doi: 10.1177/1084713809336423
Umansky, A. M., Jeffe, D. B., and Lieu, J. E. (2011). The HEAR-QL: quality of life questionnaire for children with hearing loss. J. Am. Acad. Audiol. 22, 644–653. doi: 10.3766/jaaa.22.10.3
van der Straaten, T. F. K., Briaire, J. J., Vickers, D., Boermans, P., and Frijns, J. H. M. (2021). Selection criteria for cochlear implantation in the United Kingdom and Flanders: toward a less restrictive standard. Ear Hear. 42, 68–75. doi: 10.1097/AUD.0000000000000901
van Wieringen, A., and Wouters, J. (2015). What can we expect of normally-developing children implanted at a young age with respect to their auditory, linguistic and cognitive skills? Hear. Res. 322, 171–179. doi: 10.1016/j.heares.2014.09.002
Vassar, M., and Holzmann, M. (2013). The retrospective chart review: important methodological considerations. J. Educ. Eval. Health Prof. 10:12. doi: 10.3352/jeehp.2013.10.12
Vickers, D., Salorio-Corbetto, M., Driver, S., Rocca, C., Levtov, Y., Sum, K., et al. (2021). Involving children and teenagers with bilateral cochlear implants in the design of the BEARS (Both EARS) virtual reality training suite improves personalization. Front. Digit. Health 3:759723. doi: 10.3389/fdgth.2021.759723
Vickers, D., Summerfield, Q., and Lovett, R. (2015). Candidacy criteria for paediatric bilateral cochlear implantation in the United Kingdom. Cochlear Implants Int. 16(Suppl 1), S48–S49. doi: 10.1179/1467010014Z.000000000235
Wang, N. Y., Eisenberg, L. S., Johnson, K. C., Fink, N. E., Tobey, E. A., Quittner, A. L., et al. (2008). Tracking development of speech recognition: longitudinal data from hierarchical assessments in the childhood development after cochlear implantation study. Otol. Neurotol. 29, 240–245. doi: 10.1097/MAO.0b013e3181627a37
Wang, Y., Sibaii, F., Lee, K., Gill, M. J., and Hatch, J. L. (2021). Meta-analytic findings on reading in children with cochlear implants. J. Deaf. Stud. Deaf. Educ. 26, 336–350. doi: 10.1093/deafed/enab010
Wechsler, D. (1989). Wechsler Preschool and Primary Scale of Intelligence - Revised (WPPSI-R). San Antonio, TX: The Psychological Corporation. doi: 10.1037/t48859-000
Wechsler, D. (2003). Wechsler Intelligence Scale for Children - Fourth Edition (WISC-IV). San Antonia, TX: Pearson. doi: 10.1037/t15174-000
Wechsler, D. (2011). Wechsler Abbreviated Scale of Intelligence - Second Edition (WASI-II). San Antonio, TX: NCS Pearson. doi: 10.1037/t15171-000
Weichbold, V., Tsiakpini, L., Coninx, F., and D'Haese, P. (2005). Konstruktion eines Eltern-Fragebogens zur Entwicklung des auditiven Verhaltens von Kleinkindern bis zu zwei Jahren [Development of a parent questionnaire for assessment of auditory behaviour of infants up to two years of age]. Laryngorhinootologie 84, 328–334. doi: 10.1055/s-2004-826232
Wenrich, K. A., Davidson, L. S., and Uchanski, R. M. (2017). Segmental and suprasegmental perception in children using hearing aids. J. Am. Acad. Audiol. 28, 901–912. doi: 10.3766/jaaa.16105
Wie, O. B., Torkildsen, J. V. K., Schauber, S., Busch, T., and Litovsky, R. (2020). Long-term language development in children with early simultaneous bilateral cochlear implants. Ear Hear. 41, 1294–1305. doi: 10.1097/AUD.0000000000000851
Wiseman, K. B., and Warner-Czyz, A. D. (2018). Inconsistent device use in pediatric cochlear implant users: Prevalence and risk factors. Cochlear Implants Int. 19, 131–141. doi: 10.1080/14670100.2017.1418161
Wiseman, K. B., Warner-Czyz, A. D., Kwon, S., Fiorentino, K., and Sweeney, M. (2021). Relationships between daily device use and early communication outcomes in young children with cochlear implants. Ear Hear. 42, 1042–1053. doi: 10.1097/AUD.0000000000000999
Wu, D., Woodson, E. W., Masur, J., and Bent, J. (2015). Pediatric cochlear implantation: role of language, income, and ethnicity. Int. J. Pediatr. Otorhinolaryngol. 79, 721–724. doi: 10.1016/j.ijporl.2015.02.030
Yang, H. M., Wu, J. L., Lin, Y. H., and Sher, Y. J. (2004). Development of Mandarin monosyllabic lexical neighbourhood test (LNT). Cochlear Implants Int. 5, 203–205. doi: 10.1002/cii.232
Yang, Y., Chen, M., Zheng, J., Hao, J., Liu, B., Liu, W., et al. (2020). Clinical evaluation of cochlear implantation in children younger than 12 months of age. Pediatr. Investig. 4, 99–103. doi: 10.1002/ped4.12202
Keywords: cochlear implant, contextual factors, hearing outcomes, speech perception, ecological systems, development
Citation: Corbett F and Van Zalk N (2025) Speech perception and hearing outcomes following pediatric bilateral cochlear implants: a scoping review of developmental contextual influences. Front. Audiol. Otol. 3:1583242. doi: 10.3389/fauot.2025.1583242
Received: 25 February 2025; Accepted: 27 March 2025;
Published: 17 April 2025.
Edited by:
Ilona Anderson, MED-EL, AustriaReviewed by:
Sujoy Kumar Makar, Ali Yavar Jung National Institute for the Hearing Handicapped, IndiaCopyright © 2025 Corbett and Van Zalk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fleur Corbett, Zi5jb3JiZXR0QGltcGVyaWFsLmFjLnVr
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.