
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Anesthesiol. , 24 January 2023
Sec. Perioperative Medicine
Volume 2 - 2023 | https://doi.org/10.3389/fanes.2023.1014421
Introduction: The high-opioid technique was applied in the setting of congenital cardiac surgery on the belief of severe pain management and analgesic limitation in children along with delayed extubation time and other side effects. Thoracic nerve blockade demonstrated superior postoperative analgesia and stable hemodynamics and lower perioperative opioid consumption and related complications in cardiac surgery. SAPB is a fascial plane block technique that is considered an alternative to paravertebral block for perioperative thoracic pain relief, targeting intercostal never.
Cases presentation: We present 3 cases to describe the efficacy of SAPB as an alternative to opioid-sparing analgesia performed in infant patients after sternotomy in pediatric cardiac intensive care units. It was successfully used as a part of perioperative pain management. All patients were extubated early and recovered soon with no other complications.
Conclusion: SAPB lowers perioperative opioid consumption and related complications in cardiac surgery with satisfactory postoperative analgesia and stable hemodynamics.
Cardiac surgery with cardiopulmonary bypass in the pediatric population is associated with significant costs and morbidity, along with postoperative pain, pulmonary complications, and prolonged hospitalization. Although less invasive cardiac surgical techniques have emerged, median sternotomy is still the most commonly used approach for congenital cardiac surgery. High-dose opioids remain the mainstay for postoperative pain management after pediatric cardiac surgery despite opioid-related side effects [1, 2]. The demonstration that regional anesthesia can lower perioperative opioid consumption and related complications when used with general anesthesia has propelled renewed interest in regional anesthesia techniques [3, 4].
Ultrasound-guided serratus anterior plane block is a fascial plane block technique that deposits local anesthetics between the serratus anterior muscle and latissimus dorsi muscle, targeting the lateral cutaneous branches of the intercostal nerves. This has been reported as an alternative to paravertebral block for perioperative thoracic pain relief [5, 6]. In thoracic surgery, the validity and safety of this fascial plane block technique has been well established [7, 8]. Nevertheless, there is a lack of evidence proving the feasibility of SAPB applied in poststernotomy patients, especially in infants.
Patient 1 was a 10-month-old boy weighing 7 kg who was scheduled to undergo repair of partial endocardial cushion defects. Case 2 (infant boy) and case 3 (infant girl) were both 7 months old, weighing 5 and 7 kg, respectively, and presented for elective closure of ventricular septal defects only. Informed consent forms were obtained from caregivers.
After the surgical procedure was completed, the patient was transferred to the pediatric intensive care unit (PICU) and intubated. Upon confirming the stable respiratory and circulatory function of the patients, SAPB was performed using the ultrasound-guided technique described by Blanco et al. [5] with the patient in the supine position, if possible, with the upper arm resting over the head slightly. Under aseptic conditions, a 6–14 MHz linear transducer was scanned at the sagittal plane along the midaxillary line to orient the 3rd and 4th ribs while visualizing the pleura, latissimus dorsi muscle, serratus anterior muscle (Figure 1), and intercostal muscles (from superficial to the deepest). With respect to the ultrasound probe, a nerve block needle (22 G*50 mm) was inserted in the plane between the serratus anterior muscle and the intercostal muscles near the rib. When good views of the needle were verified, 0.2% ropivacaine 2.5 mg/kg was deposited in the fascial plane between the intercostal muscles and serratus anterior muscle. No further opioids were administered intravenously before extubation in the absence of a response to intubation stimulation. Rescue analgesia was started when the FLACC score was >4. Patients were extubated in the PICU once the extubation criteria were met (hemodynamically stable, normal arterial blood gas analysis, with peak inspiratory pressure <20 cm H2O and spontaneous breathing tidal volume >5 ml/kg). Postoperative pain assessment was performed 1, 6, 12, and 24 h after extubation with Face, Legs, Activity, Cry, Consolability (FLACC) scores by nurses in the PICU. For our 3 infants, the pain scores at 1 h post extubation were 1/10, 2/10, and 0/10, those at 6 and 12 h after extubation were all 1/10, and the scores at 24 h were 1/10, 0/10, and 1/10. No extra opioid drugs were needed in the first 12 h for any of the three infants. Regular oral ibuprofen suspension (1.25 ml) was taken every 8 h during the hospital stay (0.25 ml/kg). Enteral nutrition was well established 4 h after extubation. The urinary catheters were removed on the same day, and no urinary retention or repeated urinary catheterization occurred.
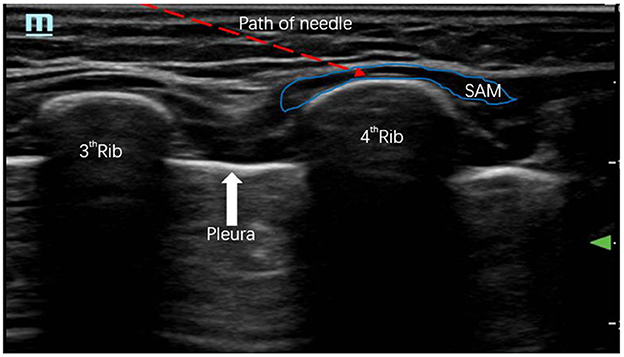
Figure 1. A 6–14 MHz linear transducer was scanned at the sagittal plane along the midaxillary line to orient the 3rd and 4th ribs while visualizing the pleura, serratus anterior muscle, and path of the needle.
In this case report, ultrasound-guided bilateral SAPB was performed in infants for median sternotomy postoperative pain management. It offers an opioid-sparing option for cardiac patients in the PICU for analgesia and shortens the intubation time for pediatric cardiac patients. In our 3 infant cases, the intubation time was <4 h, which is in accordance with the definition of “early” extubation time recommended (4–6 h) in pediatric fast-track cardiac surgery [9].
The pain after open heart surgery is intense and can be aggravated by respiratory movement, cough and position changes. Experiences of unalleviated pain in the early stage of life show negative consequences for sensory perception, immune function, and emotional health [10]. Moreover, changes in the mature brain and cognition have also been documented [11].
Pain after cardiac surgery includes not only the mid chest but also the anterior, lateral, and posterior chest wall [12]. Multimodality analgesics used in our study included intraoperative opioids, SAPB, ibuprofen and small amounts of opioids (12 h after surgery, if necessary). Early acute pain was released in a timely manner by different synergistic actions.
Multimodal pain management, including regional and systemic analgesia, is recommended for cardiac surgery analgesia [13]. Given the limitation of analgesic drug application in pediatric patients, regional anesthesia seems to be a legitimate option for opioid-sparing techniques in the population [14]. As part of the multimodal analgesic approach to pain management, many thoracic block techniques can be performed either in the back of the chest wall or in the front, targeting the thoracic intercostal nerves [15]. For patients after cardiac operation, the position change may cause unexpected complications. With limited positioning options, SAPB could be a more beneficial alternative to neuraxial block than paravertebral block or erector spinal block. Intercostal nerve block (ICNB) was also reported as an effective blockade for open heart surgery analgesia [8]; however, ICNB required repetitive applications and relatively more vascular exposure. Taking superficial wound infection around the surgical incision into consideration, transversus thoracic muscle plane block and parasternal block were not performed in these cases.
Although the analgesic mechanism of SAPB after median sternotomy is unclear, several cases have reported good analgesic effects in these patients [16, 17]. Some studies infer the fascial plane blocks exert an analgesic effect via a reduction in pectoral or intercostal muscle spasm [18]. Multimodal analgesic with SAPB were shown to be superior to opioids alone. These case reports may provide clues about SAPB in open heart surgery analgesia after surgery, and more randomized controlled studies and more fundamental studies of SAPB mechanisms are needed on this subject.
Because this study is a case report, it cannot be generalized to all patients. In addition, the superiority of deep serratus anterior plane block or superficial serratus anterior plane block is still a controversial, special issue that we did not discuss in this article. However, a randomized controlled trial is being performed to obtain clearer results in our center.
For the importance of pain management in enhanced recovery and limitation of analgesic drug application in children, we look forward to more random studies to confirm the safety and feasibility of these newly developed techniques/blocks in the pediatric population undergoing cardiac surgery in the ICU.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee on biomedical research of West China Hospital of Sichuan University (Approval No. 2021(429)). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
ZL was involved in data collection and follow-up assessments. MX and LD were responsible for literature search, study design, and finalized the manuscript. MX and YH drafted the manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Nelson KL, Yaster M, Kost-Byerly S, Monitto CLA. national survey of American Pediatric Anesthesiologists: patient-controlled analgesia and other intravenous opioid therapies in pediatric acute pain management. Anesth Analg. (2010) 110:754–60. doi: 10.1213/ANE.0b013e3181ca749c
2. Niesters M, Overdyk F, Smith T, Aarts L, Dahan A. Opioid-induced respiratory depression in paediatrics: a review of case reports. Br J Anaesth. (2013) 110:175–82. doi: 10.1093/bja/aes447
3. Jellish WS, Oftadeh M. Enhanced recovery after surgery for cardiac surgery: will we have the techniques needed to reduce opioid use and still provide appropriate analgesia? J. Cardiothorac Vasc Anesth. (2019) 33:547–8. doi: 10.1053/j.jvca.2018.10.022
4. Monahan A, Guay J, Hajduk J, Suresh S. Regional analgesia added to general anesthesia compared with general anesthesia plus systemic analgesia for cardiac surgery in children: a systematic review and meta-analysis of randomized clinical trials. Anesth Analg. (2019) 128:130–6. doi: 10.1213/ANE.0000000000003831
5. Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. (2013) 68:1107–13. doi: 10.1111/anae.12344
6. Patel SJ, Augoustides JGT. Serratus anterior plane block: a promising technique for regional anesthesia in minimally invasive cardiac surgery. J Cardiothorac Vasc Anesth. (2020) 34:2983–5. doi: 10.1053/j.jvca.2020.07.011
7. Altun GT, Arslantas MK, Dincer PC, Aykac ZZ. Ultrasound-guided serratus anterior plane block for pain management following minimally invasive repair of pectus excavatum. J Cardiothor Vasc Anesth. (2019) 33:2487–91. doi: 10.1053/j.jvca.2019.03.063
8. Kaushal B, Chauhan S, Saini K, Bhoi D, Bisoi AK, Sangdup T, et al. Comparison of the efficacy of ultrasound-guided serratus anterior plane block, pectoral nerves II block, and intercostal nerve block for the management of postoperative thoracotomy pain after pediatric cardiac surgery. J Cardiothorac Vasc Anesth. (2019) 33:418–25. doi: 10.1053/j.jvca.2018.08.209
9. Alghamdi AA, Singh SK, Hamilton BC, Yadava M, Holtby H, Van Arsdell GS, et al. Early extubation after pediatric cardiac surgery: systematic review, meta-analysis, and evidence-based recommendations. J Card Surg. (2010) 25:586–95. doi: 10.1111/j.1540-8191.2010.01088.x
10. Victoria NC, Murphy AZ. Exposure to early life pain: long term consequences and contributing mechanisms. Curr Opin Behav Sci. (2016) 7:61–8. doi: 10.1016/j.cobeha.2015.11.015
11. Attarian S, Tran LC, Moore A, Stanton G, Meyer E, Moore RP, et al. The neurodevelopmental impact of neonatal morphine administration. Brain Sci. (2014) 4:321–34. doi: 10.3390/brainsci4020321
12. Mueller XM, Tinguely F, Tevaearai HT. Pain location, distribution, and intensity after cardiac surgery. Chest. (2000) 118:391–6. doi: 10.1378/chest.118.2.391
13. Barr LF, Boss MJ, Mazzeffi MA, Taylor BS, Salenger R. Postoperative multimodal analgesia in cardiac surgery. Crit Care Clin. (2020) 36:631–51. doi: 10.1016/j.ccc.2020.06.003
14. Kar P, Ramachandran G. Pain relief following sternotomy in conventional cardiac surgery: a review of non neuraxial regional nerve blocks. Ann Card Anaesth. (2020) 23:200–8. doi: 10.4103/aca.ACA_241_18
15. Chaudhary V, Chauhan S, Choudhury M, Kiran U, Vasdev S, Talwar S, et al. Parasternal intercostal block with ropivacaine for postoperative analgesia in pediatric patients undergoing cardiac surgery: a double-blind, randomized, controlled study. J Cardiothorac Vasc Anesth. (2012) 26:439–42. doi: 10.1053/j.jvca.2011.10.012
16. Kupeli, I., and Adilovi,ć, A. Š. (2021). The “feasibility” and “safety” of ultrasound guided bilateral two level serratus anterior plane block in children with median sternotomy pain: a case series. J. Cardiothorac. Vasc. Anesth. 35, 270–273. doi: 10.1053/j.jvca.2020.03.020
17. Tewari P, Hajela K, Ahmad SS. Bilateral superficial serratus anterior plane block in a pediatric patient for post-operative analgesia undergoing asd repair via median sternotomy: a case report. Ann Card Anaesth. (2022) 25:116–8. doi: 10.4103/aca.aca_113_21
Keywords: serratus anterior plane block, intensive care unit, sternotomy, infant, case report
Citation: Xu M, Li Z, He Y and Deng L (2023) Case report: Ultrasound-guided bilateral serratus anterior plane block in intensive care unit—An alternative to opioid-sparing postoperative analgesia after sternotomy in infants. Front. Anesthesiol. 2:1014421. doi: 10.3389/fanes.2023.1014421
Received: 14 August 2022; Accepted: 09 January 2023;
Published: 24 January 2023.
Edited by:
Hong Liu, UC Davis Health, United StatesCopyright © 2023 Xu, Li, He and Deng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: LiJing Deng,  ZGVuZ19saWppbmdAMTYzLmNvbQ==
ZGVuZ19saWppbmdAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.