- 1Department of Nephrology, Beijing Shijitan Hospital, Capital Medical University, Beijing, China
- 2Department of Neurology, Beijing Shijitan Hospital, Capital Medical University, Beijing, China
- 3Division of Injury Prevention and Mental Health National Center for Chronic and Non-Communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention, Beijing, China
Background: The mechanism of cognitive impairment in hemodialysis patients is multifactorial. The relationship between cerebral blood flow and the decline of cognitive function is poorly understood.
Objective: To investigate the association between cerebral blood flow variation and decline of cognitive function in older patients undergoing hemodialysis.
Methods: In this prospective observational cohort study of 121 older patients undergoing hemodialysis, we used transcranial Doppler ultrasound (TCD) to measure cerebral arterial mean flow velocity (MFV) throughout dialysis, assessed cognitive function at baseline and 12-month follow-up, and then analyzed associations between MFV and changes on cognitive scores.
Results: TCD recordings demonstrated a significant reduction in MFV throughout dialysis, which were significantly correlated with cumulative ultrafiltration volume (rho 0.356, p < 0.001), ΔSBP (rho 0.251, p = 0.005), and ΔMAP (rho 0.194, p = 0.032). Compared with the baseline assessments, cognitive scores of participants at the 12-month follow-up were significantly worsened in global cognition (MOCA), some tests of memory (CFT-memory), executive function (TMT-B, SCWT-C, and SCWT-T), attention/processing speed (SDMT), and visuospatial function (CFT-copy) (p < 0.05). The worsening scores in global cognition (MOCA) (β = 0.066, 95% CI 0.018–0.113, p = 0.007) and some tests of memory (AVLT5) (β = 0.050, 95% CI 0.004–0.097, p = 0.035) and executive function (TMT-B, SCWT-C, SCWT-T) (β = 1.955, 95% CI 0.457–3.453, p = 0.011; β = 0.298, 95% CI 0.112–0.484, p = 0.002 and β = 1.371, 95% CI 0.429–2.303, p = 0.004, respectively) were significantly associated with the reduction of MFV.
Conclusion: Hemodialysis may significantly reduce cerebral blood flow in older patients; Repetitive intradialytic decreases in CBF may be one of the mechanisms underlying the decline of cognitive function.
Clinical trial registration: https://register.clinicaltrials.gov/prs/app/action/SelectProtocol?sid=S000C5B5&selectaction=Edit&uid=U0003QEL&ts=4&cx=-djoi2
Introduction
The heavy burden of cognitive impairment in hemodialysis patients has received great attention in the last decade, not only because it has a higher prevalence compared with that in the general population, but also because the decline of cognitive function is independently associated with poor quality of life and clinical adverse outcomes (Drew et al., 2015; Angermann et al., 2018; Cheung and LaMantia, 2019). Currently, the mechanisms of cognitive decline in hemodialysis patients are still not fully elucidated, some studies are focused on the issue of brain ischemia jury which is regarded to be one of the main etiologies of cognitive impairment, besides some common risk factors like older age, lower education level, history of stroke, and hypertension, dialysis-related risk factors like insufficient clearance of renal toxins, prolonged dialysis vintage, micro-inflammation, and hemodynamic instability were reported to be associated with cognitive impairment and its progression in hemodialysis patients (Kurella Tamura et al., 2016; O’Lone et al., 2016; Drew et al., 2019).
As conventional hemodialysis treatment includes the water removal process, it is inevitable for the patients to experience a certain degree of hemodynamic changes (Ma and Zhao, 2017). There is increasing evidence that hemodynamic instability during dialysis treatment might related to brain injury including ischemia stroke and cognitive impairments (Drew and Sarnak, 2014; Teuwafeu et al., 2023). A recent prospective study from the Netherlands applied positron emission tomography-computed tomography (PET-CT) to compare cerebral blood flow (CBF) changes before and during hemodialysis treatment, the results showed that conventional hemodialysis induces a significant reduction in global and regional CBF in older patients during hemodialysis, and repetitive intradialytic decreases in CBF may be one of the mechanisms by which hemodialysis induces cerebral ischemic injury (Polinder-Bos et al., 2018). This result provided a hint about the influence of CBF reduction on the decline of cognitive function in hemodialysis patients. However, performing the PET-CT examination during dialysis treatment is too complex in practical settings. Hence, finding alternative measures to reflect the variation in brain blood volume in hemodialysis patients is necessary.
Transcranial Doppler (TCD) ultrasound is a noninvasive, convenient tool that is capable of performing repeated measurements of cerebral blood flow throughout a hemodialysis session, it has been widely applied in the evaluation of CBF (Stefanidis et al., 2005; Shaker et al., 2018). Depending on the previously reported features of hemodynamic changes in dialysis patients and the current understanding of the relationship between brain ischemia and cognitive decline, we hypothesized that TCD-measured cerebral blood flow would be reduced during hemodialysis sessions and these repetitive changes of CBF would be associated with the progressive cognitive impairment. We validated our hypotheses in a prospective cohort, our study aimed to explore whether there was cerebral blood flow reduction in dialysis sessions and whether these changes were associated with the decline of cognitive function over a 12-month follow-up.
Materials and methods
Study design and participants
This is a prospective observational cohort study. We measured cerebral arterial mean flow velocity (MFV), an index of brain blood flow, at several time points throughout a dialysis session with TCD. Using well-validated neuropsychological batteries, we compared cognitive function at baseline and 12 months of follow-up and accessed correlations between the variation of MFV and changes in cognitive function scores. We recruited eligible patients from the hemodialysis centers of Beijing Shijitan Hospital from April to June 2022. The inclusion criteria were as follows: (1) age ≥ 50 years old, (2) end-stage kidney disease with maintained hemodialysis treatment for a minimum of 3 months, (3) willing to join the study and provide written informed consent, and (4) the patient’s native language was Chinese. The exclusion criteria were as follows: (1) unable to complete the middle cerebral artery ultrasound examination, (2) unable to complete a 90-min cognitive and physical function battery for reasons such as sensory (e.g., visual and hearing) or motor impairment, (3) experienced disturbance of consciousness or recently diagnosed with psychosis, and (4) had a plan of kidney transplantation within 12 months of baseline. This study was approved after ethical review by the Institutional Ethical Review Board of Beijing Shijitan Hospital, Capital Medical University (Approval No. sjtkyll-lx-2022-078), and registered on Clinicaltrials.gov under identifier NCT05555836. Written informed consent was completed for each participant.
Clinical variables
Patients’ sociodemographic information and basic characteristics were obtained from their medical charts at the time of enrollment. Medical history, including history of cardiovascular disease (CVD, a composite of either coronary artery disease and/or peripheral vascular disease), stroke, diabetes, hypertension, smoking, alcohol intake, and dialysis vintage, was defined by the patient’s history or documentation in the patient’s medical chart. Physical examination included mean monthly systolic blood pressure (SBP), diastolic blood pressure (DBP), and body mass index (BMI). Pre-dialysis blood tests included measurement of the serum levels of hemoglobin, albumin, calcium, phosphate, intact parathyroid hormone (iPTH), and C-reactive protein (CRP). The estimated glomerular filtration rate (eGFR) was calculated by using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation with an adjusted coefficient of 1.1 for the Asian population, the single-pool Kt/V was calculated from the pre-and post-dialysis serum urea nitrogen levels as we applied in the previous study (Guo et al., 2022).
TCD monitored cerebral arterial mean flow velocity in hemodialysis sessions
All participants underwent their routine prescribed dialysis treatment. The median blood flow rates were 280 (IQR, 240.0–320.0) mL/min. Dialysate temperature was set at 36.5°C. On the day of dialysis, the patient was in a supine position. We used transcranial Doppler ultrasound to monitor the mean flow velocity (MFV) of the middle cerebral artery (MCA) throughout dialysis. The average MCA blood flow velocity was recorded at seven time points (T1 to T7), including 15 min before dialysis, 15, 30, 60, 120, 180 min during dialysis, and after dialysis. Meanwhile, we also recorded dialysis-related variables, including SBP, DBP, and ultrafiltration volume. To minimize measurement errors, all Doppler readings were performed by two trained examiners following standardized protocols.
Assessment of cognitive function
Cognitive assessments were conducted at study enrollment and repeated at 12-month follow-up. According to the recommendation of the fifth version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), we evaluated the global cognitive function with the Beijing version of the Montreal Cognitive Assessment (MOCA), and cognitive function in five different cognitive domains (verbal and memory, complex attention, executive function, language, visual–spatial function), each domain was assessed using validated neuropsychological tests (Sachdev et al., 2014; Tian et al., 2020). It included: (1) attention/processing speed, using the Symbol Digit Modalities Test (SDMT), and the Chinese-modified version of the Trail Making Test A (TMT-A) (Eadie and Shum, 1995; Ma et al., 2015); (2) executive function, using the Chinese-modified version of the Trail Making Tests B (TMT-B), and a modified version of the Stroop Color-Word Test (SCWT) (Zhou and Jia, 2009); (3) verbal memory, using the Chinese version of the Auditory Verbal Learning Test (AVLT) for short-and long-delay free recall and complex figure for visual memory (delayed recall test; Chinese version) (Dai et al., 1990); (4) language, using the Chinese-modified versions of Boston Naming Test (BNT) and Animal Fluency Test (AFT) (Guo et al., 2009; Huang et al., 2016); and (5) visual-space function, using the Rey–Osterrieth Complex Figure (CFT) (Li et al., 2018). All of the staff for the neuropsychological assessments were trained and certified by the same neuropsychologist before the study commencement. To avoid the influence of hemodynamic changes during the dialysis treatment, a neuropsychological evaluation was conducted individually on the day after a dialysis session. Patients were kept comfortable during their cognitive assessments, including rest periods if needed.
Statistical analysis
Baseline characteristics are presented in descriptive statistics, with mean and standard deviation (SD) or median with interquartile range (IQR) given for continuous variables, and percentages given for categorical variables. MFV at each time point throughout dialysis was analyzed using a paired sample Wilcoxon signed-rank test. ΔMFV = MFV (T1) − MFV (T7). Spearman correlation analysis was performed to evaluate the association between the decline in MFV and dialysis-related variables. Cognitive scores at baseline and 12 months are also paired data and were compared using the Wilcoxon signed-rank test. The correlation between changes in cognitive scores and the percentage of decline in MFV was assessed using Spearman rank correlation.
We used multivariable linear regression models to analyze the relationship between the changes in MFV and worsening cognitive function, with worsening cognitive scores as the dependent variable, percentage of changes in MFV as independent variables, and variables associated with worsening cognition on unadjusted analyses with p ≤ 0.10 and potential clinical risk factors for cognitive impairment were entered into the multivariate linear regression models as covariates. All analyses were performed with SPSS version 21.0 statistical software (SPSS Inc., Chicago, IL, USA). Statistical significance was set at a value of p < 0.05.
Results
Baseline characteristics of participants
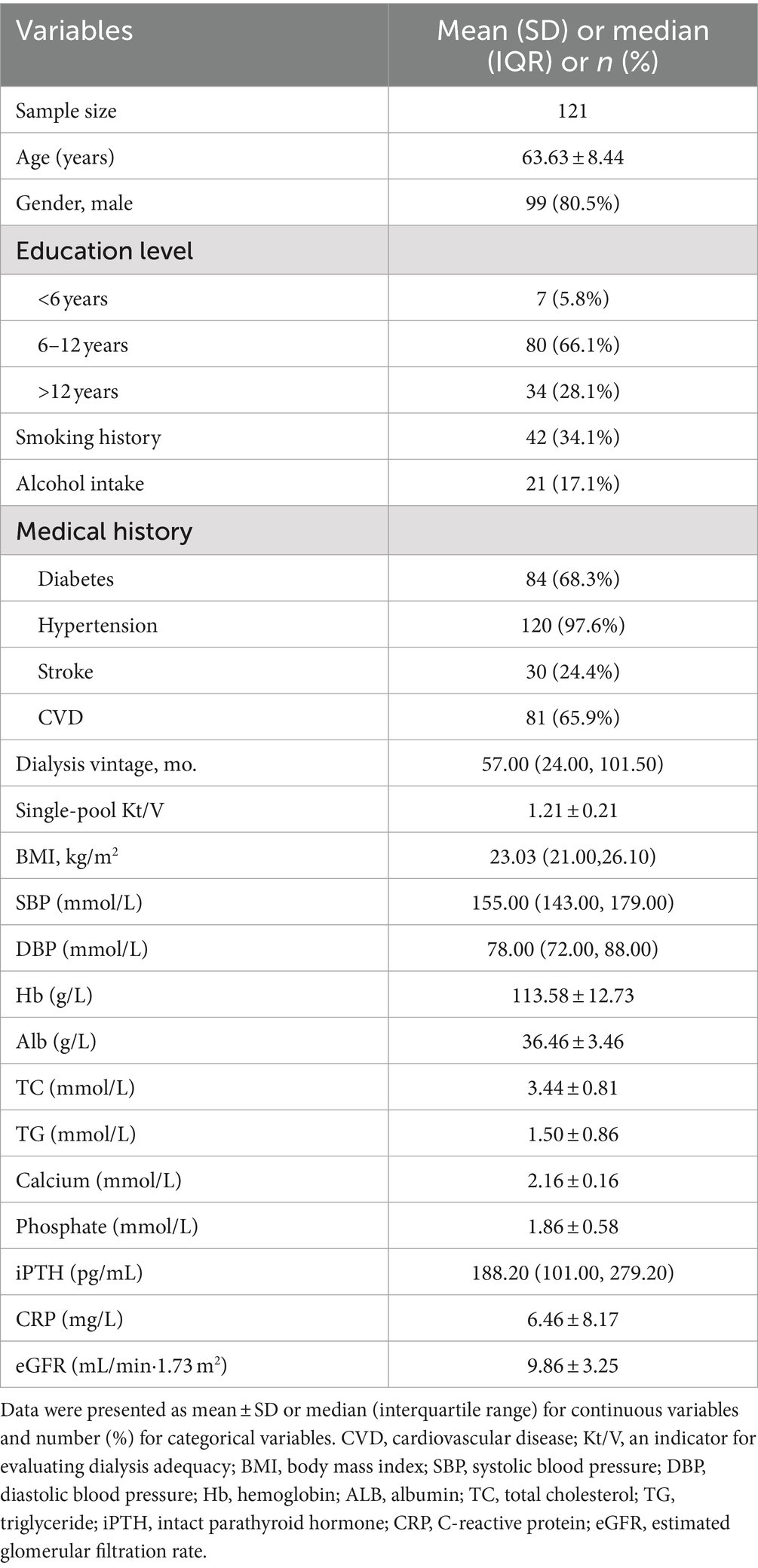
Among the 140 eligible patients, 12 patients could not complete comprehensive cognitive tests and seven patients’ middle cerebral arteries could not be detected with the TCD, a total of 19 patients were excluded. Finally, 121 patients were enrolled and finished the follow-up. Baseline characteristics of the remaining 121 patients were shown in Table 1, the mean age was 63.63 ± 8.44 years, 19.5% were women, and only 5.8% had less than 6 years of education. Hypertension (97.6%), diabetes (68.3%), and CVD (65.9%) were the most common diseases in medical history. The dialyzers with polyacrylonitrile, polysulfone, and polycarbonate membranes used for hemodialysis were 65.5, 23.4, and 11.1%, respectively. The average weekly hemodialysis treatment length was 11.40 ± 0.78 h.
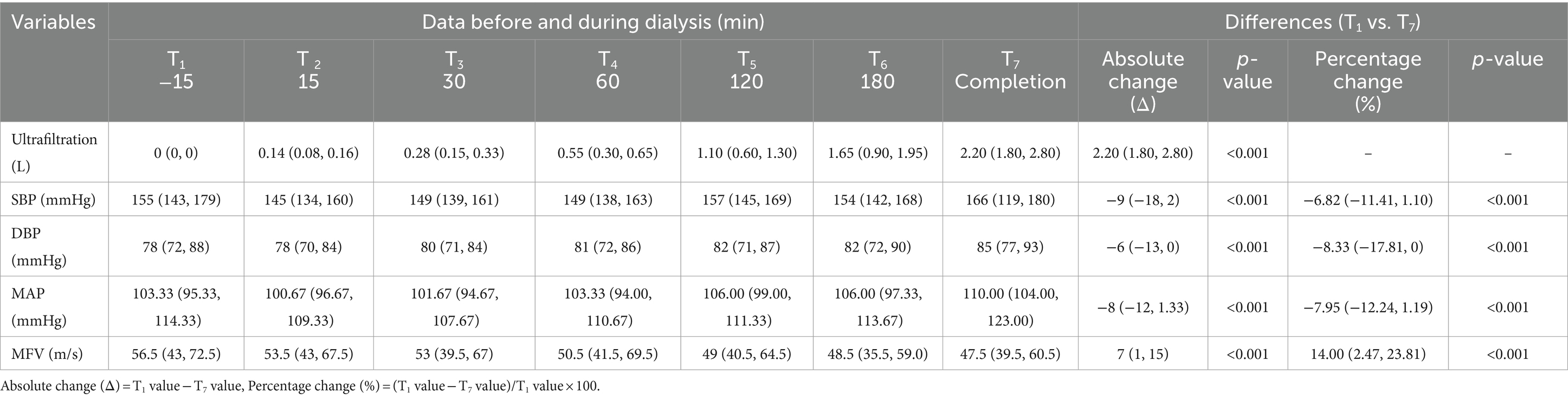
Cerebral blood flow changes in a hemodialysis session
The readings of MFV and other dialysis-related indicators (ultrafiltration volume, SBP, DBP, and MAP) before and during dialysis are shown in Table 2. MFV generally reduced after dialysis began, remaining lower up to the completion of dialysis (median MFV reading from 56.5 to 47.5 cm/s; p < 0.001). The median percentage of decline was 14.00% (IQR, 2.47–23.81%) (Figure 1; Table 2). Spearman correlation analysis results show that cumulative ultrafiltration volume (rho 0.356, p < 0.001), ΔSBP (rho 0.251, p = 0.005), ΔMAP (rho 0.194, p = 0.032), were significantly correlated with ΔMFV.
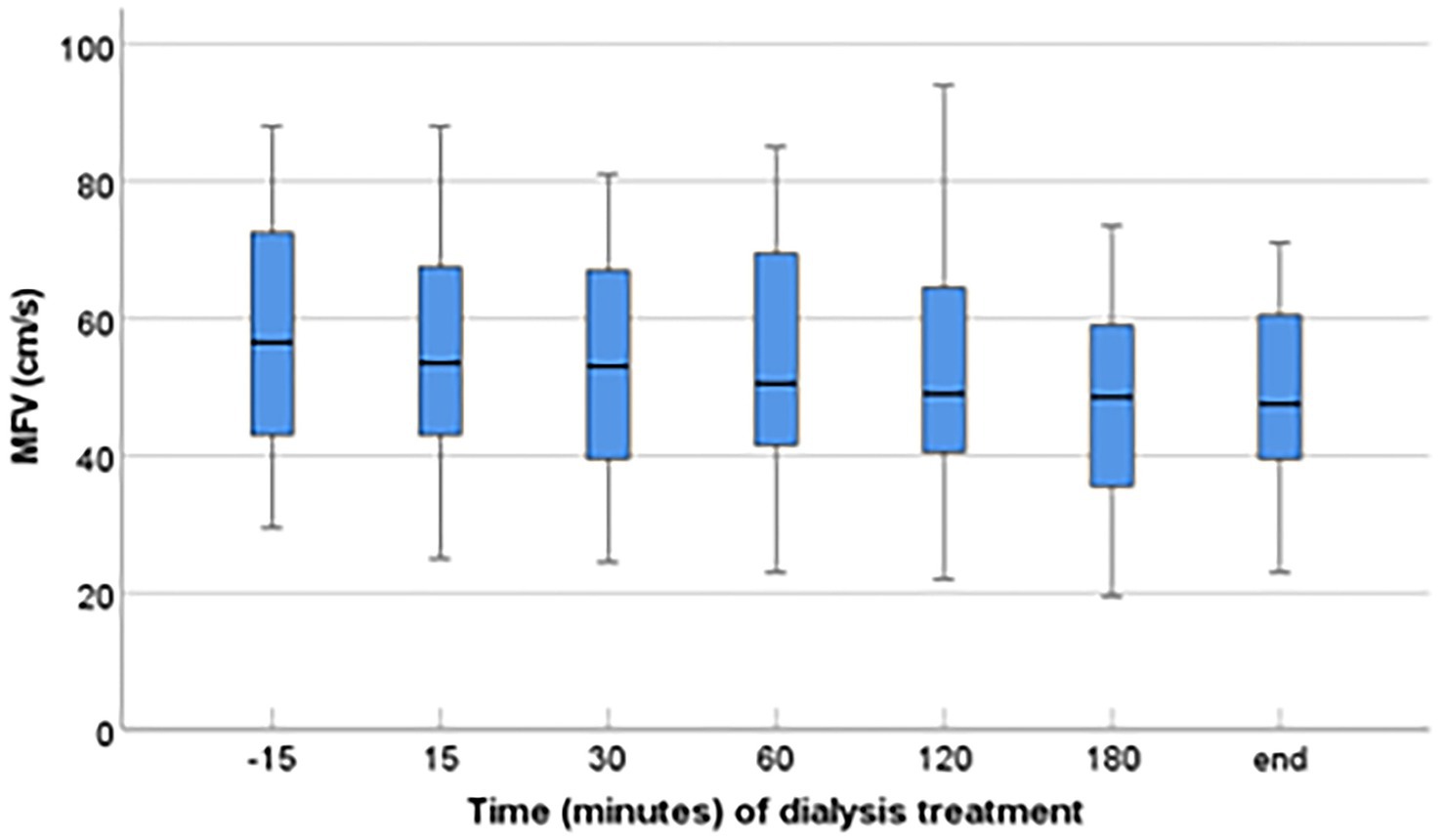
Figure 1. Variation of cerebral mean flow velocity (MFV) of the middle cerebral artery during hemodialysis session. The change in MFV during dialysis sessions is presented as a median value, IQR, maximum, and minimum values. TCD recordings were taken before and during dialysis, demonstrating a significant decline in MFV during dialysis (p < 0.001).
Cognitive function at baseline and 12 months follow-up
During the follow-up, four participants withdrew, and 13 patients died. Paired baseline and 12-month cognition assessments were possible in 104 participants. The raw scores of each test are presented in Table 3. Compared with the baseline assessments, participants’ cognitive scores at 12-month follow-up were significantly worsened in global cognition (MOCA), one test of memory (CFT-memory), three tests of executive function (TMT-B, SCWT-C, and SCWT-T), one test of attention/processing speed (SDMT), and one test of visuospatial function (CFT-copy). The worsening scores in global cognition (MOCA) and three tests of executive function (TMT-B, SCWT-C, and SCWT-T) were significantly correlated with the percentage of decline in MFV (p < 0.05) (Table 3).
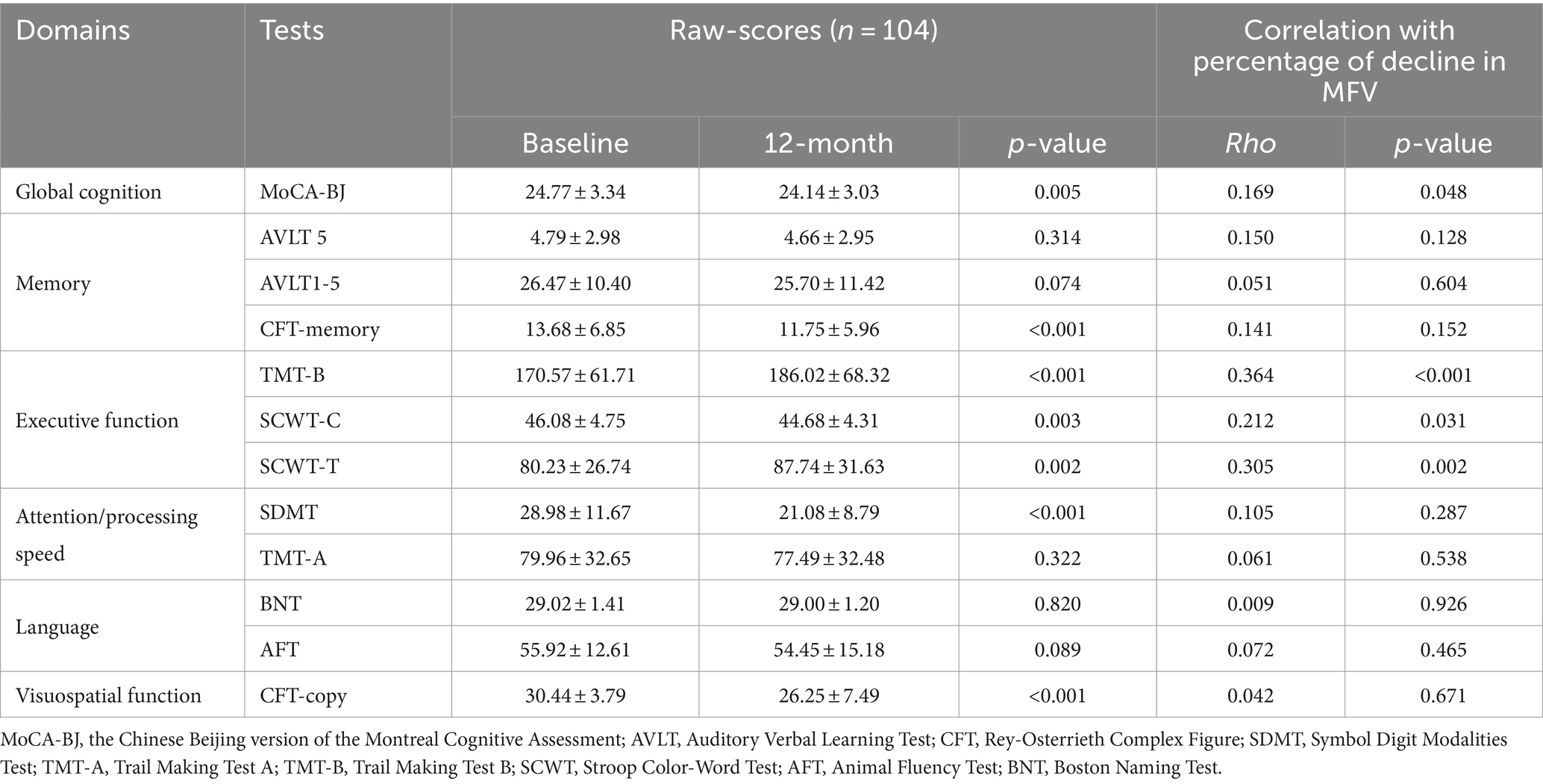
Table 3. Differences in cognitive scores between baseline and 12-month follow-up and their correlation with percentage decrease in MFV.
Association between the variation of MFV and the cognition decline
Multivariable linear regression analysis showed that the worsening scores in global cognition (MOCA) (β = 0.066, 95% CI 0.018–0.113, p = 0.007), one tests of memory (AVLT5) (β = 0.050, 95% CI 0.004–0.097, p = 0.035) and all three tests of executive function (TMT-B, SCWT-C, SCWT-T) (β = 1.955, 95% CI 0.457–3.453, p = 0.011; β = 0.298, 95% CI 0.112–0.484, p = 0.002 and β = 1.371, 95% CI 0.429–2.303, p = 0.004, respectively) were significantly associated with the percentage of decline in MFV (Table 4).
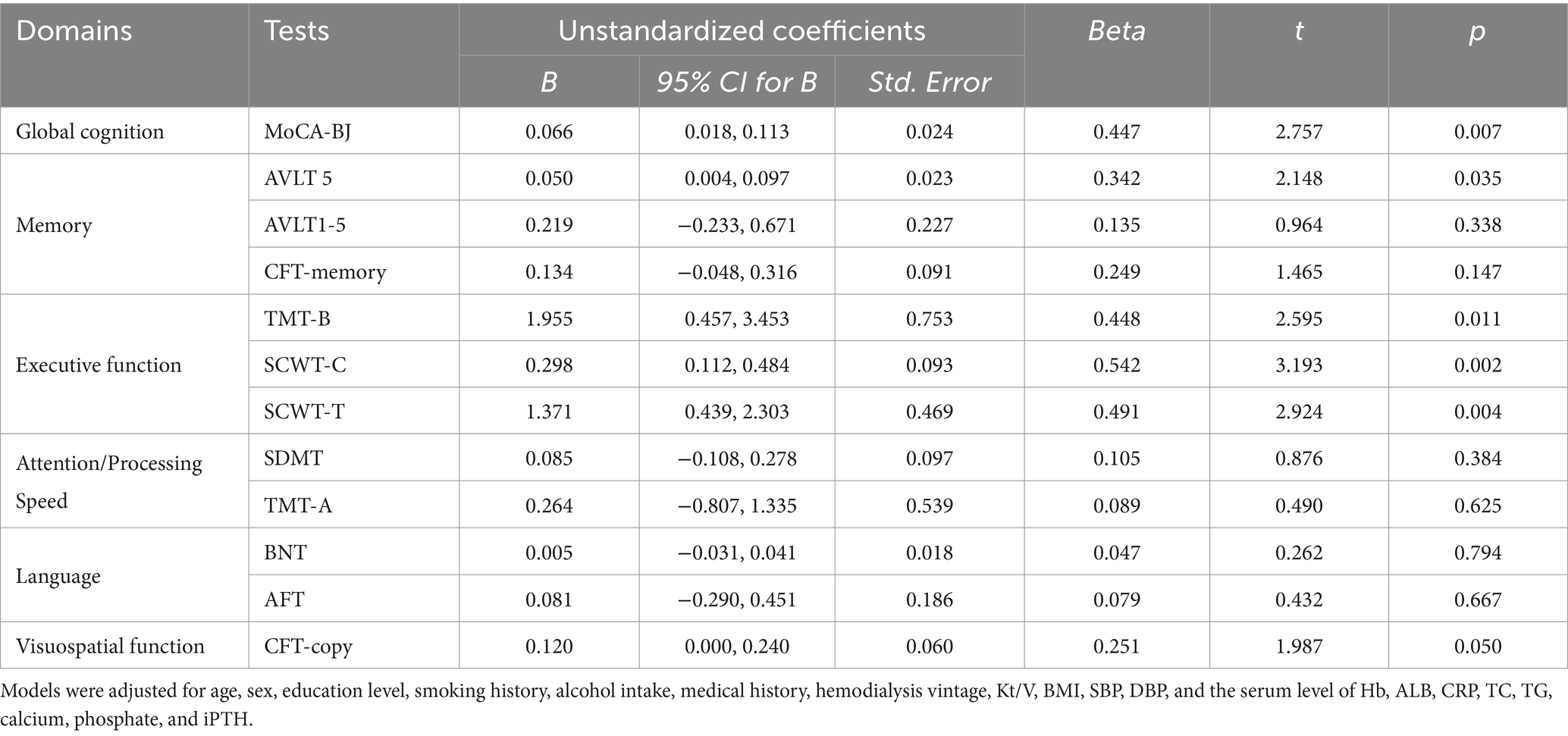
Table 4. Multivariable linear regression analysis for association between the worsening cognitive scores and percentage of reduction of MFV.
Discussion
In this prospective study, we demonstrated cerebral blood flow kept reducing in a hemodialysis session, the median percentage of this reduction was 14%. This brain hemodynamic change was closely correlated with the decline of global cognitive function, notably, the association between cerebral blood flow reduction and the cognitive decline appears to be inconsistent in different cognitive domains, only the decline of the executive domain and memory domain was found to be related to cerebral blood flow reduction. Our data validated the impact of hemodialysis-related reduction of brain blood perfusion on the progression of cognitive impairment among hemodialysis patients.
Previous studies indicated that patients undergoing hemodialysis not only have a high prevalence of cognitive impairment compared to the general population, but also experience a decline of cognitive function over time, and this is predominantly among older individuals (Polinder-Bos et al., 2018; Luo et al., 2020; Guo et al., 2022). It seems urgent to explore the potentially related risk factors and etiologies of cognitive decline. Currently, brain ischemia has been confirmed as one of the main etiologies for the pathological process of cognitive impairment, and finding brain ischemia-related risk factors has become a hot topic in this area (Romero et al., 2009; Igari et al., 2019). Older age, atherosclerosis-related factors like diabetes, hyperlipidemia, and hypertension are confirmed to be related to the impairments of cognitive function. These risk factors were also validated among hemodialysis patients with cognitive impairments. Notably, some dialysis-related risk factors like insufficient clearance of renal toxins, prolonged dialysis vintage, and hemodynamic instability were also reported to be associated with cognitive impairment and its progression in hemodialysis patients (MacEwen et al., 2017; Moist and McIntyre, 2019). However, the characteristics of the hemodynamic changes in hemodialysis patients are not fully elucidated. Polinder-Bos et al. (2018) applied [15O] H2O PET-CT to compare CBF changes before and during hemodialysis treatment, the results showed that conventional hemodialysis induces a significant reduction in global and regional CBF in older patients during hemodialysis. However, performing the [15O] H2O PET-CT examination during dialysis treatment is not convenient in practical settings, so finding alternative measures to reflect the variation in brain blood volume in hemodialysis patients is necessary. TCD ultrasound is a noninvasive, convenient tool that is capable of performing repeated measurements of cerebral blood flow throughout a hemodialysis session, it has been widely applied in the evaluation of CBF (Stefanidis et al., 2005; Ghoshal and Freedman, 2019). In our study, we measured MFV at different time points in a dialysis session, and there was an average of 14% reduction in MFV throughout dialysis, which was significantly correlated with cumulative ultrafiltration volume, and changes in blood pressure. Richerson et al. (2022) also found significant relationships between the variations of cerebral oxygenation saturation and intradialytic blood pressure change and cumulative ultrafiltration dose in 26 hemodialysis patients. Our results indicated that there is a brain blood flow reduction during hemodialysis treatment, this status might lead to brain ischemia in combination with other conventional risk factors like older age, and vascular atherosclerosis-related factors.
Another major issue in building up the relationship between brain ischemia and cognitive decline is identifying the progression features of cognitive impairment with the prolonged dialysis vintage and associated risk factors. Drew et al. (2017) demonstrated significant cognitive decline over time, particularly within tests of executive function in 314 prevalent hemodialysis patients. Older age was the only statistically significant risk factor for steeper cognitive decline, as for other potential related risk factors, the authors believed that there were 156 deaths in the 2 years of follow-up, this high mortality rate might have some influence in identifying the potential risk factors in their study. Findlay et al. (2019) reported that patients undergoing hemodialysis experienced a transient decline in cerebral blood flow using the measurement of MFV with TCD, and this reduction of brain blood flow was correlated with intradialytic cognitive decline. Compared with those studies, we tested these related issues in a group of 121 hemodialysis patients, the results of our study indicated that the worsening scores were in the test of global cognition, executive function, and some tests of memory function, the inconsistent decline of cognitive function in different domains also indicated the ischemia related injury in various parts of the brain is different. Taken together, our data provide evidence that both reduction of CBF during dialysis sessions and decline of cognitive function exist in hemodialysis patients, and this reduction of brain blood flow may play a pivotal role in the progression of cognitive impairment in hemodialysis patients. Strictly administrating the water intake between hemodialysis sessions and appropriately setting a proper ultrafiltration rate during dialysis will be helpful in keeping the hemodynamics stable during hemodialysis, which in turn retard the progression of brain ischemia-related cognitive impairment.
We demonstrated the relationship between the reduction of brain blood flow and cognitive decline in hemodialysis patients in this prospective cohort. However, we recognize the following limitations. As an observational study, we do not have data for patients who are younger than 50 because the assessment batteries were all prepared for middle and older aged populations, at the same time, some senior-aged patients who have visual and hearing impairments could not be enrolled in our study, all these could bring selection bias in our study. We also need to clarify that TCD measurement is an indirect measure of cerebral blood flow, the accuracy of the TCD measurement is inferior to the [15O] H2O PET-CT examination, which is regarded as a gold standard in this area; the MFV results may be influenced by some unaccounted variables like blood viscosity and blood vessel diameter, which we did not have records in this study.
In conclusion, there is a significant reduction in cerebral blood flow in older patients undergoing Hemodialysis, which is related to cumulative ultrafiltration volume and changes in blood pressure. This repetitive intradialytic decrease in cerebral blood flow may be one of the major mechanisms underlying the decline of cognitive function in hemodialysis patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Institutional Ethical Review Board of Beijing Shijitan Hospital, Capital Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YG: Writing – original draft, Investigation. WC: Methodology, Writing – original draft, Investigation. PY: Writing – original draft, Methodology, Investigation. YL: Writing – review & editing, Writing – original draft, Investigation, Funding acquisition, Conceptualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by a grant from the Capital’s Funds for Health Improvement and Research (CFH 2022-2-2081) and the Beijing Municipal Science & Technology Commission’s national key research and development plan matching project (Z161100002616005).
Acknowledgments
We would like to acknowledge the funding agencies-the Beijing Municipal Commission of Science and Technology and the Beijing Municipal Commission of Health. We are grateful to our study participants and the research team.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Angermann, S., Schier, J., Baumann, M., Steubl, D., Hauser, C., Lorenz, G., et al. (2018). Cognitive impairment is associated with mortality in hemodialysis patients. J. Alzheimer's Dis. 66, 1529–1537. doi: 10.3233/JAD-180767
Cheung, K. L., and LaMantia, M. A. (2019). Cognitive impairment and mortality in patients receiving hemodialysis: implications and future research avenues. Am. J. Kidney Dis. 74, 435–437. doi: 10.1053/j.ajkd.2019.06.002
Dai, X. Y., Ryan, J. J., Paolo, A. M., and Harrington, R. G. (1990). Factor analysis of the mainland Chinese version of the Wechsler Adult Intelligence Scale (WAIS-RC) in a brain-damaged sample. Int. J. Neurosci. 55, 107–111. doi: 10.3109/00207459008985956
Drew, D. A., and Sarnak, M. J. (2014). Ischemic and hemorrhagic stroke: high incidence in hemodialysis and peritoneal dialysis patients. Am. J. Kidney Dis. 63, 547–548. doi: 10.1053/j.ajkd.2014.01.009
Drew, D. A., Weiner, D. E., and Sarnak, M. J. (2019). Cognitive impairment in CKD: pathophysiology, management, and prevention. Am. J. Kidney Dis. 74, 782–790. doi: 10.1053/j.ajkd.2019.05.017
Drew, D. A., Weiner, D. E., Tighiouart, H., Duncan, S., Gupta, A., Scott, T., et al. (2017). Cognitive decline and its risk factors in prevalent hemodialysis patients. Am. J. Kidney Dis. 69, 780–787. doi: 10.1053/j.ajkd.2016.11.015
Drew, D. A., Weiner, D. E., Tighiouart, H., Scott, T., Lou, K., Kantor, A., et al. (2015). Cognitive function and all-cause mortality in maintenance hemodialysis patients. Am. J. Kidney Dis. 65, 303–311. doi: 10.1053/j.ajkd.2014.07.009
Eadie, K., and Shum, D. (1995). Assessment of visual memory: a comparison of Chinese characters and geometric figures as stimulus materials. J. Clin. Exp. Neuropsychol. 17, 731–739. doi: 10.1080/01688639508405163
Findlay, M. D., Dawson, J., Dickie, D. A., Forbes, K. P., McGlynn, D., Quinn, T., et al. (2019). Investigating the relationship between cerebral blood flow and cognitive function in hemodialysis patients. J. Am. Soc. Nephrol. 30, 147–158. doi: 10.1681/ASN.2018050462
Ghoshal, S., and Freedman, B. I. (2019). Mechanisms of stroke in patients with chronic kidney disease. Am. J. Nephrol. 50, 229–239. doi: 10.1159/000502446
Guo, Y., Tian, R., Ye, P., Li, X., Li, G., Lu, F., et al. (2022). Cognitive domain impairment and all-cause mortality in older patients undergoing hemodialysis. Front. Endocrinol. 13:828162. doi: 10.3389/fendo.2022.828162
Guo, Q., Zhao, Q., Chen, M., Ding, D., and Hong, Z. (2009). A comparison study of mild cognitive impairment with 3 memory tests among Chinese individuals. Alzheimer Dis. Assoc. Disord. 23, 253–259. doi: 10.1097/WAD.0b013e3181999e92
Huang, C. Y., Hwang, A. C., Liu, L. K., Lee, W. J., Chen, L. Y., Peng, L. N., et al. (2016). Association of dynapenia, sarcopenia, and cognitive impairment among community-dwelling older Taiwanese. Rejuvenation Res. 19, 71–78. doi: 10.1089/rej.2015.1710
Igari, R., Davy, P., Sato, H., Takahashi, Y., Iseki, C., Kato, H., et al. (2019). Cognitive impairment, brain ischemia, and shorter telomeres are predictors of mortality in the Japanese elderly: a 13-year prospective community-based study. J. Neurol. Sci. 397, 129–134. doi: 10.1016/j.jns.2018.12.038
Kurella Tamura, M., Yaffe, K., Hsu, C. Y., Yang, J., Sozio, S., Fischer, M., et al. (2016). Cognitive impairment and progression of CKD. Am. J. Kidney Dis. 68, 77–83. doi: 10.1053/j.ajkd.2016.01.026
Li, G., Tang, H., Chen, J., Qi, X., Chen, S., and Ma, J. (2018). Executive and visuospatial dysfunction in patients with primary restless legs syndrome/Willis-Ekbom disease: study of a Chinese population. J. Clin. Sleep Med. 14, 785–790. doi: 10.5664/jcsm.7106
Luo, Y., Murray, A. M., Guo, Y. D., Tian, R., Ye, P. P., Li, X., et al. (2020). Cognitive impairment and associated risk factors in older adult hemodialysis patients: a cross-sectional survey. Sci. Rep. 10:12542. doi: 10.1038/s41598-020-69482-1
Ma, J., Zhang, Y., and Guo, Q. (2015). Comparison of vascular cognitive impairment--no dementia by multiple classification methods. Int. J. Neurosci. 125, 823–830. doi: 10.3109/00207454.2014.972504
Ma, L., and Zhao, S. (2017). Risk factors for mortality in patients undergoing hemodialysis: a systematic review and meta-analysis. Int. J. Cardiol. 238, 151–158. doi: 10.1016/j.ijcard.2017.02.095
MacEwen, C., Sutherland, S., Daly, J., Pugh, C., and Tarassenko, L. (2017). Relationship between hypotension and cerebral ischemia during hemodialysis. J. Am. Soc. Nephrol. 28, 2511–2520. doi: 10.1681/ASN.2016060704
Moist, L. M., and McIntyre, C. W. (2019). Cerebral ischemia and cognitive dysfunction in patients on dialysis. Clin. J. Am. Soc. Nephrol. 14, 914–916. doi: 10.2215/CJN.00400119
O’Lone, E., Connors, M., Masson, P., Wu, S., Kelly, P. J., Gillespie, D., et al. (2016). Cognition in people with end-stage kidney disease treated with hemodialysis: a systematic review and meta-analysis. Am. J. Kidney Dis. 67, 925–935. doi: 10.1053/j.ajkd.2015.12.028
Polinder-Bos, H. A., García, D. V., Kuipers, J., Elting, J., Aries, M., Krijnen, W. P., et al. (2018). Hemodialysis induces an acute decline in cerebral blood flow in elderly patients. J. Am. Soc. Nephrol. 29, 1317–1325. doi: 10.1681/ASN.2017101088
Richerson, W. T., Schmit, B. D., and Wolfgram, D. F. (2022). The relationship between cerebrovascular reactivity and cerebral oxygenation during hemodialysis. J. Am. Soc. Nephrol. 33, 1602–1612. doi: 10.1681/ASN.2021101353
Romero, J. R., Beiser, A., Seshadri, S., Benjamin, E. J., Polak, J. F., Vasan, R. S., et al. (2009). Carotid artery atherosclerosis, MRI indices of brain ischemia, aging, and cognitive impairment: the Framingham study. Stroke 40, 1590–1596. doi: 10.1161/STROKEAHA.108.535245
Sachdev, P., Kalaria, R., O'Brien, J., Skoog, I., Alladi, S., Black, S. E., et al. (2014). Diagnostic criteria for vascular cognitive disorders: a VASCOG statement. Alzheimer Dis. Assoc. Disord. 28, 206–218. doi: 10.1097/WAD.0000000000000034
Shaker, A. M., Mohamed, O. M., Mohamed, M. F., and El-Khashaba, S. O. (2018). Impact of correction of anemia in end-stage renal disease patients on cerebral circulation and cognitive functions. Saudi J. Kidney Dis. Transpl. 29, 1333–1341. doi: 10.4103/1319-2442.248306
Stefanidis, I., Bach, R., Mertens, P. R., Liakopoulos, V., Liapi, G., Mann, H., et al. (2005). Influence of hemodialysis on the mean blood flow velocity in the middle cerebral artery. Clin. Nephrol. 64, 129–137. doi: 10.5414/cnp64129
Teuwafeu, D. G., Halle, M. P., Kenfack, N. A., Nkouonlack, C. D., Fouda, H., Nkoke, C., et al. (2023). Stroke and its correlates among patients on maintenance hemodialysis in Cameroon. Hemodial Int 27, 419–427. doi: 10.1111/hdi.13097
Tian, R., Guo, Y., Ye, P., Zhang, C., and Luo, Y. (2020). The validation of the Beijing version of the Montreal cognitive assessment in Chinese patients undergoing hemodialysis. PLoS One 15:e0227073. doi: 10.1371/journal.pone.0227073
Keywords: hemodialysis, cognitive decline, cerebral arterial mean flow velocity, transcranial Doppler ultrasound, neurocognitive battery
Citation: Guo Y, Cui W, Ye P and Luo Y (2024) Association between cerebral blood flow variation and cognitive decline in older patients undergoing hemodialysis. Front. Aging Neurosci. 16:1457675. doi: 10.3389/fnagi.2024.1457675
Edited by:
Chinedu Udeh-Momoh, Wake Forest University, United StatesReviewed by:
Anne Murray, Hennepin Healthcare, United StatesJuan Moisés De La Serna, International University of La Rioja, Spain
Copyright © 2024 Guo, Cui, Ye and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Luo, bHVveUBianNqdGguY24=
 Yidan Guo
Yidan Guo Wei Cui
Wei Cui Pengpeng Ye
Pengpeng Ye Yang Luo
Yang Luo