- 1Department of Anorectal, KongJiang Hospital of Yangpu District, Shanghai, China
- 2Department of General Surgery, Yangpu Hospital, School of Medicine, Tongji University, Shanghai, China
- 3Shanghai Changing Mental Health Center, Affiliated Mental Health Center of East China Normal University, Shanghai, China
- 4Department of Geriatric Psychiatry, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Background: Previous studies have shown that surgery under general anesthesia may diminish cognitive function; however, the proposed mechanisms need further elucidation. The purpose of the current study was twofold: (1) to compare overall and domain-specific differences in cognitive function between the surgery under general anesthesia group and the control group, and (2) to investigate the possible mechanisms of surgery under general anesthesia affecting cognitive function, using T1-structural magnetic resonance imaging.
Methods: A total of 194 older adults were included in this study. Patients were divided into a surgery under general anesthesia group (n = 92) and a control group (n = 104). The two groups were matched for age, sex, and educational level. All participants underwent clinical evaluation, neuropsychological testing, blood biochemistry analysis, and T1 phase structural magnetic resonance imaging.
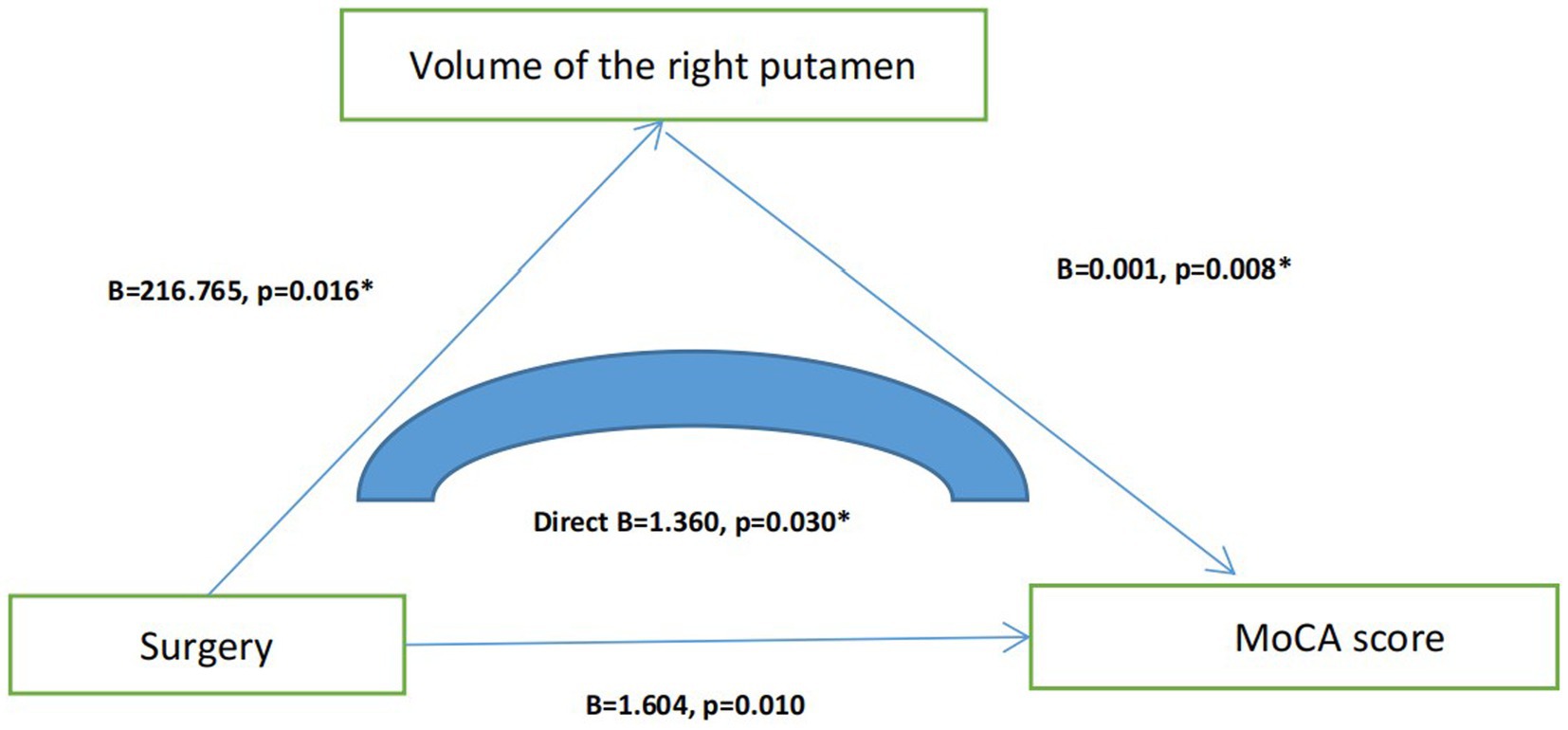
Results: We found that older adults with a history of surgery under general anesthesia had lower Montreal Cognitive Assessment (MoCA) scores and smaller right putamen volumes (p < 0.05). Linear regression analysis (mediation model) indicated that surgery under general anesthesia affected MoCA scores by diminishing the volume of the right putamen (B = 1.360, p = 0.030).
Conclusion: We found evidence that older adults who underwent surgery under general anesthesia had poorer cognitive function, which may have been caused by an apoptotic or otherwise toxic effect of anesthetic drugs on the volume of the right putamen.
1 Introduction
Alzheimer’s disease (AD), the leading cause of dementia, has rapidly become one of the most expensive, deadly, and burdensome diseases of this century (Scheltens et al., 2021). The core pathological features of Alzheimer’s disease are amyloid plaques and neurofibrillary tangles (NFTs), and factors such as immunity, inflammation, and infection may also contribute to the pathogenesis of AD (Serrano-Pozo et al., 2011). Currently, available treatments for AD include cholinesterase inhibitors and memantine. These drugs have been shown to improve the patients’ quality of life; however, they do not change the course of the disease or its rate of decline (Mossello and Ballini, 2012). Therefore, we are more concerned with early prevention than late treatment.
As the age of an individual increases, the probability of undergoing surgery under general anesthesia also increases. A substantial body of evidence from both in vivo and in vitro models suggests that exposure to anesthetics may increase the risk of AD through a mechanism similar to its neuropathology (Tsolaki et al., 2024). In addition, epidemiological studies have shown that surgery under general anesthesia is likely to increase the risk of AD. For instance, in a study by Vanderweyde et al. (2010), prostate or hernia surgery increased the risk of dementia, especially AD (Vanderweyde et al., 2010). In a nine-year follow-up of 3,100 patients, Sohn et al. found that the overall incidence of dementia was higher in those who underwent surgery under general anesthesia than in the control group (10.5 versus 8.8 per 1,000 person-years), especially among women or individuals with combined medical conditions (Sohn et al., 2021). However, a recent meta-analysis of case–control studies (N = 15) found no association between AD and prior exposure to surgery under general anesthesia (OR = 1.05, 95% CI: 0.93–1.19, p = 0.4) (Seitz et al., 2013; Seitz et al., 2011). Therefore, the link between surgery under general anesthesia and dementia needs to be further studied.
Magnetic resonance imaging (MRI) is an effective tool for studying brain and cognitive function and helps reveal the possible mechanisms through which anesthesia affects cognition. In animal studies, researchers have found that the putamen is unusually sensitive to narcotic drugs, such as sevoflurane (Burks et al., 2020). In another animal experiment, the researchers found that Fluoro-Jade C staining in the caudate putamen of mice was significantly elevated after sevoflurane exposure (Walters et al., 2020). Moreover, one study showed that when normal individuals undergo surgery under general anesthesia, blood flow in the putamen is significantly reduced (Schlünzen et al., 2007). Therefore, we speculate that the putamen is likely the target of cognitive decline induced by surgery under general anesthesia.
To test the above research hypothesis, we recruited 92 community-dwelling older adults who had undergone surgery under general anesthesia and 102 normal controls who were matched for age, sex, and education. All participants completed blood biochemical, neuropsychological, and T1 structural magnetic resonance tests. We hypothesized that: (1) older adults who have undergone surgery under general anesthesia may have poorer cognitive function, and (2) structural changes in the putamen may play an important regulatory role in the process of anesthesia-induced cognitive decline.
2 Materials and methods (Li et al., 2022)
2.1 Participants
This cross-sectional study was conducted at the KongJiang Hospital of Yangpu District between March 1, 2023 and April 1, 2024. The inclusion criteria were as follows: (1) aged 55 years and above; (2) without significant cognitive impairment before surgery, such as mild cognitive impairment (MCI) or dementia; (3) without obvious visual or hearing impairment; (4) T1-structural magnetic resonance tests. The exclusion criteria were as follows: (1) aged below 55 years; (2) non-surgery with general anesthesia, such as surgery with local anesthesia; (3) chronic diseases that may affect cognitive function, such as dementia, major depressive disorder, and schizophrenia; and (4) complicated by serious physical diseases, such as myocardial infarction, cerebral infarction, and cerebral hemorrhage. Simultaneously, we recruited a group of normal controls from the Yangpu community who had not undergone surgery under general anesthesia; their inclusion and exclusion criteria were the same as before. To exclude the effects of age, sex, and education on cognitive function, we matched the variables between the two groups.
All participants signed an informed consent form before the study was initiated, and ethical approval was obtained from the Ethics Committee of KongJiang Hospital of Yang Pu District.
2.2 Sample size evaluation
Under previous magnetic resonance imaging (fMRI) protocols, a sample size of 30 cases per group has become the “minimum requirement” and common choice for confirmatory studies (Zhou et al., 2024). Since we also needed to match sex, age, and education level, we needed at least 87 participants per group after calculating through the Power Analysis and Sample Size (PASS) software. Finally, we enrolled 92 surgical patients and 102 normal controls, matched for sex (males: 39 (42.4%) vs. 57 (55.9%), p = 0.064), age (70.02 ± 7.206 vs. 68.52 ± 7.470, p = 0.157), and years of education (8.44 ± 4.452 vs. 9.51 ± 3.601, p = 0.071). The results are summarized in Table 1.
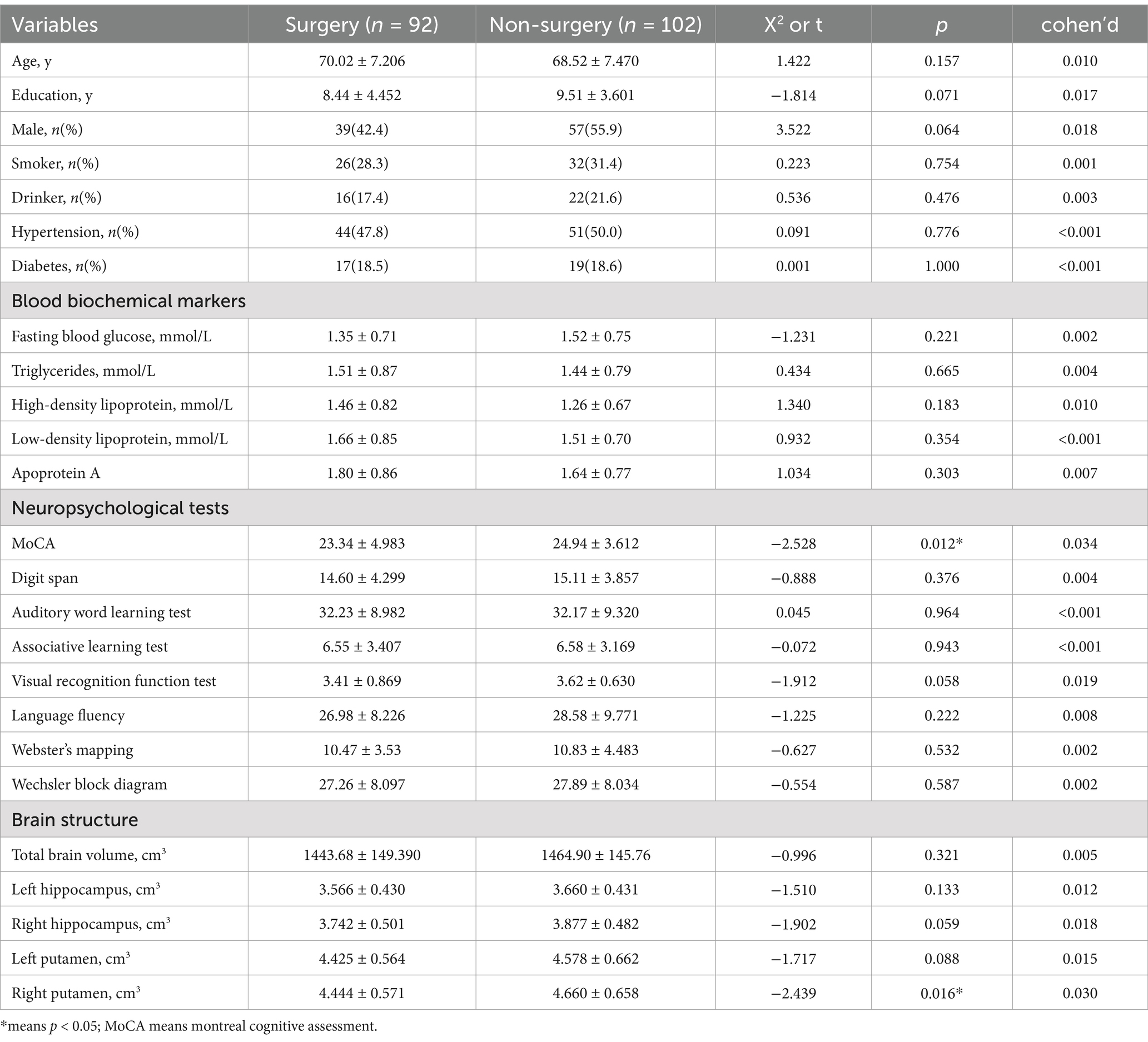
Table 1. Comparison of general demographic data, blood biochemical markers, neuropsychological tests, and brain structure between surgery and non-surgery individuals.
2.3 Clinical assessment and general demographic data collection
All participants completed a series of clinical assessments, physical examinations, and general demographic surveys. Through face-to-face interviews, we obtained general demographic data (age, sex, and education), daily living habits (smoking and drinking), and disease history (hypertension and diabetes). At the same time, we also investigated information about surgery with general anesthesia, including the age at surgery, the type of surgery as well as the main drugs used for surgery under general anesthesia.
2.4 Neuropsychological assessment
All participants completed a series of neuropsychological tests, including the Montreal Cognitive Assessment (MoCA) (Nasreddine et al., 2005), digit span (Leung et al., 2011), auditory word learning test (Hong et al., 2012), associative learning test, visual recognition function test, verbal fluency tasks (Aita et al., 2019), Webster’s mapping, and Wechsler block diagram (Li et al., 2017). The cognitive areas assessed in these scales are: overall cognitive function, attention and short-term memory, auditory memory, association and reaction speed, visual ability to distinguish numbers, letters and words, language ability, semantic memory and executive function. All scales were completed by professionally trained psychological testers and consistency training was conducted to ensure accuracy and consistency of the scale assessment.
2.5 Biochemical indexes
After an overnight fast, peripheral blood samples were collected between 7 a.m. and 9 a.m. Serum separation tubes containing activated clot gel were used to detect biochemical indices. Fasting blood glucose, triglyceride, high-density lipoprotein, low-density lipoprotein, and apoprotein A levels were measured using an Olympus AU2700 automatic biochemical analyzer (Beckman Coulter, Inc., Carlsbad, CA, United States).
2.6 T1 phase structure magnetic resonance imaging
Structural images of the brain were captured using a Magnetom Verio 3.0 T scanner (Siemens, Munich, Germany). The sequence parameters of the rapid gradient echo (MPRAGE) prepared using T1-weighted three-dimensional magnetization were as follows: TR = 2,300 ms, TE = 2.98 ms, matrix size = 240 × 256, turning angle = 9 °, film thickness = 1.2 mm, and field of view (FOV) = 240 × 256 mm. As described by Wolz et al., volume data was evaluated by an automated procedure (Wolz et al., 2014). Using FreeSurfer, we obtained the participants’ whole-brain, hippocampal, and caudate putamen volumes. In addition, to evaluate the impact of left–right differences, the asymmetry index was calculated as [right-to-left volume]/[total volume] × 100%. Quality control was ensured by overlapping the output packages on FreeSurfer templates and visual evaluations were performed.
3 Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD), and categorical variables are expressed as frequency (%). The one-sample Kolmogorov–Smirnov test was used to test whether the data conformed to a normal distribution. Independent sample t-tests and Kruskal-Wallis H tests were used to compare normal and non-normal data between the surgical and non-surgical groups, respectively. Chi-square tests were used to compare the classification variables. Next, correlation and linear regression analyses (mediating model) were used to investigate the associations between surgery and general anesthesia, cognitive-related brain areas, and cognitive scores. A two-tailed test was used for all analyses, and the significance level was set at p < 0.05. SPSS 22.0 (IBM Corporation, Armonk, NY, United States) was used for data analysis.
4 Results
4.1 Characteristics of subjects with different surgical conditions
Participants who underwent surgery under general anesthesia had lower overall MoCA scores and a smaller volume of the right putamen than participants who did not undergo surgery under general anesthesia (p < 0.05), while there was no statistical difference (p > 0.05) related to age, education, sex, smoking and drinking status, hypertension, diabetes, fasting blood glucose, triglyceride, high-density lipoprotein, low-density lipoprotein, apoprotein A, digit span, auditory word learning, associative learning, visual recognition function, language fluency, Webster’s mapping, Wechsler block diagram, total brain volume, left hippocampus, right hippocampus, and left putamen between the two groups. Table 1 shows the results.
4.2 The connection between surgery under general anesthesia and brain structure
To explain the possible mechanisms through which surgery under general anesthesia affects the overall cognitive function, we added T1-structural magnetic resonance data. We found that older adults with a history of surgery under general anesthesia had lower MoCA scores and smaller right putamen volumes (p < 0.05). Using correlation analysis, we found that the volume of the right amygdala was significantly correlated (p = 0.008, r = 0.189) with MoCA. Using linear regression analysis (mediation model), we found that surgery under general anesthesia directly affected the MoCA score by affecting the volume of the right putamen (B = 1.360, p = 0.030) (Figure 1).
5 Discussion
The purpose of this study was to investigate the relationship between surgery under general anesthesia and cognitive decline, and to explore the possible mechanism through which surgery under general anesthesia affects cognitive function. In this study, we recruited 92 community-dwelling older adults who underwent surgery under general anesthesia and 102 healthy controls matched for age, sex, and education. We found that: (1) older adults who underwent surgery under general anesthesia had poorer overall cognitive function, and (2) surgery under general anesthesia may affect cognitive function by affecting the volume of the right putamen, and there might be a causal relationship between the three factors (surgery under general anesthesia, right putamen, and cognitive function).
Several studies have explored the relationship between surgery under general anesthesia and cognitive function. Yu et al. found that whether propofol or sevoflurane was used in thoracic surgery, it would damage the cognitive function of older adults (Yu, 2017). Meng et al. found that surgery under general anesthesia and epidural anesthesia combined with general anesthesia can both damage the overall cognitive function of older adults with liver cancer (Meng et al., 2021). Moreover, Zhang et al. found that in addition to overall cognitive function, surgery under general anesthesia can also impair social cognitive function in older adults (Zhang et al., 2020). Therefore, our findings are consistent with these results.
To further explore the possible mechanisms through which surgery under general anesthesia affects overall cognitive function, we included T1 phase magnetic resonance data. We recruited two groups of older adults matched for age, sex, and education and ultimately found that individuals who underwent surgery under general anesthesia had poorer overall cognitive function than those who did not, while at the same time having a smaller right putamen volume. Using linear regression analysis (mediation model), we found that surgery under general anesthesia directly affected the MoCA score by affecting the volume of the right caudate putamen. The caudate putamen is part of the striatum and a component of the external vertebral system. Previous studies have shown that the anatomical connectivity, functional specialization, and neurochemical characteristics of the caudate putamen in patients with AD are significantly different from those in healthy controls (Selden et al., 1994). Moreover, other studies have confirmed a significant reduction in the putamen volume in patients with AD (Yoo et al., 2020; Cogswell et al., 2021). Therefore, we speculated that the putamen may also be involved in the pathogenesis of AD. However, there are few studies on the relationship between surgery under general anesthesia and the putamen. Further investigation is needed to determine whether anesthetic drugs affect cognitive function by affecting the putamen.
6 Limitations
Our study has some limitations. First, it is only a cross-sectional study that cannot establish a cause-and-effect relationship between surgery under general anesthesia and cognitive decline. Second, the relatively small sample size reduces the reliability of the study. Third, there are many confounding factors, such as different types of surgery, different choices of anesthetic drugs, and different durations of anesthesia, which may have affected the results. Fourth, our current study focuses only on the relationship between the putamen and surgery under general anesthesia without considering the impact of other cognitive brain regions, such as the hippocampus and amygdala, on the results, which is perhaps the biggest limitation of our study. Fifth, a recent review highlighted that stressful life events can also lead to cognitive deficits and even AD (not anesthesia itself, but the process of going to the hospital) (Martin et al., 2024). In addition, it is difficult to separate the effects of anesthesia from the effects of surgery on cognition, which is a major limitation of the current study (Cottrell and Hartung, 2020). Therefore, we plan to focus on solving these problems in future studies.
7 Conclusion
Surgery under general anesthesia may impair overall cognitive function in older adults, and the mechanism may be related to its effect on the right putamen volume.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of KongJiang Hospital of Yangpu district. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JJ: Conceptualization, Writing – original draft. ZZ: Data curation, Writing – original draft. HZ: Methodology, Writing – original draft. JL: Funding acquisition, Writing – review & editing. WL: Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by grants from the Fei Xiang Program of the Shanghai Mental Health Center (2020-FX-03), the National Natural Science Foundation of China (82101564), and the Medical Master’s and Doctoral Innovation Talent Base Project of Changning District (RCJD2022S07).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aita, S. L., Beach, J. D., Taylor, S. E., Borgogna, N. C., Harrell, M. N., and Hill, B. D. (2019). Executive, language, or both? An examination of the construct validity of verbal fluency measures. Appl. Neuropsychol. Adult 26, 441–451. doi: 10.1080/23279095.2018.1439830
Burks, S. M., Bowyer, J. F., Walters, J. L., and Talpos, J. C. (2020). Regions of the basal ganglia and primary olfactory system are most sensitive to neurodegeneration after extended sevoflurane anesthesia in the perinatal rat. Neurotoxicol. Teratol. 80:106890. doi: 10.1016/j.ntt.2020.106890
Cogswell, P. M., Wiste, H. J., Senjem, M. L., Gunter, J. L., Weigand, S. D., Schwarz, C. G., et al. (2021). Associations of quantitative susceptibility mapping with Alzheimer’s disease clinical and imaging markers. NeuroImage 224:117433. doi: 10.1016/j.neuroimage.2020.117433
Cottrell, J. E., and Hartung, J. (2020). Anesthesia and cognitive outcome in elderly patients: a narrative viewpoint. J. Neurosurg. Anesthesiol. 32, 9–17. doi: 10.1097/ANA.0000000000000640
Hong, X., Zhang, Z. X., Wu, L. Y., Shi, L. L., Zhao, X. H., and Wei, J. (2012). Validity of auditory verbal learning test in diagnosis of Alzheimer’s disease. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 34, 262–266. doi: 10.3881/j.issn.1000-503X.2012.03.014
Leung, J. L., Lee, G. T., Lam, Y. H., Chan, R. C., and Wu, J. Y. (2011). The use of the digit span test in screening for cognitive impairment in acute medical inpatients. Int. Psychogeriatr. 23, 1569–1574. doi: 10.1017/S1041610211000792
Li, W., Yue, L., and Xiao, S. (2022). Prospective associations of tea consumption with risk of cognitive decline in the elderly: a 1-year follow-up study in China. Front. Nutr. 9:752833. doi: 10.3389/fnut.2022.752833
Li, S., Zhang, X., Fang, Q., Zhou, J., Zhang, M., Wang, H., et al. (2017). Ginkgo biloba extract improved cognitive and neurological functions of acute ischaemic stroke: a randomised controlled trial. Stroke Vasc. Neurol. 2, 189–197. doi: 10.1136/svn-2017-000104
Martin, C. R., Preedy, V. R., Patel, V. B., and Rajendram, R. (2024). “The impact of stressful life events in Alzheimer’s disease” in Handbook of the behavior and psychology of disease. Ed. G. Vaitsa (Cham: Springer Nature Switzerland).
Meng, Z., Gao, C., Li, X., Shen, J., Hong, T., He, X., et al. (2021). Effects of combined epidural anesthesia and general anesthesia on cognitive function and stress responses of elderly patients undergoing liver cancer surgery. J. Oncol. 2021:8273722. doi: 10.1155/2021/8273722
Mossello, E., and Ballini, E. (2012). Management of patients with Alzheimer’s disease: pharmacological treatment and quality of life. Ther. Adv. Chronic Dis 3, 183–193. doi: 10.1177/2040622312452387
Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., et al. (2005). The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699. doi: 10.1111/j.1532-5415.2005.53221.x
Scheltens, P., De Strooper, B., Kivipelto, M., Holstege, H., Chételat, G., Teunissen, C. E., et al. (2021). Alzheimer’s disease. Lancet 397, 1577–1590. doi: 10.1016/S0140-6736(20)32205-4
Schlünzen, L., Vafaee, M. S., and Cold, G. E. (2007). Acupuncture of LI-4 in anesthetized healthy humans decreases cerebral blood flow in the putamen measured with positron emission tomography. Anesth. Analg. 104, 308–311. doi: 10.1213/01.ane.0000252927.10415.ec
Seitz, D. P., Reimer, C. L., and Siddiqui, N. (2013). A review of epidemiological evidence for general anesthesia as a risk factor for Alzheimer’s disease. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 47, 122–127. doi: 10.1016/j.pnpbp.2012.06.022
Seitz, D. P., Shah, P. S., Herrmann, N., Beyene, J., and Siddiqui, N. (2011). Exposure to general anesthesia and risk of Alzheimer’s disease: a systematic review and meta-analysis. BMC Geriatr. 11:83. doi: 10.1186/1471-2318-11-83
Selden, N., Geula, C., Hersh, L., and Mesulam, M. M. (1994). Human striatum: chemoarchitecture of the caudate nucleus, putamen and ventral striatum in health and Alzheimer’s disease. Neuroscience 60, 621–636. doi: 10.1016/0306-4522(94)90491-x
Serrano-Pozo, A., Frosch, M. P., Masliah, E., and Hyman, B. T. (2011). Neuropathological alterations in Alzheimer disease. Cold Spring Harb. Perspect. Med. 1:a006189. doi: 10.1101/cshperspect.a006189
Sohn, J. H., Lee, J. J., Lee, S. H., Kim, C., Yu, H., Kwon, Y. S., et al. (2021). Longitudinal study of the association between general anesthesia and increased risk of developing dementia. J. Pers. Med 11:11. doi: 10.3390/jpm11111215
Tsolaki, M., Sia, E., and Giannouli, V. (2024). Anesthesia and dementia: an up-to-date review of the existing literature. Appl. Neuropsychol. Adult 31, 181–190. doi: 10.1080/23279095.2022.2110871
Vanderweyde, T., Bednar, M., Forman, S. A., and Wolozin, B. (2010). Iatrogenic risk factors for Alzheimer’s disease: surgery and anesthesia. J. Alzheimers Dis. 22 Suppl 3, 91–104. doi: 10.3233/JAD-2010-100843
Walters, J. L., Chelonis, J. J., Fogle, C. M., Ferguson, S. A., Sarkar, S., Paule, M. G., et al. (2020). Acetyl-l-carnitine does not prevent neurodegeneration in a rodent model of prolonged neonatal anesthesia. Neurotoxicol. Teratol. 80:106891. doi: 10.1016/j.ntt.2020.106891
Wolz, R., Schwarz, A. J., Yu, P., Cole, P. E., Rueckert, D., Jack, C. R., et al. (2014). Robustness of automated hippocampal volumetry across magnetic resonance field strengths and repeat images. Alzheimers Dement. 10, 430–438.e2. doi: 10.1016/j.jalz.2013.09.014
Yoo, H. S., Lee, E. C., Chung, S. J., Lee, Y. H., Lee, S. G., Yun, M., et al. (2020). Effects of Alzheimer’s disease and lewy body disease on subcortical atrophy. Eur. J. Neurol. 27, 318–326. doi: 10.1111/ene.14080
Yu, W. (2017). Anesthesia with propofol and sevoflurane on postoperative cognitive function of elderly patients undergoing general thoracic surgery. Pak. J. Pharm. Sci. 30, 1107–1110.
Zhang, D., Ying, J., Ma, X., Gao, Z., Chen, H., Zhu, S., et al. (2020). Social cognitive dysfunction in elderly patients after anesthesia and surgery. Front. Psychol. 11:541161. doi: 10.3389/fpsyg.2020.541161
Keywords: surgery, general anesthesia, MRI, putamen, 2 cognitive function, older adults
Citation: Jiang J, Zhang Z, Zheng H, Lu J and Li W (2024) The impact of surgery with general anesthesia on cognitive function and putamen volume: a cross-sectional study among older adults. Front. Aging Neurosci. 16:1483989. doi: 10.3389/fnagi.2024.1483989
Edited by:
Enzo Emanuele, 2E Science, ItalyReviewed by:
Vaitsa Giannouli, Aristotle University of Thessaloniki, GreeceJames Cottrell, Downstate Health Sciences University, United States
John Hartung, Downstate Health Sciences University, United States, in collaboration with reviewer JC
Copyright © 2024 Jiang, Zhang, Zheng, Lu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jian Lu, MTM2MDE3NDQ5MjlAMTYzLmNvbQ==; Wei Li, ODIyMjAzODY3QHFxLmNvbQ==
†These authors have contributed equally to this work
 Jianjun Jiang
Jianjun Jiang Zhuyun Zhang2†
Zhuyun Zhang2† Hong Zheng
Hong Zheng Wei Li
Wei Li