
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Artif. Intell. , 15 November 2022
Sec. Medicine and Public Health
Volume 5 - 2022 | https://doi.org/10.3389/frai.2022.1050439
Rapid development of biotechnology has led to the generation of vast amounts of multi-omics data, necessitating the advancement of bioinformatics and artificial intelligence to enable computational modeling to diagnose and predict clinical outcome. Both conventional machine learning and new deep learning algorithms screen existing data unbiasedly to uncover patterns and create models that can be valuable in informing clinical decisions. We summarized published literature on the use of AI models trained on omics datasets, with and without clinical data, to diagnose, risk-stratify, and predict survivability of patients with non-malignant liver diseases. A total of 20 different models were tested in selected studies. Generally, the addition of omics data to regular clinical parameters or individual biomarkers improved the AI model performance. For instance, using NAFLD fibrosis score to distinguish F0-F2 from F3-F4 fibrotic stages, the area under the curve (AUC) was 0.87. When integrating metabolomic data by a GMLVQ model, the AUC drastically improved to 0.99. The use of RF on multi-omics and clinical data in another study to predict progression of NAFLD to NASH resulted in an AUC of 0.84, compared to 0.82 when using clinical data only. A comparison of RF, SVM and kNN models on genomics data to classify immune tolerant phase in chronic hepatitis B resulted in AUC of 0.8793–0.8838 compared to 0.6759–0.7276 when using various serum biomarkers. Overall, the integration of omics was shown to improve prediction performance compared to models built only on clinical parameters, indicating a potential use for personalized medicine in clinical setting.
Artificial Intelligence (AI)-based tools are being increasingly used for the early diagnosis, prediction of disease progression or survival also increases. The rapid development of biotechnology has revolutionized biomedical research by providing high-throughput molecular data, alongside clinical information collected in health records (Spann et al., 2020; Castañé et al., 2021). As part of AI, both conventional machine-learning (ML) and new deep-learning (DL) algorithms use a data-driven approach that efficiently screens high-throughput data in an unbiased manner, uncovering hidden patterns and generating results which may inform clinical decisions (Chen and Asch, 2017; Spann et al., 2020). Early detection of liver disease can be difficult with conventional methods and AI offers a more comprehensive approach wherein patterns in both clinical and molecular data could be leveraged for insight into diagnostic and prognostic predictions.
Conventional ML is the branch of AI that focuses on processing and learning from data to improve the accuracy and performance of the machine without being explicitly programmed (Bini, 2018). The algorithms are self-learning tools that can be used for efficient and accurate prediction, classification, and resource allocation. They are optimized on a training set and their performance are evaluated on a test set. Supervised ML algorithms [k-nearest neighbor (kNN), linear regression, logistic regression (LR), support vectors machines (SVM), naïve bayes (NB), decision trees and random forests (RF)] work on labeled data where each input is mapped to a corresponding label. On the contrary, unsupervised algorithms (k-means clustering, anomaly detection, association rules, and dimensionality reduction algorithms) use unlabeled input data with the scope of the creation of labels (Dhall et al., 2020).
Neural networks (NNs) or artificial neural networks (ANNs) are the subdivision of ML that focuses on emulating the neurons of the brain. They process signals from an external stimulus and determine the correct downstream course of action. NNs are made up of three layers. Initially, the neurons of the input layer receive signal from the environment. This input is passed on to the neurons in the hidden layer that perform the necessary calculations. The resulting message is then passed along to the output layer of neurons. One application of NNs, deep learning (DL), utilizes a plethora of hidden layers or abstraction units, where each unit performs non-linear operations to process the data (LeCun et al., 2015). Furthermore, the ability of DL to simultaneously accept different forms of input data elevates its performance above traditional machine learning (Esteva et al., 2019). This has led to an increase in DL applications in the field of medicine, such as the use of convolutional neural networks (CNN) for medical imaging and classification.
In liver disease, AI has been applied to various omics data, including genomics, transcriptomics, proteomics, metabolomics and microbiomics for early diagnosis, biomarker discovery, as well as prediction of disease progression and survival. This mini review aims to summarize existing literature on AI models built using a combination of high-throughput omics datasets and/or of clinical variables for the early identification, stratification, and survival prediction of non-malignant liver diseases.
A PubMed search was conducted to retrieve studies published up to Nov 18th, 2021. The inclusion criteria were defined as original papers on human participants in a non-clinical trial setting. We screened and selected eligible studies based on their title and abstract. Our search initially identified 940 papers. After applying the exclusion criteria we selected 20 studies for the final review. The exclusion criteria consisted of following: no liver disease (n = 163) or liver related (n = 104), animal studies (n = 67), clinical trials (n = 28), no ML (n = 32), non-articles (n = 16), non-English (n = 8), malignancy (n = 143), radiomics (n = 114), treatment related (n = 96,) reviews (n = 57), no clinical or omics data (n = 77), editorial/reflection/environmental/language processing or epidemiological studies (n = 15). The extracted information included: number of study participants and their clinical data, study objective, type of liver disease, omics type, AI model and performance metrics. The objectives, AI algorithms used, sample and clinical information on the studies from this mini review, classified by the liver diseases, were included in Table 1. The studies that performed comparison of AI algorithms and their performance to models using only clinical parameters, biomarkers or single features were summarized in Table 2.
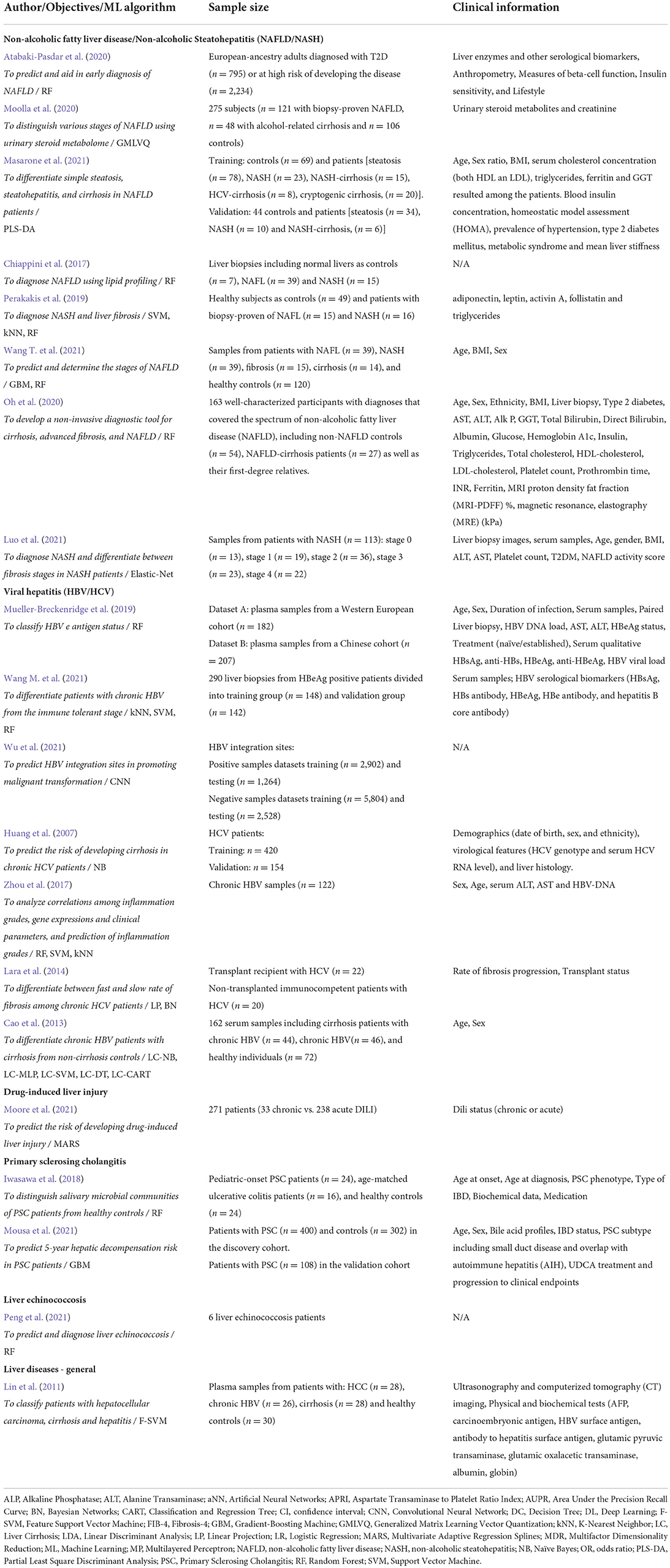
Table 1. Summary of the studies included in this review classified by the liver diseases, with details on the objectives, ML algorithm used, sample and clinical information.
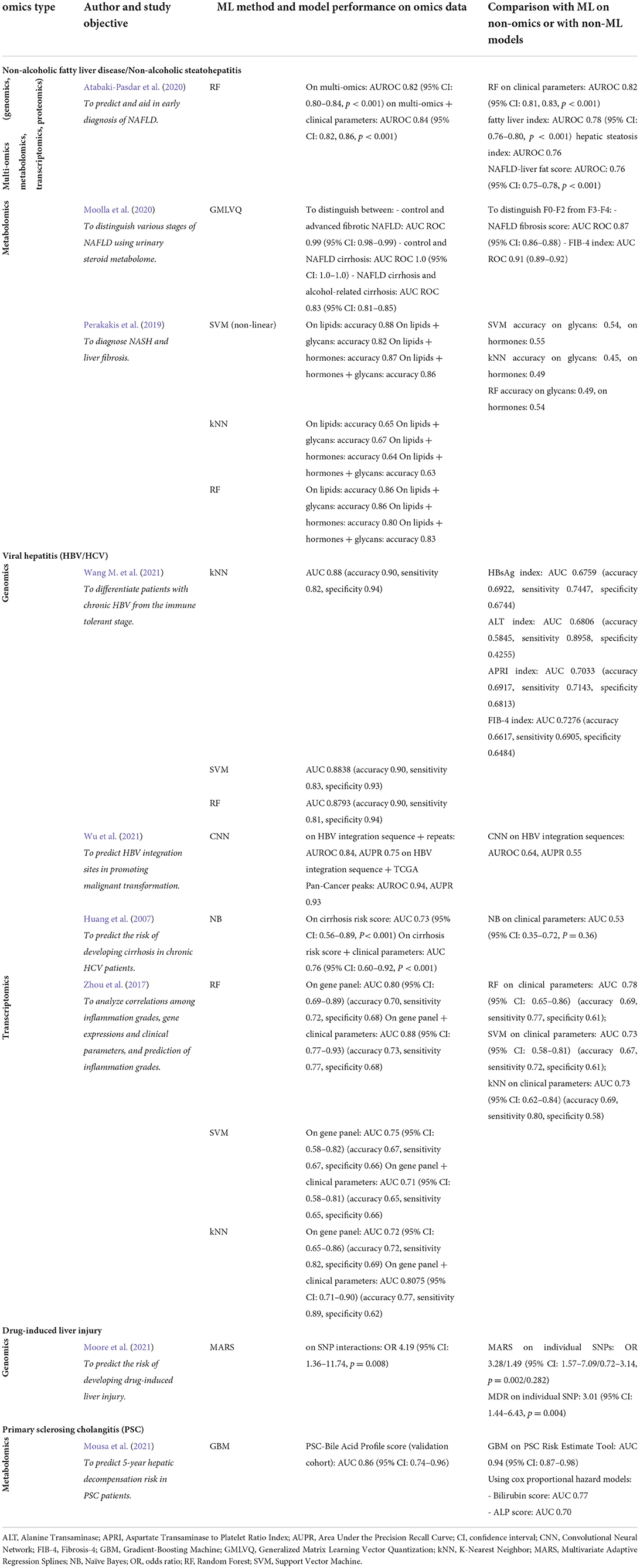
Table 2. Selected studies that performed comparison of ML methods and their performance to models using only clinical parameters, biomarkers or single features.
NAFLD/NASH was the most studied disease, being reported in eight out of the 20 included studies (Chiappini et al., 2017; Perakakis et al., 2019; Atabaki-Pasdar et al., 2020; Moolla et al., 2020; Oh et al., 2020; Masarone et al., 2021; Wang T. et al., 2021). Using multi-omics, two studies used random forest (RF) models for early diagnosis of NAFLD and prediction of the progression from NAFLD to NASH (Atabaki-Pasdar et al., 2020; Oh et al., 2020). Atabaki-Pasdar et al. conducted a multicenter prospective cohort study of 3,028 adults, who were recently diagnosed with or found at risk of developing diabetes, to develop a non-invasive NAFLD prediction tool (Atabaki-Pasdar et al., 2020). Multi-omics data including genomics, transcriptomics, proteomics and metabolomics, along with clinical parameters, were incorporated into a web interface after model validation. The RF model incorporating omics with clinical parameters yielded a cross-validated area under the receiver operating characteristic curve (AUROC) of 0.84 (95% CI 0.82, 0.86, p < 0.001) (Atabaki-Pasdar et al., 2020) that was superior than the model incorporating only clinical information (AUROC) of 0.82 (95% CI 0.81, 0.83, p < 0.001). Oh et al. employed a combination of metagenomics and metabolomics, along with typical clinical variables, to predict the progression of NAFLD to advanced fibrosis and cirrhosis (Oh et al., 2020). Their RF models distinguishes cirrhosis from NAFLD and mild or moderate fibrosis (AUROC of 0.85 and 0.84, respectively) with an improved accuracy upon incorporating serum AST level (AUROC of 0.94 and 0.91, respectively) (Oh et al., 2020). Another four studies utilized metabolomics for various purposes, including the prediction of NAFLD, diagnosis of NASH, and differentiation of NAFLD stages (Chiappini et al., 2017; Perakakis et al., 2019; Moolla et al., 2020; Masarone et al., 2021). The models included decision tree, naïve bayes (NB), random forest (RF), artificial neural network (ANN), partial least square discriminant analysis (PLS-DA), linear discriminant analysis (LDA), DL, and logistic regression (LR). Chiappini et al. used liver biopsies and lipid profiling to develop an RF model aimed to differentiate between NASH and different stages of NAFL (Chiappini et al., 2017). Their RF model based on a 32-lipid signature, associated with dysregulation in fatty acid synthesis pathway, showed 100% sensitivity and specificity, AUC = 1. Uniquely, Perakakis et al. conducted a proof-of-concept study which used SVM, kNN, linear PLS-DA and RF models to diagnose NASH and liver fibrosis based on single or combination of lipids, glycans and biochemical profile (Perakakis et al., 2019). The non-linear SVM with selection of biomolecules were the best predictive ML models for NASH vs. NAFL vs. Healthy groups, with AUC varying from 0.77 to 0.99, depending on the selected variables (see Table 2 for more details). Notably, Masarone et al. used the urinary steroid metabolome to construct both ML and DL models for differentiating between different stages, e.g., simple steatosis, steatohepatitis and cirrhosis in NAFLD patients (Masarone et al., 2021). The models include decision tree, naïve Bayes (NB), random forest (RF), artificial neural network (ANN), partial least square discriminant analysis (PLS-DA), linear discriminant analysis (LDA), DL, and logistic regression (LR), with PLS-DA showing best performance. Depending on which two-group comparison was performed to differentiate between various conditions (NAFLD and Controls, NAFLD and NASH or NASH and cirrhosis), the accuracy of the PLS-DA models was very high, ranging from 0.991 to 0.999 and quality of the prediction indicated by R2, from 0.928 to 0.968. Similarly, Moolla et al. also differentiated various stages using a ML-based generalized matrix learning vector quantization (GMLVQ) analysis on urinary metabolomic data (Moolla et al., 2020). All these models were reported to have an accuracy >0.80 (Perakakis et al., 2019; Moolla et al., 2020; Masarone et al., 2021). A proteomics study used an elastic-net algorithm to diagnose NASH and differentiate between fibrosis stages in NASH patients and built models based on a four- or 12-protein classifier (AUROC of 0.74 and 0.83, respectively) (Luo et al., 2021).
A total of seven studies reported on the omics profiling of viral hepatitis patients, specifically hepatitis B virus (HBV) and hepatitis C virus (HCV) infections (Huang et al., 2007; Cao et al., 2013; Lara et al., 2014; Zhou et al., 2017; Mueller-Breckenridge et al., 2019; Wang M. et al., 2021; Wu et al., 2021). Of these, five studies used genomics (Huang et al., 2007; Zhou et al., 2017; Mueller-Breckenridge et al., 2019; Wang M. et al., 2021; Wu et al., 2021), one study utilized transcriptomics (Lara et al., 2014), and one study generated proteomics data (Cao et al., 2013). HBV is a major risk factor for developing liver fibrosis, cirrhosis, and hepatocellular carcinoma (HCC) (Mueller-Breckenridge et al., 2019). Hepatitis B e antigen (HBeAg) is a secreted protein of HBV with a high sequence conservation and seroconversion due to HBeAg represents a biomarker in infected individuals (Mueller-Breckenridge et al., 2019). Mueller-Breckenridge et al. used the RF method to classify HBeAg status of patients with chronic HBV infection (Mueller-Breckenridge et al., 2019). The highest-ranking variables contributing to the model are known pre-core and basal core promotor mutants (n1896GA, n1934AT, n1753TC). Similarly, Wang et al. used the HBeAg biomarker and enrolled HBeAg positive patients from whom liver biopsies were taken (Wang M. et al., 2021). Using three ML models, i.e., kNN, SVM, and RF, the study aimed to differentiate the immune tolerant phase from chronic HBV. All predictive ML models using genomics (whole HBV sequencing data and viral quasispecies), showed higher AUC values (validation group AUC of 0.8838, 0.8801, and 0.8793 for SVM, kNN, and RF, respectively) compared to models commonly used for liver fibrosis, based on HBsAg, ALT, APRI, and FIB-4 (validation group AUC of 0.6759, 0.6806, 0.7033 and 0.7276, respectively), indicating better classification (Wang M. et al., 2021) (Table 2). The authors suggested to use the best performing model for future diagnosis, rather than performing invasive liver biopsies. Wu et al. used Convolutional Neural Networks (CNN) to develop an attention-based deep learning model, DeepHBV (Wu et al., 2021). It effectively learns local genomic features and uses the information to predict HBV integration sites which promotes malignant transformation. In addition to DNA sequences near the HBV integration sites, the integration of additional genomic features, such as repeat and TCGA Pan-Cancer peaks, improved the AUROC from 0.64 to 0.84 and 0.94, respectively (Wu et al., 2021). Using this tool they revealed novel integration site for HBV. Zhou et al. used gene profiles and clinical variables to predict inflammation grades in chronic HBV patients (Zhou et al., 2017). A selection of genes along with clinical parameters showed effectiveness in predicting binary classifications of inflammation grade [AUROC of 0.88 (95% CI: 0.77–0.93)] and superior performance in comparison with the model that did not include clinical variables [AUROC of 0.78 (95% CI: 0.65–0.86)]. Although liver biopsy is the reference standard for evaluating cirrhosis, it is an invasive procedure. Cao et al. used proteomics data to differentiate HBV patients with cirrhosis from non-cirrhotic controls, by testing five machine learning models (NB), multilayered perceptron (MP), SVM, decision tree, and classification and regression tree (CART) on non-invasive serum biomarkers to diagnose cirrhosis. The best predictive model was based on NB, called LC-NB, with AUC of 0.977 (sensitivity: 86.4%, specificity: 96.9%, accuracy: 93.8%) (Cao et al., 2013), where LC stands for liver cirrhosis. By comparison, other ML models derived in this study obtained AUC varying from 0.73 (LC-CART) to 0.83 (LC-DT) to 0.85 (LC-SVM) to 0.97 (LC-MLP) and accuracy ranging from 0.85 to 0.86 to 0.90 to 0.98, respectively. ML (NB) was also applied for prediction of cirrhosis among Caucasian patients with chronic hepatitis C, by developing of Cirrhosis Risk Score (CRS) (Huang et al., 2007). The model that integrated a signature of seven SNPs with clinical variables presented superior performance (AUC of 0.76) vs. the model that did not include genomics data (AUC of 0.53). Lara et al. developed LP and BN models to differentiate between fast and slow rate of fibrosis progression (RFP) among chronic HCV patients (Lara et al., 2014). The LP model showed 95% accuracy of RFP-classification with a sensitivity of 82% and a specificity of 100%. The BN classifier models are learned separately from immunocompetent and liver transplant recipient datasets, reaching an accuracy of 86.4 and 85%, respectively (Lara et al., 2014).
The inclusion criteria set out to specifically predict DILI, as diagnosed by liver biopsy, was met by one study which utilized genomics data. The study by Moore et al. employed three ML algorithms, multivariate adaptive regression splines (MARS), multifactor dimensionality reduction (MDR), and LR, with the aim of investigating single-nucleotide polymorphisms (SNPs) (Moore et al., 2021). The effect of SNP-SNP interactions on DILI susceptibility as well as their ability to predict DILI chronicity were observed. Subsequently, an RF algorithm was used to validate the ability of the three models in identifying chronic DILI associated SNP interactions achieving sensitivity, specificity, accuracy and balanced accuracy scores of 42.4, 90.3, 86.3 and 66.4%, respectively. Ultimately, both the RF and LR algorithms were unsuccessful in more accurately identifying SNP-SNP interaction terms than individual SNPs while both MARS and MDR were successful. MARS identified interactions between SNPs rs6487213 and rs3785157 with an odds ratio score of 4.74 (95% CI: 2.14–10.39, p < 0.001), while MDR achieved an odds ratio of 4.19 (95% CI: 1.36–11.74, p = 0.008) for interactions between rs5417, rs7658048, and rs12453290.
PSC accounted for two of the 20 final selected papers. One study involving metabolomic data from 400 PSC patients utilized both (univariate) Cox proportional hazard and (multivariable) GBM models (Mousa et al., 2021). They set out to predict the 5-year risk of hepatic decompensation in PSC patients. They developed a PSC bile acid profile (PSC-BAP) score able to sufficiently predict future hepatic decompensation events. For the final model with six covariates, the predictive performance was comparable in the training set (AUC of 0.95, 95%CI, 0.92–0.97) and in the validation cohort (AUC of 0.86, 95%CI, 0.74–0.96). Consequently, they elucidated a genuine potential for bile acid profiles as non-invasive biomarkers. Another study by Iwasawa et al. explored the microbiological features of the salivary microbiota to distinguish salivary microbial communities of PSC patients from healthy controls (HC) and ulcerative colitis (UC) patients, by implementing an RF algorithm on meta-genomics data (Iwasawa et al., 2018). Their study highlighted the potential of salivary microbiota as a biomarker to distinguish between PSC patients, UC patients and healthy controls. Their algorithm achieved an AUROC of 0.8756 when distinguishing between PSC and UC, and an AUROC of 0.7423 when distinguishing between PSC and healthy controls (Iwasawa et al., 2018).
A study by Peng et al. used transcriptomics to generate a predictive model for liver echinococcosis (Peng et al., 2021). Using microarray profiling, the authors identified 1,152 differentially expressed genes. These were selected for Protein-protein interaction (PPI) network analysis to reveal the most critical genes by centrality score, then a RF model was constructed based on hub genes. A particular RF model based on FCGR2B and CTLA4 genes reliably predicted liver hydatid disease with an AUROC of 0.921.
One study applied ML to metabolomics to distinguish between HCC and other liver diseases: cirrhosis, and hepatitis (Lin et al., 2011). Using a Feature Support Vector Machine (F-SVM) with selection of 22 metabolites they differentiated the latter two with an accuracy of 89.23 +/− 3.82%, suggesting that metabolites could be used in prediction of liver diseases.
AI models are hard to be understood by humans, they lack in interpretation and considered black boxes. To overcome this important issue in highly regulated areas, such as healthcare, explainable AI (XAI) methods have been developed, based on Shapley values (Shapley; Bussmann et al., 2020). Such models, however, interpret mostly the importance of local features and the contribution of each variable within each model, rather than offering a more global view.
Literature on AI applied to high-throughput omics and clinical data from non-malignant liver diseases is still somewhat limited compared to malignant liver diseases. As evident in the greater number of papers published, attention has been heavily given to studies pertaining to HCC. These were excluded from this review to highlight the use of AI in non-malignant liver diseases. Further, we found only one study on AI utilizing molecular data derived from liver transplant recipients, proving a gap of knowledge in the field of post-transplant liver diseases.
The increased availability of omics data from human samples can contribute to the advancement of precision medicine that relies on data for each individual patient, rather than applying a “one-size-fits-all” model, to fine-tune and personalize the diagnosis and risk stratification of patients. Therefore, there is significant potential for the application of AI for precision medicine in general, and in liver diseases in particular. Further efforts should be directed toward improving the predictive ability of these integrated omics-based algorithms built on a wide range of data, clinical and otherwise. Strategies should be made for the implementation, as well as standardization of such practices. For better interpretation of the AI models, a combination of more interpretable local Shapley values with more global explainable AI methods, such as the Shapley-Lorenz XAI (Giudici and Raffinetti, 2021) have been developed. The advantage of this model resides in both predictive accuracy and interpretation metric and should be used in future research involving AI models. Finally, the practicality of working with large omics datasets on a daily basis need to be considered, including the cost needed to collect and process samples, the time required for analysis and the need for trained personnel and an appropriate facility to perform various omics.
In this mini review, we screened 20 studies that employed AI on clinical and high-throughput molecular data from non-malignant liver diseases. We found that ML or DL algorithms could predict early disease, stratify different stages, and/or predict survival in liver diseases when using a diversity of omics data in addition to clinical information to build specific models. With greater availability of high-throughput molecular data, there is potential to implement AI for precision medicine in hepatology.
CB and MB: mini review design, writing of manuscript, and writing the final manuscript. CB, CX, MA, and KP: literature search, abstract selection, and editing the manuscript. KP: input into study design. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Atabaki-Pasdar, N., Ohlsson, M., Viñuela, A., Frau, F., Pomares-Millan, H., Haid, M., et al. (2020). Predicting and elucidating the etiology of fatty liver disease: a machine learning modeling and validation study in the IMI DIRECT cohorts. PLoS Med. 17, e1003149. doi: 10.1371/journal.pmed.1003149
Bini, S. A. (2018). Artificial intelligence, machine learning, deep learning, and cognitive computing: what do these terms mean and how will they impact health care? J. Arthroplasty. 33, 2358–2361. doi: 10.1016/j.arth.2018.02.067
Bussmann, N., Giudici, P., Marinelli, D., and Papenbrock, J. (2020). Explainable AI in fintech risk management. Front. Artif. Intell. 3, 26. doi: 10.3389/frai.2020.00026
Cao, Y., He, K., Cheng, M., Si, H. Y., Zhang, H. L., Song, W., et al. (2013). Two classifiers based on serum peptide pattern for prediction of HBV-induced liver cirrhosis using MALDI-TOF MS. Biomed. Res. Int. 2013, 814876. doi: 10.1155/2013/814876
Castañé, H., Baiges-Gaya, G., Hernández-Aguilera, A., Rodríguez-Tomàs, E., Fernández-Arroyo, S., Herrero, P., et al. (2021). Coupling machine learning and lipidomics as a tool to investigate metabolic dysfunction-associated fatty liver disease. A general overview. Biomolecules 11, 473. doi: 10.3390/biom11030473
Chen, J. H., and Asch, S. M. (2017). Machine learning and prediction in medicine - beyond the peak of inflated expectations. N. Engl. J. Med. 376, 2507–2509. doi: 10.1056/NEJMp1702071
Chiappini, F., Coilly, A., Kadar, H., Gual, P., Tran, A., Desterke, C., et al. (2017). Metabolism dysregulation induces a specific lipid signature of nonalcoholic steatohepatitis in patients. Sci. Rep. 7, 46658. doi: 10.1038/srep46658
Dhall, D., Kaur, R., and Juneja, M. (2020). “Machine learning: A review of the algorithms and its applications,” in Proceedings of ICRIC 2019. Lecture Notes in Electrical Engineering, Vol. 597, eds P. Singh, A. Kar, Y. Singh, M. Kolekar, and S. Tanwar (Cham: Springer). doi: 10.1007/978-3-030-29407-6_5
Esteva, A., Robicquet, A., Ramsundar, B., Kuleshov, V., DePristo, M., Chou, K., et al. (2019). A guide to deep learning in healthcare. Nat. Med. 25, 24–29. doi: 10.1038/s41591-018-0316-z
Giudici, P., and Raffinetti, E. (2021). Shapley-lorenz explainable artificial intelligence. Expert Syst. Appl. 167, 114104. doi: 10.1016/j.eswa.2020.114104
Huang, H., Shiffman, M. L., Friedman, S., Venkatesh, R., Bzowej, N., Abar, O. T., et al. (2007). A 7 gene signature identifies the risk of developing cirrhosis in patients with chronic hepatitis C. Hepatology 46, 297–306. doi: 10.1002/hep.21695
Iwasawa, K., Suda, W., Tsunoda, T., Oikawa-Kawamoto, M., Umetsu, S., Takayasu, L., et al. (2018). Dysbiosis of the salivary microbiota in pediatric-onset primary sclerosing cholangitis and its potential as a biomarker. Sci. Rep. 8, 5480. doi: 10.1038/s41598-018-23870-w
Lara, J., López-Labrador, F., González-Candelas, F., Berenguer, M., and Khudyakov, Y. E. (2014). Computational models of liver fibrosis progression for hepatitis C virus chronic infection. BMC Bioinformatics. 15 Suppl 8(Suppl 8):S5. doi: 10.1186/1471-2105-15-S8-S5
LeCun, Y., Bengio, Y., and Hinton, G. (2015). Deep learning. Nature 521, 436–444. doi: 10.1038/nature14539
Lin, X., Zhang, Y., Ye, G., Li, X., Yin, P., Ruan, Q., et al. (2011). Classification and differential metabolite discovery of liver diseases based on plasma metabolic profiling and support vector machines. J. Sep. Sci. 34, 3029–3036. doi: 10.1002/jssc.201100408
Luo, Y., Wadhawan, S., Greenfield, A., et al. (2021). SOMAscan proteomics identifies serum biomarkers associated with liver fibrosis in patients with NASH. Hepatol. Commun. 5, 760–773. doi: 10.1002/hep4.1670
Masarone, M., Troisi, J., Aglitti, A., Torre, P., Colucci, A., Dallio, M., et al. (2021). Untargeted metabolomics as a diagnostic tool in NAFLD: discrimination of steatosis, steatohepatitis and cirrhosis. Metabolomics 17, 12. doi: 10.1007/s11306-020-01756-1
Moolla, A., de Boer, J., Pavlov, D., Saikali, M. F., Bentley, L., Penning, T. M., et al. (2020). Accurate non-invasive diagnosis and staging of non-alcoholic fatty liver disease using the urinary steroid metabolome. Aliment. Pharmacol. Ther. 51, 1188–1197. doi: 10.1111/apt.15710
Moore, R., Ashby, K., Liao, T. J., and Chen, M. (2021). Machine learning to identify interaction of single-nucleotide polymorphisms as a risk factor for chronic drug-induced liver injury. Int. J. Environ. Res. Public Health. 18, 10603. doi: 10.3390/ijerph182010603
Mousa, O. Y., Juran, B. D., McCauley, B. M., Vesterhus, M. N., Folseraas, T., Turgeon, C. T., et al. (2021). Bile acid profiles in primary sclerosing cholangitis and their ability to predict hepatic decompensation. Hepatology 74:281–295. doi: 10.1002/hep.31652
Mueller-Breckenridge, A. J., Garcia-Alcalde, F., Wildum, S., et al. (2019). Machine-learning based patient classification using Hepatitis B virus full-length genome quasispecies from Asian and European cohorts. Sci. Rep. 9, 18892. doi: 10.1038/s41598-019-55445-8
Oh, T. G., Kim, S. M., Caussy, C., Fu, T., Guo, J., Bassirian, S., et al. (2020). A universal gut-microbiome-derived signature predicts cirrhosis. Cell. Metab. 32, 878–888.e6. doi: 10.1016/j.cmet.2020.06.005
Peng, J., Duan, Z., Guo, Y., Li, X., Luo, X., Han, X., et al. (2021). Identification of candidate biomarkers of liver hydatid disease via microarray profiling, bioinformatics analysis, and machine learning. J. Int. Med. Res. 49, 1–12. doi: 10.1177/0300060521993980
Perakakis, N., Polyzos, S. A., Yazdani, A., Sala-Vila, A., Kountouras, J., Anastasilakis, A. D., et al. (2019). Non-invasive diagnosis of non-alcoholic steatohepatitis and fibrosis with the use of omics and supervised learning: a proof of concept study. Metabolism 101, 154005. doi: 10.1016/j.metabol.2019.154005
Shapley, L. (1953). “A value for n-Person games,” in Contributions to the Theory of Games II, eds H. Kuhn and A. Tucker (Princeton, NJ: Princeton University Press), 307–317. doi: 10.1515/9781400881970-018
Spann, A., Yasodhara, A., Kang, J., Watt, K., Wang, B., Goldenberg, A., et al. (2020). Applying machine learning in liver disease and transplantation: a comprehensive review. Hepatology 71, 1093–1105. doi: 10.1002/hep.31103
Wang, M., Chen, L., Dong, M., Li, J., Zhu, B., Yang, Z., et al. (2021). Viral quasispecies quantitative analysis: a novel approach for appraising the immune tolerant phase of chronic hepatitis B virus infection. Emerg. Microbes Infect. 10, 842–851. doi: 10.1080/22221751.2021.1919033
Wang, T., Guo, X. K., and Xu, H. (2021). Disentangling the progression of non-alcoholic fatty liver disease in the human gut microbiota. Front. Microbiol. 12, 728823. doi: 10.3389/fmicb.2021.728823
Wu, C., Guo, X., Li, M., Shen, J., Fu, X., Xie, Q., et al. (2021). DeepHBV: a deep learning model to predict hepatitis B virus (HBV) integration sites. BMC Ecol. Evol. 21, 138. doi: 10.1186/s12862-021-01869-8
Keywords: artificial intelligence, machine learning, omics data, liver disease, clinical outcome prediction
Citation: Baciu C, Xu C, Alim M, Prayitno K and Bhat M (2022) Artificial intelligence applied to omics data in liver diseases: Enhancing clinical predictions. Front. Artif. Intell. 5:1050439. doi: 10.3389/frai.2022.1050439
Received: 21 September 2022; Accepted: 31 October 2022;
Published: 15 November 2022.
Edited by:
Holger Fröhlich, Fraunhofer Institute for Algorithms and Scientific Computing (FHG), GermanyReviewed by:
Paolo Giudici, University of Pavia, ItalyCopyright © 2022 Baciu, Xu, Alim, Prayitno and Bhat. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mamatha Bhat, TWFtYXRoYS5iaGF0QHVobi5jYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.