
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Aging Neurosci. , 25 August 2022
Sec. Neurocognitive Aging and Behavior
Volume 14 - 2022 | https://doi.org/10.3389/fnagi.2022.958744
This article is part of the Research Topic Post-Acute Sequelae of COVID-19 Infection (PASC): Implications for Geriatric and Neurological Care View all 10 articles
 Carrie A. Ciro1*
Carrie A. Ciro1* Shirley A. James1
Shirley A. James1 Hillary McGuire1
Hillary McGuire1 Vince Lepak2
Vince Lepak2 Susan Dresser3
Susan Dresser3 Amy Costner-Lark3
Amy Costner-Lark3 Wanda Robinson3
Wanda Robinson3 Terrie Fritz4
Terrie Fritz4Background: While studies recommend rehabilitation following post-hospitalization recovery from COVID-19, few implement standardized tools to assess continued needs. The aim of this study was to identify post-hospitalization recommendations using an interdisciplinary needs assessment with standardized rehabilitation measures. A secondary aim was to use these tools to measure recovery over a 30-day period.
Materials and methods: Using a 30-day longitudinal design, we completed weekly rapid needs assessments in this convenience sample of 20 people diagnosed with COVID-19 discharged from the hospital to home. We computed summary statistics and used the Wilcoxon Signed Rank Test to assess change over the 4-week course of the study with alpha level = 0.05.
Results: Our sample (65% male, 47% over 50 years of age, 35% White, 37% with a confirmed diagnosis of diabetes, and 47% obese) included no patients who had required mechanical ventilation. Initial assessments demonstrated the majority of our participants were at an increased risk of falls, had disability in activities of daily living (ADL) and instrumental activities of daily living (IADL), mild cognitive impairment, and dyspnea. At the 30-day follow-up, most were independent in mobility and basic ADLs, with continued disability in IADLs and cognitive function.
Discussion: In this sample of patients who were not mechanically-ventilated, early and individualized rehabilitation was necessary. The results of this study suggest patients would benefit from a multi-disciplinary team needs assessment after medical stabilization to minimize fall risk and disability, and to prevent secondary complications resulting from post-hospital deconditioning due to COVID-19.
As more people contract and recover from the Corona virus, knowledge of acute, post-acute and long-term physiological, physical, cognitive, and psychological sequelae evolve (Huang et al., 2021). Studies have reported people with COVID-19 who require hospitalization demonstrate long-term fatigue, cognitive difficulty, dyspnea, taste and smell impairments, muscle weakness, and poor cardiovascular endurance (Huang et al., 2021; Lopez-Leon et al., 2021; Wu et al., 2021; Zhang et al., 2021). Post-hospitalization, patients also commonly report anxiety, depression, post-traumatic stress disorder, and ICU-related neuropathy (Carenzo et al., 2021; Heesakkers et al., 2022). The majority of patients recovering from COVID-19 demonstrate impairments that hinder or restrict participation in activities of daily living (ADL), instrumental activities of daily living (IADL), the ability to live independently, return to work, and resume previous levels of social activity. Studies suggest early rehabilitation is associated with shorter recovery times and faster return to everyday activities (Choi et al., 2008; Coleman et al., 2017).
While studies recommend rehabilitation during the acute and post-acute phases of recovery (Demeco et al., 2020; Gutenbrunner et al., 2020; Sivan et al., 2020), little is known about the depth of rehabilitation needs because researchers have not utilized standardized assessment tools. Current studies examine patients 6–12 months post COVID-19 using screening tools too broad to provide detailed information about patients living in their home environment (Huang et al., 2021; Wu et al., 2021; Xiong et al., 2021; Zhang et al., 2021; Heesakkers et al., 2022). While longitudinal studies of sequelae offer critical information, a profile of the natural recovery during the early period after hospitalization is critical to improve recommendations for rehabilitation. The primary aim of this study was to identify post-hospitalization needs and services required for those diagnosed with COVID-19 using an interdisciplinary needs assessment with standardized rehabilitation tools. The secondary aim of this study was to report the natural course of recovery for people hospitalized with COVID-19 over a 30-day period using these standardized rehabilitation assessments.
We employed a modified, rehabilitation-oriented, rapid needs assessment using a longitudinal design to assess people who were discharged from hospital to home with a diagnosis of COVID-19 between April and December 2020. While a traditional needs assessment involves a reiterative process in which participants communicate needs to the researcher, in a rapid needs assessment, the timing for understanding health care needs is critical, thus the team begins with hypothetical, but informed areas of evaluation (Lee, 2019).
The team completed baseline measurements within 5°days of hospital discharge. We then assessed patients weekly over a 30-day period post-hospitalization using a battery of standardized tools utilizing nursing, occupational therapy, physical therapy, and social work utilizing cellular telephones, FaceTime, or Zoom platforms. Inclusion criteria included people at least 18 years of age, English speaking, diagnosed with COVID-19, hospitalized and subsequently discharged home, able to consent with or without caregiver assistance, and with internet access. Exclusion criteria included individuals who were discharged or met the criteria for hospice, demonstrated current drug or alcohol dependency, or who were pregnant. This study was approved by the Institutional Review Board of The University of Oklahoma Health Sciences Center (IRB#11988).
During the course of this study, the IRB required research to be conducted virtually due to COVID-19 restrictions. We recruited participants from a convenience sample of patients admitted to a Level I Trauma Hospital on an academic health sciences center campus. We consented and provided participants a COVID Assessment Kit either personally prior to hospital discharge, or a combination phone call and front door drop-off. We utilized the “Evaluation for Consent” tool because people with COVID-19 are more likely to demonstrate cognitive impairment (Resnick et al., 2019; Sasannejad et al., 2019).
Advanced practice registered nursing staff (APRN), occupational therapists (OT)s, physical therapists (PT)s, and social work staff (SW) completed virtual interviews and physiological, physical, functional, cognitive, and mental health assessments. All study personnel utilized the secure Research Electronic Data Capture (REDCap) system to enter data.
Baseline assessments utilized:
Either APRN or SW staff determined each participant’s cognitive eligibility to consent using procedures described by Resnick et al. (2019).
Advanced practice registered nursing staff staff obtained sociodemographic, medical, and mental health history using the hospital chart and interview.
This assessment characterizes patient comorbidities based on the International Classification of Function. Each co-morbidity has an associated weight from 1 to 6 based on the adjusted risk of mortality or resource use. The sum of all weights results in a single comorbidity score where “0” indicates no comorbidities. The higher the score, the more likely the predicted outcome will result in mortality or higher resource use (Charlson et al., 1987).
The MDP assesses dyspnea intensity, sensory quality, unpleasantness, and affective distress using 12 items rated on a 0–10 numerical scale. The reliability, validity, and responsiveness to clinical change of the MDP in use for both acute and follow-up care is well-established (Meek et al., 2012; Banzett et al., 2015).
The SQUEGG hand grip dynamometer measures grip strength up to 220°pounds using a smartphone application usable in the home environment. Traditional hand grip dynamometers have excellent reliability and validity (Mathiowetz, 2002).
The 5xSTS assesses strength, transitional movements, balance, and fall risk by documenting time required for a person to come to a complete stand from a sitting position five times. The 5xSTS has good reliability and validity (Schaubert and Bohannon, 2005; Bohannon, 2006; Tiedemann et al., 2008).
The TUG comprises three separate tests to assess fall risk; under normal situations, with added physical stress (manual) and with divided attention (cognitive). Examiners assess the time it takes for a person to rise from a seated position, walk three meters, turn around, and return to sitting (normal), while carrying a glass 3/4 full of water (manual), and while counting backward by 3 or 4 from 100 (cognitive). TUG scores are predictive of fall risk with an 87% success rate, and have excellent reliability (Shumway-Cook et al., 2000; Hofheinz and Schusterschitz, 2010).
The Borg RPE provides an estimate of heart rate during physical activity based on a rating scale ranging from 6 to 20 (Borg, 1982). Researchers have reported a high correlation between perceived exertion rating multiplied by 10, and the actual heart rate during physical activity (Borg, 1982; Marissa et al., 2008; Tabacof et al., 2022).
The Barthel index uses an ordinal scale to measure and monitor change in activities of daily living (Table 3), with scores based on current ability (de Morton et al., 2008; Della Pietra et al., 2011). The Barthel index delivered by phone has excellent inter-relater reliability (Kappa = 0.90 with 985% CI, 0.85–0.94).
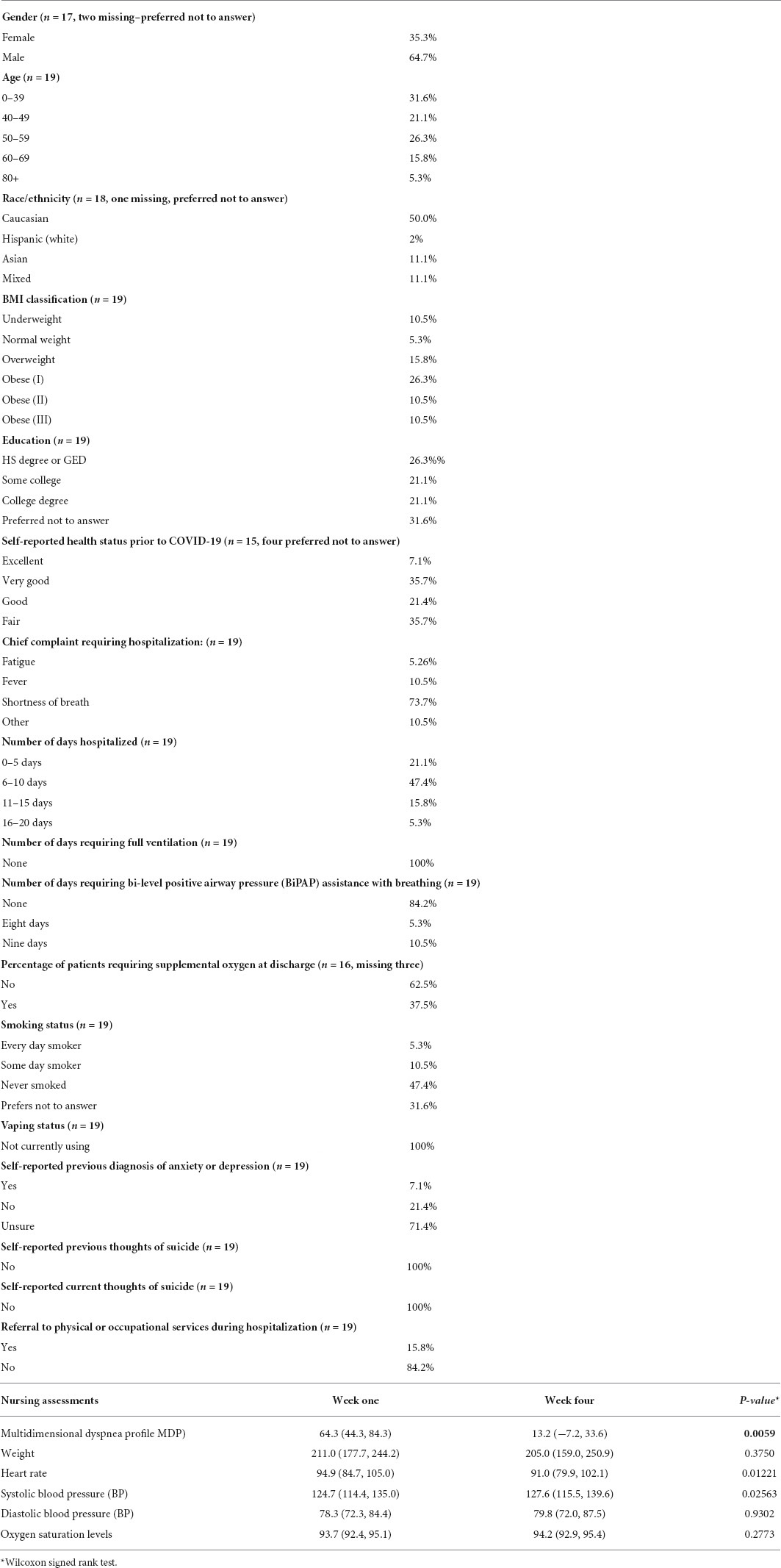
Table 1. Socio-demographic, patient chart data (n = 20), and data gathered by nursing staff over time reported at weeks 1 and 4 (mean values with 95% CI) (n = 15).
The Lawton IADL Scale uses an interview format to assess independent living skills like phone use, shopping, food preparation, medications, finance, housekeeping, and laundry (Lawton and Brody, 1969). We modified scoring for more differentiation between participants using scores of 0 (dependent), 1 (partial assistance), and 2 (independent). The maximum score of 16 indicates self-reported independence. The tool demonstrates very high internal consistency and inter-rater reliability (Siriwardhana et al., 2018).
The MoCA is a short cognitive screen predictive of mild cognitive impairment by assessing language, orientation, and memory using three items totaling a possible 15 points. The MoCA has good reliability and validity in differentiating cognitively impaired patients with executive domain impairment from those without and has excellent 30-day test-retest reliability (Pendlebury et al., 2013).
The PHQ-9 is a measure of depression using scores on nine items ranging from 0 (not occurring at all) to 3 (occurring nearly every day) for the “last 2°weeks” (Maurer, 2012). The PHQ-9 can be used to make a tentative diagnosis of depression in at-risk populations. When used as a screen for depression, the PHQ-9 has fair sensitivity and very good specificity (Maurer, 2012).
The GAD-7 is a measure of generalized anxiety with its potential causes using a seven-item scale with scores ranging from 0 (not occurring at all) to 3 (occurring nearly every day). Modeled after the PHQ9, it is quick (2–5 min) and effective when used within a primary health care setting, and can be self-administered or completed by interview, either electronically or in person (Roy-Byrne et al., 2009).
The research team attended 8°h of study protocol training and received online written protocols for future reference. Training included strict study protocol adherence, standardizing assessments, assessing, and referral for patients experiencing medical deterioration, and documentation using the secure REDCap data collection system.
The COVID Home Care Kit contained an electronic scale, blood pressure cuff, mobile oxygen saturation monitor, SQUEEG hand strength dynamometer, and a 3-meter measuring tape. After receiving the kit, research personnel contacted participants to set up FaceTime, Zoom, and biomedical assessment tool technology. Personnel delivered the baseline assessments within 5°days of hospital discharge, and spread baseline assessments over 72 h to relieve patient and caregiver burden. Because anxiety is associated with COVID-19 (Heesakkers et al., 2022), our protocol included additional 5-min phone check-ins by nursing to assess physiological measures and recommend primary care physician follow-up if needed. Nursing staff tapered the frequency of these phone calls over 4°weeks calling 7°days during Week 1, 3°days during Week 2, 2°days during Week 3, and 1°day during Week 4. Disciplines communicated regularly about the time of scheduled visits to minimize risk of fatigue caused by multiple calls and assessments during the 30-day period. We asked participants at risk for falls, with significant ADL/IADL dependence, or with immediate health concerns to call his or her primary care physician for an appointment or referral for home health services.
Upon completion of the study, one researcher downloaded and analyzed all data using a combination of Microsoft Excel and SAS 9.4 (Carey, NJ, United States). Personnel computed summary statistics including means and 95% CI for all continuous variables, along with percentages for each categorical variable. To analyze change over the 4-week course of the study in each continuous variable, we utilized the Wilcoxon Signed Rank test with an alpha level equal to 0.05.
We enrolled the first 20 patients diagnosed with COVID-19 who consented upon discharge from a Level 1 Trauma Hospital on our academic campus. One patient dropped out immediately after enrolling, making our resulting sample size 19. Several patients failed to complete portions of the assessments, or did not participate after 1 or 2°weeks. Two thirds of participants self-identified as male and almost half were over 50 years of age. One third (35%) self-identified as Caucasian, with an additional 10% White-Hispanic. Although 85% had a BMI classification of overweight or obese (overweight = 16%, obesity type I = 32%, obesity type II = 26%, and obesity type III = 11%), two thirds responded their general health prior to COVID-19 was good, very good, or excellent (64%). Education ranged from high school or GED level through college graduate level. More than half of respondents reported living alone (Table 1).
Only 16% of our participants reported being every day or someday smokers and none used vaping devices. While 7% reported previous diagnoses of anxiety or depression, none reported thoughts of suicide, either currently, or in the past. The mean Charlson Comorbidity Index score was 3 out of a maximum score of 37, representing a low risk of either mortality or high levels of resource use. While nearly three quarters (74%) revealed their chief complaint requiring hospitalization was shortness of breath, no one in this cohort required full ventilation and only 16% required bi-level positive airway pressure (Bi-PAP) assistance with breathing. Almost half (47%) of the participants in this study were hospitalized 6–10 days. Only 16% of participants in the study received inpatient physical or occupational therapy, and none had a referral for outpatient or home health therapy services (Table 1).
The mean Week 1 Multidimensional Dyspnea Profile score was 64 (M = 64.3, 95% CI: 44.3–84.3), which dropped significantly to 13 (M = 13.2, 95% CI: −7.2 to −33.6) by week 4 (p = 0.0059). Heart rate also decreased significantly from 94.9 at Week 1 to 91.0 at Week 4 (p = 0.01). Other vital signs, including blood pressure, oxygen saturation levels, and weight remained stable over the 4°weeks following discharge (Table 1). Percentage of participants reporting fatigue dropped from 75% at Week 1, to 31% at Week 4 (p = 0.0031).
The five times sit to stand test improved during the 4-week study from a mean 17.5 s to a mean 12.6 s (p = 0.0009). Participants did not fall below the cut-off time suggestive of further assessment for fall risk (12 s), during the course of the study. Timed Up and Go (TUG) scores improved during the 4-week study from a mean 15.1 s during Week 1, to a mean 12.1 s during Week 4 (p = 0.0419). Participants fell below the cut-off value suggestive of fall risk (13.5 s) after week two, meaning their fall risk was within an acceptable range. Both the Dual Task TUG (TUG-DT) and the Cognitive TUG (TUG-COG) also improved with mean values of 14.3 s and 20.5°s respectively during Week 1, to 12.1 s and 13.7 s during Week 4. These versions of the TUG represent a participant’s ability to engage cognitively or physically while executing complex motor tasks and acceptable fall risk levels are 14.5 and 15 s, respectively (Table 2).
BORG Perceived Rate of Exertion scores dropped dramatically during each of these physical exertion tests with highs of 10.7/20 during the 5xSTS test during Week 1 to 8.4/20 during the TUG-COG during Week 4. Final RPE scores for all these tasks fall within either the fairly light or very light ranges and are acceptable for physical tasks like those represented by the 5xSTS and the TUG (Table 2). Hand grip during the study changed from a mean 65 pounds in the dominant hand during week one, to a mean 78.2 pounds with the dominant hand during week four (p = 0.0020) (Table 2).
Barthel ADL Index scores indicated all participants were independent in bowel continence, bladder continence, and toilet use upon discharge from the hospital. Barthel scores for bathing, dressing, hygiene (grooming), and transfers all approached or scored independence by the end of 4°weeks. Participants significantly improved in ambulation independence, beginning with a mean score of 9.0 points and ending with a mean score of 13.0 points (p = 0.0156). The ability to climb stairs was low at Week 1 with a mean of score of 5.4, and remained low at Week 4 with a mean score of 6.1 points. BORG Rating of Perceived Exertion scores demonstrated significant decreases in bathing, with a mean change from 10.3 to 7.8 points (p = 0.0156), in dressing with a mean change from 8.9 to 7.8 points (p = 0.0313), in bed and chair transfers with a mean change from 8.5 to 6.3 points (p = 0.0313), and in ambulation with a mean change from 12.5 to 9.2 points (p = 0.0195) Perceived exertion remained high for climbing stairs (Table 3).
Lawton IADL scores revealed participants were independent in their ability to use the phone at Week 1. In more physically and mentally complex tasks, while participants improved significantly in their ability to shop (mean change from 0.9 to 1.4, p = 0.0125), prepare food (mean change from 1.4 to 1.8, p = 0.0125), and do housekeeping (mean change from 1.0 to 1.6, p = 0.0313), scores did not indicate independence. While many Borg RPE scores for IADLs changed during the 4°weeks after discharge from the hospital, the changes were not significant (Table 3).
The mean 5-min Montreal Cognitive Assessment test score in Week 1 was 11.7 points, indicating mild cognitive impairment. While this score improved to 13.3 points at Week 4, the difference was not significant (p = 0.10). Several participants demonstrated significant cognitive impairment that did not change or even declined during the course of the study (Table 3).
The mean GAD-7 total score during Week 1 was 5.9 points, which remained relatively consistent over the 4°weeks of the study ending with a mean during Week 4 of 4.5 points (p = 0.34). No individual variables of the GAD-7 changed significantly over time. The mean PHQ-9 score in Week 1 was 8.9 points, which reduced to a mean of 5.5 points in Week 4 (p = 0.10). No individual portions of the PHQ-9 changed significantly over time (Table 4).
The primary aim of this study was to identify post-hospitalization needs and services that would allow patients diagnosed with COVID-19 to be as safe and independent as possible in their home settings using an interdisciplinary rapid needs assessment. In our sample of patients, discharge planning did not appear to include functional level or prognosis. Chart reviews revealed that 80% of our participants had not received any type of rehabilitation therapy and, when asked, were uncertain about how to progress their activity levels, or how to balance movement with rest. One partial explanation may be that training by professionals might have been poorly retained due to cognitive deficits, which were prevalent in week one. Further, we found significant impairments in physiologic, physical, functional, and cognitive performance which indicated the need for referral for a multi-disciplinary assessment and rehabilitation. These findings suggest a thorough assessment by nursing, occupational therapy, physical therapy, and social work staff could assist in clarifying post-discharge needs for patients transitioning to home after hospitalization for COVID-19.
The secondary aim of this study was to report the natural course of COVID-19 recovery over a 30-day period using standardized assessment tools. We found that while many measurements returned to normal or near normal over time, patients demonstrated increases in fall risk and loss of independence during their first few weeks at home, and required assistance with basic self-care. Caregivers were also impacted as they were unable to work unless they left impaired patients at home alone during initial recovery. Participants in our study did not demonstrate significant improvement in cognition over the 4-week period.
In this study, researchers monitored physiological measures of dyspnea, blood pressure, heart rate, and weight over 4°weeks. During week one, 75% of participants experienced dyspnea, compared to week four levels of 31%. This compares to a meta-analysis by Fernández-de-Las-Peñas et al. (2021), in which dyspnea decreased from a baseline level of 13.2%, to 27.2% at 60 days, and 26.3% at 90 days. Within our study, we found a significant decrease in heart rate, an insignificant decrease in weight and an insignificant increase in oxygen saturation levels. Patients with persistent dyspnea may benefit from referrals to professionals versed in respiratory and cardiac rehabilitation to improve their breath support and reduce their energy expenditure during functional activities.
Participants in this study were not highly impacted by comorbid conditions as evidenced by their mean Charlson Co-Morbidity Index score of three. Patients with comorbidities did experience poorer outcomes. Early identification of potential comorbidities during initial assessment, as well as enhanced attention to those potential complications during acute care, and discharge planning could assist in preventing secondary complications. Patients with comorbid conditions may also require enhanced time and rehabilitation hours compared to their counterparts without these conditions (Charlson et al., 1987; Choi et al., 2008).
The participants in this study demonstrated significant levels of debilitation during their first week post hospitalization as evidenced by poor scores on the TUG, the 5x sit to stand, and the SQUEGG hand grip dynamometer. In previous studies, researchers have provided results on a 6-min Walk test. While none of our participants had the physical capacity to complete this test at hospital discharge, the 6-min walk test would have added a component of cardiovascular endurance to our measures, a factor we failed to adequately capture. By the end of week two, participants transitioned quickly to a safe level of walking and transfers and were no longer considered at fall risk. Although no participants reported falls in the 4°weeks after hospitalization, fall risk was high given their mobility status at discharge. While the physical performance assessments we utilized demonstrated improvement over the 30-day acute outpatient term, all three versions of the TUG along with the 5xSTS were probably unnecessary. Grip strength also increased significantly over 4°weeks, an important finding, as higher hand strength is associated with less mortality (Sayer and Kirkwood, 2015; De Biase et al., 2020).
Participants in this study were independent in bowel and bladder control upon hospital discharge, however required assistance with all ADLs and basic mobility tasks until week four. Assessment scores suggested that patients continued to require assistance with bathing, ambulation, and stair climbing, even at week four. Participants with stalled performance scores also continued to have higher rates of perceived exertion.
Considering IADLs, our participants were independent with telephone use upon discharge although one reported shortness of breath while talking on the phone. While scores for financial and medication management quickly improved to normal, the OT assessment team reported these scores may have reflected ability versus observed performance, given the participant’s cognitive scores. Participants continued to be partially dependent in the IADL skills of shopping, food preparation, housekeeping, laundry, and transportation at week four. Most participants continued to need assistance due to mild shortness of breath and had Borg scores greater than seven. In support of our findings, Carenzo et al. (2021) reported 87% of the participants in their study were independent in self-care by 8°weeks post-hospitalization. Our findings suggest OT and PT referrals for patients with even mild ADL and IADL disability could minimize risk of secondary complications resulting from COVID-19 (He et al., 2015).
Similar to other studies (Hampshire et al., 2021; Jaywant et al., 2021), our participant’s demonstrated mild cognitive impairment, particularly in the areas of language and memory. While these scores did not improve significantly over the 4-week trial they did trend upwardly. Participants continued to report problems with word-finding and short-term memory at week four and many requested information about how to enhance recovery. Hampshire et al. (2021) reported cognitive impairment and word-finding difficulty in their participants, and Jaywant et al. (2021) found impaired working memory in 55% of participants, impaired speed of processing in 40% of participants, and divided attention in 46% of participants recovering from COVID-19. Referrals to speech-language pathology and/or occupational therapy might enhance cognitive and communication ability (McGuire et al., 2006).
Unlike other studies (Xiong et al., 2021; Zhang et al., 2021), our participants did not experience significant or persistent self-reported anxiety and depression. Patients did report fears of re-infection, anxiety about financial concerns, and anxiety about not returning to baseline functional levels. The majorities of participants in our sample were married or had a caregiver staying with them. It is possible that social support moderated the level of anxiety noted in other studies (Viseu et al., 2018; Zhao et al., 2018). Clearly, mood should be monitored following COVID-19 as symptoms of depression and anxiety affect cognitive performance in older adults (Baune et al., 2006).
Because our samples of patients were never ventilator dependent, they most likely did not exhibit the most severe symptoms, therefore generalization to that population may be limited. Our sample size was relatively small, with some loss to follow-up. Our participants tired from meeting the demands of multiple phone calls on different days from multiple disciplines, suggesting a more streamlined approach may be beneficial. We were dependent on patient interpretation of test results as we did not conduct face-to-face assessments. We did ask caregivers to provide input when cognition may have impacted participant response reliability.
We examined the post-discharge needs of patients hospitalized with COVID-19 and followed their natural recovery over 30 days without intervention. Our physiological, physical, cognitive, and functional findings suggest patients would benefit from assessment and intervention from a multi-disciplinary to address the range of deficits patients may experience as they recover from COVID-19. Early rehabilitation may shorten recovery time and allow patients to return to normal activities; foundational for an optimal quality of life.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of Oklahoma Health Sciences Center IRB. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CC contributed to the study conceptualization and design, developed the study manual and training, collected data and contributed significantly to the development of this manuscript. SJ contributed to the study design, led all team members in RED Cap training, collected and analyzed data, developed tables, and authored significant sections of the manuscript. HM and VL participated in data collection and manuscript development. AC-L, SD, WR, and TF participated in study conceptualization and design, trained team members, collected data, and edited all portions of the manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by The University of Oklahoma Norman Campus Vice President of Research through a special call for COVID-19 related studies.
We are grateful for the contributions of Kayla Garver, DPT, and Miki Thompson, APRN for their role in assessing and consenting people in the hospital environment. We also thank the professional students, Kevin Forte, OTS, Darshit Patel, MS, DPT, Jaren Thomas, DPT, and Zachery Dunnells (social work) for their contributions in setting up technology and conducting participant assessments.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Banzett, R. B., O’Donnell, C. R., Guilfoyle, T. E., Parshall, M. B., Schwartzstein, R. M., Meek, P. M., et al. (2015). Multidimensional Dyspnea Profile: An instrument for clinical and laboratory research. Eur. Respir. J. 45, 1681–1691. doi: 10.1183/09031936.00038914
Baune, B. T., Suslow, T., Engelien, A., Arolt, V., and Berger, K. (2006). The association between depressive mood and cognitive performance in an elderly general population–the MEMO study. Dementia Geriatr. Cogn. Disord. 22, 142–149. doi: 10.1159/000093745
Bohannon, R. W. (2006). Reference values for the five-repetition sit-to-stand test: A descriptive meta-analysis of data from elders. Percept. Mot. Skills 103, 215–222. doi: 10.2466/pms.103.1.215-222
Borg, G. A. (1982). Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 14, 377–381. doi: 10.1249/00005768-198205000-00012
Carenzo, L., Protti, A., Dalla Corte, F., Aceto, R., Iapichino, G., Milani, A., et al. (2021). Short-term health-related quality of life, physical function and psychological consequences of severe COVID-19. Ann. Intensive Care 11:91. doi: 10.1186/s13613-021-00881-x
Charlson, M. E., Pompei, P., Ales, K. L., and MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 40, 373–383. doi: 10.1016/0021-9681(87)90171-8
Choi, J. H., Jakob, M., Stapf, C., Marshall, R. S., Hartmann, A., and Mast, H. (2008). Multimodal early rehabilitation and predictors of outcome in survivors of severe traumatic brain injury. J. Trauma Acute Care Surg. 65, 1028–1035. doi: 10.1097/TA.0b013e31815eba9b
Coleman, E. R., Moudgal, R., Lang, K., Hyacinth, H. I., Awosika, O. O., Kissela, B. M., et al. (2017). Early rehabilitation after stroke: A narrative review. Curr. Atheroscler. Rep. 19:59. doi: 10.1007/s11883-017-0686-6
De Biase, S., Cook, L., Skelton, D. A., Witham, M., and Ten Hove, R. (2020). The COVID-19 rehabilitation pandemic. Age Ageing 49, 696–700. doi: 10.1093/ageing/afaa118
de Morton, N. A., Keating, J. L., and Davidson, M. (2008). Rasch analysis of the Barthel Index in the assessment of hospitalized older patients after admission for an acute medical condition. Arch. Phys. Med. Rehabil. 89, 641–647. doi: 10.1016/j.apmr.2007.10.021
Della Pietra, G. L., Savio, K., Oddone, E., Reggiani, M., Monaco, F., and Leone, M. A. (2011). Validity and reliability of the Barthel index administered by telephone. Stroke 42, 2077–2079. doi: 10.1161/STROKEAHA.111.613521
Demeco, A., Marotta, N., Barletta, M., Pino, I., Marinaro, C., Petraroli, A., et al. (2020). Rehabilitation of patients post-COVID-19 infection: A literature review. J. Int. Med. Res. 48, 1–10. doi: 10.1177/0300060520948382
Fernández-de-Las-Peñas, C., Palacios-Ceña, D., Gómez-Mayordomo, V., Florencio, L. L., Cuadrado, M. L., Plaza-Manzano, G., et al. (2021). Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur. J. Intern. Med. 92, 55–70. doi: 10.1016/j.ejim.2021.06.009
Gutenbrunner, C., Stokes, E. K., Dreinhöfer, K., Monsbakken, J., Clarke, S., Côté, P., et al. (2020). Why Rehabilitation must have priority during and after the COVID-19-pandemic: A position statement of the Global Rehabilitation Alliance. J. Rehabil. Med. 50, 317–325. doi: 10.2340/16501977-2217
Hampshire, A., Trender, W., Chamberlain, S. R., Jolly, A. E., Grant, J. E., Patrick, F., et al. (2021). Cognitive deficits in people who have recovered from COVID-19. EClinicalMedicine 39:101044. doi: 10.1016/j.eclinm.2021.101044
He, S., Craig, B. A., Xu, H., Covinsky, K. E., Stallard, E., Thomas, J., et al. (2015). Unmet need for ADL assistance is associated with mortality among older adults with mild disability. J. Gerontol. A Biol. Sci. Med. Sci. 70, 1128–1132. doi: 10.1093/gerona/glv028
Heesakkers, H., van der Hoeven, J. G., Corsten, S., Janssen, I., Ewalds, E., Simons, K. S., et al. (2022). Clinical Outcomes Among Patients With 1-Year Survival Following Intensive Care Unit Treatment for COVID-19. JAMA 327, 559–565. doi: 10.1001/jama.2022.0040
Hofheinz, M., and Schusterschitz, C. (2010). Dual task interference in estimating the risk of falls and measuring change: A comparative, psychometric study of four measurements. Clin. Rehabil. 24, 831–842. doi: 10.1177/0269215510367993
Huang, C., Huang, L., Wang, Y., Li, X., Ren, L., Gu, X., et al. (2021). 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 397, 220–232. doi: 10.1016/S0140-6736(20)32656-8
Jaywant, A., Vanderlind, W. M., Alexopoulos, G. S., Fridman, C. B., Perlis, R. H., and Gunning, F. M. (2021). Frequency and profile of objective cognitive deficits in hospitalized patients recovering from COVID-19. Neuropsychopharmacology 46, 2235–2240. doi: 10.1038/s41386-021-00978-8
Lawton, M. P., and Brody, E. M. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 9, 179–186. doi: 10.1093/geront/9.3_Part_1.179
Lee, J. (2019). Rapid needs assessment: An evidence-based model. Eur. J. Train. Dev. 43, 61–75. doi: 10.1108/EJTD-08-2018-0077
Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P. A., Cuapio, A., et al. (2021). More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 11:16144. doi: 10.1038/s41598-021-95565-8
Marissa, E. M., Denise, M. C., Tom, J. O., and Robert, J. P. (2008). Validity of values for metabolic equivalents of task during submaximal all-extremity exercise and reliability of exercise responses in frail older adults. Phys. Therapy 88, 747–756. doi: 10.2522/ptj.20070161
Mathiowetz, V. (2002). Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup. Ther. Int. 9, 201–209. doi: 10.1002/oti.165
McGuire, L. C., Ford, E. S., and Ajani, U. A. (2006). The impact of cognitive functioning on mortality and the development of functional disability in older adults with diabetes: The second longitudinal study on aging. BMC Geriatr. 6:8. doi: 10.1186/1471-2318-6-8
Meek, P. M., Banzett, R., Parsall, M. B., Gracely, R. H., Schwartzstein, R. M., and Lansing, R. (2012). Reliability and validity of the multidimensional dyspnea profile. Chest 141, 1546–1553. doi: 10.1378/chest.11-1087
Pendlebury, S. T., Welch, S. J., Cuthbertson, F. C., Mariz, J., Mehta, Z., and Rothwell, P. M. (2013). Telephone assessment of cognition after transient ischemic attack and stroke: Modified telephone interview of cognitive status and telephone Montreal Cognitive Assessment versus face-to-face Montreal Cognitive Assessment and neuropsychological battery. Stroke 44, 227–229. doi: 10.1161/STROKEAHA.112.673384
Resnick, B., Gruber-Baldini, A. L., Pretzer-Aboff, I., Galik, E., Buie, V. C., Russ, K., et al. (2019). Reliability and validity of the evaluation to sign consent measure. Gerontologist 47, 69–77. doi: 10.1093/geront/47.1.69
Roy-Byrne, P., Veitengruber, J. P., Bystritsky, A., Edlund, M. J., Sullivan, G., Craske, M. G., et al. (2009). Brief intervention for anxiety in primary care patients. J. Am. Board Fam. Med. 22, 175–186. doi: 10.3122/jabfm.2009.02.080078
Sasannejad, C., Ely, E., and Lahiri, S. (2019). Long-term cognitive impairment after acute respiratory distress syndrome: A review of clinical impact and pathophysiological mechanisms. Crit. Care 23:1352. doi: 10.1186/s13054-019-2626-z
Sayer, A. A., and Kirkwood, T. B. (2015). Grip strength and mortality: A biomarker of ageing? Lancet 386, 226–227. doi: 10.1016/S0140-6736(14)62349-7
Schaubert, K. L., and Bohannon, R. W. (2005). Reliability and validity of three strength measures obtained from community-dwelling elderly persons. J. Strength Cond. Res. 19:717. doi: 10.1519/R-15954.1
Shumway-Cook, A., Brauer, S., and Woollacott, M. (2000). Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 80, 896–903. doi: 10.1093/ptj/80.9.896
Siriwardhana, D. D., Hardoon, S., Rait, G., Weerasinghe, M. C., and Walters, K. R. (2018). Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: A systematic review and meta-analysis. BMJ Open 8:e018195. doi: 10.1136/bmjopen-2017-018195
Sivan, M., Halpin, S., Hollingworth, L., Snook, N., Hickman, K., and Clifton, I. J. (2020). Development of an integrated rehabilitation pathway for individuals recovering from COVID-19 in the community. J. Rehabil. Med. 52:jrm00089. doi: 10.2340/16501977-2727
Tabacof, L., Tosto-Mancuso, J., Wood, J., Cortes, M., Kontorovich, A., McCarthy, D., et al. (2022). Post-acute COVID-19 Syndrome Negatively Impacts Physical Function, Cognitive Function, Health-Related Quality of Life, and Participation. Am. J. Phys. Med. Rehabil. 101:48. doi: 10.1097/PHM.0000000000001910
Tiedemann, A., Shimada, H., Sherrington, C., Murray, S., and Lord, S. (2008). The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing 37, 430–435. doi: 10.1093/ageing/afn100
Viseu, J., Leal, R., de Jesus, S. N., Pinto, P., Pechorro, P., and Greenglass, E. (2018). Relationship between economic stress factors and stress, anxiety, and depression: Moderating role of social suort. Psychiatry Res. 268, 102–107. doi: 10.1016/j.psychres.2018.07.008
Wu, L., Xiong, H., Mei, B., and You, T. (2021). Persistence of symptoms after discharge of patients hospitalized due to COVID-19. Front. Med. 8:761314. doi: 10.3389/fmed.2021.761314
Xiong, Q., Xu, M., Li, J., Liu, Y., Zhang, J., Xu, Y., et al. (2021). Clinical sequelae of COVID-19 survivors in Wuhan, China: A single-centre longitudinal study. Clin. Microbiol. Infect. 27, 89–95. doi: 10.1016/j.cmi.2020.09.023
Zhang, X., Wang, F., Shen, Y., Zhang, X., Cen, Y., Wang, B., et al. (2021). Symptoms and health outcomes among survivors of COVID-19 infection 1 year after discharge from hospitals in Wuhan China. JAMA Netw. Open 4:e2127403. doi: 10.1001/jamanetworkopen.2021.27403
Keywords: COVID-19, rehabilitation, multi-disciplinary, function, cognition, mobility
Citation: Ciro CA, James SA, McGuire H, Lepak V, Dresser S, Costner-Lark A, Robinson W and Fritz T (2022) Natural, longitudinal recovery of adults with COVID-19 using standardized rehabilitation measures. Front. Aging Neurosci. 14:958744. doi: 10.3389/fnagi.2022.958744
Received: 01 June 2022; Accepted: 08 August 2022;
Published: 25 August 2022.
Edited by:
Patricia C. Heyn, Marymount University, United StatesReviewed by:
Sri Sadhan Jujjavarapu, University at Buffalo, United StatesCopyright © 2022 Ciro, James, McGuire, Lepak, Dresser, Costner-Lark, Robinson and Fritz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carrie A. Ciro, Y2FycmllLWNpcm9Ab3Voc2MuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.