
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Audiol. Otol. , 11 March 2024
Sec. Clinical Research in Auditory Implants and Hearing Aids
Volume 2 - 2024 | https://doi.org/10.3389/fauot.2024.1357306
This article is part of the Research Topic The Future of Cochlear Implants: Breakthroughs in Technology and Outcome Assessment View all 6 articles
Introduction: Flexible electrode arrays have shown to be an effective solution to ensure atraumatic insertion. However, flexible full-length electrodes are not suited for patients with smaller cochleae. Therefore, this study aimed to evaluate short-term and medium-term hearing preservation (HP) in patients with low-frequency residual hearing (LFRH) who were implanted with a flexible 28-mm electrode array and who did not meet the indication criteria for electric-acoustic stimulation (EAS).
Methods: HP was determined based on the pure-tone audiogram of the implanted ear. A bisyllable sentence test was used to assess speech perception in quiet and in noise. The hearing implant sound quality index (HISQUI19) evaluated self-reported hearing quality. The tests were conducted pre- and post-operatively, at first fitting, and at 1, 3, 6, and 12 months after first fitting.
Results: At 12 months post first fitting, 2 patients had complete HP; 4 patients had partial HP. Speech perception scores improved in all patients of the study. The mean scores on the bisyllable sentence test in noise significantly increased from 30% pre-operatively to 62% 6 months post first-fitting and to 68% 12 months post first-fitting. The mean score of the HISQUI19 improved from 40.56 (poor) pre-operatively to 72.56 (moderate) 1 month post first-fitting and to 90.29 (good) 12 months post first-fitting.
Conclusion: The 28-mm flexible electrode array facilitates atraumatic surgery and HP and results in improved speech perception and subjective sound quality scores.
Hearing preservation (HP) in patients with residual hearing (RH) has gained importance since evidence of the benefit of electric-acoustic stimulation (EAS) was provided (Kiefer et al., 2005; Gstoettner et al., 2009; Skarzynski and Lorens, 2010). Patients with hearing thresholds better or equal to 70 dB HL at 125 and 250 Hz and hearing thresholds better or equal to 90 dB HL at 500 Hz are eligible for EAS.
Originally, the importance of HP was only recognized in cochlear implant (CI) recipients with RH in the low frequencies and profound hearing loss (HL) in the mid to high frequencies. Today, however, surgeons seek to preserve the structure whenever possible, since several studies showed that HP helps CI recipients obtain better speech perception scores and gain benefit from potential reimplantation or other subsequent treatment options even if the pre-operative RH is too poor to be functional (Sierra et al., 2019).
HP is achieved by applying atraumatic surgical techniques and performing atraumatic electrode insertion to ensure structure preservation and HP. Using a straight, flexible, and thin electrode array and gentle insertion into the lateral wall of the cochlea is key to structure preservation in order to ensure cochlear integrity (Moteki et al., 2018). Therefore, different types of flexible electrode arrays have specifically been developed to facilitate minimization of trauma by reducing the required insertion force by 30 to 40% compared to the insertion of standard electrode arrays (Baumgartner et al., 2007).
A flexible electrode array with a standard length of 31.5 mm was specifically designed to combine atraumatic electrode insertion with complete cochlear coverage. Several studies clearly showed that low-frequency HP can be achieved when using such an electrode array (Baumgartner et al., 2007; Punte et al., 2010; Helbig et al., 2011; Skarzynski et al., 2011; Usami et al., 2011; Mick et al., 2014). However, a full-length electrode array is not an ideal option in patients with smaller cochleae because it might lead to an over-insertion of the electrode array or to a non-insertion of basal electrode contacts. Therefore, a flexible 28-mm electrode array was developed by MED-EL to meet the needs of CI candidates who are not suited for the insertion of a full-length electrode array.
The primary aim of this study was to determine short-term and medium-term HP in patients with low-frequency residual hearing (LFRH) who were implanted with a FLEX28 electrode array and who did not meet the indication criteria for EAS. The secondary aims were to evaluate short-term and medium-term speech perception outcomes and to assess the self-reported level of sound quality.
To participate in the study, potential patients had to be (1) 18 years or older at enrolment; (2) fluent in Spanish; (3) be willing and able to participate in all test and control sessions; (4) have postlingual HL; (5) have residual hearing of 70 dB HL or better at 125 and 250 Hz, and of 90 dB HL or better at 500 Hz; (6) have pre-operative bisyllable scores in quiet of 60% or lower at 60 dB SPL in best aided condition; (7) have pre-operative open-set speech scores of 10% or higher at 60 dB SPL in the best aided condition; (8) have a cochlea anatomy which allows the insertion of a FLEX28 electrode array; (9) have a functional auditory nerve; (10) meet the clinic's candidacy criteria; and (11) be in good physical and mental health.
Potential patients were excluded from the study if they did not meet all inclusion criteria; were not motivated to participate in the study or had unrealistic expectations; had pre-lingual HL; were candidates for EAS (i.e., patients with an audiogram within the EAS thresholds); had a recent history of middle ear infection; had central auditory lesions; had contraindications for surgery in general or for cochlear implantation in particular; had autoimmune diseases or a prior history of meningitis; had otosclerosis, cochlear ossification, or any other type of malformation or obstruction of the cochlea; had any known allergy or intolerance to any of the materials used before, during, and immediately after surgery.
Nine patients were recruited for the study in 2012 from the Department of Otolaryngology of the La Paz University Hospital in Madrid.
The mean age at enrolment was 56.9 years (range: 38–80 yr). The mean age at onset of hearing loss was 33.8 years (range: 7–60 yr). Six patients (66.6%) were female and 3 were male. Five patients (55.56%) were implanted in the left ear. One patient (11.11%) had had previous ear surgery. Etiology was unknown in 4 patients (44.44%), hereditary in 1 patient (11.11%), ototoxicity in 2 patients (22.22%), progressive HL in 1 patient (11.11%), and progressive HL with chronic simple otitis media in 1 patient (11.11%). For the individual demographic data, see Table 1.
The FLEX28 electrode array is 28 mm long with 12 electrode channels, each separated by 2.1 mm. The 7 basal electrodes are paired; the 5 apical electrodes are unpaired. The basal end has a diameter of 0.8 mm. It minimizes trauma at the entry point with a 40% size reduction at the entry point compared to the FLEXSOFT electrode array. The reinforced part of the electrode array is 25 mm long. The FLEX28 electrode array was inserted following the surgical guidelines for atraumatic CI surgery in all patients.
The study was designed as a prospective and longitudinal study. RH was tested pre-operatively, post-operatively, at first fitting, 1-month post first-fitting, and 3, 6, and 12 months post first-fitting. Pure-tone thresholds were measured at 125, 250, 500, 1,000, 2,000, 4,000, and 8,000 Hz on both ears in all patients. HP was calculated using the formula reported by Skarzynski et al. (2013) based on the pure-tone audiogram of the implanted ear.
If values were missing, the existing values were interpolated. Missing pure-tone thresholds at 8,000 Hz were replaced by the maximum testing level defined by Skarzynski et al. (2013) (i.e., 95 dB). Other missing data points were interpolated by calculating the average of the thresholds of the nearest lower and upper neighbor (e.g., if the pure-tone threshold at 250 Hz was missing, it was replaced by the average of the 125 Hz and 500 Hz thresholds). Following Skarzynski et al. (2013), RH was classified as complete HP above 75%, as partial between 25% and 75%, and as minimal below 25%.
Speech perception was measured using a bisyllable sentence test in quiet and in noise. Patients were seated 1 m away from the loudspeakers at 0° azimuth. The tests were done without lip reading, at 65 dB SPL, and with a signal/noise ratio of 10 dB SPL s-noise below the signal. The bisyllable words are phonetically balanced words belonging to the everyday vocabulary; it is composed of 20 lists with 25 recorded words. The words appear in the list with the same proportion as in the spoken language (>20%). It was developed by de Cárdenas and Aguiar (1994).
Self-reported hearing quality was assessed using the hearing implant sound quality index (HISQUI19). The HISQUI19 is a validated questionnaire (Amann and Anderson, 2014; Calvino et al., 2016) used to determine an individual's sound quality in daily life. It measures how good or poor the person finds the sound quality from their hearing implant in personal, everyday listening situations. It comprises 19 items and each item is answered according to frequency on a 7-point scale, the endpoints of which are “always” (7 points) and “never” (1 point). Total scores, i.e., the sum of the individual items, are assigned a qualitative level of quality of sound: a score of 19–29 indicates very poor sound quality; 30–59 poor sound quality; 60–89 moderate sound quality; 90–109 good sound quality; and 110–133 very good sound quality.
Depending on the data distribution, the student's t-test or the Wilcoxon rank test was performed to identify differences between the different test intervals. For statistical analysis, the IBM SPSS Statistics 24 software (IBM, Armonk, New York, USA) was used.
The study was reviewed and approved by the Ethics Committee at the La Paz University Hospital in Madrid (PI-1384). All patients gave informed written consent.
Patient 9 had cochlear implantation with a subtotal petrosectomy approach because of a cerebrospinal fluid leak fistula in the ear to be implanted. So, he had complete HL at the 1-month follow-up visit.
Table 2 shows the pure-tone average (PTA) and HP at the pre-operative, post-operative (i.e., right after implantation), and 12 months post first fitting intervals. The average time between implantation and post-operative testing was 8.4 days (range: 6–12 days). Figure 1 shows the individual audiograms for all 9 patients at the pre-operative, post-operative, and 12 months post first fitting intervals. Table 3 provides an overview of patients with complete HP, partial HP, minimal HP, and HL at post-implantation, at first fitting, at 1-month post first fitting, and at 12-months post first fitting. Complete HP was achieved in 2 out of 9 patients (84.48% in Patient 5; 97.96% in Patient 6); partial HP was achieved in 4 out of 9 patients.
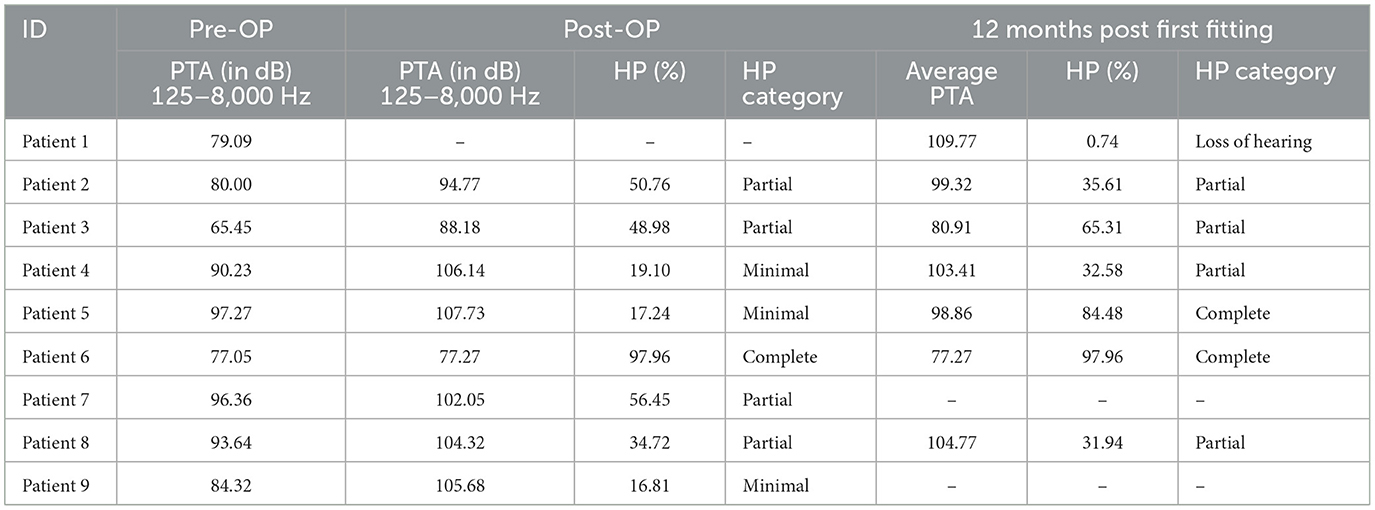
Table 2. Pure-tone average (PTA) and hearing preservation (HP) at the pre-operative visit, at the post-operative visit, and at 12 months post first fitting.
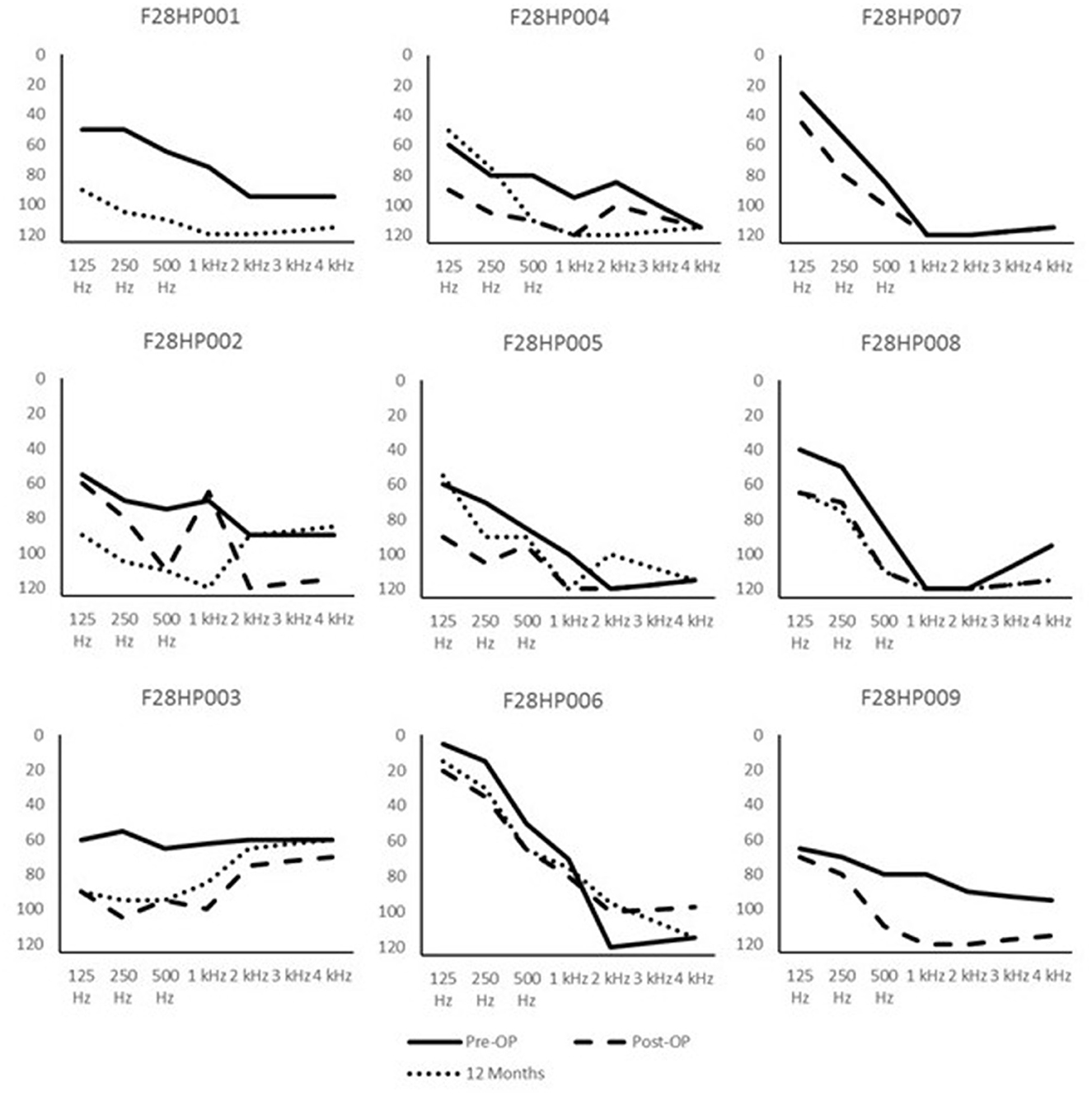
Figure 1. Individual audiograms at the pre-operative (Pre-OP), post-operative (Post-OP), and 12 months post first fitting intervals; x-axis = Hz; y-axis = dB.
Figure 2 shows the results of the bisyllable sentence test. The mean scores on the bisyllable sentence test in noise (Series 1) significantly increased from 30% (range: 9%−50%) pre-operatively to 62% (range: 49%−75%) 6 months post first-fitting and to 68% (range: 50%−79%) 12 months post first-fitting.
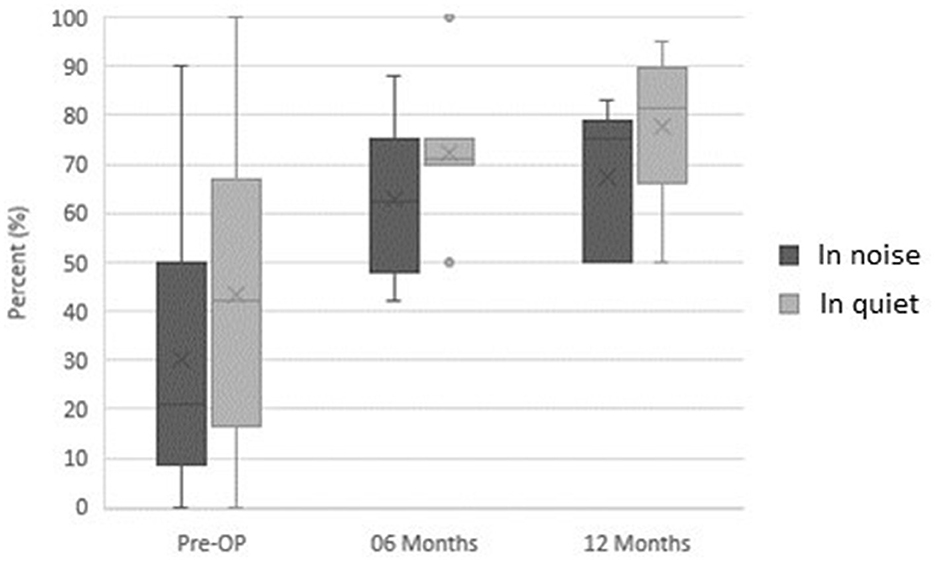
Figure 2. Bisyllable Sentence Tests. Mean scores on the bisyllable sentence test in noise and in quiet at the pre-operative visit, at 6-months post first fitting and 12 months post first fitting.
The mean scores on the bisyllable sentence test in quiet (Series 2) significantly increased from 42% (range: 17%−67%) pre-operatively to 72% (range: 70%−75%) 6 months post first-fitting and to 77% (range: 67%−90%) 12 months post first-fitting.
Figure 3 shows the results of patients completing the HISQUI19. The mean HISQUI19 score increased from 40.56 (SD: 17.91; range: 19–77) pre-operatively, which is considered poor, to 72.56 (SD: 26.24; range: 40–122) 1 month post first-fitting, which is considered moderate, and to 90.29 (SD: 21.11; range: 66–125) 12 months post first-fitting, which is considered good.
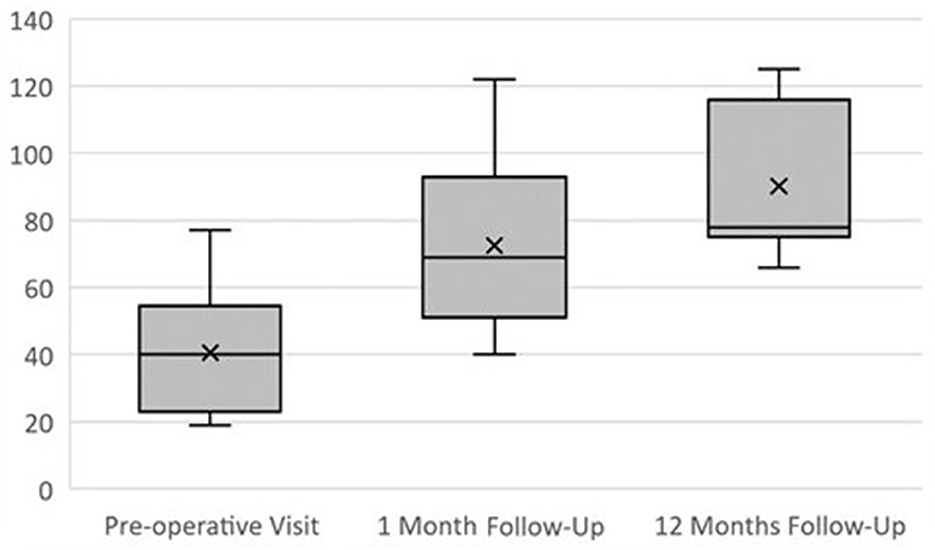
Figure 3. HISQUI19. Mean HISQUI19 score at the pre-operative visit, at 1 month post first fitting and 12 months post first fitting.
Patient 9 had cochlear implantation with a subtotal petrosectomy approach because of a cerebrospinal fluid leak fistula in the ear to be implanted. This patient had an LCR fistula that was operated on by middle fossa on the left side in 2014. He also had a fistula on the right side that was implanted, so he underwent a petrosectomy. Therefore, neither speech perception outcomes nor HISQUI19 results have been documented for patient 9.
For the individual HISQUI19 results, please see Table 4.
In our study, the FLEX28 electrode array was inserted in an atraumatic CI surgery in all patients. At 12 months post first fitting, 2 patients had complete HP, 4 patients had partial HP, and 1 patient had complete HL.
Our results resemble the findings of a similar study conducted by Sierra et al. (2019). Their research found complete HP in 7, partial HP in 3, and minimal HP in 1 of the 13 patients who were implanted with a FLEX28 electrode array; had LFRH before surgery and did not meet the criteria for EAS. Furthermore, Sierra et al. (2019) provided evidence for the association between the use of an atraumatic surgical technique and the degree of HP with different types of deep insertion electrode arrays.
An atraumatic surgical approach is by now considered a prerequisite for HP in the low frequencies. Moteki et al. (2018) also investigated and confirmed the feasibility of HP with long electrode arrays (>20 mm). Seventeen of the 18 patients had post-operative HP in the low frequencies; 50% had complete HP in the low frequencies.
In contrast, Kisser et al. (2016) showed relatively poor HP results in 56 patients implanted with a FLEX28. In most cases, hearing was partially preserved. However, HL was observed in all cases at all frequencies; 23% of the patients had complete HL. The authors ascribe the poor HP results to poor pre-operative hearing with a mean PTA of 85.4 dB in the low frequencies and 98.7 dB in the higher frequencies. This might explain the extraordinary outcome (97.96% HP) in Patient 6 of our study, who had the lowest pre-operative PTA in the low frequencies. This demonstrates that HP always depends on the baseline performance.
Interestingly, speech perception scores improved in all patients of our study, including the ones without HP or only partial HP. This is in accordance with the findings of Novak et al. (2007) and Adunka et al. (2008). The HISQUI19 results also improved in all patients, which suggests that speech perception, successful participation in conversations including telephone chats, perception of environmental sounds, and music appreciation can be achieved with the use of long electrode arrays. This topic should be the focus of future research studies in order to further boost the quality of life of CI users.
Furthermore, our study provided evidence that HP is not only feasible in young CI recipients which is in accordance with the findings of Bourn et al. (2020) who demonstrated that HP is even feasible in elderly patients aged 72 years and older.
In general, ENT surgeons recommend using deep insertion electrode arrays because they allow for stimulation of the distal cochlea in case HL progresses, which often occurs in patients with sensorineural hearing loss (Sierra et al., 2019).
The sample size was too small to justify generalizations of the outcomes of this study. Further, the cochlear duct length was not measured in the course of this study.
The 28-mm flexible electrode array facilitates atraumatic surgery and HP; and results in improved speech perception and subjective sound quality scores.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Research Ethics Committee with Medical Products Hospital Universitario La Paz Paseo de la Castellana, Madrid, Spain (PI-1384). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MC: Writing—original draft, Writing—review & editing. IS-C: Writing—original draft, Writing—review & editing. EM: Writing—original draft, Writing—review & editing. JG: Writing—original draft, Writing—review & editing. LL: Writing—original draft, Writing—review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors thank all patients for their participation in the study. They would like to thank Ursula Lehner-Mayrhofer (MED-EL Innsbruck, Austria) for her medical writing services.
EM is employed at MED-EL as a clinical engineer; this function entails technical fitting support. MED-EL was not involved in the study design, collection, analysis, and interpretation of data or the decision to submit it for publication.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Adunka, O. F., Buss, E., Clark, M. S., Pillsbury, H. C., and Buchman, C. A. (2008). Effect of pre-operative residual hearing on speech perception after cochlear implantation. Laryngoscope 118, 2044–2049. doi: 10.1097/MLG.0b013e3181820900
Amann, E., and Anderson, I. (2014). Development and validation of a questionnaire for hearing implant users to self-assess their auditory abilities in everyday communication situations: the Hearing Implant Sound Quality Index (HISQUI19). Acta Otolaryngol. 134, 915–923. doi: 10.3109/00016489.2014.909604
Baumgartner, W.-D., Jappel, A., Morera, C., Gstöttner, W., Müller, J., Kiefer, J., et al. (2007). Outcomes in adults implanted with the FLEX soft electrode. Acta Otolaryngol. 127, 579–586. doi: 10.1080/00016480600987784
Bourn, S., Goldstein, M. R., and Jacob, A. (2020). Hearing preservation in elderly cochlear implant recipients. Otol. Neurotol. 41, 618–624. doi: 10.1097/MAO.0000000000002596
Calvino, M., Gavilán, J., Sánchez-Cuadrado, I., Pérez-Mora, R. M., Muñoz, E., and Lassaletta, L. (2016). Validation of the Hearing Implant Sound Quality Index (HISQUI19) to assess Spanish-speaking cochlear implant users' auditory abilities in everyday communication situations. Acta Otolaryngol. 136, 48–55. doi: 10.3109/00016489.2015.1086021
de Cárdenas, M. R., and Aguiar, V. M. (1994). Cuaderno de logoaudiometría. Madrid: Universidad Nacional de Educación a distancia.
Gstoettner, W., Helbig, S., Settevendemie, C., Baumann, U., Wagenblast, J., Arnoldner, C., et al. (2009). A new electrode for residual hearing preservation in cochlear implantation: first clinical results. Acta Otolaryngol. 129, 372–379. doi: 10.1080/00016480802552568
Helbig, S., Baumann, U., Hey, C., and Helbig, M. (2011). Hearing preservation after complete cochlear coverage in cochlear implantation with the free-fitting FLEXSOFT electrode carrier. Otol. Neurotol. 32, 973–979. doi: 10.1097/MAO.0b013e31822558c4
Kiefer, J., Pok, M., Adunka, O., Stürzebecher, E., Baumgartner, W., Schmidt, M., et al. (2005). Combined electric and acoustic stimulation of the auditory system: results of a clinical study. Audiol. Neurotol. 10, 134–144. doi: 10.1159/000084023
Kisser, U., Wünsch, J., Hempel, J.-M., Adderson-Kisser, C., Stelter, K., Krause, E., et al. (2016). Residual hearing outcomes after cochlear implant surgery using ultra-flexible 28-mm electrodes. Otol. Neurotol. 37, 878–881. doi: 10.1097/MAO.0000000000001089
Mick, P., Amoodi, H., Shipp, D., Friesen, L., Symons, S., Lin, V., et al. (2014). Hearing preservation with full insertion of the FLEXsoft electrode. Otol. Neurotol. 35, e40–e44. doi: 10.1097/MAO.0b013e318291c66d
Moteki, H., Nishio, S.-Y., Miyagawa, M., Tsukada, K., Noguchi, Y., and Usami, S.-I. (2018). Feasibility of hearing preservation for residual hearing with longer cochlear implant electrodes. Acta Otolaryngol. 138, 1080–1085. doi: 10.1080/00016489.2018.1508888
Novak, M. A., Black, J. M., and Koch, D. B. (2007). Standard cochlear implantation of adults with residual low-frequency hearing: implications for combined electro-acoustic stimulation. Otol. Neurotol. 28, 609–614. doi: 10.1097/mao.0b013e318043014c
Punte, A. K., Vermeire, K., and Van de Heyning, P. (2010). “Bilateral electric acoustic stimulation: a comparison of partial and deep cochlear electrode insertion,” in Cochlear Implants and Hearing Preservation (Karger Publishers), 144–152. doi: 10.1159/000262606
Sierra, C., Calderón, M., Bárcena, E., Tisaire, A., and Raboso, E. (2019). Preservation of residual hearing after cochlear implant surgery with deep insertion electrode arrays. Otol. Neurotol. 40, e373–e380. doi: 10.1097/MAO.0000000000002170
Skarzynski, H., and Lorens, A. (2010). Partial deafness treatment. Cochlear Implants Int. 11, 29–41. doi: 10.1179/146701010X12671178390799
Skarzynski, H., Lorens, A., Zgoda, M., Piotrowska, A., Skarzynski, P. H., and Szkielkowska, A. (2011). Atraumatic round window deep insertion of cochlear electrodes. Acta Otolaryngol. 131, 740–749. doi: 10.3109/00016489.2011.557780
Skarzynski, H., Van de Heyning, P., Agrawal, S., Arauz, S., Atlas, M., Baumgartner, W., et al. (2013). Towards a consensus on a hearing preservation classification system. Acta Otolaryngol. 133, 3–13. doi: 10.3109/00016489.2013.869059
Keywords: hearing preservation, electrode array, cochlear implantation, outcome assessment, cochlear implant outcomes, speech perception
Citation: Calvino M, Sánchez-Cuadrado I, Muñoz E, Gavilán J and Lassaletta L (2024) Successful hearing preservation and improved subjective sound quality with the flexible 28-mm electrode array. Front. Audiol. Otol. 2:1357306. doi: 10.3389/fauot.2024.1357306
Received: 17 December 2023; Accepted: 16 February 2024;
Published: 11 March 2024.
Edited by:
Takwa Gabr, Kafrelsheikh University, EgyptReviewed by:
Brian D. Nicholas, Upstate Medical University, United StatesCopyright © 2024 Calvino, Sánchez-Cuadrado, Muñoz, Gavilán and Lassaletta. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luis Lassaletta, bGxhc3NhbGV0dGFAc2FsdWQubWFkcmlkLm9yZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.