
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Anesthesiol. , 30 May 2023
Sec. Perioperative Medicine
Volume 2 - 2023 | https://doi.org/10.3389/fanes.2023.1187234
Background: Studies have suggested racial and ethnic-based disparities in the intensity of postoperative pain experienced by patients. The objective of this study was to compare the peak and average post-anesthesia care unit (PACU) pain intensity scores of children of non-Hispanic (NH) White race to those of children of other racial/ethnic groups.
Methods: Single-institution retrospective study of children (≤18 years) who had undergone cancer-related surgical procedures from June 2016 through April 2022. Multivariable logistic regression was used to assess the association between race/ethnicity and the peak and average PACU pain intensity scores.
Results: Of the 1,009 unique patients, 74 (7.3%) were Asian, 93 (9.2%) were NH-Black, 310 (30.7%) were Hispanic/Latino, 51 (5.1%) identified as “Other” race (NH-Other), and 481 (47.7%) were NH-White. The median age [interquartile range (IQR)] was 13.7 years (IQR, 8.2–16.6), and 517 (51.2%) were female.
In the multivariable analysis, the association between race/ethnicity and a peak PACU pain score greater than 3 was not significant (p = 0.062 for overall effect of race). However, upon comparing the peak PACU pain scores of children of other racial/ethnic groups to NH-White children, NH-Black children were 50.1% less likely than NH-White children to have a peak PACU pain score greater than 3 (odds ratio [OR], 0.499, 95% confidence interval [CI], 0.304–0.818; p = 0.006). Patient race/ethnicity was not associated with an average PACU pain score greater than 3 (p = 0.778).
In the sub-group analysis of children who had undergone orthopedic or open abdominal surgeries, the proportions of children with peak and average PACU pain scores which were greater than 3 were not significantly different across racial/ethnic groups (p = 0.250 and p = 0.661, respectively).
Conclusions: In this retrospective study of children who had undergone cancer-related surgery, NH-Black children had significantly lesser odds than NH-White children of having a peak PACU pain score of moderate or severe intensity. However, in the sub-group analysis of children who had undergone orthopedic or open abdominal procedures, peak and average PACU pain scores were not significantly different across racial/ethnic groups.
In the United States, an estimated 3.9 million surgical procedures are performed on children yearly (1). Despite the availability of analgesic options and guidelines, up to 60% of children experience postoperative pain of a moderate or severe nature (2, 3).
Studies suggest that the intensity of postoperative pain experienced by children may be associated with their race or ethnicity (4–7). For example, in a prospective observational study of 194 children who underwent tonsillectomy or adenoidectomy, Sadhasivam and colleagues reported higher peak post-anesthesia care unit (PACU) pain scores and higher odds of analgesic intervention in Black children than in White children (4). In another prospective observational study of 771 children who underwent a variety of elective outpatient surgical procedures, minority children had 63% higher odds of receiving intravenous opioids in the recovery room than white children (5).
However, perhaps underlying the complexity of this subject, a retrospective cohort study of children who underwent tonsillectomy and adenoidectomy reported lesser postoperative opioid requirement in Latino children than in White children (7). Furthermore, other studies, including a retrospective review of more than 29,000 cases, found no association between a child's race or ethnicity and their postoperative pain scores (8–10).
These differences in findings suggest that the interaction between a child's race and the intensity of postoperative pain is complex, and a better understanding of the factors that influence racial and ethnic disparities in postoperative pain intensity is required. To the best of our knowledge, no studies have examined whether racial or ethnic differences exist in the postoperative pain experienced by children who have undergone cancer-related surgical procedures. Filling this knowledge gap is important since pediatric cancer patients and their parents describe procedure-related pain as the most frequent and distressing source of pain during cancer treatments (11, 12).
To that end, we conducted a single-institution retrospective study to determine whether there was any difference between the PACU pain intensity scores of Non-Hispanic (NH) White children and those of children belonging to other racial or ethnic groups. Based on the results of most available pediatric studies on this subject, we hypothesized that PACU pain scores would be similar between children of different races or ethnicities.
This study was approved by the Institutional Review Board (IRB) of the University of Texas MD Anderson Cancer Center on August 1, 2022 (IRB # PA 16-0160). Due to the retrospective nature of this study, the requirement for written informed consent was waived. Study variables were stored on the Research Electronic Data Capture web platform hosted by the University of Texas MD Anderson Cancer Center. Our findings are reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (13).
The electronic data warehouse of the University of Texas MD Anderson Cancer Center was used to identify pediatric (≤18 years of age) patients who had undergone surgical procedures between June 1, 2016, and April 30, 2022. Only the index surgical encounter for each patient was considered to avoid over-representation of individual patients. Records without patient race or ethnicity as well as those without PACU pain intensity scores were excluded. The patient selection process is illustrated in the STROBE flow diagram (Appendix A).
Baseline and several potentially confounding perioperative variables were extracted from the institutional data warehouse sub-sections and summarized in Table 1. The primary exposure variable was the parent or guardian-provided race and ethnicity of their child. Accordingly, children were divided into the following groups: Asian, NH-Black, Hispanic/Latino, NH-Other, and NH-White. Of note, due to the small number of patients (n = 4), children of American Indian or Alaska Native race were combined with those who self-identified as “Other” race.
All surgical procedures were included. However, because of their potential for confounding, the most extensive and invasive categories of pediatric surgical procedures performed at our institution (thoracotomies, open abdominal, orthopedic, and craniotomy) were selected for comparison. Opioid doses were converted to weight-based morphine daily dose equivalents (MEDD/kg).
The primary outcome variables for this study were the highest and average pain intensity scores in the PACU.
Intraoperative anesthesia management was not standardized and varied according to the type of surgical procedure and physician preferences. Opioids were administered as boluses or as a combination of boluses and infusions. The opioids administered as boluses included fentanyl, hydromorphone, methadone, morphine, and sufentanil. Opioid infusions included fentanyl, sufentanil, and remifentanil.
The attending anesthesiologist for each case was responsible for PACU pain management orders. An institutional pediatric PACU pain management order-set with options for treating mild, moderate, or severe pain was used. However, this order-set allowed for physician discretion in the choices, dosages, and timing of the analgesics to be administered.
Assessment of postoperative pain intensity was carried out by PACU nurses and recorded on the appropriate 11-point (0—no pain, to 10—worst pain) rating scale. These included, Wong-Baker FACES and Modified Behavioral Pain Scales for non-verbal children, and the Verbal Numerical Rating Scale for older children. An initial pain assessment was carried out upon arrival at the PACU and every hour thereafter. Additional pain assessments were carried out thirty minutes after administering analgesic medications.
Patients' demographics, treatment, and clinical outcomes were summarized through descriptive statistics. Wilcoxon rank-sum test was used to compare location parameters of continuous distributions between patient groups. The Chi-square test or Fisher's exact test was used to evaluate the association between two categorical variables. Univariable and multivariable logistic regression models were fitted to estimate the effects of important covariates on the highest or average PACU pain score greater than 3. Statistical software SAS 9.4 (SAS, Cary, NC) and Splus 8.2 (TIBCO Software Inc., Palo Alto, CA) were used for the analyses.
A total of 1,009 unique patients were included in the analysis. Their median age [interquartile range (IQR)] was 13.7 years (IQR, 8.2–16.6), and 517 (51.2%) were female. Of the 1,009 children, 74 (7.3%) were Asian, 93 (9.2%) were NH-Black, 310 (30.7%) were Hispanic/Latino, 51 (5.1%) identified as “Other” race, and 481 (47.7%) were NH-White. Other baseline characteristics of the study population are shown in Table 1.
There were significant differences across racial/ethnic groups in the baseline characteristics of age (p < 0.001) and body mass index (p < 0.001), with NH-White children being older and the group of Hispanic/Latino children having the highest BMI. Anesthesia duration (p < 0.001), rates of orthopedic surgery (p = 0.016), amounts of opioids administered intraoperatively (p = 0.010), and the amounts of opioids administered in the PACU (p < 0.001) were also significantly different across racial/ethnic groups. Among these significant differences, the group of NH-White children had longer anesthesia duration, had a higher proportion of those who had orthopedic surgery and had higher amounts of opioids administered intraoperatively and in the PACU (Table 1).
In the univariable analysis (Table 1), the distribution of peak PACU pain scores was significantly different across racial or ethnic groups. Specifically, the group of NH-White children had a significantly higher proportion of patients with a peak PACU pain score greater than 3 (p = 0.001) and a significantly higher median value for the peak PACU pain score (p = 0.010).
Univariable analysis of the association between peak PACU pain scores and other patient characteristics is shown in Table 2. Compared to the group of children with a peak pain score greater than 3, those with a score of 3 or less were younger (difference in mean, −3.5 years [95% confidence interval (CI), −4.1, −2.9], p < 0.001), had lower body mass index (difference in mean, −1.5 [95% CI, −2.4, −0.7], p < 0.001), and were less likely to have a history of anxiety/depression (p < 0.001) or preoperative opioid use (p < 0.001).
Furthermore, the group of children with a peak pain score of 3 or less had shorter anesthesia duration (difference in mean minutes, −85 [95% CI, −98, −72], p < 0.001), received less opioids intraoperatively (difference in mean MEDD/kg, −0.23 [95% CI, −0.27, −0.18], p < 0.001) and in the PACU (difference in mean MEDD/kg, −0.101 [95% CI, −0.112, −0.090], p < 0.001), and were less likely to have undergone open abdominal (9/38 [23.7%] vs. 29/38 [76.3%]; p = 0.006) or orthopedic procedures (28/145 [19.3%] vs. 117/145 [80.7%]; p < 0.001). Notably, compared to NH-White children, NH-Black children had shorter anesthesia duration (median 126 min vs. 144 min), received less opioids intraoperatively (median 0.36 MEDD/kg vs. 0.39 MEDD/kg), and in the PACU (median 0.00 MEDD/kg vs. 0.04 MEDD/kg), and had a lesser proportion of orthopedic procedures (10.8% vs. 18.5%).
With the adjustment of gender, American Society of Anesthesiologists physical status class (ASA), orthopedic surgery, preoperative anxiety/depression, preoperative opioid use, regional anesthesia, age, and body mass index, the association between race and a peak PACU pain score greater than 3 was not significant (p = 0.062 for the overall effect of race). However, upon comparing children of other racial or ethnic groups to NH-White children (Table 3), NH-Black children had significantly lower odds than NH-White children of having a peak PACU pain score greater than 3 (odds ratio [OR], 0.499, 95% confidence interval [CI], 0.304–0.818; p = 0.006). Other factors which were independently associated with a peak PACU pain score greater than 3 included orthopedic surgery (OR, 3.651 [95% CI, 2.308–5.777]; p < 0.001), a history of anxiety or depression (OR, 2.050 [95% CI, 1.001–4.199]; p = 0.050), opioid use within 3 months before surgery (OR, 1.905 [95% CI, 1.121–3.236]; p = 0.017) and increasing age (OR, 1.147 [95% CI, 1.110–1.185]; p < 0.001).
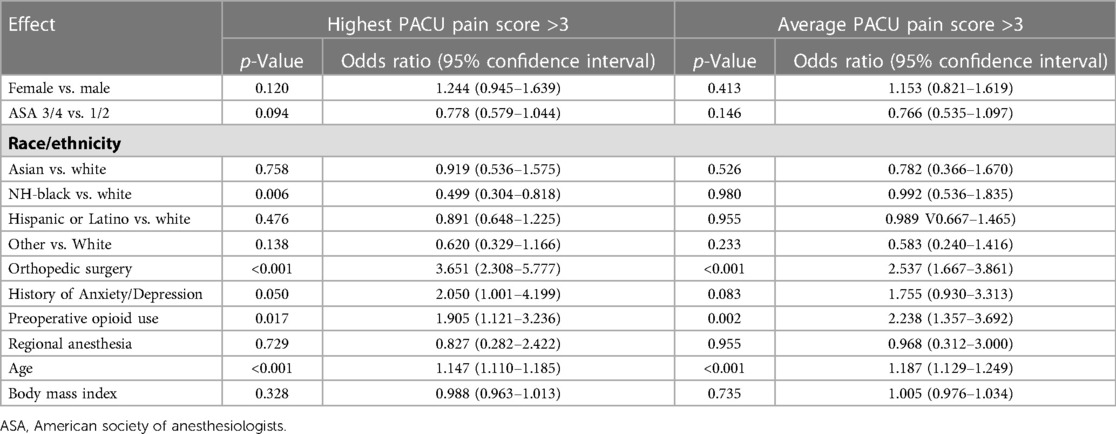
Table 3. Multivariable logistic regression analysis of the effects of important covariates on recovery room pain scores.
In the univariable analysis (Table 1), there was no difference across racial or ethnic groups in the proportions of children with an average PACU pain score greater than 3 (p = 0.273). However, the median of the average PACU pain scores differed significantly across racial or ethnic groups, with the group of NH-White children having the highest median value (p = 0.002).
Furthermore, compared to the group of children with an average PACU pain score greater than 3 (Table 2), those with a pain score of 3 or less were younger (difference in mean, −3.6 years [95% CI, −4.2, −3.0], p < 0.001), had lower body mass index (difference in mean, −2.3 [95% CI, −3.2, −1.3], p < 0.001), and more likely without a history of anxiety/depression (783/958 [81.7%] vs. 175/958 [18.3%]; p < 0.001) or preoperative opioid use (759/919 [82.6%] vs. 160/919 [17.4%]; p < 0.001).
In addition, the group of children with an average pain score of 3 or less had shorter anesthesia duration (difference in mean minutes, −68 [95% CI, −89, −47], p < 0.001), received less opioids during surgery (difference in mean MEDD/kg, −0.19 [95% CI, −0.26, −0.13], p < 0.001) and in the PACU (difference in mean MEDD/kg, −0.12 [95% CI, −0.14, −0.10], p < 0.001), and were more likely not to have undergone open abdominal (790/971 [81.4%] vs. 181/971 [18.6%]; p = 0.017) or orthopedic procedures (722/864 [83.6%] vs. 142/864 [16.4%]; p < 0.001). Similar to observations of the group of patients with peak PACU pain scores of 3 or less, the characteristics of the group with an average score of 3 or less were similar to factors associated with the group of NH-Black patients' experience.
In the multivariable analysis (Table 3), patient race was not associated with an average PACU pain score greater than 3 (p = 0.778). Factors that were independently associated with an average PACU pain score greater than 3 included orthopedic surgery (OR, 2.537 [95% CI, 1.667–3.861]; p < 0.001), preoperative opioid use (OR, 2.238 [95% CI, 1.357–3.692]; p = 0.002), and increasing age (OR, 1.187 [95% CI, 1.129–1.249]; p < 0.001).
In the sub-group analysis of children who had undergone orthopedic or open abdominal surgery (Table 4), there were no significant differences across racial/ethnic groups in the potentially confounding baseline characteristics of age (p = 0.420), anxiety/depression (p = 0.682), chronic pain (p = 1.000), and preoperative opioid use (p = 0.715). Furthermore, anesthesia duration (p = 0.321), intraoperative opioid dose (p = 0.076), and the use of regional anesthesia (p = 0.289) were similar across racial/ethnic groups.
PACU opioid requirements were similar across racial/ethnic groups (p = 0.507), and the proportions of children with peak and average PACU pain scores which were greater than 3 did not differ significantly across racial/ethnic groups (p = 0.250 and p = 0.661, respectively).
In this retrospective study of pediatric patients with cancer who had undergone surgery, race or ethnicity was not associated with peak or average PACU pain scores greater than 3. However, compared to NH-White children, NH-Black children had significantly lesser odds of having a peak PACU pain score greater than 3.
To the best of our knowledge, ours is the first study in the pediatric patient population to report lesser odds of peak PACU pain scores of a moderate or severe nature in NH-Black children than in NH-White children. There are several potential reasons for this difference in findings. Firstly, our study included a variety of surgical procedures, which despite the multivariable analysis, may have resulted in an unequal comparison of the invasiveness of the procedures. Specifically, the group of NH-Black children had shorter anesthesia duration, a lesser proportion of orthopedic procedures, and received lower doses of intraoperative opioids than NH-White children. This may suggest that NH-Black children had undergone less invasive or less painful procedures than NH-White children as a group.
In fact, in our sub-group analysis of children who had undergone orthopedic or open abdominal procedures, where the potentially confounding factors of anesthesia duration, intraoperative opioid administration, and PACU opioid administration were similar across racial/ethnic groups, peak and average PACU pain scores were not significantly different between children of different races or ethnicities. This may suggest that the intensity of postoperative pain experienced by our patient population was mostly influenced by the nociceptive response evoked by the surgical procedures.
Similar to the results of our sub-group analysis, Rosenbloom and colleagues reported similar intraoperative opioid administration and peak PACU pain scores between Black and White children who had undergone emergency appendectomy (8). Furthermore, in another retrospective study of 21,229 anesthetics of children who had undergone a variety of surgical procedures, intraoperative analgesic administration was not significantly different between Black and NH-White children. Postoperatively, Black and NH-White children had similar odds of having a pain score ≥4 on awakening. Of note, Asian children in this study had significantly lower odds of receiving non-opioid adjuncts intraoperatively and had significantly lower odds of reporting pain ≥4 on awakening (9).
On the other hand, in the prospective observational study of 194 children who underwent tonsillectomy and adenoidectomy, despite similar intraoperative morphine dosage, Sadhasivam and colleagues reported higher peak PACU pain scores and higher odds of analgesic intervention in Black children than in White children (4). The authors suggested higher morphine clearance in Black children may have contributed to their higher morphine requirements and higher pain scores.
It is not entirely clear why this finding differs from our observation. A primary reason may be due to differences in study design. Unlike our study, where several types of surgeries were included, and anesthesia and PACU care were tailored to individual patient needs, Sadhasivam and colleagues studied a specific type of surgical procedure and used standardized anesthesia and PACU protocols. This may have enabled them to detect patient-level differences in their particular surgical population. However, it is notable that in their prospective observational study of 771 children who underwent a variety of elective outpatient surgical procedures, Nafiu and colleagues observed that minority children had 63% higher odds of receiving intravenous opioids in the recovery room than white children (5). This suggests that in addition to the lack of standardization of surgical and anesthesia protocols, other factors may influence the findings in this area of research. Indeed, contrary to the findings of Nafiu and colleagues, in a cohort of children who had undergone tonsillectomy and adenoidectomy, Latino children had similar median postoperative pain scores as White children and received approximately 30% less opioid in the recovery room than White children (7). In addition to communication difficulties, the authors suggested that biological and cultural factors may have been responsible for the difference in findings.
Another potential explanation for our findings may be related to the setting in which our study was performed. Specifically, ours is single-institution study from a tertiary academic center where physician performance metrics including postoperative pain scores of patients are tracked and discussed annually with the individual physician. In addition, individual PACU nursing metrics including pediatric pain assessment, intervention, and reassessment are periodically audited. The latter may have particularly influenced the non-association between patient race or ethnicity and average PACU pain scores.
Reports of racial bias in pain assessment invariably raises concerns about provider-level bias in our study population (14). However, for the following reasons, we consider this unlikely. Firstly, NH-Black children received the least amounts of opioid in both the operating room and the PACU, whereas NH-White children had the highest or among the highest doses of opioids administered in both environments. This suggest that differences in PACU pain scores were more likely the result of differences in the invasiveness of procedures undergone. Secondly, over the duration of PACU stay, the odds of having an average PACU pain score greater than 3 was not significantly associated with patient race or ethnicity.
Similar to the results of previous studies, age, orthopedic surgery, preoperative opioid use, and anxiety or depression were each associated with higher odds for peak or average PACU pain scores of a moderate or severe nature (2, 15–17).
This study has its limitations. Firstly, including several types of surgical procedures in our analysis did not enable us to determine if there were any racial or ethnic-based differences in postoperative pain after specific procedures. In addition, there were significant differences in several patient characteristics, including age, types of surgery, and anesthesia duration which may have confounded our results. Although this may have been somewhat corrected in the sub-group analysis, the potential for confounding cannot be completely ruled out. Furthermore, studies have shown culture's influence on pain (18, 19). To that end, while disaggregating the study population into five racial/ethnic groups may have aided in identifying the observed disparity, it may not have sufficiently accounted for cultural differences within and across the racial/ethnic groups. Another significant limitation is the retrospective nature of this study and the subjective nature of the study endpoint. Thus, we cannot rule out biases in assessing pain intensity in non-verbal children.
In this study of 1,009 children who had undergone surgery at a comprehensive cancer center, NH-Black children had 50.1% lesser odds than NH-White children of having a peak PACU pain score of a moderate or severe nature. However, in a sub-group analysis of children who had undergone orthopedic or open abdominal surgeries, the proportions of children with peak and average PACU pain scores which were greater than 3 were not significantly different across racial/ethnic groups. Further studies are needed to better understand differences in postoperative pain scores between children of different races and ethnicities.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Institutional Review Board of the University of Texas MD Anderson Cancer Center. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
PO: study planning, methodology, manuscript preparation. JC: study conception, methodology, contribution to full manuscript and editing. LF: statistical analysis and editing of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rabbitts JA, Groenewald CB. Epidemiology of pediatric surgery in the United States. Paediatr Anaesth. (2020) 30(10):1083–90. doi: 10.1111/pan.13993
2. Kozlowski LJ, Kost-Byerly S, Colantuoni E, Thompson CB, Vasquenza KJ, Rothman SK, et al. Pain prevalence, intensity, assessment and management in a hospitalized pediatric population. Pain Manag Nurs. (2014) 15(1):22–35. doi: 10.1016/j.pmn.2012.04.003
3. Marchetti G, Vittori A, Tortora V, Bishop M, Lofino G, Pardi V, et al. Prevalence of pain in the departments of surgery and oncohematology of a paediatric hospital that has joined the project “towards pain free hospital”. Clin Ter. (2016) 167(5):156–60. doi: 10.7417/CT.2016.1948
4. Sadhasivam S, Chidambaran V, Ngamprasertwong P, Esslinger HR, Prows C, Zhang X, et al. Race and unequal burden of perioperative pain and opioid related adverse effects in children. Pediatrics. (2012) 129(5):832–8. doi: 10.1542/peds.2011-2607
5. Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Paediatr Anaesth. (2017) 27(7):760–7. doi: 10.1111/pan.13163
6. Nafiu OO, Thompson A, Chiravuri SD, Cloyd B, Reynolds PI. Factors associated with recovery room intravenous opiate requirement after pediatric outpatient operations. Anesth Analg. (2019) 128(6):1225–33. doi: 10.1213/ANE.0000000000003701
7. Jimenez N, Seidel K, Martin LD, Rivara FP, Lynn AM. Perioperative analgesic treatment in latino and non-latino pediatric patients. J Health Care Poor Underserved. (2010) 21(1):229–36. doi: 10.1353/hpu.0.0236
8. Rosenbloom JM, Senthil K, Long AS, Robinson WR, Peeples KN, Fiadjoe JE, et al. A limited evaluation of the association of race and anesthetic medication administration: a single-center experience with appendectomies. Paediatr Anaesth. (2017) 27(11):1142–7. doi: 10.1111/pan.13217
9. Jette CG, Rosenbloom JM, Wang E, De Souza E, Anderson TA. Association between race and ethnicity with intraoperative analgesic administration and initial recovery room pain scores in pediatric patients: a single-center study of 21,229 surgeries. J Racial Ethn Health Disparities. (2021) 8(3):547–58. doi: 10.1007/s40615-020-00811-w
10. Rosenbloom JM, De Souza E, Perez FD, Xie J, Suarez-Nieto MV, Wang E, et al. Association of race and ethnicity with pediatric postoperative pain outcomes. J Racial Ethn Health Disparities. (2023) 10(3):1414–22. doi: 10.1007/s40615-022-01327-1
11. Fuller C, Huang H, Thienprayoon R. Managing pain and discomfort in children with cancer. Curr Oncol Rep. (2022) 24(8):961–73. doi: 10.1007/s11912-022-01277-1
12. Tutelman PR, Chambers CT, Stinson JN, Parker JA, Fernandez CV, Witteman HO, et al. Pain in children with cancer: prevalence, characteristics, and parent management. Clin J Pain. (2018) 34(3):198–206. doi: 10.1097/AJP.0000000000000531
13. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. (2007) 18(6):800–4. doi: 10.1097/EDE.0b013e3181577654
14. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. (2016) 113(16):4296–301. doi: 10.1073/pnas.1516047113
15. Chung F, Ritchie E, Su J. Postoperative pain in ambulatory surgery. Anesth Analg. (1997) 85(4):808–16. doi: 10.1213/00000539-199710000-00017
16. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. (2013) 118(4):934–44. doi: 10.1097/ALN.0b013e31828866b3
17. Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. (2009) 111(3):657–77. doi: 10.1097/ALN.0b013e3181aae87a
18. O'Keefe EB, Meltzer JP, Bethea TN. Health disparities and cancer: racial disparities in cancer mortality in the United States, 2000–2010. Front Public Health. (2015) 3:51. doi: 10.3389/fpubh.2015.00051
19. Hsu DS, Ely S, Alcasid NJ, Banks KC, Santos J, Wei J, et al. Reduced opioid utilization and post-operative pain in Asian vs. Caucasian populations after video-assisted thoracoscopic surgery lobectomy with liposomal bupivacaine-based intercostal nerve blockade. Ann Palliat Med. (2022) 11(5):1635–43. doi: 10.21037/apm-21-2269
Keywords: race, ethnicity, pain, pediatric, postoperative
Citation: Owusu-Agyemang P, Feng L and Cata JP (2023) Race, ethnicity and postoperative pain in pediatric cancer patients: a single-institution retrospective study. Front. Anesthesiol. 2:1187234. doi: 10.3389/fanes.2023.1187234
Received: 15 March 2023; Accepted: 15 May 2023;
Published: 30 May 2023.
Edited by:
Hong Liu, UC Davis Health, United StatesReviewed by:
Katherine Forkin, University of Virginia, United States© 2023 Owusu-Agyemang, Feng and Cata. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pascal Owusu-Agyemang cG9hZ3llbWFuZ0BtZGFuZGVyc29uLm9yZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.