
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Aging Neurosci. , 16 March 2022
Sec. Alzheimer's Disease and Related Dementias
Volume 14 - 2022 | https://doi.org/10.3389/fnagi.2022.865933
This article is part of the Research Topic The Alzheimer's Disease Challenge, Volume II View all 14 articles
 Yuxian Li1,2†
Yuxian Li1,2† Fangda Leng1†
Fangda Leng1† Qi Xiong3†
Qi Xiong3† Jiong Zhou4
Jiong Zhou4 Ailian Du5
Ailian Du5 Feiqi Zhu6
Feiqi Zhu6 Xiaowen Kou7
Xiaowen Kou7 Wei Sun1
Wei Sun1 Luzeng Chen8
Luzeng Chen8 Huali Wang9
Huali Wang9 Hengge Xie10
Hengge Xie10 Feng Gao3*
Feng Gao3* Haiqiang Jin1*
Haiqiang Jin1* Yongan Sun1*
Yongan Sun1*
Background: The increasing prevalence of Alzheimer’s disease (AD) has emerged as a major challenge worldwide. China as the most populous country in the globe is amid rapid aging of its population, highlighting the need for appropriate social and medical policies to meet the challenge. The current multicenter cross-sectional observational study aims to provide understanding of the current status of caring given to AD patients in China and investigate the factors that influence the family burden as well as the choice of care given to AD patients.
Methods: A total of 1,675 patients with probable AD from 30 provincial regions of mainland China were enrolled in the current study from August 2019 to December 2019. We analyzed the caregiving status and its relationship with family burden and various socio-economical and medical factors.
Results: In the current study, 90.87% of the AD patients enrolled adopted family care. The choice of caregiving method was influenced by factors including age (>80 years old, OR 0.648; 95% CI, 0.427–0.983), overall family burden (high, OR 0.574; 95% CI, 0.0.373–0.884), patients’ income (OR 0.511; 95% CI, 0.330–0.789) and self-care ability (OR 0.329; 95% CI, 0.183–0.588).
Conclusion: Family care is the primary method of care for AD patients in China and the institutional care system for AD patients is still underprepared in China.
China as the world’s most populous country is amid the rapid aging of its population, which is accompanied by a drastic increase of dementia prevalence (Pei et al., 2014). Alzheimer’s disease (AD) is the most common type of senile dementia, accounting for over 60% of all-cause dementia (Alzheimer’s Association, 2018). It has been estimated that the prevalence of AD among senior citizens above 65 year old is 3.21% and increases substantially with age among Chinese population (Jia et al., 2014), which has a considerable sociological and economic impact on Mainland China. It is estimated that the average socioeconomic cost of AD per patient per year is 19,144 USD in mainland China (Jia et al., 2018). The annual total cost is predicted to reach 1.89 trillion USD in 2030 in China, rendering the care of AD patients beyond a medical issue, but also an outstanding sociological problem.
Among the issues that awaits to be addressed are how to provide AD patients with appropriate care and to reduce the burden for the families. While it has been suggested that family care might be a better method of care for patients with AD considering its emotional and psychological comfort (Luppa et al., 2010), studies from high-income countries have demonstrated that institutional care offers better functional outcome compared to family care (Afram et al., 2014; Lee et al., 2019). Further, the demands of caring responsibilities change with the stages of disease, which can be a great challenge for the family. In Europe, it has been reported that the emotional and psychological distress to family caregivers enforced by Alzheimer’s disease urged families to seek professional care for the patients (Bokberg et al., 2015). However, the domestic situation with regard to care giving for AD patients remains to be investigated in China, as such socio-economical issues are highly entangled by cultural and economic factors, with huge variabilities among different nations.
As an example, in western society, the choice of home or institutional care of a patient may mainly depend on personal needs, financial situations, and the accessibility of professional care (Genet et al., 2011), while in China, sending elderlies to care homes may be seen as a betrayal to the family. To date, few studies have been conducted on the caregiving status and the relationship between caregiver burden and patient factors in China. The lack of understanding on the current status of care given to domestic AD patients, together with the short of analytical data on the underlying factors have left policymakers in dark to improve welfare for AD patients and their families. In the current study, we hypothesized that the burden of family members is a major factor that influences the decision of home or institutional care for AD patients in China. We aimed to investigate the current caregiving status and burden as well as to analyze the relationship between caregiver burden and patient factors to suggest ideas for policy and research programs on chronic diseases.
This study was approved by the Ethics Committee of Peking University First Hospital (PUFH-2019-141), the leading institution of the study, and local ethic committees in all participating centers. informed consent were obtained from all patients and family members.
This is a large-sample, multi-center, cross-sectional study performed between August 2019 and December 2019. We collected data from 30 provincial, municipal, and autonomous regions of mainland China. Among them, the eastern provinces, such as Zhejiang, Beijing, and Hebei contributed the most participants (Figure 1).
The recruitment of participants was based on the hierarchical healthcare structure in China, where there are 3 levels of healthcare infrastructures, with the first level being community clinics and the third level being the local health centers. The participants were referred to the local health centers by local clinics or sought consultation directly from the health centers, where the patients were diagnosed as clinical probable AD by qualified neurology specialists from the local health centers. The diagnosis of probable AD dementia was based on the diagnostic criteria established by the National Institute of Aging and Alzheimer’s Association (NIA-AA) in 2011 (McKhann et al., 2011). Other inclusion criteria include: (1) capability to give written consent, (2) next of kin’s consent to participate, and (3) >5 years of education. Patients with other neurological diseases that are associated with cognitive impairment and major psychiatric disorders were excluded. In particular, patients with signs and symptoms suggesting other types of dementia, such as Parkinson’s disease dementia, Lewy body dementia, frontotemporal dementia, primary progressive aphasia, vascular dementia and mixed dementia.
All medical staff who conducted the study were given comprehensive training on the usage of the questionnaire used in the study. Family members and professional caregivers (for patients in nursing facilities) of the patients completed the questionnaire under the guidance of doctors. For those who had already been in care homes, the family members were instructed to answer the questionnaire according to the situation when the patients were last at home. The current study focused on the perceived care burden by family members as (1) in the vast majority of scenarios it were the family members who accompanied the patients to the health centers, and (2) the decisions of home care vs. institutional care were made by the patients and their families.
We designed a comprehensive questionnaire, which includes demographic characteristics, household income, medical history with regard to AD, care situation, and burden to the family. The caregiving status of the patients was divided into two categories, including family care and institutional care. Family care was defined as situations in which family members, including spouses, children, grandchildren, and other relatives, take care of AD patients with or without the help of a health professional. Institutional care indicates that the patients are taken care of by professionals in nursing facilities. Similarly, self-care ability was divided into two classes: basic self-care and partially or completely dependent. The type of caregiving was assessed by caregivers based on whether the patients could take care of themselves in their daily lives.
The caregiver burden inventory (CBI) (Chinese version) was used to describe the multidimensional burden of the caregivers and to distinguish related factors of different burden dimensions (Novak and Guest, 1989). The translation and validation of CBI in Chinese population was performed by Chou et al. (2002). The inventory consists of 24 questions that refer to five dimensions: time-dependence burden (questions 1–5), developmental burden (questions 6–10), physical burden (questions 11–14), social burden (questions 15–18), and emotional burden (questions 19–24). Each item was graded on a 4-point Likert scale according to the degree of each situation. A high score represented a high burden and the total score is 96. The point range from 0 to 32 was considered as a low burden, from 33 to 64 as a medium burden, and from 65 to 96 as a high burden.
The questionnaires were examined manually to ensure completeness and effectiveness immediate after the interview by staff. Incomplete questionnaire and those with obvious contradictory answers to the interview were considered invalid.
Patients and family members’ characteristics, including gender, age, housing condition, education, and annual household income were presented using descriptive statistics. Quantitative variables were examined for normal distribution and presented as the mean ± standard deviation. Independent-samples t-tests and one-way ANOVA were performed for group-wise comparisons of continuous variables. Chi-square tests were performed to examine cross-group differences of categorical variables. To examine the reliability performance of CBI in the settings of current study, Cronbach’s alpha was calculated for all the items in the inventory and each of the five dimensions. Cronbach’s alpha efficient >0.9 was considered to indicate excellent internal consistency, and >0.8 was considered to indicate good consistency. Factors with P < 0.2 in group-wise comparisons were then entered to binary logistic regression models to evaluate the influence of each factors in the choice of caregiving for AD patients, controlling for age and gender. All data analyses were performed using SPSS 26.0 (SPSS Inc., Chicago, IL, United States). Differences were considered statistically significant when the P-value was less than 0.05.
A total of 1,694 people participated in the survey. After eliminating the erroneous and invalid questionnaires, 1,675 valid questionnaires were left, resulting in an effectiveness of 98.88%.
The patients characteristics are presented in Table 1. The 1675 AD patients were from 30 provincial, municipal, and autonomous regions of mainland China, including 650 (38.81%) men and 1,025 (61.19%) women. The participation of patients in urban areas was higher than that in rural areas (79.76 vs. 20.24%). The geographical distribution of the patients is illustrated in Figure 1.
Of the 1,675 AD patients sampled, 1522 (90.87%) patient chose family care and 153 (9.13%) patients lived in care homes. To identify the factors associated with the choice of care, we analyzed the characteristics of the patients’ caregiving status (Table 2). Home cared and institution cared patients did not differ by gender or education level. Patients who were above 80 years (P = 0.003) and living in urban areas (P < 0.001) were more likely to choose institutional care compared to those who were younger and in rural regions. Concerning economic status, the choice of patient care is related to the annual income of the patient (P < 0.001). A greater proportion of patients living in nursing homes belong to a higher income group; however, no significant difference was found between annual household income groups (P = 0.122). According to self-care ability and CBI score, patients who are less capable of taking care of themselves and who impose a large burden to family caregivers tended to choose nursing facilities (P = 0.001).
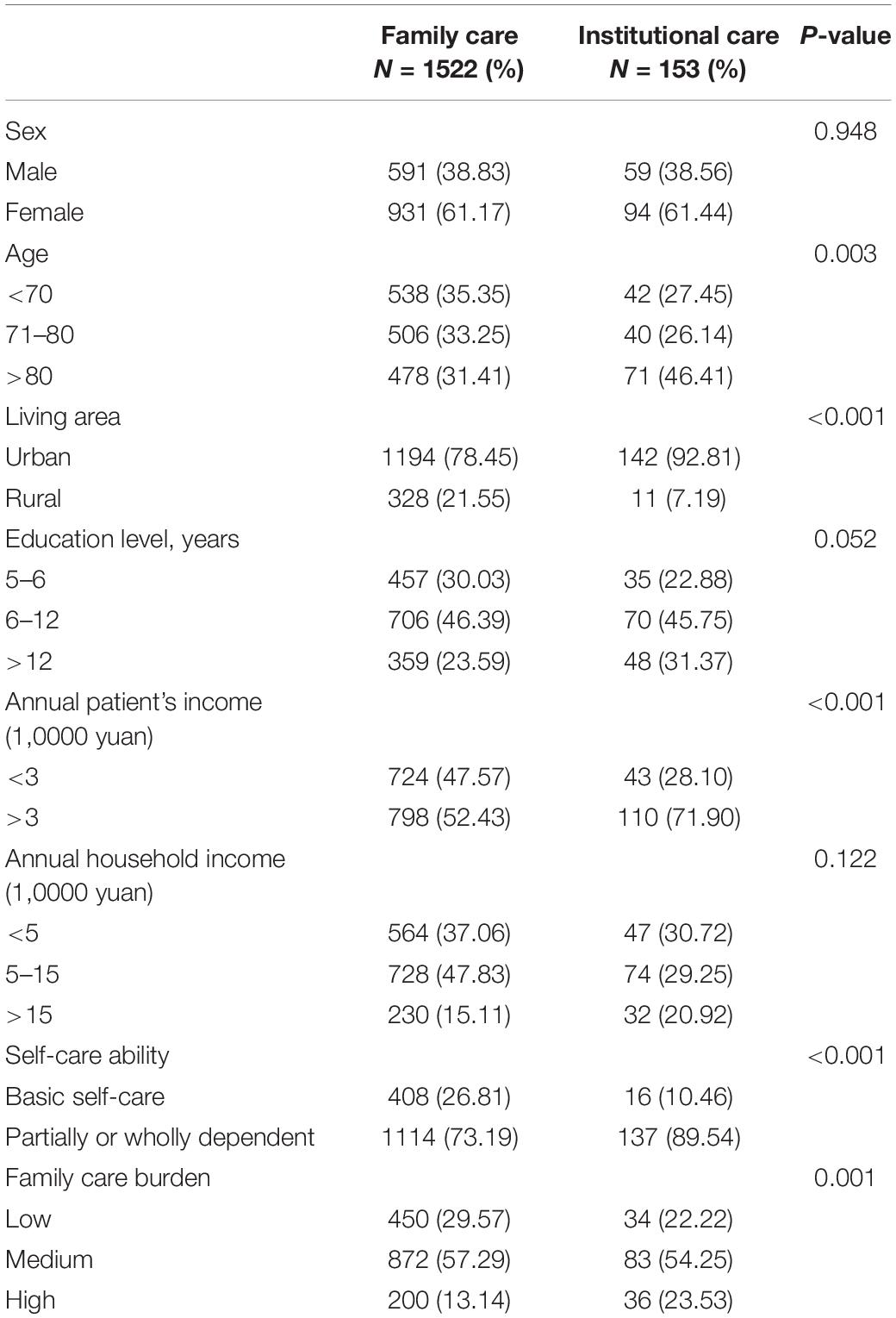
Table 2. The caregiving status of the familial caregiver of patients with AD in relation to patient and caregiver characteristics (N = 1675).
We used binary logistic regression analysis to identify the relevant factors for choosing nursing facilities for patients with AD (Table 3). Urban patients are more likely to choose nursing homes than rural patients (OR = 2.374; 95% CI, 1.228–4.588). Impaired self-care ability was also a predictor of choosing nursing homes over family care (OR = 0.329; 95% CI, 0.183–0.588). The family care burden is also a related factor, with families having higher perceived care burden being more inclined to seek institutional care (OR = 0.574; 95% CI,0.373–0.884).
In the current study, the overall Cronbach’s alpha of the CBI scale (24 items) was 0.950 (95% CI, 0.946–0.953); the time-dependence burden (5 items) dimension had a Cronbach’s alpha of 0.934 (95% CI, 0.929–0.940); developmental burden (five items) dimension had Cronbach’s alpha of 0.939 (95% CI, 0.933–0.944); physical burden (four items)’s Cronbach’s alpha was 0.954 (95% CI, 0.950–0.959); social burden (five items) dimension’s Cronbach’s alpha was 0.831 (95% CI, 0.0.815–0.845); and the Cronbach’s alpha of emotional burden (five items) was 0.854 (95% CI, 0.835–0.869). These coefficients indicated that the CBI scale had an excellent overall internal consistency and the sub-domains offered at least good reliability in the current study.
In this study, 25.31% of the patients could take basic care of themselves. The other 74.69% of patients were partially or wholly dependent on others for care. About 36.48% of patients were completely dependent on caregivers, indicating that a large proportion of AD patients had severe disabilities. According to the CBI scores, 28.90% of families had a relatively low level of burden, 14.09% of families had a high level of burden, and the remaining 57.01% had a medium level of burden. From the perspective of burden classification, all five dimensions of burden were separately calculated in the two different groups (Table 4). All aspects of family burden significantly increased when patients were not able to take care of themselves (P < 0.001). Caregiving status was also associated with burden grade. Families of patients who were at nursing facilities had a higher total burden of care (when the patients were last at home) compared to those home-cared (P < 0.001). In addition, in other aspects such as time-dependence, development limitation, health, and social contact, families bear a higher burden before the patients were sent to a nursing home than those home-cared.
The family burden was affected by both the self-care ability and caregiving status of the patients at the same time. To exclude confounding factors, we used stratified correlation analysis to determine the impact of self-care ability and caregiving status on the burden of caregivers (Table 5). There was no significant difference of family burden, either family care or nursing facility (P = 0.520), if the patients could take care of themselves. However, if the patients were incapable of self-care, the overall family burden was higher carer-dependent AD patients (P = 0.015), and the differences mainly manifested in the burden of time-dependence (P = 0.002) and the health of caregivers (P = 0.008).
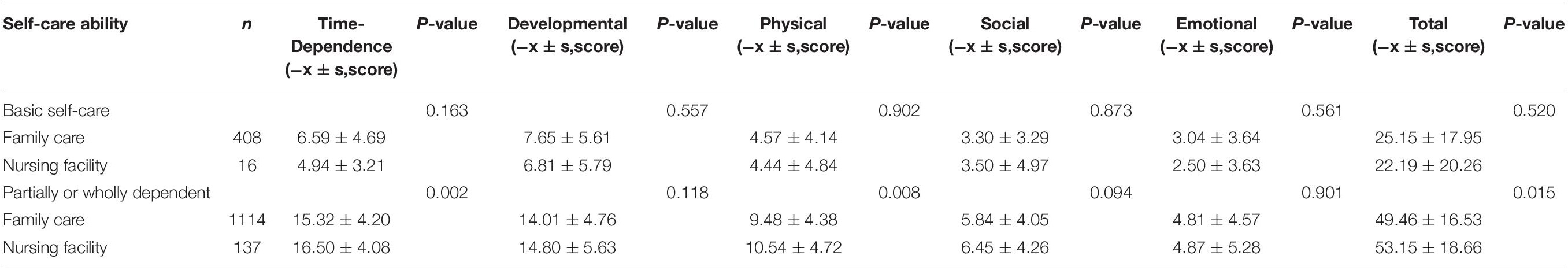
Table 5. CBI scores of family members with different care status after classification according to patient self-care ability.
Alzheimer’s disease is a progressive neurodegenerative disease, which causes cognitive decline in multiple cognitive domains including language, visuospatial, executive function, complex attention, perceptual-motor, social cognition, and most commonly, memory (McKhann et al., 2011). Behavioral and psychological symptoms gradually occur in AD patients, resulting in disability and most patients are completely dependent at later stages of the disease (Atri, 2019).
In the current study, the factors associated with the choice of home or institutional care for AD patients in China. We found that age (>80 years), living in urban areas, higher patient annual income, inability of self-care and high family care burden were associated with higher probability of choosing institutional care for AD patients in China.
Our results suggest that family care is the most common choice for families of AD patients in China, which is a common phenomenon in developing countries especially in Asia (Prince and Dementia Research Group, 2004). While increasing numbers of nursing facilities is being set up, Chinese families with AD patients have a low preference for institutional care (Table 6). Aside from the subjective reasons (disapproval by family members or patients), our questionnaire suggested that the primary reasons against institutional care were economic burden (34.9%) and insufficient service provided by the institutions (34.5%). Many people view that nursing homes cannot provide individual care to patients. It is noteworthy that some family caregivers (4.4% of all home-cared patients and 32.6% of all patients who have experienced institutional care) mention that the patients who earlier chose to live in a nursing home, for various reasons, often decide to leave the nursing home and return to family care. The striking proportion of AD patients dropping from nursing homes indicates deficiencies of Chinese institutional care system’s infrastructure and proficiency, which is evidenced by a lack of care professionals’ knowledge on dementia (Wang Y. et al., 2018). The low subjective preference of Chinese family for institutional care might be related to traditional cultural heritage, as Chinese people attach great importance to filial piety. In fact, during interview, some patients living nursing homes admitted feeling abandoned by their families. However, these socio-cultural factors were not quantitively analyzed in the current study and could be further investigated in following studies (Add some reference: agreement with literature, Cultural studies).
Most AD patients will deteriorate to a completely dependent state along disease trajectory, placing have care burdens to their families both economically and sociologically. An international multilateral cost-of-illness (COI) studies has summarized that the socioeconomic cost of AD includes direct medical, direct non-medical and indirect costs (Callahan, 2017). Jia et al. (2018) have predicted that the annual cost of AD patients worldwide to be US $9.12 trillion in 2050. The burden enforced by AD on families is not just financial, but also affects other aspects of life. For example, the symptoms of dementia often cause physical, emotional, and mental stress (D’Onofrio et al., 2015). Many studies have explored the influence factors of caregiver burden, indicating that the burden on caregivers is higher in families with lower income and disease severity (Montgomery et al., 2018; Kawano et al., 2020). In addition, disease related burden for family caregivers of AD patients increases drastically as disease progresses, and is influenced by the caregiver’s education, and being spouse of the patient (Lou et al., 2015; Liu et al., 2017b). Most families experience mental tension due to AD and a negative psychological interactions between caregivers and patients has been reported (Andren and Elmstahl, 2008). However, there are few recent and large-scale, multicenter studies on caregiver burden of Chinese AD patients, and most studies have focused on patients receiving family care (Yu et al., 2015; Liu et al., 2017a; Zhang et al., 2018). Hence, there is a lack of research on the impact of care style on family burden inflicted by AD in Chinese population.
According to the current study, the self-care ability and the burden on family members has a significant impact on care status of AD patients. The families who choose a nursing home for their elderly who lost self-care abilities usually have suffered a higher burden before and even after the decision of institutional care is made. Underdeveloped social nursing facilities in China also bring many concerns to families of AD patients, the care of whom is different from ordinary elderlies, and providing both medically and psychologically professional care for demented patients is an imminent problem for the institutional care systems in China. On the other hand, the social insurance system also results in a higher cost of living in a nursing home for the patients’ families, as reflected in by the influence of the patient’s personal income on the choice of care type. Further, the general public, including the family members’ lack of awareness and understanding of AD may also have negatively influence the caregiving status of AD patients and social burdens for their families (Dai et al., 2015; Zeng et al., 2015). Other aspects might also affect the choice, as studies have suggested that most families willing to send their elderly to nursing homes have a higher awareness of diseases, while less-caring families have lower perception of burden and tend to choose family care (Jia et al., 2020).
The current study has its implications for the improvement of China’s social insurance system, as it reflects a lack of accessible and professional nursing assistance for patients and families impacted by AD (Samus et al., 2018). For Chinese patients with AD, there are restricted alternatives and only few choices to live their lives with financial constraints (Zeng et al., 2020). According to a study in 2015, most AD patients in China have two offspring or more (80.56%), while 19.44% of participants have only one child or no child (Jia et al., 2018). However, the consequence of the one-child policy is changing the scenario dramatically in the upcoming decades, and a foreseeable challenge to the social care system is imminent, with a simulation study in has projected the economic burden associated with AD to increase by 37-fold by 2050 compared 2011 (Keogh-Brown et al., 2016). On the other hand, a more capable social support system (aside from financial aid) needs to be established both for the patients and the family members to ease their distress (Patterson et al., 1998; Wang Z. et al., 2018). Therefore, early warns should be given to policymakers to take effective measures.
The current study has some limitations that should be noted. First, due to practical limitations, we were unable to perform multistage sampling to ensure a balanced geographical sample, and the current work was lead by local health centers which volunteered to cooperate (the top level of the hierarchical structure in China). While these centers are responsible for referred patients from community clinic and walk-in outpatient services are accessible for all citizens, they are usually located in urban areas the sampling process has a predilection for urban dwellers, who could not fully represent the AD patient population in China. Secondly, the questionnaire used here was only available to patients who were diagnosed as clinically probable AD dementia and further studies could expand their scope to possible AD, MCI and all-cause dementia. Thirdly, the severity of AD was not quantified with our study design and functional health outcomes were not evaluated due to the cross-section nature of the study. The economic burden and mental stress of the patients’ family could be investigated in more detail in retrospect, for example, the service time of a family member as care giver would an important factor. All these problems warrant further investigation in a larger and more balanced patient cohort. Nevertheless, the current study has provided a basic understanding of the caregiving status and burden on Chinese families with AD patients.
In conclusion, the economic costs of AD come from all directions. Family care is the primary method of care for AD patients in China. The method of patient care is influenced by the housing condition, patient income, and disease severity. Overall, this study reveals the present situation of AD patients and their families and provides insights to help public health policymaking.
The datasets presented in this article are not readily available because of institutional privacy policy. Requests to access the datasets should be directed to YS, c3lhQGJqbXUuZWR1LmNu.
The studies involving human participants were reviewed and approved by the Ethics Committee of Peking University First Hospital. The patients/participants provided their written informed consent to participate in this study.
YL and FL contributed to the analysis and interpretation of the data, drafting and revision of the manuscript. QX, JZ, AD, FZ, WS, LC, HW, and HX contributed to collection of data, quality control, and establishing the database. XK contributed to advertising and coordination of the study. FG, HJ, and YS contributed to the conceptualization of the study, formulation of study protocol and intellectual revision of the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by the National Key R&D Program of China (2018YFC1314200), National Natural Science Foundation of China (82071306), and Group-Style Medical Aid Project for Tibet (XZ2017ZR-ZY13).
XK was employed by The People’s Daily, China.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We sincerely thank all members of the Alzheimer’s Disease China for their contributions to recruiting patients and data collection, and thank Health Times for questionnaire design and data analysis.
Afram, B., Stephan, A., Verbeek, H., Bleijlevens, M. H., Suhonen, R., Sutcliffe, C., et al. (2014). Reasons for institutionalization of people with dementia: informal caregiver reports from 8 European countries. J. Am. Med. Dir. Assoc. 15, 108–116. doi: 10.1016/j.jamda.2013.09.012
Alzheimer’s Association (2018). 2018 Alzheimer’s disease facts and figures. Alzheimers Dement. 14, 367–429. doi: 10.21926/obm.geriatr.1904079
Andren, S., and Elmstahl, S. (2008). The relationship between caregiver burden, caregivers’ perceived health and their sense of coherence in caring for elders with dementia. J. Clin. Nurs. 17, 790–799. doi: 10.1111/j.1365-2702.2007.02066.x
Atri, A. (2019). The Alzheimer’s Disease Clinical Spectrum: diagnosis and Management. Med. Clin. North. Am. 103, 263–293. doi: 10.1016/j.mcna.2018.10.009
Bokberg, C., Ahlstrom, G., Leino-Kilpi, H., Soto-Martin, M. E., Cabrera, E., Verbeek, H., et al. (2015). Care and Service at Home for Persons With Dementia in Europe. J. Nurs. Scholarsh. 47, 407–416. doi: 10.1111/jnu.12158
Callahan, C. M. (2017). Alzheimer’s Disease: individuals, Dyads, Communities, and Costs. J. Am. Geriatr. Soc. 65, 892–895. doi: 10.1111/jgs.14808
Chou, K. R., Jiann-Chyun, L., and Chu, H. (2002). The reliability and validity of the Chinese version of the caregiver burden inventory. Nurs. Res. 51, 324–331. doi: 10.1097/00006199-200209000-00009
Dai, B., Mao, Z., Wu, B., Mei, Y. J., Levkoff, S., and Wang, H. (2015). Family Caregiver’s Perception of Alzheimer’s disease and caregiving in Chinese culture. Soc. Work Public Health 30, 185–196. doi: 10.1080/19371918.2014.969858
D’Onofrio, G., Sancarlo, D., Addante, F., Ciccone, F., Cascavilla, L., Paris, F., et al. (2015). Caregiver burden characterization in patients with Alzheimer’s disease or vascular dementia. Int. J. Geriatr. Psychiatry 30, 891–899. doi: 10.1002/gps.4232
Genet, N., Boerma, W. G., Kringos, D. S., Bouman, A., Francke, A. L., Fagerstrom, C., et al. (2011). Home care in Europe: a systematic literature review. BMC Health Serv. Res. 11:207. doi: 10.1186/1472-6963-11-207
Jia, J., Wang, F., Wei, C., Zhou, A., Jia, X., Li, F., et al. (2014). The prevalence of dementia in urban and rural areas of China. Alzheimers. Dement. 10, 1–9. doi: 10.1016/j.jalz.2013.01.012
Jia, J., Wei, C., Chen, S., Li, F., Tang, Y., Qin, W., et al. (2018). The cost of Alzheimer’s disease in China and re-estimation of costs worldwide. Alzheimers. Dement. 14, 483–491. doi: 10.1016/j.jalz.2017.12.006
Jia, L., Quan, M., Fu, Y., Zhao, T., Li, Y., Wei, C., et al. (2020). Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. 19, 81–92. doi: 10.1016/S1474-4422(19)30290-X
Kawano, Y., Terada, S., Takenoshita, S., Hayashi, S., Oshima, Y., Miki, T., et al. (2020). Patient affect and caregiver burden in dementia. Psychogeriatrics 20, 189–195. doi: 10.1111/psyg.12487
Keogh-Brown, M. R., Jensen, H. T., Arrighi, H. M., and Smith, R. D. (2016). The Impact of Alzheimer’s Disease on the Chinese Economy. EBioMedicine 4, 184–190. doi: 10.1016/j.ebiom.2015.12.019
Lee, T. W., Yim, E. S., Choi, H. S., and Chung, J. (2019). Day care vs home care: effects on functional health outcomes among long-term care beneficiaries with dementia in Korea. Int. J. Geriatr. Psychiatry 34, 97–105. doi: 10.1002/gps.4992
Liu, S., Jin, Y., Shi, Z., Huo, Y. R., Guan, Y., Liu, M., et al. (2017a). The effects of behavioral and psychological symptoms on caregiver burden in frontotemporal dementia, Lewy body dementia, and Alzheimer’s disease: clinical experience in China. Aging Ment. Health 21, 651–657. doi: 10.1080/13607863.2016.1146871
Liu, S., Li, C., Shi, Z., Wang, X., Zhou, Y., Liu, S., et al. (2017b). Caregiver burden and prevalence of depression, anxiety and sleep disturbances in Alzheimer’s disease caregivers in China. J. Clin. Nurs. 26, 1291–1300. doi: 10.1111/jocn.13601
Lou, Q., Liu, S., Huo, Y. R., Liu, M., Liu, S., and Ji, Y. (2015). Comprehensive analysis of patient and caregiver predictors for caregiver burden, anxiety and depression in Alzheimer’s disease. J. Clin. Nurs. 24, 2668–2678. doi: 10.1111/jocn.12870
Luppa, M., Luck, T., Weyerer, S., Konig, H. H., Brahler, E., and Riedel-Heller, S. G. (2010). Prediction of institutionalization in the elderly. A systematic review. Age Ageing 39, 31–38. doi: 10.1093/ageing/afp202
McKhann, G. M., Knopman, D. S., Chertkow, H., Hyman, B. T., Jack, C. R. Jr., Kawas, C. H., et al. (2011). The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers. Dement. 7, 263–269. doi: 10.1016/j.jalz.2011.03.005
Montgomery, W., Goren, A., Kahle-Wrobleski, K., Nakamura, T., and Ueda, K. (2018). Alzheimer’s disease severity and its association with patient and caregiver quality of life in Japan: results of a community-based survey. BMC Geriatr. 18:141. doi: 10.1186/s12877-018-0831-2
Novak, M., and Guest, C. (1989). Application of a multidimensional caregiver burden inventory. Gerontologist 29, 798–803. doi: 10.1093/geront/29.6.798
Patterson, T. L., Semple, S. J., Shaw, W. S., Yu, E., He, Y., Zhang, M. Y., et al. (1998). The cultural context of caregiving: a comparison of Alzheimer’s caregivers in Shanghai, China and San Diego, California. Psychol. Med. 28, 1071–1084. doi: 10.1017/s0033291798007053
Pei, J. J., Giron, M. S., Jia, J., and Wang, H. X. (2014). Dementia studies in Chinese populations. Neurosci. Bull. 30, 207–216. doi: 10.1007/s12264-013-1420-1
Prince, M., and Dementia Research Group (2004). Care arrangements for people with dementia in developing countries. Int. J. Geriatr. Psychiatry 19, 170–177. doi: 10.1002/gps.1046
Samus, Q. M., Black, B. S., Bovenkamp, D., Buckley, M., Callahan, C., Davis, K., et al. (2018). Home is where the future is: the BrightFocus Foundation consensus panel on dementia care. Alzheimers. Dement. 14, 104–114. doi: 10.1016/j.jalz.2017.10.006
Wang, Y., Xiao, L. D., Luo, Y., Xiao, S. Y., Whitehead, C., and Davies, O. (2018). Community health professionals’ dementia knowledge, attitudes and care approach: a cross-sectional survey in Changsha, China. BMC Geriatr. 18:122. doi: 10.1186/s12877-018-0821-4
Wang, Z., Ma, C., Han, H., He, R., Zhou, L., Liang, R., et al. (2018). Caregiver burden in Alzheimer’s disease: moderation effects of social support and mediation effects of positive aspects of caregiving. Int. J. Geriatr. Psychiatry Epub online ahead of print. doi: 10.1002/gps.4910
Yu, H., Wang, X., He, R., Liang, R., and Zhou, L. (2015). Measuring the Caregiver Burden of Caring for Community-Residing People with Alzheimer’s Disease. PLoS One 10:e0132168. doi: 10.1371/journal.pone.0132168
Zeng, F., Xie, W. T., Wang, Y. J., Luo, H. B., Shi, X. Q., and Zou, H. Q. (2015). General public perceptions and attitudes toward Alzheimer’s disease from five cities in China. J. Alzheimers. Dis. 43, 511–518. doi: 10.3233/JAD-141371
Zeng, Q., Wang, Q., Zhang, L., and Xu, X. (2020). Comparison of the Measurement of Long-Term Care Costs between China and Other Countries: a Systematic Review of the Last Decade. Healthcare 8:117. doi: 10.3390/healthcare8020117
Keywords: Alzheimer’s disease, home care, caregiver burden, institutional care, care preference, caregiving
Citation: Li Y, Leng F, Xiong Q, Zhou J, Du A, Zhu F, Kou X, Sun W, Chen L, Wang H, Xie H, Gao F, Jin H and Sun Y (2022) Factors Associated With Alzheimer’s Disease Patients’ Caregiving Status and Family Caregiving Burden in China. Front. Aging Neurosci. 14:865933. doi: 10.3389/fnagi.2022.865933
Received: 30 January 2022; Accepted: 21 February 2022;
Published: 16 March 2022.
Edited by:
Athanasios Alexiou, Novel Global Community Educational Foundation (NGCEF), AustraliaReviewed by:
Mohammedamin Hajure Jarso, Mettu University, EthiopiaCopyright © 2022 Li, Leng, Xiong, Zhou, Du, Zhu, Kou, Sun, Chen, Wang, Xie, Gao, Jin and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongan Sun, c3lhQGJqbXUuZWR1LmNu; Feng Gao, bHVja3lnZjIwMDRAMTYzLmNvbQ==; Haiqiang Jin, amhxOTExQGJqbXUuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.