
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Aging , 10 November 2022
Sec. Healthy Longevity
Volume 3 - 2022 | https://doi.org/10.3389/fragi.2022.1002367
This article is part of the Research Topic Age as an Effect Modifier of Nutrition and Health View all 5 articles
 Ahmed Muhye Seid1,2*
Ahmed Muhye Seid1,2* Netsanet Fentahun Babbel3
Netsanet Fentahun Babbel3Background: Improved health care and rising life expectancy are creating a growing pool of old age people all over the world, including Africa. Malnutrition in the old age people is associated with both short- and long-term negative health outcomes. However, the reported burdens of malnutrition are fragmented and inconsistent, where more compiled evidence is warranted to aid decision-makers. Hence, this paper is aimed to estimate the pooled prevalence of malnutrition among old age people in Africa.
Methods: A systematic search for research reporting the prevalence of malnutrition among old age people (aged above 60 years) was conducted from HINARI/PubMed and Google Scholar databases using combination keywords. Published articles in English language starting from January 2000 to October 2021 were screened. We presented the results based on the standard for reporting systematic review and meta-analysis of observational studies. A random-effect meta-analysis was done to estimate the prevalence of malnutrition along with the 95% confidence intervals. The publication bias was assessed using the funnel plot.
Results: A total of 1,442 studies were retrieved based on the search strategy, where only 36 studies (n = 15,266 participants) reported from 11 African countries were included for meta-analysis. The reported prevalence of malnutrition ranges from 2.2 to 77.3% across Africa. Overall, the pooled prevalence of malnutrition was 18% (95% CI: 15-22; I2 = 98.1; p < 0.001). The prevalence is higher in the Central Africa (3.8%; 95% CI: 3.2-4.4), in the community (3.1%; 95% CI: 2.7-3.7), and among advanced age (3.5%; 95% CI: 2.3-5.4).
Conclusion: The prevalence of malnutrition in African old age people is high and differs by setting, assessment tool, and country of residence. Hence, due attention to geriatric nutrition is mandatory, and the need for a valid, reliable, and simple screening tool should be thought of.
The global demographic structure of the population is changing dramatically, notably in Africa, due to several social and economic milestones (United Nations Department of Economic and Social Affairs Population Division, 2019). These resulted in expanding population, improved life expectancy, and increased population size of older ages (World Health Organization, 2017; United Nations Department of Economic and Social Affairs Population Division, 2019). The absolute number of old age people [60 years and above (World Health Organization, 2002)] is expected to grow more rapidly in the coming decades than in any other part of the world (United Nations Department of Economic and Social Affairs Population Division, 2019).
In Africa, the risk of malnutrition among older people is a major challenge to the health care system and needs special and urgent attention. The usual food production practices, marketing style, and living standards have all contributed to an increase in the use of low-cost, packaged products that are high in fat, energy, and salt and yet low in nutritional quality. More importantly, poor infrastructure and limited resources, combined with conflict and poor access to healthcare services, are factors that contribute to the overwhelming levels of malnutrition and food insecurity on the continent (FAO and ECA, 2018). The lack of policy direction for old age people, combined with prevalent chronic illnesses, adds a significant load to the growing burden of malnutrition (Saka et al., 2019; United Nations and Department of Economic and Social Affairs PD (UNDESAPD), 2016). Due to these and other aggravating factors, the African government’s commitment to ending all forms of malnutrition by 2030 (United Nations and United Nations Sustainable Development, 2019) will be difficult to achieve.
While any age group may suffer from malnutrition, it is most common among old age people due to the changes in physiological, psychosocial, and health characteristics of individuals in this age group (Guisado-Clavero et al., 2018). Furthermore, malnutrition has serious and life-threatening consequences that are known to be the main causes of increased morbidity and mortality among old age people (Rosted et al., 2018). Besides, complications of malnutrition, such as osteoarthritis, osteoporosis, diabetes, cardiovascular disease, and hypertension, inflict a significant social and economic burden on them (Gutzwiller et al., 2018).
Timely diagnosis of malnutrition and risk factors is crucial for public health interventions targeting old age people. In addition, previous studies reported that the prevalence of malnutrition among old age people varies between 1.1% and 72.2% in different settings (Barusepang et al., 2017; Ghimire et al., 2018; Konda et al., 2018; Mardani et al., 2018; Wong et al., 2019), where some of the variations could be attributed to differences in the measurement tools, study settings, and demographic groups that have been studied (Visser et al., 2017; Power et al., 2019). Moreover, none of the previous reviews targeted the old age people in Africa (van der Pols-Vijlbrief et al., 2014; Cereda et al., 2016; Leij-Halfwerk et al., 2019; Wolters et al., 2019), where it is anticipated that there are several causes of malnutrition. However, having concrete evidence on the burden of malnutrition using a more rigorous and systematic manner than individual pocket studies is the first step toward enhancing the old age people’s interventions and policy direction. Thus, this paper aimed to provide comprehensive prevalence of malnutrition among old ages, which could potentially provide context-specific evidence to better inform decision-makers in making informed decisions on addressing malnutrition among old age people for a better quality of life.
Before the beginning of this systematic review, we conducted a systematic search of review papers from the Cochrane Library, the International Prospective Register of Systematic Reviews (PROSPERO), and the Joanna Briggs Institute (JBI), and no review had been conducted on malnutrition among old age people in Africa. Then, relevant publications were searched systematically from HINARI, PubMed, and Google Scholar databases from 01 January 2000 to 16 October 2021. We employed the search through relevant combinations of MeSH terms and related keywords, such as “malnutrition”, “obesity”, “overweight”, “old age people”, “older adults”, “elderly”, and “Africa” as indicated in Supplementary File. Reference lists from relevant studies were also manual-searched. Countries or territories included in Africa were defined according to the United Nations (UN) classification (United Nations, 2003). Studies were imported and checked for duplicates in Mendeley Desktop (Version 1.19.3).
Based on the condition, context, and population (CoCoPop) framework (Munn et al., 2015) we included research publications in English language from 1 January 2000 to 16 October 2021 that reported the prevalence of malnutrition among old age people aged 60 years and up in African countries. Intending to get a relatively up-to-date prevalence estimate and obtain a comparable age and malnutrition definition, we restricted studies conducted starting in 2000. All studies that reported the prevalence and/or incidence of malnutrition among old age people were considered regardless of the study design. When multiple studies reported the prevalence of malnutrition based on the same study, the one with the larger sample size was included.
Qualitative studies, study protocols, abstracts, opinions, commentaries, case reports, review papers, and studies on African-Americans who do not live on the African continent were all excluded from the review. Duplicated articles and those reporting malnutrition in post-intervention were excluded. Articles without access to the full text were managed using two strategies. First, when outcome data were not reported, we tried to calculate from other additional information in the publications. If not, second method was to contact the corresponding author via email. Contacted authors requested full-text papers until 31 October 2021. However, if both strategies were not possible, the study was removed from the review.
Studies that measured malnutrition with any standard and validated tools, including questionnaires such as Patient-Generated Subjective Global Assessment (PG-SGA), Mini Nutritional Assessment (MNA), Subjective Global Assessment tools (SGA), or Nutritional Screening Checklist (NCL), anthropometric [body mass index (BMI), mid-upper arm circumference (MUAC), calf-circumference (CC), etc.], or biochemical indices (serum haemoglobin, albumin, etc.) were considered. We used the reported prevalence of malnutrition or undernutrition based on the standard definition set for each nutritional assessment method.
A two-step process was used to select the relevant publications. First, the scan of the titles and abstracts was conducted for the inclusion of references that meet the eligibility criteria. If there were any uncertainties about the relevance of a study, the entire text was retrieved. Second, the full texts were then used to make a judgement on whether or not the study should be included in the review. The two authors work individually on all aspects of the selection process. Disagreements were settled through conversation.
The selected studies were critically appraised using a ten-item rating checklist designed for research reporting prevalence (Hoy et al., 2012), where better quality articles have a higher score as indicated in Supplementary Table S1.
Data extraction was performed by two independent authors using a prespecified standard format prepared in Excel from the full-text articles. The extract comprised the following information: general (authors, year of publication, and country), participants (age, sex, and morbidity status), and study details (study design, study setting, sample size, measurement tool used, and outcome measures). Morbidity was coded as one or multi when a single or multiple underlying health conditions were an inclusion criterion.
The pre-coded extracted data in excel format was exported to STATA software version 14 (StataCorp, 2015) for descriptive and meta-analysis. For each study, the unadjusted prevalence of malnutrition and standard errors were calculated, and a logarithmic (log) transformation for proportional data was used to reduce variance and obtain the pooled prevalence as an effect size (ES). Considering the level of methodological heterogeneity and variance within the study, a random effect model of the DerSimonian and Laird (Hanji, 2017) method was used to conduct the meta-analysis.
The heterogeneity between studies was assessed using a forest plot, Cochran’s Q test, and I-square (I2) test. The I2 values of 25, 50, and 75% with a p-value less than 0.10 represent low, medium, and high heterogeneity, respectively (Higgins et al., 2003). Publication bias was checked graphically in a funnel plot supplemented by Egger’s statistics (Shi et al., 2017). We also applied a heterogeneity subgroup analysis, an outlier sensitivity analysis, and meta-regression to identify the potential sources of heterogeneity. An effect size estimate with a P-value below 0.05 was considered statistically significant.
Atotal of 1,442 articles were identified through searches, of which 206 were removed due to duplicates. With the title and abstract screening, 971 articles were removed depending on the focus of the review (older age in the African continent), relevant nutritional assessment method, and language (other than English). Furthermore, 237 articles were found during the full-text screening. Finally, 37 and 36 articles were selected for qualitative (systematic review) and quantitative analysis (meta-analysis), respectively. Figure 1, presents the comprehensive selection process using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009).
A total of 37 studies reported the prevalence of malnutrition among old age people. While 34 studies (92%) were published within the last 10 years between 2011 and 2020, the remaining 8% were issued between 2001 and 2010. All the included studies were reported from 11 African countries, where more than half (65%, n = 24) were from four countries: Ethiopia, Egypt, Nigeria, and South Africa.
Seven studies (18.9%) were from Ethiopia (Tessfamichael et al., 2014; Hailemariam et al., 2016; Diendéré et al., 2018; Abdu et al., 2019; Adhana et al., 2019; Legesse et al., 2019; Abate et al., 2020) and six studies (16.2%) each from Egypt (Khater and Abouelezz, 2011; Esmayel et al., 2013; Mahfouz et al., 2013; El-sherbiny et al., 2016; El-desouky and Abed, 2017; Allah et al., 2020) and Nigeria (Olasunbo and Olubode, 2006; Adebusoye et al., 2012; Abd-el-gawad et al., 2014; Alao et al., 2015; Adebusoye et al., 2018; Adebusoye et al., 2019). While five studies (13.5%) were from South Africa (Marais et al., 2007; Mkhize et al., 2013; Naidoo et al., 2015; OC et al., 2015; Robb et al., 2017), four studies (10.8%) were from the Central African Republic (CAR) and the Republic of Congo (Andre et al., 2013; Rouvray et al., 2014; Pilleron et al., 2015; Jésus et al., 2017) three studies (8.1%) from Ghana (Aganiba et al., 2015; Agbozo et al., 2018; Apprey et al., 2019), and two studies (6.06%) were from Tanzania (Nyaruhucha et al., 2001; Ijarotimi and Keshinro, 2008).
Except for three studies (two cohorts (Abd-el-gawad et al., 2014; Diendéré et al., 2018) and one case-control (Alao et al., 2015)), all other identified studies were cross-sectional study designs. Malnutrition prevalence was reported in four studies as a comparison between institutional versus noninstitutional (Ijarotimi and Keshinro, 2008; Alao et al., 2015), high versus low economic classes (Robb et al., 2017), and with and without dementia (Rouvray et al., 2014). However, one study from Tanzania assessed the nutritional status after a post-supplemental food program (Burani and Longo, 2019) and was excluded from the meta-analysis. The majority of the studies (n = 22) were conducted in community settings, while 11 studies were conducted among institutionalized elders.
Moreover, a total of 15,266 study participants were found, of whom more than half (58%) were females. The included studies had sample sizes ranging from 40 (Faten et al., 2019) to 2,219 (El-sherbiny et al., 2016) people. Regarding the nutritional assessment tools used, more than half of the studies reported malnutrition based on either the full-or short-form of the Mini Nutritional Assessment tool (MNA-FF: n = 15, MNA-SF: n = 4). While 18 studies employed various anthropometric measurements such as BMI, MUAC, and CC separately or in combinations to assess malnutrition. One study used an interviewer-administered Nutritional Screening Checklist (NCL) (Esmayel et al., 2013) and another study utilized a combination of MNA and the geriatric nutrition risk index (GNRI) (Faten et al., 2019). Two-thirds (n = 23) of the studies reported single (n = 8) or multiple (n = 15) underlying clinical conditions such as fracture, heart disease, dementia, Parkinson’s disease, or cancer (Supplementary Table S2).
Based on the quality assessment checklist, studies were either in moderate (6-8 points) (Ijarotimi and Keshinro, 2008; Khater and Abouelezz, 2011; Mahfouz et al., 2013; Abd-el-gawad et al., 2014; Alao et al., 2015; OC et al., 2015; El-desouky and Abed, 2017; Adebusoye et al., 2018; Adebusoye et al., 2019; Andia et al., 2019; Faten et al., 2019; Allah et al., 2020) or high-quality groups (9 or 10 points) (Nyaruhucha et al., 2001; Olasunbo and Olubode, 2006; Marais et al., 2007; Adebusoye et al., 2012; Cheserek et al., 2012; Andre et al., 2013; Esmayel et al., 2013; Mkhize et al., 2013; Rouvray et al., 2014; Tessfamichael et al., 2014; Aganiba et al., 2015; Naidoo et al., 2015; Pilleron et al., 2015; El-sherbiny et al., 2016; Hailemariam et al., 2016; Robb et al., 2017; Agbozo et al., 2018; Diendéré et al., 2018; Abdu et al., 2019; Adhana et al., 2019; Apprey et al., 2019; Legesse et al., 2019; Abate et al., 2020). Study bias was mostly exacerbated as a result of convenience sampling and a low response rate among study participants. In almost all studies, the possibility of external validity was low as the target population was not nationally representative of the country. However, the quality of two studies (Jésus et al., 2017; Burani and Longo, 2019) was not assessed and hence not processed for quantitative data analysis. The first was (Jésus et al., 2017) due to duplication of results from previous data (Rouvray et al., 2014) and the latter (Burani and Longo, 2019) was due to the outcome variable being measured after an intervention (Supplementary Table S3).
The prevalence of malnutrition varied highly across the studies conducted in different countries, assessment tools used, and healthcare settings. We presented an overview of the findings from various studies using two assessment tools in the section below.
Seventeen studies from hospitals (n = 5), the community (n = 10), a long-term care center (n = 1), and a daycare center (n = 1), utilized body mass index (BMI) as a nutritional assessment tool. As low as zero (OC et al., 2015) and 4.0% (Mkhize et al., 2013) of research participants respectively from the old age people daycare center and hospital settings in South Africa were classified as undernourished (BMI ≤18.5 kg/m2). Furthermore, the highest prevalence of undernutrition (25.6%) was reported in a Tanzanian hospital (Nyaruhucha et al., 2001). From the community settings, undernutrition was reported at 9.9% in Ghana (Apprey et al., 2019) and 26.4% in the East Africa (Cheserek et al., 2012).
On the other hand, 77% of the old age people studied in a South African hospital (Mkhize et al., 2013) were overweight or obese. None of the study participants in Tanzania were obese or overweight (Nyaruhucha et al., 2001). While 15.3% of study participants in the East Africa (Cheserek et al., 2012) and 42.1% in Ghana (Apprey et al., 2019) were affected by overweight or obesity in the community settings.
Old age people in the community were more susceptible to malnutrition when using MNA compared to hospitals and long-term care centers. The prevalence ranged from 5.7% in Niger (Andia et al., 2019) to 56% in Egypt (Esmayel et al., 2013) and 18% in Egypt (Esmayel et al., 2013) to 58.5% in Niger (Andia et al., 2019), respectively. While 2.24% (Adebusoye et al., 2018) to 40.46% (Abd-el-gawad et al., 2014) and 11.8% (Adebusoye et al., 2012) to 52.7% (Abd-el-gawad et al., 2014) of old age people all from the Nigerian hospitals were malnourished and at risk of malnutrition, respectively. Besides, 7.3% in South Africa (Robb et al., 2017) and 10.8% in Egypt (Khater and Abouelezz, 2011) were malnourished using MNA from the long-term care center.
Similarly, 10.9% of community study participants in Egypt (El-sherbiny et al., 2016) and 77.3% in Ethiopia (Adhana et al., 2019) were malnourished, while none from Ethiopia (Adhana et al., 2019) and 41.9% from Egypt (El-sherbiny et al., 2016) were at risk of malnutrition using MNA-SF. Moreover, 4.57% of hospital study participants in Nigeria (Adebusoye et al., 2019) were malnourished, while 95.43% were either normal or at risk of malnutrition.
Sufficient data were available to conduct pooled malnutrition prevalence estimates for two nutrition screening tools: BMI (n = 16) and MNA (n = 20). Since the full-and short-form of MNA and NCL tools are similar in the interpretation of the outcome variable, they were treated as similar tools. The random pooled prevalence of malnutrition in Africa was 18% (95% CI: 15-22; p < 0.001) (Figure 2).
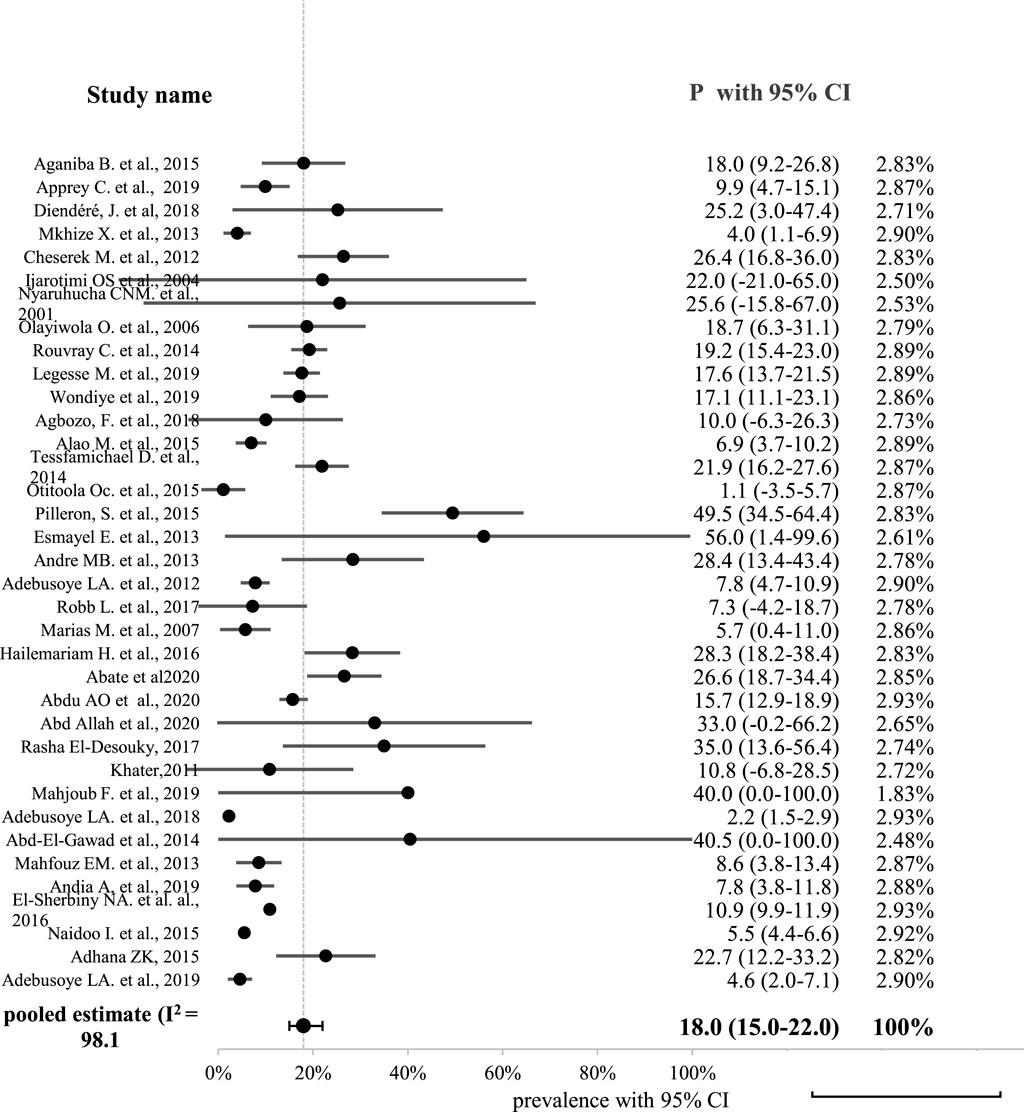
FIGURE 2. Forest plot displaying the pooled prevalence of malnutrition among old age people in Africa.
As illustrated in Figure 2, a high level of statistical heterogeneity was observed between studies (heterogeneity of Cochran Q statistics = 1828.98 with df = 35 and p-value < 0.001; I2 = 98.1%; Tau-square (τ2 = 0.01).
Moreover, a minimal publication bias has been noted in the published studies. Studies with lower standard error and larger sample size might be included, as indicated in of the funnel and Egger’s publication plots (Figure 3). Smaller studies with larger standard errors plotted on the right of the funnel plot tend to have both smaller and larger odds ratios. This may indicate the existence of bias due to small-study effects. Moreover, the Egger plot shows that the data near the origin are unsystematically elevated, where the confidence interval (CI) does not include zero, indicating asymmetry in the funnel plot and evidence of publication bias.
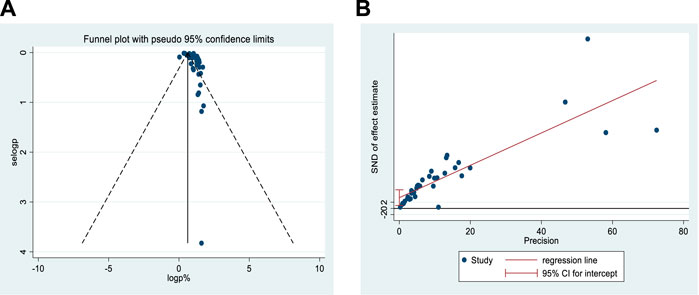
FIGURE 3. Probability of publication bias for included studies (A) funnel plot and (B) Egger’s publication bias plot.
Furthermore, Egger’s regression asymmetry test value was 3.50 (p = 0.008), suggesting publication bias. Here, the positive coefficient indicates that small studies overestimate the effect size. However, no study appeared to have a significant impact on the summary effect size in the sensitivity analysis, strongly suggesting that the effect estimate is consistent across groups and potentially giving a reliable estimate of the outcome.
Subgroup analysis and meta-regression were performed for the study regions, settings, assessment tools, age group, and presence of multimorbidity using the random-effects inverse-variance model with the DerSimonian-Laird estimate. In general, a relatively high prevalence of malnutrition was observed in central Africa (3.76%; 95% CI: 3.22-4.39) as compared to other regions of the continent. Similarly, the community old age people (3.12%; 95% CI: 2.66-3.67), older age groups (3.54%; 95% CI: 2.32–5.41), and those with no reported clinical condition (3.16%; 95CI: 2.62–3.80) had a higher malnutrition burden than their counterparts. The prevalence estimates showed a statistically significant variation among all subgroups except for the assessment tools used (p = 0.430) (Table 1).
However, only the study setting was statistically significant (adjusted R-squared = 39.2%, p = 0.049) predicting the prevalence of malnutrition in the meta-regression analysis.
We conducted this review paper with the intention of estimating the pooled prevalence of malnutrition disaggregated by relevant factors such as study setting and screening tool. According to the findings, the prevalence of malnutrition ranges from 4.0% (Mkhize et al., 2013) to 77.3% (Adhana et al., 2019) across countries, depending on the assessment tools used and the study settings. These prevalence figures are consistent with previous European estimates of 3.8–67.4% (Leij-Halfwerk et al., 2019; Wolters et al., 2019) among older people despite differences in the settings. In contrast, the highest risk of malnutrition was observed in the community-dwelling old age people assessed by the MNA (both full and short forms) than in other studies; 7.5%–77.3% versus 5% (Cereda et al., 2016) to 19% (Verlaan et al., 2017). The variation may be due to the economic variables of the countries.
Overall undernutrition was 17.1% in the African continent using BMI, which is comparable to European countries, 3.8–18.2% (Wolters et al., 2019). While 27% of the study participants in the continent were overweight or obese. Furthermore, many studies (n = 14) in our review used BMI as a nutritional assessment tool for old age people. Similar studies in Africa still preferred to use BMI for old age people where 19.9% and 30% of subjects were undernourished, overweight or obese, respectively (Mabiama et al., 2021).
However, the BMI cutoff point used to identify underweight can have a significant impact on prevalence estimates, which tend to misclassify the old age people with physical spinal deformities and other factors that can affect height measurements (Elia and Stratton, 2012). Due to such measurement errors encountered, the assessment of nutritional status in the old age people become a challenging task, which warrants more comprehensive and multidimensional assessments including clinical examination, anthropometric measures, laboratory tests, dietary surveys, and social aspects (Ahmed and Haboubi, 2010; Bharadwaj et al., 2016). This means one assessment tool may not be suitable for all settings, which need contextualization (Cereda et al., 2016). Though more than 22 best-validated nutrition screening tools were identified for older adults (Leij-Halfwerk et al., 2019; Power et al., 2019), there has long been a lack of consensus regarding the criteria needed to make a diagnosis of malnutrition.
On the other hand, the meta-analysis revealed a pooled prevalence of malnutrition of 18% (95% CI: 15-22; p < 0.001). This is in the range of the ones reported from the world, ranging from 0.8 to 24.6% (Crichton et al., 2018) depending on the study regions, settings, and assessment tools used. The increasing number of an ageing population in Africa and nutritional transitions might have contributed to a higher burden of malnutrition. Our estimate is also consistent with the pooled prevalence of Indian studies (18.29%; 95% CI: 15.24-21.57) (Kushwaha et al., 2020). However, the result is slightly higher than the prevalence of malnutrition reported from the Central Demographic Republic of Congo and Nigeria (14.5%; 95% CI: 0.0-40.4%) (Crichton et al., 2018). This discrepancy could be explained by the use of various assessment procedures and the merging of pooled estimates from two countries where the burden of malnutrition might be higher.
Surprisingly, the current prevalence estimate is lower than the reviews reported from European older persons (48.4%; 95% CI: 41.5-51.8) (Leij-Halfwerk et al., 2019). The disparity could be attributed to economic factors, health literacy, and healthcare access, and the majority of the previous review data came from hospital settings, implying that individuals with higher health risks were included. The differences may also be caused by the publication bias of data pertaining to the African continent.
Still, there was significantly high heterogeneity between the studies (Q = 1873.99; df = 36; p < 0.001; T2 = 0.01; I2 = 98.1%). Sensitivity analysis did not improve this heterogeneity, which is consistent with other previous findings (Cereda et al., 2016; Crichton et al., 2018). Because of the highly complex physiological, social, and temporal nature of malnutrition, which differs from person to person, as well as bias introduced by research design, analysis of the pooled prevalence of malnutrition is difficult to account for all sources of variation (Marshall et al., 2018).
In the subgroup analysis, the prevalence of malnutrition showed a great variation depending on the study regions, study settings, age groups, and clinical conditions of study participants. Malnutrition was found to be prevalent in central Africa (3.76%), in older age groups (3.54%), with no documented clinical condition (3.16%), and in community-dwellers (3.12%). The prevalence was statistically significant in all subgroups except between the assessment tools used (p = 0.430). These findings are consistent with the reviews from India (Kushwaha et al., 2020) and the rest of the world (Crichton et al., 2018). While the meta-regression identified the study setting as a statistically significant (adjusted R2 = 39.20%, p = 0.049) predictor of malnutrition prevalence. This is, however, different from the reviews conducted in India (Kushwaha et al., 2020) and the world (Crichton et al., 2018) where the study region (R2 = 27.1%, p = 0.026) and assessment tools (R2 = 76.47%, p < 0.001) were statistically significant predictors of the malnutrition prevalence, respectively. The variation might be due to the difference in assessment tools used between the studies.
To our knowledge, this is the first systemic review and meta-analysis that provides a comprehensive estimate of the prevalence of malnutrition among old age people in Africa, including more recent studies conducted in the continent. Even though this review has its strengths, it is not without limitations. Due to the inherent heterogeneity among the included studies (I2 = 98.08%), the interpretation of the current study needs precaution. Being limited to including only English literature and not including research published in books might limit the generalizability of the estimate.
This systematic review and meta-analysis showed high malnutrition prevalence among old age people which warrants a targeted policy intervention. The prevalence varied greatly depending on the study setting, the tool used, and the country of residence. To better monitor and evaluate, the use of a more reliable, valid, and standardized malnutrition assessment tool is strongly recommended.
The study was created and designed by AS under the supervision and approval of NB. They are both responsible for all parts of this work. The final manuscript was read and approved by both writers.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fragi.2022.1002367/full#supplementary-material
Supplementary Table S1 | Quality appraisal checklist for prevalence studies.
Supplementary Table S2 | Characteristics of Selected Studies Using Different Nutritional Assessment Tools.
Supplementary Table S3 | Summary of the quality of included studies based on Hoy et al. (24).
Supplementary File | Search items for HINARI/PubMed.
BMI, Body Mass Index; CC, Calf Circumference; HINARI, Health InterNetwork Access to Research Initiative; MeSH, Medical Subject Headings; MNA, Mini Nutritional Assessment.
Abate, T., Mengistu, B., Atnafu, A., and Derso, T. (2020). Malnutrition and its determinants among older adults people in Addis Ababa, Ethiopia. BMC Geriatr. 20 (498), 498–499. doi:10.1186/s12877-020-01917-w
Abd-el-gawad, W. M., Abou-hashem, R. M., Omar, M., Maraghy, E., Essam, G., El Maraghy, M. O., et al. (2014). The validity of Geriatric Nutrition Risk Index: Simple tool for prediction of nutritional-related complication of hospitalized elderly patients. Comparison with Mini Nutritional Assessment. Clin. Nutr. 33 (6), 1108–1116. doi:10.1016/j.clnu.2013.12.005
Abdu, A. O., Dagne, I., and Ali, A. (2019). Predictors of malnutrition among elderly people above 65 Years in East Ethiopia: Neglected public health concern. Res. Sq. 20, 1–25. doi:10.1186/s12877-020-01911-2
Adebusoye, L., Ogunbode, A., Olowookere, O., Ajayi, S., and Ladipo, M. (2018). Factors associated with sarcopenia among older patients attending a geriatric clinic in Nigeria. Niger. J. Clin. Pract. 21, 443–450. doi:10.4103/njcp.njcp_374_17
Adebusoye, L. A., Ajayi, I. O., Dairo, M. D., and Ogunniyi, A. O. (2012). Nutritional status of older persons presenting in a primary care clinic in Nigeria. J. Nutr. Gerontol. Geriatr. 31 (1), 71–85. doi:10.1080/21551197.2012.647560
Adebusoye, L. A., Cadmus, E. O., Owolabi, M. O., and Ogunniyi, A. (2019). Frailty and mortality among older patients in a tertiary hospital in Nigeria. Ghana Med. J. 53 (3), 210–216. doi:10.4314/gmj.v53i3.5
Adhana, Z. K., Tessema, G. H., and Getie, G. A. (2019). Prevalence of under nutrition ond associated factors among people of old age in debre markos town, northwest Ethiopia, 2015. J. Aging Res. Clin. Pract. 8, 20–26. doi:10.14283/jarcp.2019.4
Aganiba, B., Owusu, W., Steiner-Aseidu, M., and Dittoh, S. (2015). Association between lifestyle and health variables with nutritional of the elderly in the northern region of Ghana. Afr. J. Food, Agric. Nutr. Dev. 15 (4), 10198–10216. doi:10.18697/ajfand.71.13570
Agbozo, F., Amardi-mfoafo, J., Dwase, H., and Ellahi, B. (2018). Nutrition knowledge, dietary patterns and anthropometric indices of older persons in four peri-urban communities in Ga West municipality, Ghana. Afr. Health Sci. 18 (3), 743–755. doi:10.4314/ahs.v18i3.33
Ahmed, T., and Haboubi, N. (2010). Assessment and management of nutrition in older people and its importance to health. Clin. Interv. Aging 5, 207–216. doi:10.2147/cia.s9664
Alao, M., Akinola, O. O., and Ojofeitimie, O. (2015). Dietary intake and nutritional status of the elderly in osun state. IOSR-JNHS 4 (1), 32–35. doi:10.9790/1959-04113235
Allah, E. S. A., Gad, H. M. M., Abdel-Aziz, H. R., Abd Allah, E. S., Gad, H. M. M., and Abdel-Aziz, H. R. (2020). Nutritional status and its contributing factors among older adults with cancer receiving chemotherapy. Clin. Nurs. Res. 29 (8), 650–658. doi:10.1177/1054773820947953
Andia, A., Fourera, S., Souleymane, B., Mamane, D., and Adehossi, E. (2019). Evaluation of nutritional status at household in elderly assessed by mini nutritional assessment (MNA) in west Africa country, niamey-Niger. Am. J. Gerentol Geriatr. 2 (1), 1–4.
Andre, M. B., Dumavibhat, N., Ngatu, N. R., Eitoku, M., Hirota, R., and Suganuma, N. (2013). Mini nutritional assessment and functional capacity in community-dwelling elderly in rural luozi, democratic republic of Congo. Geriatr. Gerontol. Int. 13 (1), 35–42. doi:10.1111/j.1447-0594.2012.00852.x
Apprey, C., Gabriel, L. S., Asamoah-, O., and Reginald, A. (2019). Nutritional status and non-communicable diseases in older Ghanaians. J. Clin. Nutr. Diet. 5 (1), 1–8. doi:10.4172/2472-1921.100074
Barusepang, K., Sabariah, A. H., and Norhafizah, A. M. (2017). Prevalence of overweight and obesity in elderly people from kg BaruSepang, selangor, Malaysia. Int. J. Sci. Res. Publ. 7 (3), 421–429.
Bharadwaj, S., Ginoya, S., Tandon, P., Gohel, T. D., Guirguis, J., Vallabh, H., et al. (2016). Malnutrition: Laboratory markers vs nutritional assessment. Gastroenterol. Rep. 4, 272–280. doi:10.1093/gastro/gow013
Burani, J. C., and Longo, P. J. (2019). Undernutrition in the isolated elderly poor: Perspectives from a developing country humanitarian program. Afr. J. Food Agric. Nutr. Dev. 19 (2), 14319–14336. doi:10.18697/ajfand.85.17790
Cereda, E., Pedrolli, C., Klersy, C., Bonardi, C., Quarleri, L., Cappello, S., et al. (2016). Nutritional status in older persons according to healthcare setting: A systematic review and meta-analysis of prevalence data using MNA®. Clin. Nutr. 35, 1282–1290. doi:10.1016/j.clnu.2016.03.008
Cheserek, M., Tuitoek, P., Waudo, J., Msuya, J., and Kikafunda, J. (2012). Anthropometric characteristics and nutritional status of older adults in the lake victoria basin of East Africa: Region, sex, and age differences. South Afr. J. Clin. Nutr. 25 (2), 67–72. doi:10.1080/16070658.2012.11734408
Crichton, M., Craven, D., Mackay, H., Marx, W., Van Der, S. M. D., Marshall, S., et al. (2018). A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: Associations with geographical region and sex. Age Ageing 48, 1–11. doi:10.1093/ageing/afy144
Diendéré, J., Millogo, A., Preux, P-M., Jésus, P., Desport, J-C., Diendere, J., et al. (2018). Changes in nutritional state and dysphagia in stroke patients monitored during a 14-d period in a Burkina Faso hospital setting Nutrition 48, 55–60. doi:10.1016/j.nut.2017.10.022
El-desouky, R. S., and Abed, H. A. (2017). Screening of malnutrition and its correlates among a sample of rural elderly in Qalyobeya Governorate, Egypt. J. Egypt. Public Health Assoc. 92 (3), 156–166. doi:10.21608/epx.2017.16394
El-sherbiny, N. A., Younis, A., and Masoud, M. (2016). A comprehensive assessment of the physical, nutritional, and psychological health status of the elderly populace in the Fayoum Governorate (Egypt). Arch. Gerontol. Geriatr. 66, 119–126. doi:10.1016/j.archger.2016.06.001
Elia, M., and Stratton, R. J. (2012). An analytic appraisal of nutrition screening tools supported by original data with particular reference to age. Nutrition 28, 477–494. doi:10.1016/j.nut.2011.11.009
Esmayel, E. M. M., Eldarawy, M. M., Hassan, M. M. M., Hassanin, H. M., Ashour, W. M. R., and Mahmoud, W. (2013). Nutritional and functional assessment of hospitalized elderly: Impact of sociodemographic variables. J. Aging Res. 2013, 101725–101727. doi:10.1155/2013/101725
FAO and ECA (2018). Regional Overview of Food Security and Nutrition. Addressing the threat from climate variability and extremes for food security and nutrition. Accra: FAO.
Faten, M., Ramla, M., Nadia, B. A., Mongi, B. M., Adel, K., Inès, L., et al. (2019). Prevalence of malnutrition for elderly hemodialysis patients. Tunis. Med. 97 (4), 588–594.
Ghimire, S., Baral, B. K., Pokhrel, B. R., Pokhrel, A., Acharya, A., Amatya, D., et al. (2018). Depression, malnutrition, and health-related quality of life among Nepali older patients. BMC Geriatr. 18 (191), 191–215. doi:10.1186/s12877-018-0881-5
Guisado-Clavero, M., Roso-Llorach, A., López-Jimenez, T., Pons-Vigués, M., Foguet-Boreu, Q., Muñoz, M. A., et al. (2018). Multimorbidity patterns in the elderly: A prospective cohort study with cluster analysis. BMC Geriatr. 18 (1), 16–11. doi:10.1186/s12877-018-0705-7
Gutzwiller, J. P., Richterich, J. P., Stanga, Z., Nydegger, U. E., Risch, L., and Risch, M. (2018). Osteoporosis, diabetes, and hypertension are major risk factors for mortality in older adults: An intermediate report on a prospective survey of 1467 community-dwelling elderly healthy pensioners in Switzerland. BMC Geriatr. 18 (1), 115–119. doi:10.1186/s12877-018-0809-0
Hailemariam, H., Singh, P., and Fekadu, T. (2016). Evaluation of mini nutrition assessment (MNA) tool among community dwelling elderly in urban community of Hawassa city, Southern Ethiopia. BMC Nutr. 2 (11), 11–16. doi:10.1186/s40795-016-0050-1
Hanji, M. B. (2017). Meta-analysis in psychiatry research: Fundamental and advanced methods. USA: Apple Academic Press.
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi:10.1136/bmj.327.7414.557
Hoy, D., Brooks, P., Woolf, A., Blyth, F., March, L., Bain, C., et al. (2012). Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 65 (9), 934–939. doi:10.1016/j.jclinepi.2011.11.014
Ijarotimi, O. S., and Keshinro, O. O. (2008). Nutritional knowledge, nutrients intake and nutritional status of hypertensive patients in Ondo State, Nigeria. Tanzan. J. Health Res. 10 (2), 59–67. doi:10.4314/thrb.v10i2.14343
Jésus, P., Guerchet, M. M., Pilleron, S., Fayemendy, P., Maxime Mouanga, A., Mbelesso, P., et al. (2017). Undernutrition and obesity among elderly people living in two cities of developing countries: Prevalence and associated factors in the EDAC study. Clin. Nutr. ESPEN 21, 40–50. doi:10.1016/j.clnesp.2017.05.007
Khater, M. S., and Abouelezz, N. F. (2011). Nutritional status in older adults with mild cognitive impairment living in elderly homes in Cairo, Egypt. J. Nutr. Health Aging 15 (2), 104–108. doi:10.1007/s12603-011-0021-9
Konda, S., Rkb, P., Giri, P. A., Rk, B. P., and Giri, P. A. (2018). Prevalence of malnutrition and its determinants in an elderly people in South India. Int. J. Community Med. Public Health 5 (8), 3570–3576. doi:10.18203/2394-6040.ijcmph20183100
Kushwaha, S., Khanna, P., Srivastava, R., Jain, R., Singh, T., and Kiran, T. (2020). Estimates of malnutrition and risk of malnutrition among the elderly (≥60 years) in India: A systematic review and meta-analysis. Ageing Res. Rev. 63 (101137), 101137–101212. doi:10.1016/j.arr.2020.101137
Legesse, M., Abebe, Z., and Woldie, H. (2019). Chronic energy deficiency and associated factors among older population in Ethiopia: A community based study. PLoS One 14 (4), e0214861. doi:10.1371/journal.pone.0214861
Leij-Halfwerk, S., Verwijs, M. H., van Houdt, S., Borkent, J. W., Guaitoli, P. R., Pelgrim, T., et al. (2019). Prevalence of protein-energy malnutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults ≥65 years: A systematic review and meta-analysis. Maturitas 126, 80–89. doi:10.1016/j.maturitas.2019.05.006
Mabiama, G., Adiogo, D., Millimono, T., Fayemendy, P., Vernier, T., Boumediene, F., et al. (2021). Undernutrition, overweight and obesity among elderly living in communities in Africa: A systematic review. Proc. Nutr. Soc. 80 (4), E158. doi:10.1017/s0029665121002810
Mahfouz, E., Mohammed, E. S., and El-Rhman, T. A. A. (2013). Assessment of nutritional status of elderly populations in rural minia, Egypt. J. Aging Res. Clin. Pract. 2 (3), 7–10. doi:10.1186/s40795-022-00532-9
Marais, M. L., Marais, D., and Labadarios, D. (2007). Assessment of nutritional status of older people in home for the aged in the Somerest West area. SAJCN 20 (3), 1–7. doi:10.1080/16070658.2007.11734134
Mardani, M., Bonyadi, M., Abbasnezhad, A., Rezapour, M., Ebrahimzadeh, F., Rostami, S., et al. (2018). Mini nutritional assessment and its correlation with elderly nursing home residents in khorramabad, Iran. Iran. Rehabil. J. 16 (2), 177–184. doi:10.32598/irj.16.2.177
Marshall, S., Craven, D., Kelly, J., and Isenring, E. (2018). A systematic review and meta-analysis of the criterion validity of nutrition assessment tools for diagnosing protein-energy malnutrition in the older community setting (the MACRo study). Clin. Nutr. 37 (6), 1902–1912. doi:10.1016/j.clnu.2017.09.022
Mkhize, X., Napier, C., and Oldewage-Theron, W. (2013). The nutrition situation of free-living elderly in Umlazi township, South Africa. Health SA Gesondheid 18 (1), 1–8. doi:10.4102/hsag.v18i1.656
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Altman, D., Antes, G., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6 (7), e1000097. doi:10.1371/journal.pmed.1000097
Munn, Z., MclinSc, S. M., Lisy, K., Riitano, D., and Tufanaru, C. (2015). Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based. Healthc. 13 (3), 147–153. doi:10.1097/XEB.0000000000000054
Naidoo, I., Charlton, K. E., Esterhuizen, T. M., and Cassim, B. (2015). High risk of malnutrition associated with depressive symptoms in older South Africans living in KwaZulu-natal, South Africa: A cross-sectional survey. J. Health Popul. Nutr. 33 (19), 19. doi:10.1186/s41043-015-0030-0
Nyaruhucha, C. N. M., Msuya, J. M., and Augustino, B. (2001). Health status of hospitalised elderly in morogoro regional hospital. East Afr. Med. J. 78 (9), 489–492. doi:10.4314/eamj.v78i9.8982
Oc, O., Wn, O-T., and Egal, A. (2015). Trends in the development of obesity in elderly day care attendees in Trends in Sharpeville, South Africa, from 2007-2011. S Afr. J. Clin. Nutr. 28 (1), 12–17. doi:10.1080/16070658.2015.11734520
Olasunbo, O. I., and Olubode, K. A. (2006). Socio-demographic and nutritional assessment of the elderly Yorubas in Nigeria. Asia Pac. J. Clin. Nutr. 15 (1), 95–101.
Pilleron, S., Je´sus, P., Desport, J-C., Mbelesso, P., Ndamba-Bandzouzi, B., Cle´ment, J-P., et al. (2015). Association between mild cognitive impairment and dementia and undernutrition among elderly people in central Africa: Some results from the EPIDEMCA (epidemiology of dementia in central Africa) programme. Br. J. Nutr. 114, 306–315. doi:10.1017/S0007114515001749
Power, L., de van der Schueren, M., Leij-Halfwerk, S., Bauer, J., Clarke, M., Visser, M., et al. (2019). Development and application of a scoring system to rate malnutrition screening tools used in older adults in community and healthcare settings – a MaNuEL study. Clin. Nutr. 38 (4), 1807–1819. doi:10.1016/j.clnu.2018.07.022
Robb, L., Walsh, C. M., Nel, M., Nel, A., Odendaal, H., van Aardt, R., et al. (2017). Malnutrition in the elderly residing in long-term care facilities: A cross sectional survey using the mini nutritional assessment (MNA®) screening tool. South Afr. J. Clin. Nutr. 30 (2), 34–40. doi:10.1080/16070658.2016.1248062
Rosted, E., Prokofieva, T., Sanders, S., Schultz, M., Rosted, E., Prokofieva, T., et al. (2018). Serious consequences of malnutrition and delirium in frail older patients. J. Nutr. Gerontol. Geriatr. 37 (2), 105–116. doi:10.1080/21551197.2018.1470055
Rouvray, C., Guerchet, M., Fayemendy, P., Mouanga, A. M. M., Mbelesso, P., Preux, P. M. M., et al. (2014). The nutritional status of older people with and without dementia living in an urban setting in Central Africa: The EDAC study. J. Nutr. Health Aging 18 (10), 868–875. doi:10.1007/s12603-014-0483-7
Saka, S., Oosthuizen, F., and Nlooto, M. (2019). National policies and older people’s healthcare in sub-saharan Africa: A scoping review. Ann. Glob. Health 85 (1), 91–97. doi:10.5334/aogh.2401
Shi, X., Nie, C., Shi, S., Wang, T., Yang, H., and Zhou, Y. (2017). Effect comparison between Egger’s test and begg’s test in publication bias diagnosis in meta-analyses: Evidence from a pilot survey. Int. J. Res. Stud. Biosci. 5 (5), 14–20. doi:10.20431/2349-0365.0505003
Tessfamichael, D., Gete, A. A., and Wassie, M. M. (2014). High prevalence of undernutrition among elderly people in northwest Ethiopia: A cross sectional study. J. Nutr. Heal Food Sci. 2 (4), 1–5. doi:10.15226/JNHFS.2014.00131
United Nations Department of Economic and Social Affairs Population Division (2019). World population prospects 2019: Highlights. New York: United Nations. ST/ESA/SER.A/423.
United Nations (2003). United Nations statistics division: Millennium indicators [internet]. Available from: https://unstats.un.org/unsd/mi/africa.htm (Accessed Dec 7, 2019).
United Nations, Department of Economic and Social Affairs PD (UNDESAPD) (2016). Direectory of reseearch on ageing in Africa: 2004-2015. New York: United Nations. ST/ESA/SER.A/391.
United Nations, United Nations Sustainable Development (2019). Knowledge Platform. Sustainable Development Goal 2; End hunger, achieve food security and improved nutrition and promote sustainable agriculture. Available at: https://sustainabledevelopment.un.org/sdg2 (Accessed Nov 9, 2019).
van der Pols-Vijlbrief, R., Wijnhoven, H. A. H., Schaap, L. A., Terwee, C. B., and Visser, M. (2014). Determinants of protein-energy malnutrition in community-dwelling older adults: A systematic review of observational studies. Ageing Res. Rev. 18, 112–131. doi:10.1016/j.arr.2014.09.001
Verlaan, S., Ligthart-Melis, G. C., Wijers, S. L. J. J., Cederholm, T., Maier, A. B., Van Der, S. M., et al. (2017). High prevalence of physical frailty among community-dwelling malnourished older adults–A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 18 (5), 374–382. doi:10.1016/j.jamda.2016.12.074
Visser, M., Volkert, D., Corish, C., Geisler, C., de Groot, L. C., Cruz-Jentoft, A. J., et al. (2017). Tackling the increasing problem of malnutrition in older persons: The malnutrition in the elderly (MaNuEL) knowledge hub. Nutr. Bull. 42 (2), 178–186. doi:10.1111/nbu.12268
Wolters, M., Volkert, D., Streicher, M., Kiesswetter, E., Torbahn, G., O’Connor, E. M., et al. (2019). Prevalence of malnutrition using harmonized definitions in older adults from different settings – a MaNuEL study. Clin. Nutr. 38 (5), 2389–2398. doi:10.1016/j.clnu.2018.10.020
Wong, M. M. H., So, W. K. W., Choi, K. C., Cheung, R., Chan, H. Y. L., Sit, J. W. H., et al. (2019). Malnutrition risks and their associated factors among home-living older Chinese adults in Hong Kong: Hidden problems in an affluent Chinese community. BMC Geriatr. 19 (138), 138–212. doi:10.1186/s12877-019-1148-5
World Health Organization (2017). Integrated care for older people: Guidelines on community-level interventions to manage declines in intrinsic capacity. Geneva: WHO.
World Health Organization (2002). Proposed working definition of an older person in Africa for the MDS project. Available at: http://www.who.int/healthinfo/survey/ageingdefnolder/en/index.html (Accessed Jun 20, 2017).
Keywords: Africa, malnutrition, old age people, prevalence, systematic-review, meta-analysis
Citation: Seid AM and Babbel NF (2022) Prevalence of malnutrition among old age people in Africa. Front. Aging 3:1002367. doi: 10.3389/fragi.2022.1002367
Received: 25 July 2022; Accepted: 10 October 2022;
Published: 10 November 2022.
Edited by:
Caroline Sarah Stokes, Humboldt University of Berlin, GermanyReviewed by:
Paulo Jose Fortes Villas Boas, São Paulo State University, BrazilCopyright © 2022 Seid and Babbel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmed Muhye Seid, YWhtZWRtdWh5ZTIwMDVAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.