
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Audiol. Otol. , 25 April 2023
Sec. Clinical Research in Auditory Implants and Hearing Aids
Volume 1 - 2023 | https://doi.org/10.3389/fauot.2023.1167853
Adults with all levels of hearing loss have faced financial and accessibility constraints in obtaining prescription hearing aids. To increase access to hearing aids, the Food and Drug Administration (FDA) has created a new designation of over-the-counter (OTC) hearing aids for adults with perceived mild to moderate hearing loss. The goal of this article is to describe the incorporation of OTC hearing aid users into established audiology services. A proposed workflow was created by otolaryngologists and audiologists at Johns Hopkins University School of Medicine and is being implemented at outpatient audiology offices. We used published criteria for appropriate OTC hearing aid usage and disqualifying criteria hearing specialists should be aware of. The proposed workflow describes the multiple entry points for OTC hearing aid users seeking access to care and appropriate objectives for these visits. The new FDA ruling has increased the accessibility of hearing assistance devices; however, the varying degrees of retailer support systems could lead to improper fitting and other technical problems for some patients trialing new hearing aids. Our proposed workflow aims to describe the incorporation of established hearing assistance services with the new OTC hearing aid market.
On August 17th, 2022, the Food and Drug Administration (FDA) issued a final rule establishing a new category of over-the-counter (OTC) hearing aids for perceived mild to moderate hearing impairment for adults 18 years and older (FDA, 2022). This allows adults with perceived mild to moderate hearing loss to purchase hearing aids directly from stores or online retailers without the assistance of a healthcare professional. The ruling was made in part to lower the costs and to increase access of hearing aids which previously required the involvement of an audiologist or hearing aid dispenser for proper assessment and fitting of the hearing aids (Blustein et al., 2022). The ruling also established certain criteria for the OTC hearing aids to provide standards of patient safety and efficacy of these devices (FDA, 2022). These criteria include the following: lowering the maximum sound output of the hearing aids to reduce risk of over-amplification, establishing an insertion depth limit of the hearing aid, requiring the devices to have user-adjustable volume controls, simplify language for the labeling of devices, and including performance specifications and design requirements of the OTC hearing aids (FDA, 2022).
The traditional workflow for prescription hearing aids was designed to treat and monitor patients with all degrees of hearing loss, from mild to profound. In this model, most patients would require a healthcare professional—likely a primary care physician—for a referral to audiology after reporting a perceived deterioration in hearing (Yong et al., 2019) (Figure 1A). They would then be seen by an audiologist for a comprehensive audiologic evaluation which could include a full hearing evaluation and audiogram to assess the extent of their hearing loss (Figure 1A). The hearing aid evaluation includes reviewing the patient's hearing test and symptoms, discussing the patient's hearing goals and needs, and addressing any questions and concerns related to hearing aids. After the hearing aid evaluation, patients are fitted for their hearing aids (Figure 1A). At these fitting appointments, audiologists can use proprietary software created by the individual manufacturers to adjust the gain of the hearing aid to match the patients' need determined by the audiogram and patient preferences. Audiologists can also use a methods of gain verification such as subjective tests to assess function or programs such as Real Ear Measurement, where the output of the hearing aid is measured while in the patient's ear to ensure the patient is receiving adequate benefit from amplification (Zelisko et al., 1992).
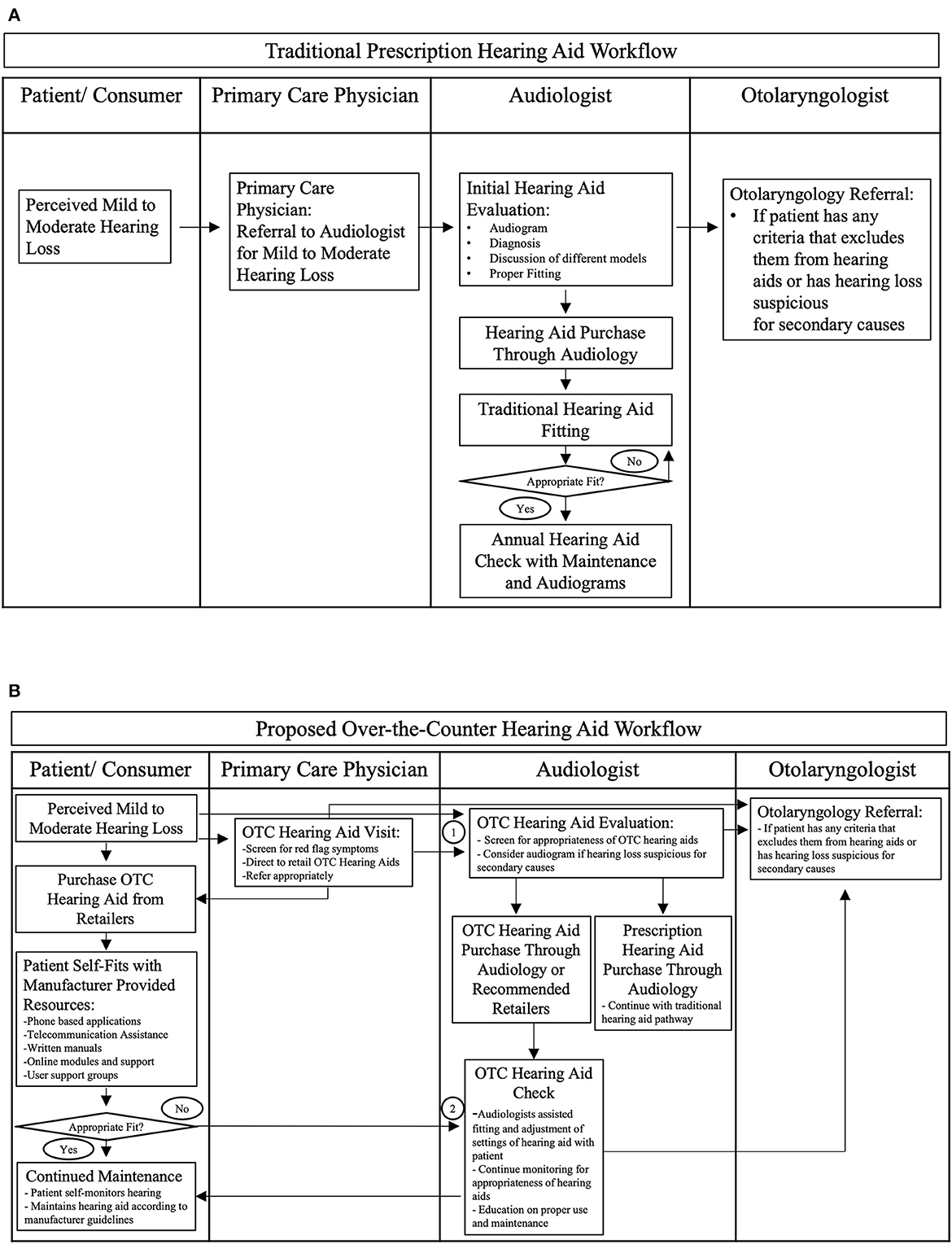
Figure 1. Hearing aid workflows. (A) Traditional prescription hearing aid workflow. (B) Proposed over-the-counter hearing aid workflow. “1” indicate the first entry point into audiology care before a prospective hearing aid user has bought an over-the-counter hearing aid. “2” indicates the second entry point into audiology care after someone has bought an over-the-counter hearing aid.
The next steps for these patients may involve multiple hearing aid checks in the following months as the devices may need to be adjusted to match the patient's needs (Figure 1A). Under certain institutional guidelines, these patients are counseled to receive a hearing test and a hearing aid check every year to monitor use of the hearing aid and to monitor progression of their hearing loss with audiograms. These hearing aid check visits will generally involve a discussion of the patient's use of the hearing aid, perceived changes in their hearing, and questions they have about the care and maintenance of the hearing aid (Figure 1A). In these visits, audiologists can adjust the gain of the hearing aids to match the changes in hearing reflected in the audiograms.
The FDA's new regulation was made considering the strong benefits of hearing aid use for patients with mild to moderate hearing loss as well as the increasing evidence that some patients may not require professional fitting of hearing aids to receive benefit from them (Convery et al., 2017; Humes et al., 2017; Mackersie et al., 2020; Sabin et al., 2020). Previous research has shown that with preprogrammed settings to choose from on their hearing aids, most people with hearing impairment can pick settings that provide significant improvement in their hearing and listening abilities (Mackersie et al., 2020; Sabin et al., 2020). However, certain populations are more likely to be able to self-fit hearing aids without assistance than others. Some of the characteristics of patients who can properly fit their hearing aids include those with previous hearing aid experience, mobile phone ownership, and preserved cognition function (Convery et al., 2017; Humes et al., 2017; Mackersie et al., 2020; Sabin et al., 2020). Even when patients are effectively fit with prescription hearing aids, some studies suggest that many users may discontinue use of these devices due to the barriers including continual maintenance of the devices, associated costs or fees for service, and negative stigmas with wearing hearing aids (Fuentes-López et al., 2019; Saunders et al., 2021).
The over-the-counter hearing aid manufacturers are managing this potential gap in self-fitting through the customer support they offer. The support can range from in-depth virtual assistance via phone applications, online training modules, to device manuals with printed instructions (Ferguson et al., 2016; Dragan, 2022; Siber, 2022). However, the different levels of support can generally correlate with the retail price of the products and can thus lead to varying degrees of success of self-fitting for these devices (Dragan, 2022; Siber, 2022).
Along with the self-fitting process, users will need to maintain these devices and potentially troubleshoot errors that can occur with regular use such as battery issues, connectivity problems with mobile devices, and ear wax clogs. This role was also filled by audiologists in regular checkup visits; however, these patients will now need to rely on the services provided by OTC hearing aid manufacturers. Hearing aid manufacturers are likely to continue utilizing such established methods of assisting people with their hearing aids, including online modules, to improve the efficacy and accessibility of their products for a wider range of individuals with hearing loss (Barker et al., 2016; Ferguson et al., 2016). However, the change in access to hearing assistance may lead to certain patients discontinuing use of their hearing aids over time. Previous research has shown that people with lower cognitive performance, closed off personality types, and lower education levels are all associated with reduced ability to manage their hearing aid devices (Fuentes-López et al., 2019; Sarangi and Johnson, 2022). It has been shown that those with the least self-efficacy and most dissatisfaction with their devices are those with trouble managing their devices (Johnson et al., 2018). In addition to that, people with multiple comorbidities (Parkinson's disease, diabetes, arthritis, or visual impairment) have been shown to have lower rates of hearing aid persistence (Saunders et al., 2021). Considering these factors in limiting use, and around 30% of hearing aid users may reduce or stop using their hearing aids after fitting or prescription hearing aids, this population is at risk of experiencing trouble fitting and maintaining use of their devices (Saunders et al., 2021).
The change in regulation of hearing aids has opened the market to an increasing number of hearing aid devices, but the role of audiologists in this new hearing aid environment has not been addressed. The lack of consistent support across OTC hearing aid manufacturers and the problems which may arise while using hearing aids will necessitate audiologists to bridge this gap in care. This proposed workflow underscores the role of audiologists in assisting and evaluating patients who may have trouble obtaining and successfully utilizing OTC hearing aids. This workflow should also clarify when it is appropriate to refer patients to audiologists and to otolaryngologists.
The proposed OTC Hearing Aid Workflow was developed by a neurotologist, three audiologists, an otolaryngology resident, and a medical student. The proposed workflow is meant to serve as a guideline for primary care providers, audiologists, and other healthcare professionals encountering patients with perceived mild to moderate hearing loss. The workflow describes multiple entry points for patients interested in hearing aids and appropriate goals of care for the health professionals to assist the patients in. This workflow was designed to utilize the current structure of audiology care and provides tangible goals of care.
With the change in hearing aid regulation, patients can access hearing aids without a diagnosis from a healthcare provider. Now, when a patient perceives deterioration in their hearing, they can purchase a hearing aid directly from a retailer (Figure 1B). Once a patient has purchased a hearing aid on their own, they can use the manufacturer-created resources to self-fit the hearing aid to their needs (Figure 1B). The resources provided can range from video consultations with support staff, online training videos, and printed resources for the patients (Barker et al., 2016; Ferguson et al., 2016; Bass, 2022; Dragan, 2022, 2023).
Patients may also seek assistance from their primary care physicians for evaluation of other causes of their hearing loss or guidance about OTC hearing aids. Before purchasing an OTC hearing aid, prospective OTC hearing aid users should still be made aware of certain red flags or exclusion criteria as reported by the FDA, American Academy of Otolaryngology, and the Hearing Loss Association of America including the following: ear pain or discomfort, unusual ear shape, history of muffled hearing, dizziness, tinnitus, rapidly progressing hearing loss, or drainage from either ear in the last 6 months (American Academy of Otolaryngology- Head and Neck Surgery, 2022; Federal Register, 2022; Hearing Loss Association of America, 2022). These criteria were made to screen for potential secondary causes of hearing loss before a patient purchases a hearing aid (Kuhn et al., 2011; Lee and Bance, 2019). For patients still unsure if they require medical evaluation before obtaining a hearing aid, the Consumer Ear Disease Risk Assessment (CEDRA) provides a more in-depth analysis to determine risk for ear disease before obtaining a hearing aid (Klyn et al., 2019). When a prospective hearing aid user does visit their primary care physician, the physician is able to assess for risk of secondary causes of their hearing and determine if they need referral to hearing specialists. In addition, primary care providers should also consider referring patients interested in OTC hearing aids to audiology care with the following risk factors: no mobile phone ownership, cognitive impairments, patients with multiple comorbidities, and lower education levels (Table 1). Due to their increased risk of lower self-efficacy with using these devices, these patients may benefit from the extra support from audiologists (Fuentes-López et al., 2019; Saunders et al., 2021; Sarangi and Johnson, 2022).
Once patients obtain their OTC hearing aid, if they can properly self-fit, they will be more likely to maintain usage of these devices and obtain the benefit from them (Humes et al., 2017; Convery et al., 2019) (Figure 1B). On the other hand, patients who are dissatisfied with the fit or sound quality of their hearing aids will be able to visit local audiologists for an OTC hearing aid check visit (Figure 1B). These hearing aid check visits are an entry point into audiology care and will be similar to the visit in the traditional model where the audiologists can assess whether the gain of the devices is appropriate and check the physical fit of the hearing aids within the ear. These visits may also allow audiologists to assess symptoms that make them ineligible for OTC hearing aids (Hearing Loss Association of America, 2022). Patients experiencing any of the red flag symptoms such as dizziness, drainage, pain, tinnitus, or sudden changes in hearing should be screened and appropriately referred to otolaryngologists at this stage to help exclude infectious, autoimmune, functional, metabolic, or neoplastic causes of hearing loss that could have been missed when the patient first purchased an OTC hearing aid (Table 1) (Kuhn et al., 2011; Lee and Bance, 2019). Audiologists may also be able to troubleshoot maintenance and care for these devices. Once connected to care with an audiologist, these patients can continue seeking maintenance or follow-up care with these healthcare professionals as needed (Figure 1B).
Alternatively, patients who perceive their hearing loss to be mild to moderate may decide to directly enter audiology care by visiting an audiologist for assistance in choosing a hearing aid (Figure 1B). The audiologists in these visits may directly dispense OTC hearing aids to these patients or they can provide a list of recommended OTC hearing aids to purchase from retailers (Figure 1B). After acquiring hearing aids, these patients can continue to have hearing aid checks with an audiologist to troubleshoot any difficulties in fitting or maintaining their devices (Figure 1B).
Age-related hearing loss has been reported to be an important and potentially modifiable risk factor in age related cognition and mood disorders in older adults, and some studies suggest that hearing aids may improve general quality of life in these adults (Lin et al., 2013; Choi et al., 2016; Ferguson et al., 2017; Livingston et al., 2020). In younger adults, previous work suggests that hearing aids are effective at allowing young adults with hearing impairment to participate in a predominantly hearing society (Rijke et al., 2022). Even with the clear benefit of these devices, prescription hearing aids are not covered by all insurance packages (Reddy, 2017; Yong et al., 2019). This dynamic has placed the financial responsibility of these devices on many patients. This can be especially difficult for patients when a pair of hearing aids can cost anywhere from $3,000 to $7,000 (Reddy, 2017; Yong et al., 2019; Dragan, 2022, 2023; Virdi, 2022). The FDA's ruling establishing the availability of OTC hearing aids has changed the way many adults may access hearing services in the future (FDA, 2022). The ruling was made to lower the overall costs and to increase access of hearing aids which previously required the help of an audiologist or hearing aid dispenser for proper assessment and fitting (Blustein et al., 2022).
The proposed workflow to incorporate OTC hearing aid users into the established healthcare system provides two entry points for OTC hearing aid users to be evaluated by an audiologist, either to purchase OTC hearing aids directly or to troubleshoot and optimize use of their existing OTC devices. In these visits, hearing professionals can assess if OTC hearing aids are appropriate for the patient, or they may require a further work-up which could include an audiogram and an otolaryngology referral. These OTC hearing aid checks will be comparable to the hearing aid checks normally performed in the traditional prescription hearing aid model, where audiologists are able to troubleshoot the use, maintenance, and efficacy of these devices. One of the limitations of hearing aid check visits in the OTC hearing aid workflow is that audiologists are not able to use the proprietary software provided by the manufacturers of the prescription hearing aids to more precisely adjust the gain of the hearing aids to match the patient's audiogram and preferences (FDA, 2022; Virdi, 2022). Instead, with OTC hearing aids, audiologists will only be able to help adjust the hearing aids to the programmed settings available on these devices. This may limit the sound quality of the hearing aid and restrict how accurately audiologists can match patients' preferences. As the market for OTC hearing aids is expanding, the interface for working with these devices can vary (Girouard, 2022; Siber, 2022). This may lead to a learning curve in not only the patients but also the health care professionals who will assist with the use of these devices. As OTC hearing aids become more common, audiologists and other health care professionals may become more familiar with these devices and be able to assist patients more efficiently with these devices.
The OTC system offers a significant advantage in reducing the number of required patient visits and associated professional fees (Lin, 2012). Specifically, the complete hearing evaluation visit with an audiogram will no longer be required for these OTC models (FDA, 2022). Although this may result in cost saving, it is possible that patients with a more severe hearing prognosis or asymmetric hearing loss may be missed, or certain patients may be an inappropriately fit for OTC hearing aids. To mitigate this risk, it is crucial to be aware of red flag warnings and use risk assessment tools such as CEDRA to identify potential ear diseases (Klyn et al., 2019). However, the risk of inappropriate usage remains, and the OTC hearing aid checks beneficial to patients whose hearing loss could be due to secondary causes such as infection, vascular pathologies, or malignancy. While these hearing aid check visits would normally be covered by the original cost of the prescription hearing aid, these visits may need to be paid out of pocket in the cases of OTC hearing aids until insurance coverage changes to include these types of visits (Jilla et al., 2020).
The FDA's decision has created regulation to provide effective hearing devices to people with perceived mild to moderate hearing loss. The introduction of OTC hearing aids in the marketplace is a great step in increasing patient autonomy in accessing hearing aids. However, due to varying degrees of support offered to assist with these devices, the use of established hearing care may help bridge the gap between patients who are able to self-fit and those who may need more assistance. This proposed workflow highlights the entry points for patients with perceived hearing loss with healthcare professionals trained in managing hearing aids. Future studies will evaluate the efficacy of both this proposed workflow and how best to support users of OTC hearing aids.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
CP-H, CZ, LR, CR, and YA contributed to conception and design of the project. CP-H organized the workflow. CP-H and ZS wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Note that this content is solely the responsibility of the authors and does not necessarily reflect the official views of Johns Hopkins School of Medicine.
American Academy of Otolaryngology- Head Neck Surgery (2022). OTC Hearing Aids FAQs. Available online at: https://www.enthealth.org/be_ent_smart/otc-hearing-aids-faqs/ (accessed November 15, 2022).
Barker, F., Mackenzie, E., Elliott, L., Jones, S., and de Lusignan, S. (2016). Interventions to improve hearing aid use in adult auditory rehabilitation. Cochrane Database Syst. Rev. 2016, CD010342. doi: 10.1002/14651858.CD010342
Bass, A. (2022). Best Hearing Aids of 2022, Aging In Place. Available online at: https://aginginplace.org/hearing-aids/best/ (accessed December 13, 2022).
Blustein, J., Weinstein, B. E., and Chodosh, J. (2022). Over-the-counter hearing aids: what will it mean for older Americans? J. Am. Geriatr. Soc. 70, 2115–2120. doi: 10.1111/jgs.17781
Choi, J. S., Betz, J., Li, L., Blake, C. R., Sung, Y. K., Contrera, K. J., et al. (2016). Association of using hearing aids or cochlear implants with changes in depressive symptoms in older adults. JAMA Otolaryngol. Head Neck Surg. 142, 652–657. doi: 10.1001/jamaoto.2016.0700
Convery, E., Keidser, G., Hickson, L., and Meyer, C. (2019). Factors associated with successful setup of a self-fitting hearing aid and the need for personalized support. Ear Hear. 40, 794–804. doi: 10.1097/AUD.0000000000000663
Convery, E., Keidser, G., Seeto, M., and McLelland, M. (2017). Evaluation of the self-fitting process with a commercially available hearing aid. J. Am. Acad. Audiol. 28, 109–118. doi: 10.3766/jaaa.15076
Dragan, L. (2022). Over-the-counter hearing aids could finally give people an affordable, convenient hearing solution. New York Times, Aug 22, 2022.
Dragan, L. (2023). The best over-the-counter hearing aids and other hearing solutions. The New York Times, January 13.
FDA (2022). FDA Finalizes Historic Rule Enabling Access to Over-the-Counter Hearing Aids for Millions of Americans. Available online at: https://www.fda.gov/news-events/press-announcements/fda-finalizes-historic-rule-enabling-access-over-counter-hearing-aids-millions-americans (accessed August 26, 2022).
Federal Register. (2022). Medical Devices; Ear, Nose, and Throat Devices; Establishing Over-the-Counter Hearing Aids. Washington, DC: Federal Register. Available online at: https://www.federalregister.gov/documents/2022/08/17/2022-17230/medical-devicesear-nose-and-throat-devices-establishing-over-the-counter-hearing-aids (accessed August 30, 2022).
Ferguson, M., Brandreth, M., Brassington, W., Leighton, P., and Wharrad, H. A. (2016). randomized controlled trial to evaluate the benefits of a multimedia educational program for first-time hearing aid users. Ear Hear. 37, 123–136. doi: 10.1097/AUD.0000000000000237
Ferguson, M. A., Kitterick, P. T., Chong, L. Y., Edmondson-Jones, M., Barker, F., Hoare, D. J., et al. (2017). Hearing aids for mild to moderate hearing loss in adults. Cochrane Database Syst. Rev. 9, CD012023. doi: 10.1002/14651858.CD012023.pub2
Fuentes-López, E., Fuente, A., Valdivia, G., and Luna-Monsalve, M. (2019). Does educational level predict hearing aid self-efficacy in experienced older adult hearing aid users from Latin America? Validation process of the Spanish version of the MARS-HA questionnaire. PLoS ONE. 14, e0226085. doi: 10.1371/journal.pone.0226085
Girouard, A. (2022). Best Over-the-Counter Hearing Aids for 2022. Aging in Place. Available online at: https://aginginplace.org/hearing-aids/over-the-counter/ (accessed November 16, 2022).
Hearing Loss Association of America (2022). Over-the-Counter Hearing Aids. Available online at: https://www.hearingloss.org/hearing-help/technology/otc-hearing-devices/otc-hearing-aids/ (accessed December 12, 2022).
Humes, L. E., Rogers, S. E., Quigley, T. M., Main, A. K., Kinney, D. L., Herring, C., et al. (2017). The effects of service-delivery model and purchase price on hearing-aid outcomes in older adults: a randomized double-blind placebo-controlled clinical trial. Am. J. Audiol. 26, 53–79. doi: 10.1044/2017_AJA-16-0111
Jilla, A. M., Johnson, C. E., and Huntington-Klein, N. (2020). Hearing aid affordability in the United States. Disabil. Rehabil. Assist. Technol. 18, 246–252. doi: 10.1080/17483107.2020.1822449
Johnson, C. E., Jilla, A. M., Danhauer, J. L., Sullivan, J. C., and Sanchez, K. R. (2018). Benefits from, satisfaction with, and self-efficacy for advanced digital hearing aids in users with mild sensorineural hearing loss. Semin. Hear. 39, 158–171. doi: 10.1055/s-0038-1641742
Klyn, N. A. M., Kleindienst Robler, S., Bogle, J., Alfakir, R., Nielsen, D. W., Griffith, J. W., et al. (2019). CEDRA: a tool to help consumers assess risk for ear disease. Ear Hear. 40, 1261–1266. doi: 10.1097/AUD.0000000000000731
Kuhn, M., Heman-Ackah, S. E., Shaikh, J. A., and Roehm, P. C. (2011). Sudden sensorineural hearing loss. Trends Amplif. 15, 91–105. doi: 10.1177/1084713811408349
Lee, J. W., and Bance, M. L. (2019). Hearing loss. Pract. Neurol. 19, 28–35. doi: 10.1136/practneurol-2018-001926
Lin, F., Yaffe, K., Xia, J., Xue, Q. L., Harris, T. B., Purchase-Helzner, E., et al. (2013). Hearing loss and cognitive decline in older adults. JAMA Intern. Med. 173, 293–299. doi: 10.1001/jamainternmed.2013.1868
Lin, F. R. (2012). Hearing loss in older adults: who's listening? JAMA 307, 1147–1148. doi: 10.1001/jama.2012.321
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 396, 413–446. doi: 10.1016/S0140-6736(20)30367-6
Mackersie, C. L., Boothroyd, A., and Garudadri, H. (2020). Hearing aid self-adjustment: effects of formal speech-perception test and noise. Trends Hear. 24, 2331216520930545. doi: 10.1177/2331216520930545
Reddy, S. (2017). Should Hearing Aids Be Sold Over-the-Counter? Lawmakers consider legislation to allow less expensive hearing aids to be sold over-the-counter. The Wall Street Journal Online, May 1, 2017.
Rijke, W. J., Vermeulen, A. M., Willeboer, C., Knoors, H. E. T., Langereis, M. C., van der Wilt, G. J., et al. (2022). Wellbeing as capability: findings in hearing-impaired adolescents and young adults with a hearing aid or cochlear implant. Front. Psychol. 13, 895868. doi: 10.3389/fpsyg.2022.895868
Sabin, A. T., Van Tasell, D. J., Rabinowitz, B., and Dhar, S. (2020). Validation of a self-fitting method for over-the-counter hearing aids. Trends Hear. 24, 2331216519900589. doi: 10.1177/2331216519900589
Sarangi, L., and Johnson, J. (2022). An exploration of associations between hearing aid self-efficacy and other measurable characteristics of naïve and experienced hearing aid users. Int. J. Audiol. 62, 343–349. doi: 10.1080/14992027.2022.2042607
Saunders, G. H., Dillard, L. K., Zobay, O., Cannon, J. B., and Naylor, G. (2021). Electronic health records as a platform for audiological research: data validity, patient characteristics, and hearing-aid use persistence among 731,213 U.S. Veterans. Ear Hear. 42, 927–940. doi: 10.1097/AUD.0000000000000980
Siber, T. (2022). Hearable Technology Guide: Products, Features, Prices, and More. Hearing Tracker. Available online at: https://www.hearingtracker.com/hearables (accessed November 16, 2022).
Yong, M., Willink, A., McMahon, C., McPherson, B., Nieman, C. L., Reed, N. S., et al. (2019). Access to adults' hearing aids: policies and technologies used in eight countries. Bull. World Health Organ. 97, 699–710. doi: 10.2471/BLT.18.228676
Keywords: hearing loss, hearing, hearing aid (HA), over-the- counter, audiology clinic
Citation: Perez-Heydrich CA, Zenczak C, Roque L, Ryan C, Agrawal Y and Sayyid ZN (2023) The role of hearing professionals for over-the-counter hearing aids. Front. Audiol. Otol. 1:1167853. doi: 10.3389/fauot.2023.1167853
Received: 16 February 2023; Accepted: 06 April 2023;
Published: 25 April 2023.
Edited by:
Z. Jason Qian, Stanford University, United StatesReviewed by:
Melanie Ferguson, Curtin University, AustraliaCopyright © 2023 Perez-Heydrich, Zenczak, Roque, Ryan, Agrawal and Sayyid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlos A. Perez-Heydrich, Y3BlcmV6aDFAamhtaS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.