- Department of Anesthesiology, The Jikei University School of Medicine, Minatoku, Japan
Backgrounds: Hypoxemia develops more quickly in children than in adults due to their high oxygen consumption relative to their body weight and small functional residual capacity. Therefore, cricothyroid puncture must be performed promptly in cannot-intubate and cannot-ventilate situations. However, the success rate of cricothyroid puncture in children is <1%. We hypothesized that the low success rate of cricothyroid puncture in children may be related to the cricothyroid membrane's hypermobility. The aim of the present study was to measure the deviation of the cricothyroid membrane from the midline when applying compressive pressure.
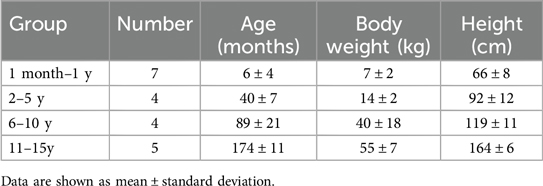
Methods: After obtaining institutional ethics committee approval, written informed consent was obtained from the patients’ parents. Children aged from 1 month to 15 years who had undergone scheduled operations under general anesthesia and with an American Society of Anesthesiologists Physical Status Classification grade of 1 or 2 were enrolled in this study. The patients were divided into the following four different age groups: 1 month–1 year, 2–4 years, 5–10 years, and 11–15 years. After the intravenous injection of fentanyl, propofol, and rocuronium, the airway was identified using a linear hockey stick ultrasound probe. The cricothyroid membrane was compressed with a force of 5 newtons (N), and cricothyroid membrane deflection was recorded. The primary outcome was the cricothyroid membrane deviation from the midline relative to the tracheal diameter.
Results: Twenty patients were enrolled in this study. No adverse events were noted. The mean cricothyroid membrane deviations from the midline divided by the tracheal diameter was 0.16 ± 0.09, 0.05 ± 0.04, 0.04 ± 0.04, and 0.02 ± 0.03 in children aged 1 month–1 year, 2–4 years, 5–10 years, and 11–15 years, respectively.
Conclusion: The cricothyroid membrane deviation due to the application of a compressive force to the overlying skin tended to be larger in younger patients.
Introduction
Hypoxemia, which can lead to cannot-intubate cannot-ventilate (CICV) events, is well known to develop more rapidly in children than in adults. Hypoxemia in children is caused by high oxygen consumption to body weight ratio and small functional residual capacity. Although CICV events are rare in children, it is important to be prepared for emergency airway management. However, the success rate of cricothyroid puncture in children is very low. In many institutions, in the absence of well-trained otolaryngologists, an anesthesiologist performs cricothyroid puncture in emergency situations (1). Contrarily, most cases of pediatric cardiac arrest reportedly are caused by airway obstruction. Conversely, if oxygenation is maintained, pediatric patients with airway obstruction have satisfactory prognosis (2).
Recent guidelines of pediatric difficult airway management highlight the importance of invasive airway techniques including surgical cricothyroidotomy and needle cricothyroidotomy (3). In neonates, the mean SD length and width of the cricothyroid membrane is only 2.6 mm and 3.0 mm, respectively such a small cricothyroid membrane.
Such a small cricothyroid membrane makes identification of anatomical landmarks extremely difficult. Moreover, a healthy amount of the subcutaneous tissue may prevent the cricoid membrane from being fixed during the procedure, potentially making the cricothyroidotomy technically more challenging. This fact is very important to know in an emergency situation.
We hypothesized that the low success rate of cricothyroid puncture in children may be related to the deviation of the cricothyroid membrane when anesthesiologists attempt to puncture the cricothyroid membrane. In this study, we measured the cricothyroid membrane deviation from the midline induced when an echo probe was used to apply a force of 5 N, which is similar to the pressure applied during cricothyroid membrane puncture procedures.
Methods
After obtaining ethical approval from the Research Ethics Committee of Jikei University Hospital (No. 30-286), written informed consent was obtained from the patients’ parents. Patients aged 1 month to 15 years who underwent a scheduled operation under general anesthesia between May 01, 2019 and October 31, 2020 and who had an American Society of Anesthesiologists Physical Status Classification (ASA-PS) grade of 1 or 2 were enrolled in this study. The exclusion criteria were patients with an ASA-PS of 3 and/or a history of tracheostomy or anticipated airway difficulty.
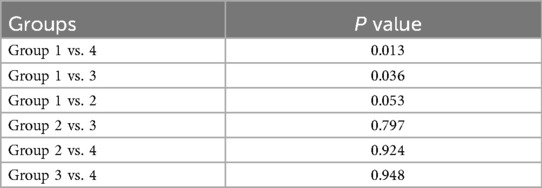
All patients underwent preoperative fasting, and none of them had received premedication as was practiced in this institution. Standard monitoring, such as electrocardiography, pulse oximetry, noninvasive arterial pressure monitoring, and bispectral index monitoring were used in the operating room. General anesthesia was induced by inhalation of sevoflurane or intravenous anesthesia. Fentanyl, propofol, and rocuronium were administered to all patients. Towels were placed under the patients’ shoulder to flex the back and maintain the tracheotomy position (Figure 1). Data correction was performed by two anesthesiologists. One anesthesiologist placed an ultrasound hockey stick probe on the skin over the cricothyroid membrane, whereas the other anesthesiologist ventilated the patient with a face mask. The cricothyroid membrane was identified through the skin using ultrasound (Figure 1). The skin over the cricothyroid cartilage was then compressed using the hockey stick probe. A digital force gauge was used to apply a 5-N compressive force. The cricothyroid membrane deviation from the midline was measured using the function mode of the ultrasound machine. A 5-N force level, much lower than that used in the Sellick maneuver (20–40 N), was chosen to avoid study-related complications and discomforts. Patients were stratified by age into the following four groups: group 1, patients aged 1 month–1 year; group 2, those aged 2–4 years; group 3, those aged 5–10 years; and group 4, those aged 11–15 years. Based on a preliminary study, the appropriate sample size to achieve a power of 80% and a statistical significance of p < 0.05 was calculated to be four patients per group. After the completion of this study, the chest X-ray scan of each patient was used to measure the tracheal diameter at the level of the first thoracic vertebra. The pressure-induced deviation divided by the tracheal diameter was used to calculate a correction for distance traveled for different ages and body sizes. The primary outcome was the data of the pressure-induced deviation divided by the tracheal diameter in each age group. All data are expressed as the mean ± standard deviation. Statistical analysis was performed using SigmaPlot version 13 (Systat Software, Inc., San Jose, CA, United States). The normal distribution of the primary outcome was determined using the Shapiro–Wilk test followed by the Brown–Forsythe test for equal variances. For each age category, multiple pairwise comparisons were evaluated using the Holm–Šidák method. p Values of <0.05 were considered statistically significant.
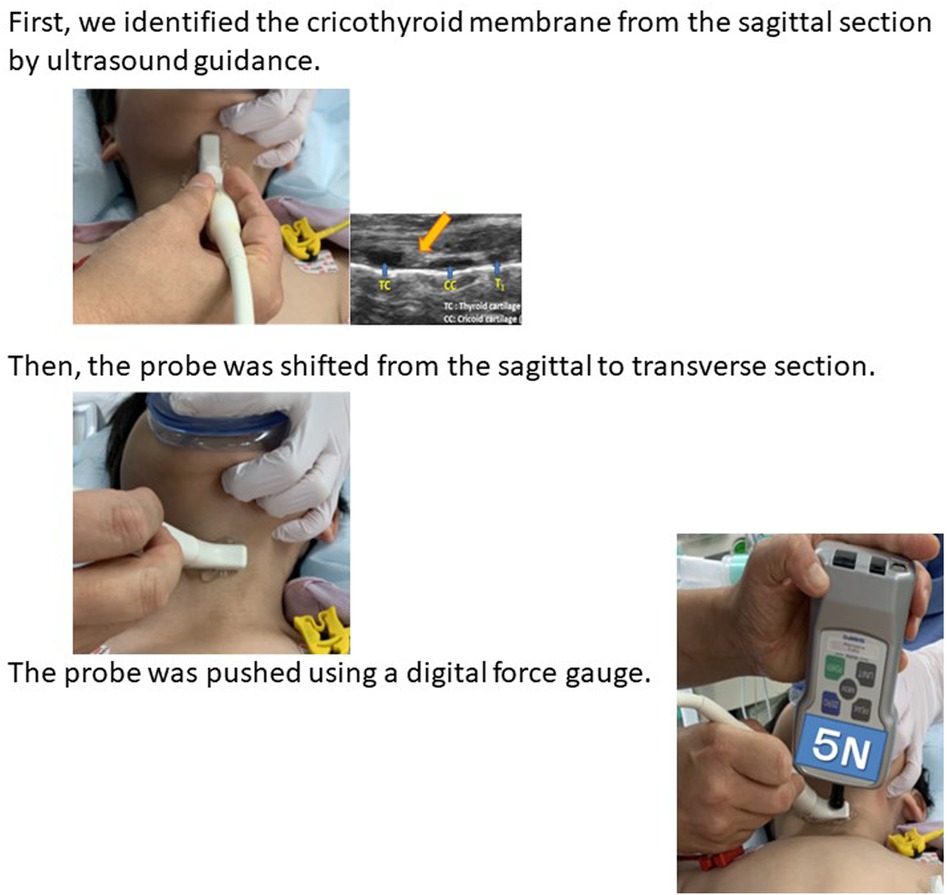
Figure 1. Methods of measurement. First, we identified the cricothyroid membrane from the sagittal section by ultrasound guidance. Then, the probe was shifted from the sagittal to transverse section. The probe was pushed using a digital force gauge.
Results
Altogether, 24 patients were included in this study. Four children were excluded because their patients did not provide informed consent. Therefore, a total of 20 patients were included in the analysis. No adverse events occurred during the study. The patients’ characteristics are shown in Table 1. The median deviations of the cricothyroid membrane from the midline divided by the tracheal diameter were 0.16 ± 0.09, 0.05 ± 0.04, 0.04 ± 0.04, and 0.02 ± 0.03 in groups 1, 2, 3, and 4, respectively (Table 2). A significant difference was noted between group 1 and groups 3 and 4. However, no statistical difference was noted between groups 1 and 2 (Table 3). A p-value was 0.053. The 9-month-old baby in group 1 showed the migration of the cricothyroid membrane while the 7-year-old boy in group 3, showed less migration and more compression (Figure 2). Figure 3 shows that the deviation of the cricothyroid membrane divided by the tracheal diameter decreased with increasing age.
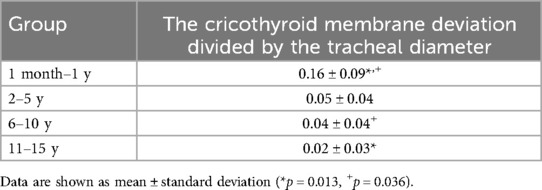
Table 2. The cricothyroid membrane deviation from the midline induced by compressing the cricothyroid membrane divided by the tracheal diameter.
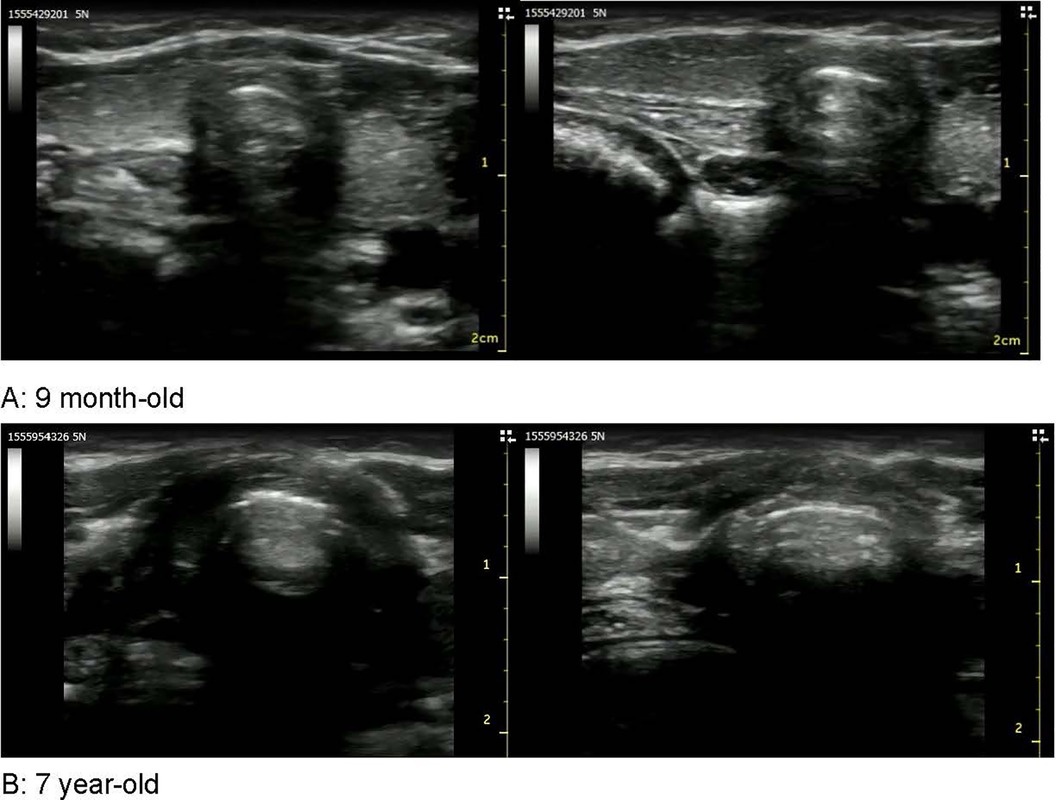
Figure 2. Images of the cricothyroid membrane. These images showed the cricothyroid membranes of a 9-month-old (A) and a 7-year-old (B). The 9-month-old showed the migration of the cricothyroid membrane while the 7-year-old showed less migration and more compression.
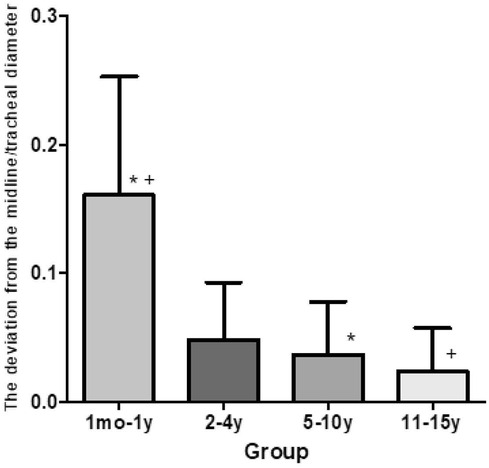
Figure 3. The deviation of the cricothyroid membrane divided by the tracheal diameter. The deviation of the cricothyroid membrane induced by applying compressive force to the overlying skin was larger in the infants aged 1 month to 1 year rather than in children aged 5–10 and 11–15 years.
Discussion
The present study measured the deviation of the cricothyroid membrane from the midline when applying compressive force. We hypothesized that the main reason for the low success rate of pediatric cricothyroid puncture in children may be related to the cricothyroid membrane deviation.
We found that the cricothyroid membrane deviation induced by applying a compressive force to the overlying skin was greater in younger patients. The anatomy of the pediatric cricothyroid membrane is further obscured by the amount of adipose tissue in the subcutaneous tissue, which makes it difficult to palpate the lower edge of the thyroid membrane. Our study results suggest that, in young children, attempting cricothyroid puncture under ultrasound guidance might be beneficial.
In adults, the mean length and width of the cricothyroid membrane were 13.7 mm (range: 8–19 mm) and 12.4 (range: 9–19 mm) mm, respectively (3, 4). Contrarily, the equivalent figures for neonates are only 2.6 ± 0.7 and 3.0 ± 0.6 mm, respectively (5). It is easy to imagine that if the cricoid membrane was shift from midline, correct catheter insertion becomes difficult. These results indicated that cricothyroid membrane puncture should not be performed in infants, not only because of the small size of their cricothyroid membrane, but also because of the added factor of pressure-induced deviation. Moreover, recent studies have shown that only 36%–55% of clinicians can accurately identify the pediatric cricothyroid membrane by palpation (6, 7). In our previous study, anesthesiologists could identify the cricothyroid membrane by palpation in 38% (5/13) of infants aged <1 year, in 67% (4/6) of children aged 2 years, and in 85% (17/20) of children aged 3–15 years (2015, Annual Meeting of Society of Anesthesiologist in Japan).
The main strength of the present study was that the same compressive force was applied through the skin in each case; therefore, no adverse complication occurred. We compressed the cricothyroid membrane with a force of 5 newtons (N) by the digital force gauge. It has previously been discussed that it is inappropriate to apply cricoid pressure in children, particularly infants and neonates. This technique is unpleasant in children. Therefore, we had to dothis research safety. That is the reason why we compressed pediatric cricothyroid membrane with low pressure. Other power as 10 N or 20 N, might have influenced the results by inducing a consistent effect across all patients.
Recently, Aleah M. De Schmidt et al. reported that data of puncture forces of the cricothyroid membrane and tracheal annular ligaments were collected from 39 to 42 excised human donor tracheas (8). The average puncture force of the cricothyroid membrane using an 11-blade scalpel was 1.01 ± 0.36 N, and the average puncture force of the tracheal annular ligaments using a sharp 16-gauge needle was 0.98 ± 0.34 N. They used the cricothyroid membrane without skin and tissue. According to their research, puncture force was low as 1 N. Further research was needed.
Moreover, the main limitation of this study was that the number of analyzed patients were small. Future studies must include pediatric patients with airway difficulties, such as those with multiple congenital anomaly syndromes, as their cricothyroid membranes can differ from those of healthy patients.
Conclusion
Our study data showed that the deviation of the cricothyroid membrane induced by the application of compressive force to the overlying skin tended to be larger in infants aged 1 month to 1 year. Hence, cricothyroid membrane puncture should not be performed in infants. It may also be beneficial to attempt a cricothyroid puncture under ultrasound guidance in older children.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Jikei University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SF: Data curation, Visualization, Writing – review & editing. YH: Writing – original draft, Validation, Visualization. YoS: Data curation, Writing – review & editing. KT: Data curation, Writing – review & editing. YuS: Data curation, Writing – review & editing. EH: Data curation, Writing – review & editing. AK: Data curation, Writing – review & editing. YA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported in part by Jikei University’s internal clinical research budget and Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science, grant Numbers was 19K18282.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Black AE, Flynn PE, Smith HL, Thomas ML, Wilkinson KA. Development of a guideline for the management of the unanticipated difficult airway in pediatric practice. Paediatr Anaesth. (2015) 25:346–62. doi: 10.1111/pan.12615
2. Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of hospital cardiac arrests: a prospective, nationwide, population-based cohort study. Lancet. (2010) 375:1347–54. doi: 10.1016/S0140-6736(10)60064-5
3. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American society of anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. (2022) 136:31–81. doi: 10.1097/ALN.0000000000004002
4. Bennett JD, Guha SC, Sankar AB. Cricothyrotomy: the anatomical basis. J R Coll Surg Edinb. (1996) 41:57–60.8930047
5. Goumas P, Kokkinis K, Petrocheilos J, Naxakis S, Mochloulis G. Cricothyroidotomy and the anatomy of the cricothyroid space. An autopsy study. J Laryngol Otol. (1997) 111:354–6. doi: 10.1017/s0022215100137296
6. Navsa N, Tossel G, Boon JM. Dimensions of the neonatal cricothyroid membrane - how feasible is a surgical cricothyroidotomy? Paediatr Anaesth. (2005) 15:402–6. doi: 10.1111/j.1460-9592.2005.01470.x
7. Fennessy P, Walsh B, Laffey JG, McCarthy KF, McCaul CL. Accuracy of pediatric cricothyroid membrane identification by digital palpation and implications for emergency front of neck access. Paediatr Anaesth. (2020) 30:69–77. doi: 10.1111/pan.13773
8. Basaran B, Egilmez AI, Alatas N, Yilbas AA, Sargin M. Accuracy of identifying the cricothyroid membrane in children using palpation. J Anesth. (2018) 32:768–73. doi: 10.1007/s00540-018-2538-0
Keywords: cricothyroid membrane, infant, cricothyroid puncture, digital force gauge, ultrasound
Citation: Fujioka S, Hobo Y, Suga Y, Takano K, Sano Y, Hosaka E, Kimura A and Abukawa Y (2024) Analysis of pressure-induced deviation of the cricothyroid membrane among pediatric patients. Front. Anesthesiol. 3:1428448. doi: 10.3389/fanes.2024.1428448
Received: 6 May 2024; Accepted: 16 September 2024;
Published: 18 October 2024.
Edited by:
Marco Fiore, Università degli Studi della Campania "Luigi Vanvitelli", ItalyReviewed by:
Jesus Rico-Feijoo, Hospital Universitario Río Hortega, SpainAntonio Corrente, Università of Campania "L.Vanvitelli", Italy
Copyright: © 2024 Fujioka, Hobo, Suga, Takano, Sano, Hosaka, Kimura and Abukawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yukako Abukawa, eXVrYWtvYWJ1a2F3YXNhbmR5QHlhaG9vLmNvLmpw; eXVrYWtvYWJ1a2F3YUBqaWtlaS5hYy5qcA==
 Shoko Fujioka
Shoko Fujioka Yuko Hobo
Yuko Hobo Ayano Kimura
Ayano Kimura Yukako Abukawa
Yukako Abukawa