
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Aging Neurosci. , 29 June 2023
Sec. Neurocognitive Aging and Behavior
Volume 15 - 2023 | https://doi.org/10.3389/fnagi.2023.1148048
This article is part of the Research Topic Two for the Price of One - Effects and Underlying Mechanisms of Combined Motor-Cognitive Interventions on the Body and the Brain, Volume II View all 4 articles
 Huanying Yang1†
Huanying Yang1† Xiangfu Wang2*†
Xiangfu Wang2*† Xuetao Wang1
Xuetao Wang1 Jianxia Yang1
Jianxia Yang1 Wanqian Zhang2
Wanqian Zhang2 Yanfang Ding1
Yanfang Ding1 Tingrui Sang1
Tingrui Sang1 Weiguo Chen2
Weiguo Chen2 Wanhong Wang3
Wanhong Wang3Background/objectives: Although mindfulness-based mind-body therapy (MBMBT) is an effective non-surgical treatment for patients with non-specific low back pain (NLBP), the best MBMBT mode of treatment for NLBP patients has not been identified. Therefore, a network meta-analysis (NMA) was conducted to compare the effects of different MBMBTs in the treatment of NLBP patients.
Methods: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases were searched for randomized controlled trials (RCTs) applying MBMBT for the treatment of NLBP patients, with all of the searches ranging from the time of database creation to January 2023. After 2 researchers independently screened the literature, extracted information, and evaluated the risks of biases in the included studies, the data were analyzed by using Stata 16.0 software.
Results: A total of 46 RCTs were included, including 3,886 NLBP patients and 9 MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance). The results of the NMA showed that Craniosacral Therapy [surface under the cumulative ranking (SUCRA): 99.2 and 99.5%] ranked the highest in terms of improving pain and disability, followed by Other Manipulations (SUCRA: 80.6 and 90.8%) and Pilates (SUCRA: 54.5 and 71.2%). In terms of improving physical health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Pilates (SUCRA: 72.3%) and Meditation (SUCRA: 55.9%). In terms of improving mental health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Meditation (SUCRA: 70.7%) and Pilates (SUCRA: 63.2%). However, in terms of improving pain, physical health, and mental health, Usual Care (SUCRA: 7.0, 14.2, and 11.8%, respectively) ranked lowest. Moreover, in terms of improving disability, Dance (SUCRA: 11.3%) ranked lowest.
Conclusion: This NMA shows that Craniosacral Therapy may be the most effective MBMBT in treating NLBP patients and deserves to be promoted for clinical use.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/, PROSPERO [CRD42023389369].
Low back pain is a major public health problem in modern society and one of the common symptoms in orthopedics and rehabilitation medicine. According to current surveys (Deyo and Bass, 1989), low back pain is one of the most common prevalent symptoms, and its attendance rate is second only to upper respiratory tract disorders. Globally, ~80% of the population will experience low back pain at least once in their lifetime, with a prevalence rate of 7.3%; in addition, ~6.3–15.3% of the population will develop this condition for the first time each year (Hartvigsen et al., 2018; Knezevic et al., 2021). According to surveys (Clark and Horton, 2018), people aged 40–69 years have the highest probability of suffering from low back pain, and its occurrence is gradually being observed at younger ages, with a prevalence of ~1–6% in children aged 7–10 years and ~18% in adolescents aged 11–19 years. The annual socioeconomic losses due to low back pain in the United States exceed $100 billion, with indirect losses in lost wages and decreased productivity accounting for two-thirds of these losses (Katz et al., 2006). An epidemiological survey of 195 countries worldwide showed that (James et al., 2018) years lived with disability in low back pain was the highest of all diseases, and it severely affects the physical and mental health and work capacity of patients, while also becoming the leading cause of productivity loss. In contrast, non-specific low back pain (NLBP) is the most common low back pain, accounting for ~90% of cases (Hartvigsen et al., 2018). NLBP is defined as low back pain produced by non-pathological anatomical factors other than specific low back pain (such as lumbar spinal stenosis, lumbar fracture, lumbar spine slippage, lumbar spine deformity, lumbar spine infection, malignancy, cauda equina syndrome, rheumatoid arthritis, neurogenic diseases and metabolic diseases, among other factors), which cannot be clinically determined in the etiology. The probability of recurrence in NLBP patients within 1 year is ~33% (Gatchel et al., 1995; Itz et al., 2013; da Silva et al., 2017), and NLBP has become a salient condition threatening human health.
Although there is currently no complete cure for NLBP, only some methods can be used to relieve the symptoms to a certain extent; however, the symptoms of most NLBP patients are fortunately mild and self-limited and can have a good effect through non-surgical treatment (Hlaing et al., 2021). Non-surgical treatment of NLBP mainly includes anti-inflammatory and analgesic drugs, acupuncture, traction, manual therapy, exercise and interventional therapies. Among these methods, oral anti-inflammatory and analgesic drugs are currently the most common choice to relieve NLBP; however, this method not only causes side effects such as bone loss, depression and gastric pain but also creates drug resistance with long-term use (Bishop and Wing, 2003; Maher et al., 2017). Coupled with the particularity of the disease, NLBP patients suffer from both physical pain and disability and also psychological pressure from personal, family and social aspects during the treatment period, which leads to an increased physical and mental burden on patients and seriously affects their quality of life and disease regression. Therefore, it is urgent to adopt a safe, effective, and feasible method to alleviate the symptoms and maintain the physical and mental health of NLBP patients.
There is consensus in current guidelines that the treatment of NLBP should focus on non-surgical therapy and psychosocial interventions (Bernstein et al., 2017; Qaseem et al., 2017; Stochkendahl et al., 2018). Mindfulness-based mind-body therapy (MBMBT) is an approach that emphasizes the curing of both mind and body. Mindfulness is utilized to make individuals actively aware of what they are doing at the moment, such as breathing, walking and reading, after which they can accept their feelings, look at everyone and everything around them with a new attitude, and finally return to the tranquility of the mind to find the balance between themselves and the surrounding environment (Green and Kinchen, 2021). Mind-body therapy emphasizes the interplay among the brain, mind, body, and behavior, with the intent to use the mind to affect physical functioning and to promote health (Dossett et al., 2020). Based on this connection, MBMBT utilizes mindfulness as its skeleton and specific mind-body therapies as its flesh and blood. Specifically, this concept allows individuals to listen to their own voice through current actions, thoughts, and words to change automatized behavior patterns and to heal the body's pain while enhancing the power of the mind (Fogaça et al., 2021). In recent years, the application of mindfulness-based mind-body therapy to improve the quality of life of pain patients has gradually become a research hotspot and has been widely considered and recognized by the international medical community.
Numerous studies have shown that (Okafor et al., 2012; Vohra et al., 2016; Kumar et al., 2017; Haller et al., 2019; Shi et al., 2022) Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance use mindfulness as the backbone of the therapy, both of which combine mental relaxation and physical therapy, which can effectively improve the pain and quality of life of patients with pain, as well as promote psychological wellbeing. Moreover, they are effective treatments for patients with NLBP. However, for MBMBT, different treatment modalities have different characteristics and produce different effects on NLBP patients. Lee et al. (2009) considered Qigong as an effective pain management modality; however, the difference is that (Blodt et al., 2015) observed that other exercise therapies reduced pain and dysfunction more than Qigong in 114 NLBP patients. Compared with Qigong, Yoga is also an easy-to-implement MBMBT. Nambi et al. (2014) demonstrated that Yoga better improved pain than other exercises in NLBP patients through a 12-month randomized controlled trial. Based on the trials of Nambi et al. (2014) and Blodt et al. (2015), Yoga should be superior to Qigong in the treatment of NLBP patients. However, Teut et al. (2016) directly compared the effectiveness of pranayama and Yoga in treating NLBP patients and found that pranayama was superior to Yoga in improving pain and mental health.
Although a large number of clinical trials have confirmed the advantages of MBMBT in treating NLBP patients, the findings of different studies have exhibited significant differences (de Freitas et al., 2020). To date, no research has conducted a systematic evidence-based medical study on this topic. Therefore, there is an immediate need to identify an optimal modality in MBMBT to improve the symptoms associated with NLBP patients. A network meta-analysis (NMA) can subsequently directly and indirectly compare the efficacy of multiple interventions, synthesize the pros and cons of multiple interventions, and rank the effectiveness of multiple treatments to select the most suitable clinical treatment option for the patient. Based on this scenario, this paper performed an NMA on randomized controlled trials (RCTs) of different MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance) for NLBP patients to compare the effectiveness of nine approaches in improving pain, disability, and the physical and mental health of NLBP patients and to select the optimal MBMBT, which contributes to a better understanding of the effectiveness of MBMBT for patients and clinicians.
This NMA has been successfully registered with PROSPERO (ID: CRD42023389369) and was performed in strict compliance with the Cochrane Handbook (Cumpston et al., 2019) and the PRISMA-NMA statement (Hutton et al., 2015).
The researchers of this review searched the PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases for relevant literature from inception to January 2023 to identify RCTs of MBMBT for NLBP patients. The full search strategy is available in Table 1 (using PubMed as an example). Additionally, lists of references of relevant systematic reviews and meta-analyses were checked.
The inclusion criteria were framed according to the PICOS strategy. (P) Population: people over 18 years of age with NLBP; (I) Intervention: different MBMBT as a categorized intervention (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Qigong, Tai Chi or Dance); (C) Comparator: control participants with only usual care and appropriate rehabilitation measures being used; (O) Outcomes: self-reported outcomes in people with NLBP (including at least one of the following outcomes of interest: pain, disability, physical health or mental health); and (S) Study type: RCTs.
The following exclusion criteria were used. (1) Studies with duplicate publications; (2) studies with incomplete data; and (3) studies from non-RCTs (including protocols, animal studies, conference abstracts, correspondences, case reports, or quasirandomized controlled trials).
All of the search results were managed by using the literature management software Endnote 20. First, duplicates were excluded by using Endnote 20, after which Ding and Sang read the titles and abstracts of the literature to independently perform an initial screening of the literature based on the inclusion and exclusion criteria. Afterwards, they further read the full text for rescreening to determine inclusion or not. Finally, Wang synthesized the remaining literature and adjudicated all of the disagreements.
In this study, the data extraction were classified into the following six categories: (1) author's name, (2) year of publication, (3) place, (4) sample features (size, age, and sex), (5) intervention measures, and (6) outcomes. All of the abovementioned data extractions were independently completed by Ding and Chen, and all disagreements were adjudicated by Wang.
Although the assessment methods in each extracted outcome measure in this NMA are not consistent, they all belong to the most commonly used and recognized methods of NLBP assessment in the medical community. Pain measures were extracted from the results of the visual analog scale (VAS), Numerical Pain Intensity Scale (NPRS), McGill Pain Questionnaire (MPQ), and brief pain inventory (BPI). In addition, disability measures were extracted from the results of the Oswestry Disability Index (ODI), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire (RMDQ). Both physical and mental health measures were extracted from the results of the SF-36 and SF-12.
Sang and Chen independently evaluated the risk of bias in the included literature in this study according to the Cochrane Risk of Bias Tool in the Cochrane handbook (Sterne et al., 2019). The following seven domains of risk of bias were analyzed: (1) randomized sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective outcome reporting, and (7) other sources of bias. The risk of bias in each domain was categorized into three levels: low risk, high risk, and unclear risk. All disagreements were adjudicated by Wang.
In all of the included literature, variables were continuous, and the extracted outcome data included the postintervention mean and standard deviation, which were converted to means and standard deviations before inclusion when the data were expressed in other forms in the literature. Standardized mean differences (SMDs) and their 95% confidence intervals (CIs) were calculated and analyzed for all of the extracted data. Accounting for the potential differences between different types of literature, this NMA used a random-effects model for analysis rather than a fixed-effects model.
First, a network map of direct comparisons between different interventions was drawn by using Stata software (version 16.0). Each node in the map represents an intervention, and the size of the node indicates the sample size receiving the intervention. The presence of a line between two nodes indicates that they have a direct comparison relationship, and a thicker line indicates a higher number of comparisons. Subsequently, the agreement between direct and indirect comparisons was assessed via the node-splitting method and was considered good if P > 0.05.
Additionally, the effects of various interventions were quantitatively analyzed by using the surface under the cumulative ranking (SUCRA) to rank the effects of different interventions. SUCRA values range from 0 to 100%, and if the SUCRA value for an intervention is closer to 100%, it indicates that the intervention is more effective. However, this conclusion should be interpreted with caution if there is not a clinically meaningful difference between the two interventions. Finally, network funnel plots were drawn and visually checked by using the symmetry criterion to determine if there was a possibility of bias leading to NMA publication.
A total of 3,137 relevant types of literature were obtained from the initial search of the four databases. In the initial search results, 1,009 duplicates were first excluded by using Endnote 20. A total of 1,293 articles were eliminated by the initial reading of the titles and abstracts. Subsequently, a further full-text analysis of the literature according to inclusion and exclusion criteria excluded 64 studies, including non-RCTs (n = 21), incomplete data (n = 13), articles in meeting outcomes that were included in this review (n = 4), and non-meeting interventions included in this review (n = 26). The final 46 pieces of literature were obtained (Figure 1). Detailed search results for different databases are shown in Supplementary Table 1.
The quality assessment of the included studies is shown in Figures 2, 3. Thirty-six studies reported of specific random sequence generation methods, and 10 studies did not specify specific random sequence generation methods. Twenty-four studies reported of specific allocation concealment methods, one study in which the principal investigator was involved in random allocation, and 21 studies in which the specific allocation concealment method was unclear. In addition, 10 studies were blinded to participants and study personnel, nine studies were not blinded to study personnel, two studies were not blinded to participants, and there were 25 studies in which participants and researchers were not specifically blinded. Nine studies blinded outcome raters, three studies did not blind outcome raters, and 34 studies did not specify whether outcome raters were blinded. Moreover, 21 studies did not report incomplete outcome data, and 25 publications were lost to follow-up; however, only two studies provided a clear explanation of the specific reasons for loss to follow-up. Selectivity was not reported in any literature.
A total of 46 RCTs involving 3,886 NLBP patients were included in this review. The interventions in the trial group included Yoga (Williams et al., 2005, 2009; Saper et al., 2009, 2017; Cox et al., 2010; Sherman et al., 2011; Nambi et al., 2014; Telles et al., 2016; Groessl et al., 2017; Michalsen et al., 2021) (10 studies), Ayurvedic massage (Kumar et al., 2017) (one study), Pilates (Gladwell et al., 2006; Wajswelner et al., 2012; Miyamoto et al., 2013, 2018; Mostagi et al., 2015; Natour et al., 2015; Kofotolis et al., 2016; Patti et al., 2016; Hasanpour-Dehkordi et al., 2017; Kliziene et al., 2017; Valenza et al., 2017; Cruz-Díaz et al., 2018; Mazloum et al., 2018; Batibay et al., 2021; Siddique et al., 2021; Ravindran et al., 2022) (16 studies), cranio-sacral therapy (Bialoszewski et al., 2014; Castro-Sánchez et al., 2016; Ghasemi et al., 2020, 2021) (four studies), Meditation (Morone et al., 2008, 2009; Banth and Ardebil, 2015; Michalsen et al., 2016; Zgierska et al., 2016) (five studies), Meditation + Yoga (Cherkin et al., 2016; Turner et al., 2016; Chen et al., 2023) (three studies), Qigong (Blodt et al., 2015; Teut et al., 2016; Phattharasupharerk et al., 2019) (three studies), Tai Chi (Hall et al., 2011; Weifen et al., 2013; Liu et al., 2019) (three studies), and Dance (Okafor et al., 2012) (one study). There were three control groups to compare (including Usual Care, Other Exercises, and Other Manipulation). The characteristics of the included literature are shown in Table 2.
The NMA map is shown in Figures 4A–D.
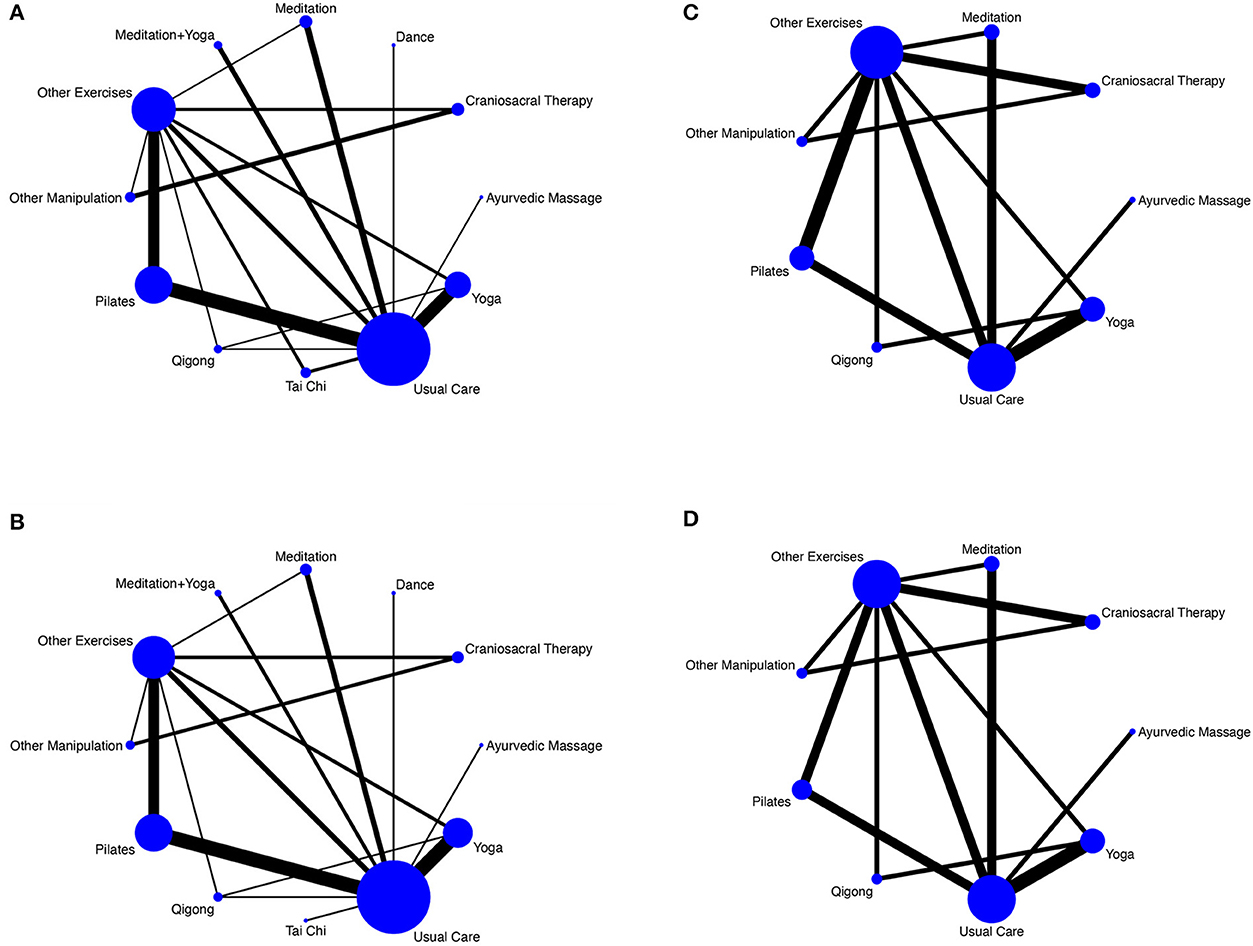
Figure 4. (A) NMA figure for pain. (B) NMA figure for disability. (C) NMA figure for physical health. (D) NMA figure for mental health.
A total of 44 studies reported of pain, including 12 interventions and 3,411 participants. The results of the NMA showed that compared with Usual Care, Craniosacral Therapy [SMD = −4.59, 95% CI = (−6.76 to −2.42)], Other Manipulation [SMD = −2.74, 95% CI = (−5.06 to −0.42)], Pilates [SMD = −1.30, 95% CI = (−2.08 to −0.51)], and Yoga [SMD = −1.02, 95% CI = (−1.89 to −0.14)] were all superior to Usual Care in improving pain. Details are shown in Table 3A. There was no significant inconsistency in the results of the node-splitting method for most of the comparisons (P > 0.05), thus suggesting good agreement between direct and indirect comparisons for most of the studies. The details of this analysis are shown in Supplementary Table 2A. The results of the SUCRA ranking of different interventions in terms of improving pain were Craniosacral Therapy (99.2%) > Other Manipulations (80.6%) > Pilates (54.5%) > Qigong (54.1%) > Tai Chi (53.7%) > Meditation + Yoga (50.6%) > Dance (48.6%) > Ayurvedic Massage (44.2%) > Yoga (43.1%) > Meditation (42.1%) > Other Exercises (22.4%) > Usual Care (7.0%). The details of this ranking are shown in Figure 5A.
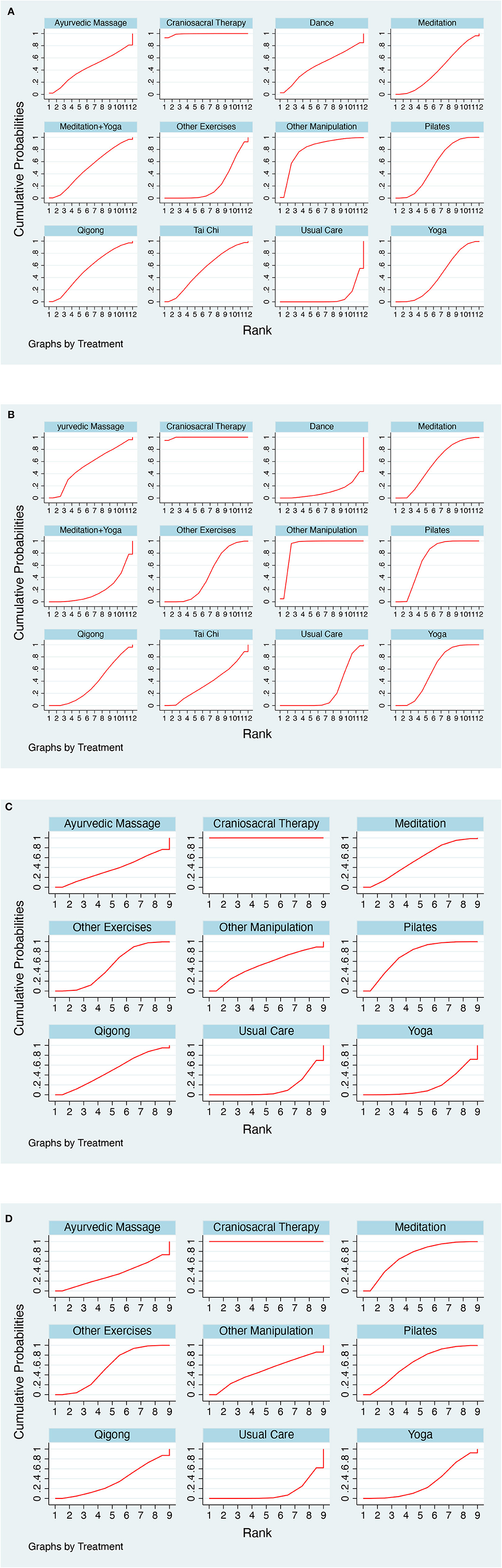
Figure 5. (A) SUCRA plot for pain. (B) SUCRA plot for disability. (C) SUCRA plot for physical health. (D) SUCRA plot for mental health.
A total of 36 studies reported of disability, including 12 interventions and 2,921 participants. The results of the NMA showed that Usual Care was worse than Craniosacral Therapy [SMD = 4.47, 95% CI = (2.81–6.13)] and Other Manipulation [SMD = 3.34, 95% CI = (1.51–5.17)] in improving disability. The details are shown in Table 3A. There were no significant inconsistencies in any of the comparisons in the results of the node-splitting method (P > 0.05), thus suggesting good agreement between direct and indirect comparisons for all the studies. The details are shown in Supplementary Table 2B. The results of the SUCRA ranking of different interventions in terms of improving disability were Craniosacral Therapy (99.5%) > Other Manipulation (90.8%) > Pilates (71.2%) > Yoga (57.7%) > Meditation (56.1%) > Ayurvedic Massage (53.6%) > Other Exercises (43.7%) > Tai Chi (36.8%) > Qigong (36.6%) > Usual Care (24.0%) > Meditation + Yoga (18.6%) > Dance (11.3%). The details of this ranking are shown in Figure 5B.
A total of 15 studies reported on physical health, including nine interventions and 1,269 participants. The results of the NMA showed that compared with Usual Care, only cranio-sacral therapy [SMD = 4.27, 95% CI = (2.70–5.84)] was better than Usual Care in improving physical health. The details of this analysis are shown in Table 3B. There were no significant inconsistencies in any of the comparisons in the results of the node-splitting method (P > 0.05), thus suggesting good agreement between direct and indirect comparisons for all of the studies. The details are shown in Supplementary Table 2C. The results of the SUCRA ranking of different interventions in terms of improving disability were Craniosacral Therapy (100.0%) > Pilates (72.3%) > Meditation (55.9%) > Other Manipulation (52.9%) > Other Exercises (50.5%) > Qigong (48.6%) > Ayurvedic Massage (37.7%) > Yoga (18.0%) > Usual Care (14.2%). The details of this ranking are shown in Figure 5C.
A total of 14 studies reported of physical health, including nine interventions and 1,216 participants. The results of the NMA showed that Usual Care was worse in improving mental health than the following treatments: Craniosacral Therapy [SMD = −3.62, 95% CI = (−4.70 to −2.54)], Pilates [SMD = −0.70, 95% CI = (−1.31 to −0.09)], Meditation [SMD = −0.83, 95% CI = (−1.47 to −0.19)], and Other Exercises [SMD = −0.59, 95% CI = (−1.11 to −0.07)]. The details are shown in Table 3B. There were no significant inconsistencies in any of the comparisons in the results of the node-splitting method (P > 0.05), thus suggesting good agreement between direct and indirect comparisons for all of the studies. The details are shown in Supplementary Table 2D. The results of the SUCRA ranking of different interventions in terms of improving disability were Craniosacral Therapy (100.0%) > Meditation (70.7%) > Pilates (63.2%) > Other Exercises (55.9%) > Other Manipulation (48.9%) > Qigong (36.0%) > Ayurvedic Massage (32.5%) > Yoga (31.0%) > Usual Care (11.8%). The details of this ranking are shown in Figure 5D.
Funnel plots for all of the outcome indicators showed that most studies were evenly distributed on both sides of the red centerline, thus suggesting that publication bias is less likely to exist in this review. Details are shown in Figure 6.
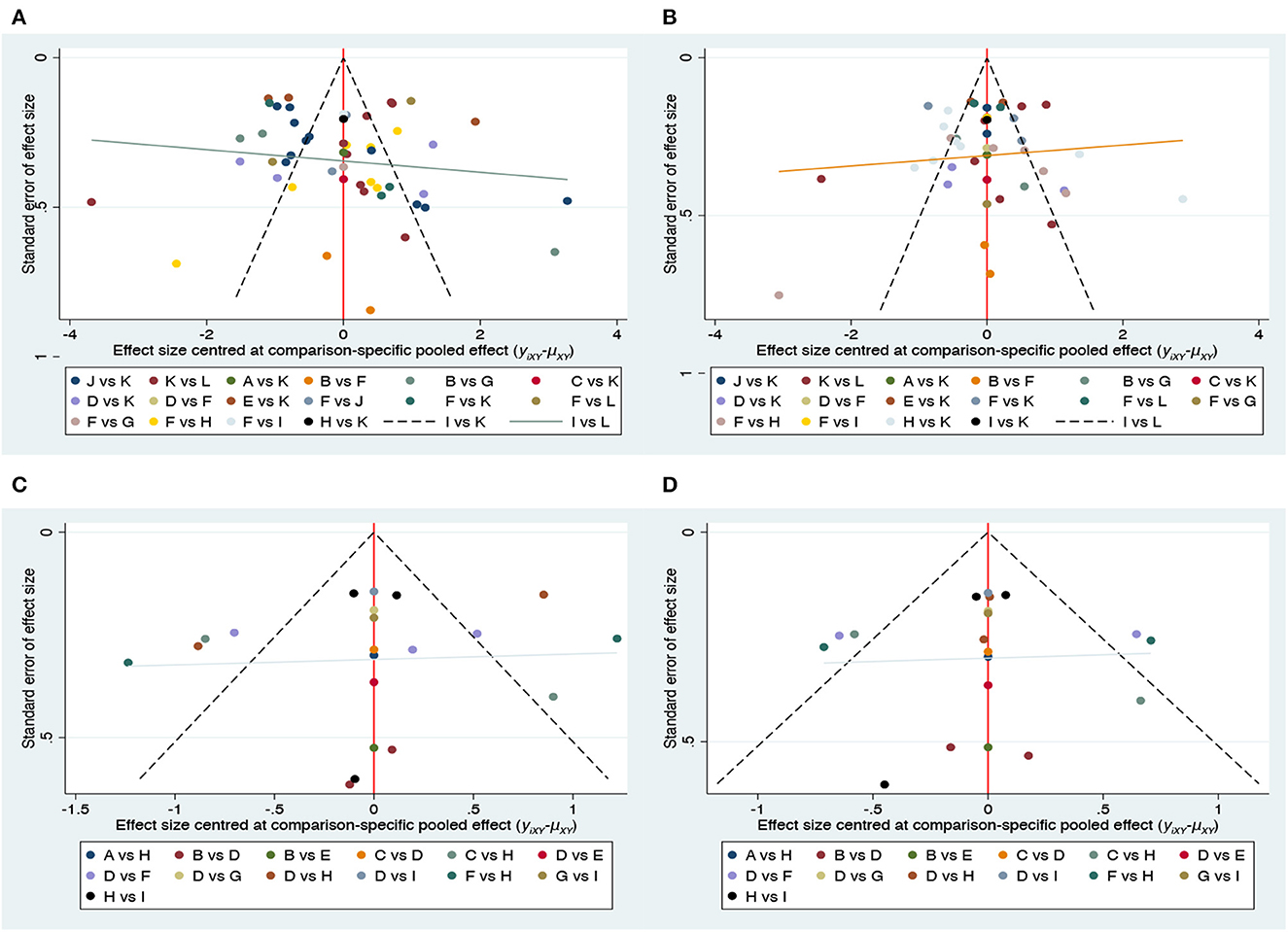
Figure 6. Funnel plot on publication bias. (A) Pain; (B) disability; (C) physical health; (D) mental health.
To identify the best model of MBMBT for NLBP patients, this NMA is the first to compare the effectiveness of nine different therapeutic interventions in improving patients' pain, disability, physical health, and mental health based on RCTs of 3,886 NLBP patients. This NMA showed that in terms of improving pain and disability, Craniosacral Therapy was the most effective intervention, followed by Other Manipulation and Pilates. In terms of improving physical health, Craniosacral Therapy was the most effective intervention, followed by Pilates and Meditation. In terms of improving mental health, Craniosacral Therapy was the most effective intervention, followed by Meditation and Pilates.
NLBP often includes diseases such as lumbar strain, third lumbar transverse synovial syndrome, lumbar dorsal myofasciitis, and myofibrillar tissue inflammation, with low back pain as the main symptom; in addition, the pain sites are mainly concentrated in the lower lumbar spine and lumbosacral region. NLBP patients have dysfunction of the sensorimotor system that controls muscle strength and coordination due to local pain, which reduces the activation ability and coordination of the lumbar muscles and makes them unable to withstand the daily load, which largely affects the functional activities and quality of life of patients (Pourahmadi et al., 2020). In addition, the pain produced by NLBP is not only related to physiological factors but also closely related to psychological factors. In 2020, the International Association for the Study of Pain updated the definition of pain as (Raja et al., 2020) “Pain is a distressing experience associated with actual or potential tissue damage with sensory, emotional, cognitive, and social components”, thus emphasizing the importance of the patient's subjective feelings and reinforcing the importance of the mental and psychological dimensions. This scenario indicates that physicians should consider the patient's symptoms, signs, and psychological status during treatment. This effect was also confirmed by Dinakar and Stillman (2016), who stated that pain is first transmitted to the spinal cord through afferent fibers and subsequently moves up to the thalamus for processing and integration, after which the information projects to various brain areas involved in perception, cognition and emotional components in the cerebral cortex, which elicits unpleasant emotions in patients. The patient's negative emotions are then consciously perceived, regulated, and transformed, thus resulting in an increase in the body's pain sensation and a vicious cycle of “pain-negative emotions” (Cosci et al., 2021). Therefore, in this NMA, four indicators (pain, disability, physical health, and mental health) were selected to evaluate the effects of different MBMBTs on NLBP patients.
The new finding of this NMA is that Craniosacral Therapy is the most effective MBMBT for NLBP. Cerebrospinal fluid circulates between the brain and spinal cord, which not only protects the spinal cord by cushioning vibrations but also removes metabolites and inflammatory exudates from the spinal cord and provides adequate nutrition, which is closely related to the treatment of CLBP (Laura et al., 2020). Levy (1999) applied MRI techniques to cerebrospinal fluid circulation and conducted a kinetic study; they found that the cerebrospinal fluid flow rate was slower in older individuals, thus indirectly suggesting that the cerebrospinal fluid flow rate is lower in patients with spinal degeneration than in normal subjects. Therefore, cerebrospinal fluid circulation may be the key to improving the condition of patients with NLBP. Craniosacral therapy, which was created by John E. Upledger in the United States in the 20th century, is a manipulation that loosens muscles and improves microcirculation and neurological dysfunction in the body by gently touching different parts of the entire mesolimbic system of the body from the cranial to the pelvic-sacral regions, thus adjusting the craniosacral rhythm, improving the flow of cerebrospinal fluid, and restoring normal connections and natural movements between the central nervous system and other systems of body therapy (Upledger, 1995). In addition, as a type of MBMBT, Craniosacral therapy focuses more on the interplay between brain, mind, body, and behavior, wherein patients in a relaxed state use the body's natural healing power and wisdom by noticing changes in the body in the present moment to integrate mind and body and to reregulate the body's balance while also promoting physical, emotional, and spiritual wellbeing (Haller et al., 2019). Consistent with the results of a previously published meta-analysis, Craniosacral Therapy significantly improved pain intensity, disability function, and physical and psychological quality of life in patients with chronic pain containing NLBP compared to conventional treatment (Haller et al., 2019). The multifidus is an important paravertebral muscle group that plays a key role in maintaining lumbar spine stability and is correspondingly closely related to the treatment of NLBP (James et al., 2022). Bialoszewski et al. (2014) compared the effects of Craniosacral Therapy with Other Manipulations in patients with NLBP and found that Craniosacral Therapy could differentially reduce pain intensity and frequency in patients with NLBP by decreasing the resting tension of the multifidus. In addition, the advantage of Craniosacral Therapy over other MBMBT is that it is gentle, applicable to any age group, and can stimulate the patient's potential to obtain a lasting and stable treatment effect.
The results of this NMA also showed that Pilates may be the MBMBT with the closest effectiveness to Craniosacral Therapy in the treatment of patients with NLBP. Consistent with the results of previous studies by other researchers (Fernández-Rodríguez et al., 2022; Shi et al., 2022), both demonstrate the unparalleled advantages of Pilates in the treatment of NLBP, which not only affects the stability of the lumbar spine but also causes impairment in the body's control of movement. Even if the patient's low back pain symptoms disappear and the ability to perform normal activities is restored, the muscle groups that have significant control over the stability of the human lumbar spine are difficult to restore. Therefore, in the treatment of NLBP, exercise intervention to strengthen the control of the core muscles and to restore the protective mechanism of the posterior lumbar spine to its normal biological structure is considered an effective approach. Pilates, which was also created in the 20th century, is an exercise that works with proper breathing methods to soothe the muscles of the whole body and to improve the control of the human trunk, thus aiming to improve the strength, flexibility, and posture of the body, as well as to enhance mental awareness and achieve physical and mental balance (Geneen et al., 2017). Several studies have demonstrated (Cruz-Díaz et al., 2018; Öner Suata and Karagün, 2022) that Pilates can activate deep paravertebral muscle groups, improve muscle strength and fatigue resistance, effectively improve patients' lumbar pain and dysfunction, help reduce negative emotions (such as anxiety and depression), relieve stress, enhance psychological tolerance, and improve quality of life.
All MBMBT for NLBP (a total of nine) were included in this NMA, in addition to Craniosacral Therapy and Pilates, Meditation, Yoga, Ayurvedic Massage, Yoga + Meditation, Qigong, Tai Chi, and Dance. Among them, Craniosacral Therapy and Ayurvedic Massage belong to the category of manipulation, whereas Pilates, Meditation, Yoga, Yoga + Meditation, Qigong, Tai Chi, and Dance belong to the category of movement. Ayurvedic massage and cranio-sacral therapy both have therapeutic effects by improving cerebrospinal fluid circulation and stimulating Aδ and C nerve fibers (Kumar et al., 2017; Haller et al., 2019). However, Ayurvedic massage was significantly less effective than Craniosacral Therapy, and the reason for this analysis may be because only one study on Ayurvedic massage was retrieved and could not be compared with other similar studies. Similar to the results of Park et al. (2020), Yoga, Tai Chi, and Qigong were effective in improving low back pain, dysfunction, physical health, and mental health; however, they fell into the mid-range in terms of their effectiveness in treating NLBP compared to the other therapies in this NMA. The reason for this result may be that all three therapies are a set of exercises possessing complex movements, which are initially difficult to independently complete without the leadership of a teacher. Although Meditation is more effective in terms of physical and mental health, it is less effective in terms of pain and disability. A review of previous studies found (Michalsen et al., 2016) that Meditation improves the physical and mental health of patients with NLBP; however, its efficacy is not significant because patients are plagued by long intervention times and slow results, thus resulting in poor compliance. Meditation + Yoga is a combined therapy that is supposed to be more effective than Meditation alone or Yoga alone. However, this is not the case, as Meditation or Yoga alone has better results for disability than the combination of the two. The reason for this effect may be due to the difficulty of the combined therapy and the excessive time that is needed, thus resulting in a poorer quality of movement for the patient. Dance exhibits the worst results in terms of disability, which may be due to the fact that there are fewer articles on Dance therapy NLBP, in addition to the complexity of Dance movements, which makes it difficult for most people to master its techniques in a short period of time (even with the guidance of a teacher).
Overall, this NMA provides further evidence for the effectiveness of MBMBT in the treatment of NLBP, which has certain clinical implications. First, the findings demonstrate that Craniosacral Therapy is significantly effective in improving pain, disability, physical health, and mental health in NLBP and may be the most effective MBMBT for treating patients with NLBP. In addition, Pilates is also one of the recommended treatments. Second, clinicians may consider and promote MBMBT as a good non-pharmacological treatment for NLBP management. Finally, the standardization of MBMBT application should also be guaranteed in the future; in addition, basic research on MBMBT may be considered to explore its mechanism of action.
First, this NMA is the first analysis to compare the effectiveness of different MBMBTs for NLBP, thus identifying an optimal measure to improve pain, disability, physical health, and mental health with scientific value, as well as providing reliable evidence for the treatment of NLBP patients. No language restrictions were made during the search, and no specific interventions were prescribed. A total of 46 RCTs and 3,886 patients were involved in the analysis. Moreover, the study results were reported with authenticity and completeness. Therefore, this NMA provides comprehensive and rigorous evidence-based recommendations for managing NLBP patients.
However, there were some limitations to this NMA. As it was not possible to obtain sufficient data for individual patients in the RCTs, the analysis could only be performed at the general level; therefore, confounding factors could not be eliminated. However, we considered the particular individuals that were mentioned in each RCT; thus, these factors had little impact on the results of the NMA. In addition, the insufficient number of studies and small sample sizes that were included in some interventions may have led to the probability of false-positive results for comparison. Therefore, until more high-quality RCTs are included, readers should view these results with caution.
This NMA shows that Craniosacral Therapy may be the best MBMBT for treating patients with NLBP and deserves clinical promotion. When multiple MBMBTs are simultaneously applied, the results may be counterproductive and are subsequently not recommended. However, limited by the number and quality of the included studies, as well as the small number of studies with direct comparisons between MBMBT, the results may be subject to some error, and more large samples and high-quality RCTs are needed for further validation to ensure the scientific validity of the findings.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
HY and XiW wrote the manuscript. WZ, YD, TS, and WC conducted the literature search, screening, data extraction, and analysis. XiW adjudicated all disagreements and provided technical guidance. XuW and JY contributed to the design and revision of the manuscript. WW contributed to the revision of the manuscript. All authors contributed to this paper, read the full text, and agreed to send the manuscript.
This study was supported by Lanzhou Talents Innovation and Entrepreneurship Project (Grant number: 2020-RC-54).
We thank all authors for their contributions to this review and reviewers for their valuable suggestions.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2023.1148048/full#supplementary-material
Banth, S., and Ardebil, M. D. (2015). Effectiveness of mindfulness meditation on pain and quality of life of patients with chronic low back pain. Int. J. Yoga 8, 128–133. doi: 10.4103/0973-6131.158476
Batibay, S., Kulcu, D. G., Kaleoglu, O., and Mesci, N. (2021). Effect of Pilates mat exercise and home exercise programs on pain, functional level, and core muscle thickness in women with chronic low back pain. J. Orthopaed. Sci. 26, 979–985. doi: 10.1016/j.jos.2020.10.026
Bernstein, I. A., Malik, Q., Carville, S., and Ward, S. (2017). Low back pain and sciatica: summary of NICE guidance. BMJ 356, i6748. doi: 10.1136/bmj.i6748
Bialoszewski, D., Bebelski, M., Lewandowska, M., and Slupik, A. (2014). Utility of craniosacral therapy in treatment of patients with non-specific low back pain. Preliminary report. Ortop. Traumatol. Rehabil. 16, 605–615. doi: 10.5604/15093492.1135120
Bishop, P. B., and Wing, P. C. (2003). Compliance with clinical practice guidelines in family physicians managing worker's compensation board patients with acute lower back pain. Spine J. 3, 442–450. doi: 10.1016/S1529-9430(03)00152-9
Blodt, S., Pach, D., Kaster, T., Ludtke, R., Icke, K., Reisshauer, A., et al. (2015). Qigong versus exercise therapy for chronic low back pain in adults–a randomized controlled non-inferiority trial. Eur. J. Pain 19, 123–131. doi: 10.1002/ejp.529
Castro-Sánchez, A. M., Lara-Palomo, I. C., Matarán-Peñarrocha, G. A., Saavedra-Hernández, M., Pérez-Mármol, J. M., and Aguilar-Ferrándiz, M. E. (2016). Benefits of craniosacral therapy in patients with chronic low back pain: a randomized controlled trial. J. Altern. Comp. Med. 22, 650–657. doi: 10.1089/acm.2016.0068
Chen, J. A., Anderson, M. L., Cherkin, D. C., Balderson, B. H., Cook, A. J., Sherman, K. J., et al. (2023). Moderators and nonspecific predictors of treatment benefits in a randomized trial of mindfulness-based stress reduction vs. cognitive-behavioral therapy vs. usual care for chronic low back pain. J. Pain 24, 282–303 doi: 10.1016/j.jpain.2022.09.014
Cherkin, D. C., Sherman, K. J., Balderson, B. H., Cook, A. J., Anderson, M. L., Hawkes, R. J., et al. (2016). Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. JAMA 315, 1240–1249. doi: 10.1001/jama.2016.2323
Clark, S., and Horton, R. (2018). Low back pain: a major global challenge. Lancet 391, 2302. doi: 10.1016/S0140-6736(18)30725-6
Cosci, F., Svicher, A., Mansueto, G., Benemei, S., Chiarugi, A., De Cesaris, F., et al. (2021). Mental pain and pain-proneness in patients with migraine: results from the PAINMIG cohort-study. CNS Spectr. 26, 491–500. doi: 10.1017/S1092852920001480
Cox, H., Tilbrook, H., Aplin, J., Semlyen, A., Torgerson, D., Trewhela, A., et al. (2010). A randomised controlled trial of yoga for the treatment of chronic low back pain: results of a pilot study. Comp. Ther. Clin. Pract. 16, 187–193. doi: 10.1016/j.ctcp.2010.05.007
Cruz-Díaz, D., 2, Romeu, M., Velasco-González, C., Martínez-Amat, A., and Hita-Contreras, F. (2018). The effectiveness of 12 weeks of Pilates intervention on disability, pain and kinesiophobia in patients with chronic low back pain: a randomized controlled trial. Clin. Rehabil. 32, 1249–1257. doi: 10.1177/0269215518768393
Cumpston, M., Li, T., Page, M. J., Chandler, J., Welch, V. A., Higgins, J. P., et al. (2019). Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochr. Database Syst. Rev. 10, ED000142. doi: 10.1002/14651858.ED000142
da Silva, T., Mills, K., Brown, B. T., Herbert, R. D., Maher, C. G., and Hancock, M. J. (2017). Risk of recurrence of low back pain: a systematic review. Orthop. Sports Phys. Ther. 47, 305–313. doi: 10.2519/jospt.2017.7415
de Freitas, C. D., Costa, D. A., Carvas, N., and Civile, V. T. (2020). Effects of the pilates method on kinesiophobia associated with chronic non-specific low back pain: systematic review and meta-analysis. J. Bodyw. Mov. Ther. 24, 300–306. doi: 10.1016/j.jbmt.2020.05.005
Deyo, R. A., and Bass, J. E. (1989). Lifestyle and low-back pain. The influence of smoking and obesity. Spine 14, 501–506. doi: 10.1097/00007632-198905000-00005
Dinakar, P., and Stillman, A. M. (2016). Pathogenesis of pain. Semin. Pediatr. Neurol. 23, 201–208. doi: 10.1016/j.spen.2016.10.003
Dossett, M. L., Fricchione, G., and Benson, H. (2020). A new era for mind-body medicine. N. Engl. J. Med. 382, 1390–1391. doi: 10.1056/NEJMp1917461
Fernández-Rodríguez, R., Álvarez-Bueno, C., Cavero-Redondo, I., Torres-Costoso, A., Pozuelo-Carrascosa, D. P., Reina-Gutiérrez, S., et al. (2022). Best exercise options for reducing pain and disability in adults with chronic low back pain: pilates, strength, core-based, and mind-Body. A network meta-analysis. J. Orthop. Sports Phys. Ther. 52, 505–521. doi: 10.2519/jospt.2022.10671
Fogaça, L. Z., Portella, C. F. S., Ghelman, R., Abdala, C. V. M., and Schveitzer, M. C. (2021). Mind-body therapies from traditional chinese medicine: evidence map. Front. Public Health 9, 659075. doi: 10.3389/fpubh.2021.659075
Gatchel, R. J., Polatin, P. B., Mayer, T. G., and Mayer, T. G. (1995). The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine(Phila Pa 1976) 20, 2703–2709. doi: 10.1097/00007632-199512150-00011
Geneen, L. J., Moore, R. A., Clarke, C., Martin, D., Colvin, L. A., and Smith, B. H. (2017). Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochr. Database Syst. Rev. 1, CD011279. doi: 10.1002/14651858.CD011279.pub2
Ghasemi, C., Amiri, A., Sarrafzadeh, J., and Dadgoo, M. (2021). Effects of craniosacral therapy and sensorimotor training on pain, disability, depression and quality of life of patients with nonspecific chronic low back pain: a randomized clinical trial. Anaesth. Pain Intens. Care 25, 189–198. doi: 10.35975/apic.v25i2.1458
Ghasemi, C., Amiri, A., Sarrafzadeh, J., Dadgoo, M., and Maroufi, N. (2020). Comparison of the effects of craniosacral therapy, muscle energy technique, and sensorimotor training on non-specific chronic low back pain. Anaesth. Anaesth. Pain Intens. Care 24, 532–543. doi: 10.35975/apic.v24i5.1362
Gladwell, V., Head, S., Haggar, M., and Beneke, R. (2006). Does a program of pilates improve chronic non-specific low back pain? J. Sport Rehabil. 15, 338–350. doi: 10.1123/jsr.15.4.338
Green, A. A.-O., and Kinchen, E. V. (2021). The effects of mindfulness meditation on stress and burnout in nurses. J. Holist. Nurs. 39, 356–368. doi: 10.1177/08980101211015818
Groessl, E. J., Liu, L., Chang, D. G., Wetherell, J. L., Bormann, J. E., Atkinson, J. H., et al. (2017). Yoga for military veterans with chronic low back pain: a randomized clinical trial. Am. J. Prev. Med. 53, 599–608. doi: 10.1016/j.amepre.2017.05.019
Hall, A. M., Maher, C. G., Lam, P., Ferreira, M., and Latimer, J. (2011). Tai chi exercise for treatment of pain and disability in people with persistent low back pain: a randomized controlled trial. Arthrit. Care Res. 63, 1576–1583. doi: 10.1002/acr.20594
Haller, H., Lauche, R., Sundberg, T., Dobos, G., and Cramer, H. (2019). Craniosacral therapy for chronic pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet. Disord. 21, 1. doi: 10.1186/s12891-019-3017-y
Hartvigsen, J., Hancock, M. J., Kongsted, A., Louw, Q., Ferreira, M. L., Genevay, S., et al. (2018). What low back pain is and why we need to pay attention. Lancet 391, 2356–2367. doi: 10.1016/S0140-6736(18)30480-X
Hasanpour-Dehkordi, A., Dehghani, A., and Solati, K. (2017). A Comparison of the effects of pilates and McKenzie training on pain and general health in men with chronic low back pain: a randomized trial. Indian J. Palliat. Care 23, 36–40. doi: 10.4103/0973-1075.197945
Hlaing, S. S., Puntumetakul, R., Khine, E. E., and Boucaut, R. (2021). Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet. Disord. 22, 998. doi: 10.1186/s12891-021-04858-6
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmid, C. H., Cameron, C., et al. (2015). The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern. Med. 162, 777–784. doi: 10.7326/M14-2385
Itz, C. J., Geurts, J. W., van Kleef, M., and Nelemans, P. (2013). Clinical course of non-specific low back pain: a systematic review of prospective cohort studies set in primary care. Eur. J. Pain 17, 5–15. doi: 10.1002/j.1532-2149.2012.00170.x
James, G., Stecco, C., Blomster, L., Hall, L., Schmid, A. B., Shu, C. C., et al. (2022). Muscle spindles of the multifidus muscle undergo structural change after intervertebral disc degeneration. Eur. Spine J. 31, 1879–1888. doi: 10.1007/s00586-022-07235-6
James, S. L., Abate, D., Abate, K. H., Abay, S. M., Abbafati, C., Abbasi, N., et al. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1789–1858. doi: 10.1016/S0140-6736(18)32279-7
Katz, J. N., Alaranta, H., Kallio, V., and Christensen, F. B. (2006). Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J. Bone Joint Surg. Am. 88(Suppl. 2), 21–24. doi: 10.2106/00004623-200604002-00005
Kliziene, I., Sipaviciene, S., Vilkiene, J., Astrauskiene, A., Cibulskas, G., Klizas, S., et al. (2017). Effects of a 16-week Pilates exercises training program for isometric trunk extension and flexion strength. J. Bodyw. Mov. Ther. 21, 124–132. doi: 10.1016/j.jbmt.2016.06.005
Knezevic, N. N., Candido, K. D., Vlaeyen, J. W. S., Van Zundert, J., and Cohen, S. P. (2021). Low back pain. Lancet 398, 78–92. doi: 10.1016/S0140-6736(21)00733-9
Kofotolis, N., Kellis, E., Vlachopoulos, S. P., Gouitas, I., and Theodorakis, Y. (2016). Effects of Pilates and trunk strengthening exercises on health-related quality of life in women with chronic low back pain. J. Back Musculoskelet. Rehabil. 29, 649–659. doi: 10.3233/BMR-160665
Kumar, S., Rampp, T., Kessler, C., Jeitler, M., Dobos, G. J., Ludtke, R., et al. (2017). Effectiveness of ayurvedic massage (Sahacharadi Taila) in patients with chronic low back pain: a randomized controlled trial. J. Altern. Comp. Med. 23, 109–115. doi: 10.1089/acm.2015.0272
Laura, P., Claudia, B., Jessica, C., Farida, B., Mark, S., and Lancaster, M. A. (2020). Human CNS barrier-forming organoids with cerebrospinal fluid production. Science 369, eaaz5626. doi: 10.1126/science.aaz5626
Lee, M. S., Pittler, M. H., and Ernst, E. (2009). Internal qigong for pain conditions: a systematic review. J. Pain 10, 1121–1127.e14. doi: 10.1016/j.jpain.2009.03.009
Levy, L. M. (1999). MR imaging of cerebrospinal fluid flow and spinal cord motion in neurologic disorders of the spine. Magn. Reson. Imaging Clin. N. Am. 7, 573–587. doi: 10.1016/S1064-9689(21)00576-6
Liu, J., Yeung, A., Xiao, T., Tian, X., Kong, Z., Zou, L., et al. (2019). Chen-style Tai Chi for individuals (aged 50 years old or above) with chronic non-specific low back pain: a randomized controlled trial. Int. J. Environ. Res. Public Health 16, 517. doi: 10.3390/ijerph16030517
Maher, C., Underwood, M., and Buchbinder, R. (2017). Non-specific low back pain. Lancet 389, 736–747. doi: 10.1016/S0140-6736(16)30970-9
Mazloum, V., Sahebozamani, M., Barati, A., Nakhaee, N., and Rabiei, P. (2018). The effects of selective pilates versus extension-based exercises on rehabilitation of low back pain. J. Bodyw. Mov. Ther. 22, 999–1003. doi: 10.1016/j.jbmt.2017.09.012
Michalsen, A., Jeitler, M., Kessler, C. S., Steckhan, N., Robens, S., Ostermann, T., et al. (2021). Yoga, eurythmy therapy and standard physiotherapy (YES-Trial) for patients with chronic non-specific low back pain: a three-armed randomized controlled trial. J. Pain 22, 1233–1245. doi: 10.1016/j.jpain.2021.03.154
Michalsen, A., Kunz, N., Jeitler, M., Brunnhuber, S., Meier, L., Ludtke, R., et al. (2016). Effectiveness of focused meditation for patients with chronic low back pain-A randomized controlled clinical trial. Comp. Ther. Med. 26, 79–84. doi: 10.1016/j.ctim.2016.03.010
Miyamoto, G. C., Costa, L. O. P., Galvanin, T., and Cabral, C. M. N. (2013). Efficacy of the addition of modified pilates exercises to a minimal intervention in patients with chronic low back pain: a randomized controlled trial. Phys. Ther. 93, 310–320. doi: 10.2522/ptj.20120190
Miyamoto, G. C., Franco, K. F. M., van Dongen, J. M., Franco, Y. R. D. S., de Oliveira, N. T. B., Amaral, D. D. V., et al. (2018). Different doses of pilates-based exercise therapy for chronic low back pain: a randomised controlled trial with economic evaluation. Br. J. Sports Med. 52, 859–868. doi: 10.1136/bjsports-2017-098825
Morone, N. E., Greco, C. M., and Weiner, D. K. (2008). Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain 134, 310–319. doi: 10.1016/j.pain.2007.04.038
Morone, N. E., Rollman, B. L., Moore, C. G., Li, Q., and Weiner, D. K. (2009). A mind-body program for older adults with chronic low back pain: results of a pilot study. Pain Med. 10, 1395–1407. doi: 10.1111/j.1526-4637.2009.00746.x
Mostagi, F. Q., Dias, J. M., Pereira, L. M., Obara, K., Mazuquin, B. F., Silva, M. F., et al. (2015). Pilates versus general exercise effectiveness on pain and functionality in non-specific chronic low back pain subjects. J. Bodyw. Mov. Ther. 19, 636–645. doi: 10.1016/j.jbmt.2014.11.009
Nambi, G. S., Inbasekaran, D., Khuman, R., Devi, S., and Shanmugananth, Jagannathan, K. (2014). Changes in pain intensity and health related quality of life with Iyengar yoga in nonspecific chronic low back pain: a randomized controlled study. Int. J. Yoga 7, 48–53. doi: 10.4103/0973-6131.123481
Natour, J., Cazotti, L. D., Ribeiro, L. H., Baptista, A. S., and Jones, A. (2015). Pilates improves pain, function and quality of life in patients with chronic low back pain: a randomized controlled trial. Clin. Rehabil. 29, 59–68. doi: 10.1177/0269215514538981
Okafor, U. A. C., Solanke, T. A., Akinbo, S. R. A., and Odebiyi, D. O. (2012). Effect of aerobic dance on pain, functional disability and quality of life on patients with chronic low back pain. S. Afr. J. Physiother. 68, 11–14. doi: 10.4102/sajp.v68i3.18
Öner Suata, C., and Karagün, E. (2022). Effect of Pilates exercise on cognitive distortion, stress coping and psychological endurance of women victim of violence. J. Sports Med. Phys. Fitness 62, 280–287. doi: 10.23736/S0022-4707.21.12080-8
Park, J., Krause-Parello, C. A., and Barnes, C. M. (2020). A narrative review of movement-based mind-body interventions: effects of Yoga, Tai Chi, and Qigong for back pain patients. Holist. Nurs. Pract. 34, 3–23. doi: 10.1097/HNP.0000000000000360
Patti, A., Bianco, A., Paoli, A., Messina, G., Montalto, M. A., Bellafiore, M., et al. (2016). Pain perception and stabilometric parameters in people with chronic low back pain after a pilates exercise program: a randomized controlled trial. Medicine 95, e2414. doi: 10.1097/MD.0000000000002414
Phattharasupharerk, S., Purepong, N., Eksakulkla, S., and Siriphorn, A. (2019). Effects of Qigong practice in office workers with chronic non-specific low back pain: a randomized control trial. J. Bodyw. Mov. Ther. 23, 375–381. doi: 10.1016/j.jbmt.2018.02.004
Pourahmadi, M., Sahebalam, M., and Bagheri, R. (2020). Effectiveness of proprioceptive neuromuscular facilitation on pain intensity and functional disability in patients with low back pain: a systematic review and meta-analysis. Arch. Bone Jt. Surg. 8, 479–501. doi: 10.22038/abjs.2020.45455.2245
Qaseem, A., Wilt, T. J., McLean, R. M., Forciea, M. A., and Clinical Guidelines Committee of the American College of Physicians Denberg, T. D.. (2017). Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the american college of physicians. Ann. Intern. Med. 166, 514–530. doi: 10.7326/M16-2367
Raja, S. N., Carr, D. B., Cohen, M., Finnerup, N. B., Flor, H., Gibson, S., et al. (2020). The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain 161, 1976–1982. doi: 10.1097/j.pain.0000000000001939
Ravindran, A. K., Javed, J., Parthiban, R., and Sherrif, B. (2022). Effectiveness of aerobic exercise versus pilates in postmenopausal women with non-specific chronic low back pain. Ind. J. Physiother. Occup. Therapy 16, 1–8. doi: 10.37506/ijpot.v16i2.18026
Saper, R. B., Lemaster, C., Delitto, A., Sherman, K. J., Herman, P. M., Sadikova, E., et al. (2017). Yoga, physical therapy, or education for chronic low back pain: a randomized noninferiority trial. Ann. Intern. Med. 167, 85–94. doi: 10.7326/M16-2579
Saper, R. B., Sherman, K. J., Cullum-Dugan, D., Davis, R. B., Phillips, R. S., and Culpepper, L. (2009). Yoga for chronic low back pain in a predominantly minority population: a pilot randomized controlled trial. Altern. Ther. Health Med. 15, 18–27. doi: 10.1016/j.explore.2009.03.047
Sherman, K. J., Cherkin, D. C., Wellman, R. D., Cook, A. J., Hawkes, R. J., Delaney, K., et al. (2011). A randomized trial comparing yoga, stretching, and a self-care book for chronic low back pain. Arch. Intern. Med. 171, 2019–2026. doi: 10.1001/archinternmed.2011.524
Shi, J., Hu, Z. Y., Wen, Y. R., Wang, Y. F., Lin, Y. Y., Zhao, H. Z., et al. (2022). Optimal modes of mind-body exercise for treating chronic non-specific low back pain: systematic review and network meta-analysis. Front. Neurosci. 16, 1046518. doi: 10.3389/fnins.2022.1046518
Siddique, N., Siddiqi, M. I., Anwar, N., Ali, S., Fatima Ali, M. L., et al. (2021). Comparison of pilates exercises and motor control exercises on nonspecific low back pain patients. Ann. Med. Health Sci. Res. 11, 29–32.
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., et al. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898. doi: 10.1136/bmj.l4898
Stochkendahl, M. J., Kjaer, P., Hartvigsen, J., Kongsted, A., Aaboe, J., Andersen, M., et al. (2018). National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. Eur. Spine J. 27, 60–75. doi: 10.1007/s00586-017-5099-2
Telles, S., Bhardwaj, A. K., Gupta, R. K., Sharma, S. K., Monro, R., and Balkrishna, A. (2016). A randomized controlled trial to assess pain and magnetic resonance imaging-based (MRI-based) structural spine changes in low back pain patients after yoga practice. Med. Sci. Monit. 22,3228–3247. doi: 10.12659/MSM.896599
Teut, M., Knilli, J., Daus, D., Roll, S., and Witt, C. M. (2016). Qigong or yoga versus no intervention in older adults with chronic low back pain-a randomized controlled trial. J. Pain 17, 796–805. doi: 10.1016/j.jpain.2016.03.003
Turner, J. A., Anderson, M. L., Balderson, B. H., Cook, A. J., Sherman, K. J., and Cherkin, D. C. (2016). Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain 157, 2434–2444. doi: 10.1097/j.pain.0000000000000635
Valenza, M. C., Rodriguez-Torres, J., Cabrera-Martos, I., Diaz-Pelegrina, A., Aguilar-Ferrandiz, M. E., and Castellote-Caballero, Y. (2017). Results of a Pilates exercise program in patients with chronic non-specific low back pain: a randomized controlled trial. Clin. Rehabil. 31, 753–760. doi: 10.1177/0269215516651978
Vohra, S., McClafferty, H., Becker, D., Bethell, C., Culbert, T., King-Jones, S., et al. (2016). Mind-body therapies in children and youth. Pediatrics 138, e20161896. doi: 10.1542/peds.2016-1896
Wajswelner, H., Metcalf, B, and Bennell, K. (2012). Clinical pilates versus general exercise for chronic low back pain: randomized trial. Med. Sci. Sports Exerc. 44, 1197–1205. doi: 10.1249/MSS.0b013e318248f665
Weifen, W., Muheremu, A., Chaohui, C., Md, L. W., and Lei, S. (2013). Effectiveness of tai chi practice for non-specific chronic low back pain on retired athletes: a randomized controlled study. J. Musculoskelet. Pain 21, 37–45. doi: 10.3109/10582452.2013.763394
Williams, K., Abildso, C., Steinberg, L., Doyle, E., Epstein, B., Smith, D., et al. (2009). Evaluation of the effectiveness and efficacy of Iyengar yoga therapy on chronic low back pain. Spine (Phila Pa 1976) 34, 2066–2076. doi: 10.1097/BRS.0b013e3181b315cc
Williams, K. A., Petronis, J., Smith, D., Goodrich, D., Wu, J., Ravi, N., et al. (2005). Effect of Iyengar yoga therapy for chronic low back pain. Pain 115, 107–117. doi: 10.1016/j.pain.2005.02.016
Zgierska, A. E., Burzinski, C. A., Cox, J., Kloke, J., Stegner, A., Cook, D. B., et al. (2016). Mindfulness meditation and cognitive behavioral therapy intervention reduces pain severity and sensitivity in opioid-treated chronic low back pain: pilot findings from a randomized controlled trial. Pain Med. 17, 1865–1881. doi: 10.1093/pm/pnw006
Keywords: mindfulness, mind-body therapies, non-operative therapy, non-specific low back pain, network meta-analysis
Citation: Yang H, Wang X, Wang X, Yang J, Zhang W, Ding Y, Sang T, Chen W and Wang W (2023) Effect of mindfulness-based mind-body therapies in patients with non-specific low back pain—A network meta-analysis of randomized controlled trials. Front. Aging Neurosci. 15:1148048. doi: 10.3389/fnagi.2023.1148048
Received: 19 January 2023; Accepted: 09 June 2023;
Published: 29 June 2023.
Edited by:
Notger G. Müller, University of Potsdam, GermanyReviewed by:
Fei Luo, Chinese Academy of Sciences, ChinaCopyright © 2023 Yang, Wang, Wang, Yang, Zhang, Ding, Sang, Chen and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangfu Wang, wangxf_1969@163.com
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.