
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Aging Neurosci. , 04 May 2023
Sec. Neurocognitive Aging and Behavior
Volume 15 - 2023 | https://doi.org/10.3389/fnagi.2023.1121190
Objective: The present study aimed to explore the combined associations of depression and cognitive impairment with functional disability and mortality, and whether the joint effects of depression and cognitive impairment on mortality were influenced by functional disability.
Methods: A total of 2,345 participants aged 60 and above from the 2011–2014 cycle of the National Health and Nutrition Examination Survey (NHANES) were included in the analyses. Questionnaires were used to evaluated depression, global cognitive function and functional disability (including disability in activities of daily living (ADLs), instrumental activities of daily living (IADLs), leisure and social activities (LSA), lower extremity mobility (LEM), and general physical activity (GPA)). Mortality status was ascertained up to December 31, 2019. Multivariable logistic regression was performed to investigate the associations of depression and low global cognition with functional disability. Cox proportional hazards regression models were conducted to evaluate the effect of depression and low global cognition on mortality.
Results: Interactions between depression and low global cognition were observed when exploring associations of depression and low global cognition with IADLs disability, LEM disability, and cardiovascular mortality. Compared with normal participants, participants with both depression and low global cognition had the highest odds ratios of disability in ADLs, IADLs, LSA, LEM, and GPA. Besides, participants with both depression and low global cognition also had the highest hazard ratios of all-cause mortality and cardiovascular mortality, and these associations remained after adjusting for disability in ADLs, IADLs, LSA, LEM, and GPA.
Conclusion: Older adults with both depression and low global cognition were more likely to have functional disability, and had the highest risk of all-cause mortality and cardiovascular mortality.
Depression and cognitive impairment are two common disorders among the older adults (Polyakova et al., 2014). The prevalence of depression and cognitive impairment were reported to be 11.2 and 18.6% among the US older adults, respectively (Steffens et al., 2009; Hale et al., 2020). Emerging evidence indicates that depression and cognitive impairment are closely intertwined, and these two symptoms can be mutually prompted (Scult et al., 2017; Zheng et al., 2018).
Functional ability–the ability to conduct physical activities of daily living—is helpful for older individuals to live independently (Kuo et al., 2007). Studies found that functional disability was associated with an increased risk of poor quality of daily life and premature death (WHO, 2001; Murad et al., 2015; Wu et al., 2016), which highlighted the importance of identifying risk factors for functional disability.
Previous studies reported that depression and cognitive impairment were associated with functional disability (Mehta et al., 2002; Yochim et al., 2008; Li and Conwell, 2009; Olaya et al., 2016; Wu, 2021; Yang et al., 2021). However, only a few studies have explored the combined associations of depression and cognitive impairment with functional disability, and the results were inconsistent (Mehta et al., 2002; Li and Conwell, 2009; Olaya et al., 2016; Wu, 2021). A longitudinal study conducted in older adults found that improvement of depression could further attenuate the adverse effect of cognitive impairment on instrumental activities of daily living disability (Li and Conwell, 2009). In contrast, the other two prospective studies found that the interactive effect between depression and cognitive impairment not existed for disability in activities of daily living or disability in instrumental activities of daily living disability (Mehta et al., 2002; Wu, 2021). In addition, a community-based study of 7,987 older adults found that country-specific difference is implicated in the combined associations of depression and cognitive impairment with functional disability (Olaya et al., 2016). They found that the interactive effect between depression and cognitive impairment on disability only existed in older adults from Finland but not in older adults from Poland and Spain, and the direction of interaction effects contradicted the previous study (Olaya et al., 2016).
Furthermore, few studies have investigated the joint effects of depression and cognitive impairment on mortality, and it is not well understood whether these effects were affected by functional disability (Arfken et al., 1999; Georgakis et al., 2016).
Hence, the present study aimed to investigate the combined associations of depression and cognitive impairment with functional disability and mortality, and whether the joint effects of depression and cognitive impairment on mortality were influenced by functional disability.
The National Health and Nutrition Examination Survey (NHANES) used a stratified, multistage, probability cluster sampling design to assess the nationally representative health and nutritional status of the non-institutionalized US civilian. The present study included data from 3,632 adults aged 60 and above from the NHANES (2011–2012 and 2013–2014). The present study further excluded 1,287 participants with missing information on depression, cognitive function assessment, and functional disability. Finally, a total of 2,345 participants were included in the analyses.
The NHANES procedures and protocols were approved by the National Center for Health Statistics Research Ethics Review Board. All participants provided written informed consent for participation in the NHANES (Parsons et al., 2014). More information on the NHANES is available on: https://www.cdc.gov/nchs/nhanes/index.htm.
Depression was assessed using the Nine-item Patient Health Questionnaire (PHQ-9), which was widely used for screening for non-psychiatric depression (Kroenke et al., 2001). PHQ-9 has 9 items and each item scored from 0 (“not at all”) to 3 (“nearly every day”). The total PHQ-9 score ranges from 0 to 27, and participants with a total PHQ-9 score ≥ 10 were diagnosed as having major depression. This cutoff has a sensitivity of 88% and a specificity of 88% for diagnosing major depression (Kroenke et al., 2001).
Cognitive function was evaluated using the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD), the Animal Fluency test, and the Digit Symbol Substitution Test (DSST; Morris et al., 1989; Wechsler, 1997; Strauss et al., 2006). The CERAD test consists of three consecutive learning trials and one delayed recall, which was used to assess the immediate and delayed learning ability for new verbal information. The score of each trial ranges from 0 to 10, and the total scores range from 0 to 40 (Morris et al., 1989). The Animal Fluency test was conducted to examine categorical verbal fluency, with the total scores ranging from 0 to 40 (Strauss et al., 2006). The Digit Symbol Substitution test (DSST) was performed to evaluate processing speed, visual scanning, sustained attention, and short-term memory, with the scores ranging from 0 to 133 (Wechsler, 1997). Higher scores of the three tests indicated better cognitive performance.
Then, the scores of each cognitive test were Z-score transformed. The overall cognitive score was calculated as the average of the standardized scores from three cognitive tests. Because there is no well-defined threshold for identifying low cognitive performance, we defined participants with an overall cognitive score in the lowest unweighted quartile in the study population as having low global cognition (Brody et al., 2019; Huang and Ren, 2022).
Functional disability was evaluated using the 19-item physical functioning questionnaire (Cosiano et al., 2020). Physical functioning consisted of five main domains: (Polyakova et al., 2014) activities of daily living (ADLs) (getting in and out of bed, eating, and dressing); (Steffens et al., 2009) instrumental activities of daily living (IADLs) (managing money, performing house chores, preparing meals); (Hale et al., 2020) leisure and social activities (LSA) (going to the movies, attending social events, performing leisure activity at home); (Scult et al., 2017) lower extremity mobility (LEM) (walking a quarter mile, walking up to 10 steps, walking between rooms on the same floor); and (Zheng et al., 2018) general physical activity (GPA) (lifting or carrying heavy objects, reaching up overhead, grasping/holding small objects, standing for long periods, sitting for long periods). The answer to each item was “no difficulty,” “some difficulty,” “much difficulty” or “unable to do.” Participants were defined as having a functional disability in this domain if some difficulty in one or more items was reported in a given domain (Cosiano et al., 2020).
Mortality status and cause of death were identified by linking to death records in the National Death Index public access files through December 31, 2019 (Statistics NCfH, 2021). Cardiovascular mortality and cancer mortality were ascertained based on the underlying causes of death from the International Classification of Diseases codes.
Information on age (60–64, 65–69, 70–74, 75–79, and 80+), gender (male and female), race (Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, and other race), marital status (never married, married or living with a partner, and widowed or separated or divorced), education (less than high school, high school, and college education or above), smoke (never, former, and current), alcohol drinking (yes and no), and social economic status were obtained by questionnaire survey. A modified Global Physical Activity Questionnaire was used to measure physical activity and participants were classified as physically active if their consumed metabolic equivalent scores (MET) ≥ 600 MET-minutes/week. Social economic status was classified using the ratio of family income to poverty (PIR) as low (PIR ≤ 1.3), middle (PIR > 1.3 to ≤1.85) or high (PIR > 1.85). Body mass index (BMI) was categorized as underweight (< 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), obese class I (30–34.9 kg/m2), and obese class II or class III (≥ 35 kg/m2).
Participants with a self-reported history of coronary heart disease (CHD), angina, or myocardial infarction were defined as having CHD. Diabetes was ascertained if participants had a self-reported diagnosis of diabetes, were taking medicine for diabetes, or had glycosylated hemoglobin ≥6.5%. Hypertension was determined if participants reported a history of hypertension, were taking prescription for hypertension, or had a mean systolic blood pressure ≥ 140 mm Hg or a mean diastolic blood pressure ≥ 90 mm Hg. Stroke was defined if participants had a history of stroke. Cancer was defined if participants had a history of cancer or malignancy. Comprehensive descriptions of methodology and data collection were provided elsewhere (Prevention CfDCa, n.d.).
According to the status of depression and global cognition, participants were classified into four groups: normal, depression only, low global cognition only, and coexistence of depression and low global cognition. Differences in baseline characteristics between groups were compared using weighted chi-square tests.
We conducted weighted multivariate logistic regression models to explore the separate and combined associations of depression and low global cognition with each component of functional disability, and interactions between depression and low global cognition were examined. Age categories, gender, race, marital status, education, smoke, alcohol drinking, physical activity, PIR category, BMI category, CHD, diabetes, hypertension, stroke, and cancer were adjusted in the regression models.
Kaplan–Meier (weighted) analysis was conducted to describe the survival of participants with different status of depression and global cognition. Weighted Cox proportional hazards regression models were performed to evaluate the separate and joint effect of depression and low global cognition on all-cause mortality, cardiovascular mortality, and cancer mortality. Age categories, gender, race, marital status, education, smoke, alcohol drinking, physical activity, PIR category, BMI category, CHD, diabetes, hypertension, stroke, and cancer were adjusted in the Cox model 1. To further explore whether the joint effects of depression and low global cognition on all-cause mortality, cardiovascular mortality and cancer mortality were influenced by functional disability, we additionally adjusted for disability in ADLs, IADLs, LSA, LEM, and GPA based on Cox model 1 (Cox model 2).
All statistical analyzes were conducted using STATA 15.0. A two-sided p-value of <0.05 was considered statistically significant.
The characteristics of participants with different status of depression and low global cognition are shown in Table 1. Among 2,345 participants, 112 (4.8%) participants had depression only, 499 (21.3%) participants had low global cognition only, and 88 (3.8%) participants had both depression and low global cognition. Significant differences in age categories, gender, race, marital status, education, alcohol drinking, physical activity, PIR category, prevalence of CHD, diabetes, hypertension, and stroke, and prevalence of disability in ADLs, IADLs, LSA, LEM, and GPA were observed between groups.
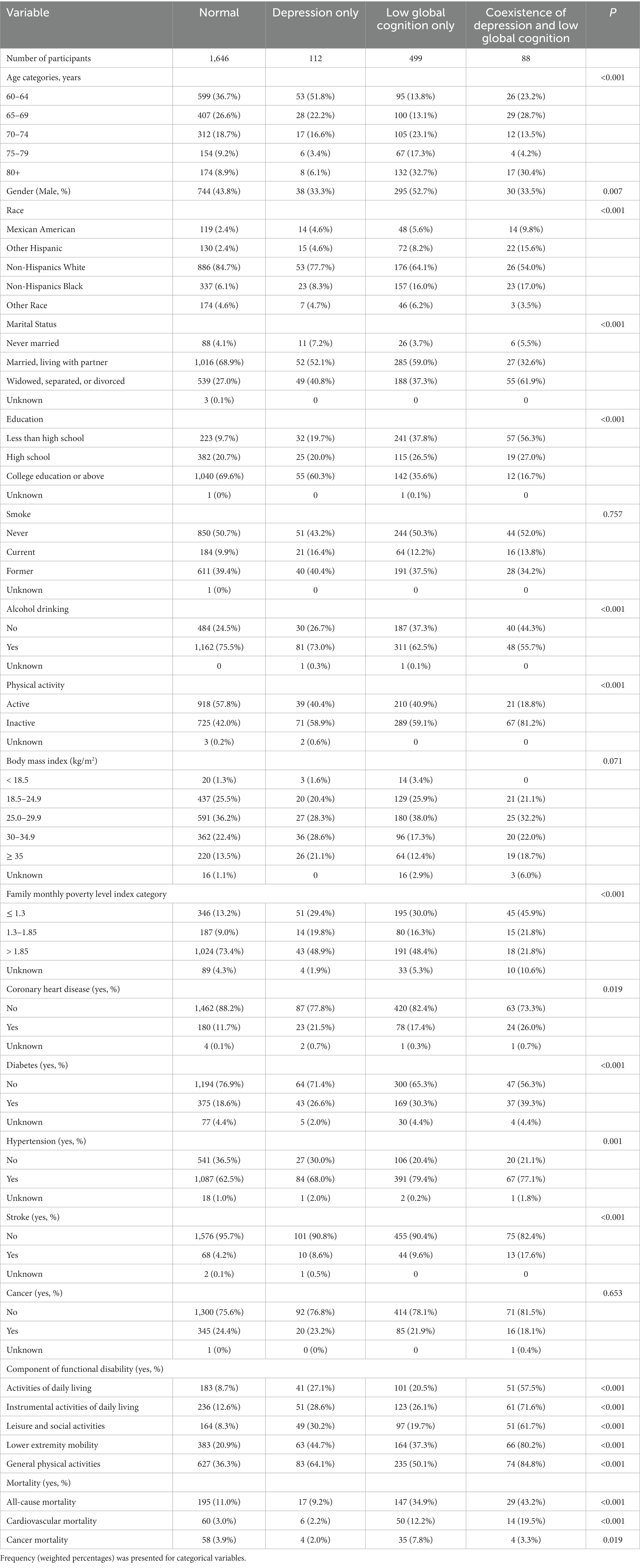
Table 1. Characteristics of participants with different status of depression and low global cognition.
The separate associations of depression and low global cognition with each component of functional disability are shown in Table 2. Both depression and low global cognition were positively associated with disability in ADLs, IADLs, LSA, and LEM, and depression was positively associated with disability in GPA. Significant interactions between depression and low global cognition were observed for disability in IADLs (P for interaction = 0.008) and LEM (P for interaction = 0.019).
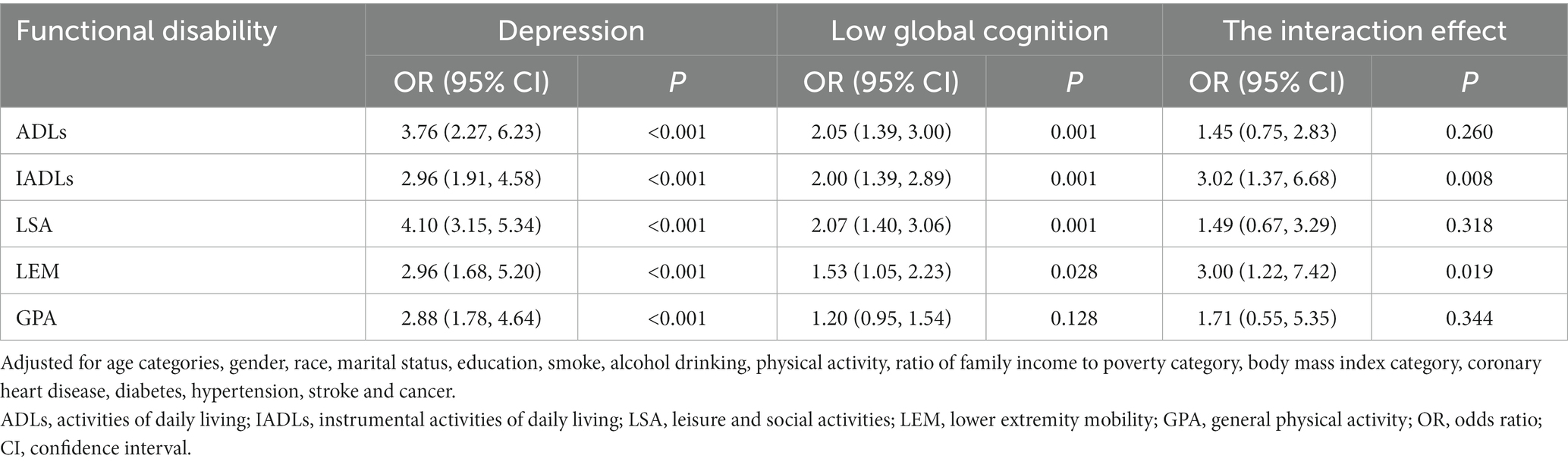
Table 2. Separate associations of depression and low global cognition with each component of functional disability.
The combined associations of depression and low global cognition with each component of functional disability are shown in Table 3. Compared with normal group, depression only, low global cognition only and coexistence of depression and low global cognition were positively associated with disability in ADLs, IADLs, and LSA, and the odd ratios (ORs) were highest in participants with both depression and low global cognition. Compared with normal group, depression only and coexistence of depression and low global cognition were positively associated with disability in LEM and GPA, and the ORs were highest in the coexistence of depression and low global cognition group.
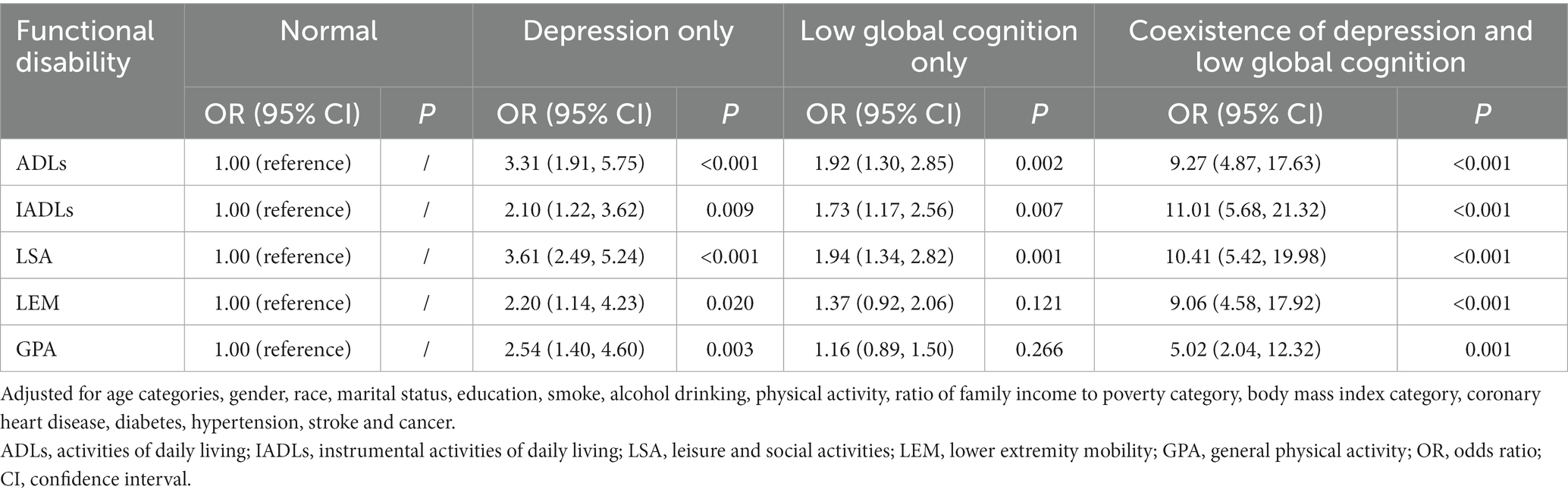
Table 3. Combined associations of depression and low global cognition with each component of functional disability.
Information on death was successfully followed up for 2,341 participants, and 388 participants died during the follow-up. The median follow-up time for all participants was 6.5 years. The separate effects of depression and low global cognition on all-cause mortality, cardiovascular mortality, and cancer mortality are shown in Table 4. Low global cognition but not depression was associated with increased hazard ratios (HRs) for all-cause mortality and cardiovascular mortality. Neither depression nor low global cognition was associated with cancer mortality. A significant interaction between depression and low global cognition was observed for cardiovascular mortality (P for interaction = 0.037).
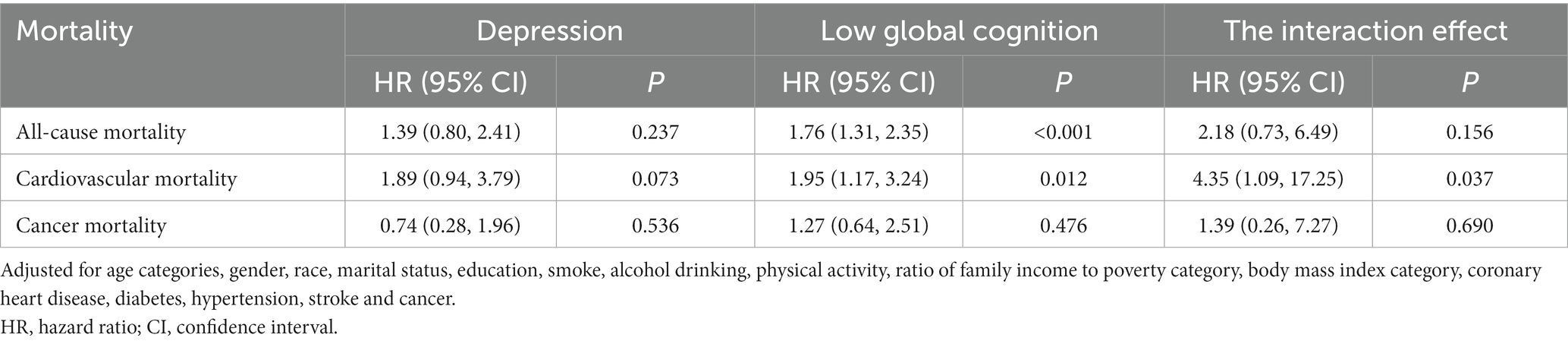
Table 4. Hazard ratios of depression and low global cognition for all-cause mortality, cardiovascular mortality and cancer mortality.
Weighted Kaplan–Meier survival curves of participants with different status of depression and low global cognition are shown in Figure 1. Among four groups, the coexistence of depression and low global cognition group fared the worst for survival. The joint effects of depression and low global cognition on all-cause mortality, cardiovascular mortality, and cancer mortality are shown in Table 5. Compared with normal groups, low global cognition only and coexistence of depression and low global cognition had higher HRs for all-cause mortality and the HRs were highest in the coexistence of depression and low global cognition group. The HRs for cardiovascular mortality were highest in the coexistence of depression and low global cognition group. No such associations were observed for cancer mortality. Further adjusting for disability in ADLs, IADLs, LSA, LEM, and GPA attenuated these associations, but the HRs for all-cause mortality and cardiovascular mortality remained the highest in the coexistence of depression and low global cognition group.
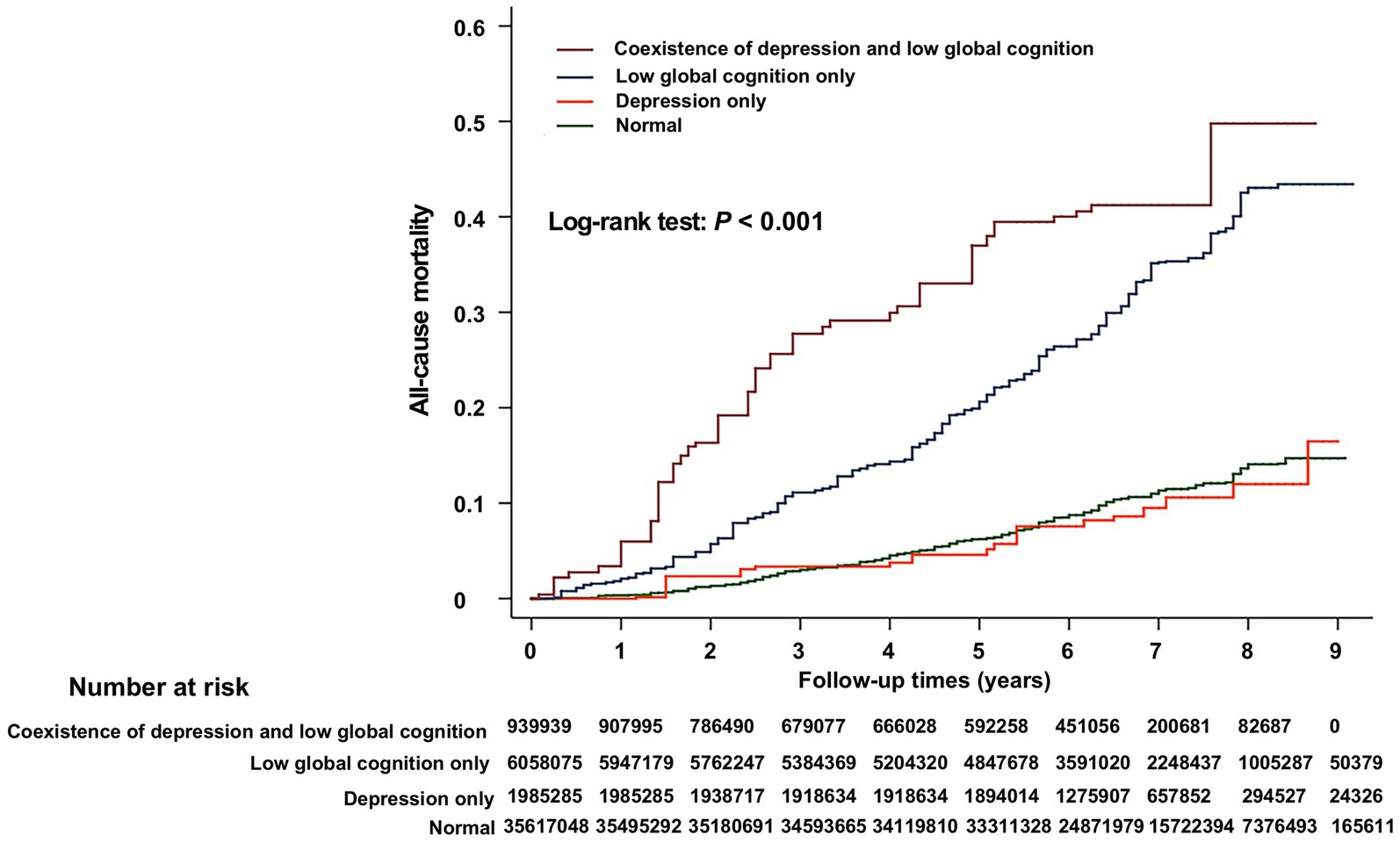
Figure 1. Weighted Kaplan–Meier survival curves of participants with different status of depression and low global cognition. The numbers in the figure are the weighted numbers of at-risk participants.
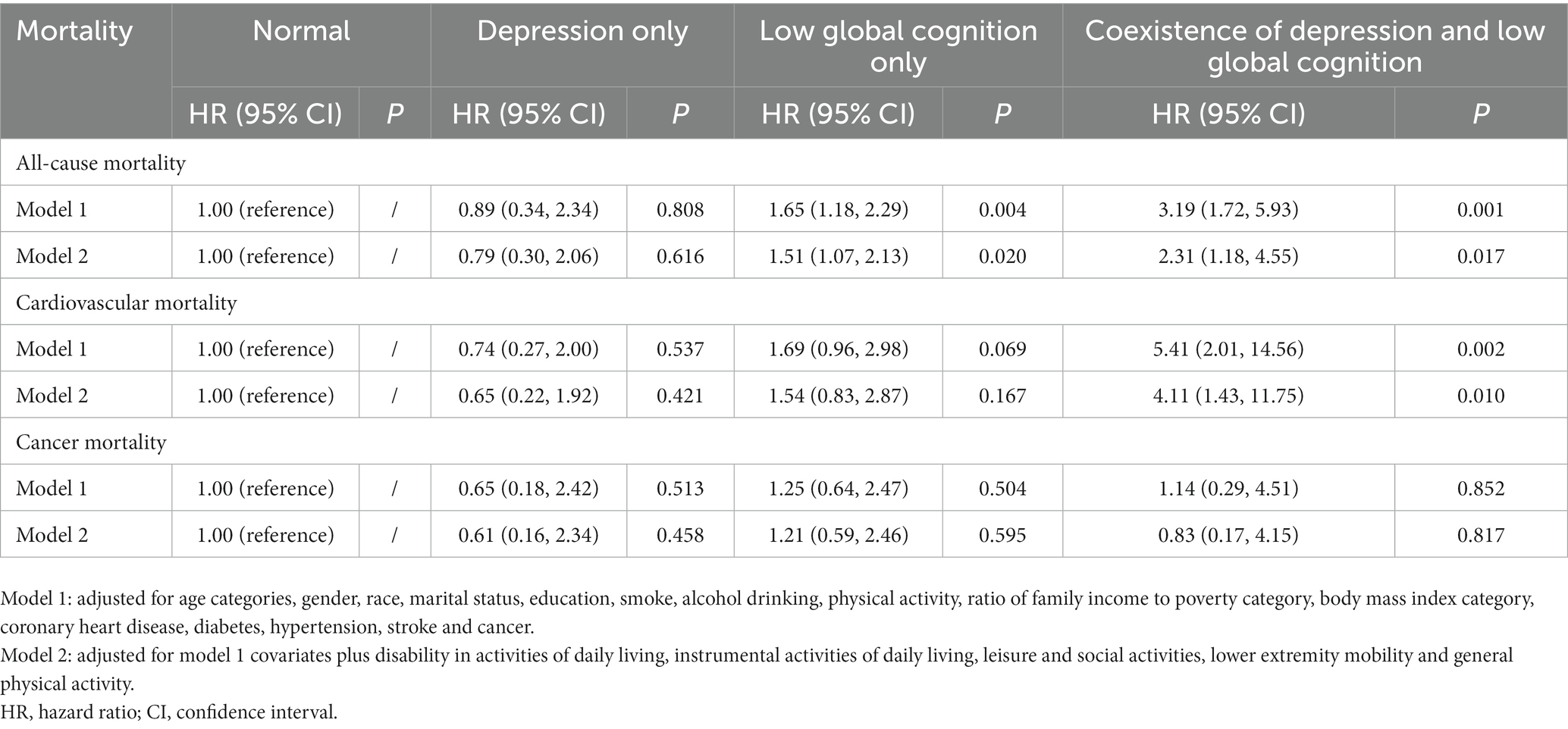
Table 5. Joint effects of depression and low global cognition on all-cause mortality, cardiovascular mortality and cancer mortality.
The study provides the finding that interactions between depression and low global cognition existed for disability in IADLs and LEM, and cardiovascular mortality. Compared with normal participants, participants with both depression and low global cognition had the highest risk of disability in ADLs, IADLs, LSA, LEM, and GPA. Besides, participants with both depression and low global cognition also had the highest risk of all-cause mortality and cardiovascular mortality, and these associations remained after adjusting for disability in ADLs, IADLs, LSA, LEM, and GPA.
Investigating the combined associations of depression and low global cognition with functional disability and mortality is critical because coexistence of depression and cognitive impairment is common in older adults. The prevalence of coexistence of mild cognitive impairment and depression was 9.1% in older patients with diabetes and 5.1% in older Japanese (Hidaka et al., 2012; Gorska-Ciebiada et al., 2014). Hence, elucidating the joint effects of depression and cognitive impairment on functional disability and mortality is especially helpful for old adults to realize the adverse effect of the coexistence of depression and cognitive impairment, which may prompt them to adopt efficient intervention. Our finding also highlighted the importance of early screening of depression and cognitive impairment in older adults.
The combined associations of depression and low global cognition with functional disability are debated (Mehta et al., 2002; Raji et al., 2002; Li and Conwell, 2009; Olaya et al., 2016; Jarvis et al., 2019; Wu, 2021). Previous studies observed an interaction effect between depressive syndrome and cognitive impairment for disability in IADLs and lower body function (Raji et al., 2002; Li and Conwell, 2009), while other studies found no interaction effect existed (Mehta et al., 2002; Wu, 2021). A study conducted in older adults also found interaction effects between depression and cognitive impairment for disability, but the direction of the interaction was different (Olaya et al., 2016). They found that the risk of disability was higher in participants with depression and good cognitive function than participants with depression and poor cognitive function. Through data analyzed from the national survey, the present study further supported the view that interactions between depression and low global cognition existed for disability in IADLs and LEM. Although no such significant interaction was observed for disability in ADLs, LSA, and GPA, the directions of interaction terms were all positive. Participants with both depression and low global cognition had the highest risk of disability in ADLs, IADLs, LSA, LEM, and GPA. The reason for these non-significant results might be that the sample size of this study is relatively small.
The present study also found that participants with both depression and low global cognition had the highest risk of all-cause mortality and cardiovascular mortality, and interaction between depression and cognitive impairment existed for cardiovascular mortality. Our finding was consistent with some previous studies (Mehta et al., 2003; Georgakis et al., 2016). Considering the combined associations of depression and low global cognition with functional disability and the effect of functional disability on mortality (Murad et al., 2015; Wu et al., 2016), we further explored whether the joint effects of depression and cognitive impairment on mortality were influenced by their effects on functional disability. We found that the HRs of all-cause mortality and cardiovascular mortality remained highest in participants with both depression and low global cognition after adjusting for disability in ADLs, IADLs, LSA, LEM, and GPA, which suggested that the combined effects of depression and cognitive impairment on mortality were independent of functional disability. Our finding suggested that interventions might be needed for older participants with both depression and cognitive impairment in preventing functional disability and premature death.
The reason why interactions between depression and low global cognition existed for IADLs disability, LEM disability, and cardiovascular mortality might be complicated. Depression might lead old adults with cognitive impairment unwilling to engage in physical activity, receive medical treatment, and adopt healthy lifestyles (Raji et al., 2002; Brummett et al., 2009; Li and Conwell, 2009; Jarvis et al., 2019), which may further increase the risk of IADLs disability, LEM disability, and cardiovascular mortality. In addition, older adults with cognitive impairment were more likely to have the poor neurological function, which was closely related to functional disability and cardiovascular mortality. Studies thought that good emotion might be helpful in recovering neurological function and slowing the decline in cognitive performance (Matsunaga et al., 2008; Santos et al., 2013; Stegemoller, 2014; Jarvis et al., 2019). These findings suggested that except for the positive effect itself, good emotion may further reduce the risk of functional disability and cardiovascular mortality by attenuating the adverse impact of cognitive impairment on functional disability and cardiovascular mortality.
We examined the interactions between depression and low global cognition for IADLs disability, LEM disability, and cardiovascular mortality in different age groups, and we only observed significant interactions between depression and low global cognition for disability in LEM in participants aged 80 and above (data not shown). These results should be interpreted in caution because the numbers of participants in different age groups were small in the present study. Further studies with large sample size were needed to determine whether age might influence the interactions between depression and low global cognition for disability in IADLs and LEM, and cardiovascular mortality.
Several strengths existed in the present study. First, this study evaluated several domains of functional disability, and explored the separate and combined associations of depression and low global cognition with each domain of functional disability at the same time. Second, participants of this study were from a national representative survey. Third, a series of covariates were considered in the regression models.
This study has several limitations. First, the causality of depression and cognitive impairment with functional disability was unable to clarify due to the cross-sectional design. Second, the evaluations of depression, cognitive impairment, and functional disability were based on questionnaire survey, which means recall bias might exist in this study. Third, the sample size of this study was relatively small. Fourth, the outbreak of covid19 occurred at the end of the 2019, which might influence the combined associations of depression and cognitive impairment with mortality.
In conclusion, participants with both depression and low global cognition were more likely to have functional disability, and had the highest risk of all-cause mortality and cardiovascular mortality. Interactions between depression and low global cognition existed for IADLs disability, LEM disability, and cardiovascular mortality. More studies are needed to further explore the associations of depression and low global cognition with functional disability and mortality.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the National Center for Health Statistics Research Ethics Review Board. The patients/participants provided their written informed consent to participate in this study.
SH, YG, and DG designed the study. SH analyzed the data and wrote the manuscript. YG and DG revised the manuscript and supervised the study. All authors read and approved the final version of the manuscript.
The present study was supported by grants from the Zhejiang Provincial Natural Science Foundation of China (LQ21C110001), the National Natural Science Foundation of China (82100904), and the Construction Fund of Key Medical Disciplines of Hangzhou (No. OO20200055).
We thank the National Center for Health Statistics (NCHS) of the Center for Disease Control (CDC) and Prevention, and all staffs and participants of the National Health and Nutrition Examination Survey. The authors thank Ziyang Wang (Carnegie Mellon University) for critical proofreading and editing of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Arfken, C. L., Lichtenberg, P. A., and Tancer, M. E. (1999). Cognitive impairment and depression predict mortality in medically ill older adults. J. Gerontol. A Biol. Sci. Med. Sci. 54, M152–M156. doi: 10.1093/gerona/54.3.M152
Brody, D. J., Kramarow, E. A., Taylor, C. A., and McGuire, L. C. (2019). Cognitive performance in adults aged 60 and over: National Health and nutrition examination survey, 2011-2014. Natl. Health Stat Rep. 126, 1–23.
Brummett, B. H., Morey, M. C., Boyle, S. H., and Mark, D. B. (2009). Prospective study of associations among positive emotion and functional status in older patients with coronary artery disease. J. Gerontol. B Psychol. Sci. Soc. Sci. 64, 461–469. doi: 10.1093/geronb/gbp041
Cosiano, M. F., Jannat-Khah, D., Lin, F. R., Goyal, P., McKee, M., and Sterling, M. R. (2020). Hearing loss and physical functioning among adults with heart failure: data from NHANES. Clin. Interv. Aging 15, 635–643. doi: 10.2147/CIA.S246662
Georgakis, M. K., Papadopoulos, F. C., Protogerou, A. D., Pagonari, I., Sarigianni, F., Biniaris-Georgallis, S. I., et al. (2016). Comorbidity of cognitive impairment and late-life depression increase mortality: results from a cohort of community-dwelling elderly individuals in rural Greece. J. Geriatr. Psychiatry Neurol. 29, 195–204. doi: 10.1177/0891988716632913
Gorska-Ciebiada, M., Saryusz-Wolska, M., Ciebiada, M., and Loba, J. (2014). Mild cognitive impairment and depressive symptoms in elderly patients with diabetes: prevalence, risk factors, and comorbidity. J. Diabetes Res. 2014:179648, 1–7. doi: 10.1155/2014/179648
Hale, J. M., Schneider, D. C., Gampe, J., Mehta, N. K., and Myrskyla, M. (2020). Trends in the risk of cognitive impairment in the United States, 1996-2014. Epidemiology 31, 745–754. doi: 10.1097/EDE.0000000000001219
Hidaka, S., Ikejima, C., Kodama, C., Nose, M., Yamashita, F., Sasaki, M., et al. (2012). Prevalence of depression and depressive symptoms among older Japanese people: comorbidity of mild cognitive impairment and depression. Int. J. Geriatr. Psychiatry 27, 271–279. doi: 10.1002/gps.2715
Huang, G., and Ren, G. (2022). Interaction between omega-6 fatty acids intake and blood cadmium on the risk of low cognitive performance in older adults from National Health and nutrition examination survey (NHANES) 2011-2014. BMC Geriatr. 22:292. doi: 10.1186/s12877-022-02988-7
Jarvis, J. M., Downer, B., Baillargeon, J., Khetani, M., Ottenbacher, K. J., and Graham, J. E. (2019). The modifying effect of positive emotion on the relationship between cognitive impairment and disability among older Mexican Americans: a cohort study. Disabil. Rehabil. 41, 1491–1498. doi: 10.1080/09638288.2018.1432080
Kroenke, K., Spitzer, R. L., and Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Kuo, H. K., Leveille, S. G., Yu, Y. H., and Milberg, W. P. (2007). Cognitive function, habitual gait speed, and late-life disability in the National Health and nutrition examination survey (NHANES) 1999-2002. Gerontology 53, 102–110. doi: 10.1159/000096792
Li, L. W., and Conwell, Y. (2009). Effects of changes in depressive symptoms and cognitive functioning on physical disability in home care elders. J. Gerontol. A Biol. Sci. Med. Sci. 64, 230–236. doi: 10.1093/gerona/gln023
Matsunaga, M., Isowa, T., Kimura, K., Miyakoshi, M., Kanayama, N., Murakami, H., et al. (2008). Associations among central nervous, endocrine, and immune activities when positive emotions are elicited by looking at a favorite person. Brain Behav. Immun. 22, 408–417. doi: 10.1016/j.bbi.2007.09.008
Mehta, K. M., Yaffe, K., and Covinsky, K. E. (2002). Cognitive impairment, depressive symptoms, and functional decline in older people. J. Am. Geriatr. Soc. 50, 1045–1050. doi: 10.1046/j.1532-5415.2002.50259.x
Mehta, K. M., Yaffe, K., Langa, K. M., Sands, L., Whooley, M. A., and Covinsky, K. E. (2003). Additive effects of cognitive function and depressive symptoms on mortality in elderly community-living adults. J. Gerontol. A Biol. Sci. Med. Sci. 58, M461–M467. doi: 10.1093/gerona/58.5.M461
Morris, J. C., Heyman, A., Mohs, R. C., Hughes, J. P., van Belle, G., Fillenbaum, G., et al. (1989). The consortium to establish a registry for Alzheimer's disease (CERAD). Part I. clinical and neuropsychological assessment of Alzheimer's disease. Neurology 39, 1159–1165.
Murad, K., Goff, D. C. Jr., Morgan, T. M., Burke, G. L., Bartz, T. M., Kizer, J. R., et al. (2015). Burden of comorbidities and functional and cognitive impairments in elderly patients at the initial diagnosis of heart failure and their impact on Total mortality: the cardiovascular health study. JACC Heart Fail. 3, 542–550. doi: 10.1016/j.jchf.2015.03.004
Olaya, B., Moneta, M. V., Koyanagi, A., Lara, E., Miret, M., Ayuso-Mateos, J. L., et al. (2016). The joint association of depression and cognitive function with severe disability among community-dwelling older adults in Finland, Poland and Spain. Exp. Gerontol. 76, 39–45. doi: 10.1016/j.exger.2016.01.010
Parsons, V. L., Moriarity, C., Jonas, K., Moore, T. F., Davis, K. E., and Tompkins, L.. (2014). Design and Estimation for the National Health Interview Survey, 2006-2015. Vital Health Stat 2. pp. 1–53.
Polyakova, M., Sonnabend, N., Sander, C., Mergl, R., Schroeter, M. L., Schroeder, J., et al. (2014). Prevalence of minor depression in elderly persons with and without mild cognitive impairment: a systematic review. J. Affect. Disord. 152-154, 28–38. doi: 10.1016/j.jad.2013.09.016
Prevention CfDCa. (n.d.). National Health and Nutrition Examination Survey. Available at: https://wwwcdcgov/nchs/nhanes/index.htm.
Raji, M. A., Ostir, G. V., Markides, K. S., and Goodwin, J. S. (2002). The interaction of cognitive and emotional status on subsequent physical functioning in older mexican americans: findings from the Hispanic established population for the epidemiologic study of the elderly. J. Gerontol. A Biol. Sci. Med. Sci. 57, M678–M682. doi: 10.1093/gerona/57.10.M678
Santos, N. C., Costa, P. S., Cunha, P., Cotter, J., Sampaio, A., Zihl, J., et al. (2013). Mood is a key determinant of cognitive performance in community-dwelling older adults: a cross-sectional analysis. Age (Dordr.) 35, 1983–1993. doi: 10.1007/s11357-012-9482-y
Scult, M. A., Paulli, A. R., Mazure, E. S., Moffitt, T. E., Hariri, A. R., and Strauman, T. J. (2017). The association between cognitive function and subsequent depression: a systematic review and meta-analysis. Psychol. Med. 47, 1–17. doi: 10.1017/S0033291716002075
Statistics NCfH. (2021). The Linkage of National Center for Health Statistics Survey Data to the National Death Index–2019 Linked Mortality File (LMF): Linkage Methodology and Analytic Considerations. Hyattsville, Maryland.
Steffens, D. C., Fisher, G. G., Langa, K. M., Potter, G. G., and Plassman, B. L. (2009). Prevalence of depression among older Americans: the aging, demographics and memory study. Int. Psychogeriatr. 21, 879–888. doi: 10.1017/S1041610209990044
Stegemoller, E. L. (2014). Exploring a neuroplasticity model of music therapy. J. Music. Ther. 51, 211–227. doi: 10.1093/jmt/thu023
Strauss, E., Sherman, E. M., and Spreen, O.. (2006). A Compendium of Neuropsychological Tests: Administration, Norms and Commentary. 3rd Edn. New York: Oxford University Press.
WHO. (2001). International Classification of Functioning, Disability and Health (ICF). Geneva: World Health Organization.
Wu, C. (2021). The mediating and moderating effects of depressive symptoms on the prospective association between cognitive function and activities of daily living disability in older adults. Arch. Gerontol. Geriatr. 96:104480. doi: 10.1016/j.archger.2021.104480
Wu, L. W., Chen, W. L., Peng, T. C., Chiang, S. T., Yang, H. F., Sun, Y. S., et al. (2016). All-cause mortality risk in elderly individuals with disabilities: a retrospective observational study. BMJ Open 6:e011164. doi: 10.1136/bmjopen-2016-011164
Yang, R., Xu, D., Wang, H., and Xu, J. (2021). Longitudinal trajectories of physical functioning among Chinese older adults: the role of depressive symptoms, cognitive functioning and subjective memory. Age Ageing 50, 1682–1691. doi: 10.1093/ageing/afab135
Yochim, B. P., Lequerica, A., MacNeill, S. E., and Lichtenberg, P. A. (2008). Cognitive initiation and depression as predictors of future instrumental activities of daily living among older medical rehabilitation patients. J. Clin. Exp. Neuropsychol. 30, 236–244. doi: 10.1080/13803390701370006
Keywords: depression, cognitive impairment, functional disability, mortality, older adults
Citation: Han S, Gao Y and Gan D (2023) The combined associations of depression and cognitive impairment with functional disability and mortality in older adults: a population-based study from the NHANES 2011–2014. Front. Aging Neurosci. 15:1121190. doi: 10.3389/fnagi.2023.1121190
Received: 11 December 2022; Accepted: 03 April 2023;
Published: 04 May 2023.
Edited by:
Franca Rosa Guerini, Fondazione Don Carlo Gnocchi Onlus (IRCCS), ItalyReviewed by:
Nadine Correia Santos, University of Minho, PortugalCopyright © 2023 Han, Gao and Gan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yue Gao, Z3k5ODIxQHNpbmEuY29t; Da Gan, Z2FuZGFAemp1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.