
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Aging, 22 May 2024
Sec. Interventions in Aging
Volume 5 - 2024 | https://doi.org/10.3389/fragi.2024.1337418
This article is part of the Research TopicObesity Across the Life CourseView all 4 articles
Introduction: Older adults are not protected from obesity, which has been linked to frailty, cognitive impairment, and other aging-related factors. Intensive lifestyle interventions have been shown to be effective for weight loss in older adults; however, these have typically been highly intensive and less feasible for dissemination. This analysis describes weight loss in a large-scale, commercially available, digital intervention in a subset of older adults.
Methods: Older adults (N = 20,443, males = 6,238; females = 14,205) between 65 and 85 years of age with overweight (43.3%) or obesity (46.7%) participated in an online, self-directed weight loss program. Behavioral-based content was delivered through weekly video lessons within an online platform that included weight and physical activity tracking, an online community, a reference library, and access to coaching support. Self-reported measures taken at the time of entry into the program were used for this analysis (demographics, height, body weight, and health status). Weight was reported across weeks of engagement in the curriculum.
Results: The average weight loss was −3.15 kg (95% CI: [−3.20, −3.11]) at 15.5 weeks. Weight loss was significantly greater in male individuals (−3.79 kg [95% CI: −3.89, −3.71]) versus female individuals (−2.87 kg [95% CI: −2.94, −2.82]) (p < 0.001), with a similar engagement in curriculum weeks. Percent weight loss was statistically significant for all age categories (p < 0.05) and self-reported health conditions (p < 0.05).
Discussion: Short-term weight loss was observed in older adults exposed to a low-touch, self-guided, and digital behavioral-based weight loss program. Weight loss was also observed even in the presence of various chronic health conditions.
Obesity continues to be a major public health concern due to its high prevalence and its association with chronic health conditions. These include, but are not limited to, cardiovascular disease, diabetes, some forms of cancer, musculoskeletal disorders, and mental health concerns (Jensen et al., 2014; Bray et al., 2018). Of significant concern, older adults are not protected from obesity and its deleterious health effects, with recent estimates of more than 40 percent of older adults classified as obese in the United States (Hales et al., 2020). Excess body weight in older adults has been linked to frailty, cognitive impairment, and other aging-related factors (Miller and Spencer, 2014; Crow et al., 2019; Villareal, 2023). This supports the need for interventions to promote sustainable weight loss in older adults. Moreover, it is important to understand the response to various interventions for weight loss in older adults as this may affect the types of programs offered specifically to individuals in this age group. This may have implications for access to care and financial coverage for intervention approaches targeting weight loss treatment.
Intensive lifestyle interventions have been shown to reduce body weight and improve various health outcomes in older adults. For example, the age-group analysis of the Diabetes Prevention Program showed that the intervention was equally effective for weight loss across all age groups and, compared to metformin for the prevention of type 2 diabetes, was more effective in older adults (≥60 years of age) than people of younger ages (Knowler et al., 2002). The intensive lifestyle intervention for Look AHEAD resulted in significantly greater weight loss at 1 year in older adults (65–74 years of age) compared to those of younger ages (Wadden et al., 2009). However, these interventions were conducted within the context of structured university-based research centers and involved intensive in-person individual or group-based sessions, which may not be feasible for broader dissemination.
Alternative delivery approaches to these interventions have been examined. For example, the MOVE-UP study was a community-based intervention based on Look AHEAD delivered by community healthcare workers. This was applied to older adults (∼67 years of age) and resulted in a median weight loss of 5% of baseline weight (Albert et al., 2022). This study also showed that 5% weight loss was associated with improvements in mobility and function. Alternative deliveries of the Diabetes Prevention Program that have included various digital and mobile approaches have also shown effectiveness for weight loss but have not been examined specifically in older adults (Fukuoka et al., 2015). Broadly available commercial weight loss interventions have reported the inclusion of older adults; however, these studies have not reported on the effectiveness of these programs for this population (Tate et al., 2022b). Thus, there is a need to examine dissemination of behavioral-based weight loss interventions that can be applied on a broad scale to older adults with obesity.
This analysis examined weight loss in a large-scale, commercially available, self-guided digital intervention in a subset of adults ≥65 years of age. Additionally, weight loss was examined based on the presence of selective cardiometabolic risk factors and other health conditions.
This analysis describes the weight loss outcomes of a large sample of 20,443 older adults with overweight or obesity who participated in an online, commercial weight loss program for company employees from March 2018 to November 2021. Companies provided program participation information to their employees via emails, post cards, and flyers at worksites. This was required for all workers, regardless of age. If benefits were retained after retirement, they were contacted through the appropriate entity providing these benefits. Participants from all regions of the continental United States voluntarily engaged in the program. This analysis used a de-identified dataset, and therefore, the requirement to document informed consent was waived, and the study was determined to be exempted from IRB oversight, according to the tenets of the US Department of Health and Human Services regulations at 45 CFR 46.
The weight loss program (Wondr Health™, formerly Naturally Slim, Dallas, TX, USA) is a completely digital intervention delivered on a web-based distance learning platform. This platform allowed participants to flexibly engage at their convenience from any location with Internet access. Content was delivered through video lessons released each week across a period of 52 weeks, with each week having 20–30 min of material. The program curriculum was designed with constructs found in standard behavioral weight loss interventions such as self-monitoring, goal setting, stimulus control, modification of eating habits, and problem solving with additional focus on evaluating hunger signals and mindful eating. The focus of the core curriculum included the following: 1) mindful eating and portion control, stimulus control, medical considerations, and weight Loss; 2) stop eating cues and introduction to physical activity; 3) stress and emotions, mindless eating, goal setting, and problem solving physical activity; 4) hidden sugar, mindful activities, and energy balance; 5) nutrition 101, stress management, physical activity, and weight maintenance; 6) weight fluctuations, food cravings vs. easily accessible food, and Centers for Disease Control and Prevention (CDC) exercise recommendations; 7) emotions and eating, importance of self-monitoring, and making exercise a habit; 8) grocery shopping and meal planning, metabolic syndrome, and cognitive behavioral techniques; 9) serving sizes, social support, dealing with saboteurs; and 10) review of eating skills and tools, maintaining motivation, and long-term action planning. An outline of all program objectives has been previously published (Earnest et al., 2019). The platform also includes a participant weight and physical activity tracking area, online support community, a reference library, and access to coaching to answer questions.
Recommendations for dietary modification did not focus on eliminating specific foods or macronutrients but did recommend reducing refined sugar and carbohydrate intake while maintaining protein consumption at 25%–30% of total calories. However, the focus of the dietary approach is based on the Mediterranean and DASH diets to promote a balanced nutrient intake. The program curriculum also encouraged participation in moderate-intensity physical activity, such as brisk walking, based on the NIH consensus development panel on physical activity and cardiovascular health (NIH Consensus Development Panel on Physical Activity and Cardiovascular Health, 1996). The physical activity components were developed to promote weight loss and cardiometabolic health, and therefore, the physical activity was not specifically tailored to include activity specific for older adults (e.g., balance training).
Demographic characteristics are based on a self-report by the participant at the time of enrollment in the program. Demographic characteristics include age, sex, and the presence of selective self-reported health conditions (hypertension, diabetes status [type 2 diabetes mellitus and pre-type 2 diabetes mellitus], non-alcoholic fatty liver disease, low high-density lipoprotein (HDL), elevated triglycerides, osteoporosis, and sleep apnea). Height and weight were also reported at baseline, and these data were used to compute body mass index (BMI, kg/m2). Moreover, weight was reported across weeks of engagement in the curriculum, which was used to compute absolute and percentage weight changes.
Statistical analysis was conducted using SAS on demand for academics. Statistical significance was a priori defined as p ≤ 0.05. Demographic characteristics are presented as mean ± standard deviation for continuous variables and as percentages for categorical variables. Absolute weight change and percent weight change were compared between male and female individuals using general linear modeling (GLM), with gender as a class variable. The GLM procedure uses the method of least squares to fit general linear models. Among the statistical methods available in PROC GLM are regression, analysis of variance, analysis of covariance, multivariate analysis of variance, and partial correlation. These analyses were repeated and included only those participants who completed ≥9 curriculum sessions, which is modeled after the same cut point used in prior published analyses (Earnest and Church, 2020). Percentage weight change adjusted for gender is presented as mean [95% confidence interval] across the number of weeks in the program (1–4, 5–8, 9–12, 13–16, and 17+).
Percentage weight change is also presented by age categories (65–69, 70–74, 75–79, and 80–85 years) and by the presence of self-reported health conditions. These data are presented for the entire sample and also by participants who completed ≥9 curriculum sessions. It has also been shown that a program based on the Diabetes Prevention Program attending nine or more sessions during the weight loss program was associated with improved outcomes related to the participant’s willingness to take action related to their weight loss behaviors, and therefore, this cut-point was adopted for the analyses in this study (Skrine Jeffers et al., 2019). By week 9 of the current intervention, participants had viewed content and practiced foundational weight management skills around awareness of hunger and satisfaction signals, basic nutrition, and meal planning, along with strategies to increase physical activity, improve sleep quality, manage stress and food cravings, elicit social support, and address challenges around emotional eating, social situations, and dichotomous thinking related to weight loss efforts. These data are presented as mean 95% confidence interval, with confidence intervals for the weight change that do not contain 0 as a value being significant at p < 0.05.
The demographic characteristics of the study sample are shown in Table 1. In general, the participants were 68.7 ± 3.8 years of age with a BMI of 32.0 ± 5.3 kg/m2 (43.3% overweight and 46.7% obese) and primarily female individuals (69.5%). The most prevalent chronic health condition was hypertension (64% of participants).
For the entire sample, based on the difference between the last weight obtained and baseline weight, weight loss measured was −3.15 kg (95% CI: [-3.20, −3.11]), and this was achieved following an average of 15.5 weeks of participation in the curriculum (Table 2). Weight loss was significantly greater in male individuals −3.79 kg (95% CI: [-3.89, −3.71]) versus female individuals (−2.87 kg [95% CI: −2.94, −2.82]) (p < 0.001), with male individuals completing 15.6 and female individuals completing 15.5 weeks of the curriculum. Similar findings were observed when the data were examined for percent weight loss. These analyses were repeated for participants who completed ≥9 weeks of the curriculum, with this being 19.2 weeks for male individuals and 19.7 weeks for female individuals. The weight loss expressed as changes in kg or percent weight change remained significantly greater in male individuals compared to female individuals (see Table 2).
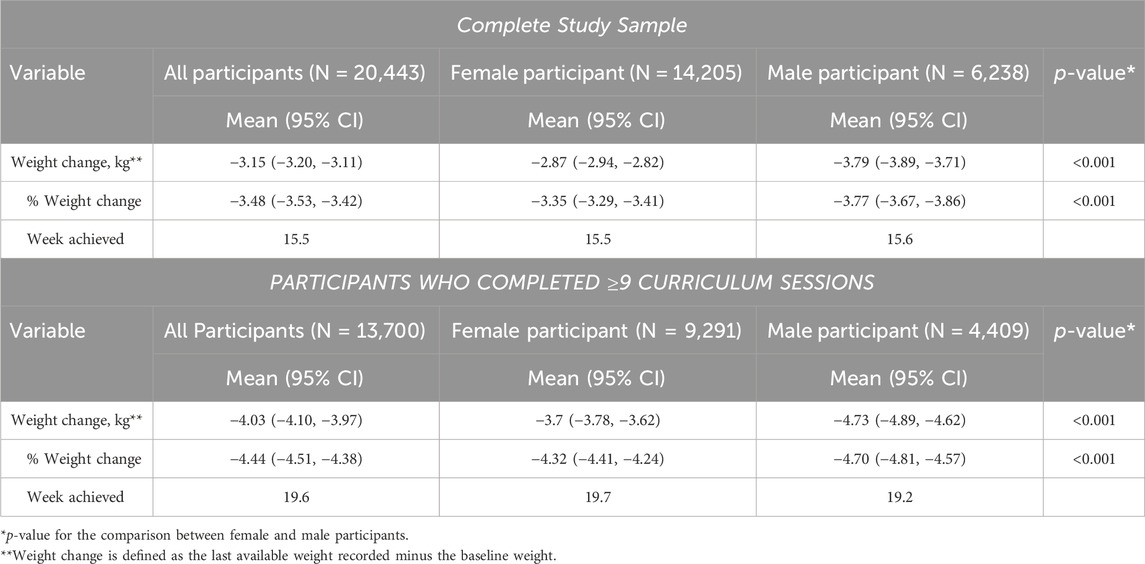
Table 2. Absolute and percent weight change for the entire sample, participants, and participants who completed ≥9 curriculum sessions.
The data were further examined by weeks of participation in the program adjusted for age and gender (Figure 1). Weight loss increased across program participation from 1.1% with engagement in 1–4 sessions to 5.3% with engagement in 17 or more sessions.
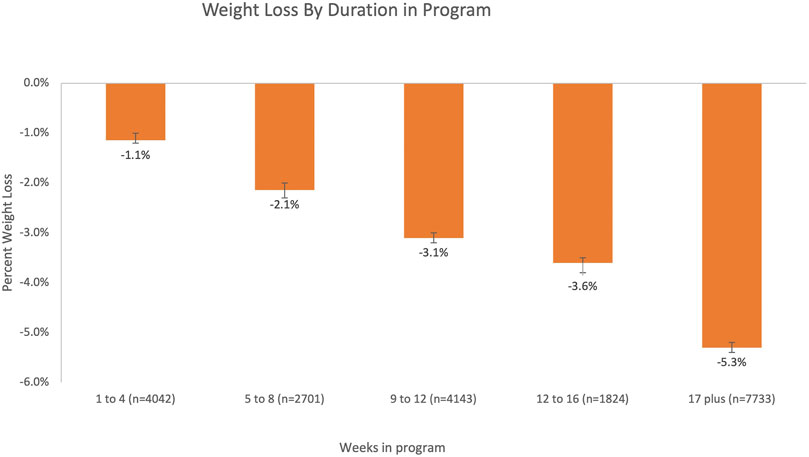
Figure 1. Percent weight loss (mean [95% CI]) by duration of participation in the program adjusting for age and gender.
Percentage weight loss obtained from the final measured weight was examined by age category controlling for sex (Table 3). Percent weight loss was statistically significant (p < 0.05) for all age categories. A similar pattern of results was observed when only participants who completed ≥9 curriculum sessions were examined.
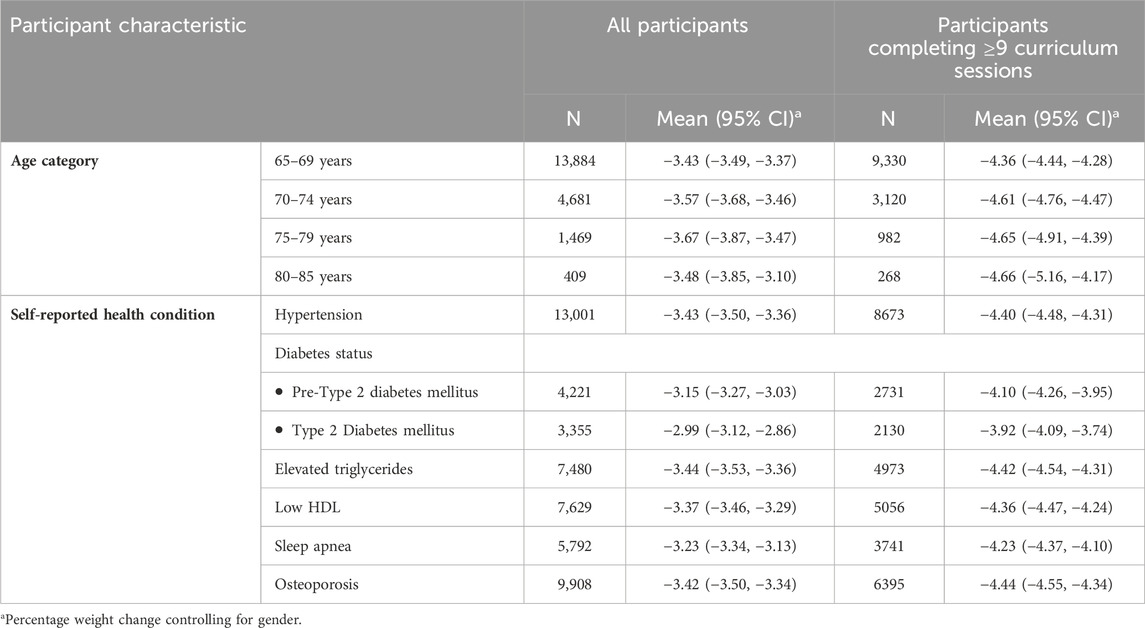
Table 3. Percentage weight change by age category and the presence of selective health conditions for all participants and for participants completing ≥9 curriculum sessions.
Percentage weight loss obtained from the final measured weight was also examined by different self-reported health conditions controlling for sex (Table 3). Percentage weight loss was statistically significant (p < 0.05) for all the health conditions examined. A similar pattern of results was observed when only participants who completed ≥9 curriculum sessions were examined.
This study reports on the weight change observed, following a large-scale, commercially available, self-guided digital intervention applied in a subset of adults ≥65 years of age. Key findings from this study include that weight loss occurred in all age strata, in all chronic health conditions examined, was greater in male vs. female individuals, and was greater as engagement in the study was lengthened.
This study demonstrated the overall weight loss of −3.15 kg (95% CI: −3.20, −3.11), and this was observed at a mean exposure of 15.5 weeks of intervention. The weight loss improved to −4.03 kg at a mean of 19.6 weeks for participants who completed at least 9 sessions of the curriculum. By comparison, the Diabetes Prevention Program was delivered by DVD, which is similar to the video-based curriculum evaluated in this study, and 12-week weight loss of −5.4 kg was observed in adults with a mean age of 59.7 years (Kramer et al., 2010). When implemented in adult senior/community centers, the Diabetes Prevention Program demonstrated a 6-month weight loss of −5.4 kg in adults with a mean age of 62.8 years (Kramer et al., 2018). The 6-month weight loss in an in-person behavioral intervention delivered by community health workers to older adults (mean age = 67.7 years) was approximately 5% of baseline weight (Albert et al., 2022). Similar to this current study, these weight losses reflect the change from baseline in response to these interventions and not the difference compared to a comparison group.
In comparison to other commercial weight loss programs, a 12-week online weight loss intervention resulted in the weight loss of −2.7 kg compared to −1.3 kg in a newsletter control condition (Thomas et al., 2017). However, when delivered as an in-person intervention, weight loss was −4.9 kg at 6 months (Rogers RJ et al., 2020), and others have reported that this commercial program resulted in −3.8 kg at 3 months (Tate et al., 2022b), and these weight losses reflect the change from baseline. However, although these other studies recruited participants across a broad age range, weight loss results were not presented by age category, and therefore, the effectiveness of these other commercial approaches on weight loss in older adults is unclear. In the current study, weight loss was significant in the age categories of 65–69, 70–74, 75–79, and 80–85 years. It is also important to note that significant weight loss was also observed even in the presence of any of the chronic health conditions examined in this study.
The data presented represent weight loss in older adults. To provide a comparison, an in-person weight loss intervention with young adults (18.5–35.9 years) demonstrated a median weight loss of −7.8 kg at 6 months (25th percentile = −12.2 and 75th percentile = −3.7 kg) (Jakicic et al., 2015). In another study of young adults (29.4 ± 4.3 years), a 6-month personal coaching intervention resulted in a −1.92 kg (95th percent CI: −3.17 to −0.67 kg) weight change compared to control (Svetkey et al., 2015). In a study of middle-aged adults (50.9 ± 11.0 years), a 6-month Internet-based intervention resulted in a −4.49 kg (S.E. = 0.38 kg) weight change (Tate et al., 2022a). This may suggest that the weight loss observed in older adults in response to a self-guided digital intervention in the current study is blunted compared to what might be observed in younger age groups using different intervention platforms.
An important finding of this study was that weight loss improved as engagement in the intervention increased. These findings are consistent with other behavioral interventions for weight loss that demonstrated an association between a greater intervention engagement and greater weight loss (Wadden et al., 2009; Jakicic et al., 2015). Stevens et al. suggested that a weight change of <3% reflects weight stability, whereas reducing weight by at least 3% reflects weight loss, and this was achieved in this study when engagement in the intervention was at least 9–12 weeks in duration (Stevens et al., 2006). Moreover, a weight loss of at least 5% has been suggested to reflect a clinically meaningful weight loss, and this was achieved when the engagement in the intervention was at least 17 weeks. This may reflect the need to examine strategies for retaining engagement in this type of weight loss intervention for at least these durations to achieve a meaningful weight loss in older adults.
There are numerous strengths to this study that warrant recognition. This is a study of a commercially available, self-guided digital intervention and reports on weight loss observed in older adults. This study also included a large sample of older adults, both men and women, and participants with various health conditions, which may reflect real-world engagement in a weight loss intervention. However, despite these strengths, there are limitations that warrant consideration. The outcome data on weight along with the presence of chronic health conditions are based on the self-report. Moreover, weight rather than body composition data is available, and therefore, it is not possible to determine the contribution of lean body mass and adipose tissue to weight loss, which may be clinically important for older adults. This study also used an observational, non-randomized design and did not include a non-intervention comparison condition. Data are not available to determine the level of engagement of the participant while viewing the videos, and measures of dietary intake, eating behavior, and physical activity are not available to determine how these factors may contribute to the outcomes observed.
In summary, weight loss was observed in older adults 65–85 years of age with exposure to a commercial program that is low-touch, self-guided, and digital behavioral-based. This study also showed that a longer engagement in the program was associated with greater weight loss, suggesting the need for strategies to enhance the engagement of participants in this type of program. Of potential clinical importance, weight loss was also achieved even in the presence of various chronic health conditions. These findings warrant replication along with future studies to understand how the magnitude of intentional weight loss observed in this study may be associated with reducing chronic health conditions in older adults.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
This analysis used a de-identified dataset, and therefore, the requirement to document informed consent was waived, and the study was determined to be exempted from IRB oversight, according to the tenets of the US Department of Health and Human Services regulations at 45 CFR 46. The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin.
RR: conceptualization, writing–original draft, and writing–review and editing. MD: data curation, formal analysis, and writing–review and editing. DJ: data curation, formal analysis, and writing–review and editing. JJ: writing–review and editing. TC: conceptualization, formal analysis, validation, and writing–review and editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
RR is a consult for Wondr Health, Inc. MD and DJ are employed by Wondr Health, Inc. JJ is on the scientific advisory board of Wondr Health, Inc. TC is the Chief Medical Officer of Wondr Health, Inc.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Albert, S. M., Venditti, E. M., Boudreau, R. M., Kieffer, L. A., Rager, J. R., Zgibor, J. C., et al. (2022). Weight loss through lifestyle intervention improves mobility in older adults. Gerontologist 62 (6), 931–941. doi:10.1093/geront/gnab048
Bray, G. A., Heisel, W. E., Afshin, A., Jensen, M. D., Dietz, W. H., Long, M., et al. (2018). The science of obesity management: an endocrine society scientific statement. Endocr. Rev. 39 (2), 79–132. doi:10.1210/er.2017-00253
Crow, R. S., Lohman, M. C., Titus, A. J., Cook, S. B., Bruce, M. L., Mackenzie, T. A., et al. (2019). Association of obesity and frailty in older adults: NHANES 1999-2004. J. Nutr. Health Aging 23 (2), 138–144. doi:10.1007/s12603-018-1138-x
Earnest, C. P., and Church, T. S. (2020). Retrospective examination of class attendance on corporately sponsored weight loss programming: the naturally Slim experience. J. Occup. Environ. Med. 62 (3), e102–e110. doi:10.1097/jom.0000000000001807
Earnest, C. P., Dufour, C., and Church, T. S. (2019). The efficacy of Re-engaging in an employer sponsored weight loss program. J. Occup. Environ. Med. 61 (12), e516–e522. doi:10.1097/jom.0000000000001746
Fukuoka, Y., Gay, C. L., Joiner, K. L., and Vittinghoff, E. (2015). A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am. J. Prev. Med. 49 (2), 223–237. doi:10.1016/j.amepre.2015.01.003
Hales, C. M., Carroll, M. D., Fryar, C. D., and Ogden, C. L. (2020). Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 360, 1–8.
Jakicic, J. M., King, W. C., Marcus, M. D., Davis, K. K., Helsel, D., Rickman, A. D., et al. (2015). Short-term weight loss with diet and physical activity in young adults: the IDEA study. Obes. (Silver Spring) 23 (12), 2385–2397. doi:10.1002/oby.21241
Jensen, M. D., Ryan, D. H., Apovian, C. M., Ard, J. D., Comuzzie, A. G., Donato, K. A., et al. (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American college of cardiology/American heart association task force on practice guidelines and the obesity society. J. Am. Coll. Cardiol. 63 (25 Pt B), 2985–3023. doi:10.1016/j.jacc.2013.11.004
Knowler, W. C., Barrett-Connor, E., Fowler, S. E., Hamman, R. F., Lachin, J. M., Walker, E. A., et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N. Engl. J. Med. 346 (6), 393–403. doi:10.1056/NEJMoa012512
Kramer, M. K., Kriska, A. M., Venditti, E. M., Semler, L. N., Miller, R. G., McDonald, T., et al. (2010). A novel approach to diabetes prevention: evaluation of the Group Lifestyle Balance program delivered via DVD. Diabetes Res. Clin. Pract. 90 (3), e60–e63. doi:10.1016/j.diabres.2010.08.013
Kramer, M. K., Vanderwood, K. K., Arena, V. C., Miller, R. G., Meehan, R., Eaglehouse, Y. L., et al. (2018). Evaluation of a diabetes prevention program lifestyle intervention in older adults: a randomized controlled study in three senior/community centers of varying socioeconomic status. Diabetes Educ. 44 (2), 118–129. doi:10.1177/0145721718759982
Miller, A. A., and Spencer, S. J. (2014). Obesity and neuroinflammation: a pathway to cognitive impairment. Brain Behav. Immun. 42, 10–21. doi:10.1016/j.bbi.2014.04.001
NIH Consensus Development Panel on Physical Activity and Cardiovascular Health (1996). Physical activity and cardiovascular health. NIH consensus development panel on physical activity and cardiovascular health. JAMA 276 (3), 241–246.
Rogers Rj, K. S., Collins, K., Raybuck, S., Collins, A. M., Marcin, M. L., Foster, G. D., et al. (2020). Observations of a commercial weight loss program on physical function and selected CVD risk factors. Transl. J. Am. Coll. Sports Med. 5 (12), e000137. doi:10.1249/TJX.0000000000000137
Skrine Jeffers, K., Castellon-Lopez, Y., Grotts, J., Mangione, C. M., Moin, T., Tseng, C. H., et al. (2019). Diabetes prevention program attendance is associated with improved patient activation: results from the prediabetes informed decisions and education (PRIDE) study. Prev. Med. Rep. 16, 100961. doi:10.1016/j.pmedr.2019.100961
Stevens, J., Truesdale, K. P., McClain, J. E., and Cai, J. (2006). The definition of weight maintenance. Int. J. Obes. (Lond) 30 (3), 391–399. doi:10.1038/sj.ijo.0803175
Svetkey, L. P., Batch, B. C., Lin, P. H., Intille, S. S., Corsino, L., Tyson, C. C., et al. (2015). Cell phone intervention for you (CITY): a randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology. Obes. (Silver Spring) 23 (11), 2133–2141. doi:10.1002/oby.21226
Tate, D. F., Kraschnewski, J. L., Martinez, C., Diamond, M., Veldheer, S., Hwang, K. O., et al. (2022a). A cluster-randomized controlled trial of automated internet weight-loss programs in primary care: role of automated provider feedback. Obes. (Silver Spring) 30 (12), 2363–2375. doi:10.1002/oby.23506
Tate, D. F., Lutes, L. D., Bryant, M., Truesdale, K. P., Hatley, K. E., Griffiths, Z., et al. (2022b). Efficacy of a commercial weight management program compared with a do-it-yourself approach: a randomized clinical trial. JAMA Netw. Open 5 (8), e2226561. doi:10.1001/jamanetworkopen.2022.26561
Thomas, J. G., Raynor, H. A., Bond, D. S., Luke, A. K., Cardoso, C. C., Foster, G. D., et al. (2017). Weight loss in Weight Watchers Online with and without an activity tracking device compared to control: a randomized trial. Obes. (Silver Spring) 25 (6), 1014–1021. doi:10.1002/oby.21846
Villareal, D. T. (2023). Editorial: obesity and accelerated aging. J. Nutr. Health Aging 27 (5), 312–313. doi:10.1007/s12603-023-1922-0
Keywords: weight loss, obesity, aging, intervention, digital health
Citation: Rogers RJ, Doherty M, Jones D, Jakicic JM and Church TS (2024) Impact of a digital employer-based weight loss program on individuals age 65 or older. Front. Aging 5:1337418. doi: 10.3389/fragi.2024.1337418
Received: 13 November 2023; Accepted: 25 April 2024;
Published: 22 May 2024.
Edited by:
Penny Breeze, the University of Sheffield, United KingdomReviewed by:
Pilar Pérez-Ros, University of Valencia, SpainCopyright © 2024 Rogers, Doherty, Jones, Jakicic and Church. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Renee J. Rogers, cnJvZ2VyczEwQGt1bWMuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.