
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Aging Neurosci., 01 June 2022
Sec. Neurocognitive Aging and Behavior
Volume 14 - 2022 | https://doi.org/10.3389/fnagi.2022.868158
This article is part of the Research TopicInnovative Approaches for Assessing and Improving Perioperative Neurocognitive DisordersView all 9 articles
Background: Identifying useful markers is essential for diagnosis and prevention of perioperative neurocognitive disorders (PNDs). Here, we attempt to understand the research basis and status, potential hotspots and trends of predictive markers associated with PNDs after cardiac surgery via bibliometric analysis.
Methods: A total of 4,609 original research articles and reviews that cited 290 articles between 2001 and 2021 were obtained from the Web of Science Core Collection (WoSCC) as the data source. We used the software CiteSpace to generate and analyze visual networks of bibliographic information, including published years and journals, collaborating institutions, co-cited references, and co-occurring keywords.
Results: The number of annual and cumulative publications from 2001 to 2021 has been increasing on the whole. The Harvard Medical School was a very prolific and important institution in this field. The journal of Ann Thorac Surg (IF 4.33) had the most publications, while New Engl J Med was the most cited journal. Neuron-specific enolase (NSE), S100b and kynurenic acid (KYNA) were frequently discussed as possible markers of PNDs in many references. Cardiopulmonary bypass (CPB) was a keyword with high frequency (430) and sigma (6.26), and inflammation was the most recent burst keyword.
Conclusion: Potential markers of PNDs has received growing attention across various disciplines for many years. The research basis mainly focuses on three classic biomarkers of S100b, NSE, and KYNA. The most active frontiers are the inflammation-related biomarkers (e.g., inflammatory cells, cytokines, or mediators) and surgery-related monitoring parameters (e.g., perfusion, oxygen saturation, and the depth of anesthesia).
Neurocognitive disorders (NCDs), one of the most common complications after cardiac surgery, has long been a question of great interest in a wide range of fields (Gao et al., 2005; Lingehall et al., 2017; O'Brien et al., 2017). With the development in surgical procedures and anesthesia techniques, cardiac surgery is becoming much safer than ever before and fewer patients die from normal operation. Unfortunately, despite these improvements, neurocognitive complications such as delirium or cognitive decline still occasionally happen, particularly in the elderly with numerous comorbidities (Jensen et al., 2008; Kotfis et al., 2018). The reported incidences of them vary dramatically depending on different study populations, evaluation time, assessment tools and forth (Selnes et al., 2009; Langer et al., 2019; Subramaniam et al., 2019). Previous researches have shown that these complications tend to be associated with longer hospital stays, higher readmission rates, added economic costs, decreased living quality, increased mortality, and a possible increased risk for developing Alzheimer's disease (AD) (Kirfel et al., 2021; Pereira et al., 2021). Therefore, it should be of paramount importance to explore exact mechanisms and effective therapies of perioperative neurocognitive disorders (PNDs), an overarching term recommended by Evered et al. (2018).
In order to improve identification and prevention of these neurocognitive sequelae, many researchers have been seeking potential markers with high sensitivity and specificity (Alifier et al., 2020; Szwed et al., 2020; Du et al., 2021). As an objective parameter, markers can capture complex pathophysiological changes of bodies, assist in risk stratification and prognosis monitoring, and facilitate diagnosis and assessment of PNDs. To date, extensive studies have investigated related makers of patients who suffered PNDs after cardiac surgery, involving stress, trauma, inflammation, metabolism, endocrine and so on (Luo et al., 2021). However, the results are still controversial, and there is no general agreement about which useful marker should be chosen in clinical practice. To this end, it is necessary to sort out critical research findings on makers of PNDs after cardiac surgery for the purpose of better further studies.
CiteSpace, a web-based Java application for bibliometric analysis and visualization, was developed in 2004 by Professor Chen (2004). It takes a set of bibliographic records as its input and generate a synthesized network based on multiple individual networks derived from each year's literature. CiteSpace allows users to analyze the intellectual structure of different knowledge networks visually, including collaboration network, co-occurrence network, and co-citation networks of cited authors, journals, or references (Chen and Song, 2019). Compared with traditional systematic reviews, this intuitive and flexible approach can provides a valuable overview of how a scientific field has been evolving over time and helps researchers to track the development of some areas they are really interested in Chen (2017).
Here, this review set out to detect the research basis, hotspots and frontiers of potential markers associated with PNDs after cardiac surgery through quantitative analysis of vast academic documents.
Relevant publications between 2001 and 2021 were collected from the Science Citation Index Expanded (SCI-E) of the Web of Science Core Collection (WoSCC). The search strategy was “TS = (heart or cardiac or cardio*) AND TS = (surgery) AND TS = (cognition or *cognitive or delirium) AND TS = (*marker*).” The initial topic search resulted in 290 records. We expanded the dataset by citation indexing and found 5,109 citing original research articles and review articles in English between 2001 and 2021. After preprocessing by CiteSpace to remove duplicates and rejects, 4,609 records were identified and used in the subsequent analysis. The detailed search strategy is presented in Supplementary Figure 1. All data were retrieved and downloaded in August 21, 2021.
A new version of CiteSpace (v5.8.R3) and Excel (2019) was used to visualize and analyze the dataset. The knowledge maps formed by CiteSpace consist of nodes and links. The size of nodes in a map represents frequency of different items such as author, institution, and country, and links between nodes represent the strength of the cooperation, co-occurrence, and co-citation relationships. Several commonly used structural metrics of CiteSpace are betweenness centrality, burstness and sigma score. Nodes with high betweenness centrality are likely to sit in the middle of two large groups of nodes which are usually regarded as turn points in a field. The intensity and duration of a citation burst indicate the degree of abrupt changes in the scientific community caused by a specific publication or keyword. If a node is strong in both centrality and burstness, it will have a high sigma score. In a map, a purple ring and red ring of a node mean that it has high betweenness centrality and strong citation burst (Chen et al., 2012).
In Figure 1, there was a clearly upward trend of the cumulative publications between 2001 and 2021, which increased from 50 to 4,609. The polynomial trendlines fitted the annual and cumulative number of them well (R2 = 0.9483, 0.9943). Although the annual number in 2019 and 2020 were slightly less than previous 2 years, the number of publications in 2021 was 547 up to now, which was the most productive year over the past two decades. These results indicate that the issue of markers associated with PNDs after cardiac surgery has received continuous attention and extensive research is being conducted recently.
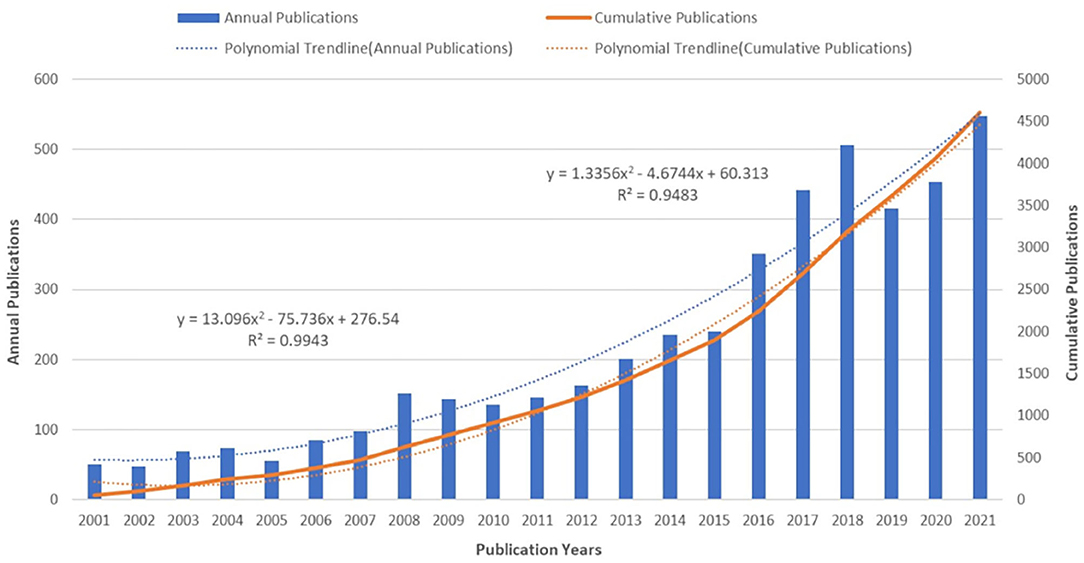
Figure 1. The number of annual publications and growth trends on makers of PNDs after cardiac surgery from 2001 to 2021.
As shown in Table 1, the top five prolific institutions were Duke University (102), Harvard Medical School (101), University of Pennsylvania (100), University of Toronto (94), Johns Hopkins University (89). As regards sigma score, the lead institution was Harvard University (3.09), followed by the Harvard Medical School (1.56), King's College London (1.37), University College London (1.31), and Yale University (1.28). Most of them are American institutions, suggesting that the United States is staying ahead in this research field, and is playing a vital role in the world. Though the number of articles published by many academic institutions from England or other countries was fewer than those in US, these institutions are active in multi-institutional cooperation and have still produced many groundbreaking research outcomes.
Journals are the main carrier of scientific research results, through which we can know the widespread distribution and dissemination of the relevant literature in a given field. Looking at Table 2, the Ann Thorac Surg (IF 4.33) had the most publications, followed by J Cardiothor Vasc An (IF 2.628), Anesth Analg (IF 5.178), J Thorac Cardiov Sur (IF 5.209), and Brit J Anaesth (IF 9.166). The Ann Thorac Surg is a professional peer-reviewed medical journal intended for promoting scholarship in cardiothoracic surgery patient care, clinical practice, research, education, and policy. According to the Journal Citation Report (JCR) on the Web of Science (WOS), the journal has 509 publications, with 41,620 citations in 2020. It ranked 36 out of 211 in surgery and 51 out of 142 in cardiovascular system.
As can be seen from the Table 3, the top five co-cited journals were New Engl J Med, Lancet, Circulation, Ann Thorac Surg, Anesthesiology and the top five in terms of sigma were Am J Clin Nutr, J Thorac Cardiov Sur, J Trace Elem Med Bio, Brain Res Bull, Obesity Facts. The fundamentals of the research field mostly came from above journals. Among the top 15 co-cited journals, New Engl J Med, Lancet, JAMA-J Am Med Assoc are top journals in medical area, and the rest are the most important journals in the fields of anesthesiology and cardiothoracic surgery. In addition, from the top journals ranked by sigma score we can know that part of articles also involved the nutrition, endocrinology, molecular and cellular mechanisms associated with cognition and other brain functions.
Co-cited references are the theoretical basis of a research field, the most cited of which can be seen as hotspots and landmarks because they have attracted much attention and made great contributions to the field. The most cited articles in each year between 2001 and 2021 were chosen in accordance with g-index (Egghe, 2006) to construct a year's individual network.
The integrated reference co-citation network was shown in Figure 2. It contained 1,558 nodes, 7,598 linkes, and 150 clusters. The modularity was 0.8531, which means that the structure of the network is clear and well-organized. The silhouette score of 0.9629 was very high, suggesting the clustering result was highly reliable. Each tree ring of a node represents the citation history of an article. Its size, color and thickness imply the cited times, year of publication and citations in a single time slice, respectively. What stand out in this figure were the references with high centrality, such as “van Dijk et al. (2007),” “Uhlig et al. (2016),” “Zheng et al. (2013),” “Liu et al. (2009),” and “Abildstrom et al. (2004)”. They were key hubs connecting different groups of nodes, which can be regarded as structurally essential references in this network. The color bar, ranging from cold colors to warm colors, indicated a specified period starting from 2001 to 2021. For example, lines or areas in purple generated in 2012, were earlier than those in red or orange.
The top 30 references with strong citation bursts can be grouped by the beginning time of burst (Figure 3). Instead of introduced all the 30 references, the reference with the strongest citation burst of PNDs in each group will be discussed as the most representative article. Among citation bursts starting in 2001 and 2002, the strongest bursts are associated with a 2000 paper by Diegeler et al. and a 2001 paper by Newman et al. Coronary artery bypass grafting (CABG) is a well-established surgical procedure for heart disease and can be performed with or without cardiopulmonary bypass (CPB), namely on- or off-pump CABG. Diegeler et al. (2000) investigated the impact of CPB on neuropsychological function of patients who underwent on-pump and off-pump CABG using transcranial Doppler ultrasound (TCD) and S-100 analytical method. Around the same year, some researchers focused on the role of neurobiochemical markers of brain damage and the change of inflammatory response during cardiac surgery. In 2001, Newman et al. (2001) undertook a prospective study to confirm the significant effect of perioperative cognitive decline after CABG on long-term cognitive function 5 years later. Since then, many randomized controlled trials (RCTs) have compared cognitive outcomes in different postoperative stages after on- vs. off-pump CABG.
In order to avoid possible confounding of those adverse events in surgeries caused by failed non-technical operations, the article published by Yule et al. (2006) developed a behavior rating system specifically for surgeons' non-technical skills (e.g., awareness, communication, and teamwork), aiming to allow surgeons to structure observations and improve safety and efficiency of surgical performances further.
Cibelli, Fidalgo, Terrando, Ma, Monaco and Feldmann (2010) published in 2010 suggested that inflammation plays a prominent role in the pathogenesis of postoperative cognitive dysfunction (POCD) using a mouse model of orthopedic surgery. Citation bursts starting in 2016 and 2018 are, respectively, led by Meybohm et al. (2015) and Yumuk et al. (2015) article published in 2015. The former was a prospective, double-blind, multicenter, randomized, controlled trial aiming to prove whether remote ischemic preconditioning (RIPC) can improve clinical outcomes in patients undergoing elective cardiac surgery, while the latter provided many explicit guidelines for obesity management in adults. In 2018, Evered et al. (2018) revised the nomenclature for PNDs to enhance consistency of communication and reporting in this field. It has the strongest citation burst starting in 2019, and it is still going strong.
These articles, identified based on citation bursts, indicated that researchers primarily focused on the following issues in past 20 years: the assessment, comparison and definition of neurocognitive outcomes in all stages during cardiac surgery, the predictive value of markers and tools in PNDs such as trauma-related or inflammation-related substances, the prevention and treatment of PNDs such as performing RIPC or managing high-risk population groups. In the different period, there are different focuses on this topic.
Each cluster is displayed as a horizontal timeline from left to right. The three most cited references in every year are listed below each timeline. Figure 4 lists the first 18 large clusters and demonstrates that Cluster #0 is the largest cluster and it is active in recent years. The field's focus has been gradually expanded from Cluster #5 postoperative delirium (POD) and Cluster #4 POCD to the Cluster #0 PNDs. Interestingly, remote ischemic preconditioning and obese individual are another two active clusters now. This is probably a hint that we can try to investigate the level of specific markers in different conditions or population.
In these timelines, there were three clusters labeled with specific markers, which is Cluster #7, #8, and #20. Although they were neither the largest clusters nor the most active fields, they were closely associated with our purpose to explore the potential markers of PNDs. It was much important for us to understand how these markers work and why they were studied in this field.
S100b and Neuron-specific enolase (NSE) were both first described in 1965 (Moore and McGregor, 1965), while kynurenic acid was initially found as a constituent of canine urine in 1853 (Liebig, 1853). In 2001, Donato (2001) published a paper in which he demonstrated that S100b is a member of a multigenic family of Ca2+-modulated proteins of the EF-hand type. It not only acts as an intracellular regulator to modulate cell proliferation, migration and differentiation, but can be seen as an extracellular signal playing a neurotrophic or neurotoxic role under different conditions (Donato et al., 2009). Additionally, Kleindienst et al. (2007) analyzed the value of S100b as a marker of brain damage and possible treatment option, and they concluded that the positive effect of S100b on cognition and neurogenesis can improved the functional prognosis of patients with brain injury, which probably had a therapeutic potential. But it should be noted that serum S100b levels can't reflect the corresponding cerebral S100b release.
NSE, a glycolytic enzyme found in the neuronal cytoplasm and involved in the energy metabolic process, has been widely studied in many nervous system diseases. Neuronal damage or death can increases its levels in cerebrospinal fluid (CSF) or serum (Marangos and Schmechel, 1987; Rasmussen et al., 1999). Herrmann et al. (2000) reported that postoperative serum concentrations and kinetics of S100b and NSE after cardiac surgery not only reflected early different neuropsychological outcomes but also might mirror underlying damage to neuronal and glial brain tissue. As a metabolite of tryptophan produced in the kynurenine pathway, kynurenic acid (KYNA) possesses neuroactive function, which may influence important neurophysiological and neuropathological processes. Forrest et al. (2011) reported that KYNA was a significant correlate of performance in the Stroop C and Trail A and B tests, and predicted cognitive function in patients following cardiac surgery. However, due to their poor specificity, inadequate sensitivity and inaccurate assay methods (Smith et al., 2019), the correlations between these biomarkers and postoperative cognitive function have been controversial.
Nine major clusters were listed in the Table 4. The titles of citing articles were extracted to label the corresponding clusters, which are generally considered as the research fronts of these clusters. All labels chosen by the log-likelihood ratio test method (LLR) were used for analysis. Of those nine clusters, Cluster #7 and #8 have been mentioned in Section Timeline View, while other clusters such as Cluster #1, #2, #3, and #6 were related to operation ways and neurodevelopmental problems. Hence, We selectively interpreted the Cluster #0 PNDs, #4 POCD, #5 POD in detail since they were directly related to neurocognitive disorders after cardiac surgery, the topic we're interested in. Besides, in each cluster, we emphatically discussed those references with high citations and high topic relevance.
As Table 5 shows, the top 10 cited references in Cluster #0 were mostly published in the past 5 years. Inouye et al. (2014), the most cited reference in this cluster, summarized the epidemiology, etiology, diagnosis, evaluation and management of delirium in elderly people. It offered many potential pathophysiologic contributors to delirium, including neurotransmitters (e.g., acetylcholine, melatonin, and serotonin), inflammation (e.g., IFN α/β, IL-6/8/10, and TNF-α), physiological stressors (e.g., cortisol and neopterin), electrolyte disorders (e.g., sodium, calcium, and magnesium), metabolic derangements (e.g., lactate, glucose, and IGF-1) and so on. More specifically, Hughes et al. (2020), the citing article with coverage of 34%, provided evidence-based consensus statements and practice recommendations regarding POD identification and prevention, based on an established iterative Delphi process and Grading of Recommendations Assessment, Development and Evaluation (GRADE) Criteria in the Sixth Perioperative Quality Initiative (POQI-6) consensus conference.
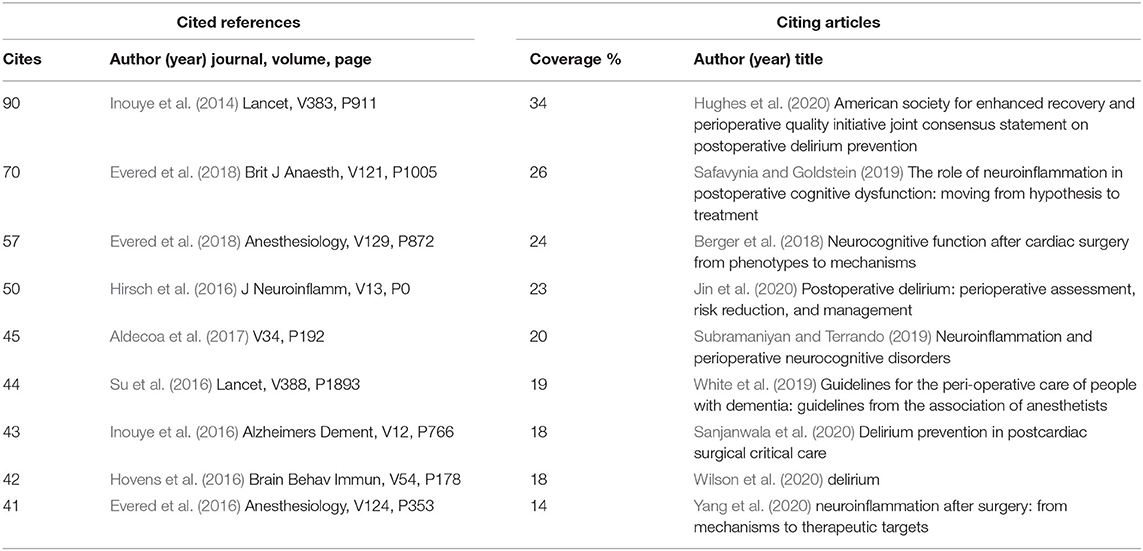
Table 5. Top 10 cited references and citing articles of Cluster #0 perioperative neurocognitive disorder.
Evered et al. (2018), the second most cited reference, recommended using PNDs to describe cognitive impairment identified in the perioperative period, which includes pre-existing mild or major neurocognitive disorders (NCD) before operation, POD after surgery, delayed neurocognitive recovery within postoperative 30 days, and mild or major POCD from postoperative 30 days to 12 months. Both of cited references are major milestones in Cluster #0. Other citing articles mainly focused on the assessment, prevention and comprehensive management of PNDs, especially the part of neuroinflammation-related medicators and pathways.
In CiteSpace, key concepts can be algorithmically extracted from the titles of citing articles in Cluster #0 (Supplementary Figure 2). When it comes to potential diagnostic or prognostic indicators, some of them referred to certain soluble molecular substances in biological fluids such as serum, plasma or CSF, mostly associated with inflammation, brain injury, stress response, metabolism, neurotransmitter or key regulators in these processes, such as C-reactive protein (CRP), glial fibrillary acidic protein (GFAP), visinin-like/galectin-3 protein.
In Figure 4, some of more recent and highly cited members in Cluster #0 include a review of different experimental approaches and models that have been used in preclinical postoperative cognitive dysfunction research (Eckenhoff et al., 2020), a prospective biomarker cohort study of POD is associated with increased plasma neurofilament light (NfL) (Casey et al., 2020), and a mechanism research of BDNF/TrkB signaling disruption mediated by NMDAR/Ca2+/calpain might contribute to POCD in aging mice (Qiu et al., 2020).
Cited references and citing articles of Cluster #4 POCD were listed in Table 6. van Harten et al. (2012) suggested that more biochemical markers specific to neuronal damage should be identified, such as glial fibrillary-associated protein and brain- and heart-type fatty acid binding protein. The five citing articles are all reviews, which largely summarized many common studied markers associated with Alzheimer's disease pathophysiology (e.g., ApoE, Aβ1-42, and p-tau), inflammatory process (e.g., NF-kappaB, MMP9, and MCP-1), neuronal injury. Androsova et al. (2015) emphasized the importance of systems biology methods encompassing experimental measurements, imaging techniques and mathematical/computational modeling, so that we can not only understand the pathomechanisms of PNDs at different levels, but also integrate sparse markers into a complete knowledge network through some known molecular interactions and pathways. In this way, more potential markers and underlying pathways can be found easier than ever before with purposeful design.
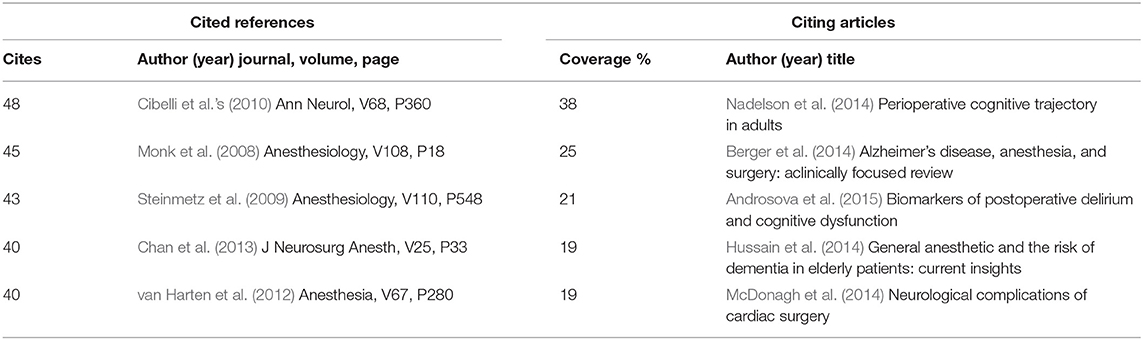
Table 6. Top 5 cited references and citing articles of Cluster #4 postoperative cognitive dysfunction.
The most cited members of Cluster #5 represent important mileposts in relation to POD (Table 7), such as Saczynski et al. (2012) article on the cognitive trajectory after POD during the first year, and Lin, Chen and Wang (2012) article on the risk factors of delirium after cardiac surgery. The citing article with the highest citation coverage of 21% in this cluster, Maldonado (2013), summarized seven complementary theories and their interrelation: the hypotheses of “neuroinflammatory,” “neuronal aging,” “oxidative stress,” “neuroendocrine,” “diurnal dysregulation,” and “network disconnectivity” can acted together to lead to a final pathway associated with neurotransmitter alterations, which generally were deficiencies in acetylcholine (Ach) and melatonin; excess of dopamine (DA), norepinephrine (NE), and/or glutamate (GLU); and decrease or increase in serotonin (5HT), histamine, and/or γ-aminobutyric acid (GABA).
The structural variation analysis can identify the potentially transformative articles published in recent years according to their contributions to the global or local structure of the knowledge domain of interest. To great extent, the method compensates for the limitation of citation-based analysis relies on citations that are greatly influenced by the publication time of articles.
Table 8 lists the first five articles in each of the last 3 years, which were ranked by the harmonic mean (H) of three different structural variation variables, namely ΔM, ΔCLw, and CKL (Chen, 2012). The five highly ranked articles in 2021 focused on the pathophysiologic mechanisms of PNDs, such as anesthetic regimen, cerebral perfusion pressure management, cerebral oximetry monitoring and so on (Akhtar et al., 2021; Evered and Goldstein, 2021; Pisano et al., 2021; Snyder et al., 2021; Zugni et al., 2021). In 2019 and 2020, there were two valuable articles providing evidence-based recommendations on perioperative delirium care and prevention (White et al., 2019; Hughes et al., 2020). Also, several articles studied related neurovascular and immune mechanisms of PNDs and their possible markers (Luo et al., 2019; Yang and Terrando, 2019; Fong et al., 2020; Majewski et al., 2020; Wang et al., 2020).
Keywords, usually concise and refined concepts, are the core topics of academic articles. In CiteSpace, co-occurring keywords reflect research hotspots and focus points in a field. The top 15 keywords were ranked by frequency and sigma in Table 9. In addition to search terms of “cardiac” and “surgery”, CPB was the keyword with highest frequency (430) and sigma (6.26). It is a technique commonly utilized in cardiac surgery to temporarily maintain the function of the heart and lungs, which was first performed by Dr. John H. Gibbon, Jr in May 1953 (Bauer and Tchantchaleishvili, 2018).
Seeing from the Table 9, several major issues during cardiac surgery can be identified:
(1) Operation and Prognosis: According to a systematic review on clinical outcomes of CABG by Møller et al. (2008), opinions differed as to whether on-pump or off-pump surgery can offer patients better outcomes. They included 66 randomized trials and found no convincing evidence that off-pump surgery reduces any of the major clinical outcomes such as death, myocardial infarction, stroke, coronary reintervention except for atrial fibrillation. In 2017, Filardo et al. (2018) published a meta-analysis assessing efficacy [randomized controlled trials (RCTs)] and effectiveness (observational studies) of on- vs. off-pump CABG, and concluded that off-pump CABG has greater operative safety than the former but may harm lasting survival gains of patients.
(2) Neurologic Complications and Risk factors: Throughout the history of cardiac surgery and anesthesia, neurologic complications have been a primary concern, for instance, early or late stoke, delirium, cognitive decline and even dementia (Bedford, 1955; Gilman, 1965; Eagle et al., 1999; McDonagh et al., 2014). Thus, a bulk of literature have explored risk factors associated with these adverse events (Hedberg et al., 2011; Hood et al., 2018; Gaudino et al., 2019; Greaves et al., 2020), mainly divided into several categories: baseline patient characteristics (e.g., age, sex, genetics, physical fitness, multiple comorbidities, mental attitude, premorbid intelligence or cognitive function, alcohol, or drug abuse), surgery-related procedural variables (e.g., surgical approaches and duration, intraoperative monitoring and management of temperature, perfusion pressure, oxygen saturation, blood glucose and embolic load, anesthetic protocols, drugs, and dosage), and perioperative care (e.g., sedation, analgesia, mobilization, nutrition, and sleep enhancement). Also, it is of great significance for proposing effective prophylaxis to divide them into modifiable, partly modifiable and non-modifiable or pre, mid, and postoperative factors.
(3) Mechanisms and potential markers: The researches on these two aspects are essential and paramount for earlier diagnosis, prevention and treatment of PNDs. They can complement and reinforce each other, that is, the change of certain thing or index in an established mechanism may indicates its clinical application value as a predictive marker and vice versa. In a review, Berger et al. (2018) discussed six partly overlapped pathophysiologic mechanisms that may underlie PNDs: neuronal damage/aging, inflammation, embolism, cerebral autoregulation/oxygen delivery/temperature management, neurodegenerative disease pathology, and brain network dysfunction. Additionally, a growing body of literature has reported that gut microbiota might also play a critical role in PNDs (Xu et al., 2020). Therefore, a variety of markers can be found during these processes, which mainly consist of two types: biochemical markers and monitoring parameters, and two sources: biological fluids (CSF, blood, saliva, urine, sweat, and tears) and monitoring devices [magnetic resonance imaging (MRI), electroencephalographic (EEG), Near-infrared spectroscopy (NIRS), TCD, BIS monitor, Transesophageal echocardiography (TEE)].
Figure 5 shows the top 30 keywords with the strongest bursts. The strongest ones include “cardiopulmonary bypass,” “release,” and “revascularization”. The most recent burst of keywords is “inflammation”, which is regarded as a research frontier in this field, and may well be studied intensively and deeply in the future. Briefly speaking, there are probably a couple of reasons for studying inflammation: on the one hand, inflammation can be regarded as a bridge connecting the cardiac surgery and neurocognitive disorders. Through upregulating cyclooxygenase 2 isozyme (COX-2) and matrix metalloproteinases (MMPs), peripheral pro-inflammatory cytokines can disrupt the integrity of the blood-brain barrier (BBB), allowing bone-marrow-derived monocytes (BMDM) to activate microglia cells and trigger neuroinflammation (Tan et al., 2021). Besides, Thackeray et al. (2018) reported that biphasic peaks of neuroinflammation in early acute and late chronic stages of cardiac injury were similar to a biphasic microglial activation pattern with peaks at initial onset of mild cognitive impairment and late advanced Alzheimer's disease. In addition, many animal studies have provided evidence that the anti-neuroinflammatory therapy after cardiac surgery can diminish microglial activation, attenuates neurogenesis suppression, and improve functional outcomes (Wang et al., 2022). And further research on clinical trials is still ongoing. On the other hand, with the advance of immunology, molecular biology, and examining techniques, researchers can consider questions from totally novel angles and merge a variety of accurate ways to explore potential inflammatory pathways and mechanisms in great depth.
Inevitably, there are several limitations in the study. Firstly, we subjectively chose specific search strategy and only analyzed the characteristics of those English publications retrieved from single database WOSCC. This probably let us ignore some valuable articles in other languages or data archives such as PubMed, Embase or MEDLINE. Secondly, we collected our data using general terms associated with this topic rather than POD or POCD and expanded the dataset through including lots of citing articles, which introduced many less relevant publications. Therefore, we selectively discussed significant articles and closely related clusters to make the interest points more prominent. Furthermore, CiteSpace may be a controversial tool and it is constantly being improved. We just directly described the top subjects, sketched the broad outline of this field as intuitively as possible and obtained an overview of potential markers on PNDs, rather than a list for certain specific markers. Thus, the depth was possibly insufficient and many details of articles were not summarized adequately.
In general, the issue of neurocognitive disorders after cardiac surgery has received significant attention in past 20 years. Many outstanding institutions in United States such as Duke University, Harvard Medical School and University of Pennsylvania have made great amount of excellent academic achievements in this field. Most of these publications are associated with cardiothoracic surgery and anesthesiology, but they also involve nutrition, endocrinology, molecular and cellular biology and neuroscience. From this perspective, multi-institutional cooperation and interdisciplinary collaboration are crucial to the progress and development of this scientific area.
Taken together, the most frequently cited literature comprise the basis of this field. According to the cluster analysis and timeline view, the knowledge base can be divided into four thematic domains: (1) the classification, definition and assessment of every neurocognitive disorder during cardiac surgery (e.g., PNDs, POD, and POCD), (2) the types of cardiac diseases and corresponding operation or anesthesia (e.g., congenital heart disease, CABG, and fentanyl-induced), (3) the risk factors and possible prophylactic measures (e.g., obese individual and RIPC), (4) the predictive markers and potential pathophysiology (e.g., S100b, NSE, and KYNA). Obviously, three classic biomarkers of S100b, NSE, and KYNA were frequently studied by researchers in past 20 years.
As far as the research focuses are concerned, the co-occurring keywords with high frequency can represent various scientific hotspots in the field. They include several pivotal topics: cardiac disease and surgery, short- or long-term postoperative outcomes, brain injury and cognitive dysfunction, risk factors and complex relationship among possible events. From the burst analysis of co-occurring keywords and co-cited references, we get to know that the main research hotspots of this field have transferred from hemodynamic changes and mechanisms during kinds of cardiac surgery, release of markers associated with tissue damage (2001–2010), promotion of non-technical operation skills and teamwork, improvement of operation patterns and protection of multiple organs (2008–2018) to standardized management and individualized treatment, inflammation-related mechanisms and pathways (2018–2021).
The citations of articles published in recent year are usually not very high due to their short time. Therefore, we performed the structural variation analysis. From the results of it, 15 potentially transformative articles published in 2019–2021 have three main themes: neuromonitoring such as cerebral oxygen saturation, perfusion and the depth of anesthesia in the operation, comprehensive management and prevention of delirium, and diagnosis with biomarkers of PNDs involving neurovascular or immune mechanisms. To some extent, these topics are likely to be the research frontiers. In addition, combined with the results of the burst keywords and the burst references in recent years, the research of inflammation between cardiac diseases or surgery and the research applying the nomenclature of PNDs are the currently main research directions.
The current review examined valuable diagnostic and prognostic markers for treating neurocognitive disorders after cardiac surgery via CiteSpace, which is a convenient citation visual analysis tool for researchers to quickly and objectively understand the foundation, status, hotspots and frontiers of a scientific field. In this context, we can attempt to impersonally describe what we saw and what we knew according to the results. Rather, with the purpose of answering a defined question or proving a certain assumption, some traditional systematic reviews and meta-analysis tend to subjectively filter the articles, explain the results from their own points of view, and then unavoidably introduced more potential bias. Compared with those approaches, CiteSpace, a more efficient way, can provide multi-faceted and multi-dimensional information of a research field based on massive publications, for example, the distribution of institutions/countries or journals, the valuable references and hot keywords, the evolution of main focuses and so on. We can grasp the whole developing tendency of a field on a macro level and understand the temporal and spatial characteristics of this area. However, being limited to the specific search strategy, different database and diverse parameter settings, the results may vary in some details, so the interpretation should be cautious.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
LJ: design of the study, analysis, writing, and revision of the article. FL: design of the study and revision of the article. Both authors contributed to the article and approved the submitted version.
The research has received funding from Excellent Talents Training Grant Program of Xicheng District, Beijing, China (202153).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2022.868158/full#supplementary-material
Abildstrom, H., Christiansen, M., Siersma, V. D., and Rasmussen, L. S. (2004). Apolipoprotein E genotype and cognitive dysfunction after noncardiac surgery. Anesthesiology. 101, 855–861. doi: 10.1097/00000542-200410000-00009
Akhtar, M. I., Gautel, L., Lomivorotov, V., Neto, C. N., Vives, M., El Tahan, M. R., et al. (2021). Multicenter international survey on cardiopulmonary bypass perfusion practices in adult cardiac surgery. J. Cardiothorac. Vasc. Anesth. 35, 1115–1124. doi: 10.1053/j.jvca.2020.08.043
Aldecoa, C., Bettelli, G., Bilotta, F., Sanders, R. D., Audisio, R., Borozdina, A., et al. (2017). European society of anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur. J. Anaesthesiol. 34, 192–214. doi: 10.1097/EJA.0000000000000594
Alifier, M., Olsson, B., Andreasson, U., Cullen, N. C., Czyzewska, J., Jakubów, P., et al. (2020). Cardiac surgery is associated with biomarker evidence of neuronal damage. J. Alzheimers Dis. 74, 1211–1220. doi: 10.3233/JAD-191165
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association. doi: 10.1176/APPI.BOOKS.9780890425596
Androsova, G., Krause, R., Winterer, G., and Schneider, R. (2015). Biomarkers of postoperative delirium and cognitive dysfunction. Front. Aging Neurosci. 7, 112. doi: 10.3389/fnagi.2015.00112
Bauer, T. M., and Tchantchaleishvili, V. (2018). The person behind the inventor of the heart-lung machine: John H. Gibbon Jr, MD (1903-1973). Artif. Organs. 42, 765–775. doi: 10.1111/aor.13280
Bedford, P. D. (1955). Adverse cerebral effects of anaesthesia on old people. Lancet. 269, 259–263. doi: 10.1016/S0140-6736(55)92689-1
Berger, M., Burke, J., Eckenhoff, R., and Mathew, J. (2014). Alzheimer's disease, anesthesia, and surgery: A clinically focused review. J. Cardiothorac. Vasc. Anesth. 28, 1609–1623. doi: 10.1053/j.jvca.2014.04.014
Berger, M., Terrando, N., Smith, S. K., Browndyke, J. N., Newman, M. F., and Mathew, J. P. (2018). Neurocognitive function after cardiac surgery: from phenotypes to mechanisms. Anesthesiology. 129, 829–851. doi: 10.1097/ALN.0000000000002194
Casey, C. P., Lindroth, H., Mohanty, R., Farahbakhsh, Z., Ballweg, T., Twadell, S., et al. (2020). Postoperative delirium is associated with increased plasma neurofilament light. Brain. 143, 47–54. doi: 10.1093/brain/awz354
Chan, M. T., Cheng, B. C., Lee, T. M., and Gin, T. (2013). BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J. Neurosurg. Anesthesiol. 25, 33–42. doi: 10.1097/ANA.0b013e3182712fba
Chen, C. (2004). Searching for intellectual turning points: progressive knowledge domain visualization. Proc. Natl. Acad. Sci. U. S. A. 101, 5303–5310. doi: 10.1073/pnas.0307513100
Chen, C. (2012). Predictive effects of structural variation on citation counts. J. Am. Soc. Inform. Sci. Technol. 63, 431–449. doi: 10.1002/asi.21694
Chen, C. (2017). Science mapping: a systematic review of the literature. J. Data Inform. Sci. 2, 1–40. doi: 10.1515/jdis-2017-0006
Chen, C., Hu, Z., Liu, S., and Tseng, H. (2012). Emerging trends in regenerative medicine: a scientometric analysis in CiteSpace. Expert Opin. Biol. Ther. 12, 593–608. doi: 10.1517/14712598.2012.674507
Chen, C., and Song, M. (2019). Visualizing a field of research: a methodology of systematic scientometric reviews. PLoS ONE. 14, e0223994. doi: 10.1371/journal.pone.0223994
Cibelli, M., Fidalgo, A. R., Terrando, N., Ma, D., Monaco, C., Feldmann, M., et al. (2010). Role of interleukin-1beta in postoperative cognitive dysfunction. Ann. Neurol. 68, 360–368. doi: 10.1002/ana.22082
Cunningham, C., and Maclullich, A. M. (2013). At the extreme end of the psychoneuroimmunological spectrum: delirium as a maladaptive sickness behaviour response. Brain Behav. Immun. 28, 1–13. doi: 10.1016/j.bbi.2012.07.012
de Rooij, S. E., and van Munster, B. C. (2013). Melatonin deficiency hypothesis in delirium: a synthesis of current evidence. Rejuvenation Res. 16, 273–278. doi: 10.1089/rej.2012.1405
Diegeler, A., Hirsch, R., Schneider, F., Schilling, L. O., Falk, V., Rauch, T., et al. (2000). Neuromonitoring and neurocognitive outcome in off-pump versus conventional coronary bypass operation. Ann. Thorac. Surg. 69, 1162–1166. doi: 10.1016/S0003-4975(99)01574-X
Donato, R. (2001). S100: a multigenic family of calcium-modulated proteins of the EF-hand type with intracellular and extracellular functional roles. Int. J. Biochem. Cell Biol. 33, 637–668. doi: 10.1016/S1357-2725(01)00046-2
Donato, R., Sorci, G., Riuzzi, F., Arcuri, C., Bianchi, R., Brozzi, F., et al. (2009). S100B's double life: intracellular regulator and extracellular signal. Biochim. Biophys. Acta. 1793, 1008–1022. doi: 10.1016/j.bbamcr.2008.11.009
Du, X., Gao, Y., Liu, S., Zhang, J., Basnet, D., Yang, J., et al. (2021). Early warning value of ASL-MRI to estimate premorbid variations in patients with early postoperative cognitive dysfunctions. Front. Aging Neurosci. 13, 670332. doi: 10.3389/fnagi.2021.670332
Eagle, K. A., Guyton, R. A., Davidoff, R., Ewy, G. A., Fonger, J., Gardner, T. J., et al. (1999). ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation. 100, 1464–1480. doi: 10.1161/01.CIR.100.13.1464
Eckenhoff, R. G., Maze, M., Xie, Z., Culley, D. J., Goodlin, S. J., Zuo, Z., et al. (2020). Perioperative neurocognitive disorder: state of the preclinical science. Anesthesiology. 132, 55–68. doi: 10.1097/ALN.0000000000002956
Egghe, L. (2006). Theory and practise of the g-index. Scientometrics. 69, 131–152. doi: 10.1007/s11192-006-0144-7
Evered, L., Silbert, B., Knopman, D. S., Scott, D. A., DeKosky, S. T., Rasmussen, L. S., et al. (2018). Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br. J. Anaesth. 121, 1005–1012. doi: 10.1016/j.bja.2017.11.087
Evered, L., Silbert, B., Scott, D. A., Ames, D., Maruff, P., and Blennow, K. (2016). Cerebrospinal fluid biomarker for alzheimer disease predicts postoperative cognitive dysfunction. Anesthesiology 124, 353–361. doi: 10.1097/ALN.0000000000000953
Evered, L. A., and Goldstein, P. A. (2021). Reducing perioperative neurocognitive disorders (PND) through depth of anesthesia monitoring: a critical review. Int. J. Gen. Med. 14, 153–162. doi: 10.2147/IJGM.S242230
Filardo, G., Hamman, B. L., da Graca, B., Sass, D. M., Machala, N. J., Ismail, S., et al. (2018). Efficacy and effectiveness of on- versus off-pump coronary artery bypass grafting: a meta-analysis of mortality and survival. J. Thorac. Cardiovasc. Surg. 155, 172–179.e5. doi: 10.1016/j.jtcvs.2017.08.026
Fong, T. G., Vasunilashorn, S. M., Ngo, L., Libermann, T. A., Dillon, S. T., Schmitt, E. M., et al. (2020). Association of plasma neurofilament light with postoperative delirium. Ann. Neurol. 88, 984–994. doi: 10.1002/ana.25889
Forrest, C. M., Mackay, G. M., Oxford, L., Millar, K., Darlington, L. G., Higgins, M. J., et al. (2011). Kynurenine metabolism predicts cognitive function in patients following cardiac bypass and thoracic surgery. J. Neurochem. 119, 136–152. doi: 10.1111/j.1471-4159.2011.07414.x
Gao, L., Taha, R., Gauvin, D., Othmen, L. B., Wang, Y., and Blaise, G. (2005). Postoperative cognitive dysfunction after cardiac surgery. Chest. 128, 3664–3670. doi: 10.1378/chest.128.5.3664
Gaudino, M., Rahouma, M., Di Mauro, M., Yanagawa, B., Abouarab, A., Demetres, M., et al. (2019). Early versus delayed stroke after cardiac surgery: a systematic review and meta-analysis. J. Am. Heart Assoc. 8, e012447. doi: 10.1161/JAHA.119.012447
Gilman, S. (1965). Cerebral disorders after open-heart operations. N. Engl. J. Med. 272, 489–498. doi: 10.1056/NEJM196503112721001
Girard, T. D., Ware, L. B., Bernard, G. R., Pandharipande, P. P., Thompson, J. L., Shintani, A. K., et al. (2012). Associations of markers of inflammation and coagulation with delirium during critical illness. Intens. Care Med. 38, 1965–1973. doi: 10.1007/s00134-012-2678-x
Greaves, D., Psaltis, P. J., Davis, D., Ross, T. J., Ghezzi, E. S., Lampit, A., et al. (2020). Risk factors for delirium and cognitive decline following coronary artery bypass grafting surgery: a systematic review and meta-analysis. J. Am. Heart Assoc. 9, e017275. doi: 10.1161/JAHA.120.017275
Guenther, U., Theuerkauf, N., Frommann, I., Brimmers, K., Malik, R., Stori, S., et al. (2013). Predisposing and precipitating factors of delirium after cardiac surgery: a prospective observational cohort study. Ann. Surg. 257, 1160–1167. doi: 10.1097/SLA.0b013e318281b01c
Hedberg, M., Boivie, P., and Engström, K. G. (2011). Early and delayed stroke after coronary surgery - an analysis of risk factors and the impact on short- and long-term survival. Eur. J. Cardiothorac. Surg. 40, 379–387. doi: 10.1016/j.ejcts.2010.11.060
Herrmann, M., Ebert, A. D., Galazky, I., Wunderlich, M. T., Kunz, W. S., and Huth, C. (2000). Neurobehavioral outcome prediction after cardiac surgery: role of neurobiochemical markers of damage to neuronal and glial brain tissue. Stroke. 31, 645–650. doi: 10.1161/01.STR.31.3.645
Hirsch, J., Vacas, S., Terrando, N., Yuan, M., Sands, L. P., Kramer, J., et al. (2016). Perioperative cerebrospinal fluid and plasma inflammatory markers after orthopedic surgery. J. Neuroinflammation 113:211 doi: 10.1186/s12974-016-0681-9
Hood, R., Budd, A., Sorond, F. A., and Hogue, C. W. (2018). Peri-operative neurological complications. Anaesthesia. 73(Suppl. 1), 67–75. doi: 10.1111/anae.14142
Hovens, I. B., van Leeuwen, B. L., Mariani, M. A., Kraneveld, A. D., and Schoemaker, R. G. (2016). Postoperative cognitive dysfunction and neuroinflammation: Cardiac surgery and abdominal surgery are not the same. Brain Behav. Immun. 54, 178–193. doi: 10.1016/j.bbi.2016.02.003
Hughes, C. G., Boncyk, C. S., Culley, D. J., Fleisher, L. A., Leung, J. M., McDonagh, D. L., et al. (2020). American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative delirium prevention. Anesth. Analg. 130, 1572–1590. doi: 10.1213/ANE.0000000000004641
Hussain, M., Berger, M., Eckenhoff, R. G., and Seitz, D. P. (2014). General anesthetic and the risk of dementia in elderly patients: current insights. Clin. Interv. Aging. 9, 1619–1628. doi: 10.2147/CIA.S49680
Inouye, S. K., Marcantonio, E. R., Kosar, C. M., Tommet, D., Schmitt, E. M., Travison, T. G., et al. (2016). The short-term and long-term relationship between delirium and cognitive trajectory in older surgical patients. Alzheimers Dement. 12, 766–775. doi: 10.1016/j.jalz.2016.03.005
Inouye, S. K., Westendorp, R. G., and Saczynski, J. S. (2014). Delirium in elderly people. Lancet. 383, 911–922. doi: 10.1016/S0140-6736(13)60688-1
Jensen, B. Ø., Rasmussen, L. S., and Steinbrüchel, D. A. (2008). Cognitive outcomes in elderly high-risk patients 1 year after off-pump versus on-pump coronary artery bypass grafting. A randomized trial. Eur. J. Cardiothorac. Surg. 34, 1016–1021. doi: 10.1016/j.ejcts.2008.07.053
Jin, Z., Hu, J., and Ma, D. (2020). Postoperative delirium: perioperative assessment, risk reduction, and management. Br. J. Anaesth. 125, 492–504. doi: 10.1016/j.bja.2020.06.063
Kirfel, A., Menzenbach, J., Guttenthaler, V., Feggeler, J., Mayr, A., Coburn, M., et al. (2021). Postoperative delirium after cardiac surgery of elderly patients as an independent risk factor for prolonged length of stay in intensive care unit and in hospital. Aging Clin. Exp. Res. 33, 3047–3056. doi: 10.1007/s40520-021-01842-x
Kleindienst, A., Hesse, F., Bullock, M. R., and Buchfelder, M. (2007). The neurotrophic protein S100B: value as a marker of brain damage and possible therapeutic implications. Prog. Brain Res. 161, 317–325. doi: 10.1016/S0079-6123(06)61022-4
Kotfis, K., Szylińska, A., Listewnik, M., Strzelbicka, M., Brykczyński, M., Rotter, I., et al. (2018). Early delirium after cardiac surgery: an analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin. Interv. Aging. 13, 1061–1070. doi: 10.2147/CIA.S166909
Langer, T., Santini, A., Zadek, F., Chiodi, M., Pugni, P., Cordolcini, V., et al. (2019). Intraoperative hypotension is not associated with postoperative cognitive dysfunction in elderly patients undergoing general anesthesia for surgery: results of a randomized controlled pilot trial. J. Clin. Anesth. 52, 111–118. doi: 10.1016/j.jclinane.2018.09.021
Liebig, J. (1853). Ueber Kynurensäure. Justus Liebigs Ann. Chem. 86, 125–126. doi: 10.1016/S0021-9258(18)97483-1
Lin, Y., Chen, J., and Wang, Z. (2012). Meta-analysis of factors which influence delirium following cardiac surgery. J. Card. Surg. 27, 481–492. doi: 10.1111/j.1540-8191.2012.01472.x
Lingehall, H. C., Smulter, N. S., Lindahl, E., Lindkvist, M., Engström, K. G., Gustafson, Y. G., et al. (2017). Preoperative cognitive performance and postoperative delirium are independently associated with future dementia in older people who have undergone cardiac surgery: a longitudinal cohort study. Crit. Care Med. 45, 1295–1303. doi: 10.1097/CCM.0000000000002483
Liu, Y. H., Wang, D. X., Li, L. H., Wu, X. M., Shan, G. J., Su, Y., et al. (2009). The effects of cardiopulmonary bypass on the number of cerebral microemboli and the incidence of cognitive dysfunction after coronary artery bypass graft surgery. Anesth. Analg. 109, 1013–1022. doi: 10.1213/ane.0b013e3181aed2bb
Luo, A., Yan, J., Tang, X., Zhao, Y., Zhou, B., and Li, S. (2019). Postoperative cognitive dysfunction in the aged: the collision of neuroinflammaging with perioperative neuroinflammation. Inflammopharmacology. 27, 27–37. doi: 10.1007/s10787-018-00559-0
Luo, G., Wang, X., Cui, Y., Cao, Y., Zhao, Z., and Zhang, J. (2021). Metabolic reprogramming mediates hippocampal microglial M1 polarization in response to surgical trauma causing perioperative neurocognitive disorders. J. Neuroinflammation. 18, 267. doi: 10.1186/s12974-021-02318-5
Majewski, P., Zegan-Barańska, M., Karolak, I., Kaim, K., Zukowski, M., and Kotfis, K. (2020). Current evidence regarding biomarkers used to aid postoperative delirium diagnosis in the field of cardiac surgery-review. Medicina. 56, 493. doi: 10.3390/medicina56100493
Maldonado, J. R. (2013). Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am. J. Geriatr. Psychiatry. 21, 1190–1222. doi: 10.1016/j.jagp.2013.09.005
Marangos, P. J., and Schmechel, D. E. (1987). Neuron specific enolase, a clinically useful marker for neurons and neuroendocrine cells. Annu. Rev. Neurosci. 10, 269–295. doi: 10.1146/annurev.ne.10.030187.001413
McDonagh, D. L., Berger, M., Mathew, J. P., Graffagnino, C., Milano, C. A., and Newman, M. F. (2014). Neurological complications of cardiac surgery. Lancet Neurol. 13, 490–502. doi: 10.1016/S1474-4422(14)70004-3
Meybohm, P., Bein, B., Brosteanu, O., Cremer, J., Gruenewald, M., Stoppe, C., et al. (2015). A multicenter trial of remote ischemic preconditioning for heart surgery. N. Engl. J. Med. 373, 1397–1407. doi: 10.1056/NEJMoa1413579
Møller, C. H., Penninga, L., Wetterslev, J., Steinbrüchel, D. A., and Gluud, C. (2008). Clinical outcomes in randomized trials of off- vs. on-pump coronary artery bypass surgery: systematic review with meta-analyses and trial sequential analyses. Eur. Heart J. 29, 2601–2616. doi: 10.1093/eurheartj/ehn335
Monk, T. G., Weldon, B. C., Garvan, C. W., Dede, D. E., van der Aa, M. T., Heilman, K. M., et al. (2008). Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 108, 18–30. doi: 10.1097/01.anes.0000296071.19434.1e
Moore, B. W., and McGregor, D. (1965). Chromatographic and electrophoretic fractionation of soluble proteins of brain and liver. J Biol Chem. 240, 1647–1653.
Nadelson, M. R., Sanders, R. D., and Avidan, M. S. (2014). Perioperative cognitive trajectory in adults. Br. J. Anaesth. 112, 440–451. doi: 10.1093/bja/aet420
Newman, M. F., Kirchner, J. L., Phillips-Bute, B., Gaver, V., Grocott, H., Jones, R. H., et al. (2001). Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N. Engl. J. Med. 344, 395–402. doi: 10.1056/NEJM200102083440601
O'Brien, H., Mohan, H., Hare, C. O., Reynolds, J. V., and Kenny, R. A. (2017). Mind over matter? The hidden epidemic of cognitive dysfunction in the older surgical patient. Ann. Surg. 265, 677–691. doi: 10.1097/SLA.0000000000001900
Pereira, J. V., Aung Thein, M. Z., Nitchingham, A., and Caplan, G. A. (2021). Delirium in older adults is associated with development of new dementia: a systematic review and meta-analysis. Int. J. Geriatr. Psychiatry. 36, 993–1003. doi: 10.1002/gps.5508
Pisano, A., Torella, M., Yavorovskiy, A., and Landoni, G. (2021). The impact of anesthetic regimen on outcomes in adult cardiac surgery: a narrative review. J. Cardiothorac. Vasc. Anesth. 35, 711–729. doi: 10.1053/j.jvca.2020.03.054
Plaschke, K., Fichtenkamm, P., Schramm, C., Hauth, S., Martin, E., Verch, M., et al. (2010). Early postoperative delirium after open-heart cardiac surgery is associated with decreased bispectral EEG and increased cortisol and interleukin-6. Intensive Care Med. 36, 2081–2089. doi: 10.1007/s00134-010-2004-4
Qiu, L. L., Pan, W., Luo, D., Zhang, G. F., Zhou, Z. Q., Sun, X. Y., et al. (2020). Dysregulation of BDNF/TrkB signaling mediated by NMDAR/Ca2+/calpain might contribute to postoperative cognitive dysfunction in aging mice. J. Neuroinflammation. 17, 23. doi: 10.1186/s12974-019-1695-x
Rasmussen, L. S., Christiansen, M., Hansen, P. B., and Moller, J. T. (1999). Do blood levels of neuron-specific enolase and S-100 protein reflect cognitive dysfunction after coronary artery bypass? Acta Anaesthesiol. Scand. 43, 495–500. doi: 10.1034/j.1399-6576.1999.430502.x
Saczynski, J. S., Marcantonio, E. R., Quach, L., Fong, T. G., Gross, A., Inouye, S. K., et al. (2012). Cognitive trajectories after postoperative delirium. N. Engl. J. Med. 367, 30–39. doi: 10.1056/NEJMoa1112923
Safavynia, S. A., and Goldstein, P. A. (2019). The role of neuroinflammation in postoperative cognitive dysfunction: Moving from hypothesis to treatment. Front. Psychiatry. 9, 752. doi: 10.3389/fpsyt.2018.00752
Sanjanwala, R., Stoppe, C., Khoynezhad, A., Hill, A., Engelman, D. T., and Arora, R. C. (2020). Delirium prevention in postcardiac surgical critical care. Crit. Care Clin. 36, 675–690. doi: 10.1016/j.ccc.2020.06.001
Selnes, O. A., Grega, M. A., Bailey, M. M., Pham, L. D., Zeger, S. L., Baumgartner, W. A., et al. (2009). Do management strategies for coronary artery disease influence 6-year cognitive outcomes? Ann. Thorac. Surg. 88, 445–454. doi: 10.1016/j.athoracsur.2009.04.061
Smith, R., Chepisheva, M., Cronin, T., and Seemungal, B. M. (2019). “Diagnostic approaches techniques in concussion/mild traumatic brain injury: Where are we?” in Neurosensory Disorders in Mild Traumatic Brain Injury, eds M. E. Hoffer and C. D. Balaban (London: Academic Press), 247–277. doi: 10.1016/B978-0-12-812344-7.00016-9
Snyder, B., Simone, S. M., Giovannetti, T., and Floyd, T. F. (2021). Cerebral hypoxia: its role in age-related chronic and acute cognitive dysfunction. Anesth. Analg. 132, 1502–1513. doi: 10.1213/ANE.0000000000005525
Steinmetz, J., Christensen, K. B., Lund, T., Lohse, N., and Rasmussen, L. S. (2009). Long-term consequences of postoperative cognitive dysfunction. Anesthesiology 110, 548–555. doi: 10.1097/ALN.0b013e318195b569
Su, X., Meng, Z. T., Wu, X. H., Cui, F., Li, H. L., Wang, D. X., et al. (2016). Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet 388, 1893–1902. doi: 10.1016/S0140-6736(16)30580-3
Subramaniam, B., Shankar, P., Shaefi, S., Mueller, A., O'Gara, B., Banner-Goodspeed, V., et al. (2019). Effect of intravenous acetaminophen vs. placebo combined with propofol or dexmedetomidine on postoperative delirium among older patients following cardiac surgery: the DEXACET randomized clinical trial. JAMA. 321, 686–696. doi: 10.1001/jama.2019.0234
Subramaniyan, S., and Terrando, N. (2019). Neuroinflammation and perioperative neurocognitive disorders. Anesth. Analg. 128, 781–788. doi: 10.1213/ANE.0000000000004053
Sun, Y., Jiang, M., Ji, Y., Sun, Y., Liu, Y., and Shen, W. (2019). Impact of postoperative dexmedetomidine infusion on incidence of delirium in elderly patients undergoing major elective noncardiac surgery: a randomized clinical trial. Drug Des. Devel. Ther. 13, 2911–2922. doi: 10.2147/DDDT.S208703
Szwed, K., Słomka, A., Pawliszak, W., Szwed, M., Anisimowicz, L., Zekanowska, E., et al. (2020). Novel markers for predicting type 2 neurologic complications of coronary artery bypass grafting. Ann. Thorac. Surg. 110, 599–607. doi: 10.1016/j.athoracsur.2019.10.071
Tan, X. X., Qiu, L. L., and Sun, J. (2021). Research progress on the role of inflammatory mechanisms in the development of postoperative cognitive dysfunction. Biomed. Res. Int. 2021, 3883204. doi: 10.1155/2021/3883204
Thackeray, J. T., Hupe, H. C., Wang, Y., Bankstahl, J. P., Berding, G., Ross, T. L., et al. (2018). Myocardial inflammation predicts remodeling and neuroinflammation after myocardial infarction. J. Am. Coll. Cardiol. 71, 263–275. doi: 10.1016/j.jacc.2017.11.024
Uhlig, C., Bluth, T., Schwarz, K., Deckert, S., Heinrich, L., De Hert, S., et al. (2016). Effects of volatile anesthetics on mortality and postoperative pulmonary and other complications in patients undergoing surgery: a systematic review and meta-analysis. Anesthesiology. 124, 1230–1245. doi: 10.1097/ALN.0000000000001120
van der Wulp, K., van Wely, M. H., Rooijakkers, M., Brouwer, M. A., van den Boogaard, M., Pickkers, P., et al. (2020). Delirium after TAVR: Crosspassing the limit of resilience. JACC Cardiovasc. Interv. 13, 2453–2466. doi: 10.1016/j.jcin.2020.07.044
van Dijk, D., Spoor, M., Hijman, R., Nathoe, H. M., Borst, C., Jansen, E. W., et al. (2007). Cognitive and cardiac outcomes 5 years after off-pump vs. on-pump coronary artery bypass graft surgery. JAMA. 297, 701–708. doi: 10.1001/jama.297.7.701
van Harten, A. E., Scheeren, T. W., and Absalom, A. R. (2012). A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anaesthesia. Anaesthesia. 67, 280–293. doi: 10.1111/j.1365-2044.2011.07008.x
van Munster, B. C., Bisschop, P. H., Zwinderman, A. H., Korevaar, J. C., Endert, E., Wiersinga, W. J., et al. (2010). Cortisol, interleukins and S100B in delirium in the elderly. Brain Cogn. 74, 18–23. doi: 10.1016/j.bandc.2010.05.010
Wang, P., Velagapudi, R., Kong, C., Rodriguiz, R. M., Wetsel, W. C., Yang, T., et al. (2020). Neurovascular and immune mechanisms that regulate postoperative delirium superimposed on dementia. Alzheimers Dement. 16, 734–749. doi: 10.1002/alz.12064
Wang, Y., Machizawa, M. G., Lisle, T., Williams, C. L., Clarke, R., Anzivino, M., et al. (2022). Suppression of neuroinflammation attenuates persistent cognitive and neurogenic deficits in a rat model of cardiopulmonary bypass. Front. Cell Neurosci. 16, 780880. doi: 10.3389/fncel.2022.780880
White, S., Griffiths, R., Baxter, M., Beanland, T., Cross, J., Dhesi, J., et al. (2019). Guidelines for the peri-operative care of people with dementia: guidelines from the Association of Anaesthetists. Anaesthesia. 74, 357–372. doi: 10.1111/anae.14530
Wilson, J. E., Mart, M. F., Cunningham, C., Shehabi, Y., Girard, T. D., MacLullich, A., et al. (2020). Delirium. Nat. Rev. Dis. Primers. 6:90. doi: 10.1038/s41572-020-00223-4
Wu, L., Zhao, H., Weng, H., and Ma, D. (2019). Lasting effects of general anesthetics on the brain in the young and elderly: “mixed picture” of neurotoxicity, neuroprotection and cognitive impairment. J. Anesth. 33, 321–335. doi: 10.1007/s00540-019-02623-7
Xu, X., Hu, Y., Yan, E., Zhan, G., Liu, C., and Yang, C. (2020). Perioperative neurocognitive dysfunction: thinking from the gut? Aging. 12, 15797–15817. doi: 10.18632/aging.103738
Yang, T., and Terrando, N. (2019). The evolving role of specialized pro-resolving mediators in modulating neuroinflammation in perioperative neurocognitive disorders. Adv. Exp. Med. Biol. 1161, 27–35. doi: 10.1007/978-3-030-21735-8_4
Yang, T., Velagapudi, R., and Terrando, N. (2020). Neuroinflammation after surgery: From mechanisms to therapeutic targets. Nat. Immunol. 21, 1319–1326. doi: 10.1038/s41590-020-00812-1
Yule, S., Flin, R., Paterson-Brown, S., Maran, N., and Rowley, D. (2006). Development of a rating system for surgeons' non-technical skills. Med. Educ. 40, 1098–1104. doi: 10.1111/j.1365-2929.2006.02610.x
Yumuk, V., Tsigos, C., Fried, M., Schindler, K., Busetto, L., Micic, D., et al. (2015). European guidelines for obesity management in adults. Obes Facts. 8, 402–424. doi: 10.1159/000442721
Zheng, F., Sheinberg, R., Yee, M. S., Ono, M., Zheng, Y., and Hogue, C. W. (2013). Cerebral near-infrared spectroscopy monitoring and neurologic outcomes in adult cardiac surgery patients: a systematic review. Anesth. Analg. 116, 663–676. doi: 10.1213/ANE.0b013e318277a255
Keywords: markers, perioperative neurocognitive disorders, postoperative cognitive dysfunction, postoperative delirium, CiteSpace, scientometrics
Citation: Ji L and Li F (2022) Potential Markers of Neurocognitive Disorders After Cardiac Surgery: A Bibliometric and Visual Analysis. Front. Aging Neurosci. 14:868158. doi: 10.3389/fnagi.2022.868158
Received: 02 February 2022; Accepted: 20 April 2022;
Published: 01 June 2022.
Edited by:
Rodrigo Gutierrez, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Juan C. Pedemonte, Pontificia Universidad Católica de Chile, ChileCopyright © 2022 Ji and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Li, bGlfZmFuZ0BjY211LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.