- Department of Epidemiology and Medical Statistics, Xiangya School of Public Health, Central South University, Changsha, China
Objectives: Studies have shown that the frequent participation of the elderly in cognitive stimulation activities is associated with a reduced risk of dementia, but the prospective evidence of this association is limited.
Methods: We used data from a prospective cohort study of the Chinese Longitudinal Healthy Longevity Survey (CLHLS), and included 11,821 community-living Chinese individuals aged 65 years or older at 2008 baseline who were free of dementia, and were followed up every 2–3 years until 2018. Cox proportional hazards models were applied to generate the hazard ratios (HRs) and 95% confidence intervals (CIs) for analyzing the associations between the frequency of playing cards/mahjong and the incidence of dementia.
Results: A total of 821 participants were diagnosed with dementia during the 10-year follow-up. The average age of patients with dementia and non dementia were 89 and 90 years old, respectively. Compared with participants who rarely or never played cards/mahjong, participants who played cards/mahjong almost every day had a significantly lower risk of dementia (HR = 0.63; 95%CI, 0.42–0.95) after the multivariable-adjusted model. Similar results were observed in subgroup analyses based on sex (male: HR = 0.52, 0.28–0.96; female: HR = 0.62, 0.36–0.98), age (<85years: HR = 0.55, 0.32–0.89), regularly exercise (yes: HR = 0.44, 0.28–0.87) and MMSE score [above median (25): HR = 0.66, 0.41–0.92].
Conclusions: Playing cards/mahjong in the elderly may contribute to reducing the risk of dementia.
Introduction
Dementia, as a central nervous degenerative disease in middle-aged and older adults, can cause progressive cognitive impairment and behavioral damage, and often causes great pain to the elderly over 65 years old all over the world (Li et al., 2015; Charlson et al., 2016; GBD 2016 Dementia Collaborators, 2019). With the considerable rise in life expectancy and the aggravation of the aging process, the number of individuals with dementia is increasing. An estimated population of more than 46 million people worldwide suffered from dementia in 2016. The number is expected to exceed 130 million by 2050 (GBD 2016 Dementia Collaborators, 2019), and Chinese dementia patients account for about 25% of the total number of dementia patients in the world (Alzheimer’s Disease International, 2015). Because dementia cannot be cured, it will bring a huge burden to the country, healthcare professionals, and family members. Therefore, it is necessary to explore some effective methods to prevent dementia in the elderly and delay the onset of the disease.
As we all know, mahjong and cards are very popular in China, and they are also one of the favorite leisure and entertainment activities for the elderly. Previous studies conducted in North America and Europe (Wilson et al., 2002a, b; Akbaraly et al., 2009; Paillard-Borg et al., 2009; Yates et al., 2016) showed that the active participation of the elderly in leisure and recreational activities, especially intellectual activities, such as reading, playing chess or playing cards, can improve cognitive reserve, protect and restore cognitive function, and help reduce the risk of dementia in the elderly (Fratiglioni et al., 2004; Valenzuela et al., 2007; Cheng, 2016; Nelson et al., 2021). However, researches on this aspect are still scarce in China (Lee et al., 2018), and relevant issues are worth exploring. Those who often actively participate in intellectual activities usually pay more attention to health and have a healthier lifestyle, such as regular exercise, a balanced diet and less smoking. These factors have been shown to be beneficial in preventing dementia (Lovden et al., 2013; Di Marco et al., 2014; Hussenoeder and Riedel-Heller, 2018; Lee et al., 2019). Whether participation in intellectual activities, particularly mahjong/cards in China, can prevent and delay the onset of dementia independently of these adverse lifestyles remains to be determined. Hence, We used the 10-year follow-up data of the Chinese Longitudinal Healthy Longevity Survey (CLHLS) for individuals aged 65 and above (Gu et al., 2017) to investigate the associations between the frequency of playing cards/mahjong and dementia. The long interval between the assessment of exposure factors and the diagnosis of dementia may make us more confident about the time effect and causality of this association (Scarmeas and Stern, 2003).
Our study objectives were to estimate the hazard ratios (HRs) for dementia from the different frequencies of playing cards/mahjong, using never playing cards/mahjong as a reference; estimated dementia risk across age, sex, regular exercise status, and the Mini-Mental State Examination (MMSE) score stratifications; to ensure the stability and reliability of our results, we conducted sensitivity analysis by excluding participants who were MMSE scores <18 at baseline, further excluding participants suffering from epilepsy or stroke at baseline, and participants suffering from dementia during the first year of follow-up in turn.
Methods
Study design and participants
The CLHLS study is an ongoing, population-based, prospective cohort study that was conducted in 1998 and randomly selected half of the counties or cities in 22 of 31 provinces in China. These areas include approximately 85% of the total Chinese population (National Bureau of Statistics, 2012). Our study analysis selects data from 2008 to 2018 waves and mainly collects information on the health status and quality of life of older adults individuals aged 65 and older. Details of the study design and methods have been described elsewhere (Deng et al., 2020).
The CLHLS data were collected by trained staff through face-to-face interviews with the older adults themselves or their relatives or caregivers. After evaluation, the data quality and the report information reliability of the CLHLS are reasonably good (Zeng et al., 2008). A total of 16,954 Chinese elderly over 65 years old participated in the 2008 baseline survey, which included rich information about playing cards/mahjong and dementia. After excluding cases with missing information on key variables, with dementia at baseline and loss to follow-up, the final 11,821 participants available were included for the analysis of the association of frequency of playing cards/mahjong and dementia. The full screening process of research participants is presented in Figure 1.
Assessment of frequency of playing cards/mahjong
To obtain the data on playing mahjong/cards status at the baseline, we invited participants themselves or a close relative of the interviewee to answer some questions, such as “do you now perform the following activities regularly?”, with options of “almost every day”, “not every day, but at least once a week”, “not every week, but at least once a month”, “not every month, but sometimes”, and “rarely or never”. Based on the frequency of playing mahjong/cards in the 2008 baseline survey, Finally, we classified four types of mahjong/card players. Those who “not every month, but sometimes” or “never” played mahjong/cards at the baseline were classified as “rarely or never players”, which was the reference category in the regression analyses.
Identification of dementia
The outcome of this study was incident dementia in the following up to 10 years. The identification of individuals with dementia came from reports through family members or caregivers, diagnosed by qualified medical institutions, or taking dementia treatment drugs. For those participants who were dead during follow-up, we asked their family members or caregivers whether they had dementia before death.
Evaluation of other variables
To control the potential confoundings, covariates, such as socio-demographic information, lifestyle factors, and health status, were included in our analyses. Socio-demographic variables included age (continuous), sex, education (no schooling received/1 year or more), household income [low (<10,000 RMB); middle (10,000–30,000 RMB); high (>30,000 RMB)], marital status (married/unmarried), living with household members (yes/no). Lifestyle factors included smoking status (current smoker/current non-smoker), drinking status (current drinker/current non-drinker), and regular exercise (yes/no). Health status information included body mass index (BMI) [underweight (<18.5), normal (18.5–23.9), overweight (24–27.9), obese (≥28)] (Lv et al., 2018). The identification of individuals with hypertension or diabetes came from reports through family members or caregivers, diagnosed by qualified medical institutions, or taking hypertension or diabetes treatment drugs. Because of the close relationship between cognitive function and dementia (Petersson and Philippou, 2016), we carefully analyzed the role of cognitive function in dementia. Cognitive function was measured by the Chinese version of the Mini-Mental State Examination (MMSE) in the CLHLS. The validity and reliability of the Chinese MMSE have been verified (Zeng et al., 2017). The MMSE score ranged from 0 to 30, and a higher score indicated better cognitive function (Yi and Vaupel, 2002; Lv et al., 2019). A score below 18 was considered to be a cognitive impairment among older adults in China (Hao et al., 2018; Mao et al., 2020).
Statistical analysis
Baseline characteristics were described as medians and interquartile ranges (IQR) for continuous variables (not normally distributed), the count and percentage for categorical variables according to different groups of playing mahjong/cards frequency and with and without incident dementia. The χ2 test was used for comparing differences among groups in categorical variables and the Kruskal-Wallis H test or the Mann-Whitney test in continuous variables. We calculated crude incidence rates (IR; per 1,000 person-years) of dementia across categories of playing cards/mahjong frequency. The person-years were calculated by summing each participant’s contribution to follow-up time (from baseline to the year of assessment when the participant was found to have dementia, or to the year of the last assessment if the participant remained free of dementia). All analyses were performed using R version 4.0.5 (R Foundation for Statistical Computing), and all reported P < 0.05 (2-tailed) were considered statistically significant.
Cox proportional hazards models were applied to generate the hazard ratios (HRs) and 95% confidence intervals (CIs) for analyzing the associations between the frequency of playing cards/mahjong and the risk of dementia. Initially, we constructed models without any adjusted covariates (unadjusted model), additionally adjusted only for age and sex (age and sex-adjusted model), and further adjusted for education, household income, marital status, smoking status, drinking status, regular exercise, BMI, living with family members, history of hypertension and diabetes and MMSE score (multivariable-adjusted model).
To further explore the influence of sex, age, regular exercise, and MMSE score (median) on the association of the frequency of playing cards/mahjong with the risk of dementia, we conducted subgroup analyses. To ensure the stability and reliability of our study results and exclude more interference, we carried out sensitivity analysis, first excluding participants who were MMSE scores <18 at baseline, then further excluding participants who suffer from epilepsy or stroke at baseline, and finally excluding dementia that occurred during the first year of follow-up.
Results
Participant characteristics
A total of 11,821 participants were included in our study (Figure 1). As shown in Table 1, at baseline, compared with other groups, those participants who rarely or never played cards/mahjong were older, with a median (IQR) age of 90 (81–98) years, more female (60.1%), lower married rate (26.3%), and lower MMSE score (24 points). With the increasing frequency of playing cards/mahjong (divided into four groups), the proportion of educated (34.0%, 42.9%, 46.2%, and 49.2%, respectively) smokers (34.0%, 42.9%, 46.2%, and 49.2%, respectively), drinkers (34.0%, 42.9%, 46.2%, and 49.2%, respectively) and regular exercisers (34.0%, 42.9%, 46.2%, and 49.2%, respectively) also increased among participants (shown in Table 1). There was no significant difference in the proportion of living with family members and suffering from hypertension and diabetes among the groups. A total of 821 participants developed incident dementia during the 10-year follow-up. As summarized in Table 1, those who developed incident dementia were older [age: median (IQR), 90 (82–96)] than those who remained free of dementia [age: median (IQR), 89 (79–97)], and were predominantly female [530 (64.6%) vs. 6,248 (56.8%)]; with a significantly higher percentage of uneducated [629 (76.6%) vs. 8,013 (72.9%)], married, smokers, drinkers, and less MMSE score, with a higher prevalence of hypertension, diabetes.
Table 1. Characteristics of the study participants according to the frequency of playing cards/mahjong and Dementia status at end of follow-up at baseline.
Association of playing cards/mahjong with risk of dementia
Overall, with the increase in playing cards/mahjong frequency, the crude rate of dementia events decreased gradually. The incidence rate (95%CI) per 1,000 person-year in the rarely or never group, sometimes, at least once for a month group, regularly, at least once for a weekly group, and the almost everyday group were 16.4 (15.3–17.6), 8.8 (6.2–12.4), 8.2 (5.4–12.5) and 6.7 (4.5–9.9), respectively (Table 2).
Table 2. Associations between frequency of playing card/mahjong and dementia for Chinese older adults.
In Cox proportional hazards models reported in Table 2; the corresponding unadjusted HR (95%CI) for dementia was significantly lower in those who almost every day played cards/mahjong (HR = 0.38; 95%CI, 0.25–0.57) than those who rarely or never played cards/mahjong. It was associated with the risk of dementia after adjusting for sex and age (HR = 0.55; 95%CI, 0.36–0.82). It remained significant after further adjusting for additional education, household income, marital status, smoking status, drinking status, regular exercise, BMI, living with family members, hypertension, diabetes, and MMSE score (HR = 0.63; 95%CI, 0.42–0.95). There was no clear evidence of an association between the other two groups.
Subgroup analysis
We performed subgroup analysis by sex, age, regular exercise, and MMSE score median. In the sex-stratified analysis, the risk of dementia in almost everyday playing cards/mahjong group (male: HR = 0.52, 0.28–0.96; female: HR = 0.62, 0.36–0.98) was lower than that in other the frequency of playing cards/mahjong groups. In age-stratified analysis, the risk of dementia in almost everyday playing cards/mahjong group in less than 85 years (HR = 0.55, 0.32–0.89) was lower than in more than 85 years (HR = 0.87, 0.45–1.28). Similar pattern was observed in regular exercise-stratified analysis (yes: HR = 0.44, 0.28–0.87), and MMSE score-stratified analysis [above median (25): HR = 0.66, 0.41–0.92] (Figure 2). There is no evidence that there is an interaction between whether the elderly play mahjong/cards and sex, age, regular exercise, and MMSE score median groups.
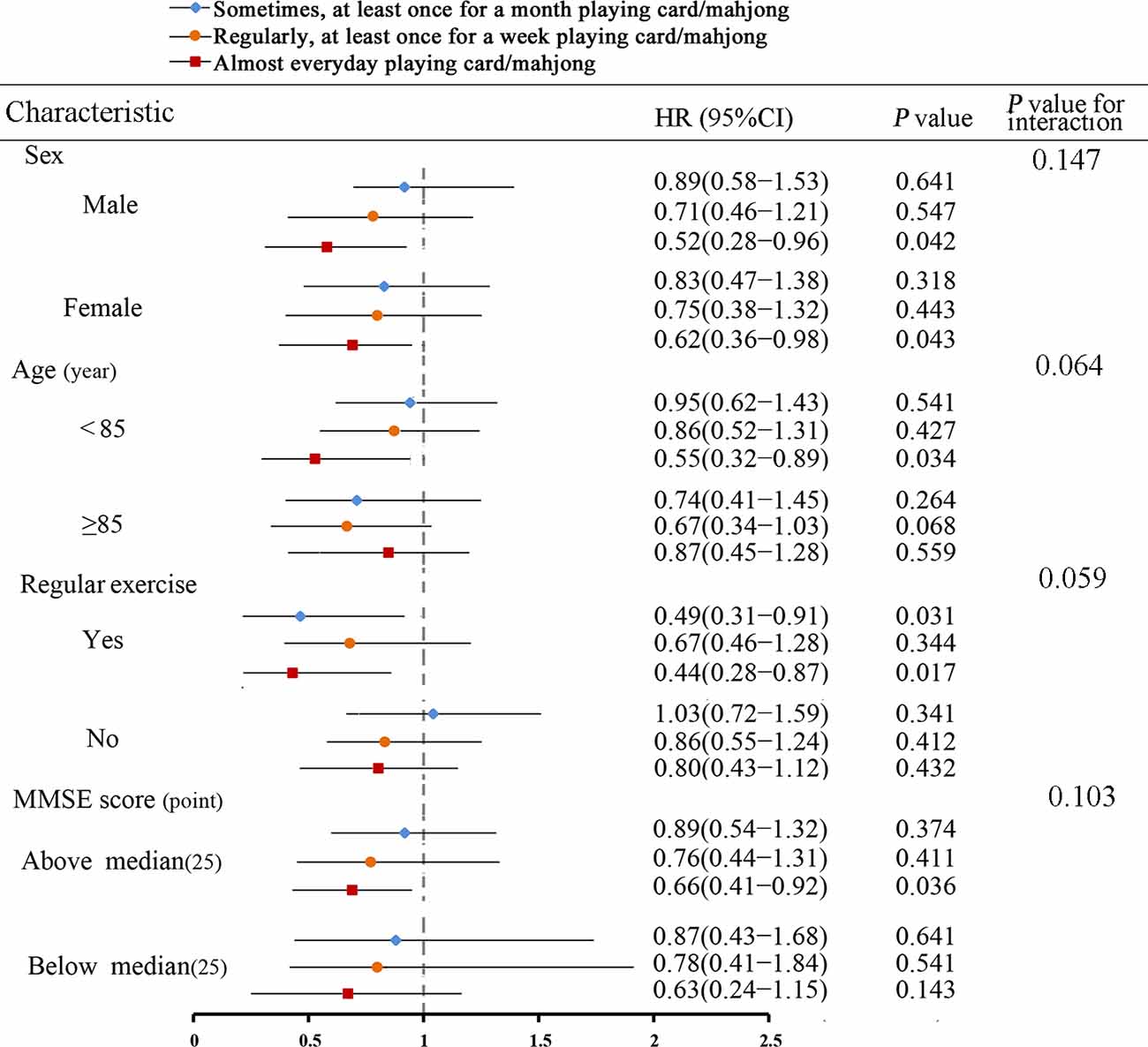
Figure 2. Hazard ratios (HRs) and confidence intervals (CIs) for the association between frequency of playing cards/mahjong and dementia, with rarely or never playing cards/mahjong as a reference group, by baseline sex, age, regular exercise, and MMSE score, adjusting for baseline age, sex, education, household income, marital status, smoking status, drinking status, exercise, BMI, living with family members, hypertension, diabetes, and MMSE score.
Sensitivity analysis
The results of the sensitivity analyses are presented in Table 3. We still used three models (unadjusted, age- and sex-adjusted, multivariable-adjusted) to analyze the association of the frequency of playing cards/mahjong with the risk of dementia. The unadjusted, age- and sex-adjusted, and multivariable-adjusted models excluded participants who were MMSE scores <18 at baseline, further excluding participants who suffer from epilepsy or stroke at baseline, or additionally excluding dementia that occurred during the first year of follow-up did not make a big difference to the original results.
Discussion
This extensive community-based, prospective cohort study showed that more frequency of playing cards/mahjong was associated with a significant reduction in the risk of dementia among older adults individuals aged 65 and older. Furthermore, we found that the protective association was stronger for older adults who reported playing cards/mahjong almost every day with regular exercise than those without regular exercise. We did not find any significant difference in age, sex, and MMSE score median, and further sensitivity analysis yielded no substantial changes in our findings after adjusting confounding factors.
The present findings align with several previous studies that active participation in stimulating intellectual activities (such as playing cards or checkers), especially among older adults, is associated with better cognitive functioning (Leung et al., 2010). In addition, some studies had also found that more frequently playing stimulating intellectual games (such as cards, bingo, chess, mahjong, and crossword puzzle) were associated with a decreased risk of dementia (Wang et al., 2006; Qiu et al., 2019; Sommerlad et al., 2020). The reasons why these stimulating intellectual games can reduce the risk of dementia may be explained by the fact that playing cards or mahjong (game activities welcomed by the Chinese circle) is a strong and comprehensive stimulating activity in cognitive domains (involving attention, reasoning, memory, and initiative capacity; Marioni et al., 2015). Some studies have found that social isolation and loneliness are also risk factors for dementia (Shankar et al., 2013; Rafnsson et al., 2020; Shen et al., 2022). Meanwhile, playing cards or mahjong is a group entertainment and can not only promote communication between the elderly but also give them good social support and emotional comfort, which is also proven to help to reduce the risk of dementia or cognitive impairment (Wang et al., 2012; Raz et al., 2016). However, as we know, many previous studies did not fully consider other confounding factors (such as education level and whether live with family members) and baseline cognitive status, both of which can lead to potentially biased results. Our finding was consistent with a recent prospective study result that active participation in playing cards/mahjong might be in favor of decreasing the risk of dementia in older adults (Lee et al., 2018). However, the study was followed-up for only 3 years, and relevant evidence showed that dementia was considered to develop slowly over many years (Laurin et al., 2001), so the causality of this study’s conclusion was still controversial. Additionally, most studies had incorporated various types of stimulating intellectual activities as independent variables, while our study included playing cards/mahjong as the only factor to explore the independent impact on the risk of dementia in older adults through adjusting as many confounding factors as possible.
Some prospective studies also investigated the relationship between other types of leisure activities (such as social, entertainment and physical) and cognitive decline or dementia, but they did not determine the frequency of social or entertainment participation, or physical activities (Wilson et al., 2002b; Lee et al., 2018; Kim et al., 2021). These results were contrary to the relationship between stimulating intellectual activities and cognitive decline or dementia, but these findings were significant because they showed that the association of cognitive decline or dementia risk reflected mental stimulation rather than nonspecific results of other types of leisure activities. Compared with stimulating intellectual activities, these activities are usually more passive and have less cognitive involvement, so we deduce that stimulating intellectual activities might be more effective than engaging in various nonintellectual leisure activities (such as recreational, social, and physical) in preventing dementia.
There is no consensus on the potential mechanism of stimulating intellectual activities and preventing dementia. One hypothesis is that, frequent participation in cognitively stimulating activities can protect the cognitive function of older adults from decline (Wilson et al., 2000) because repeating some cognitive skills can make neurons more active and less vulnerable to disruption by dementia pathology (Alexander et al., 1997). Another similar view points out that frequent cognitive stimulating activity may strengthen thought processing skills, such as ratiocination, calculation, and perceptual speed, which may be conducive to compensating and resist for age-related decline in other cognitive systems (Beyer et al., 2021). Some studies had explored possible biological mechanisms for the association of cognitively stimulating activities with cognitive function (Stern, 2012). These findings manifested that being mentally active may delay the onset of clinical dementia by improving cognitive reserve. According to cognitive reserve theory in neuroscience, people with a higher level of cognitive reserve can buffer the effects of neuropathology in brain anatomical substrate and function, and also have greater dynamic neural network compensation such that the larger cognitive reserve, the more serious the pathological damage needed to cause functional impairment (Richards and Deary, 2005). A recent study showed that cognitive stimulation can improve functional connectivity between the hippocampus and superior frontal cortex to resist cognitive function decline (Suo et al., 2016). The above findings show that cognitive training may improve cognition, possibly through different neural regulation mechanisms, which can explain our findings that more frequency of playing mahjong/cards lowers the risk of dementia.
Regarding the strengths of this study, it is a community-based, national-wide prospective design, a large sample of over 65 older adults, a relatively long follow-up period with about 3 years of evenly spaced observations per individual, and adjustment for established and potential confounders. Of course, our study also has some limitations. First, our findings only apply to older adults in China. Due to the cognitive function effects of playing cards/mahjong may be different between young and older adults individuals, this effect should be carefully extended to young people. Second, information on covariates and dementia status is collected through self-reported in the form of a questionnaire, thus, recall bias and information bias are possible, and some undiagnosed dementia cases may be omitted, which may affect the research results. Third, As the subjects of our study were older and the number of deaths was as high as 9,318 in the 10-year follow-up period, although we repeatedly confirmed to the family members whether the deceased had been diagnosed with dementia, some family members still did not give a clear response, which made us miss some dementia cases and had a certain impact on the outcome. Fourth we do not control other types of leisure activities. Although this is also important, it does not alter the main results in that frequent playing cards/mahjong is associated with a significantly decreased risk of dementia.
Conclusion
Our study provides evidence that frequently playing cards/mahjong may decrease the risk of dementia among Chinese elderly over 65 years old. Given China’s huge population base and increasing aging population, proper and rational participation of the elderly in this activity could provide a certain degree of social support and emotional comfort.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The datasets supporting this article are publicly available from the project of the CLHLS. The study was approved by the Research Ethics Committee of Peking University (IRB00001052-13074). All study participants or their legal proxy respondents must obtain and sign written informed consent before completing each study questionnaire.
Author Contributions
GT participated in the design, data analysis, and writing of this study. YY provided supervision and guidance at all stages including the analyses. JS, RL, and TZ assisted with drafting the article. YS and GC prepared the manuscript for publication. All authors reviewed and commented on drafts of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The Chinese Longitudinal Healthy Longevity Survey (CLHLS) has been supported by NIA/NIH grants R01 AG023627-01 and P01 AG008761, awarded to Duke University, with Chinese matching support for personnel costs and some local expenses. The CLHLS was supported by funds from the US National Institute on Aging (NIA), the China Natural Science Foundation, the China Social Science Foundation, and the United Nations Fund for Population Activities (UNFPA) and was managed by the Center for Healthy Aging and Development Studies, Peking University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are very grateful to all the participants and all the staff who contributed to the data collection and collation in this study.
References
Akbaraly, T. N., Portet, F., Fustinoni, S., Dartigues, J. F., Artero, S., Rouaud, O., et al. (2009). Leisure activities and the risk of dementia in the elderly: results from the three-city study. Neurology 73, 854–861. doi: 10.1212/WNL.0b013e3181b7849b
Alexander, G. E., Furey, M. L., Grady, C. L., Pietrini, P., Brady, D. R., Mentis, M. J., et al. (1997). Association of premorbid intellectual function with cerebral metabolism in Alzheimer’s disease: implications for the cognitive reserve hypothesis. Am. J. Psychiatry 154, 165–172. doi: 10.1176/ajp.154.2.165
Alzheimer’s Disease International (2015). World Alzheimer Report 2015. The Global Impact of Dementia. An analysis of prevalence, incidence, cost and trends. London: Alzheimer’s Disease International. Available online at: https://www.alzint.org/u/WorldAlzheimerReport2015.tif.
Beyer, L., Meyer-Wilmes, J., Schönecker, S., Schnabel, J., Sauerbeck, J., Scheifele, M., et al. (2021). Cognitive reserve hypothesis in frontotemporal dementia: a FDG-PET study. Neuroimage Clin. 29:102535. doi: 10.1016/j.nicl.2020.102535
Charlson, F. J., Baxter, A. J., Cheng, H. G., Shidhaye, R., and Whiteford, H. A. (2016). The burden of mental, neurological and substance use disorders in China and India: a systematic analysis of community representative epidemiological studies. The Lancet 388, 376–389. doi: 10.1016/S0140-6736(16)30590-6
Cheng, S. T. (2016). Cognitive reserve and the prevention of dementia: the role of physical and cognitive activities. Curr. Psychiatry Rep. 18:85. doi: 10.1007/s11920-016-0721-2
Deng, Y., Gao, Q., Yang, D., Hua, H., Wang, N., Ou, F., et al. (2020). Association between biomass fuel use and risk of hypertension among Chinese older people: a cohort study. Environ Int. 138:105620. doi: 10.1016/j.envint.2020.105620
Di Marco, L. Y., Marzo, A., Muñoz-Ruiz, M., Ikram, M. A., Kivipelto, M., Ruefenacht, D., et al. (2014). Modifiable lifestyle factors in dementia: a systematic review of longitudinal observational cohort studies. J Alzheimers Dis. 42, 119–135. doi: 10.3233/JAD-132225
Fratiglioni, L., Paillard-Borg, S., and Winblad, B. (2004). An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 3, 343–353. doi: 10.1016/S1474-4422(04)00767-7
GBD 2016 Dementia Collaborators (2019). Global, regional and national burden of Alzheimer’s disease and other dementias, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 18, 88–106. doi: 10.1016/S1474-4422(18)30403-4
Gu, D., Feng, Q., Yi, Z. (2017). Chinese Longitudinal Healthy Longevity Study. Available online at: https://cpha.duke.edu/research/chinese-longitudinal-healthy-longevity-survey-clhls.
Hao, Q., Dong, B., Yang, M., Dong, B., and Wei, Y. (2018). Frailty and cognitive impairment in predicting mortality among oldest-old people. Front. Aging Neurosci. 10:295. doi: 10.3389/fnagi.2018.00295
Hussenoeder, F. S., and Riedel-Heller, S. G. (2018). Primary prevention of dementia: from modifiable risk factors to a public brain health agenda? Soc. Psychiatry Psychiatr. Epidemiol. 53, 1289–1301. doi: 10.1007/s00127-018-1598-7
Kim, J., Woo, S. Y., Kim, S., Jang, H., Kim, J., Kim, J., et al. (2021). Differential effects of risk factors on the cognitive trajectory of early- and late-onset Alzheimer’s disease. Alzheimers Res. Ther. 13:113. doi: 10.1186/s13195-021-00857-w
Laurin, D., Verreault, R., Lindsay, J., MacPherson, K., and Rockwood, K. (2001). Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch. Neurol. 58, 498–504. doi: 10.1001/archneur.58.3.498
Lee, A. T. C., Richards, M., Chan, W. C., Chiu, H. F. K., Lee, R. S. Y., Lam, L. C. W., et al. (2018). Association of daily intellectual activities with lower risk of incident dementia among older chinese adults. JAMA Psychiatry 75, 697–703. doi: 10.1001/jamapsychiatry.2018.0657
Lee, H., Kim, D., Lee, W., Kim, H. Y., and Kim, Y. (2019). Preventive approach for overcoming dementia. Arch. Pharm. Res. 42, 647–657. doi: 10.1007/s12272-019-01168-3
Leung, G. T., Fung, A. W., Tam, C. W., Lui, V. W., Chiu, H. F., Chan, W. M., et al. (2010). Examining the association between participation in late-life leisure activities and cognitive function in community-dwelling elderly Chinese in Hong Kong. Int. Psychogeriatr. 22, 2–13. doi: 10.1017/S1041610209991025
Li, N., Zhang, L., Du, W., Pang, L., Guo, C., Chen, G., et al. (2015). Prevalence of dementia-associated disability among Chinese older adults: results from a national sample survey. Am. J. Geriatr. Psychiatry 23, 320–325. doi: 10.1016/j.jagp.2014.06.002
Lovden, M., Xu, W., and Wang, H. X. (2013). Lifestyle change and the prevention of cognitive decline and dementia: what is the evidence? Curr. Opin. Psychiatry 26, 239–243. doi: 10.1097/YCO.0b013e32835f4135
Lv, X., Li, W., Ma, Y., Chen, H., Zeng, Y., Yu, X., et al. (2019). Cognitive decline and mortality among community-dwelling Chinese older people. BMC Med. 17:63. doi: 10.1186/s12916-019-1295-8
Lv, Y. B., Liu, S., Yin, Z. X., Gao, X., Kraus, V. B., Mao, C., et al. (2018). Associations of body mass index and waist circumference with 3-year all-cause mortality among the oldest old: evidence from a chinese community-based prospective cohort study. J. Am. Med. Dir. Assoc. 19, 672–678.e4. doi: 10.1016/j.jamda.2018.03.015
Mao, C., Li, Z. H., Lv, Y. B., Gao, X., Kraus, V. B., Zhou, J. H., et al. (2020). Specific leisure activities and cognitive functions among the oldest-old: the chinese longitudinal healthy longevity survey. J. Gerontol. A Biol. Sci. Med. Sci. 75, 739–746. doi: 10.1093/gerona/glz086
Marioni, R. E., Proust-Lima, C., Amieva, H., Brayne, C., Matthews, F. E., Dartigues, J. F., et al. (2015). Social activity, cognitive decline and dementia risk: a 20-year prospective cohort study. BMC Public Health 15:1089. doi: 10.1186/s12889-015-2426-6
National Bureau of Statistics (2012). Chinese Population Census in 2010. Beijing: China Statistics Press.
Nelson, M. E., Jester, D. J., Petkus, A. J., and Andel, R. (2021). Cognitive reserve, Alzheimer’s neuropathology and risk of dementia: a systematic review and meta-analysis. Neuropsychol. Rev. 31, 233–250. doi: 10.1007/s11065-021-09478-4
Paillard-Borg, S., Fratiglioni, L., Winblad, B., and Wang, H. X. (2009). Leisure activities in late life in relation to dementia risk: principal component analysis. Dement. Geriatr. Cogn. Disord. 28, 136–144. doi: 10.1159/000235576
Petersson, S. D., and Philippou, E. (2016). Mediterranean diet, cognitive function and dementia: a systematic review of the evidence. Adv. Nutr. 7, 889–904. doi: 10.3945/an.116.012138
Qiu, J., Sun, H., Zhong, C., Ma, Q., Wang, C., Zhou, X., et al. (2019). Reclassified cognitive leisure activity and risk of cognitive impairment in Chinese older adults aged ≥80years: a 16-year prospective cohort study. Geriatr. Gerontol. Int. 19, 1041–1047. doi: 10.1111/ggi.13774
Rafnsson, S. B., Orrell, M., d’Orsi, E., Hogervorst, E., and Steptoe, A. (2020). Loneliness, social integration and incident dementia over 6 years: prospective findings from the english longitudinal study of ageing. J. Gerontol. B Psychol. Sci. Soc. Sci. 75, 114–124. doi: 10.1093/geronb/gbx087
Raz, L., Knoefel, J., and Bhaskar, K. (2016). The neuropathology and cerebrovascular mechanisms of dementia. J. Cereb. Blood Flow. Metab. 36, 172–186. doi: 10.1038/jcbfm.2015.164
Richards, M., and Deary, I. J. (2005). A life course approach to cognitive reserve: a model for cognitive aging and development? Ann. Neurol. 58, 617–622. doi: 10.1002/ana.20637
Scarmeas, N., and Stern, Y. (2003). Cognitive reserve and lifestyle. J. Clin. Exp. Neuropsychol. 25, 625–633. doi: 10.1076/jcen.25.5.625.14576
Shankar, A., Hamer, M., McMunn, A., and Steptoe, A. (2013). Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the english longitudinal study of ageing. Psychosom. Med. 75, 161–170. doi: 10.1097/PSY.0b013e31827f09cd
Shen, C., Rolls, E., Cheng, W., Kang, J., Dong, G., Xie, C., et al. (2022). Associations of social isolation and loneliness with later dementia. Neurology 8:10.1212/WNL.0000000000200583. doi: 10.1212/WNL.0000000000200583
Sommerlad, A., Sabia, S., Livingston, G., Kivimaki, M., Lewis, G., Singh-Manoux, A., et al. (2020). Leisure activity participation and risk of dementia: an 18-year follow-up of the Whitehall II study. Neurology 95, e2803–e2815. doi: 10.1212/WNL.0000000000010966
Stern, Y. (2012). Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 11, 1006–1012. doi: 10.1016/S1474-4422(12)70191-6
Suo, C., Singh, M. F., Gates, N., Wen, W., Sachdev, P., Brodaty, H., et al. (2016). Therapeutically relevant structural and functional mechanisms triggered by physical and cognitive exercise. Mol. Psychiatry 21, 1633–1642. doi: 10.1038/mp.2016.19
Valenzuela, M. J., Breakspear, M., and Sachdev, P. (2007). Complex mental activity and the aging brain: molecular, cellular and cortical network mechanisms. Brain Res. Rev. 56, 198–213. doi: 10.1016/j.brainresrev.2007.07.007
Wang, H. X., Xu, W., and Pei, J. J. (2012). Leisure activities, cognition and dementia. Biochim. Biophys. Acta 1822, 482–491. doi: 10.1016/j.bbadis.2011.09.002
Wang, J. Y., Zhou, D. H., Li, J., Zhang, M., Deng, J., Tang, M., et al. (2006). Leisure activity and risk of cognitive impairment: the chongqing aging study. Neurology 66, 911–913. doi: 10.1212/01.wnl.0000192165.99963.2a
Wilson, R. S., Bennett, D. A., Bienias, J. L., Aggarwal, N. T., Mendes De Leon, C. F., Morris, M. C., et al. (2002a). Cognitive activity and incident AD in a population-based sample of older persons. Neurology 59, 1910–1914. doi: 10.1212/01.wnl.0000036905.59156.a1
Wilson, R. S., Mendes De Leon, C. F., Barnes, L. L., Schneider, J. A., Bienias, J. L., Evans, D. A., et al. (2002b). Participation in cognitively stimulating activities and risk of incident Alzheimer disease. JAMA 287, 742–748. doi: 10.1001/jama.287.6.742
Wilson, R. S., Bennett, D. A., Gilley, D. W., Beckett, L. A., Barnes, L. L., Evans, D. A., et al. (2000). Premorbid reading activity and patterns of cognitive decline in Alzheimer disease. Arch. Neurol. 57, 1718–1723. doi: 10.1001/archneur.57.12.1718
Yates, L. A., Ziser, S., Spector, A., and Orrell, M. (2016). Cognitive leisure activities and future risk of cognitive impairment and dementia: systematic review and meta-analysis. Int. Psychogeriatr. 28, 1791–1806. doi: 10.1017/S1041610216001137
Yi, Z., and Vaupel, J. W. (2002). Functional capacity and self-evaluation of health and life of oldest old in china. J. Soc. Issues 58, 733–748. doi: 10.1111/1540-4560.00287
Zeng, Y., Feng, Q., Hesketh, T., Christensen, K., and Vaupel, J. W. (2017). Survival, disabilities in activities of daily living and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet 389, 1619–1629. doi: 10.1016/S0140-6736(17)30548-2
Keywords: dementia, cognitively stimulating activities, playing cards/mahjong, Chinese older adults, prospective study
Citation: Tian G, Shuai J, Li R, Zhou T, Shi Y, Cheng G and Yan Y (2022) Association between playing cards/mahjong and risk of incident dementia among the Chinese older adults: a prospective cohort study. Front. Aging Neurosci. 14:966647. doi: 10.3389/fnagi.2022.966647
Received: 11 June 2022; Accepted: 22 July 2022;
Published: 22 August 2022
Edited by:
Gang Wang, Shanghai Jiao Tong University, ChinaReviewed by:
Ling Yue, Shanghai Jiao Tong University, ChinaGang Xu, Shanghai Jiao Tong University, China
Copyright © 2022 Tian, Shuai, Li, Zhou, Shi, Cheng and Yan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Yan, eWFueWFuODAyMzk0QDEyNi5jb20=
† These authors have contributed equally to this work
 Gang Tian
Gang Tian Jingliang Shuai†
Jingliang Shuai† Rui Li
Rui Li Tong Zhou
Tong Zhou Yan Yan
Yan Yan