
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Anesthesiol., 30 November 2022
Sec. Neuroanesthesiology
Volume 1 - 2022 | https://doi.org/10.3389/fanes.2022.1041959
Background: Ketamine is a non-barbiturate general anesthetic commonly used in a variety of medical settings for pain and sedation. Its use in treatment for psychiatric illnesses has been increasing in recent years, showing promise in reducing depressive and suicidal symptoms in patients, particularly surgical patients. However, it has a history of association with schizophrenia-like and psychotomimetic symptoms following administration, particularly in patient populations with previous mental illness and youths.
Objective: Using a retrospective cohort study of patient records from a large health database, we sought to investigate psychiatric outcomes in age-specific cohorts following ketamine administration for orthopedic surgical anesthesia.
Methods: This was a retrospective analysis of the TriNetX health database. We identified all patients undergoing orthopedic surgeries with anesthesia. We then performed four total group analyses between cohorts of patients receiving ketamine and cohorts not receiving ketamine. We had three sets of analysis based on age stratification and one ageless: pediatric (<18 years), adult (18–60 years), elderly (>60 years), and a reference analysis of all patients.
Results: In 406,384 patients studied, nearly every measured event displayed an increased risk for patients receiving ketamine as part of their anesthesia. Apart from anhedonia, which had a decreased risk of occurrence, every event displayed increased incidence in at least two of the cohorts. For all but one event, nicotine use, the significant differences between groups were in concordance with each other.
Conclusion: Our findings suggest ketamine use should be investigated further in different age groups and corresponding psychiatric outcomes.
Ketamine is a non-barbiturate general anesthetic commonly used in a variety of medical settings for pain and sedation. Its use in treatment for psychiatric illnesses has been increasing in recent years, showing promise in reducing depressive and suicidal symptoms in patients, particularly surgical patients [1, 2]. However, it has a history of association with schizophrenia-like and psychotomimetic symptoms following administration, particularly in patient populations with previous mental illness and youths [3]. This association has prevented some providers from utilizing ketamine, while others prefer it for the ease of administration and reduction of polypharmacy [4].
Orthopedic surgery is a specialty with a wide variety of procedures, many of which require differing styles of anesthesia [5]. Therefore, anesthesiologists who are involved in orthopedic surgery need to be keenly aware of potential adverse effects of each medication they use. Research into psychiatric outcomes following ketamine administration has been relatively limited and has not been researched with sufficient power [6]. As ketamine becomes more common, psychiatric outcomes are an important consideration for practicing anesthesiologists, particularly those who supervise advanced care providers who may use ketamine in their routine anesthetic care. One specific area of ketamine use requiring further investigation is its use in different age groups and their corresponding psychiatric outcomes. Using a retrospective cohort study of patient records from a large health database, we sought to investigate psychiatric outcomes in age-specific cohorts following ketamine administration for orthopedic surgical anesthesia.
We performed a retrospective cohort study through the TriNetX database. This database contains electronic medical records from large healthcare organizations nationwide and has shown utility for a variety of medical fields including cancer and infectious disease [7, 8]. TriNetX, LLC is compliant with the Health Insurance Portability and Accountability Act (HIPAA), the US federal law which protects the privacy and security of healthcare data, and any additional data privacy regulations applicable to the contributing HCO [9]. TriNetX is certified to the ISO 27001:2013 standard and maintains an Information Security Management System (ISMS) to ensure the protection of the healthcare data it has access to and to meet the requirements of the HIPAA Security Rule. Any data displayed on the TriNetX Platform in aggregate form, or any patient level data provided in a data set generated by the TriNetX Platform only contains de-identified data as per the de-identification standard defined in Section §164.514(a) of the HIPAA Privacy Rule [9].
We identified all patients undergoing orthopedic surgery between June 4, 2002, and June 4, 2022, as the data were extracted on June 4, 2022. Using CPT codes, we identified orthopedic surgeries as surgical procedures occurring on the spine, shoulder, humerus, elbow, wrist, fingers, pelvis, hip joint, femur, knee joint, tibia, fibula, ankle joint, toes, or use of an arthroscope (CPT:1004038, 1004147, 1004279, 1004420, 1004616, 1004841, 1004987, 1005155, 1005312, and 1005610, respectively). We compared outcomes across these patients based on whether there was administration of ketamine. The following outcomes were assessed: anhedonia (ICD-10: R45.84), bipolar disorder (ICD-10: F31), altered cognition (ICD-10: R41), Delusional disorders (ICD-10: F22), depressive episode (ICD-10: F32), dizziness/giddiness (ICD-10: R42), hallucinations (ICD-10: R44.3), nicotine dependence (ICD-10: F17), non-mood psychotic disorders (ICD-10: F20-29), opioid related disorders (ICD-10: F11), other anxiety disorders (ICD-10: F41), other psychoactive substance disorder (ICD-10: F19), PTSD (ICD-10: F43.1), suicidal/homicidal ideation (ICD-10: R45.85), and sleep disorders not substance or psych related (ICD-10: F51). The time window for analysis began within 24 h of completion of the surgery and ended 30 days after, which is a time window established in prior anesthetic studies [10]. To best analyze the effect of ketamine itself, and analysis for each outcome only included patients without the outcome of interest prior to surgery.
Statistical analysis was performed using the TriNetX software. We performed 4 total group analyses between cohorts of patients receiving ketamine and cohorts not receiving ketamine. We had 3 sets of analysis based on age stratification and one ageless: pediatric (<18 years), adult (18–60 years), elderly (>60 years), and a reference analysis of all patients. Comparison between cohorts based on ketamine status was performed with a t-test to compare risk differences. Odds ratios were calculated from outcome incidence within each cohort. To prevent confounding variables, we balanced each set of analysis cohorts on age, sex, and race using propensity score matching with a difference between propensity scores <0.1. Significance for this study was set at p < 0.05. As this study contained only deidentified aggregate data, the Colorado Multiple Institutional Review Board (COMIRB) designated it as non-human research not in need of approval.
Following the matching on age, sex, and race, we had 203,192 patients in each of the reference ageless cohorts, for a total of 406,384 patients. For the pediatric cohorts, we had 19,024 pairs of matched patients, for a total of 38,048. For the adult cohorts, we had 102,896 pairs of matched patients, for a total of 205,792. For the elderly cohorts, we had 85,564 pairs of matched patients, for a total of 171,128. As the statistical analysis for each outcome excluded patients with the event of interest before the time window, the cohort size varied slightly for each outcome, as shown in Table 1.
Nearly every outcome of interest had significant risk increases for at least one of the ketamine cohorts, with 14 of 15 outcomes having at least two significant cohort differences. The overall ketamine cohort had decreased risk for anhedonia (OR = 0.8), and increased risk for all other outcomes, ranging from nicotine dependence (OR = 1.07) to opiate related disorders (OR = 3.26). Figure 1 contains the odds ratio for each outcome of interest, where numbers <1 indicate a reduced risk and numbers >1 indicating increased risks, and asterisks denoting a statistically significant difference. Eleven of 15 outcomes had results for specific events, including cohort size, absolute risk, odds ratio with 95% confidence interval, and p-values are compiled in Table 1.
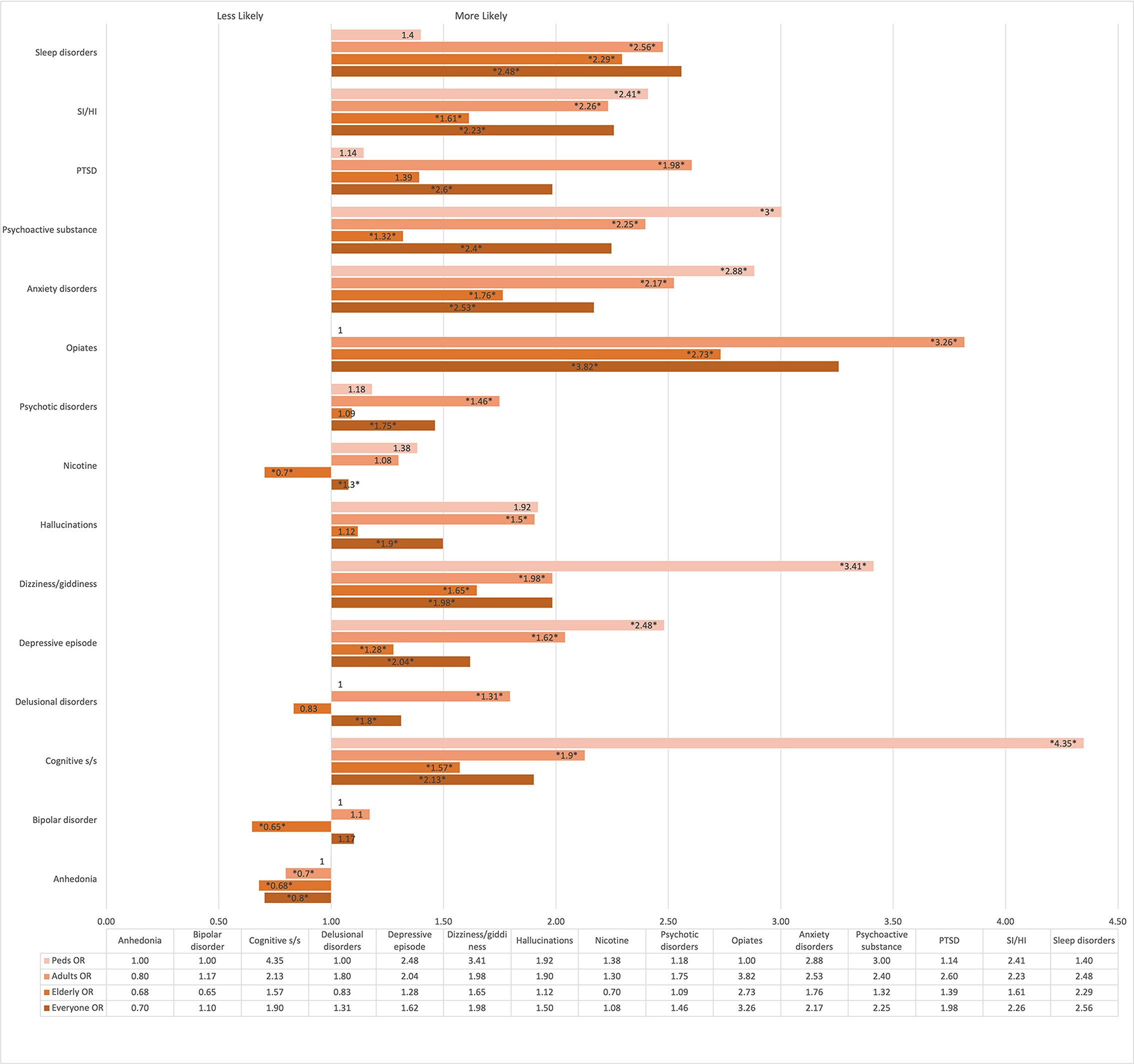
Figure 1. Odds ratio comparing cohorts receiving ketamine to matched peer cohorts. *Asterisked* values indicate a statistically significant 95% CI.
Nearly every measured event displayed an increased risk for patients receiving ketamine as part of their anesthesia. Apart from anhedonia, which had a decreased risk of occurrence, every event displayed increased incidence in at least two of the cohorts. For all but one event, nicotine use, the significant differences between groups were in concordance with each other, displaying the same direction of risk in varying amounts. The ageless cohort displayed increased risk of delusional disorders, but for all other events was in concordance with any significant differences in the three age-specific cohorts.
There were significant group differences as well. For example, patients under 18 displayed greater risks for nearly all outcomes compared to the other cohorts. Interestingly, the pediatric cohort also displayed the greatest number of no difference in event risk between ketamine and non-ketamine surgeries. This could be due to some of the events studied, such as PTSD, nicotine dependence, or opioid use disorder, which may be unlikely to occur in kids regardless of anesthesia type [11]. Another explanation for the increased risk could relate to increased provider attention due to the use of ketamine, as two of the largest increases were in dizziness/giddiness and altered cognition, both of which could arise as part of the post-operative state [12].
The cohort with patients over 65 had substantial differences as well. Compared to other cohorts, the elderly patients receiving ketamine had smaller differences in event risk for nearly all outcomes. Nicotine dependence even displayed decreased risk in elderly patients receiving ketamine compared to those not receiving ketamine, while for the adults and ageless cohorts, there was an increased risk. As with the child cohort, some of the difference in risk may be due to the overall prevalence of events within that age group; bipolar was only significantly decreased for the elderly population, who may have a decreased risk due to their age at baseline [13]. Similarly, due to our analysis eliminating any patients with the event of interest prior to their surgery, it is logical that the studied elderly cohort had lower rates of neuropsychiatric disorders, as these would have been present at some point in their lives before their surgery.
Finally, the cohort between 18 and 65 displayed risks between those of the elderly and pediatric cohorts for nearly all events. Notable differences were in the following events: sleep disorders, opioid dependence, psychotic disorders, and PTSD. For each of these, adults displayed the most increase in risk of the three cohorts, compared to matched patients not receiving ketamine. As with the other cohorts, some of the risk difference may be due to initial baseline prevalence; sleep disorders and mood disorders are commonly diagnosed in adulthood, which is also a larger spread of years compared to <18 or >60 [14]. Furthermore, providers who are aware of the possible effects of ketamine on psychiatric disturbances may be more likely to diagnose those disorders in patients receiving ketamine.
Risk factors for adverse reactions to ketamine are known and well-studied [15]. As sex, age, and race are three of the most common risk factors, we eliminated these from difference using cohort matching on those three characteristics. As mentioned above, we used nearest-neighbor matching to a propensity score of <0.1, so any impact of those three factors on the risk difference is low. However, there are multiple known factors such as obesity, duration of surgery, premedication with benzodiazepine use, and use of invasive devices (e.g., chest tube, intra-urethral catheter) that may have affected any of the groups [16, 17]. Additionally, while factors such as obesity are common in all ages, certain known factors such as attention-deficit/hyperactivity disorder (ADHD), parental anxiety, and rapid awakening are more common in children, which may have contributed to large difference between event risk in pediatric patients compared to adults [16]. Similarly, alcohol use and smoking may be more common in adults, while chronic lung disease and cognitive impairment are more common in elderly patients [12].
Our findings have a high level of utility for anesthesia providers, particularly those anesthesiologists in supervisory roles of advanced care providers such as nurse anesthetists. The ease of ketamine has led to an increasing number of providers utilizing it on a regular basis [15]. While this may lessen the need for observation and supervision during the induction phase, the responsible anesthesiologist must weigh the convenience of one medication against the potential increased risk of adverse psychiatric outcomes in the future. Furthermore, the drastic increase in particularly harmful outcomes, such as suicidal ideation, suggests that advanced care providers could benefit from increased training around ketamine specifically prior to utilizing it in anesthesia. The costs and benefits of ketamine vs. another anesthetic should be considered in every surgery, in contrast to routinely and automatically electing to use ketamine in all procedures.
As with all studies, certain limitations apply to our findings. Due to the deidentified, aggregate nature of our data, we were unable to control for certain things such as length of individual surgeries. Similarly, provider type was unable to be examined, which is of particular importance due to the large and increasing number of advanced-care providers in anesthesia, such as nurse anesthetists [18]. Additionally, the ketamine cohorts included patients who had different doses and dose-regimens for ketamine. Therefore, the dose-dependent effects of ketamine cannot be estimated- rather, this paper presents findings only on the associations with any ketamine use. Finally, we did not examine individual types of surgery, but rather examined any orthopedic surgeries using ICD-10 codes. While many orthopedic surgical procedures are similar, it is possible that ketamine use may have different outcomes in emergent, traumatic surgeries when compared to routine, elective surgeries.
Research into psychiatric outcomes following ketamine administration has been relatively limited and has not been researched with sufficient power. Our study presents a large analysis of nearly half a million patients, which furthers the debate within the anesthesia community on appropriate ketamine use. Our findings suggest that ketamine use should be investigated further regarding its use in different age groups and their corresponding psychiatric outcomes. As ketamine becomes more common, these findings offer interesting and useful information for the practicing anesthesiologist, particularly those who supervise advanced care providers who may use ketamine in their routine anesthetic care.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
As this study contained only deidentified aggregate data, the Colorado Multiple Institutional Review Board (COMIRB) designated it as non-human research not in need of approval.
EH had full access to the data and takes responsibility for the findings presenting. DS provided critical revision, data, and statistical analysis support. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Siegel AN, di Vincenzo JD, Brietzke E, Gill H, Rodrigues NB, Lui LMW, et al. Antisuicidal and antidepressant effects of ketamine and esketamine in patients with baseline suicidality: a systematic review. J Psychiatr Res. (2021) 137:426–36. doi: 10.1016/j.jpsychires.2021.03.009
2. Zhou Y, Wang C, Lan X, Zheng W, Li H, Chao Z, et al. The potential pro-cognitive effects with intravenous subanesthetic ketamine in adults with treatment-resistant major depressive or bipolar disorders and suicidality. J Psychiatr Res. (2021) 144:312–9. doi: 10.1016/j.jpsychires.2021.10.037
3. Beck K, Hindley G, Borgan F, Ginestet C, McCutcheon R, Bruggar S, et al. Association of ketamine with psychiatric symptoms and implications for its therapeutic use and for understanding schizophrenia: a systematic review and meta-analysis. JAMA Netw Open. (2020) 3:e204693. doi: 10.1001/jamanetworkopen.2020.4693
4. Jung SM. Drug selection for sedation and general anesthesia in children undergoing ambulatory magnetic resonance imaging. Yeungnam Univ J Med. (2020) 37:159–68. doi: 10.12701/yujm.2020.00171
5. Opperer M, Danninger T, Stundner O, Memtsoudis SG. Perioperative outcomes and type of anesthesia in hip surgical patients: an evidence based review. World J Orthop. (2014) 5:336–43. doi: 10.5312/wjo.v5.i3.336
6. Zhou Y, Sun W, Zhang G, Wang A, Lin S, Chan MTV, et al. Ketamine alleviates depressive symptoms in patients undergoing intracranial tumor resection: a randomized controlled trial. Anesth Analg. (2021) 133:1588–97. doi: 10.1213/ANE.0000000000005752
7. Hoffman MJ, Hale DD, Hale EW. Patient characteristics in oral cancer staging. Front Oral Health. (2022) 3:923032. doi: 10.3389/froh.2022.923032
8. Singer ME, Taub IB, Kaelber DC. Risk of myocarditis from COVID-19 infection in people under age 20: a population-based analysis. medRxiv. (2022) 3:923032. doi: 10.1101/2021.07.23.21260998
9. TriNetX. (2022). Available online at: https://trinetx.com/real-world-resources/publications/trinetx-publication-guidelines/ (accessed September 29, 2022).
10. Tzimas P, Samara E, Petrou A, Korompilias A, Chalkias A, Papadopoulos G. The influence of anesthetic techniques on postoperative cognitive function in elderly patients undergoing hip fracture surgery: general vs spinal anesthesia. Injury. (2018) 49:2221–6. doi: 10.1016/j.injury.2018.09.023
11. Bovin MJ, Wells SY, Rasmusson AM, Hayes JP, Resick PA. Post-traumatic Stress Disorder. Int J Occup Environ Med. (2012) 3:457–96. doi: 10.1002/9781118775349.ch23
12. Kotekar N, Shenkar A, Nagaraj R. Postoperative cognitive dysfunction - current preventive strategies. Clin Interv Aging. (2018) 13:2267–73. doi: 10.2147/CIA.S133896
13. Shobassy A. Elderly bipolar disorder. Curr Psychiatry Rep. (2021) 23:5. doi: 10.1007/s11920-020-01216-6
14. Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. (2005) 66:1254–69. doi: 10.4088/JCP.v66n1008
15. Moon TS, Smith KM. Ketamine use in the surgical patient: a literature review. Curr Pain Headache Rep. (2021) 25:17. doi: 10.1007/s11916-020-00930-3
16. Lee SJ, Sung TY. Emergence agitation: current knowledge and unresolved questions. Korean J Anesthesiol. (2020) 73:471. doi: 10.4097/kja.20097
17. Evans SI, Hale EW, Silverman MS. Mechanisms of bodily harm in emergency department youths with ADHD. Front Child Adolesc Psychiatry. (2022) 1:5. doi: 10.3389/frcha.2022.1033822
Keywords: neuropsychiatric symptoms, ketamine, ketamine—adverse effects, anesthesia, orthopedic
Citation: Mansour AE, Hale EW and Saks DS (2022) Psychiatric outcomes following ketamine administration for orthopedic surgical anesthesia. Front. Anesthesiol. 1:1041959. doi: 10.3389/fanes.2022.1041959
Received: 12 September 2022; Accepted: 07 November 2022;
Published: 30 November 2022.
Edited by:
Hossam El Beheiry, University of Toronto, CanadaReviewed by:
Dominic Pisano, Tufts Medical Center, United StatesCopyright © 2022 Mansour, Hale and Saks. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elijah W. Hale, ZWxpamFoLmhhbGVAY3VhbnNjaHV0ei5lZHU=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.