
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Artif. Intell. , 31 January 2025
Sec. Medicine and Public Health
Volume 8 - 2025 | https://doi.org/10.3389/frai.2025.1455341
Background and aims: Artificial intelligence (AI)-driven medical assistive technology has been widely used in the diagnosis, treatment and prognosis of diabetes complications. Here we conduct a bibliometric analysis of scientific articles in the field of AI in diabetes complications to explore current research trends and cutting-edge hotspots.
Methodology: On April 20, 2024, we collected and screened relevant articles published from 1988 to 2024 from PubMed. Based on bibliometric tools such as CiteSpace, Vosviewer and bibliometix, we construct knowledge maps to visualize literature information, including annual scientific production, authors, countries, institutions, journals, keywords and research hotspots.
Results: A total of 935 articles meeting the criteria were collected and analyzed. The number of annual publications showed an upward trend. Raman, Rajiv published the most articles, and Webster, Dale R had the highest collaboration frequency. The United States, China, and India were the most productive countries. Scientific Reports was the journal with the most publications. The three most frequent diabetes complications were diabetic retinopathy, diabetic nephropathy, and diabetic foot. Machine learning, diabetic retinopathy, screening, deep learning, and diabetic foot are still being researched in 2024.
Conclusion: Global AI research on diabetes complications is expected to increase further. The investigation of AI in diabetic retinopathy and diabetic foot will be the focus of research in the future.
Diabetes is a global disease, and with the large-scale urbanization and aging population, the number of diabetic patients is rapidly increasing. According to the International Diabetes Federation Atlas, by 2045, the global prevalence of diabetes among the 20–79 age group will rise to 12.2% (783.2 million people) (Sun et al., 2022). Diabetes complications are the leading cause of death for diabetic patients, including diabetic retinopathy (DR), diabetic peripheral neuropathies (DPN), diabetic foot (DF), diabetic nephropathy (DN), diabetic cardiomyopathies, hyperglycemic hyperosmolar nonketotic coma, and diabetic ketoacidosis (DKA). As the number of affected individuals continues to rise, diabetes and its complications will consume substantial public health resources and pose numerous economic challenges.
The concept of artificial intelligence (AI) was first proposed in 1955 (Hamet and Tremblay, 2017). It is a highly complex discipline primarily composed of machine learning (ML), deep learning (DL), convolutional neural networks (CNNs), and recurrent neural networks. AI can assist computers in analyzing vast amounts of clinical data, enabling them to learn the most predictive features and establish predictive models, which aid in personalized treatment and improve diagnosis (Sarker, 2022; Jiang et al., 2017). In recent years, AI has been widely applied to the screening (Vaľková et al., 2024; Farahat et al., 2024), treatment and prediction (Kim et al., 2020; Shin et al., 2022) of diabetes complications. It is anticipated that AI-driven precision medicine will be developed in the future to predict and diagnose diabetes complications (Huang et al., 2023). However, there are still challenges in the future in terms of data standardization, interpretability of results, and generalizability to other scenarios (Spasić et al., 2014).
While numerous reviews have been published on the application of AI in diabetes complications, they primarily focus on the early diagnosis, treatment, and prediction of individual complications, such as diagnostic screening of DR (Bai et al., 2024), early detection and prediction of DF ulcers (Wu et al., 2024), and diagnosis and prognosis of DN (Dholariya et al., 2024). A search on PubMed revealed that bibliometric studies in this field are predominantly concentrated on DR (Poly et al., 2023; Wang et al., 2022; Xiao et al., 2023; Shao et al., 2022). Consequently, there is still a lack of systematic review and visualization analysis of AI research in diabetes complications as a whole. Based on this, we conducted a bibliometric analysis and review of literature on AI in diabetes complications to further understand the applications, trends, and future prospects of AI in predicting, diagnosing, and treating diabetes complications.
PubMed, as the most widely used database in the field of medicine, encompasses a vast array of medical literature covering a broad spectrum of knowledge. Moreover, it is freely accessible to all medical professionals. Therefore, we utilized PubMed as the database for conducting Mesh term searches and subsequently performed bibliometric analysis on the retrieved results.
On April 20, 2024, we downloaded the required literature data from the PubMed database using the following search strategy: (“Artificial Intelligence”[Mesh]) AND (“Diabetes Complications”[Mesh]). For our search, we opted for Mesh term searching. The subheadings under AI included: Computer Heuristics, Expert Systems, Fuzzy Logic, Knowledge Bases, Biological Ontologies, Gene Ontology, ML, DL, Supervised Machine Learning, Support Vector Machine, Unsupervised Machine Learning, Natural Language Processing, Neural Networks, Computer, Robotics, Sentiment Analysis. Similarly, the subheadings under Diabetes Complications included: Diabetic Angiopathies, DF, DR, Diabetic Cardiomyopathies, Diabetic Coma, Hyperglycemic Hyperosmolar Nonketotic Coma, DKA, DN, DPN, Fetal Macrosomia. To encompass a wider range of literature, we set the search timeframe from 1988 to 2024. The specific search strategy is outlined in Figure 1.
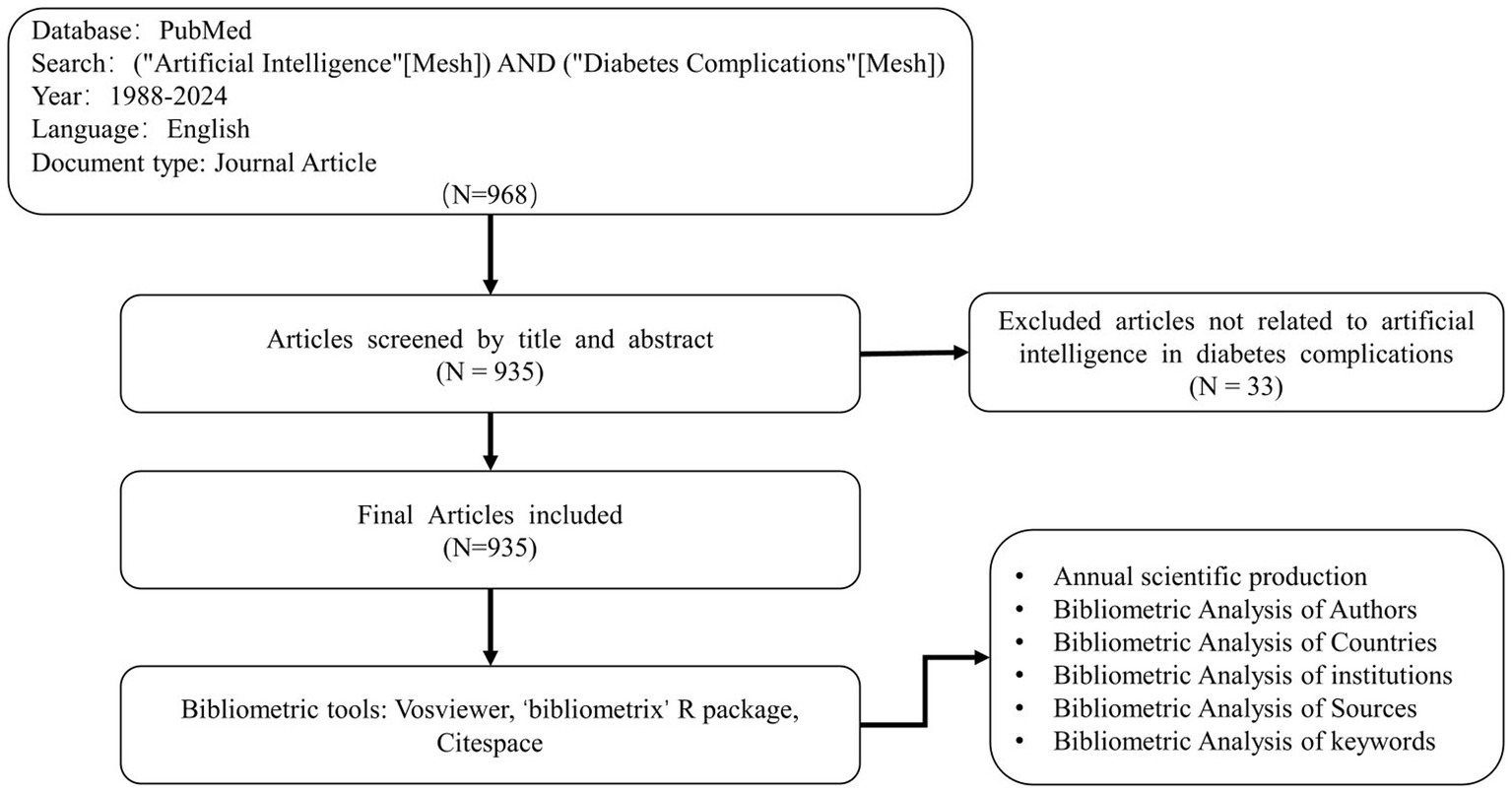
Figure 1. Search flow diagram. The diagram shows details selection criteria for AI related to diabetes complications from PubMed and bibliometric analyses.
Bibliometrics involves analyzing a large volume of literature in a specific field to gain an overall understanding of that domain. Pan et al. (2018) compared 10 bibliometric mapping software tools and the number of web of science papers mentioning these tools in the field in 2018. They found that CiteSpace was the most widely used, with a total of 78 papers, followed by Vosviewer, with 70 papers. Therefore, for this study, we selected CiteSpace and Vosviewer as analysis tools. Additionally, bibliometrix was also utilized, which is a software package in the R language capable of visualizing and analyzing retrieved literature.
A bibliometric analysis was conducted on 935 articles to provide insight into the research landscape of AI in diabetes complications. This analysis included annual scientific production, authors, countries, institutions, journals, keywords and research hotspots.
According to Price Law (De Solla Price, 1963): (m corresponds to minimum number of publications and nmax corresponds to the number of papers by the most prolific authors in a field), we can calculated the minimum number of publications for core authors in a field.
The growth rate of publications was calculated as follows: (where a1 refers to the number of publications in the most recent year, a2 refers to the number of publications in the first year, and n is the number of years) (García-Jaramillo et al., 2024).
Network analysis was used to examine the scientific, social, intellectual, and conceptual structures of scientific production in the field of interest (Omotehinwa, 2022). We conducted network analysis of authors, countries, institutions, and keywords in Vosviewer and CiteSpace. In Vosviewer, each node represents an object (an author/institution/keyword), and the size of the node indicates the frequency of occurrence, and the color of the node represents different clusters. The connections between nodes represent the level of collaboration among objects, referred to as total link strength (TLS) in bibliometric analysis. TLS is primarily determined by factors such as the number of co-authored publications, co-citations, or joint research projects. A stronger connection indicates a higher degree of collaboration or citation relationships. In CiteSpace, the concepts are consistent except for centrality. Centrality signifies the number of shortest paths passing through a node in a network. The purple circle surrounding a node represents the centrality value, with thicker purple circle indicating higher value. A higher centrality value indicates greater influence in communication among other nodes, suggesting higher prominence. Keywords with the strongest burst in citations was used to explore the continuity and variability of research hotspots in the application of AI in diabetes complications from 1988 to the present using CiteSpace.
All original data used in this research were sourced from the publicly accessible PubMed database, therefore no ethical approval was required.
We categorized the retrieved 935 documents into four main classes based on different diabetes complications: DR (695 articles), DPN and DF(96 articles), DN(78 articles), other complications(66 articles).
Based on the analysis of publications retrieved from the PubMed database regarding the application of AI in diabetes complications, a total of 935 articles were selected. These articles originated from 2,748 institutions and were authored by 4,757 authors from 70 countries. They were published across 249 journals. Figure 2 illustrates the temporal distribution of publications in the field of AI for diabetes complications. Overall, the research on the application of AI in diabetes complications began with the publication of the first paper by Wiener (1988) titled “SMR (simulating medical reasoning): an expert shell for non-AI experts” in 1988. The number of publications gradually increased after 2005, with a small growth rate. However, after 2016, there was a significant increase in publications. The number of publications remained consistently above 100 between 2020 and 2023, reaching its peak in 2022 with 183 publications. We calculated the growth rate of publications for this topic to be approximately 15% based on the number of articles published in 2023 as the most recent year. This indicates sustained interest among scholars in this research area, gradually establishing it as a new hotspot in the field of diabetes complications research.
A total of 4,757 authors have published articles related to the research on AI in diabetes complications. Among them, 4,086 authors have published only one article, accounting for 85.9%, while 671 authors have published two or more articles, accounting for 14.1%. The minimum number of publications for core authors in this field is approximately 2.9. Authors who have published three or more articles (including three articles) are identified as core authors in this field, totaling 224 individuals. Figure 3 illustrates a co-authorship network map of core authors. Among these core authors, connections exist between some of them. Table 1 presents the top 16 productive authors and TLS. The top three most productive authors are Raman, Rajiv (publication = 15, TLS = 61), Webster, Dale R (publication = 11, TLS = 102), and Cuadros, Jorge (publication = 11, TLS = 68). The top three authors with the highest TLS are Webster, Dale R (publication = 11, TLS = 102), Peng, Lily (publication = 10, TLS = 93), and Corrado, Greg S (publication = 8, TLS = 76). It is noteworthy that Webster, Dale R has a significant number of publications and the tightest connections, indicating substantial academic contributions in this field and extensive collaboration with other authors.
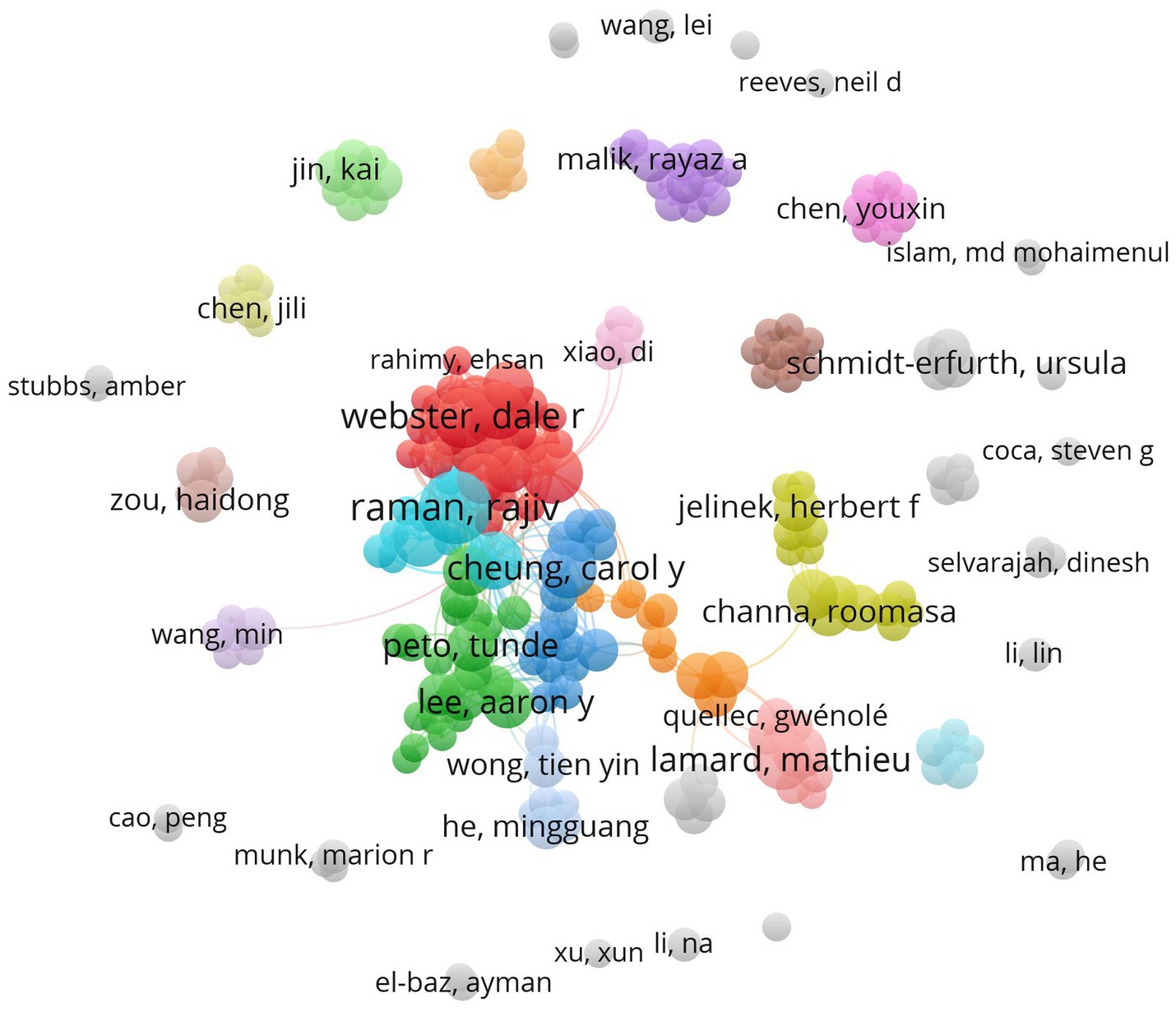
Figure 3. Co-authorship network map of core authors. Each node in the map represents a core author, and the size of the node corresponds to the author’s productivity (i.e., the number of publications). The lines connecting the nodes illustrate the collaboration between the authors, with the thickness of the links indicating the level of collaboration between them.
The United States leads in publication output, with 200 articles published, accounting for 21.39% of the included research articles. China and India follow closely with 190 and 80 articles, respectively, placing second and third. Additionally, the United States has the highest centrality (0.86), followed by China (0.29) and Australia (0.16) (Figure 4; Table 2). The United States is considered the most influential country in this field. It’s noteworthy that although Australia ranks sixth in publication output, it ranks third in centrality, indicating that articles published by Australia have considerable influence.
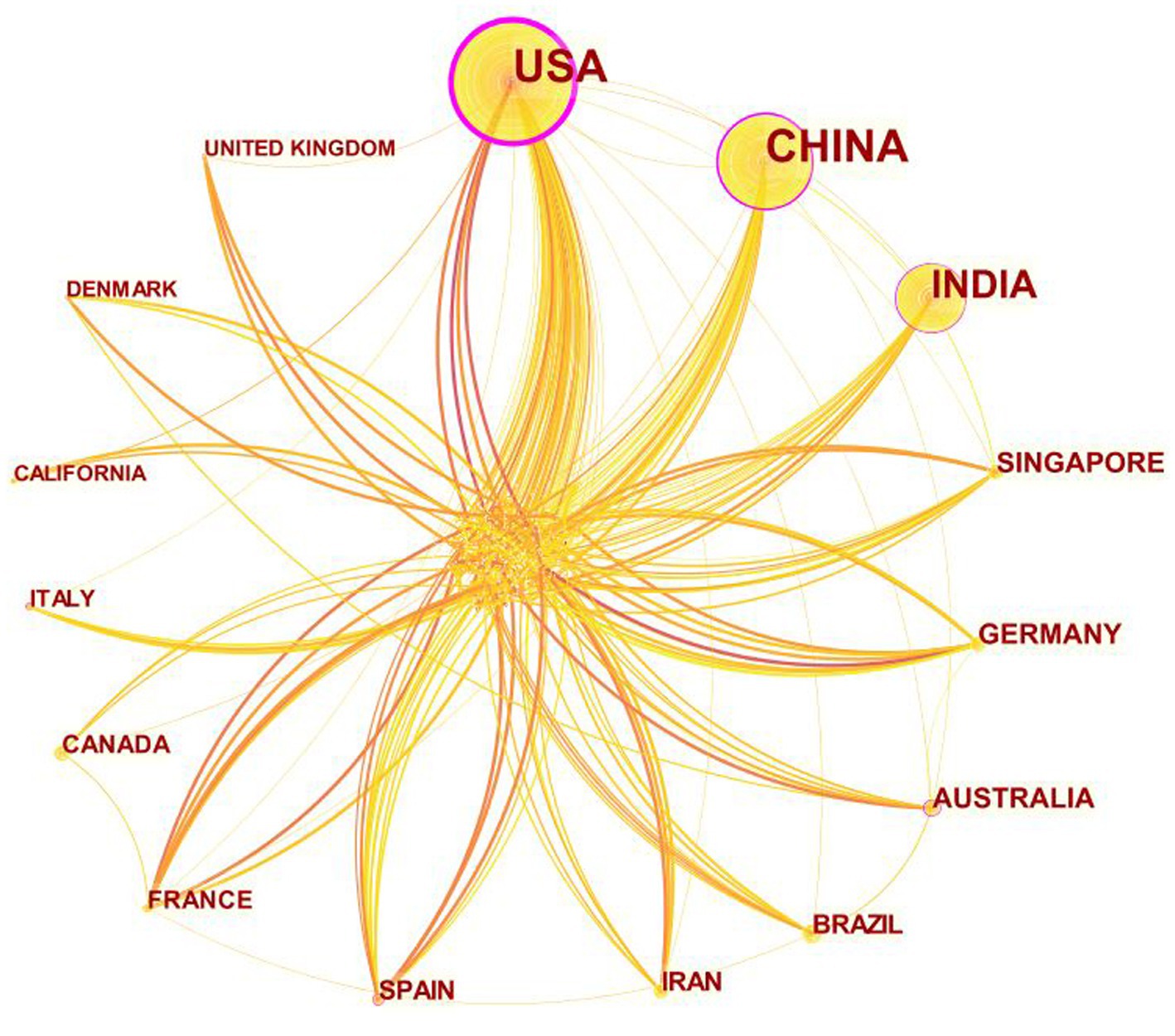
Figure 4. Cooperation of Countries that contributed to publications on the use of AI in diabetes complications from 1988 to 2024. Each yellow node represents a country. The yellow lines connecting the nodes illustrate the collaboration between the countries, with the thickness of the links indicating the level of collaboration between them. The purple circle surrounding a node represents the centrality value, with thicker purple circle indicating higher value.
A total of 2,748 institutions worldwide have participated in research on AI in diabetes complications. 30 institutions have published more than 3 articles. It can be observed that there is relatively little collaboration among institutions, and the overall distribution of institutions is quite scattered from Figure 5. The largest institutional collaboration cluster is the red cluster centered around Google Health. Table 3 presents the top 10 productive institutions and TLS. The institutions with the highest number of publications are Google Health (5), Department of Electrical Engineering, Qatar University (5), NIHR Biomedical Research Centre (4), Department of Ophthalmology and Optometry, Medical University of Vienna (4), and Zhongshan Ophthalmic Center, Sun Yat-Sen University (4). The remaining 5 institutions have a publication output of 3 articles each. In terms of TLS, Google Health ranks first with a value of 5, while Qatar, Austria, China, and Singapore have a TLS of 0. The remaining institutions all have a TLS of 3. It is noteworthy that among the top 10 research institutions ranked by publication output, three institutions are from the United States, highlighting the dominant position of the United States in the field.
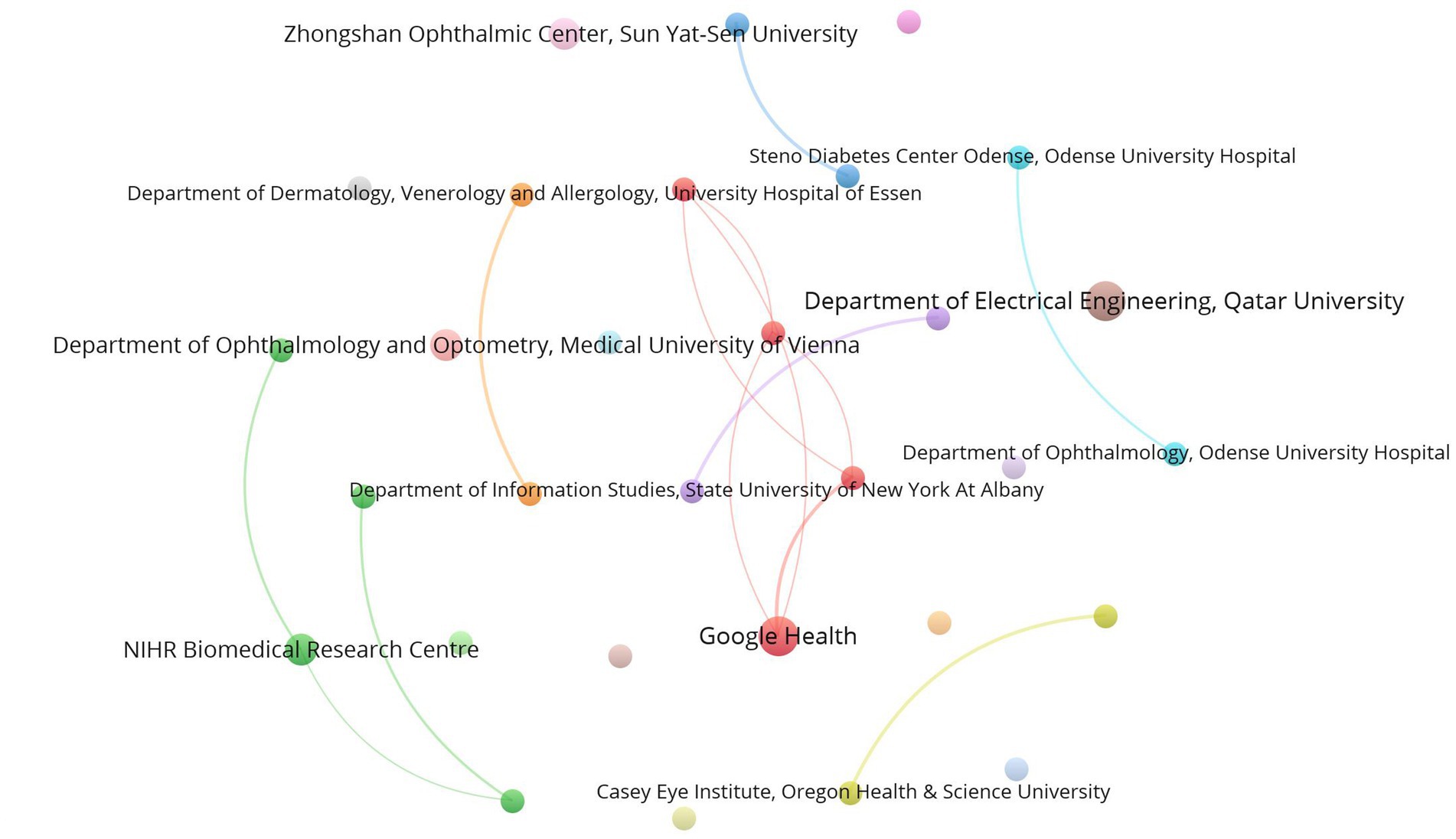
Figure 5. Co-authorship Network Map of Institutions. These 30 institutions have been divided into 19 clusters with 14 links and a total link strength of 27. Each node represents an institution, and its size indicates its productivity. The lines connecting the nodes depict their collaboration, and the thickness of the links represents the level of collaboration.
A total of 249 different journals have published articles related to AI in diabetes complications. Thirteen core journals are shown in Figure 6. Table 4 presents detailed information on 13 core journals, including the number of publications, journal impact factor (JIF), h-index, and cite-score. Scientific Reports leads with 45 publications, followed by IEEE Transactions on Biomedical Engineering with 43 publications, and Sensors-Basel with 30 publications, ranking second and third, respectively. Medical Image Analysis has the highest JIF at 10.9, followed by Computers in Biology and Medicine and IEEE Journal of Biomedical and Health Informatics, both at 7.7. The journals with the highest h-index are PLoS One (332), Scientific Reports (213), and IEEE Transactions on Biomedical Engineering (200). Medical Image Analysis leads with a cite-score of 19.9, followed by IEEE Journal of Biomedical and Health Informatics (11.9) and Journal of Medical Systems (11.8).
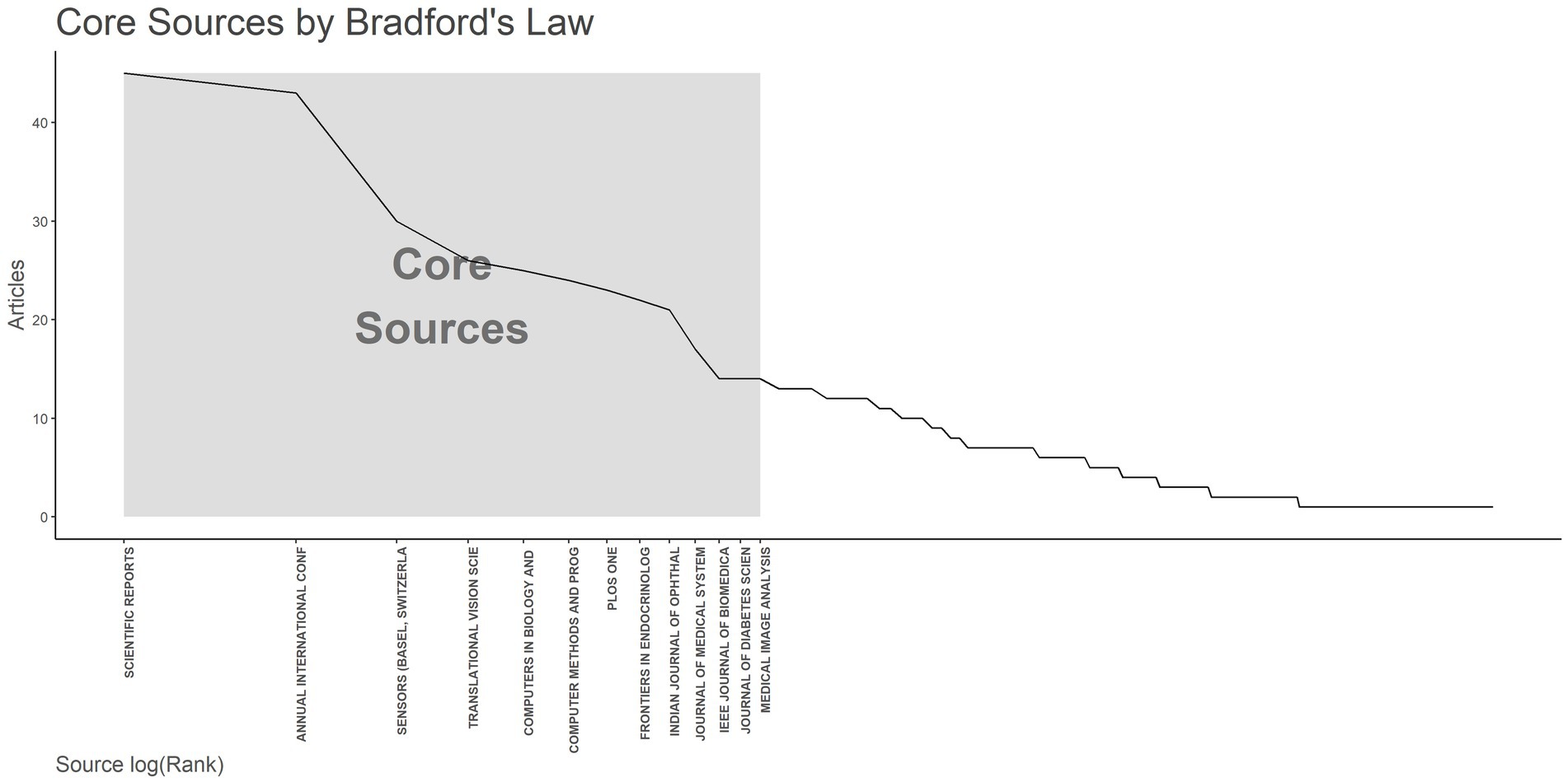
Figure 6. Core Journals by Bradford’s law. The x-axis represents the journal names, and the y-axis represents the number of publications. The gray area represents core journals, totaling 13.
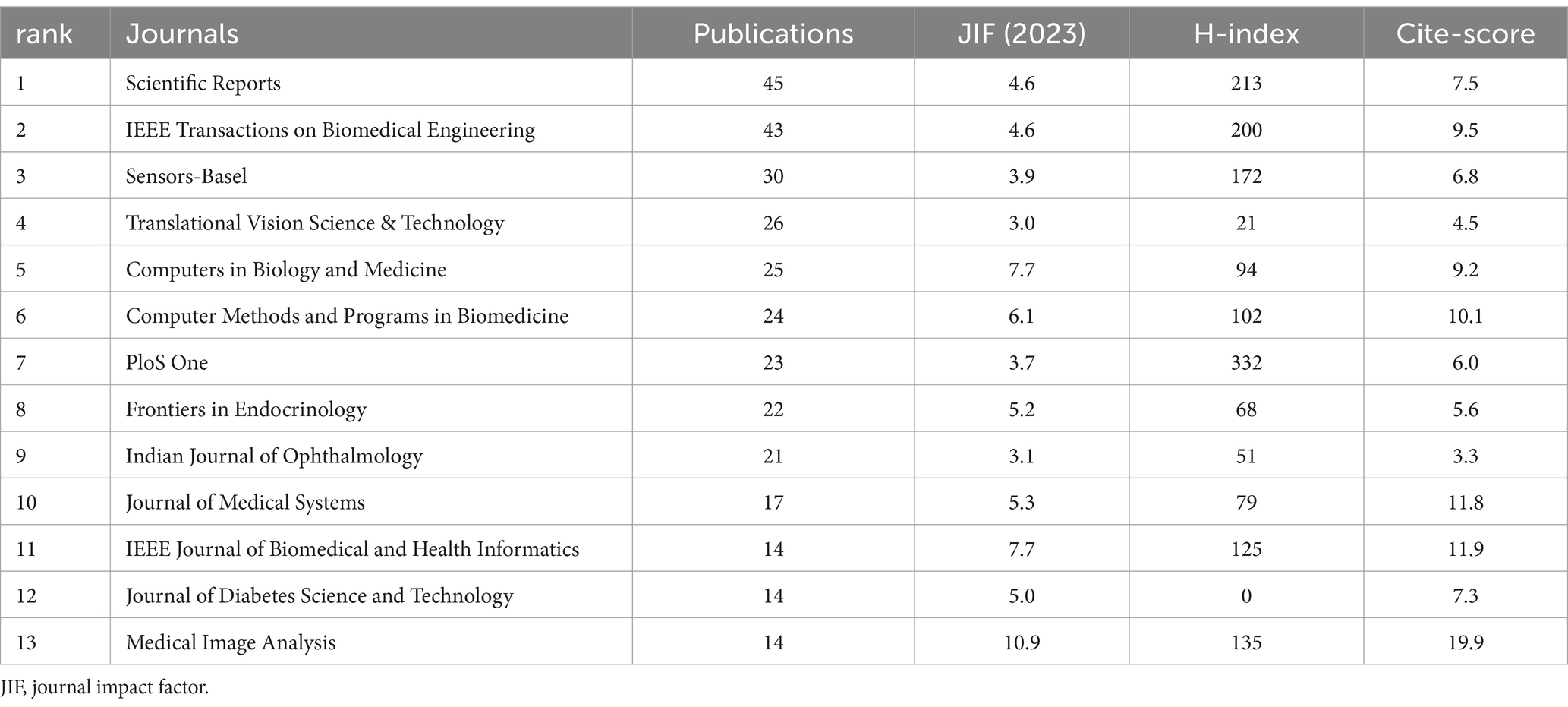
Table 4. Top 13 core journals by publication productivity, journal impact factor, h-index, cite-score.
We conducted a co-occurrence analysis of author keywords for the retrieved 935 documents in Vosviewer, revealing a total of 1,182 keywords, of which 48 keywords appear more than 5 times. The visual network map of these 48 keywords is shown in Figure 7. The largest nodes in the graph are DR, followed by DL, AI, and ML, with DR and DL belonging to the yellow cluster, suggesting widespread application of DL in DR. Additionally, we selected the top 10 keywords based on frequency of occurrence, as shown in Table 5. The three most frequent diabetes complications are DR (Occurrences = 260, TLS = 457), DN (Occurrences = 28, TLS = 34), and DF (Occurrences = 26, TLS = 54). Notably, publications on DR have the earliest average publication year (2021), while those on the latter two have relatively later publication years (2022).

Figure 7. Author keywords co-occurrence network map. These 48 author keywords have been divided into 6 clusters with 341 links and a total link strength of 1,318. Each node represents an author keyword, and its size indicates the frequency of keyword occurrence. The lines connecting the nodes represent the cooccurrence relationship, and the thickness of the links represents the level of collaboration.
The top 15 keywords with the strongest burst in citations are shown in Figure 8. It can be observed that the field is continually developing and maturing over time. DL has the highest strength, mainly concentrated in 2020. Natural language processing and retina rank second and third, respectively, with natural language processing having the earliest appearance (2013–2015) and retina having the latest appearance (2023–2024). The remaining keywords have burst intensities below 3.0. Retinal image and exudate have the longest durations, spanning 5 years.
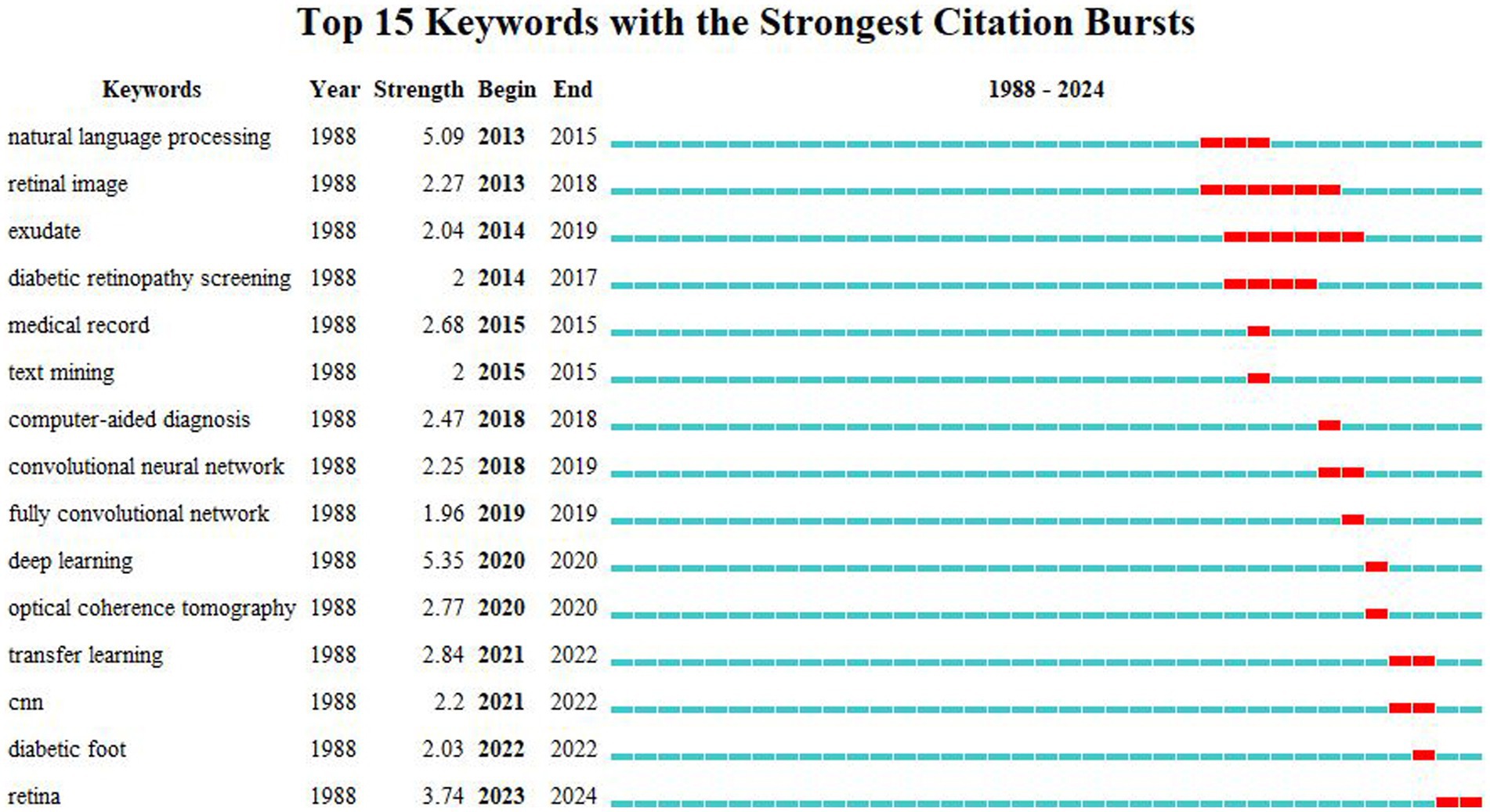
Figure 8. Top 15 keywords with the strongest citation bursts. The blue lines represent the base timeline, while the red segments represent the duration of the keyword burst, and the two endpoints correspond to the beginning and end times of the burst.
Furthermore, we conducted keyword timeline maps analysis for closely related and similar keywords in the field of AI in diabetes complications, as shown in Figure 9. Each horizontal line represents a cluster, and a total of 10 clusters have been researched since 2013. Clusters #0 ML, #1 DR, #2 screening, #4 DL, and #8 DF are still being researched in 2024, indicating that these topics are the focus of research in the field in the future.

Figure 9. Timeline view based on cluster analysis. Each horizontal timeline represents a cluster, which is named after the most prominent node in each timeline, and nodes on the timeline represents keywords. The lines connecting the nodes represent the cooccurrence relationship, and the thickness of the links represents the level of collaboration. The timeline from left to right corresponds to 2013–202.
To the best of our knowledge, this study is the first comprehensive bibliometric analysis of the application of AI in the field of diabetes complications. Unlike focusing on diabetes, this study focuses on the serious diabetes complications, covering all AI technologies, providing researchers with a broader perspective.
It can be observed that the research on AI in diabetes complications is becoming more and more extensive, and the number of published papers is increasing year by year, which is mainly due to the rapid development of emerging industries and the rapid progress of AI-assisted medical technology, which also highlights the huge potential of AI in healthcare applications. In this research field, the United States and China rank among the top in terms of the number of publications, international influence, and number of publishing institutions, which is closely related to the high level of science and technology development and the huge investment of the two countries. As one of the world’s leading countries in the development of AI, the United States has strong scientific and technological strength, educational background, investment environment and policy support in the field of AI. And for China, the huge population base is one of the key factors. At the same time, there are some differences in AI research on diabetes complications between the two countries. The United States focuses on precision medicine, technological innovation, and the development of high-end equipment, with an emphasis on developing decision support systems that can be applied clinically. For example, the United States has developed various AI-based decision support systems to optimize insulin dosage calculations and monitor diabetic complications (Li et al., 2020). In contrast, China places greater emphasis on the accessibility, cost-effectiveness, and coverage of primary healthcare services by AI, considering the practical needs of large-scale populations. For instance, Professor Huang Tianyin, in collaboration with teams from Shanghai Jiao Tong University and the National University of Singapore, has developed DeepDR-LLM, an integrated visual-large language model system, which can effectively improve DR screening and diabetes management at the grassroots level (Li et al., 2024). In the future, international cooperation should be further strengthened, combining large-scale data from China and cutting-edge technology from the United States to jointly promote the overall progress in the field of AI in diabetes complications (Sheng et al., 2024). In addition, the overall distribution of authors in this field is uneven, and the denser places form unique academic clusters, and the relationship between authors is not very close, which suggests that scholars in this field need more academic exchanges and closer academic cooperation in the future.
It is worth noting that the most rapid development of AI applications is in DR. On the one hand, this is made possible by the public Kaggle dataset (Kaggle, 2015) containing 100,000 retinal images. A number of algorithms have been developed by applying this dataset, which has given a huge boost to the development of AI. On the other hand, this is attributed to the increase in computer power and the application of CNNs and other DL techniques, which serve as assisting technologies capable of automatically screening DR from fundus photographs without manual input, exhibiting high sensitivity and specificity (>85%) (Rajesh et al., 2023). Our study also found that DR and DL are the two most frequently used terms and have the strongest citation bursts, further illustrating the high level of interest in both within this research area. Ahmed and Thrishulamurthy (2023) discussed the current research status of OCT imaging and CNNs integration for DR diagnosis, suggesting its transformative potential in DR diagnosis, facilitating early intervention, personalized treatment, and improving patient prognosis. By 2021, the FDA had approved the use of multiple AI-based DR screening systems for clinical application, such as IDx-DR and EyeArt (Abràmoff et al., 2018; Bhaskaranand et al., 2019). Furthermore, Dai et al. (2024) trained and validated a DL system named DeepDR Plus, using multi-ethnic datasets, demonstrating its capability to predict individualized risk and the time to DR progression within 5 years, thus enabling personalized screening intervals. Studies suggest that by 2030, AI algorithms will be applied in numerous large-scale DR screenings worldwide, either as fully autonomous systems or in hybrid systems where algorithms function as assistive tools (Xie et al., 2020). As AI image recognition algorithms become increasingly accurate, the diagnosis of DR will become more precise, significantly alleviating screening burdens.
Early identification of risk factors for DPN and appropriate interventions can greatly delay the occurrence and development of DF. AI can help establish well-performing DPN risk prediction models to determine the most closely related risk factors for DPN. Lian et al. (2023) based on data from 1,278 diabetic patients, trained six ML models [logistic regression, k-nearest neighbor, decision tree, naive bayes, random forest (RF), and extreme gradient boosting (XGBoost)], finding that the XGBoost model outperformed others. Besides, AI is also crucial for DPN screening and diagnosis.
DF is a multifactorial severe complication more suitable for AI analysis and auxiliary diagnosis (Howard et al., 2023). To identify clinical and biochemical risk factors for DF, Nanda et al. (2022) analyzed patients with and without DF using various ML algorithms, discovering new risk factors for DF. They also proposed that the decision fusion strategy of the Stacking C algorithm improves prediction accuracy and can be used as a supplementary method for DF and its subtypes calculation. Moreover, Sharma et al. (2023) successfully developed a thermal DF dataset, effectively classifying the severity of DF using conventional ML and CNNs technologies, enhancing the detection and management of DF, and effectively improving patient prognosis. Although the current advanced ML algorithms can also detect, locate and segment the DF image to determine whether it contains diabetic foot ulcer, how to predict the occurrence of DF is a challenge. To do this, a large dataset of images annotated by specialists is needed for AI to learn and develop more advanced algorithms. Basiri et al. (2024) established a comprehensive dataset named Zivot, laying the foundation for further exploration of holistic and multimodal approaches to DF research. In addition, more and more researches are using AI to predict the risk of ulcers (Xiaoling et al., 2024; Hong et al., 2024), sepsis (Matsinhe et al., 2024) and amputation (Oei et al., 2024; Demirkol et al., 2024) in DF patients. In the future, more attention will continue to be paid to the diagnosis, classification, and prediction of DPN and DF, providing continuous health care for patients.
Early detection of DN is crucial to prevent its progression to renal failure. By performing a keyword network analysis, we found that there is a strong connection between DN and biomarkers. Although some biomarkers for DN have been identified, none are sufficiently reliable for accurate diagnosis and prognosis prediction. To address this challenge, researchers have focused on identifying DN-related biomarkers and elucidating their pathogenic mechanisms, leading to the development of novel diagnostic and therapeutic approaches. At present, some valuable hub genes have been identified—FSTL1, CX3CR1, and AGR2 (Chen et al., 2024); VWF and DNASE1L3 (Dong et al., 2024); G6PC and HSD17B14 (Bi et al., 2024)— as innovative diagnostic biomarkers and therapeutic targets for DN by applying different AI methods. Furthermore, some researchers have utilized AI algorithms to predict the progression of DN in susceptible patients, enhancing early detection rates. Yin et al. (2024) demonstrated that XGBoost had the best performance in screening DN, highlighting the critical role of the least absolute shrinkage and selection operator (LASSO) in model selection accuracy and stability. In the future, with continued advancements in AI algorithms, researchers aim to develop more precise algorithmic models to aid in the discovery of new highly specific biomarkers, facilitating early diagnosis and treatment of DN.
In addition to the three most common diabetic complications discussed above, AI can also assist in diagnosing and treating other complications such as diabetic cardiomyopathies and DKA. Diabetic cardiomyopathy is one of the leading causes of increased mortality in diabetic patients. Predicting the progression of diabetic cardiomyopathy using ML algorithms combined with multiple cardiac biomarkers can facilitate early intervention (Segar et al., 2024; Irlik et al., 2024). DKA is a life-threatening but preventable acute diabetes complication. Both conventional ML (logistic regression and LASSO) and flexible ML (XGBoost, RF and feedforward network) methods can identify overlapping but distinct risk factors for DKA (Li et al., 2021). Future research on these complications will continue to focus on identifying more highly specific biomarkers, integrating AI for efficient identification, and intervening in treatment during the early stages of the disease, thereby significantly reducing mortality and disability rates for patients.
At present, DL is one of the most widely used AI research methods in the field of diabetes complications, and commonly used models include: logistic regression, LASSO, k-nearest neighbor, decision tree, naive bayes, RF, and XGBoost. A commonly used type of data is unstructured data (images). For the dimensions of the data, the higher the dimension, the more features it contains, but at the same time, it will lead to a decrease in the performance of the model unless the sample size increases accordingly. The accuracy of a model depends primarily on the size of the training data and the quality of the algorithms employed. Although various databases currently exist [e.g., NCBI, EyePACS (Wang et al., 2024), Global Diabetes Atlas, DIARETDB1 (Kauppi et al., 2007), https://d2h2.maayanlab.cloud/, etc.], there are still some challenges to data quality and consistency. Firstly, missing values and noisy data. There may be missing values or measurement errors in diabetes complications data, reducing the accuracy of the models. Secondly, the data is not standardized enough. Data formats, recording methods, and indicator ranges may not be uniform across different medical institutions and devices, making it difficult to integrate and analyze data. Thirdly, there is a shortage of high-quality annotated data. Labeling medical data, such as lesion markers in imaging data, requires expert involvement, which is time-consuming and costly. Finally, due to patient privacy protection, factors such as racial, gender, and regional differences, and uneven disease distribution make it more difficult to obtain large-scale, high-quality data.
In terms of model performance and adaptability, it often faces problems such as insufficient generalization ability, overfitting risks, and complexity and interpretability of the models. AI algorithms are often considered “black boxes” (Chun and Kim, 2023) with opaque decision-making, making it difficult for doctors and patients to understand their decision-making logic. Based on this, new research has emerged in the direction of explainable AI. For example, Srinivasu PN et al. proposed an explainable diabetes prediction AI software system, XAI, which can effectively identify individuals with elevated blood glucose levels and explain expected outcomes and decision-making models (Srinivasu et al., 2024). Similarly, Hendawi R et al. developed the XAI4Diabetes framework, providing transparent and interpretable explanations for the diabetes prediction process and prediction outcomes, enhancing trust in AI predictions (Hendawi et al., 2023). However, more studies are needed on explainable deep learning for diabetes diagnosis with DeepNetX2. In the future, it is necessary to further strengthen the research in the direction of explainable AI to make its decision-making process more transparent and understandable.
In addition, ethics and fairness are another major challenge for AI. In AI research, it is necessary to place greater emphasis on data privacy protection and ethical issues, ensuring the security and confidentiality of patient data during storage and processing. At the same time, attention should be paid to whether AI systems have fully considered differences in race, gender, and economic status during design and training, so as to avoid exacerbating the unfair distribution of medical resources.
Although AI is widely used in the diagnosis, treatment and prevention of diabetes complications and there are many literatures, there is a lack of systematic analysis. This study aims to address this gap by conducting a comprehensive and detailed bibliometric analysis of these publications using various analytical tools. However, it is important to acknowledge that there are still some limitations to this study. Firstly, we only selected the PubMed database for bibliometric analysis, which is popular in medicine and widely accepted for bibliometric analysis. However, there is a possibility that some studies were not included, potentially affecting the research findings. Secondly, we only selected articles in the English language category without analyzing or statistically evaluating articles in other language categories, introducing potential selection bias. Thirdly, citation analysis was not performed in this study as the data downloaded from the PubMed did not include citation data.
Over the past few decades, there has been a steady increase in the number of publications related to the research of AI in diabetes complications. The investigation of AI in DR and DF will be future research hotspots and frontier. This area of study can be further promoted by enhancing cooperation between countries, institutions, and authors. According to the current growth trend, it is expected that global research on AI applications in diabetes complications will be increased further. Future research will further focus on the clinical application of AI in the diagnosis, treatment, and prediction of diabetes complications. These findings can assist researchers in identifying future research directions and provide valuable insights and references for scholars.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Ethics Committee of Air Force Medical Center. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
YT: Writing – original draft, Writing – review & editing. JH: Writing – original draft. GZ: Writing – original draft. DZ: Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by a grant from the Clinical Trial Project of Air Force Medical Center (2021LC018).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abràmoff, M. D., Lavin, P. T., Birch, M., Shah, N., and Folk, J. C. (2018). Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ Digit. Med. 1:39. doi: 10.1038/s41746-018-0040-6
Ahmed, H. S., and Thrishulamurthy, C. J. (2023). Advancing diabetic retinopathy diagnosis: leveraging optical coherence tomography imaging with convolutional neural networks. Rom. J. Ophthalmol. 67, 398–402. doi: 10.22336/rjo.2023.63
Bai, P., Beversluis, C., Song, A., Alicea, N., Eisenberg, Y., Layden, B., et al. (2024). Opportunities to apply human-centered Design in Health Care with Artificial Intelligence-based Screening for diabetic retinopathy. Int. Ophthalmol. Clin. 64, 5–8. doi: 10.1097/IIO.0000000000000531
Basiri, R., Manji, K., LeLievre, P. M., Toole, J., Kim, F., Khan, S. S., et al. (2024). Protocol for metadata and image collection at diabetic foot ulcer clinics: enabling research in wound analytics and deep learning. Biomed. Eng. Online 23:12. doi: 10.1186/s12938-024-01210-6
Bhaskaranand, M., Ramachandra, C., Bhat, S., Cuadros, J., Nittala, M. G., Sadda, S. R., et al. (2019). The value of automated diabetic retinopathy screening with the EyeArt system: a study of more than 100,000 consecutive encounters from people with diabetes. Diabetes Technol. Ther. 21, 635–643. doi: 10.1089/dia.2019.0164
Bi, Z., Wang, L. J., Lin, Y. X., Zhang, Y. Y., Wang, S. H., and Fang, Z. H. (2024). Development of a clinical prediction model for diabetic kidney disease with glucose and lipid metabolism disorders based on machine learning and bioinformatics technology. Eur. Rev. Med. Pharmacol. Sci. 28, 863–878. doi: 10.26355/eurrev_202402_35324
Chen, Y., Liao, L., Wang, B., and Wu, Z. (2024). Identification and validation of immune and cuproptosis - related genes for diabetic nephropathy by WGCNA and machine learning. Front. Immunol. 15:1332279. doi: 10.3389/fimmu.2024.1332279
Chun, J. W., and Kim, H. S. (2023). The present and future of artificial intelligence-based medical image in diabetes mellitus: focus on analytical methods and limitations of clinical use. J. Korean Med. Sci. 38:e253. doi: 10.3346/jkms.2023.38.e253
Dai, L., Sheng, B., Chen, T., Wu, Q., Liu, R., Cai, C., et al. (2024). A deep learning system for predicting time to progression of diabetic retinopathy. Nat. Med. 30, 584–594. doi: 10.1038/s41591-023-02702-z
Demirkol, D., Erol, Ç. S., Tannier, X., Özcan, T., and Aktaş, Ş. (2024). Prediction of amputation risk of patients with diabetic foot using classification algorithms: a clinical study from a tertiary center. Int. Wound J. 21:e14556. doi: 10.1111/iwj.14556
Dholariya, S., Dutta, S., Sonagra, A., Kaliya, M., Singh, R., Parchwani, D., et al. (2024). Unveiling the utility of artificial intelligence for prediction, diagnosis, and progression of diabetic kidney disease: an evidence-based systematic review and meta-analysis. Curr. Med. Res. Opin. 40, 2025–2055. doi: 10.1080/03007995.2024.2423737
Dong, B., Liu, X., and Yu, S. (2024). Utilizing machine learning algorithms to identify biomarkers associated with diabetic nephropathy: a review. Medicine (Baltimore) 103:e37235. doi: 10.1097/MD.0000000000037235
Farahat, Z., Zrira, N., Souissi, N., Bennani, Y., Bencherif, S., Benamar, S., et al. (2024). Diabetic retinopathy screening through artificial intelligence algorithms: a systematic review. Surv. Ophthalmol. 69, 707–721. doi: 10.1016/j.survophthal.2024.05.008
García-Jaramillo, M., Luque, C., and León-Vargas, F. (2024). Machine learning and deep learning techniques applied to diabetes research: a bibliometric analysis. J. Diabetes Sci. Technol. 18, 287–301. doi: 10.1177/19322968231215350
Hamet, P., and Tremblay, J. (2017). Artificial intelligence in medicine. Metabolism 69, S36–S40. doi: 10.1016/j.metabol.2017.01.011
Hendawi, R., Li, J., and Roy, S. (2023). A Mobile app that addresses interpretability challenges in machine learning-based diabetes predictions: survey-based user study. JMIR Form. Res. 7:e50328. doi: 10.2196/50328
Hong, S., Chen, Y., Lin, Y., Xie, X., Chen, G., Xie, H., et al. (2024). Personalized prediction of diabetic foot ulcer recurrence in elderly individuals using machine learning paradigms. Technol. Health Care 32, 265–276. doi: 10.3233/THC-248023
Howard, T., Ahluwalia, R., and Papanas, N. (2023). The advent of artificial intelligence in diabetic foot medicine: a new horizon, a new order, or a false Dawn? Int J Low Extrem Wounds 22, 635–640. doi: 10.1177/15347346211041866
Huang, J., Yeung, A. M., Armstrong, D. G., Battarbee, A. N., Cuadros, J., Espinoza, J. C., et al. (2023). Artificial intelligence for predicting and diagnosing complications of diabetes. J. Diabetes Sci. Technol. 17, 224–238. doi: 10.1177/19322968221124583
Irlik, K., Aldosari, H., Hendel, M., Kwiendacz, H., Piaśnik, J., Kulpa, J., et al. (2024). Artificial intelligence-enhanced electrocardiogram analysis for identifying cardiac autonomic neuropathy in patients with diabetes. Diabetes Obes. Metab. 26, 2624–2633. doi: 10.1111/dom.15578
Jiang, F., Jiang, Y., Zhi, H., Dong, Y., Li, H., Ma, S., et al. (2017). Artificial intelligence in healthcare: past, present and future. Stroke Vasc. Neurol. 2, 230–243. doi: 10.1136/svn-2017-000101
Kaggle (2015). Your machine learning and data science community. Available at: https://www.kaggle.com/ (Accessed July 22, 2022).
Kauppi, T, Kalesnykiene, V, Kamarainen, JK, Lensu, L, Sorri, I, Raninen, A, et al. (2007). “The diaretdb1 diabetic retinopathy database and evaluation protocol.” in Proceedings of the British machine vision conference. BMVA Press. 15.1–15.10.
Kim, R. B., Gryak, J., Mishra, A., Cui, C., Soroushmehr, S. M. R., Najarian, K., et al. (2020). Utilization of smartphone and tablet camera photographs to predict healing of diabetes related foot ulcers. Comput. Biol. Med. 126:104042. doi: 10.1016/j.compbiomed.2020.104042
Li, J., Guan, Z., Wang, J., Cheung, C. Y., Zheng, Y., Lim, L. L., et al. (2024). Integrated image-based deep learning and language models for primary diabetes care. Nat. Med. 30, 2886–2896. doi: 10.1038/s41591-024-03139-8
Li, J., Huang, J., Zheng, L., and Li, X. (2020). Application of artificial intelligence in diabetes education and management: present status and promising Prospect. Front. Public Health 8:173. doi: 10.3389/fpubh.2020.00173
Li, L., Lee, C. C., Zhou, F. L., Molony, C., Doder, Z., Zalmover, E., et al. (2021). Performance assessment of different machine learning approaches in predicting diabetic ketoacidosis in adults with type 1 diabetes using electronic health records data. Pharmacoepidemiol. Drug Saf. 30, 610–618. doi: 10.1002/pds.5199
Lian, X., Qi, J., Yuan, M., Li, X., Wang, M., Li, G., et al. (2023). Study on risk factors of diabetic peripheral neuropathy and establishment of a prediction model by machine learning. BMC Med. Inform. Decis. Mak. 23:146. doi: 10.1186/s12911-023-02232-1
Matsinhe, C., Kagodora, S. B., Mukheli, T., Mokoena, T. P., Malebati, W. K., Moeng, M. S., et al. (2024). Machine learning algorithm-aided determination of predictors of mortality from diabetic foot Sepsis at a regional Hospital in South Africa during the COVID-19 pandemic. Medicina (Kaunas) 60:1718. doi: 10.3390/medicina60101718
Nanda, R., Nath, A., Patel, S., and Mohapatra, E. (2022). Machine learning algorithm to evaluate risk factors of diabetic foot ulcers and its severity. Med. Biol. Eng. Comput. 60, 2349–2357. doi: 10.1007/s11517-022-02617-w
Oei, C. W., Chan, Y. M., Zhang, X., Leo, K. H., Yong, E., Chong, R. C., et al. (2024). Risk prediction of diabetic foot amputation using machine learning and explainable artificial intelligence. J. Diabetes Sci. Technol. 570837822:8606. doi: 10.1177/19322968241228606
Omotehinwa, T. O. (2022). Examining the developments in scheduling algorithms research: a bibliometric approach. Heliyon 8:e09510. doi: 10.1016/j.heliyon.2022.e09510
Pan, X., Yan, E., Cui, M., and Hua, W. (2018). Examining the usage, citation, and diffusion patterns of bibliometric mapping software: a comparative study of three tools. J. Informet. 12, 481–493. doi: 10.1016/j.joi.2018.03.005
Poly, T. N., Islam, M. M., Walther, B. A., Lin, M. C., and Jack Li, Y. C. (2023). Artificial intelligence in diabetic retinopathy: bibliometric analysis. Comput. Methods Prog. Biomed. 231:107358. doi: 10.1016/j.cmpb.2023.107358
Rajesh, A. E., Davidson, O. Q., Lee, C. S., and Lee, A. Y. (2023). Artificial intelligence and diabetic retinopathy: AI framework, prospective studies, head-to-head validation, and cost-effectiveness. Diabetes Care 46, 1728–1739. doi: 10.2337/dci23-0032
Sarker, I. H. (2022). Ai-based modeling: techniques, applications and research issues towards automation, intelligent and smart systems. SN Comput. Sci. 3, 1–20. doi: 10.1007/s42979-022-01043-x
Segar, M. W., Usman, M. S., Patel, K. V., Khan, M. S., Butler, J., Manjunath, L., et al. (2024). Development and validation of a machine learning-based approach to identify high-risk diabetic cardiomyopathy phenotype. Eur. J. Heart Fail. 26, 2183–2192. doi: 10.1002/ejhf.3443
Shao, A., Jin, K., Li, Y., Lou, L., Zhou, W., and Ye, J. (2022). Overview of global publications on machine learning in diabetic retinopathy from 2011 to 2021: bibliometric analysis. Front. Endocrinol. 13:1032144. doi: 10.3389/fendo.2022.1032144
Sharma, N., Mirza, S., Rastogi, A., Singh, S., and Mahapatra, P. K. (2023). Region-wise severity analysis of diabetic plantar foot thermograms. Biomed Tech (Berl) 68, 607–615. doi: 10.1515/bmt-2022-0376
Sheng, B., Pushpanathan, K., Guan, Z., Lim, Q. H., Lim, Z. W., Yew, S. M. E., et al. (2024). Artificial intelligence for diabetes care: current and future prospects. Lancet Diabetes Endocrinol. 12, 569–595. doi: 10.1016/S2213-8587(24)00154-2
Shin, J., Kim, J., Lee, C., Yoon, J. Y., Kim, S., Song, S., et al. (2022). Development of various diabetes prediction models using machine learning techniques. Diabetes Metab. J. 46, 650–657. doi: 10.4093/dmj.2021.0115
Spasić, I., Livsey, J., Keane, J. A., and Nenadić, G. (2014). Text mining of cancer related information: review of current status and future directions. Int. J. Med. Inform. 83, 605–623. doi: 10.1016/j.ijmedinf.2014.06.009
Srinivasu, P. N., Ahmed, S., Hassaballah, M., and Almusallam, N. (2024). An explainable artificial intelligence software system for predicting diabetes. Heliyon 10:e36112. doi: 10.1016/j.heliyon.2024.e36112
Sun, H., Saeedi, P., Karuranga, S., Pinkepank, M., Ogurtsova, K., Duncan, B. B., et al. (2022). IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183:109119. doi: 10.1016/j.diabres.2021.109119
Vaľková, J., Adam, M., and Hlaváček, J. (2024). Artificial intelligence in diabetic retinopathy screening: from idea to a medical device in clinical practice. Cas. Lek. Cesk. 162, 290–293.
Wang, V. Y., Lo, M. T., Chen, T. C., Huang, C. H., Huang, A., and Wang, P. C. (2024). A deep learning-based ADRPPA algorithm for the prediction of diabetic retinopathy progression. Sci. Rep. 14:31772. doi: 10.1038/s41598-024-82884-9
Wang, R., Zuo, G., Li, K., Li, W., Xuan, Z., Han, Y., et al. (2022). Systematic bibliometric and visualized analysis of research hotspots and trends on the application of artificial intelligence in diabetic retinopathy. Front. Endocrinol. 13:1036426. doi: 10.3389/fendo.2022.1036426
Wiener, F. (1988). SMR (simulating medical reasoning): an expert shell for non-AI experts. Comput. Methods Prog. Biomed. 26, 19–31. doi: 10.1016/0169-2607(88)90071-5
Wu, L., Huang, R., He, X., Tang, L., and Ma, X. (2024). Advances in machine learning-aided thermal imaging for early detection of diabetic foot ulcers: a review. Biosensors (Basel). 14:614. doi: 10.3390/bios14120614
Xiao, H., Tang, J., Zhang, F., Liu, L., Zhou, J., Chen, M., et al. (2023). Global trends and performances in diabetic retinopathy studies: a bibliometric analysis. Front. Public Health 11:1128008. doi: 10.3389/fpubh.2023.1128008
Xiaoling, W., Shengmei, Z., BingQian, W., Wen, L., Shuyan, G., Hanbei, C., et al. (2024). Enhancing diabetic foot ulcer prediction with machine learning: a focus on localized examinations. Heliyon 10:e37635. doi: 10.1016/j.heliyon.2024.e37635
Xie, Y., Nguyen, Q. D., Hamzah, H., Lim, G., Bellemo, V., Gunasekeran, D. V., et al. (2020). Artificial intelligence for teleophthalmology-based diabetic retinopathy screening in a national programme: an economic analysis modelling study. Lancet Digit. Health 2, e240–e249. doi: 10.1016/S2589-7500(20)30060-1
Keywords: artificial intelligence, diabetes complications, bibliometric analysis, deep learning, machine learning
Citation: Tao Y, Hou J, Zhou G and Zhang D (2025) Artificial intelligence applied to diabetes complications: a bibliometric analysis. Front. Artif. Intell. 8:1455341. doi: 10.3389/frai.2025.1455341
Received: 08 August 2024; Accepted: 15 January 2025;
Published: 31 January 2025.
Edited by:
Dmytro Chumachenko, National Aerospace University—Kharkiv Aviation Institute, UkraineReviewed by:
Shailesh Tripathi, University of Applied Sciences Upper Austria, AustriaCopyright © 2025 Tao, Hou, Zhou and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Da Zhang, emhhbmdkYTc5QGFsaXl1bi5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.