- Department of Anesthesiology, First Hospital of Jilin University, Changchun, Jilin, China
Purpose: To verify the feasibility of classic laryngeal mask airways (cLMA) combined with self-created adaptors in the interventional bronchoscopy of subglottic lesions for pediatric patients.
Methods: Three children who were diagnosed with upper airway lesions, subglottic stenosis (scar hyperplasia), and congenital laryngomalacia were respectively subjected to fiberoptic bronchoscopy (FOB) and therapeutic interventions. A classic laryngeal mask airway combined with a self-created adaptor was applied during the FOB procedures.
Results: In our cases, the vocal cord, glottis, trachea, and lesions were easily exposed, which provided an effective ventilation or oxygenation for the patients. Furthermore, both surgeons and patients were comfortable with the technique. Vital signs were stable during the procedures, including blood pressure, heart rate, and the saturation of pulse oximetry.
Conclusion: By retaining spontaneous breathing, the application of a classic laryngeal mask airway combined with a self-created adaptor is a feasible alternative method of airway management during FOB interventional procedures for pediatric patients.
Introduction
Upper airway lesions are difficult for patients to tolerate and are life-threatening [1]. A variety of endoscopic treatment modalities are available, including laser, electrocautery, and cryotherapy, as well as argon plasma coagulation (APC) via fiberoptic bronchoscopy (FOB) and rigid bronchoscope [2]. A flexible FOB is used for the examination and treatment of children and infants [3].
The airway is shared by anesthetists and surgeons during the resection of airway lesions, therefore, different degrees of airway obstructions might exist during the operation, bringing great challenges to both anesthetists and surgeons [4].
The laryngeal mask airway (LMA), a kind of supraglottic airway device, can be utilized for bronchoscopic procedures. Since the first introduction of LMAs into clinical practice, they have been widely applied due to their advantages including easy insertion and removal, effective airway management during general anesthesia, and permission for the passage of large FOBs [2]. These advantages render an easy reaching of subglottic lesions and reduce the possibility of ignition [3].
The use of classic laryngeal mask airways (cLMAs) combined with a self-created adaptor in the interventional bronchoscopy procedures of upper airway lesions and stenosis for pediatric patients is reported in this case series.
Consent
Institutional review board (IRB) approval was not required for this case report. Written informed consent was signed by the patients' parents regarding the use of their data for teaching and publication purposes.
Case presentation
Case 1
An 8-month-old boy was admitted to the Department of Pediatric Intensive Care Unit (PICU) in our hospital due to intermittent cough; he had been wheezing for 30 consecutive days with aggravation for 3 days. This boy was a test-tube baby born prematurely at 25 weeks, whose Apgar score was three at the first minute after delivery, and was successfully discharged from the hospital after 95 days of mechanical ventilation. The child was admitted to the Pediatric Respiratory Department for cough and wheezing, but the symptoms or signs were not relieved after 2 days of ceftazidime treatment. Therefore, he was transferred to the PICU. Physical examination results were generally normal except for a few rales in both lungs and throat singing sounds. A routine blood test provided the following results: WBC 12.84 × 109/L, RBC 4.09 × 1012/L, PLT 981 × 109/L, HGB 100 g/L; arterial blood gas analysis: pH 7.48, pCO2 48 mmHg, pO2 94 mmHg, Na+ 140 mmol/L, K+ 4.7 mmol/L, Ca++ 1.19 mmol/L, Glu 6.7 mmol/L, and Lac 0.5 mmol/L. A chest X-ray indicated an enhanced lung texture in both lungs. A homogeneous hyperechoic cyst was shown just below the glottis through the computed tomography (CT) of the neck with tracheal stenosis (Figure 1C).
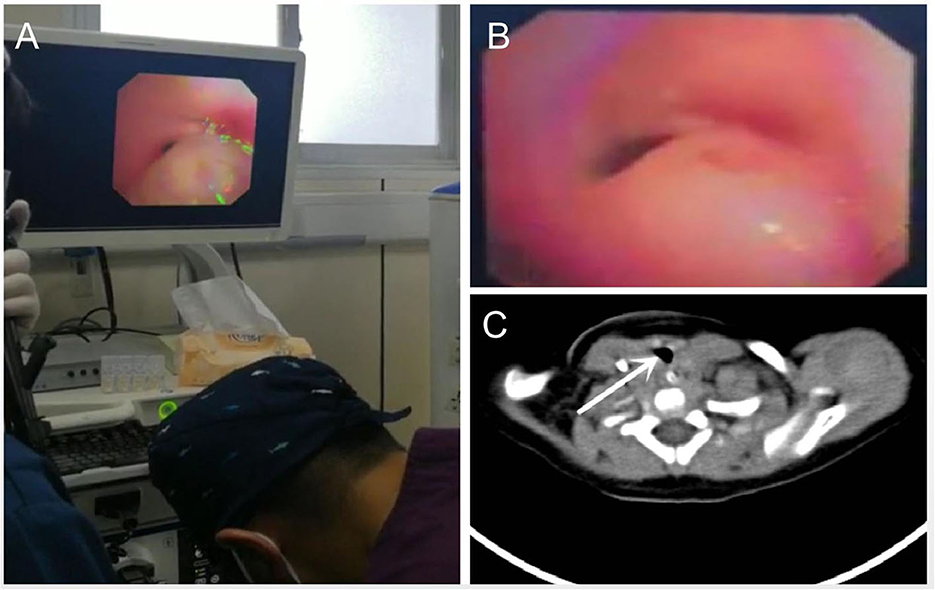
Figure 1. (A) During bronchoscopy, a large cyst was found just below glottis and on the right posterior wall of the trachea; (B) The cyst obstructed more than 90% of trachea; (C) Preoperative CT showing a subglottic mass and the cross-sectional area of the obstructed airway (white arrow).
The physicians of the PICU suggested that the patient undergo a bronchoscopy to determine the accurate location and nature of the cyst. To this end, 2% lidocaine was used for endotracheal topical anesthesia. The cyst sized 0.5 × 0.6 cm was located just below the glottis on the right posterior wall of the tracheal swing with breaths, which obstructed almost the entire (more than 90%) trachea as the patient was inspired (Figures 1A,B). During the bronchoscopy, the patient showed significant dyspnea combined with a descending oxygen saturation.
Considering both the patient's medical history and the results of the bronchoscopy, physicians of the PICU suggested that a subglottic mass holmium laser ablation via a bronchoscope be performed for the patient. We premedicated corticosteroids with methylprednisolone to prevent bronchospasm, along with a bronchodilator (aminophylline). Salbutamol was also prepared for intraoperative emergency bronchospasm. After watching the video through the bronchoscope, we decided to apply a cLMA (Derlar, Pudong, Shanghai, China) with the aperture bars transected (removal of the aperture bars may improve the observation of the glottis and reduce the drag on the bronchoscope—details are shown in Figure 2), so as to manage the airway and retain spontaneous breaths throughout the procedures. In the case of an acute airway obstruction and bleeding during lesion resection, an endotracheal tube was inserted through the mass to seal the upper airway. Because the surgeon had to change devices with different diameters during the procedures, we applied a self-created adaptor (EM07-004, Emedical, Huizhou, Guangdong, China) to prevent air leakage (details are displayed in Figure 3).
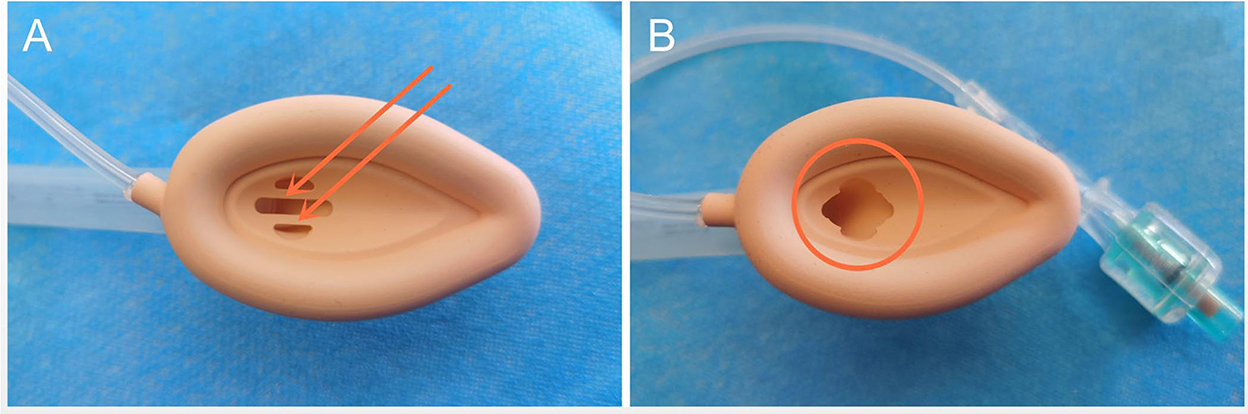
Figure 2. (A) We transected the aperture bars of the cLMA that red arrows indicate. (B) The cLMA with aperture bars were transected (red circle) to improve the view of the glottis and allow passage of the bronchoscope with low friction.
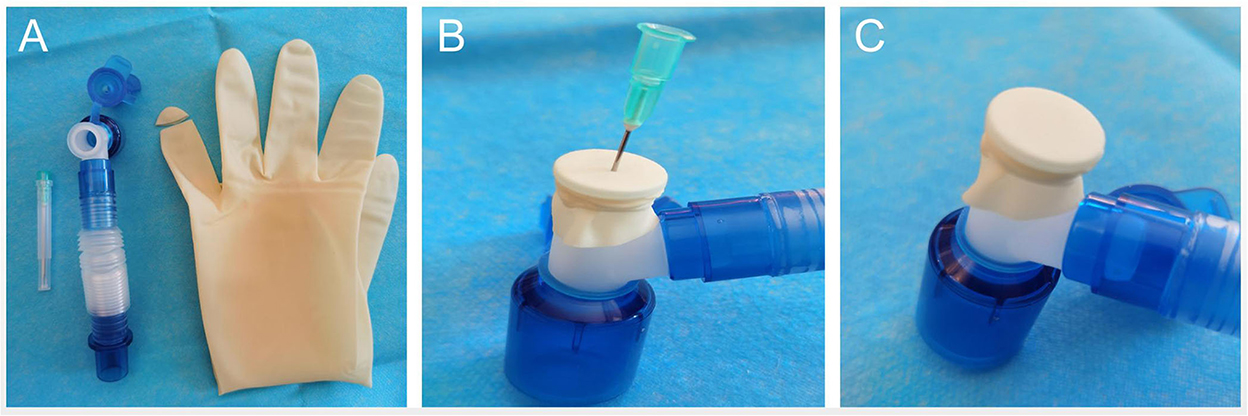
Figure 3. (A) It was made from a common adaptor with a cut finger of a glove fastened over the opening; (B) A small hole was made by a 22G syringe needle; (C) The self-created adaptor was presented.
The boy was kept fasting for 6 h before the operation, his peripheral venous access was established and monitored through electrocardiogram (ECG), and his noninvasive blood pressure (NIBP) and pulse oximetry (SpO2) were monitored after entry into the operating room. The preoperative vital signs of the boy were a SpO2 of 99% in room air with a NIBP of 82/45 mmHg, a heart rate (HR) of 145 beats/min (bpm), and a respiratory rate (RR) of 35 breaths/min. The induction of anesthesia was accomplished with the inhalation of 6% sevoflurane and the intravenous administration of 1 μg/kg dexmedetomidine for 10 min. Afterward, a 1.5-sized cLMA was promptly inserted without difficulty. We retained spontaneous breaths for the boy throughout the procedure. Proper placement of the cLMA was confirmed by end-tidal carbon dioxide (etCO2) tracing and the tidal volume (VT) shown on the ventilator. The vital signs were a SpO2 of 99%, a BP of 90/46 mmHg, a HR of 150 bpm, and an etCO2 of 35 mmHg after induction. The peak and mean airway pressures were 18 and 7 cmH2O respectively. The concentration of sevoflurane was adjusted to 5% with 6 L/min oxygen flow, and dexmedetomidine was decreased to 0.5 μg/(kg·h) for maintenance.
After double confirmation for the position of the cLMA and the injection of 0.7 mg/kg 2% lidocaine for the glottis as well as the endotracheal topical anesthesia through a 2.8-mm diameter bronchoscope (BF-XP260F, Olympus America, Center Valley, PA, USA), a foreign body forceps was inserted into the boy's trachea via the bronchoscope. When the cyst was managed with the bronchoscope, etCO2 was increased to 50 mmHg (Figure 4A). Thus, mechanical ventilation was administered for the boy with 60 ml of VT and RR of 22 bpm. The holmium laser technique (DHL-1-B, Dahua-laser, Wuxi, Jiangsu, China) was applied after the forceps could not rupture the cyst (Figure 5A). However, when lasers were applied, airway resistance was so dramatically increased that the boy could barely breathe, with etCO2 almost disappearing. We immediately switched to manual breathing for the boy, which increased his etCO2 (~18 mmHg), although it was still below the normal range (Figure 4B). When the pressure of manual ventilation was increased, we found that the large cyst could be blown away a little by the air. Fortunately, as the surgeon switched to devices with different diameters, there was no air leak as we expected and SpO2 remained at 99%. When the cyst was punctured by the holmium laser, a small amount of fluid flowed out. Fortunately, the fluid was immediately sucked by the surgeon, which did not cause barriers to aspiration. When the base of the cyst was punctured with the holmium laser, we had to transiently interrupt oxygen supply to prevent ignition. There was a small amount of eschar attached and the airway was clear after laser treatment (Figure 5B), meanwhile the airway resistance, etCO2, peak, and mean airway pressure returned to normal (Figures 4C,D). The surgery was accomplished, without tracheal bleeding or cysts.
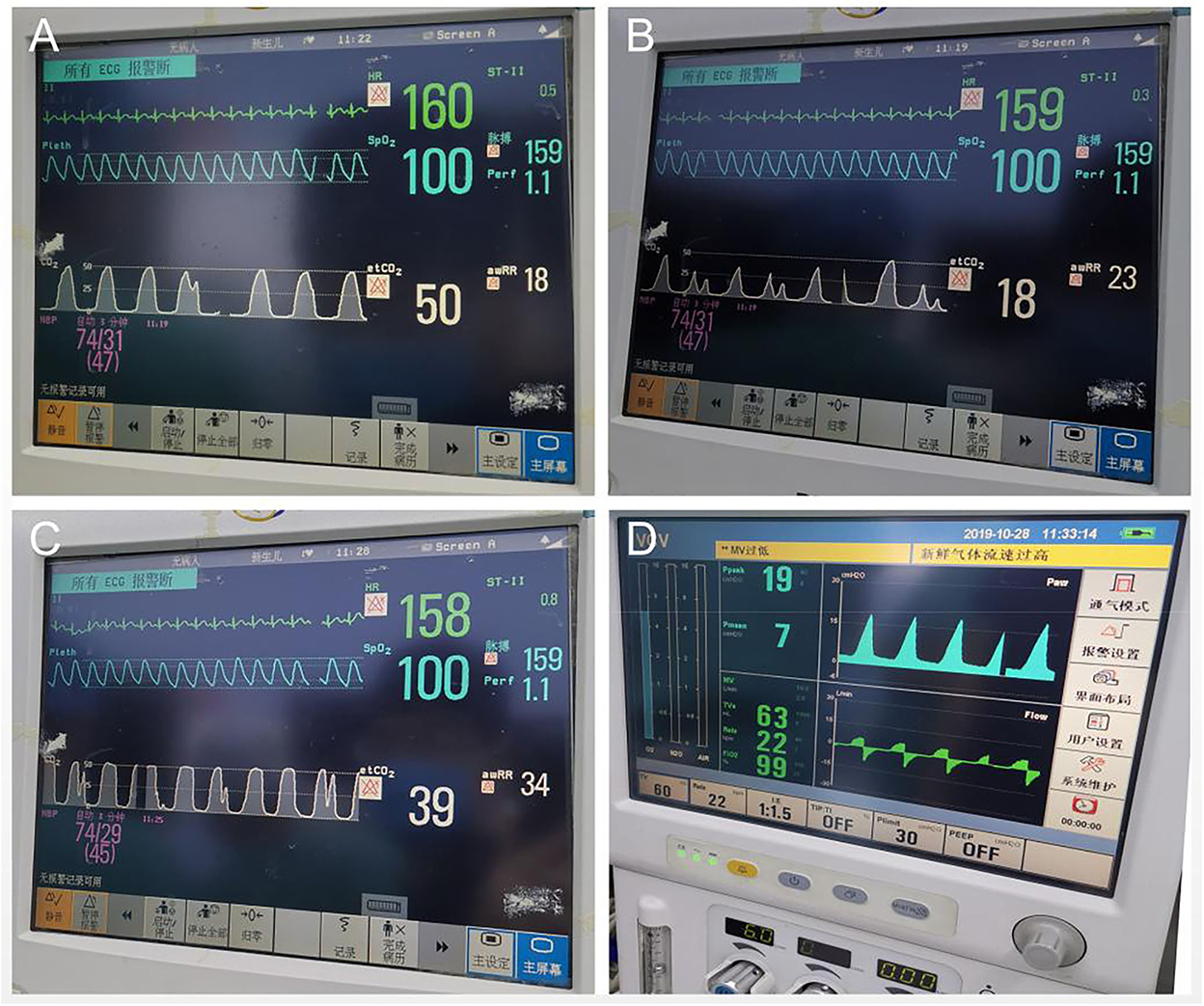
Figure 4. (A) When the surgeon treated the cyst with bronchoscope, etCO2 was increased to 50 mmHg; (B) When the laser was applied, airway resistance increased dramatically, the etCO2 almost disappeared. We switched to manual breathe for the boy immediately and got the value of etCO2 back, although it was still below the normal; (C,D) When the cyst was removed, the airway resistance, etCO2, peak and mean airway pressure were backed to normal.
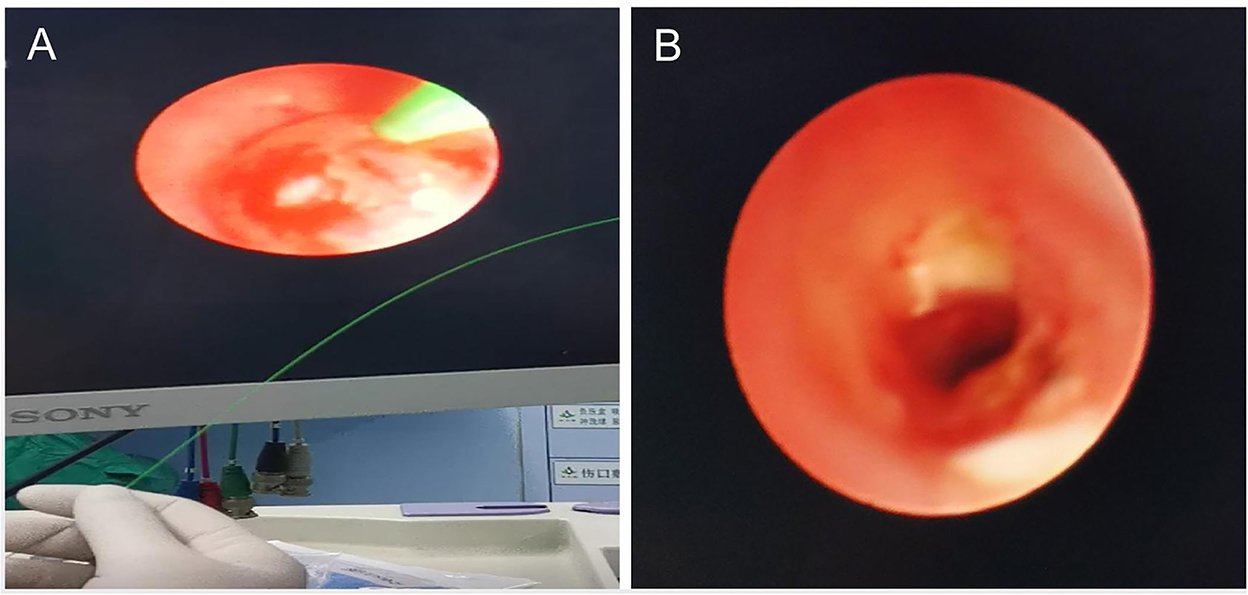
Figure 5. (A) The bronchoscope physician treated the cyst with holmium laser technique through our self-created adaptor via cLMA; (B) There was a small amount of eschar (white attachments) attached and the airway was clear after laser treatment.
The boy was transferred to the Department of Post Anesthesia Care Unit (PACU) where he woke up completely 10 min later. The cLMA was removed uneventfully. He was comfortable in the PACU and had no adverse complications. After observation in the PACU for an hour, the boy returned to the PICU.
The surgeon checked the trachea again through the bronchoscope 7 days after the surgery, at which time a clear airway was revealed with no stenosis or other cysts. The patient was discharged on the 10th postoperative day uneventfully.
Case 2
A 10-month-old boy presented intermittent cough, an inhaling throat, and hoarseness 5 months after esophagostomy and tracheal esophageal fistula repair surgeries. Endobronchial inflammation and tracheobronchial stenosis were found after preoperative bronchoscopy (Figure 6A). Scattered wet rales were found in both lungs during pulmonary auscultation. A routine blood test provided the following results: WBC 9.90 × 109/L, RBC 5.00 × 1012/L, PLT 366 × 109/L, HGB 133 g/L; arterial blood gas analysis: pH 7.35, pCO2 51 mmHg, pO2 46 mmHg, Na+ 141 mmol/L, K+ 4.8 mmol/L, Ca++ 1.33 mmol/L, Glu 4.9 mmol/L, and Lac 1.7 mmol/L. An enhanced lung texture was shown in both lungs via a chest X-ray. Cicatricial hyperplasia causing tracheal stenosis was shown through CT. After a preoperative consultation, the boy was scheduled to undergo a tracheal stenosis stent implantation. A FOB was performed after inserting a cLMA (size 1.5; Figure 6B). The tracheal mucosa under the glottis showed annular hyperplasia, and the lumen was narrow, accounting for approximately 50% of the airway. The trachea surgeon placed a silicone stent at a distance of 0.5 to 3 cm from the carina. The procedures were smooth. and there was no SpO2 desaturation or other unexpected conditions. The boy was treated with intravenous dexamethasone, budesonide, and ipratropium bromide atomization due to slight laryngeal edema after the surgery. The postoperative symptoms of the boy were significantly improved, and he was discharged on the fifth day after surgery following a FOB examination. No abnormalities were revealed in the bronchoscopy reexamination 1 month after the surgery (Figure 6C).

Figure 6. (A) Endobronchial inflammation and tracheobronchial stenosis were found during bronchoscopy; (B) The cLMA combined with the self-created adaptor is well sealed when inserteci into a FOB; (C) A reexamination of the bronchoscopy one month after the surgery did not reveal any abnormalities.
Case 3
A 2-month-old boy diagnosed with congenital laryngomalacia presented wheezing cough for 1 month and dyspnea for 7 days. Preoperative bronchoscopy showed that the posterior pharyngeal cavity was slightly soft, with the epiglottis crimp retracting when inhaling, which completely covered the glottis (Figure 7A). Obvious dry rales and wet wheezing were found in both lower lungs during preoperative auscultation. A routine blood test provided the following results: WBC 10.33 × 109/L, RBC 3.14 × 1012/L, PLT 352 × 109/L, HGB 81 g/L; arterial blood gas analysis: pH 7.44, pCO2 58 mmHg, pO2 80 mmHg, Na+ 138 mmol/L, K+ 3.6 mmol/L, Ca++ 1.22 mmol/L, Glu 5.1 mmol/L, and Lac 0.4 mmol/L. An enhanced lung texture was shown in both lungs with high-density shadows through a chest X-ray, indicating inflammation. The surgeon planned to perform a holmium laser epiglottoplasty for this boy. A 1.5-sized cLMA was prepared to maintain intraoperative ventilation, which, with aperture bars, was transected to improve the view of the epiglottis and allow the passage of the bronchoscope with low friction. Epiglottoplasty was successfully performed for the boy via the bronchoscopist using the holmium laser. Intraoperative vital signs were stable, and SpO2 was no <98%. The dyspnea of the boy was significantly relieved after the operation, and he left the hospital on the fifth day after surgery. The boy recovered very well after bronchoscopy reexamination on the 15th postoperative day (Figure 7B).
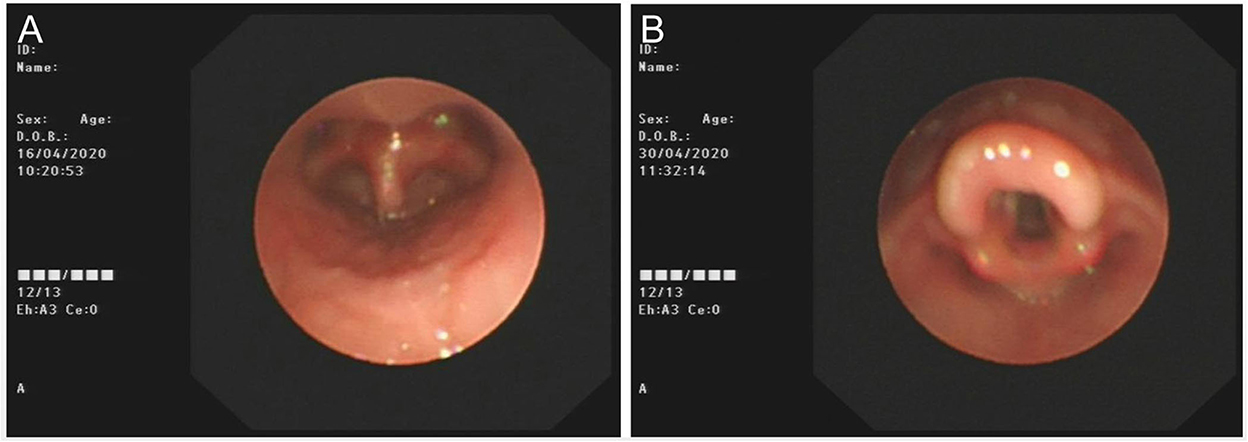
Figure 7. (A) The posterior pharyngeal cavity is slightly soft, with epiglottis crimp retracting when inhaling, completely covered the glottis; (B) The patient recovered very well after reexamining bronchoscopy on the 15th postoperative day.
Discussion
Primary tracheal tumors, mostly malignant, are rare, accounting for <0.1% of all tumors [5]. The optimal treatment for primary tracheal tumors is surgical resection, which is the only approach with a curative potential [6].
A variety of endoscopic treatment modalities are available, including lasers, electrocautery, cryotherapy, and APC via FOB, as well as rigid bronchoscope [2]. These methods require airway protection in addition to endotracheal intubation because lesions can cause tracheal stenosis, edema, bleeding, and burning in the airway during FOB thermal treatment [7].
Although multiple modes of airway management are accessible to secure the airway, for the optimal decision, the pathology and location of the lesions, the procedures to be scheduled, the instruments to be used during the surgery, and possible risks should all be considered in advance.
Cheng et al. [8] used the mode of high-frequency jet ventilation and retained spontaneous breathing in the rigid bronchoscopy. The advantages of high-frequency jet ventilation include a small tidal volume, low airway pressure, and suitability for open airways. However, high-frequency jet ventilation is accompanied with a decreased expiratory time, which is likely to cause complications such as gas retention, increased end-tidal CO2, and an uncertain end-expiratory positive pressure [9]. It can also be associated with pneumomediastinum, subcutaneous emphysema, and pneumothorax. Meanwhile, excessive pressure in the lungs can also impair venous return and lead to a dangerous reduction in cardiac output.
When the endotracheal lesions are huge, combined with CT, preoperative tracheotomy below the lesions is a safe method. For lesions in the middle one-third segment of the trachea whose treatment is the most difficult, the plan should be selected according to specific situations [10]. The lower tracheotomy can be successfully performed for patients with middle-segment lesions in the trachea by tilting their heads back [11].
The preoperative carbon dioxide retention indicates that the degree of airway obstruction is particularly serious, meanwhile respiratory muscle fatigue, spontaneous breathing, and mechanical ventilation are all at high risk of failure [12–14]. The patients should adopt a cardiopulmonary bypass to ensure normal gas exchange, which provides a safety guarantee for the next attempt of endotracheal intubation [15, 16].
The LMA is a supraglottic ventilation device, which can provide an excellent visual field of the glottis during FOB treatment, thus enabling the smooth resection of subglottic and endotracheal lesions [17, 18]. There are many advantages of the application of LMAs in pediatric airway surgeries: easy insertion, atraumatic benefit, optional spontaneous or mechanical ventilation, and the maintenance of airway patency without occupying surgical paths or overlying any possible pathology of interest [19].
In our case, the symptoms of the patient included intermittent cough and wheezing for 30 consecutive days, and the accurate location and nature of the lesions were confirmed through CT and bronchoscopy. A cyst sized 0.5 × 0.6 cm was located just below the glottis on the right posterior wall of the tracheal swing with breaths, which obstructed almost the entire (more than 90%) trachea as the patient was inspired. For an 8-month-old boy, endotracheal intubation could affect the surgery, meanwhile, a tracheotomy was an invasive operation and was rejected by the boy's family. Thus, we adopted the airway management method of inserting a cLMA while simultaneously retaining the boy's spontaneous breathing.
In order to prevent the emergent intraoperative complications, several strategies were established in advance. In the case of an acute airway obstruction caused by lesions falling off from the trachea, we planned to push the falling lesions to one of the common bronchi with a bronchoscope to ensure oxygen supply. If a massive hemorrhage occurred during the resection, an endotracheal tube would be inserted into the hemorrhage to seal the lower airway.
In general airway surgeries, a bronchoscope can be accessed through a small hole in the vent cap whose caliber is fixed. However, it often occurs that the surgeons need to change equipment with different diameters during the procedures, so the sealability cannot be elastically guaranteed by a normal vent cap through fitting the external diameters of different bronchoscopes. To this end, we adopted a self-created adaptor (details are shown in Figure 3) to ensure continuous ventilation throughout the procedures without air leakage utilizing the material characteristics of rubber. Surgeons were highly satisfied with the adaptor, which was another highlight in our case.
Oral and laryngeal laser therapy is widely applied; thus, the possibility of airway fire is increased. FiO2 was decreased to 30% during the lasering period. Fortunately, the boy did not experience any desaturation. Additionally, the power applied by the surgeons did not exceed 4W [20].
Conclusion
In conclusion, the boy showed a good tolerance to the cLMA and did not experience any intra- or postoperative desaturation or other complications. By retaining spontaneous breathing, the application of a cLMA combined with a self-created adaptor could be considered a reliable and secure alternative method of airway management for pediatric patients during interventional bronchoscopic procedures.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was signed by the patient's mothers for using the patient's data for teaching and publication purposes.
Author contributions
ZL: the chief anesthetist of these cases, analyses, and interpretations. XS: manuscript drafting and critical revision of important intellectual content. ZZ and NY: data analysis, interpretation of data, and follow-up. All authors contributed to the article and approved the submitted version.
Funding
The work was supported by Interdisciplinary Integration and Innovation Project of JLU (No. 419021421663).
Acknowledgments
First of all, the authors would like to express our sincere gratitude to ZL for his instructive advice and useful suggestions on this manuscript. We also thank ZZ and NY for data analyses, interpretations of data, and follow-up. In addition, the authors would like to thank the reviewers who have helped to improve the article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Veres J, Slavei K, Errhalt P, Seyr M, Ihra G. The Veres adapter: clinical experience with a new device for jet ventilation via a laryngeal mask airway during flexible bronchoscopy. Anesth Analg. (2011) 112:597–600. doi: 10.1213/ANE.0b013e3182080407
2. Fadaizadeh L, Hoseini MS, Bagheri M. Anaesthesia management during interventional bronchoscopic procedures: laryngeal mask airway or rigid bronchoscope. Turk J Anaesthesiol Reanim. (2014) 42:302–7. doi: 10.5152/TJAR.2014.85579
3. Yazbeck-Karam V, Aouad M, Baraka A. Laryngeal mask airway for ventilation during diagnostic and interventional fibreoptic bronchoscopy in children. Paediatr Anaesth. (2003) 13:691–4. doi: 10.1046/j.1460-9592.2003.01145.x
4. Rana SS, Balamurali S, Dronamraju VA, Batra YK, Vasishta RK, Kumar Y, et al. Unusual malignant tracheal tumour presenting with acute airway obstruction. Indian J Chest Dis Allied Sci. (2007) 49:49–51.
5. Macchiarini P. Primary tracheal tumours. Lancet Oncol. (2006) 7:83–91. doi: 10.1016/S1470-2045(05)70541-6
6. Grillo HC, Mathisen DJ. Primary tracheal tumors: treatment and results. Ann Thorac Surg. (1990) 49:69–77. doi: 10.1016/0003-4975(90)90358-D
7. Fadaizadeh L, Hosseini MS, Dabir S. Role of laryngeal mask airway in interventional bronchoscopy procedures for upper tracheal stenosis: case series. Middle East J Anaesthesiol. (2013) 22:223–7.
8. Cheng Q, Li L, Sun L, Wang B, Cai H. Anesthesia management for minimally invasive treatment of endotracheal masses. J Clin Anesthesiol. (2009) 25:71–2.
9. Rezaie-Majd A, Burian M, Bigenzahn W, Denk DM, Alloy A. Superimposed high frequency jet ventilation (SHFJV) for endoscopic laryngotracheal surgery, experiences with 1515 patients. Eur J Anaesthesiol. (2005) 22:69. doi: 10.1097/00003643-200505001-00243
10. Gao H, Yi J, Huang YG. Airway management and anesthesia for tracheal masses in 15 patients. Acta Acad Med Sin. (2013) 35:322−6. doi: 10.3881/j.issn.1000-503X.2013.03.000
12. Patel A. Pearce, Progress in management of the obstructed airway. Anaesthesia. (2011) 66:93–100. doi: 10.1111/j.1365-2044.2011.06938.x
13. Isono S, Kitamura Y, Asai T, Cook TM. Case scenario: perioperative airway management of a patient with tracheal stenosis. Anesthesiology. (2010) 112:970–8. doi: 10.1097/ALN.0b013e3181d4051a
14. Nouraei SAR, Giussani DA, Howard DJ, Sandhu GS, Ferguson C, Patel A. Physiological comparison of spontaneous and positive-pressure ventilation in laryngotracheal stenosis. Br J Anaesth. (2008) 101:419–23. doi: 10.1093/bja/aen171
15. Nakamura H, Taniguchi Y, Miwa K, Adachi Y, Fujioka S, Kamihira S, et al. Primary adenocarcinoma of the trachea resected using percutaneous cardiopulmonary support (PCPS). Ann Thorac Cardiovasc Surg. (2007) 13:338–40.
16. Chen H-h, Pan W, An X-x. Resection of tracheal tumor under cardiopulmonary bypass: a case report. Chin Med J. (2005) 118:1047-1049. doi: 10.1503/cmaj.1041549
17. Jameson JJ, Moses RD, Vellayappan U, Lathi KG. Use of the laryngeal mask airway for laser treatment of the subglottis. Otolaryngol Head Neck Surg. (2000) 123:100–2. doi: 10.1067/mhn.2000.107457
18. Chhetri DK, Long JL. Airway management and CO2 laser treatment of subglottic and tracheal stenosis using flexible bronchoscope and laryngeal mask anesthesia. Oper Tech Otolayngol Head Neck Surg. (2011) 22:131–4. doi: 10.1016/j.otot.2011.01.001
19. Somri M, Teszler CB, Tome R, Kugelman A, Vaida S, Gaitini L, et al. Flexible fiberoptic bronchoscopy through the laryngeal mask airway in a small, premature neonate. Am J Otolaryngol. (2005) 26:268–71. doi: 10.1016/j.amjoto.2005.01.001
Keywords: upper airway lesions, cLMA, self-created adaptor, spontaneous breath, pediatric
Citation: Song X, Yan N, Zhao Z and Li Z (2022) The application of classic laryngeal mask airway combined with a self-created adaptor in interventional bronchoscopy for pediatric patients: A case series and literature review. Front. Anesthesiol. 1:992072. doi: 10.3389/fanes.2022.992072
Received: 12 July 2022; Accepted: 23 August 2022;
Published: 30 November 2022.
Edited by:
Ke Peng, The First Affiliated Hospital of Soochow University, ChinaReviewed by:
Xisheng Shan, The First Affiliated Hospital of Soochow University, ChinaChristian Bohringer, UC Davis Medical Center, United States
Copyright © 2022 Song, Yan, Zhao and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiwen Li, bGl6aGl3ZW5Aamx1LmVkdS5jbg==
†ORCID: Zhiwen Li orcid.org/0000-0003-2970-5832
 Xuesong Song
Xuesong Song Na Yan
Na Yan Zhuang Zhao
Zhuang Zhao Zhiwen Li
Zhiwen Li