- 1The First Affiliated Hospital of University of Science and Technology of China Anhui Provincial Hospital, Hefei, China
- 2Fuyang Hospital of TCM, Fuyang, Anhui, China
- 3Fuyang Hospital of Anhui Medical University, Fuyang, Anhui, China
- 4GE HealthCare, Shanghai, China
Introduction: We aimed (i) to explore the diagnostic value of deep gray matter magnetic susceptibility in Alzheimer’s disease (AD) in China and (ii) to analyze its correlation with neuropsychiatric scales. Moreover, we conducted subgroup analysis based on the presence of the APOE-ε4 gene to improve the diagnosis of AD.
Methods: From the prospective studies of the China Aging and Neurodegenerative Initiative (CANDI), a total of 93 subjects who could undergo complete quantitative magnetic susceptibility imaging and APOE-ε4 gene detection were selected. Differences in quantitative susceptibility mapping (QSM) values between and within groups, including AD patients, individuals with mild cognitive impairment (MCI), and healthy controls (HCs), both APOE-ε4 carriers and non-carriers, were analyzed.
Results: In primary analysis, the magnetic susceptibility values of the bilateral caudate nucleus and right putamen in the AD group and of the right caudate nucleus in the MCI group were significantly higher than those in the HCs group (P < 0.05). In APOE-ε4 non-carriers, there were significant differences in more regions between the AD, MCI, and HCs groups, such as the left putamen and the right globus pallidus (P < 0.05). In subgroup analysis, the correlation between QSM values in some brain regions and neuropsychiatric scales was even stronger.
Discussion: Exploration of the correlation between deep gray matter iron levels and AD may provide insight into the pathogenesis of AD and facilitate early diagnosis in elderly Chinese. Further subgroup analysis based on the presence of the APOE-ε4 gene may further improve the diagnostic efficiency and sensitivity.
Highlights
– The magnetic susceptibility of caudate nucleus and right putamen can diagnose Alzheimer’s disease.
– Further subgroup analysis revealed more differential brain regions.
– Significantly increased correlation with clinical scales after further subgroup analysis.
1. Introduction
Alzheimer’s disease (AD) is a genetically related neurodegenerative disease that is associated with impaired language, memory, and cognitive function. For many years, the APOE-ε4 gene, which encodes an apolipoprotein, has been considered the most important genetic risk factor for AD pathogenesis. Its presence is highly correlated with AD (Huang et al., 2019; Serrano-Pozo et al., 2021). The association of APOE genes with senile plaques and neurofibrillary tangles has often been reported, but the relationship with brain iron content has not been reported.
Histochemical studies have shown that iron is the most abundant paramagnetic substance in the brain (Hare et al., 2013) and is involved in various brain activities such as neurotransmitter synthesis, oligodendrocyte differentiation, and myelination, as well as changes in mitochondrial function (Hallgren and Sourander, 1958; Cheli et al., 2021). Iron may play an important role in the pathogenesis of AD (Ayton et al., 2020). Excessive iron accumulation can lead to oxidative damage and cell death. Abnormal iron deposits are found in microglia, astrocytes, and senile plaques and around senile plaques and neurofibrillary tangles in AD patients (Connor et al., 1992; Smith et al., 1997; Rao and Adlard, 2018). Abnormally deposited iron will further promote beta-amyloid (Aβ) plaque formation and neurofibrillary tangles and accelerate disease progression (Liu et al., 2011; Teller et al., 2015; Ayton et al., 2017, 2018; Peters et al., 2018). This synergistic phenomenon seems to indicate that abnormal iron levels may have important implications for disease status assessment (van Bergen et al., 2016, 2018; O’Callaghan et al., 2017; Telling et al., 2017; Spotorno et al., 2020). However, Ayton et al. (2017) reported that in patients without Aβ deposition, iron deposition in the frontal lobe and caudate nucleus is associated with a decline in language function, whereas iron deposition in the hippocampus is associated with slightly improved cognitive function. Their study shows that dysregulation of iron content in different regions causes changes in cognitive function even without the effects of Aβ. Clinical experiments have shown that brain iron content intervention has a good alleviating effect on the decline of the self-care ability of AD patients (Crapper McLachlan et al., 1991). Therefore, efficient methods are needed to monitor the relationship between iron levels and AD.
Recently, it has been suggested that iron accumulation may be accurately measured in vivo using quantitative susceptibility mapping (QSM) (Zhu et al., 2009; Li et al., 2014; Liu et al., 2015; Kim et al., 2017; Du et al., 2018), a non-invasive magnetic resonance imaging (MRI) technique capable of inferring local tissue susceptibility secondary to the existence of iron (Langkammer et al., 2012; Zheng et al., 2013; Wang and Liu, 2015; Wang et al., 2017, 2022; Gong et al., 2019). In a longitudinal study, Damulina et al. (2020) found that throughout the brain, only the basal ganglia showed a significant increase in iron levels. White matter is rich in diamagnetic myelin and anisotropic fiber bundles, which can largely counteract the paramagnetic effects of iron. With QSM, the iron content can be better evaluated in deep gray matter than in white matter regions (Langkammer et al., 2012). Autopsy can only reveal final total iron levels, whereas QSM can be used to examine changes in magnetic susceptibility caused by long-term changes in iron levels, which may have important implications for disease prediction and progression. Several studies have only reported differences in iron levels between AD patients and those with mild cognitive impairment (MCI) (Zhu et al., 2009; Moon et al., 2016; Du et al., 2018; Guan et al., 2022; Yang et al., 2022; Kuchcinski et al., 2023). Therefore, the purpose of the present study was to investigate (i) the differences in deep gray matter magnetic susceptibility between APOE-ε4 carriers and non-carriers in Chinese AD patients, MCI individuals, and healthy controls (HCs) and (ii) the correlation between deep gray matter magnetic susceptibility and MMSE and MoCA scores.
2. Materials and methods
2.1. Participants
This study was approved by the Institutional Ethics Committee. This is a retrospective study, from May 2019 to October 2021, subjects who participated in the single center prospective study of the China Aging and Neurodegenerative Initiative (CANDI) (Gao et al., 2022) and could undergo complete quantitative magnetic susceptibility imaging were selected for enrolled. All participants were evaluated by a trained physician with extensive experience in the diagnosis of dementia. Laboratory tests were conducted and the medical history was retrieved. All participants filled in the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment scale (MoCA), and Clinical Dementia Rating Scale (CDR) questionnaires for quick assessment of their cognitive ability. Finally, MRI analysis and APOE genotype determination were performed. The main inclusion criteria were as follows. All subjects were 40–80 years old and had no contraindications for MRI. AD and MCI patients or their families had confirmed cognitive decline. Patients were diagnosed with AD according to the National Institute on Aging Alzheimer’s Association 2011 (NIA-AA 2011) AD dementia core clinical criteria (McKhann et al., 2011). The MCI diagnosis was made based on the Peterson criteria (Petersen et al., 2018). Exclusion criteria for this study include individuals with other types of dementia, a medical history that may cause neurological diseases, previous brain injury or psychiatric disorders, and poor image quality. Additionally, all subjects were enrolled based on a comprehensive evaluation using the A/T/N framework detection system. This framework comprises three components: “A” for Aβ deposition, which can be detected through positron emission tomography (PET) or cerebrospinal fluid (CSF) Aβ42/Aβ40 ratios; “T” for aggregated tau, which can be detected through PET tau or CSF phosphorylated tau; and “N” for neuronal degeneration or injury, which can be detected through 18-fluorodeoxyglucose-PET and structural magnetic resonance imaging (Gao et al., 2022).
A total of 93 subjects were enrolled, comprising 43 AD patients (29 APOE-ε4 carriers and 14 non-carriers), 23 MCI patients (10 APOE-ε4 carriers and 13 non-carriers), and 27 age-matched HCs (4 APOE-ε4 carriers, 22 non-carriers, from which one subject was excluded due to lack of APOE-ε4 gene data in further analysis) with no history of neurological injury.
2.2. MRI and APOE gene detection
The QSM scans were made with a 3.0-T MR750w scanner using a head and neck coil (GE Healthcare, Milwaukee, WI, USA). Earplugs and foam padding were used to reduce scanner noise and head movements. Imaging parameters were as follows: repetition time = 31.4 ms, flip angle = 12°, field of view = 25.6 cm, matrix size = 256 × 256, acceleration factor = 2, number of echoes = 12, first echo time = 2.0 ms, echo time spacing = 2.35 ms, slice number = 136, the total acquisition time = 7 min.
For APOE gene detection, all subjects fasted for>8 h, and 3 ml of venous blood was collected from the cubital vein and placed in dipotassium ethylenediaminetetraacetic anticoagulant tubes at room temperature. The APOE gene was detected within 2 h by PCR.
2.3. Image processing and analysis
Images were processed as previously described (Li et al., 2011). Images were reconstructed referring to the mean susceptibility value of the whole brain based on the Larmor frequency. Then the spherical average method was used to remove the background phase and set the filter radius to 8 (Schweser et al., 2011). The improved Laplacian phase unwrapping method and temporal fitting were used (Li et al., 2011, 2015) and the regularization threshold for Laplace filtering was set to 0.04 to obtain the susceptibility map from the brain tissue frequency map.
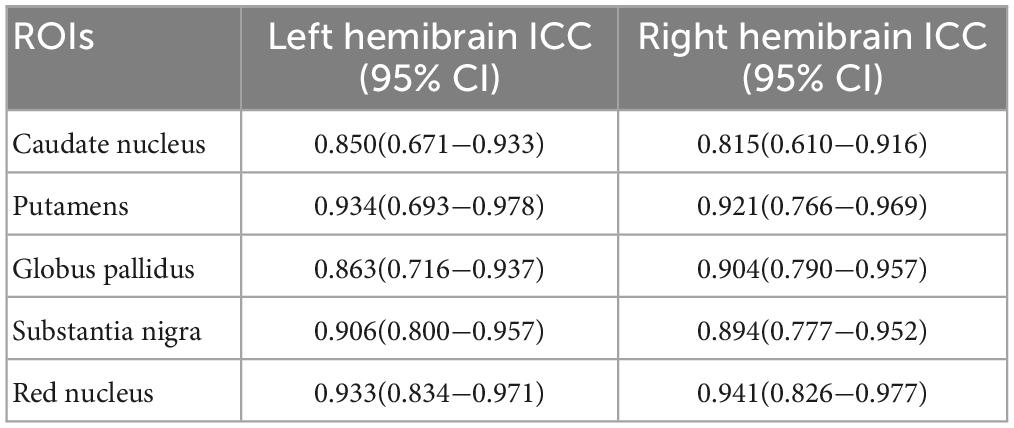
The QSM values for each deep gray matter nucleus were gained from all visible areas. Regions of interest (ROIs) included the bilateral caudate nucleus (CN), putamen (PUT), globus pallidus (GP), substantia nigra (SN), and red nucleus (RN). All ROIs were manually outlined on all consecutive levels using MRIcro software1 by one neuroradiologist who was blinded to the subject group. QSM values were measured again after 2 and 4 weeks, and the average value was taken. To confirm the reliability of the results, 25 subjects were randomly selected from all subjects with post-processed QSM images, and their ROIs were manually outlined on all consecutive levels by another neuroradiologist (>16 years) using the same method.
2.4. Statistical analysis
Data were statistically analyzed using SPSS (SPSS version 22.0, SPSS, Chicago, IL, USA) and GraphPad software (GraphPad Prism version 8.0, GraphPad Software Inc., San Diego, CA, USA). One-way ANOVA was conducted for normally distributed data with homogeneity of variance. The Kruskal–Wallis test was used for non-normally distributed data. We further conducted Bonferroni correction analysis to make comparisons between the AD and HCs, MCI and HCs, and AD and MCI groups. QSM values were compared between the APOE-ε4 carrier and non-carrier subgroups in the AD, MCI, and HCs groups, and between males and females within groups using the independent samples t-test. ROC curve analysis was conducted to evaluate the sensitivity and specificity of the QSM values in the three groups. Between-group gender analysis was conducted using the chi-square test. P < 0.05 was considered statistically significant. Partial correlation analysis of magnetic susceptibility in three groups was performed based on the MMSE and MoCA scores in different brain regions after adjusting for age and gender. Considering the small number of HCs in the APOE-ε4 carrier group, they were excluded from the within group gender analysis and partial correlation analysis.
3. Results
3.1. Clinical data
Interobserver variability was analyzed based on the intraclass correlation coefficient. The results show satisfactory consistency (0.815–0.941) (Table 1).
Ninety-three patients (61.81 ± 8.46, 30 men) were evaluated. The gender ratio (men 13/7/10, women 30/16/17, P = 0.820), age (62.63 ± 8.10, 63.91 ± 7.77, 58.70 ± 8.99, P = 0.077), and educational level (8.98 ± 4.07, 8.91 ± 4.69, 11.04 ± 3.86, P = 0.099) were not significantly different between the three groups. As expected, the MMSE and MoCA scores were ordered as AD < MCI < HCs, and the CDR scores were ordered as AD > MCI > HCs (P < 0.05) (Table 2).
3.2. Comparison of QSM values among three groups
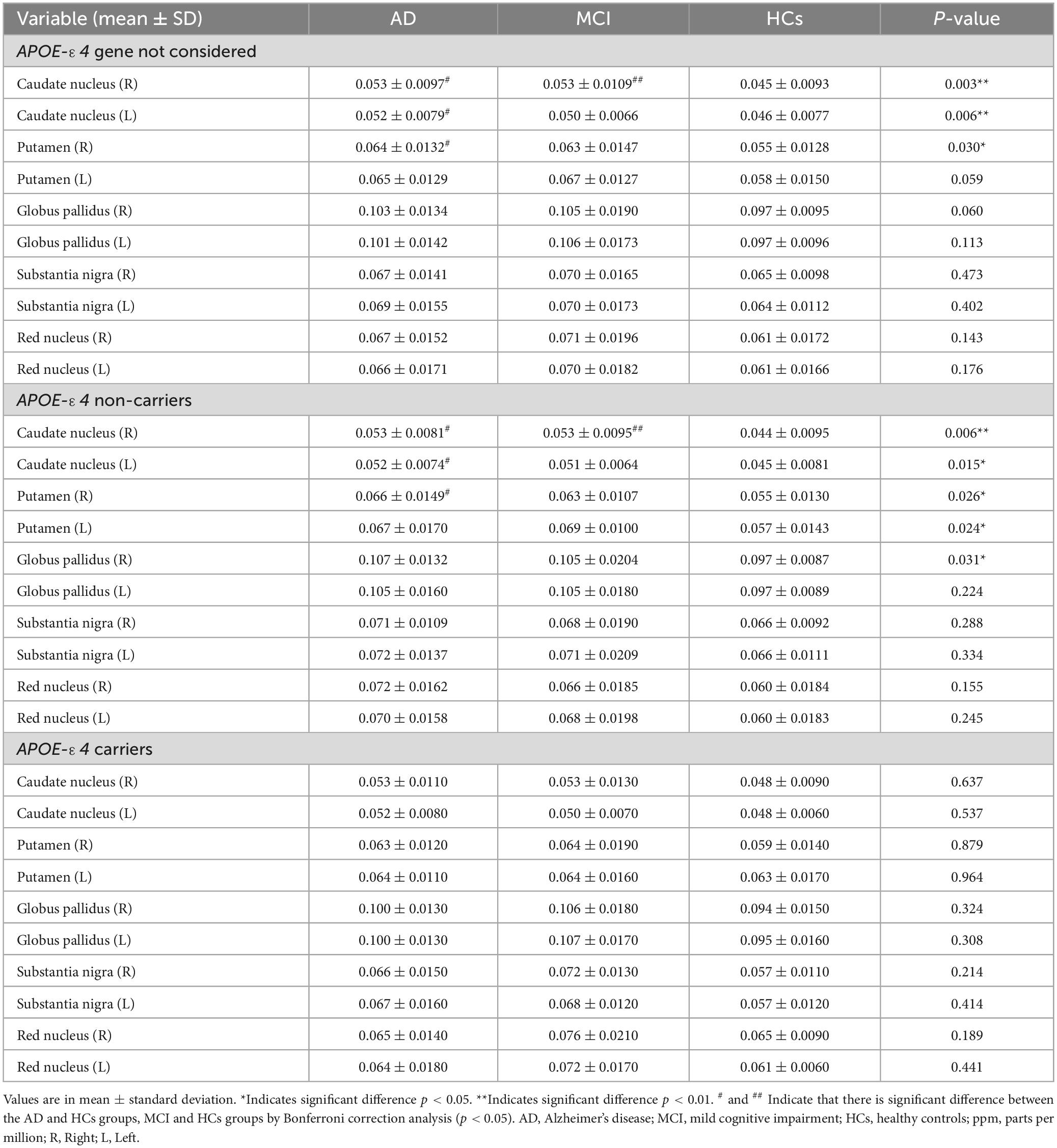
In all subjects, there were statistically significant differences in QSM values of the bilateral caudate nucleus and right putamen between the AD, MCI, and HCs groups (Figure 1A and Table 3). Among APOE-ε4 non-carriers, QSM values in the bilateral caudate nucleus, bilateral putamen, and right globus pallidus were significantly different between the AD, MCI, and HCs groups (Figure 1B and Table 3). No significant difference in QSM values was observed among APOE-ε4 carriers (Figure 1C and Table 3).
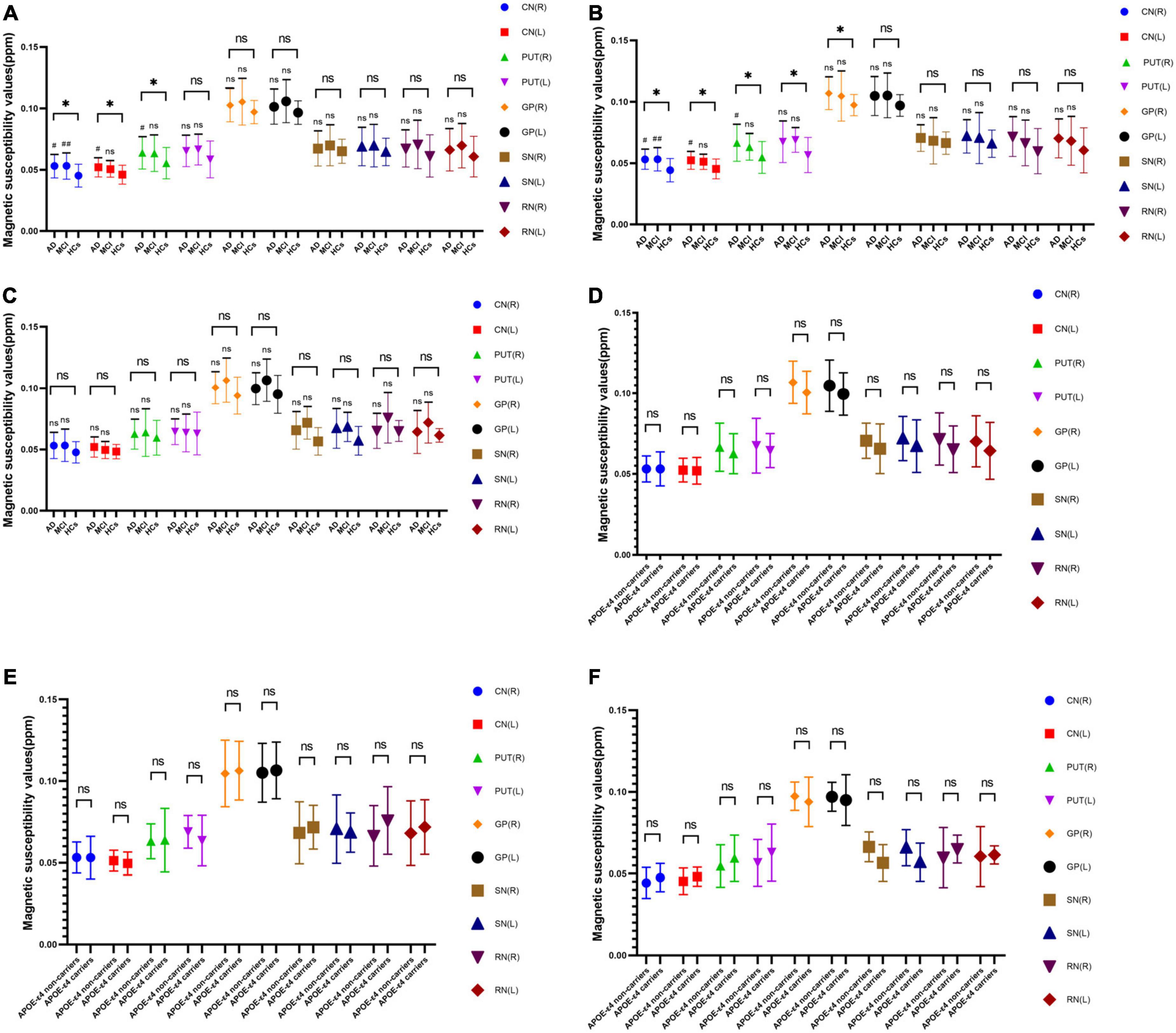
Figure 1. Without APOE-ε4 consideration (A), APOE-ε4 non-carriers (B), and APOE-ε4 carriers (C). Statistical analysis of QSM values of each group. APOE-ε4 gene of AD (D), MCI (E), and HCs (F) groups. Statistical analysis of QSM values between non-carriers and carriers. *Indicates that there is significant difference among the AD, MCI, and HCs groups by one-way ANOVA (p < 0.05). # and ## indicate that there is significant difference between the AD and HCs groups, MCI and HCs groups by Bonferroni Correction Analysis (P < 0.05). AD, Alzheimer’s disease. MCI; mild cognitive impairment; HCs, Healthy controls; ppm, parts per million.
3.3. Comparison of QSM values between two groups
The QSM values of the bilateral caudate and right putamen in the AD group and of the right caudate nucleus in the MCI group were significantly higher than those in the HCs group (Figure 1B and Table 3). Among APOE-ε4 non-carriers, QSM values of the bilateral caudate and right putamen in the AD group and of the right caudate nucleus in the MCI group were significantly higher than those in the HCs group (Figure 1B and Table 3). No significant differences were observed in QSM values between the AD and MCI groups for APOE-ε4 non-carriers or between the AD, MCI, and HCs groups for APOE-ε4 carriers (Figures 1B, C and Table 3).
Within the AD, MCI, and HCs groups, no significant differences in QSM values were observed between APOE-ε4 carriers and non-carriers (Figures 1D–F).
3.4. Comparison of QSM values between genders within groups
Among APOE-ε4 non-carriers, there was a significant gender differences in QSM values of the right pallidus (95% CI: -0.017 to -0.001; P = 0.030) in the HCs group (Figure 2F). Among APOE-ε4 carriers, there were significant gender differences in QSM values of the bilateral putamen (Right; 95% CI: -0.0208 to -0.0021; P = 0.019), (Left; 95% CI: -0.0166 to -0.0002; P = 0.045) in the AD group (Figure 2G) and of the left caudate nucleus (95% CI: 0.0003 to 0.0148; P = 0.044) in the MCI group (Figure 2H). No significant differences were observed in QSM values of different genders between the AD and MCI groups for APOE-ε4 non-carriers or between the AD, MCI, and HCs groups for APOE-ε4 gene not considered (Figures 2A–E).
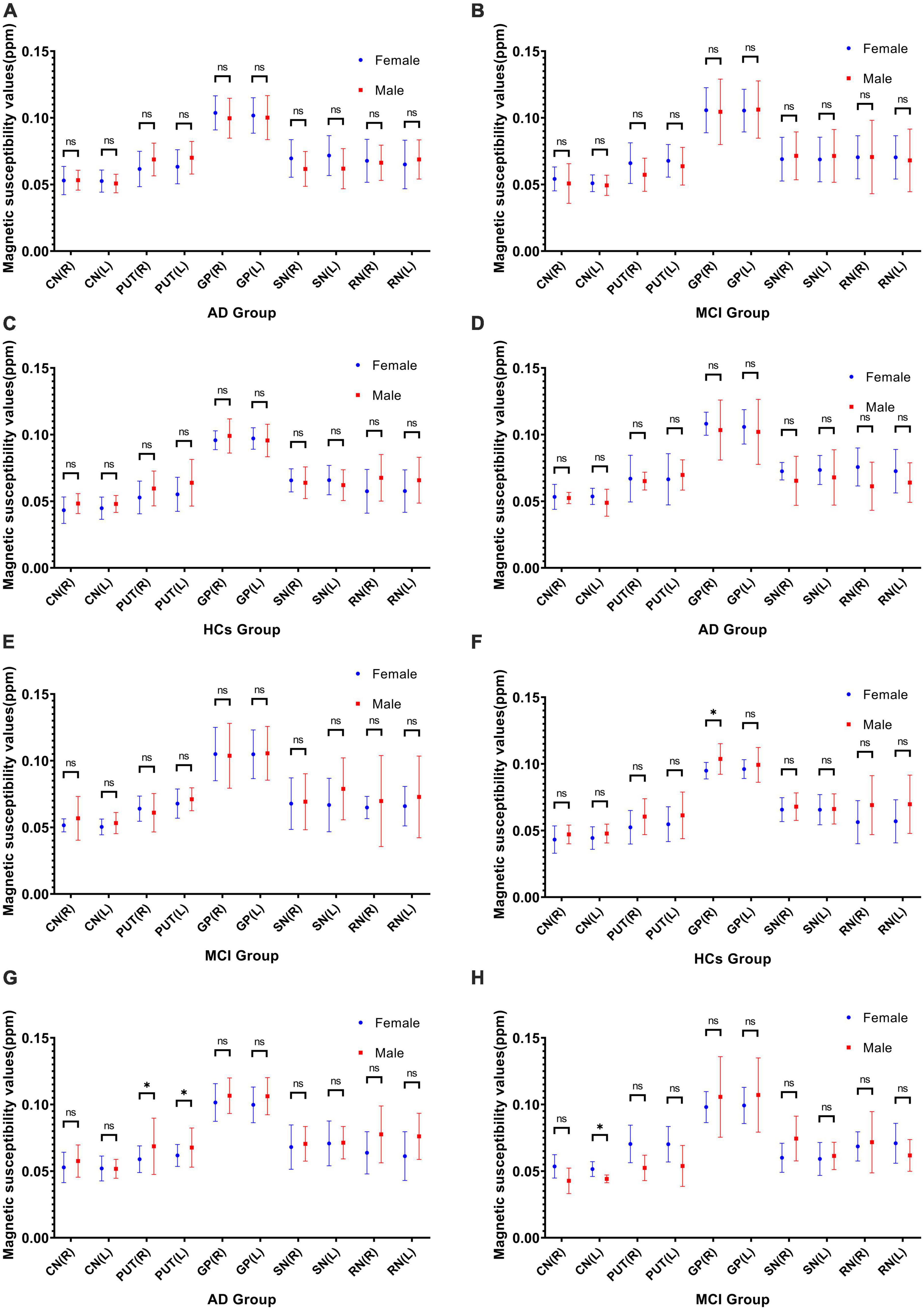
Figure 2. Not considering APOE-ε4 gene comparison of QSM values between genders within three groups: AD (A), MCI (B), and HCs (C). APOE-ε4 non-carriers comparison of QSM values between genders within three groups: AD (D), MCI (E), and HCs (F). APOE-ε4 carriers comparison of QSM values between genders within AD (G) and MCI (H) groups. * Indicates that there is significant difference by independent samples t-test (P < 0.05). CN, caudate nucleus; PUT, putamen; GP, globus pallidus; SN; substantia nigra; RN, red nucleus; R, right; L, left; ppm, parts per million.
3.5. ROC curve analysis
In all subjects, the area under the ROC curve (AUC) values of the bilateral caudate nucleus and the right putamen in the AD group were (Right caudate nucleus; AUC, 0.715; 95% CI: 0.59–0.84; P = 0.003), (Left caudate nucleus; AUC, 0.699; 95% CI: 0.57–0.82; P = 0.005), and (Right putamen; AUC, 0.689; 95% CI: 0.56–0.82; P = 0.008) (Figure 3A), and the AUC value of the right caudate nucleus in the MCI group was (AUC, 0.702; 95% CI: 0.56–0.85; P = 0.015) (Figure 3B). In APOE-ε4 non-carriers, the AUC values of the bilateral caudate nucleus and the right putamen in the AD group were (Right caudate nucleus; AUC, 0.756; 95% CI: 0.60–0.91; P = 0.010), (Left caudate nucleus; AUC, 0.737; 95% CI: 0.57–0.91; P = 0.018), and (Right putamen; AUC, 0.74; 95% CI: 0.56–0.92; P = 0.016) (Figure 3C), and the AUC value of the right caudate nucleus in the MCI group was (AUC, 0.762; 95% CI: 0.60–0.93; P = 0.010) (Figure 3D).
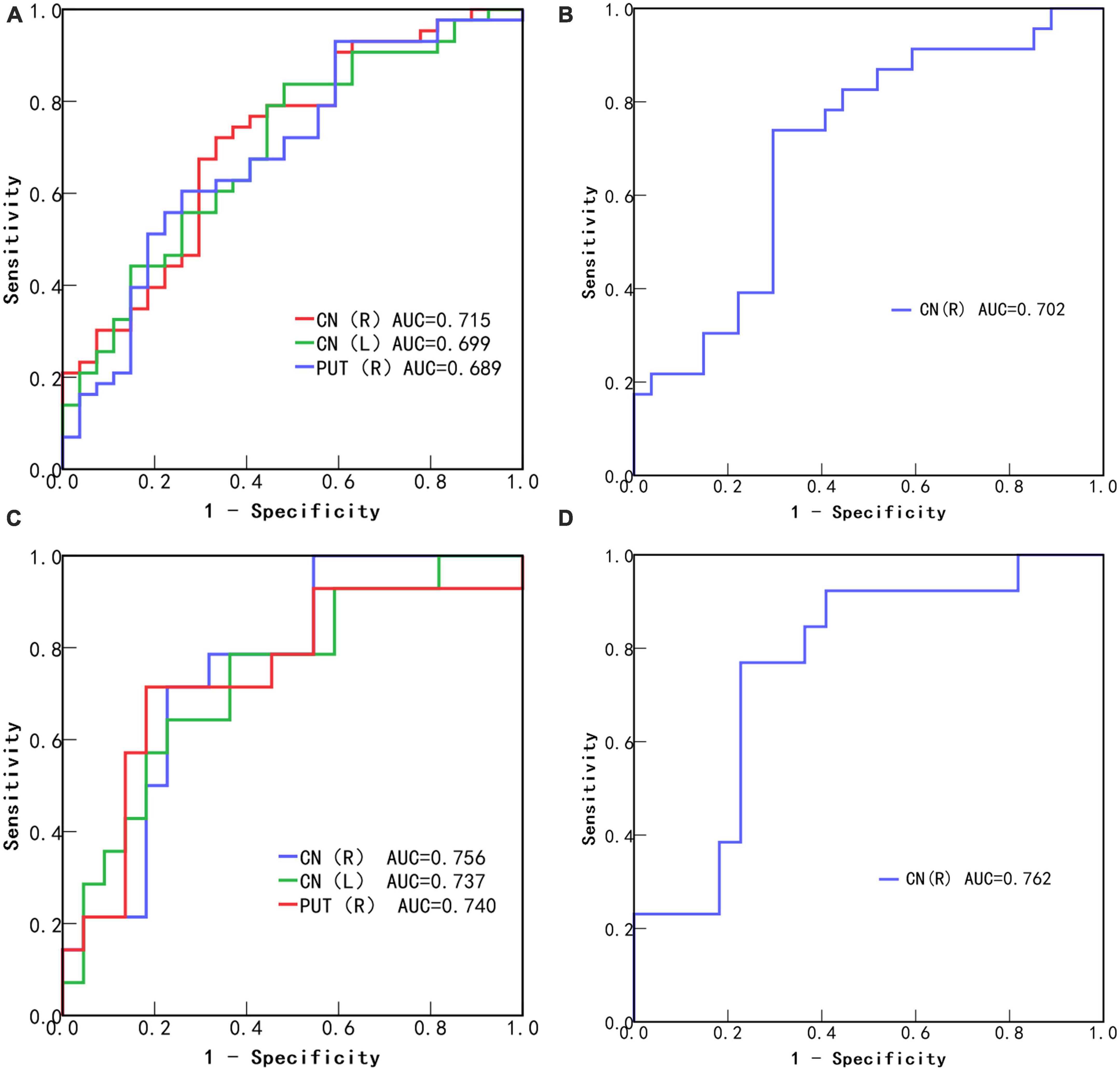
Figure 3. Receiver operating characteristic (ROC) curves of statistically significant brain region QSM values to diagnose Alzheimer’s disease (A) and mild cognitive impairment (B) without considering APOE-ε4. ROC curves of statistically significant brain region QSM values to diagnose Alzheimer’s disease (C) and mild cognitive impairment (D) in APOE-ε4 non-carriers. CN, caudate nucleus; PUT, putamen; R, Right; L, Left.
3.6. Correlation analysis
For all subjects, left red nucleus QSM values in the AD group was negatively correlated with MMSE (r = -0.313, P = 0.046) and MoCA scores (r = -0.356, P = 0.022), and right putamen (r = -0.465, P = 0.019) and right globus pallidus (r = -0.425, P = 0.034) QSM values in HCs groups was negatively correlated with MoCA scores (Figures 4A–D).
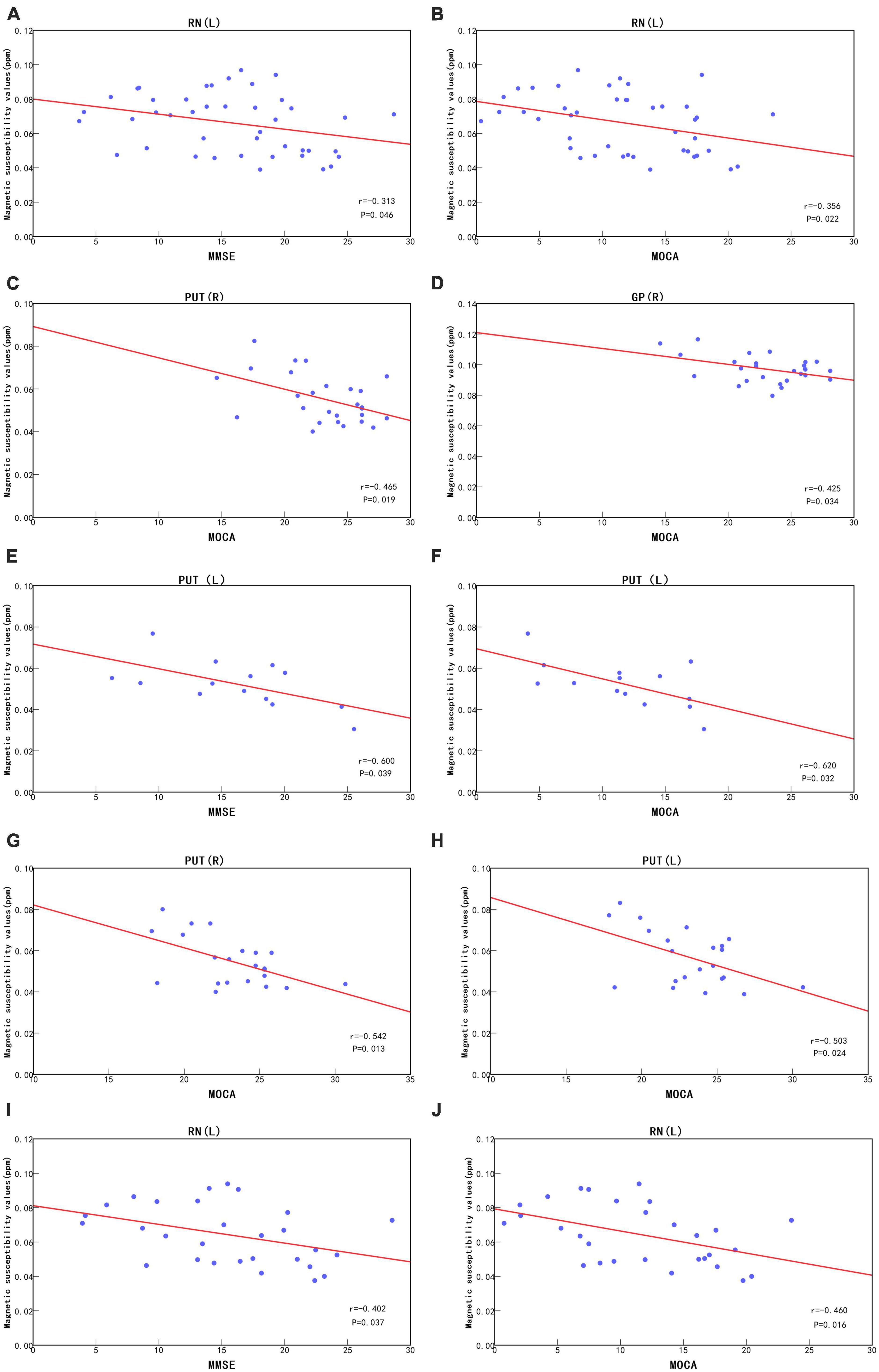
Figure 4. Under no consideration of APOE-ε4, correlation analysis between left red nucleus QSM values and MMSE scores (A) and MOCA scores (B) in the AD group and correlation analysis between right putamen and right globus pallidus QSM values and MOCA scores (C,D) in the HCs group. In APOE-ε4 non-carriers, correlation analysis between left putamen QSM values and MMSE scores (E) and MOCA scores (F) in the AD group and correlation analysis between bilateral putamen QSM values and MOCA scores (G,H) in the HCs group. In APOE-ε4 carriers, correlation analysis between left red nucleus QSM values and MMSE scores (I) and MOCA scores (J) in the AD group. PUT, putamen; RN, red nucleus; GP, globus pallidus; R, Right; L, Left; ppm, parts per million.
In APOE-ε4 non-carriers, QSM values of the left putamen in the AD group were negatively correlated with the MMSE (r = -0.600, P = 0.039) and MoCA scores (r = -0.620, P = 0.032), and QSM values in the bilateral putamen in the HCs group were negatively correlated with MoCA scores (Right, r = -0.542, P = 0.013) (Left, r = -0.503, P = 0.024) (Figures 4E–H). In APOE-ε4 carriers, QSM values of the left red nucleus in the AD group were negatively correlated with the MMSE (r = -0.402, P = 0.037) and MoCA scores (r = -0.460, P = 0.016) (Figures 4I, J). In APOE-ε4 carriers and non-carriers in the MCI group, QSM values were not significantly correlated with the MMSE and MoCA scores (P > 0.05).
4. Discussion
In the present study, we examined the differences in magnetic susceptibility in deep gray matter in the AD, MCI, and HCs groups, including both APOE-ε4 carriers and non-carriers, and their correlation with cognitive performance. Changes in deep gray matter magnetic susceptibility in APOE-ε4 carriers and non-carriers were further investigated in the AD and MCI groups, and its correlation with neuropsychiatric scales was analyzed.
As with previous reports (Bailly et al., 2019; Rajan et al., 2021; Alzheimer’s Association, 2023), the number of female patients in our study was notably higher than that of males. Our findings align with the van der Weerd study (van der Weerd et al., 2022), showing no significant gender differences within the AD, MCI, and HCs groups. It is important to highlight that in further analysis of APOE-ε4 gene subgroups, there were significant differences in QSM values among various brain regions and gender groups. Specifically, in HCs without APOE-ε4, the right pallidus had higher QSM values in males compared to females, while in individuals with AD and APOE-ε4, the bilateral putamen had higher QSM values in males compared to females. Additionally, in individuals with MCI and the APOE-ε4, the left caudate nucleus had higher QSM values in females compared to males. Currently, no other comparable results have been discovered. It remains uncertain whether this outcome is indicative of a more nuanced subgroup analysis or if it is potentially biased due to a smaller sample size. Therefore, additional research is necessary to identify the underlying cause of this result.
We found that the APOE-ε4 gene may have potential effects on iron levels. When the APOE-ε4 gene was not considered, there were significant differences in magnetic susceptibility between the bilateral caudate nucleus and right putamen among the AD, MCI, and HCs groups, consistent with Moon’s discovery of abnormal iron deposition in the caudate and putamen (Moon et al., 2016; Guan et al., 2022). Compared with the HCs group, the QSM values of the bilateral caudate nucleus and the right putamen in the AD group and of the right caudate nucleus in the MCI group were significantly increased. It is worth noting that more brain regions showed an increase in magnetic susceptibility in the AD group than in the MCI group, suggesting that iron levels may gradually increase with disease progression. This is partially consistent with other reported results (Zhu et al., 2009; Du et al., 2018; Guan et al., 2022). In APOE-ε4 non-carriers, we not only found similar results, but we also observed significant differences in QSM values for the left putamen and right pallidus. Whether there are more regions with changes in iron content requires further study. However, the same results were not observed in APOE-ε4 carriers, possibly because of bias caused by the small number of subjects in the HCs group. An increase in brain iron content in multiple regions in AD and MCI patients compared to the HCs group could be observed, although these differences were not statistically significant. Although the QSM values in some brain regions of APOE-ε4 carriers were slightly increased compared with those of APOE-ε4 non-carriers, no statistically significant differences were observed. This contradicts the results reported by Yim that APOE-ε4 carry leads to elevated iron levels (Yim et al., 2022) but is consistent with most of the findings reported by van Berge (van Bergen et al., 2016). A reason for this discrepancy may be that in other studies, only one or a few slices of the ROI were selected, while we selected all consecutive slices of the ROI.
Our data suggest that changes in magnetic susceptibility can be used to distinguish between different groups. The preliminary analysis results showed that, among all subjects, QSM values in the bilateral caudate nucleus and right putamen showed the highest changes in the AD group. More importantly, in the early MCI stage of the disease, the QSM value of the right caudate nucleus showed the strongest changes. Further subgroup analysis based on the presence of the APOE-ε4 gene further improved the diagnostic specificity and diagnostic performance. However, the AUC values obtained did not surpass 0.8, indicating that the diagnostic efficacy of this biomarker may not be optimal. Further studies may require a larger sample size, selection of additional regions of interest, or utilization of multimodal imaging techniques to enhance diagnostic performance. In APOE-ε4 non-carriers, local iron levels were more strongly associated with cognitive changes, providing more clues for the prediction and diagnosis of AD and MCI. We observed significant differences in more brain regions, such as the left putamen and right globus pallidus, between the AD, MCI, and HCs groups in APOE-ε4 non-carriers. However, no differences were observed when the AD and MCI groups were compared with the HCs group, possibly because of the small sample size. Further research is required to expand the sample size.
In all subjects, we observed weak correlations between (i) the QSM values of the left red nucleus in the AD group and the right putamen and right globus pallidus in the HCs group and (ii) the neuropsychiatric scale scores. We observed no significant correlations for other brain regions. This is consistent with the findings of Moon et al. (2016) and Yim et al. (2022). However, Du et al. (2018) reported a correlation between the left caudate nucleus and scale scores in the AD group. AD and MCI patients in the present study had significantly lower MMSE and MoCA scores than in the study by Du et al. (2018), possibly because Du selected mild-to-moderate patients with relatively good cognitive function, whereas cognitive function was relatively poor in the present study. Although QSM values were significantly elevated in the AD and MCI groups, there was no significant correlation between magnetic susceptibility of the caudate nucleus and cognitive scale scores. The basal ganglia play an important role in learning and cognitive processes (Choi et al., 2020), but significant correlations between clinical scales and iron levels in other brain regions have not been observed. This lack of significant correlation could be due to several reasons. First, despite changes in cognitive function (Ayton et al., 2017, 2018), we only used MMSE and MoCA as cognitive impairment assessment criteria, which may not reflect the cognitive status of the patients in detail. Second, factors such as neuroinflammation can also lead to increases in iron levels (Ayton et al., 2020), and a significant increase in iron levels only reflects neurodegeneration, not cognitive decline. Third, even a significant increase in iron levels does not result in cognitive decline. Interestingly, subgroup analysis based on the presence of the APOE-ε4 gene revealed a weak correlation between the QSM value of the left red nucleus and neuropsychiatric scale scores in the AD group only in APOE-ε4 carriers. Among APOE-ε4 non-carriers, there was a strong correlation between (i) QSM values in the left putamen in the AD group and the bilateral putamen in the HCs group and (ii) neuropsychiatric scale scores. Our research has certain limitations. Due to the small sample size of this study, the ROI only included deep gray matter nuclei, so other disease-related ROIs might have been excluded. Moreover, the presence of substances such as copper, zinc, and myelin in the brain may has a certain effect on magnetic susceptibility. We conducted only a horizontal comparative study with a limited sample size, so more data are needed to investigate the relationship between AD progression and magnetic susceptibility.
Although iron levels in AD and MCI patients have been reported, we investigated iron levels in the AD, MCI, and HCs groups based on the presence of the APOE-ε4 gene. Expanding on previous studies, we revealed that the crucial role of identifying MCI specifically in the right caudate nucleus, and the detecting AD in both the bilateral caudate nucleus and the right putamen nucleus is equally critical.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. Requests to access these datasets should be directed to KD, ZGVuZ2tleHVlLWFuaHVpQDE2My5jb20=.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Research Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements. Written informed consent was not obtained from the individual (s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CH, JL, and KD contributed to conception and design of the study. CL, QT, XL, and MR organized the database. CH and YZ performed the statistical analysis. CH and JL wrote the first draft of the manuscript. CL, YZ, QT, XL, and MR wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Acknowledgments
Thanks to YZ from GE for technical support in image post-processing.
Conflict of interest
CH was employed by Fuyang Hospital of TCM, Anhui, China. YZ was employed by company GE HealthCare.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
Aβ, beta-amyloid plaques; AD, Alzheimer’s disease; MCI, mild cognitive impairment; HCs, healthy controls; QSM, quantitative susceptibility mapping; ApoE, apolipoprotein E; MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment Scale; CDR, Clinical Dementia rating Scale.
Footnotes
References
Alzheimer’s Association (2023). 2023 Alzheimer’s disease facts and figures. Alzheimers Dement. 19, 1598–1695. doi: 10.1002/alz.13016
Ayton, S., Diouf, I., Bush, A. I., and Alzheimer’s disease Neuroimaging Initiative. (2018). Evidence that iron accelerates Alzheimer’s pathology: a CSF biomarker study. J. Neurol. Neuro. Psychiatry 89, 456–460. doi: 10.1136/jnnp-2017-316551
Ayton, S., Fazlollahi, A., Bourgeat, P., Raniga, P., Ng, A., Lim, Y. Y., et al. (2017). Cerebral quantitative susceptibility mapping predicts amyloid-β-related cognitive decline. Brain 140, 2112–2119. doi: 10.1093/brain/awx137
Ayton, S., Wang, Y., Diouf, I., Schneider, J. A., Brockman, J., Morris, M. C., et al. (2020). Brain iron is associated with accelerated cognitive decline in people with alzheimer pathology. Mol. Psychiatry 25, 2932–2941. doi: 10.1038/s41380-019-0375-7
Bailly, L., David, R., Chevrier, R., Grebet, J., Moncada, M., Fuch, A., et al. (2019). Alzheimer’s disease: estimating its prevalence rate in a French geographical unit using the national alzheimer data bank and national health insurance information systems. PLoS One 14:e0216221. doi: 10.1371/journal.pone.0216221
Cheli, V. T., Santiago González, D. A., Wan, Q., Denaroso, G., Wan, R., Rosenblum, S. L., et al. (2021). H-ferritin expression in astrocytes is necessary for proper oligodendrocyte development and myelination. Glia 69, 2981–2998. doi: 10.1002/glia.24083
Choi, Y., Shin, E. Y., and Kim, S. (2020). Spatiotemporal dissociation of fMRI activity in the caudate nucleus underlies human de novo motor skill learning. Proc. Natl. Acad. Sci. U.S.A. 117, 23886–23897. doi: 10.1073/pnas.2003963117
Connor, J. R., Menzies, S. L., St Martin, S. M., and Mufson, E. J. (1992). A histochemical study of iron, transferrin, and ferritin in Alzheimer’s diseased brains. J. Neurosci. Res. 31, 75–83. doi: 10.1002/jnr.490310111
Crapper McLachlan, D. R., Dalton, A. J., Kruck, T. P., Bell, M. Y., Smith, W. L., Kalow, W., et al. (1991). Intramuscular desferrioxamine in patients with Alzheimer’s disease. Lancet 337, 1304–1308. doi: 10.1016/0140-6736(91)92978-b
Damulina, A., Pirpamer, L., Soellradl, M., Sackl, M., Tinauer, C., Hofer, E., et al. (2020). Cross-sectional and longitudinal assessment of brain iron level in alzheimer disease using 3-T MRI. Radiology 296, 619–626. doi: 10.1148/radiol.2020192541
Du, L., Zhao, Z., Cui, A., Zhu, Y., Zhang, L., Liu, J., et al. (2018). Increased iron deposition on brain quantitative susceptibility mapping correlates with decreased cognitive function in Alzheimer’s disease. ACS Chem. Neurosci. 9, 1849–1857. doi: 10.1021/acschemneuro.8b00194
Gao, F., Lv, X., Dai, L., Wang, Q., Wang, P., Cheng, Z., et al. (2022). A combination model of AD biomarkers revealed by machine learning precisely predicts Alzheimer’s dementia: China aging and neurodegenerative initiative (CANDI) study. Alzheimer’s Dem. 2022:12700. doi: 10.1002/alz.12700
Gong, N. J., Dibb, R., Bulk, M., van der Weerd, L., and Liu, C. (2019). Imaging beta amyloid aggregation and iron accumulation in Alzheimer’s disease using quantitative susceptibility mapping MRI. Neuroimage 191, 176–185. doi: 10.1016/j.neuroimage.2019.02.019
Guan, X., Guo, T., Zhou, C., Wu, J., Zeng, Q., Li, K., et al. (2022). Altered brain iron depositions from aging to Parkinson’s disease and Alzheimer’s disease: a quantitative susceptibility mapping study. NeuroImage 264:119683. doi: 10.1016/j.neuroimage.2022.119683
Hallgren, B., and Sourander, P. (1958). The effect of age on the non-haemin iron in the human brain. J. Neuro. 3, 41–51. doi: 10.1111/j.1471-4159.1958.tb12607.x
Hare, D., Ayton, S., Bush, A., and Lei, P. (2013). A delicate balance: iron metabolism and diseases of the brain. Front. Aging Neurosci. 5:34. doi: 10.3389/fnagi.2013.00034
Huang, Y. A., Zhou, B., Nabet, A. M., Wernig, M., and Südhof, T. C. (2019). Differential signaling mediated by ApoE2, ApoE3, and ApoE4 in human neurons parallels Alzheimer’s disease risk. J. Neurosci. 39, 7408–7427. doi: 10.1523/JNEUROSCI.2994-18.2019
Kim, H. G., Park, S., Rhee, H. Y., Lee, K. M., Ryu, C. W., Rhee, S. J., et al. (2017). Quantitative susceptibility mapping to evaluate the early stage of Alzheimer’s disease. Neuro. Clin. 16, 429–438. doi: 10.1016/j.nicl.2017.08.019
Kuchcinski, G., Patin, L., Lopes, R., Leroy, M., Delbeuck, X., Rollin-Sillaire, A., et al. (2023). Quantitative susceptibility mapping demonstrates different patterns of iron overload in subtypes of early-onset Alzheimer’s disease. Eur. Radiol. 33, 184–195. doi: 10.1007/s00330-022-09014-9
Langkammer, C., Schweser, F., Krebs, N., Deistung, A., Goessler, W., Scheurer, E., et al. (2012). Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage 62, 1593–1599. doi: 10.1016/j.neuroimage.2012.05.049
Li, W., Wang, N., Yu, F., Han, H., Cao, W., Romero, R., et al. (2015). A method for estimating and removing streaking artifacts in quantitative susceptibility mapping. Neuroimage 108, 111–122. doi: 10.1016/j.neuroimage.2014.12.043
Li, W., Wu, B., and Liu, C. (2011). Quantitative susceptibility mapping of human brain reflects spatial variation in tissue composition. Neuroimage 55, 1645–1656. doi: 10.1016/j.neuroimage.2010.11.088
Li, W., Wu, B., Batrachenko, A., Bancroft-Wu, V., Morey, R. A., Shashi, V., et al. (2014). Differential developmental trajectories of magnetic susceptibility in human brain gray and white matter over the lifespan. Hum. Brain Mapp. 35, 2698–2713. doi: 10.1002/hbm.22360
Liu, B., Moloney, A., Meehan, S., Morris, K., Thomas, S. E., Serpell, L. C., et al. (2011). Iron promotes the toxicity of amyloid beta peptide by impeding its ordered aggregation. J. Biol. Chem. 286, 4248–4256. doi: 10.1074/jbc.M110.158980
Liu, C., Li, W., Tong, K. A., Yeom, K. W., and Kuzminski, S. (2015). Susceptibility-weighted imaging and quantitative susceptibility mapping in the brain. J. Magn. Reson. Imaging 42, 23–41. doi: 10.1002/jmri.24768
McKhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R. Jr., Kawas, C. H., et al. (2011). The diagnosis of dementia due to Alzheimer’s disease: recommendations from the national institute on aging-Alzheimer’s association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dem. 7, 263–269. doi: 10.1016/j.jalz.2011.03.005
Moon, Y., Han, S. H., and Moon, W. J. (2016). Patterns of brain iron accumulation in vascular dementia and Alzheimer’s dementia using quantitative susceptibility mapping imaging. J. Alzheimers Dis. 51, 737–745. doi: 10.3233/JAD-151037
O’Callaghan, J., Holmes, H., Powell, N., Wells, J. A., Ismail, O., Harrison, I. F., et al. (2017). Tissue magnetic susceptibility mapping as a marker of tau pathology in Alzheimer’s disease. Neuroimage 159, 334–345. doi: 10.1016/j.neuroimage.2017.08.003
Peters, D. G., Pollack, A. N., Cheng, K. C., Sun, D., Saido, T., Haaf, M. P., et al. (2018). Dietary lipophilic iron alters amyloidogenesis and microglial morphology in Alzheimer’s disease knock-in APP mice. Metallomics 10, 426–443. doi: 10.1039/c8mt00004b
Petersen, R. C., Lopez, O., Armstrong, M. J., Getchius, T., Ganguli, M., Gloss, D., et al. (2018). Practice guideline update summary: mild cognitive impairment: report of the guideline development, dissemination, and implementation subcommittee of the american academy of neurology. Neurology 90, 126–135. doi: 10.1212/WNL.0000000000004826
Rajan, K. B., Weuve, J., Barnes, L. L., McAninch, E. A., Wilson, R. S., and Evans, D. A. (2021). Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020-2060). Alzheimer’s Dem. J. Alzheimer’s Assoc. 17, 1966–1975. doi: 10.1002/alz.12362
Rao, S. S., and Adlard, P. A. (2018). Untangling tau and iron: exploring the interaction between iron and tau in neurodegeneration. Front. Mol. Neurosci. 11:276. doi: 10.3389/fnmol.2018.00276
Schweser, F., Deistung, A., Lehr, B. W., and Reichenbach, J. R. (2011). Quantitative imaging of intrinsic magnetic tissue properties using MRI signal phase: an approach to in vivo brain iron metabolism? Neuroimage 54, 2789–2807. doi: 10.1016/j.neuroimage.2010.10.070
Serrano-Pozo, A., Das, S., and Hyman, B. T. (2021). APOE and Alzheimer’s disease: advances in genetics, pathophysiology, and therapeutic approaches. Lancet Neurol. 20, 68–80. doi: 10.1016/S1474-4422(20)30412-9
Smith, M. A., Harris, P. L., Sayre, L. M., and Perry, G. (1997). Iron accumulation in alzheimer disease is a source of redox-generated free radicals. Proc. Natl. Acad. Sci. U.S.A. 94, 9866–9868. doi: 10.1073/pnas.94.18.9866
Spotorno, N., Acosta-Cabronero, J., Stomrud, E., Lampinen, B., Strandberg, O. T., van Westen, D., et al. (2020). Relationship between cortical iron and tau aggregation in Alzheimer’s disease. Brain 143, 1341–1349. doi: 10.1093/brain/awaa089
Teller, S., Tahirbegi, I. B., Mir, M., Samitier, J., and Soriano, J. (2015). Magnetite-amyloid-β deteriorates activity and functional organization in an in vitro model for Alzheimer’s disease. Sci. Rep. 5:17261. doi: 10.1038/srep17261
Telling, N. D., Everett, J., Collingwood, J. F., Dobson, J., van der Laan, G., Gallagher, J. J., et al. (2017). Iron biochemistry is correlated with amyloid plaque morphology in an established mouse model of Alzheimer’s disease. Cell Chem. Biol. 24, 1205–1215. doi: 10.1016/j.chembiol.2017.07.014
van Bergen, J. M., Li, X., Hua, J., Schreiner, S. J., Steininger, S. C., Quevenco, F. C., et al. (2016). Colocalization of cerebral iron with amyloid beta in mild cognitive impairment. Sci. Rep. 6:35514. doi: 10.1038/srep35514
van Bergen, J., Li, X., Quevenco, F. C., Gietl, A. F., Treyer, V., Meyer, R., et al. (2018). Simultaneous quantitative susceptibility mapping and flutemetamol-PET suggests local correlation of iron and β-amyloid as an indicator of cognitive performance at high age. Neuroimage 174, 308–316. doi: 10.1016/j.neuroimage.2018.03.021
van der Weerd, L., Lefering, A., Webb, A., Egli, R., and Bossoni, L. (2022). Effects of Alzheimer’s disease and formalin fixation on the different mineralised-iron forms in the human brain. Sci. Rep. 10:16440. doi: 10.1038/s41598-020-73324-5
Wang, C., Martins-Bach, A. B., Alfaro-Almagro, F., Douaud, G., Klein, J. C., Llera, A., et al. (2022). Phenotypic and genetic associations of quantitative magnetic susceptibility in UK biobank brain imaging. Nat. Neurosci. 25, 818–831. doi: 10.1038/s41593-022-01074-w
Wang, Y., and Liu, T. (2015). Quantitative susceptibility mapping (QSM): decoding MRI data for a tissue magnetic biomarker. Magn. Reson. Med. 73, 82–101. doi: 10.1002/mrm.25358
Wang, Y., Spincemaille, P., Liu, Z., Dimov, A., Deh, K., Li, J., et al. (2017). Clinical quantitative susceptibility mapping (QSM): biometal imaging and its emerging roles in patient care. JMRI 46, 951–971. doi: 10.1002/jmri.25693
Yang, A., Du, L., Gao, W., Liu, B., Chen, Y., Wang, Y., et al. (2022). Associations of cortical iron accumulation with cognition and cerebral atrophy in Alzheimer’s disease. Quant Imaging Med. Surg. 12, 4570–4586. doi: 10.21037/qims-22-7
Yim, Y., Choi, J. D., Cho, J. H., Moon, Y., Han, S. H., and Moon, W. J. (2022). Magnetic susceptibility in the deep gray matter may be modulated by apolipoprotein E4 and age with regional predilections: a quantitative susceptibility mapping study. Neuroradiology 64, 1331–1342. doi: 10.1007/s00234-021-02859-9
Zheng, W., Nichol, H., Liu, S., Cheng, Y. C., and Haacke, E. M. (2013). Measuring iron in the brain using quantitative susceptibility mapping and X-ray fluorescence imaging. Neuroimage 78, 68–74. doi: 10.1016/j.neuroimage.2013.04.022
Keywords: Alzheimer’s disease, mild cognitive impairment, quantitative susceptibility mapping, APOE, MRI
Citation: Huang C, Li J, Liu C, Zhang Y, Tang Q, Lv X, Ruan M and Deng K (2023) Investigation of brain iron levels in Chinese patients with Alzheimer’s disease. Front. Aging Neurosci. 15:1168845. doi: 10.3389/fnagi.2023.1168845
Received: 18 February 2023; Accepted: 05 May 2023;
Published: 22 May 2023.
Edited by:
Gang Wang, Shanghai Jiao Tong University, ChinaReviewed by:
Liangdong Zhou, Cornell University, United StatesYafu Yin, Shanghai Jiao Tong University School of Medicine, China
Copyright © 2023 Huang, Li, Liu, Zhang, Tang, Lv, Ruan and Deng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kexue Deng, ZGVuZ2tleHVlLWFuaHVpQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Chuanbin Huang
Chuanbin Huang Jing Li3†
Jing Li3† Qiqiang Tang
Qiqiang Tang