
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Aging Neurosci. , 13 September 2022
Sec. Neurocognitive Aging and Behavior
Volume 14 - 2022 | https://doi.org/10.3389/fnagi.2022.935326
This article is part of the Research Topic Physical Exercise for Age-Related Neuromusculoskeletal Disorders View all 36 articles
 Xiaobo Liu1†
Xiaobo Liu1† Chengzhi Jiang2†
Chengzhi Jiang2† Rong Fan3†
Rong Fan3† Tianyu Liu4
Tianyu Liu4 Yuxi Li1
Yuxi Li1 Dongling Zhong1
Dongling Zhong1 Luxiang Zhou1
Luxiang Zhou1 Tao Liu1
Tao Liu1 Juan Li1*
Juan Li1* Rongjiang Jin1,5*
Rongjiang Jin1,5*Background: Tai Chi may be a promising exercise to prevent and control bone loss in postmenopausal women. This meta-analysis and trial sequential analysis aimed to evaluate the effect and safety of Tai Chi on bone health in postmenopausal women.
Method: Seven databases were searched from their inceptions to 11 May 2022 to collect randomized controlled trials (RCTs) investigating the effect and safety of Tai Chi on bone health in postmenopausal women. Two independent reviewers identified the eligible studies, extracted data, and assessed the risk of bias of included studies using the revised Cochrane risk-of-bias tool for randomized trials. The primary outcome was the bone mineral density (BMD), and secondary outcomes included bone turnover markers and calcaneus quantitative ultrasound. Subgroup analyses were conducted based on the duration of Tai Chi. Sensitivity analyses and publication bias assessment were performed. RevMan software (version 5.4.1) and R software (version 3.6.1) were used for data synthesis. The certainty of evidence was rated with the Grading of recommendations assessment, development, and evaluation (GRADE) system. We also performed the trial sequential analysis to evaluate the reliability of the evidence.
Results: A total of 25 reports involving 24 studies were included. Four studies were considered as high overall risk of bias, and the rest were some concerns. Among included studies, there were three comparisons including Tai Chi vs. non-intervention, Tai Chi vs. other exercises, and Tai Chi plus nutraceutical vs. nutraceutical. Compared with non-intervention, Tai Chi was more effective to improve BMD of lumbar spine (MD = 0.04, 95% CI 0.02 to 0.07, I2 = 0%, low certainty), femoral neck (MD = 0.04, 95% CI 0.02 to 0.06, I2 = 0%, low certainty), and trochanter (MD = 0.02, 95% CI 0.00 to 0.03, I2 = 0%, very low certainty), but there was no significant difference in increasing the BMD of Ward's triangle (MD = 0.02, 95% CI −0.01 to 0.04, I2 = 0%, very low certainty). Trial sequential analysis showed that the effect of Tai Chi vs. non-intervention on the BMD of lumbar spine and femoral neck was reliable, but the effect on the BMD of trochanter and Ward's triangle needed further verification. The subgroup analyses suggested that Tai Chi training for over 6 months had greater improvement in BMD of the lumbar spine, femoral neck, and trochanter than non-intervention. No significant differences were observed in the above outcomes of Tai Chi vs. other exercises, and Tai Chi plus nutraceutical vs. nutraceutical. There was insufficient evidence to support the effect of Tai Chi on bone turnover markers and calcaneus quantitative ultrasound. Few Tai Chi relevant adverse events occurred.
Conclusion: Tai Chi may be an optional and safe exercise for improving BMD loss in postmenopausal women, and practicing Tai Chi for more than 6 months may yield greater benefits. However, more rigorously designed RCTs are required to verify the benefits and to explore the optimal protocol of Tai Chi exercise for bone health.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=309148, identifier: CRD42022309148.
Post-menopause is a period of women's life following the permanent cessation of the menstrual cycles, during which time the women's bone health is threatened due to the decrease and cessation of ovarian estrogen secretion (Cauley, 2015). Bone mineral density (BMD) decreases rapidly during the menopause transition and continues to decline in post-menopause. According to a cohort study involving 1,038 women (Shieh et al., 2022), each additional year after the final menstrual period was associated with 0.006 and 0.004 g/cm2 lower BMD of lumbar spine and femoral neck, respectively. The 10-year cumulative loss of BMD was 10.6% at the lumbar spine and 9.1% at the femoral neck (Cauley, 2015). Low BMD was one of the most important determinants of fracture risk (Barron et al., 2020). Approximately 30–40% of postmenopausal women were reported to have osteoporosis or low bone mass (Wright et al., 2014; Thulkar et al., 2016), and more than 30% experienced at least one fracture (Lippuner et al., 2009; Si et al., 2015; Jiang and Ni, 2016). Almost every fracture was associated with an increased risk of premature mortality (Center, 2017). Researchers found mortality increased over 2.43- and 1.82-fold following hip fractures and vertebral fractures in community-dwelling older women, respectively (Bliuc et al., 2009). Therefore, effective intervention to prevent and attenuate bone loss in postmenopausal women is necessary.
Bone is a dynamic tissue, with a capacity to remodel its material and structural properties to adapt mechanical loading (Feng and McDonald, 2011). Increased loading stimuli and vigorous muscular activity can augment bone mass and promote bone health (Wang et al., 2020). Therefore, exercise is recommended to maintain bone mass or slow bone loss for postmenopausal women (Daly et al., 2019; Kanis et al., 2019; Society, 2021). High impact and high weight-bearing exercises were found to be beneficial for postmenopausal women to increase BMD (Martyn-St James and Carroll, 2006; Kelley et al., 2012; Zhao et al., 2015; Kitsuda et al., 2021). However, due to safety and operability concerns, it's difficult to implement such exercise patterns for post-menopause women.
Tai Chi, a traditional Chinese exercise, is becoming popular around the world. According to the theory of traditional Chinese medicine, Tai Chi can promote the circulation of Qi and blood. Tai Chi is characterized by coordinated body posture and movements, deep rhythmic breathing, and meditation (Yeung et al., 2018). During Tai Chi practice, practitioners perform a series of slow and rhythmic circular motions and a lot of half-squats, and gravity-shift movements, which may introduce dynamic loading on bone. Evidence showed Tai Chi can prevent falls, enhance flexibility and improve balance function with good security (Del-Pino-Casado et al., 2016; Zhong et al., 2020). In addition, it is an easily acceptable exercise that can be practiced anywhere and anytime without special equipment. Therefore, Tai Chi may be a promising exercise to prevent and reduce bone loss in postmenopausal women.
Recently, Zhang et al. (2021) conducted a network meta-analysis and found mind-body exercise (e.g. Tai Chi, yoga, dance, Wuqinxi) might be an optimal exercise type to increase the BMD of the lumbar spine and femoral neck among patients with osteoporosis and osteopenia. Previous two systematic reviews (SRs) of Tai Chi for BMD in postmenopausal women had been published in 2016 (Sun et al., 2016) and 2017 (Liu and Wang, 2017) respectively, but their conclusions were contradictory. As more relevant trials have been conducted in recent years, we performed this meta-analysis of randomized controlled trials (RCTs) to update the evidence about the effect and safety of Tai Chi on bone health in postmenopausal women and used the trial sequential analysis (TSA) to assess the reliability of the evidence.
The protocol of this meta-analysis and TSA has been registered on the International Prospective Register of Systematic Reviews (PROSPERO) (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=309148) (Registration No: CRD42022309148). We conducted this meta-analysis and TSA according to A Measurement Tool to Assess Systematic Reviews (AMSTAR 2) and reported in the light of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 statement (Appendix 1).
Reviewers (YXL and DLZ) searched PubMed, Embase, The Cochrane Library, China National Knowledge Infrastructure (CNKI), Chinese Science and Technology Periodical Database (VIP), Chinese Biomedical Literature Database (CBM), and Wanfang Database from their inceptions to 11 May 2022. According to the retrieval rules of each database, the search strategies were developed by combining Medical Subject Headings (MeSH) and free text words of Tai Chi and bone density. To identify more potential studies, we manually searched gray literature, reference lists of identified studies, and relevant registration websites (ClinicalTrials.gov and www.chictr.org.cn), and consulted experts in this field. The full search strategies for all databases are shown in Appendix 2.
We included RCTs published in Chinese and English which studied the effect or/and safety of Tai Chi on bone health in postmenopausal women.
Postmenopausal women (author reported) or women (≥ 50 years old) (Wang et al., 2021) were included. There was no restriction on race or nation.
We included RCTs that used Tai Chi (e.g. Tai Chi Quan, Tai Chi push hands, Tai Chi sword, etc.), or Tai Chi combined anti-osteoporosis medications (e.g. bisphosphonates, denosumab, calcitonin, etc.) or nutraceutical (e.g. calcium and vitamin D, etc.) as the experimental group. There were no restrictions on the duration and frequency of Tai Chi.
Participants in the control group received non-intervention, anti-osteoporosis drug, nutraceutical, or other exercises (e.g. walking, running, resistance training, etc.).
The primary outcome included BMD using dual-energy x-ray absorptiometry (lumbar spine, femoral neck, trochanter, Ward's triangle, and total hip). Secondary outcomes were indicators related to bone health, including: 1) Calcaneus quantitative ultrasound: BMD of the calcaneus, bone quality index, broadband ultrasound attenuation, speed of sound; 2) Bone turnover markers: serum bone formation markers: procollagen type I N-terminal propeptide (PINP), alkaline phosphatase (ALP), bone-specific alkaline phosphatase (BAP), osteocalcin (OSC), etc.; serum bone resorption markers: C-terminal telopeptide of type I collagen (CTX), tartrate-resistant acid phosphatase (TRAP), etc.; 3) Tai Chi-related adverse events.
Studies were excluded if they met any of the following conditions: 1) Cross-sectional studies, reviews, case-control studies, N of one RCTs (Li et al., 2022); 2) Full text or the data cannot be obtained through various approaches; 3) Repeated publications.
All the retrieved records were imported into Endnote software (X9), and duplicates were removed. Two independent reviewers (LXZ and TL) screened the rest records by reading titles and abstracts. Then, full texts of all potential studies were obtained and scrutinized. After that, the two reviewers cross-checked the included studies. In case of disagreements, a third reviewer (JL) was involved. If there were multiple publications from the same study, we included the publication with more complete data or included multiple publications with complementary data.
Two reviewers (CZJ and RF) independently extracted the following data: 1) Study characteristics: first author, publication year, country, sample size; 2) Participants' characteristics at study level: age, menopausal duration; 3) Interventions: frequency, duration, and style of Tai Chi; 4) Comparators: type, dosage, frequency and duration of medication or nutraceutical; frequency, duration, type of other exercises; 5) Outcomes: primary outcome, secondary outcomes, and adverse events; 6) Information related to the risk of bias. Then two reviewers cross-checked the extracted data to ensure no mistakes. We resolved discrepancies through group discussion or with the participation of a third reviewer (JL). For multi-arm RCTs, we included the eligible comparisons or extracted the comparison with inferior effect size to obtain more conservative results.
We contacted the original authors via email for more information if the necessary data was missing or incomplete. If there was no reply, we analyzed the available data.
Two independent reviewers (XBL and TYL) used the revised Cochrane risk-of-bias tool for randomized trials (ROB 2) to assess the risk of bias of included studies from five domains: the randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Each domain was judged as “low risk,” “some concerns,” or “high risk” according to corresponding algorithms. After learning the Cochrane risk-of-bias tool and pre-assessed, two independent reviewers assessed the risk of bias and then cross-checked. Two reviewers discussed the disagreements or consulted with a third reviewer (RJJ).
Among the included studies, three comparisons were involved, including Tai Chi vs. non-intervention, Tai Chi vs. other exercises, and Tai Chi plus nutraceutical vs. nutraceutical. For continuous variable, we used the post-intervention data. Since included outcomes for meta-analysis used the same units, we calculated the mean difference (MD). We conducted descriptive analysis for the data which couldn't be quantitatively analyzed. Heterogeneity was measured by the chi-squared test and I2 statistic. When P < 0.1 or I2 values > 50%, the random-effect model was used to pool data. Otherwise, the fixed-effect model was performed. Forest plots and tables were utilized to present the pooled results. RevMan software (version 5.4.1) and R software (version 3.6.1) were used for data synthesis.
Subgroup analyses of Tai Chi vs. non-intervention were conducted according to the duration of Tai Chi ( ≤ 6 or > 6 months).
We performed sensitivity analysis by eliminating studies one by one to verify the robustness of the results.
We used a funnel plot and Egger's test to detect publication bias when ≥10 studies with the same outcome were included in the analysis.
We conducted TSA for primary outcome using the TSA software (version 0.9.5.10-Beta). Fixed effects model with a maximum type I error of 5%, and a maximum type II error of 20% (80% power) were applied. Two-sided significance testing boundaries, required information size, trial sequential monitoring boundaries, futility boundaries, and cumulative z-score were presented in the TSA graph. The situation that included sample size over required information size, or the cumulative Z curve crossed the trial sequential monitoring boundaries or futility boundaries indicated that the results were reliable.
We applied the Grading of recommendations assessment, development, and evaluation (GRADE) system to assess the certainty of evidence. Each outcome was evaluated from the following five aspects: limitations, inconsistency, indirectness, imprecision, and publication bias. Then the certainty of evidence was accordingly graded as “high,” “moderate,” “low,” or “very low” (Balshem et al., 2011). GRADEpro (version 3.6) software was used to present the summary of findings.
A total of 1,506 records were searched from databases and three records from websites. After removing 538 duplicated records, we further excluded irrelevant 839 records. Finally, we included 25 reports (Qin et al., 2000; Zhou, 2003, 2004; Chan et al., 2004; Zhou et al., 2005; Gao, 2006; Woo et al., 2007; Mao, 2009; Liu, 2010; Shen et al., 2010, 2012; Song et al., 2010, 2018; Zhu, 2011; Wayne et al., 2012; Kuo et al., 2014; Yu et al., 2014; Lu and Song, 2015; Wang et al., 2015; Xue, 2015; Ye et al., 2016; Xu, 2017; Cheng and Ba, 2020; Zhang, 2020; Zou, 2020), involving 24 studies through full-text reading (Figure 1). The list of excluded records with reasons is provided in Appendix 3. Shen et al. (2010, 2012) pertained to the same study. Among included studies, two studies was undertaken in America (Shen et al., 2010, 2012; Wayne et al., 2012), one from South Korea (Song et al., 2010), and the others were in China. Eight reports were published in English journals (Chan et al., 2004; Woo et al., 2007; Shen et al., 2010, 2012; Song et al., 2010; Wayne et al., 2012; Wang et al., 2015; Cheng and Ba, 2020), 9 were in Chinese journals (Zhou, 2003, 2004; Zhou et al., 2005; Mao, 2009; Yu et al., 2014; Lu and Song, 2015; Ye et al., 2016; Xu, 2017; Song et al., 2018), six were master's theses (Gao, 2006; Liu, 2010; Zhu, 2011; Xue, 2015; Zhang, 2020; Zou, 2020), and two were conference abstracts (Qin et al., 2000; Kuo et al., 2014). The duration of Tai Chi practice ranged from 2 to 24 months, and sample size varied from 16 to 344. Sixteen studies evaluated the BMD by dual-energy x-ray absorptiometry (Qin et al., 2000; Zhou, 2003, 2004; Chan et al., 2004; Zhou et al., 2005; Woo et al., 2007; Mao, 2009; Song et al., 2010, 2018; Wayne et al., 2012; Kuo et al., 2014; Yu et al., 2014; Wang et al., 2015; Ye et al., 2016; Xu, 2017; Cheng and Ba, 2020), six used calcaneus quantitative ultrasound (Gao, 2006; Liu, 2010; Zhu, 2011; Lu and Song, 2015; Zhang, 2020; Zou, 2020), and four observed the change of bone turnover markers (Liu, 2010; Shen et al., 2010, 2012; Wayne et al., 2012; Xue, 2015). Table 1 provides the characteristics of included studies.
Seven studies (Woo et al., 2007; Song et al., 2010, 2018; Wayne et al., 2012; Lu and Song, 2015; Ye et al., 2016; Xu, 2017) specified the methods of randomization, and all studies did not provide information about allocation concealment. Seventeen studies (Qin et al., 2000; Zhou, 2003; Chan et al., 2004; Woo et al., 2007; Liu, 2010; Shen et al., 2010, 2012; Song et al., 2010, 2018; Wayne et al., 2012; Kuo et al., 2014; Yu et al., 2014; Lu and Song, 2015; Wang et al., 2015; Xue, 2015; Ye et al., 2016; Cheng and Ba, 2020; Zhang, 2020) reported the number of drop-outs or lost to follow-up. Two (Shen et al., 2010; Wayne et al., 2012) studies performed the intent-to-treat analysis and the remaining studies used per-protocol analysis. The primary and secondary outcomes were objective indicators. Two studies (Shen et al., 2010, 2012; Wayne et al., 2012) provided the registration numbers. In summary, four studies (Qin et al., 2000; Liu, 2010; Yu et al., 2014; Ye et al., 2016) were considered as high overall risk of bias, and the rest of the studies were rated as some concerns. The results of the ROB assessment are shown in Figure 2.
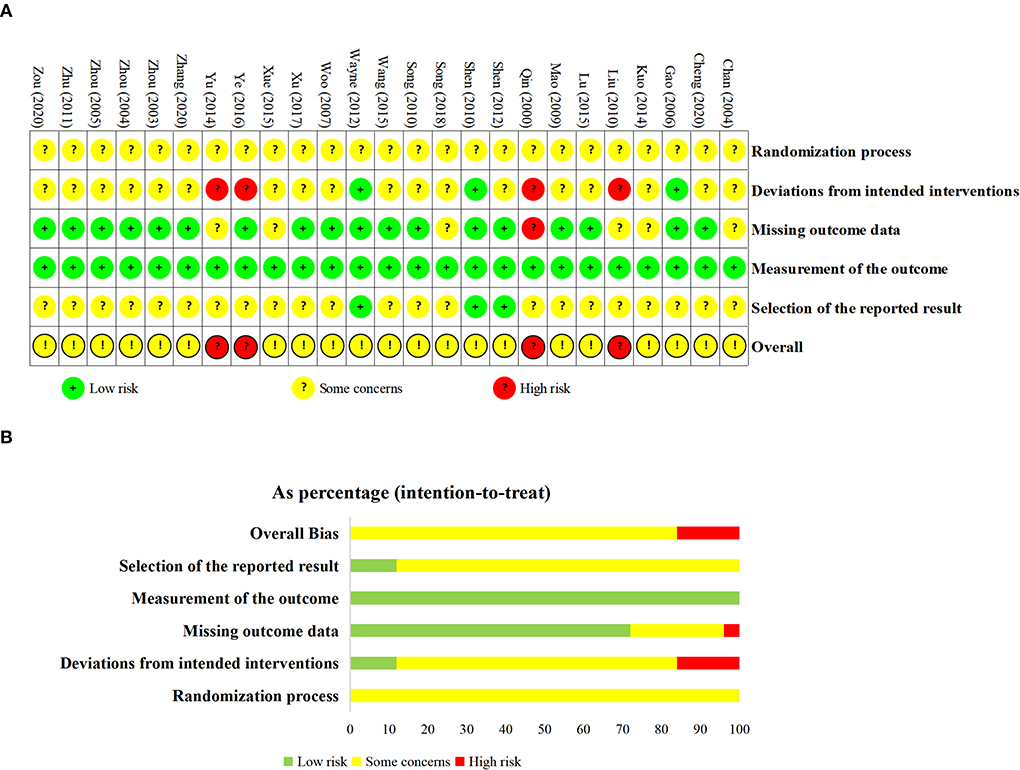
Figure 2. Results of risk of bias assessment. (A) the domain and overall judgments study-by-study; (B) proportions of studies at low risk, some concerns or high risk of bias for each domain.
Compared with non-intervention group, participants in Tai Chi group had higher BMD of lumbar spine (MD = 0.04, 95% CI 0.02 to 0.07, P < 0.0001, I2 = 0%), femoral neck (MD = 0.04, 95% CI 0.02 to 0.06, P < 0.0001, I2 = 0%), and trochanter (MD = 0.02, 95% CI 0.00 to 0.03, P = 0.04, I2 = 0%). Notwithstanding, there was no difference between Tai Chi and non-intervention group in the BMD of Ward's triangle (MD = 0.02, 95% CI −0.01 to 0.04, P = 0.18, I2 = 0%) (Figure 3).
Results of BMD in the lumbar spine, femoral neck, and Ward's triangle were stable after excluding studies one by one. But the pooled result of trochanter altered to insignificant after excluding Chan et al. (2004) (MD = 0.02, 95% CI −0.00 to 0.04, P = 0.10, I2 = 0%) or Xu (2017) (MD = 0.02, 95% CI −0.00 to 0.03, P = 0.11, I2 = 0%). The plots of sensitivity analysis results are shown in Figure S1 in Appendix 4.
Three studies (Qin et al., 2000; Woo et al., 2007; Yu et al., 2014) evaluated the percentage change of BMD. No differences between Tai Chi and non-intervention group were found in the percentage change of BMD in lumbar spine (MD = 0.83, 95% CI −0.12 to 1.77, P = 0.09, I2 = 28%), Ward's triangle (MD = 1.81, 95% CI −0.28 to 3.90, P = 0.09, I2 = 31%) and trochanter (MD = −0.07, 95% CI −1.35 to 1.22, P = 0.92, I2 = 0%) (Figure S2 in Appendix 4). Two studies reported that the percentage change of BMD of femoral neck (Qin et al., 2000) and total spine (Woo et al., 2007) in the Tai Chi group did not differ from the non-intervention group. However, Woo et al. (2007) found that Tai Chi could attenuate greater BMD loss of total hip than non-intervention.
One study (Song et al., 2010) showed that the improvement of BMD T score of femoral neck, Ward's triangle, and trochanter was significantly higher in the Tai Chi group than that in the education program group.
There were no differences between Tai Chi and other exercises in increasing BMD of lumbar spine (MD = 0.01, 95% CI −0.04 to 0.07, P = 0.63, I2 = 0%) (Figure 4). The result did not change during sensitivity analysis (Figure S3 in Appendix 4).
Song et al. (2018) observed Tai Chi did not differ from brisk walking in improving the BMD of femoral neck, Ward's triangle and trochanter. Woo et al. (2007) found no difference existed in the percentage change of BMD of total hip between Tai Chi and resistance exercise group, and resistance exercise increased more BMD of total spine than Tai Chi. Kuo et al. (2014) reported that Tai Chi plus calcium and vitamin D supplements was not superior to circuit training program (aerobic training, resistance training, and stretching) plus calcium and vitamin D supplements in increasing BMD of femoral neck and lumbar spine.
No significant difference between Tai Chi plus nutraceutical and nutraceutical was found in BMD of lumbar spine (MD = 0.01, 95% CI −0.03 to 0.05, P = 0.60, I2 = 0%) (Figure 5). The results remained unchanged according to the sensitivity analysis (Figure S4 in Appendix 4).
Kuo et al. (2014) observed that the BMD of femoral neck did not differ significantly between Tai Chi plus nutraceutical group and nutraceutical group. Wayne et al. (2010) reported there was no difference in BMD of lumbar spine, femoral neck, and total hip between Tai Chi plus standard care and standard care group.
Compared with the non-intervention group, the Tai Chi group had a significantly greater speed of sound, while had no difference in BMD of calcaneus, broadband ultrasonic attenuation, and bone quality index (Table 2). Based on sensitivity analysis, the results of speed of sound (MD = 17.09, 95% CI −1.09 to 35.28, P = 0.07, I2 = 0%) became non-significant after excluding Gao (2006) (Figure S5 in Appendix 4).
There were no significant differences in the BMD of calcaneus, speed of sound, broadband ultrasonic attenuation, and bone quality index between Tai Chi and other exercises (Table 2). And the above results did not alter after excluding studies one by one. The plots of sensitivity analysis are shown in Figure S6 in Appendix 4.
Xue (2015) found that the Tai Chi plus education group had a higher level of serum PINP than the education group, but there was no difference in the level of serum CTX. Liu (2010) observed no difference of the comparisons of Tai Chi vs. non-intervention and Tai Chi vs. brisk walking in the level of serum ALP. Two articles reported Tai Chi plus nutraceutical group was not superior to the nutraceutical group in the level of serum ALP (Shen et al., 2010), BAP (Shen et al., 2012), TRAP (Shen et al., 2012). There were no differences between Tai Chi plus standard care and standard care in level of serum OSC (Wayne et al., 2012) and CTX (Wayne et al., 2012).
Compared with non-intervention, practicing Tai Chi for more than 6 months showed greater BMD of the lumbar spine, femoral neck, and trochanter, while practicing it for less than or equal to 6 months was not superior to non-intervention in increasing BMD of the lumbar spine, femoral neck, and Ward's triangle (Table 3). The forest plots of subgroup analyses are shown in Figure S7 in Appendix 4.
Four studies (Shen et al., 2010, 2012; Wayne et al., 2012; Wang et al., 2015; Xue, 2015) stated no adverse events were attributed to Tai Chi practice. Chan et al. (2004) reported that one proximal fibular fracture occurred in the Tai Chi group due to a fall. Woo et al. (2007) observed no significant difference in the number of falls between Tai Chi, resistance exercise, and non-intervention groups during the study period. The remaining studies did not provide any information about adverse events.
According to TSA of Tai Chi vs. non-intervention, the included sample size reached the required information size in BMD of the lumbar spine (508 vs. 197) and femoral neck (390 vs. 197). Therefore, there was sufficient evidence favoring the effect of Tai Chi on BMD of the lumbar spine and femoral neck. However, the included sample size of BMD of Ward's triangle (287 vs. 785) and trochanter (282 vs. 785) did not achieve the required information size, and their cumulative Z curves did not cross the trial sequential monitoring boundaries or futility boundaries. Thus more studies are needed to verify the effect of Tai Chi on Ward's triangle and trochanter (Appendix 5).
Ten studies reported the BMD of lumbar spine of Tai Chi vs. non-intervention, thus we evaluated the publication bias. The funnel plot (Figure 6) and Egger's test (P = 0.17) suggested no evidence of publication bias existed.
The results of certainty of evidence are shown in Appendix 6. The certainty of evidence for three outcomes (BMD of the lumbar spine and femoral neck of Tai Chi vs. non-intervention, and BMD of the lumbar spine of Tai Chi practicing for over 6 months vs. non-intervention) was graded as low. The evidence of the remaining outcomes was rated as very low certainty. The reasons for downgrading were mainly attributed to the risk of bias of included studies, imprecision and publication bias.
In this meta-analysis and TSA, we included 24 studies that investigated the effect and safety of Tai Chi on bone health in postmenopausal women. We found that Tai Chi training was superior to non-intervention in improving BMD of the lumbar spine and femoral neck, and the above evidence was reliable according to TSA. Tai Chi might improve the BMD of trochanter better than non-intervention, but sensitivity analysis and TSA indicated the result needed further verification. There were no significant differences in BMD of the lumbar spine, femoral neck, trochanter, and Ward's triangle when comparing Tai Chi with other exercises. Tai Chi plus nutraceuticals also did not differ from nutraceuticals in improving BMD of the lumbar spine and femoral neck. Insufficient data was obtained to support the effect of Tai Chi on bone turnover markers and calcaneus quantitative ultrasound. Subgroup analysis demonstrated that practicing Tai Chi for over 6 months improved more BMD of the lumbar spine, femoral neck, and trochanter than non-intervention. The certainty of evidence was low for three outcomes, including the BMD of the lumbar spine and femoral neck of Tai Chi vs. non-intervention and the BMD of the lumbar spine of Tai Chi practicing for over 6 months vs. non-intervention. The certainty of evidence of the rest outcomes was very low. Few Tai Chi-related adverse events occurred.
Previous relevant SRs hold contradictory conclusions. Liu and Wang (2017) included 350 participants from six studies published up to 2016 and concluded that Tai Chi was not effective to attenuate BMD loss of the lumbar spine and femoral neck in postmenopausal women. Sun et al. (2016) pooled data from six studies before May 2015 and reported that Tai Chi had a significant effect on BMD of the lumbar spine when compared with no treatment, which was consistent with our results. While, Sun et al. (2016) included perimenopausal and postmenopausal women. Furthermore, Sun et al. (2016) double-counted the participants in the control group from a 3-arm study (Zhou, 2004), which might introduce a unit-of-analysis error (Rücker et al., 2017). Compared to Sun et al. (2016) and Liu and Wang (2017), we updated more RCTs, introduced more outcomes, validated results with TSA, and confirmed the effect of Tai Chi on BMD of lumbar spine and femoral neck in postmenopausal women.
During Tai Chi exercise, the practitioners hold a half-squat posture and switch between double-stance and single-stance weight-bearing, along with pivoting and twisting the trunk. Researchers found Tai Chi movements could produce vertical weight-bearing force and activate the lumbar erector spine muscle and lower extremity muscle (Chan et al., 2003; Wu and Hitt, 2005). Compared with a normal gait, the Tai Chi gait had a greater peak shear force and larger frontal-plane joint moment in the hip (Wu and Millon, 2008; Yang and Liu, 2020). Previous meta-analysis (Yang et al., 2021) demonstrated that Tai Chi could improve the thoracolumbar spine flexibility and enhance lower limb muscle strength. In our study, we found Tai Chi increased more BMD of the lumbar spine, femoral neck, and trochanter. However, sensitivity analysis suggested the effect of Tai Chi for the BMD in trochanter was unstable. Additionally, Tai Chi was not superior to non-intervention in improving the BMD of Ward's triangle. We speculated that the reason might be related to the small sample size.
In our study, Tai Chi-induced BMD gain in the lumbar spine and femoral neck was 0.04 g/cm2 when compared with non-intervention. Since the minimum clinically important difference (MCID) for BMD was not reported, we failed to determine the clinical significance. While Chen et al. (2006) found that an increase in lumbar spine BMD of 0.09 g/cm2 reduced the risk of vertebral fracture in postmenopausal women with osteoporosis by 30–41%, Jacques et al. (2012) reported that among postmenopausal women with osteoporosis, patients with 3-year increase in BMD of 0–0.032 and 0.032 g/cm2 were 0.48 and 0.27 times more likely to suffer from vertebral fracture than those with change of BMD <0 g/cm2, respectively. Future studies are needed to establish an MCID for BMD of different sites in postmenopausal women.
During bone remodeling, bone resorption lasts 4–6 weeks and subsequently bone formation maintains 4–5 months (Eastell and Szulc, 2017). Thus, in the previous SRs exploring the effect of exercise on BMD (Zhao et al., 2014, 2015; Kemmler et al., 2020; Mohammad Rahimi et al., 2020), they preferred to include trials in which exercise lasted for at least 6 months. Our results also found that practicing Tai Chi for less than or equal to 6 months had no effect on BMD while practicing Tai Chi over 6 months could improve more BMD than non-intervention. However, it must be acknowledged that our subgroup analysis of Tai Chi practicing for less than or equal to 6 months vs. non-intervention included few RCTs, which might decrease the statistical power.
Among included studies, the control exercises involved aerobic exercise combined with resistance training (Kuo et al., 2014), rope skipping (Zhou, 2004), running combined with walking (Zhou, 2003), and brisk walking (Song et al., 2018). These exercises were reported to improve BMD in premenopausal women (Pellikaan et al., 2018; Kemmler et al., 2020; Lan and Feng, 2022). Our results showed that Tai Chi was an effective exercise to increase BMD of lumbar spine and femoral neck, but no better than other exercises. Results of a network meta-analysis (Zhang et al., 2021) showed that mind-body exercise was the optimal exercise type to improve the BMD of the lumbar spine and femoral neck, while aerobic exercise and resistance exercise had a better effect on BMD of the total hip than mind-body exercise. It was inferred that different exercise patterns might have advantages in improving the BMD of different sites.
Previous studies demonstrated that nutraceuticals, such as calcium and vitamin D supplements might increase BMD of the lumbar spine and femoral neck among postmenopausal women with osteoporosis (Liu et al., 2020). However, nutraceuticals did not decrease the risk of fractures among community-dwelling older adults (Zhao et al., 2017). Propensity to fall was a significant risk factor for fracture. Tai Chi was reported to improve balance and reduce the incidence of falls in older people by 30% (Li et al., 2018; Zhong et al., 2020). Therefore, it's believed that a combination of Tai Chi and nutraceutical may have potential advantages to prevent falls and fractures.
Calcaneal quantitative ultrasound is an alternative approach to assess bone health, which was suggested for pre-screening and risk evaluation for osteoporosis (Gao et al., 2021; Yen et al., 2021). Notwithstanding, Frost et al. (2001) found that the precision of calcaneal quantitative ultrasound was not good enough to be used for monitoring response to treatment. Moreover, the Chinese Society of Osteoporosis and Bone Mineral Research did not recommend to use quantitative ultrasound for the evaluation of intervention efficacy (Xia et al., 2019). In our study, the results of calcaneal quantitative ultrasound seemed to be erratic, and high heterogeneity existed among studies. Therefore, researchers should combined calcaneal quantitative ultrasound with other more sensitive detection methods (e.g. dual-energy x-ray absorptiometry) to assess the response to intervention.
Due to limited included studies, we failed to confirm the effect of Tai Chi on bone turnover marks quantitatively. Xue (2015) observed that Tai Chi could improve the level of serum PINP. PINP is recommended as the preferred bone formation marker. That might indicate that Tai Chi can promote bone formation to improve the BMD. However, we found Tai Chi had no effect on other bone turnover markers. A recent SR (Kistler-Fischbacher et al., 2021) summarized that there was limited evidence to favor the effect of low-moderate-intensity exercise on bone turnover markers. Future studies can focus on this issue.
This is the latest meta-analysis of Tai Chi for bone health in postmenopausal women and we performed TSA to explore whether the evidence in our meta-analysis was reliable. However, some limitations should be considered. Firstly, the BMD is a surrogate endpoint for fracture risk, and the MCIDs of BMD of different sites were unclear. Therefore, whether the improvement of BMD that we found would lead to eventual clinical benefits is unknown. Secondly, the optimal protocol of Tai Chi training was not yet been investigated. Thirdly, the majority of included participants were Chinese women, which might limit the general applicability of these results.
Tai Chi may be an optional and safe exercise for improving BMD loss in postmenopausal women, and practicing Tai Chi for more than 6 months may yield greater benefits. However, more rigorously designed RCTs are required to verify the benefits and to explore the optimal protocol of Tai Chi exercise for bone health.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
RJ and JL conceptualized the study and provided methodological support. YL and DZ designed the search strategy. LZ and TaL selected the studies. CJ and RF extracted the data. XL and TiL assessed the risk of bias. XL, CJ, and RF wrote and edited the manuscript. All authors contributed to the article and approved the submitted version.
This work was financially funded by the National Natural Science Foundation of China (No: 81873356), the Science and technology project of Sichuan Province (No: 2020YFS0283), Sichuan Province Science and Technology Support Program in Sichuan (No: 2014SZ0154), 2021 Education and Scientific Research Project of National Higher Education of Traditional Chinese Medicine in the 14th Five-Year Plan (No: YB-20-13), and National Natural Science Foundation of China (No: 82104976).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2022.935326/full#supplementary-material
Balshem, H., Helfand, M., Schünemann, H. J., Oxman, A. D., Kunz, R., Brozek, J., et al. (2011). GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 64, 401–406. doi: 10.1016/j.jclinepi.2010.07.015
Barron, R. L., Oster, G., Grauer, A., Crittenden, D. B., and Weycker, D. (2020). Determinants of imminent fracture risk in postmenopausal women with osteoporosis. Osteoporos. Int. 31, 2103–2111. doi: 10.1007/s00198-020-05294-3
Bliuc, D., Nguyen, N. D., Milch, V. E., Nguyen, T. V., Eisman, J. A., and Center, J. R. (2009). Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301, 513–521. doi: 10.1001/jama.2009.50
Cauley, J. A. (2015). Estrogen and bone health in men and women. Steroids 99(Pt A), 11–15. doi: 10.1016/j.steroids.2014.12.010
Center, J. R. (2017). Fracture burden: what two and a half decades of dubbo osteoporosis epidemiology study data reveal about clinical outcomes of osteoporosis. Curr. Osteoporos. Rep. 15, 88–95. doi: 10.1007/s11914-017-0352-5
Chan, K., Qin, L., Lau, M., Woo, J., Au, S., Choy, W., et al. (2004). A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Arch. Phys. Med. Rehabil. 85, 717–722. doi: 10.1016/j.apmr.2003.08.091
Chan, S. P., Luk, T. C., and Hong, Y. (2003). Kinematic and electromyographic analysis of the push movement in tai chi. Br. J. Sports Med. 37, 339–344. doi: 10.1136/bjsm.37.4.339
Chen, P., Miller, P. D., Delmas, P. D., Misurski, D. A., and Krege, J. H. (2006). Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J. Bone Miner. Res. 21, 1785–1790. doi: 10.1359/jbmr.060802
Cheng, L., and Ba, H. (2020). Effect of Tai Chi exercise with the same frequency and different exercise duration on the bone mineral density of older women. J. Sports Med. Phys. Fitness 60, 1396–1400. doi: 10.23736/S0022-4707.20.10940-X
Daly, R. M., Dalla Via, J., Duckham, R. L., Fraser, S. F., and Helge, E. W. (2019). Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz. J. Phys. Ther. 23, 170–180. doi: 10.1016/j.bjpt.2018.11.011
Del-Pino-Casado, R., Obrero-Gaitán, E., and Lomas-Vega, R. (2016). The effect of Tai Chi on reducing the risk of falling: a systematic review and meta-analysis. Am. J. Chin. Med. 44, 895–906. doi: 10.1142/S0192415X1650049X
Eastell, R., and Szulc, P. (2017). Use of bone turnover markers in postmenopausal osteoporosis. Lancet Diabetes Endocrinol 5, 908–923. doi: 10.1016/S2213-8587(17)30184-5
Feng, X., and McDonald, J. M. (2011). Disorders of bone remodeling. Annu. Rev. Pathol. 6, 121–145. doi: 10.1146/annurev-pathol-011110-130203
Frost 2001, Frost, M. L., Blake, G. M., Fogelman, et al. (2001). Changes in QUS and BMD measurements with antiresorptive therapy: a two-year longitudinal study. Calcif. Tissue Int. 69, 138–146. doi: 10.1007/s002230020037
Gao, C., Song, H., Chen, B., Zhang, Z., and Yue, H. (2021). The Assessment of the osteoporosis self-assessment tool for asians and calcaneal quantitative ultrasound in identifying osteoporotic fractures and falls among chinese people. Front. Endocrinol. 12, 684334. doi: 10.3389/fendo.2021.684334
Gao, Y. (2006). The Comparison Research on Influence Different Exercise Ways of Exercise Prescription to Body Function of Middle and Aged Women (Master Dissertation). Shaanxi Normal University.
Jacques, R. M., Boonen, S., Cosman, F., Reid, I. R., Bauer, D. C., Black, D. M., et al. (2012). Relationship of changes in total hip bone mineral density to vertebral and nonvertebral fracture risk in women with postmenopausal osteoporosis treated with once-yearly zoledronic acid 5 mg: the HORIZON-Pivotal Fracture Trial (PFT). J. Bone Miner. Res. 27, 1627–1634. doi: 10.1002/jbmr.1644
Jiang, Y., and Ni, W. (2016). Expected lifetime numbers, risks, and burden of osteoporotic fractures for 50-year old Chinese women: a discrete event simulation incorporating FRAX. J. Bone Miner. Metab. 34, 714–722. doi: 10.1007/s00774-015-0724-9
Kanis, J. A., Cooper, C., Rizzoli, R., and Reginster, J. Y. (2019). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 30, 3–44. doi: 10.1007/s00198-018-4704-5
Kelley, G. A., Kelley, K. S., and Kohrt, W. M. (2012). Effects of ground and joint reaction force exercise on lumbar spine and femoral neck bone mineral density in postmenopausal women: a meta-analysis of randomized controlled trials. BMC Musculoskelet. Disord. 13, 177. doi: 10.1186/1471-2474-13-177
Kemmler, W., Shojaa, M., Kohl, M., and von Stengel, S. (2020). Effects of different types of exercise on bone mineral density in postmenopausal women: a systematic review and meta-analysis. Calcif. Tissue Int. 107, 409–439. doi: 10.1007/s00223-020-00744-w
Kistler-Fischbacher, M., Weeks, B. K., and Beck, B. R. (2021). The effect of exercise intensity on bone in postmenopausal women (part 1): a systematic review. Bone 143, 115696. doi: 10.1016/j.bone.2020.115696
Kitsuda, Y., Wada, T., Noma, H., Osaki, M., and Hagino, H. (2021). Impact of high-load resistance training on bone mineral density in osteoporosis and osteopenia: a meta-analysis. J. Bone Miner. Metab. 39, 787–803. doi: 10.1007/s00774-021-01218-1
Kuo, L. T., Hsu, R. W. W., Hsu, W. H., and Lin, Z. R. (2014). The comparison of impact of circuit exercise training and Tai-Chi exercise on multiple fracture-related risk factors in postmenopausal osteopenic women. J. Clin. Densitometry 17, 427–428. doi: 10.1016/j.jocd.2014.04.102
Lan, Y. S., and Feng, Y. J. (2022). The volume of brisk walking is the key determinant of BMD improvement in premenopausal women. PLoS ONE 17, e0265250. doi: 10.1371/journal.pone.0265250
Li, F., Harmer, P., Fitzgerald, K., Eckstrom, E., Akers, L., Chou, L. S., et al. (2018). Effectiveness of a Therapeutic Tai Ji Quan Intervention vs a Multimodal exercise intervention to prevent falls among older adults at high risk of falling: a randomized clinical trial. JAMA Intern. Med. 178, 1301–1310. doi: 10.1001/jamainternmed.2018.3915
Li, Y. F., Chu, X. J., Lu, C. C., Han, J. N., Zheng, Z. L., Li, X. X., et al. (2022). Interpretation of SPIRIT extension for N-of-1 trials (SPENT 2019). Chin. J. Evidence Based Med.22, 475–482. doi: 10.7507/1672-2531.202112091
Lippuner, K., Johansson, H., Kanis, J. A., and Rizzoli, R. (2009). Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos. Int. 20, 1131–1140. doi: 10.1007/s00198-008-0779-8
Liu, C., Kuang, X., Li, K., Guo, X., Deng, Q., and Li, D. (2020). Effects of combined calcium and vitamin D supplementation on osteoporosis in postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. Food Funct. 11, 10817–10827. doi: 10.1039/D0FO00787K
Liu, D. (2010). Effect of Tai Chi and brisk Walking exercise on bone mass in the middle-aged elderly women (Master Dissertation). Shandong Institute of Physical Education and sports.
Liu, F., and Wang, S. (2017). Effect of Tai Chi on bone mineral density in postmenopausal women: a systematic review and meta-analysis of randomized control trials. J. Chin. Med. Assoc. 80, 790–795. doi: 10.1016/j.jcma.2016.06.010
Lu, T., and Song, Q. H. (2015). Effects of Tai Chi quan, walking and dancing on muscle strength, bone mineral density and balance ability of lower limbs in elderly women. Chin. J. Phys. Med. Rehabil. 37, 124–127. doi: 10.3760/cma.j.issn.0254-1424.2015.02.012
Mao, H. N. (2009). Effects of taijiquan exercises combined with orally calcium supplement on postmenopausal women's bone mineral density. Chin. J. Rehabil. Med. 24, 814–816. doi: 10.3969/j.issn.1001-1242.2009.09.022
Martyn-St James, M., and Carroll, S. (2006). High-intensity resistance training and postmenopausal bone loss: a meta-analysis. Osteoporos. Int. 17, 1225–1240. doi: 10.1007/s00198-006-0083-4
Mohammad Rahimi, G. R., Smart, N. A., Liang, M. T. C., Bijeh, N., Albanaqi, A. L., Fathi, M., et al. (2020). The impact of different modes of exercise training on bone mineral density in older postmenopausal women: a systematic review and meta-analysis research. Calcif. Tissue Int. 106, 577–590. doi: 10.1007/s00223-020-00671-w
Pellikaan, P., Giarmatzis, G., Vander Sloten, J., Verschueren, S., and Jonkers, I. (2018). Ranking of osteogenic potential of physical exercises in postmenopausal women based on femoral neck strains. PLoS ONE 13, e0195463. doi: 10.1371/journal.pone.0195463
Qin, L., Chen, Q. M., Qu, S. Q., Cai, Y. Y., Kong, Y. Y., Liu, M. Z., et al. (2000). “Tai Chi is beneficial to slow down bone loss in postmenopausal women,” in National Symposium on Osteoporosis in the Aged, Vol. 2, Xiamen.
Rücker, G., Cates, C. J., and Schwarzer, G. (2017). Methods for including information from multi-arm trials in pairwise meta-analysis. Res. Synth. Methods 8, 392–403. doi: 10.1002/jrsm.1259
Shen, C. L., Chyu, M. C., Yeh, J. K., Zhang, Y., Pence, B. C., Felton, C. K., et al. (2010). Green tea polyphenols and Tai Chi exercise for postmenopausal osteopenic women: Safety report from a 24-week placebo-controlled randomized trial. FASEB J. 24, lb669-lb669. doi: 10.1096/fasebj.24.1_supplement.946.8
Shen, C. L., Chyu, M. C., Yeh, J. K., Zhang, Y., Pence, B. C., Felton, C. K., et al. (2012). Effect of green tea and Tai Chi on bone health in postmenopausal osteopenic women: a 6-month randomized placebo-controlled trial. Osteoporosis Int. 23, 1541–1552. doi: 10.1007/s00198-011-1731-x
Shieh, A., Ruppert, K. M., Greendale, G. A., Lian, Y., Cauley, J. A., Burnett-Bowie, S. A., et al. (2022). Associations of age at menopause with postmenopausal bone mineral density and fracture risk in women. J. Clin. Endocrinol. Metab. 107, e561–e569. doi: 10.1210/clinem/dgab690
Si, L., Winzenberg, T. M., Chen, M., Jiang, Q., and Palmer, A. J. (2015). Residual lifetime and 10 year absolute risks of osteoporotic fractures in Chinese men and women. Curr. Med. Res. Opin. 31, 1149–1156. doi: 10.1185/03007995.2015.1037729
Society, T. N. A. M. (2021). Management of osteoporosis in postmenopausal women: the 2021 position statement of the North American Menopause Society. Menopause 28, 973–997. doi: 10.1097/GME.0000000000001831
Song, J. L., Cheng, L., and Chang, S. W. (2018). Effects of 48-week Taichi, brisk walking and square dance on bone mineral density in elderly women. Journal of Shandong Sport University 34, 105–108. doi: 10.14104/j.cnki.1006-2076.2018.06.018
Song, R., Roberts, B. L., Lee, E. O., Lam, P., and Bae, S. C. (2010). A randomized study of the effects of t'ai chi on muscle strength, bone mineral density, and fear of falling in women with osteoarthritis. J. Altern. Complement. Med. 16, 227–233. doi: 10.1089/acm.2009.0165
Sun, Z., Chen, H., Berger, M. R., Zhang, L., Guo, H., and Huang, Y. (2016). Effects of tai chi exercise on bone health in perimenopausal and postmenopausal women: a systematic review and meta-analysis. Osteoporos. Int. 27, 2901–2911. doi: 10.1007/s00198-016-3626-3
Thulkar, J., Singh, S., Sharma, S., and Thulkar, T. (2016). Preventable risk factors for osteoporosis in postmenopausal women: Systematic review and meta-analysis. J. Midlife. Health 7, 108–113. doi: 10.4103/0976-7800.191013
Wang, H., Yu, B., Chen, W., Lu, Y., and Yu, D. (2015). Simplified Tai Chi resistance training versus traditional Tai Chi in slowing bone loss in postmenopausal women. Evidence Based Complement. Altern. Med. 2015, 379451. doi: 10.1155/2015/379451
Wang, L., You, X., Lotinun, S., Zhang, L., Wu, N., and Zou, W. (2020). Mechanical sensing protein PIEZO1 regulates bone homeostasis via osteoblast-osteoclast crosstalk. Nat. Commun. 11, 282. doi: 10.1038/s41467-019-14146-6
Wang, M., Kartsonaki, C., Guo, Y., Lv, J., Gan, W., Chen, Z. M., et al. (2021). Factors related to age at natural menopause in China: results from the China Kadoorie Biobank. Menopause 28, 1130–1142. doi: 10.1097/GME.0000000000001829
Wayne, P., Kiel, D., Buring, J., Bonato, P., Yeh, G., Cohen, C., et al. (2012). Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic, randomized trial. BMC Complement. Altern. Med. 12, 7. doi: 10.1186/1472-6882-12-7
Wayne, P. M., Buring, J. E., Davis, R. B., Connors, E. M., Bonato, P., Patritti, B., et al. (2010). Tai Chi for osteopenic women: Design and rationale of a pragmatic randomized controlled trial. BMC Musculoskeletal Disord. 11, 40. doi: 10.1186/1471-2474-11-40
Woo, J., Hong, A., Lau, E., and Lynn, H. (2007). A randomised controlled trial of Tai Chi and resistance exercise on bone health, muscle strength and balance in community-living elderly people. Age Ageing 36, 262–268. doi: 10.1093/ageing/afm005
Wright, N. C., Looker, A. C., Saag, K. G., Curtis, J. R., Delzell, E. S., Randall, S., et al. (2014). The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J. Bone Miner. Res. 29, 2520–2526. doi: 10.1002/jbmr.2269
Wu, G., and Hitt, J. (2005). Ground contact characteristics of Tai Chi gait. Gait Posture 22, 32–39. doi: 10.1016/j.gaitpost.2004.06.005
Wu, G., and Millon, D. (2008). Joint kinetics during Tai Chi gait and normal walking gait in young and elderly Tai Chi Chuan practitioners. Clin. Biomech. 23, 787–795. doi: 10.1016/j.clinbiomech.2008.02.001
Xia, W. B., Zhang, Z. L., Lin, H., Jin, X. L., Yu, W., and Fu, Q. (2019). Guidelines for the diagnosis and management of primary osteoporosis(2017). Chin. J. Osteoporosis 25, 281–309. doi: 10.3969/j.issn.1006-7108.2019.03.001
Xu, F. (2017). Effect of 24-type simplified Taijiquan on bone mineral density in postmenopausal women. J. Pract. Tradit. Chin. Med. 33, 1428–1429. doi: 10.3969/j.issn.1004-2814.2017.12.064
Xue, Y. (2015). The Effects of Enhanced Exercise and Vitamin D Supplement Combined with Calcium on Muscle Strength, Fracture and Life Quality of Postmenopausal Women in Dongcheng District of Beijing (Master Dissertation). Shandong University
Yang, F., and Liu, W. (2020). Biomechanical mechanism of Tai-Chi gait for preventing falls: a pilot study. J. Biomech. 105, 109769. doi: 10.1016/j.jbiomech.2020.109769
Yang, Y., Li, J. H., Xu, N. J., Yang, W. Y., and Liu, J. (2021). Meta-analysis of elderly lower body strength: different effects of Tai Chi exercise on the knee joint-related muscle groups. Evid. Based Complement. Alternat. Med. 2021, 8628182. doi: 10.1155/2021/8628182
Ye, C. Q., Wang, C. W., Wang, G. Y., Wang, C. L., and Ji, B. M. (2016). Effect of Tai Chi quan on health status of middle-aged and elderly women. Chin. J. Health Care Med. 18, 494–495. doi: 10.3969/.issn.1674-3245.2016.06.022
Yen, C. C., Lin, W. C., Wang, T. H., Chen, G. F., Chou, D. Y., Lin, D. M., et al. (2021). Pre-screening for osteoporosis with calcaneus quantitative ultrasound and dual-energy X-ray absorptiometry bone density. Sci. Rep. 11, 15709. doi: 10.1038/s41598-021-95261-7
Yeung, A., Chan, J. S. M., Cheung, J. C., and Zou, L. (2018). Qigong and Tai-Chi for mood regulation. Focus 16, 40–47. doi: 10.1176/appi.focus.20170042
Yu, D. H., Wang, H. R., Xie, Y. L., Chen, W. H., Yu, B., and Lu, Y. Z. (2014). Effect of Tai Chi on bone mineral density of postmenopausal women. J. Shanghai Univer. Sport 38, 100–104. doi: 10.16099/j.cnki.jsus.2014.06.019
Zhang, R. Y. (2020). Research on the influence of 32 style Tai Chi sword on the body balance ability of middle-aged and elderly women (Master Dissertation). Liaoning Normal University.
Zhang, S., Huang, X., Zhao, X., Li, B., Cai, Y., Liang, X., et al. (2021). Effect of exercise on bone mineral density among patients with osteoporosis and osteopenia: a systematic review and network meta-analysis. J. Clin. Nurs. 31, 2100–2111. doi: 10.1111/jocn.16101
Zhao, J. G., Zeng, X. T., Wang, J., and Liu, L. (2017). Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: a systematic review and meta-analysis. JAMA 318, 2466–2482. doi: 10.1001/jama.2017.19344
Zhao, R., Zhao, M., and Xu, Z. (2015). The effects of differing resistance training modes on the preservation of bone mineral density in postmenopausal women: a meta-analysis. Osteoporos. Int. 26, 1605–1618. doi: 10.1007/s00198-015-3034-0
Zhao, R., Zhao, M., and Zhang, L. (2014). Efficiency of jumping exercise in improving bone mineral density among premenopausal women: a meta-analysis. Sports Med. 44, 1393–1402. doi: 10.1007/s40279-014-0220-8
Zhong, D., Xiao, Q., Xiao, X., Li, Y., Ye, J., Xia, L., et al. (2020). Tai Chi for improving balance and reducing falls: an overview of 14 systematic reviews. Ann. Phys. Rehabil. Med. 63, 505–517. doi: 10.1016/j.rehab.2019.12.008
Zhou, Y. (2003). Effect of exercise for prevention and treatment of postmenopausal women with lumbar l2-4 osteoporosis. Chin. J. Sports Med. 72–74.
Zhou, Y. (2004). Effect of Traditional Chinese Exercise on Bone Mineral Density in Postmenopausal Women. Journal of Beijing Sport University. 27, 354–355. doi: 10.3969/j.issn.1007-3612.2004.03.024
Zhou, Y., Li, J., Chen, Y. B., and Jia, J. Y. (2005). Effect of tai Chi pushing hand exercise and calcium supplement on bone mineral density in postmenopausal women. Chin. J. Sports Med. 24, 106–108. doi: 10.3969/j.issn.1000-6710.2005.01.026
Keywords: Tai Chi, post-menopause, BMD, meta-analysis, trial sequential analysis
Citation: Liu X, Jiang C, Fan R, Liu T, Li Y, Zhong D, Zhou L, Liu T, Li J and Jin R (2022) The effect and safety of Tai Chi on bone health in postmenopausal women: A meta-analysis and trial sequential analysis. Front. Aging Neurosci. 14:935326. doi: 10.3389/fnagi.2022.935326
Received: 03 May 2022; Accepted: 01 July 2022;
Published: 13 September 2022.
Edited by:
Xue-Qiang Wang, Shanghai University of Sport, ChinaReviewed by:
Jiao Liu, Fujian University of Traditional Chinese Medicine, ChinaCopyright © 2022 Liu, Jiang, Fan, Liu, Li, Zhong, Zhou, Liu, Li and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juan Li, Nzg1OTM5MDE2QHFxLmNvbQ==; Rongjiang Jin, Y2R6eXlkeGpyakAxMjYuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.