- 1Department of Ophthalmology, Wenzhou Medical University, Wenzhou, China
- 2Department of Neurology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 3Department of Neurology, The Yuhuan People’s Hospital, Taizhou, China
- 4Department of Traditional Chinese Medicine, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
Purpose: Lower serum vitamin D has been reported to be associated with stroke. This study aimed to analyze the risk factors of vitamin deficiency in Chinese stroke patients, and further analyze its impact in different gender and their clinical variables.
Methods: 982 stroke patients were enrolled. Laboratory parameters such as serum vitamin D, apolipoprotein A-I (ApoA-I), apolipoprotein B (ApoB), ApoA-I/ApoB, cholesterol (CH), fibrinogen (FIB), blood glucose (Glu), high-density lipoprotein (HDL), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) were collected and recorded. The severity of stroke was assessed by National Institute of Health Stroke Scale (NIHSS) score. Based on their serum vitamin D level, patients were divided into three groups: Vitamin D deficiency (<50 nmol/L), vitamin D insufficiency (≥50–75 nmol/L) and vitamin D sufficiency (≥75 nmol/L) and differences were compared among the three groups. Statistical analyses were done to assess the risk factors for serum vitamin D deficiency in our ischemic stroke patients.
Results: Gender, NIHSS, and FIB showed significant differences among the vitamin D groups (P < 0.001 ∼ P = 0.002). The female gender (OR = 2.422, P < 0.001), severity of stroke using NIHSS (OR = 1.055, P = 0.008) and FIB (OR = 1.256, P = 0.005) were risk factors of vitamin D deficiency in ischemic stroke patients. In subgroup analysis, NIHSS was significantly associated with vitamin D deficiency in the male group (OR = 1.087, P = 0.002) and higher FIB group (OR = 1.078, P = 0.001).
Conclusions: The female gender, severity of stroke using NIHSS and FIB were risk factors for vitamin D deficiency in our incident stroke patients. NIHSS was more sensitive to vitamin D deficiency in male ischemic stroke patients. Besides, under higher FIB circumstance, the increasing NIHSS score was more related to the vitamin D deficiency. Levels of vitamin D in patients with ischemic stroke should be well monitored during the disease cascade.
Introduction
Recent reports have shown a major rise in the aging population worldwide especially in China, the country with the largest population. Stroke has been reported to be one of the common cause of death worldwide but has been shown to be the leading cause of death in China (Zhou et al., 2019). Zhou et al. (2019) showed that more 80% of death cases in China were due to stroke. Nonetheless, reports of stroke in the Chinese population were neither population based or of reduced range and diagnostic precision; additionally most of these reports were done over two decades ago. Moreover, China has experienced rapid changes in their sociodemographic and health transitions have shown a significant impact on the prevalence of risk factors associated with stroke (Yang et al., 2013). Statistics have shown that there’s been a significant rise in the occurrence of smoking, hypertension and diabetes, all of which have been reported to be risk factors for stroke (Feigin et al., 2016). With these rapid changes in China, it would be helpful to obtain an up to date and accurate risk factor(s) to help in the recently implemented therapies and prevention measures.
Vitamin D, also known as 25-hydroxyvitamin D [25(OH) D] is known for its effects on the metabolism on bones and homeostasis of calcium (Berghout et al., 2019). A meta-analysis suggested that vitamin D helps reduces hazard of cardiovascular diseases and cognitive disorders, shedding light on its non-skeletal effects on the body (Zhou R. et al., 2018). A previous report showed the neuro-protective effects of vitamin D and its effect on the integrity of the blood brain barrier (Theodoratou et al., 2014). Since deficiency in vitamin D can be treated, vitamin D may have an important public health inference in the prevention of age-related neurodegenerative diseases such as stroke, especially in this part of the world, China.
Recent reports on the association between vitamin D and its risk on stroke have been inconclusive. A report showed that insufficient levels of vitamin D increases the risk of stroke (Zhou R. et al., 2018) while some reports showed no effect of low levels vitamin D as a risk factor of stroke (Perna et al., 2013; Skaaby et al., 2014). Nonetheless, it has been reported that 78% of patients with ischemic stroke have vitamin D deficiency in China (Si et al., 2019). Due to the inconsistent reports, we aimed to assess the association of vitamin D deficiency with ischemic stroke in a Chinese population (Han race). We also aimed to analyze the risk factors of vitamin D deficiency in stroke patients using different models.
Materials and Methods
Demographics
This study was conducted at The First Affiliated Hospital of Wenzhou Medical University. Patients were enrolled from a retrospective database which included sequential patients who were admitted and diagnosed at the Neurology Department. Patients were enrolled within 24 h after ischemic stroke between 2017 and 2020. The ethics of committee of The First Affiliated Hospital of Wenzhou Medical University approved of the study and it followed the declaration of Helsinki. All participants provided informed written consent.
All patients underwent cerebral computed tomography (CT) or magnetic resonance imaging (MRI) to confirm the diagnosis ischemic stroke within 24 h of admission. The exclusion criteria were the following: 1. Confirmed diagnosis of transient ischemic attack (TIA); 2. Had preventive antibacterial treatment; 3. Had an infection 2 – 3 weeks before admission; 4. History of neurodegenerative disease such as Alzheimer’s disease, Parkinson’s disease, cerebral hemorrhage, and brain trauma; 5. Incomplete medical information; 6. Severe hepatic disease; 7. Severe renal disease; and 8. Patient was on vitamin D supplement before occurrence of ischemic stroke or has osteoporosis.
Assessing the Concentration of Vitamin D
Concentration levels of vitamin D was done using an competitive electrochemiluminescence protein binding assay (COBAS Roche Diagnostic GmbH, Germany) as previously reported (Huang et al., 2019). Blood samples were taken within 24 h of admission. Patients were vitamin D levels less than 50 nmol/L were described as being vitamin D deficient (Park et al., 2015; Zainel et al., 2019).
Other Clinical Characteristics and Laboratory Parameters
All patients’ demographics and clinical information were collected and recorded. Clinical information such as history of hypertension, diabetes, systolic (SBP) and diastolic (DBP) blood pressures were collected; classification of stroke was done according to TOAST criteria (Arsava et al., 2017). Other clinical parameters included blood routine examination to assess apolipoprotein A-I (ApoA-I), apolipoprotein B (ApoB), ApoA-I/ApoB, cholesterol (CH), fibrinogen (FIB), fasting blood glucose (Glu), high-density lipoprotein (HDL), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG). Severity of stroke was assessed using National Institute of Health Stroke Scale (NIHSS) score (Kwah and Diong, 2014) within 24 h of admission.
Statistical Analyses
All statistical analyses were performed using SPSS software version 22, SPSS Inc., Chicago, IL, United States. Descriptive analyses were used to compare participant characteristics across the categories of vitamin D. Vitamin D categories were classified using the following as previously reported: sufficient was defined as vitamin D greater than or equal to 75 nmol/L; insufficiency was defined as vitamin D greater or equal to 50 and less than 75 nmol/L; deficiency was defined as vitamin D less than 50 nmol/L. Continuous variables were described by mean (standard deviations), and frequencies and percentages were used to describe categorical variables. Statistical analyses among the three groups were done with one-way analysis of variance (ANOVA) or Kruskal–Wallis in continuous variables. Pearson’s chi-square or Fisher’s exact tests were used where appropriate. The clinical characteristics and laboratory parameters associated to the NIHSS was confirmed by univariate and multivariate linear regression analysis (the factors which showed P < 0.05 were used to create a multivariate model) and univariate logistic regression was used to predict risk factors for vitamin D deficiency in stroke patients. The significant factors for the univariate analysis were further selected for further multiple logistic regression models to predict the occurrence of vitamin D deficiency. Furthermore, all patients were divided to two group depending on gender and FIB level (Low FIB < 3.18, high FIB ≥ 3.18) (Zhou X. et al., 2018). Univariate analysis was used to analyze the association between the significant risk factors and vitamin D deficiency, and the multiple logistic regression was further used to adjust for potential confounding or risk factors. P-values less than 0.05 were considered statistically significant.
Results
Baseline Characteristics of the Patients Base on the Vitamin D Level
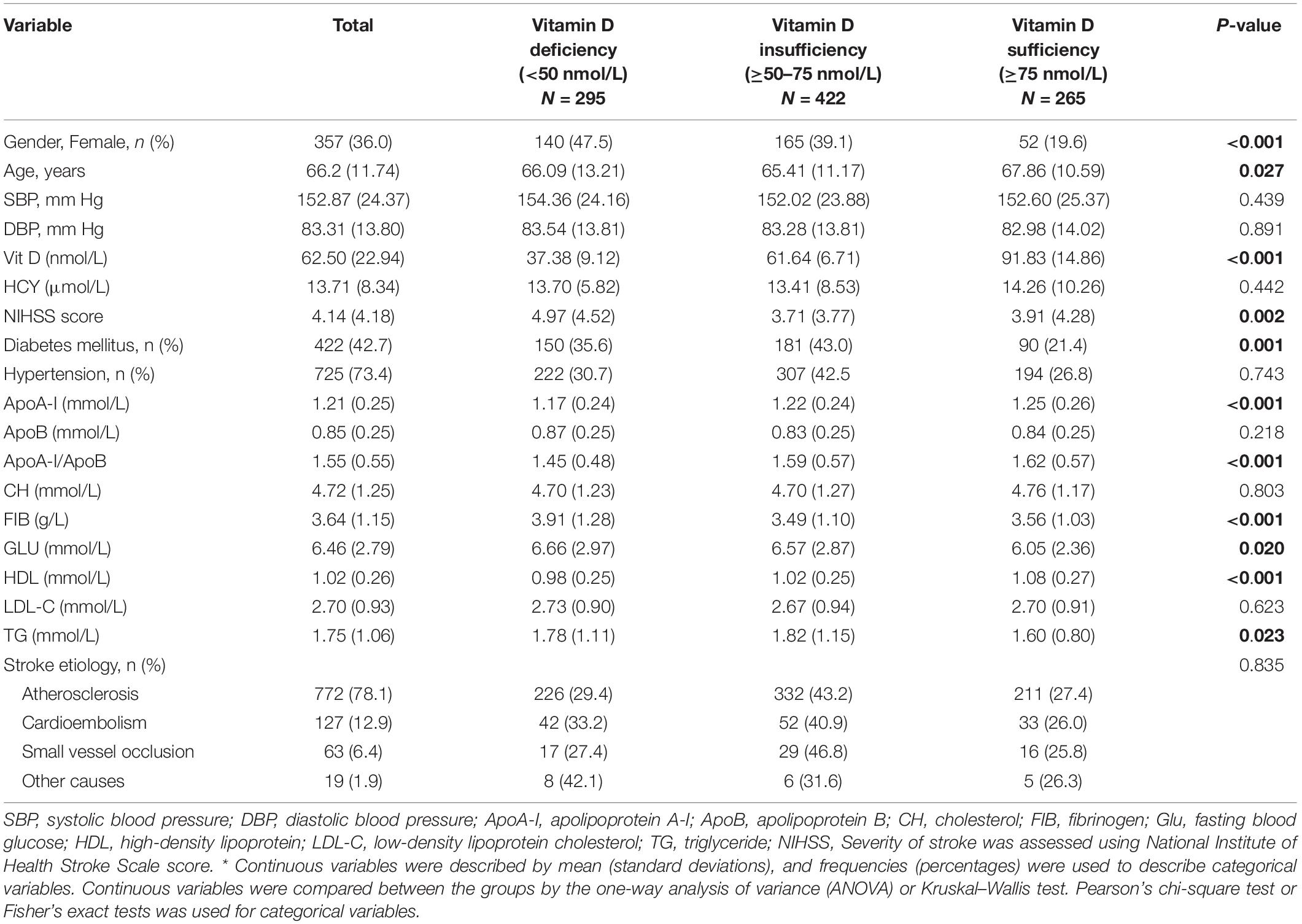
In this study, we enrolled a total of 982 ischemic stroke patients from the Neurology Department of The First Affiliated Hospital of Wenzhou Medical University between 2017 and 2020 [629 males (63.3%), 357 female (36.0%); mean age was 66.2 ± 11.7 years; Table 1]. Based on the vitamin D level, 295 patients were grouped as vitamin D deficiency (vitamin D level = 37.38 ± 9.12 nmol/L; Table 1), 422 patients were vitamin D insufficiency (vitamin D level = 61.64 ± 6.71 nmol/L; Table 1) and 265 patients were vitamin D sufficiency (vitamin D level = 91.83 ± 14.86 nmol/L; Table 1). The percentage of patients with vitamin D deficiency was 295 (30.0%); 155 (15.8%) males, and 140 (14.3%) females were vitamin D deficient. The clinical information and differences among the three groups using the vitamin D levels are shown in Table 1.
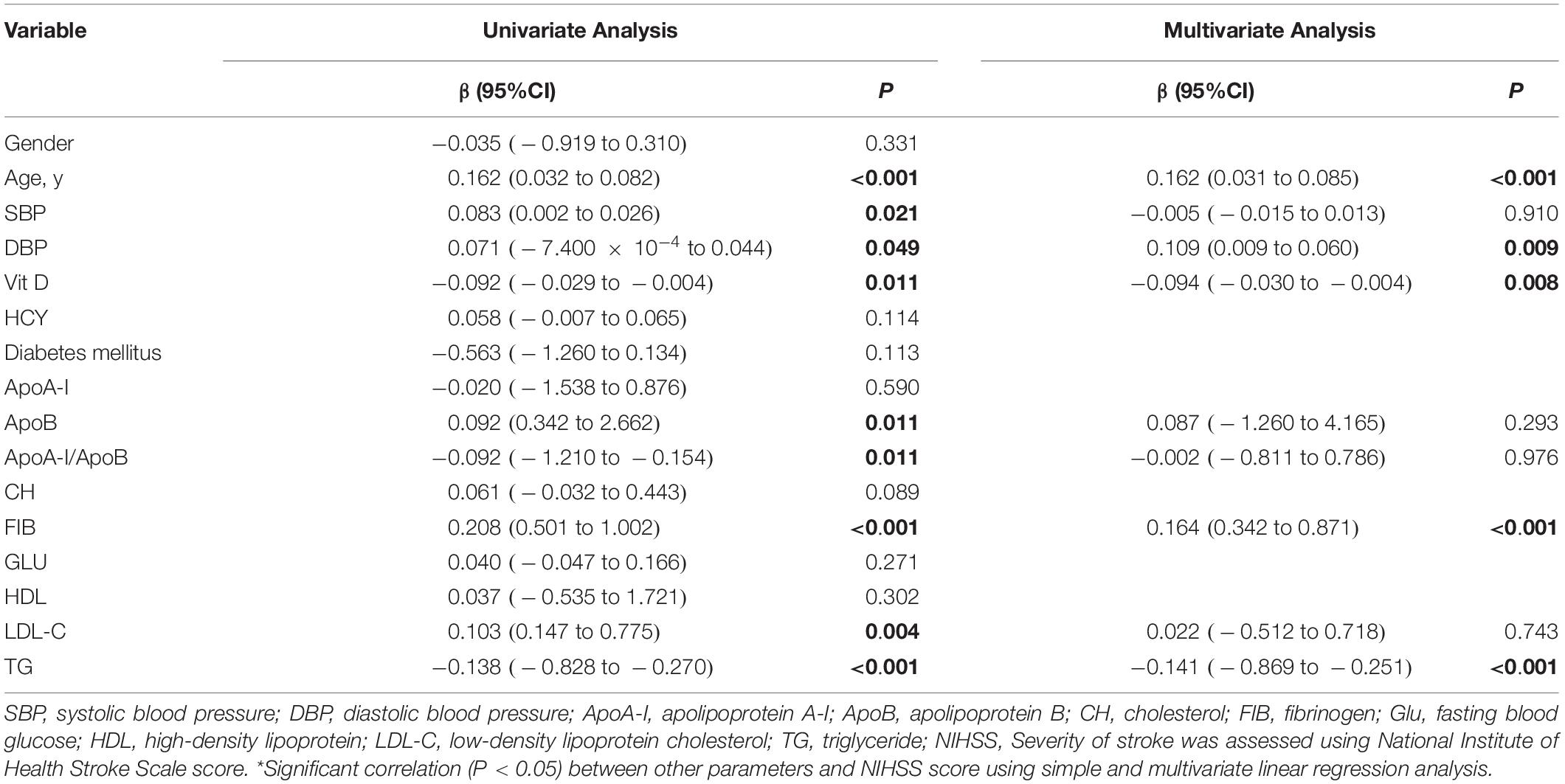
The Risk Factors Associated With NIHSS in All Stroke Patients
In a univariate linear regression analysis, age, SBP, DBP, vitamin D, ApoB, ApoA-I/ApoB, FIB LDL-C, and TG were significantly associated to NIHSS (P < 0.001 ∼ 0.049; Table 2), respectively. Parameters with significant associations were then put into a multivariate linear regression model; age, DBP, vitamin D, FIB, and TG showed significant association with NIHSS (P < 0.001 ∼ 0.009; Table 2), respectively.
The Risk Factors of Vitamin D Deficiency in All Patients
In a univariate binary logistic regression analysis, female, NIHSS, diabetes mellitus, and FIB were risk factors of vitamin D deficiency in all patients (OR = 1.066 ∼ 1.584, P ≤ 0.001; Table 3), while the ApoA-I, ApoA-I/ApoB and HDL were protective factors (OR = 0.331 ∼ 0.569, P < 0.001; Table 3). In a multivariate logistic regression model analysis, female (OR = 2.422, P < 0.001; Table 3), NIHSS (OR = 1.005, P = 0.008; Table 3) and FIB (OR = 1.256, P = 0.005; Table 3) showed greater significant risk of predicting vitamin D deficiency in stroke patients.
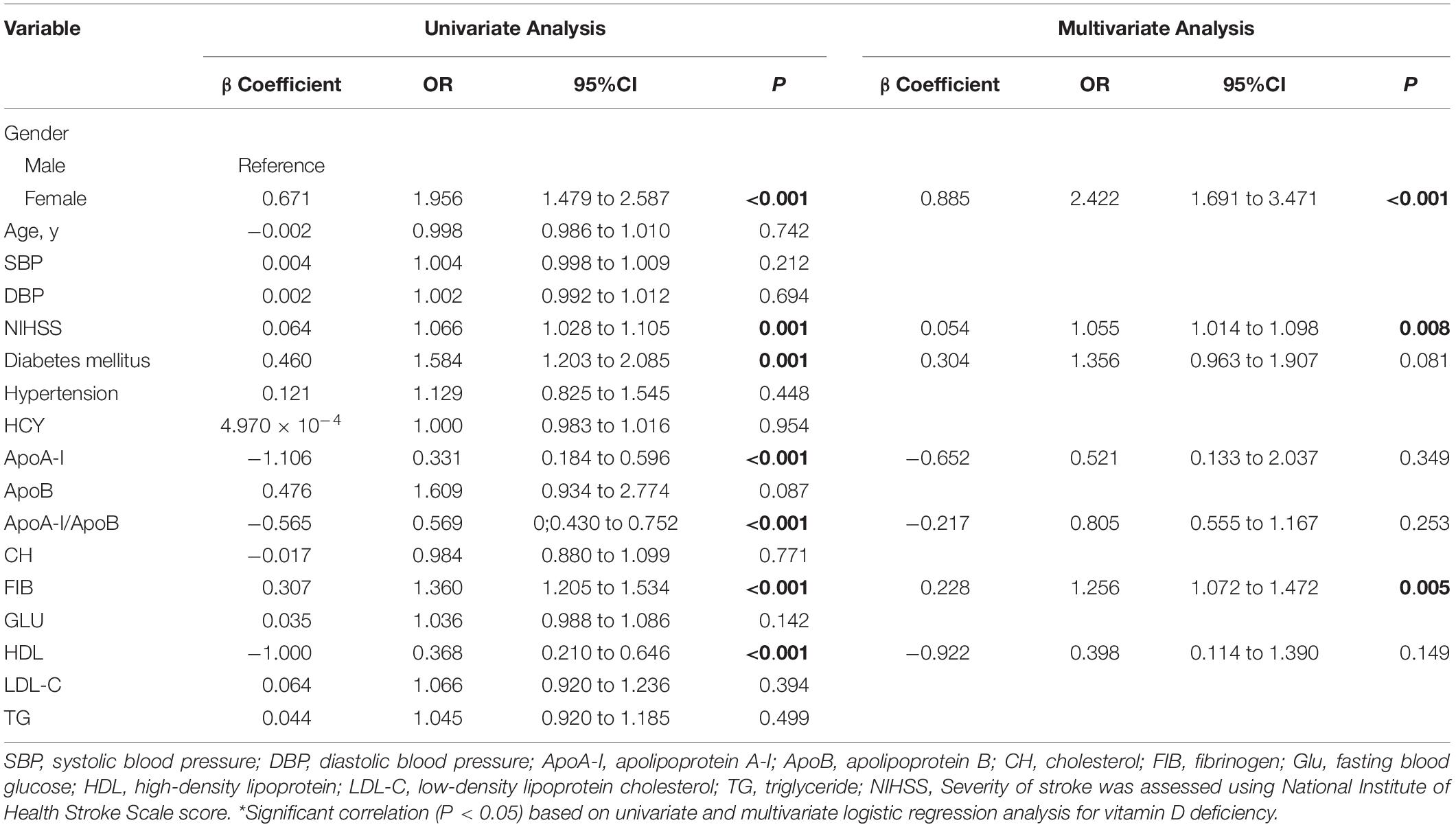
Table 3. Univariate and multivariate logistic regression analysis for vitamin D deficiency occurrence in all patients.
The Risk Factors of Vitamin D Deficiency in Female Group and Male Group
Table 4 shows the risk factors which were inclined to vitamin D deficiency in different gender groups. In a univariate logistic regression analysis, FIB significantly associated with vitamin D deficiency in both gender (female: OR = 1.476, P = 0.001; male: OR = 1.328, P < 0.001; Table 4). NIHSS was associated with vitamin D in male (OR = 1.087, P = 0.002; Table 4), and significant difference still remained after adjusting for risk factors.
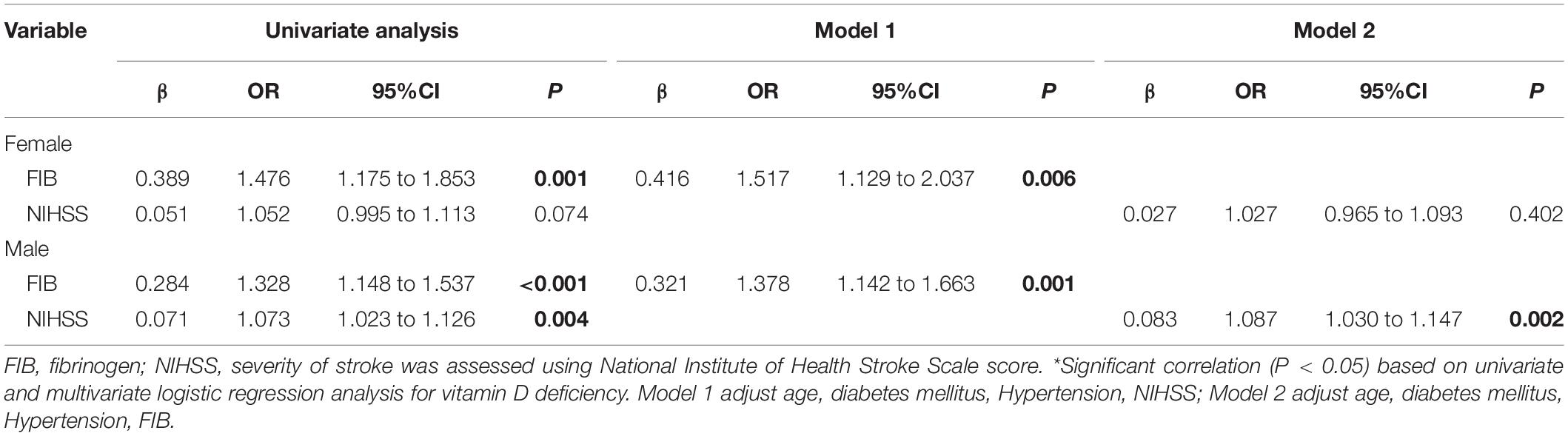
Table 4. Univariate and multivariate logistic regression analysis for vitamin D deficiency occurrence in gender groups.
The Risk Factors of Vitamin D Deficiency in Different FIB Level
In a univariate logistic regression, female showed significant risk implications in both FIB level (lower FIB: OR = 2.124, P = 0.003; higher FIB: OR = 1.722, P = 0.002; Table 5), while increasing NIHSS was a risk factor in higher FIB level (OR = 1.067, P = 0.003; Table 5). After adjusting for risk factors, Female (lower FIB: OR = 2.075, P = 0.015; higher FIB: OR = 1.807, P = 0.004; Table 5), NIHSS (higher FIB: OR = 1.078, P = 0.001; Table 5) showed the same results aforementioned in different FIB level.
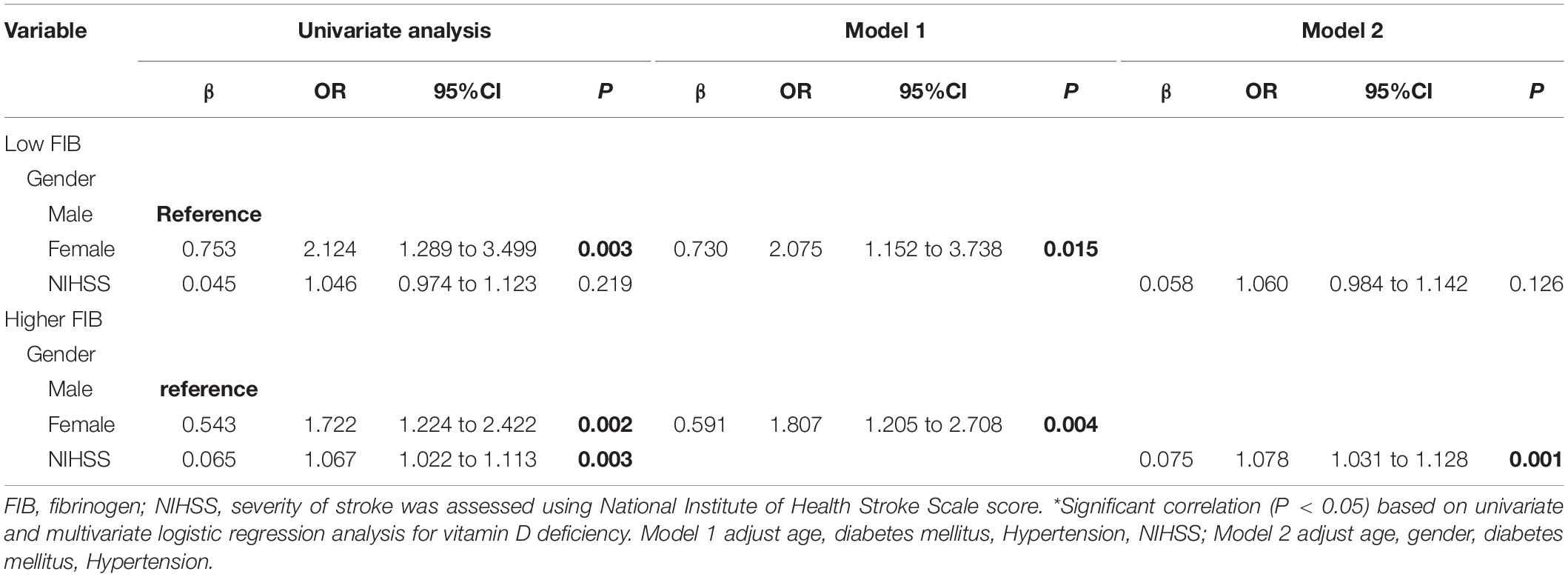
Table 5. Univariate and multivariate logistic regression analysis for vitamin D deficiency occurrence in different FIB levels.
Discussion
Our current study showed that deficiency of vitamin D is associated with severity of stroke using NHISS in our Chinese ischemic stroke patients. We also showed that the risk factors of vitamin D deficiency in stroke patients were the female gender, severity of stroke using NHISS and FIB.
Our results showed an association between vitamin D deficiency and severity of incident stroke suggesting that low levels of serum vitamin D may be a consequence of stroke. It has been reported that low vitamin D principally may be associated with both non-fatal and terminal stroke (Tu et al., 2014). Our current report is congruent with previous reports which showed that vitamin D deficiency is associated with the severity of ischemic stroke (Tu et al., 2014; Li et al., 2018). Reports on the association between vitamin D and stroke have been varying due to several explanations (Skaaby et al., 2014; Zhou R. et al., 2018). To start with, most studies used different cut-off values of serum 25(OH) D in their analyses and this may have swayed their findings. A study used below 45 nmol/L which did not yield a substantial relationship while another study used less than 35 nmol/L which led to significant results (Schneider et al., 2015). Our current study used less than 50 nmol/L as deficient vitamin D and found a significant association with the severity of incident stroke. Although the cutoff values for deficiency in vitamin D used in previous reports vary, our current report suggests less than 50 nmol/L used in the Chinese population may be of significance in the clinical field and a sufficient level of 75 nmol/L may be ideal for health benefits which is congruent with a previous report (Holick et al., 2011).
Vitamin D has been reported to stimulate dilation of vessels, reduce arterial pressure and recuperate blood flow post stroke to neurons by increasing the effect of nitric oxide synthase (NOS) (Yalbuzdag et al., 2015; Nie et al., 2017). Low and deficient levels of vitamin D has been reported to lead to vascular stiffness (Suthar et al., 2018). Moreover, deficient levels of vitamin D leads to narrower and stiffer vessels which increases the risk occlusion; besides, deficient levels of vitamin D in patients with ischemic stroke has been reported to be a risk factor for deep venous thrombosis (Wu and He, 2018). Furthermore, very low levels of vitamin D in ischemic stroke patients has been reported to be associated with severe white matter microstructural damage and cerebral small-vessel disease burden seen on MRI (Feng et al., 2019). As such, the association between deficiency of vitamin D and severity of stroke seen in our patients indicates that the lower the vitamin D levels the more severe the ischemic stroke patient is. Our report urges clinicians to pay close attention to the levels of vitamin D in patients with ischemic stroke to reduce worsen patient’s condition.
Several reports have shown on the gender association between vitamin D deficiency and stroke (Sun et al., 2012; Hu et al., 2019). A previous Swedish study showed that females with less than 50 nmol/L had a higher risk for stroke and morbidity (Leu Agelii et al., 2017). Another study also showed that females with less than 50 nmol/L of serum vitamin D had a moderate risk increase for stroke (Sun et al., 2012). On the other hand, a report found that deficiency in vitamin D increased the risk for stroke in males (Bajaj et al., 2014). A Japanese study also showed that males with vitamin D deficiency had a slight increase in the risk for stroke (Kojima et al., 2012, 2014). Our current study showed that vitamin D deficiency as risk factor in females was severe than that in males which is congruent with previous stroke reports done on middle-aged stroke patients (Kojima et al., 2012; Leu Agelii et al., 2017); however, the reason(s) behind this is still vague. A review reported that males are at a greater risk of stroke and vascular diseases when compared to females; the authors suggested that this may be due to the impact of androgens and estrogens (Abi-Ghanem et al., 2020) in the body. Another research showed that females had a lower risk of stroke incidence in 45–74 years old when compared to the male gender (Jiang et al., 2020). Our report suggests that the risk of vitamin D deficiency in ischemic stroke patients is more significant in the female gender. Further studies with longitudinal reports are needed to elucidate this.
It has been reported that ischemic stroke triggers an acute phase response in the vascular system resulting in an increase of circulating inflammatory markers (Aleva et al., 2020). The initiation of tissue injury in the cerebral vessels triggers inflammatory response which triggers upregulation of hepatic fibrinogen and recruits coagulation cascade. High concentrations of fibrinogen in acute stroke patients have been reported to be a response to brain damage and the underlying vessel wall disease (Rothwell et al., 2004; Di Napoli and Singh, 2009). Our current study showed that high serum fibrinogen in acute ischemic stroke patients is a risk factor for vitamin D deficiency. We also suggest that high concentration of fibrinogen (which translates as increase in the activation of platelets) may be a risk factor for low serum concentrations of vitamin D less than 50 nmol/L in ischemic stroke patients. To the best of our knowledge, this is the first study to report on high concentration of fibrinogen being a risk factor for vitamin D deficiency in ischemic stroke; besides, it has been reported that high levels of FIB will increase plasma viscosity, which may lead to low cerebral blood flow and impaired perfusion ultimately leading to a higher severity of stroke (Rasyid et al., 2019; Tao et al., 2020). This may explain why NIHSS is more sensitive to the vitamin D deficiency group with high FIB level. Further reports are needed to validate our results and speculations.
Our results should be interpreted with caution given the cross-sectional observational design. A longitudinal study is also needed to validate our hypotheses as well. Another limitation is our study is that our patients were only Chinese patients from the Han ethnicity and majority of our stroke patients were of atherosclerotic etiology, thus, limiting its generalizability to other populations of different ethnic groups. Our study could not perform repeated vitamin D measurement over periods of time to assess the stability of vitamin D. Even so, the measurement of only one vitamin D metabolite. Moreover, studies (Brot et al., 2001) have shown that exposure of sun is an important determinant of 25(OH) D levels; nonetheless, we did not assess the duration and region of sun exposure levels for each participant. Dietary intake (Clements et al., 1987) is another crucial factor that affects vitamin D status; unfortunately, we did not assess and record the dietary intake of each participant.
Although deficient levels of vitamin D are risk factor for ischemic stroke and our current report showed that deficiency of vitamin D is associated with severity of stroke using NHISS. Our results also showed that the risk factors of vitamin D deficiency in stroke patients are the female gender, severity of stroke using NHISS and FIB in all incident stroke patients. Although supplementation of vitamin D has been reported to reduce ischemic stroke and its outcome, reports on this is inconclusive. However, our study urges clinicians to pay close attention to the levels of vitamin D in patients with ischemic stroke.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of The First Affiliated Hospital of Wenzhou Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
HM contributed to conception, data curation, formal analysis, and writing original draft. HZ contributed to the data curation, formal analysis. XL and GH contributed to the data curation. MC contributed to conceptualization and project administration. ZY contributed to funding acquisition, resources, and writing-review and editing. ZW contributed to conceptualization, resources, and writing-review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Traditional Chinese Medicine Administration National Traditional Chinese Medicine Experts Inheritance Studio Construction Project [Ministry of Medicine in China, No. (2019)41] and the Projects of Science and Technology Bureau of Taizhou (No. 1902ky172).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the study participants and the clinical staff at all participating hospitals for their support and contribution to this project.
References
Abi-Ghanem, C., Robison, L. S., and Zuloaga, K. L. (2020). Androgens’ effects on cerebrovascular function in health and disease. Biol. Sex. Differ. 11:35.
Aleva, F. E., Tunjungputri, R. N., van der Vorm, L. N., Li, Y., Heijdra, Y. F., Oosting, M., et al. (2020). Platelet integrin alphaiibbeta3 activation is associated with 25-Hydroxyvitamin D concentrations in healthy adults. Thromb. Haemost. 120, 768–775. doi: 10.1055/s-0040-1709523
Arsava, E. M., Helenius, J., Avery, R., Sorgun, M. H., Kim, G. M., Pontes-Neto, O. M., et al. (2017). Assessment of the predictive validity of etiologic stroke classification. JAMA Neurol. 74, 419–426. doi: 10.1001/jamaneurol.2016.5815
Bajaj, A., Stone, K. L., Peters, K., Parimi, N., Barrett-Connor, E., Bauer, D., et al. (2014). Circulating vitamin D, supplement use, and cardiovascular disease risk: the MrOS Sleep Study. J. Clin. Endocrinol. Metab. 99, 3256–3262. doi: 10.1210/jc.2013-4178
Berghout, B. P., Fani, L., Heshmatollah, A., Koudstaal, P., Ikram, M. A., Zillikens, M. C., et al. (2019). Vitamin D status and risk of stroke: the rotterdam study. Stroke 50, 2293–2298. doi: 10.1161/strokeaha.119.025449
Brot, C., Vestergaard, P., Kolthoff, N., Gram, J., Hermann, A. P., and Sorensen, O. H. (2001). Vitamin D status and its adequacy in healthy Danish perimenopausal women: relationships to dietary intake, sun exposure and serum parathyroid hormone. Br. J. Nutr. 86(Suppl. 1), S97–S103.
Clements, M. R., Johnson, L., and Fraser, D. R. (1987). A new mechanism for induced vitamin D deficiency in calcium deprivation. Nature 325, 62–65. doi: 10.1038/325062a0
Di Napoli, M., and Singh, P. (2009). Is plasma fibrinogen useful in evaluating ischemic stroke patients: why, how, and when. Stroke 40, 1549–1552. doi: 10.1161/strokeaha.108.537084
Feigin, V. L., Roth, G. A., Naghavi, M., Parmar, P., Krishnamurthi, R., Chugh, S., et al. (2016). Global burden of stroke and risk factors in 188 countries, during 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol. 15, 913–924. doi: 10.1016/s1474-4422(16)30073-4
Feng, C., Tang, N., Huang, H., Zhang, G., Qi, X., and Shi, F. (2019). 25-Hydroxy vitamin D level is associated with total MRI burden of cerebral small vessel disease in ischemic stroke patients. Int. J. Neurosci. 129, 49–54. doi: 10.1080/00207454.2018.1503182
Holick, M. F., Binkley, N. C., Bischoff-Ferrari, H. A., Gordon, C. M., Hanley, D. A., Heaney, R. P., et al. (2011). Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 1911–1930. doi: 10.1210/jc.2011-0385
Hu, W., Liu, D., Li, Q., Wang, L., Tang, Q., and Wang, G. (2019). Decreasing serum 25-hydroxyvitamin D levels and risk of early neurological deterioration in patients with ischemic stroke. Brain Behav. 9:e01227. doi: 10.1002/brb3.1227
Huang, G. Q., Cheng, H. R., Wu, Y. M., Cheng, Q. Q., Wang, Y. M., Fu, J. L., et al. (2019). Reduced Vitamin D levels are associated with stroke-associated pneumonia in patients with acute ischemic stroke. Clin. Interv. Aging 14, 2305–2314. doi: 10.2147/cia.s230255
Jiang, M., Ma, C., Li, H., Shen, H., Li, X., Sun, Q., et al. (2020). Sex dimorphisms in ischemic stroke: from experimental studies to clinic. Front. Neurol. 11:504. doi: 10.3389/fneur.2020.00504
Kojima, G., Bell, C., Abbott, R. D., Launer, L., Chen, R., Motonaga, H., et al. (2012). Low dietary vitamin D predicts 34-year incident stroke: the honolulu heart program. Stroke 43, 2163–2167. doi: 10.1161/strokeaha.112.651752
Kojima, G., Bell, C. L., Chen, R., Ross, W., Abbott, R. D., Launer, L., et al. (2014). Low dietary vitamin D in mid-life predicts total mortality in men with hypertension: the honolulu heart program. J Am. Coll Nutr. 33, 129–135. doi: 10.1080/07315724.2013.875363
Kwah, L. K., and Diong, J. (2014). National institutes of health stroke scale (NIHSS). J. Physiother. 60:61. doi: 10.1016/j.jphys.2013.12.012
Leu Agelii, M., Lehtinen-Jacks, S., Zetterberg, H., Sundh, V., Bjorkelund, C., and Lissner, L. (2017). Low vitamin D status in relation to cardiovascular disease and mortality in Swedish women - Effect of extended follow-up. Nutr. Metab. Cardiovasc. Dis. 27, 1143–1151. doi: 10.1016/j.numecd.2017.10.013
Li, Y. Y., Wang, Y. S., Chen, Y., Hu, Y. H., Cui, W., Shi, X. Y., et al. (2018). Association of serum 25(OH) D levels with infarct volumes and stroke severity in acute ischemic stroke. J. Nutr. Health Aging 22, 97–102. doi: 10.1007/s12603-017-0926-z
Nie, Z., Ji, X. C., Wang, J., and Zhang, H. X. (2017). Serum levels of 25-hydroxyvitamin D predicts infarct volume and mortality in ischemic stroke patients. J. Neuroimmunol. 313, 41–45. doi: 10.1016/j.jneuroim.2017.10.002
Park, K. Y., Chung, P. W., Kim, Y. B., Moon, H. S., Suh, B. C., Won, Y. S., et al. (2015). Serum Vitamin D status as a predictor of prognosis in patients with acute ischemic stroke. Cerebrovasc. Dis. 40, 73–80. doi: 10.1159/000434691
Perna, L., Schottker, B., Holleczek, B., and Brenner, H. (2013). Serum 25-hydroxyvitamin D and incidence of fatal and nonfatal cardiovascular events: a prospective study with repeated measurements. J. Clin. Endocrinol. Metab. 98, 4908–4915. doi: 10.1210/jc.2013-2424
Rasyid, A., Harris, S., Kurniawan, M., Mesiano, T., and Hidayat, R. (2019). Fibrinogen and LDL influence on blood viscosity and outcome of acute ischemic stroke patients in indonesia. Ann. Neurosci. 26, 30–34. doi: 10.1177/0972753119900630
Rothwell, P. M., Howard, S. C., Power, D. A., Gutnikov, S. A., Algra, A., Gijn, J., et al. (2004). Fibrinogen concentration and risk of ischemic stroke and acute coronary events in 5113 patients with transient ischemic attack and minor ischemic stroke. Stroke 35, 2300–2305. doi: 10.1161/01.str.0000141701.36371.d1
Schneider, A. L., Lutsey, P. L., Selvin, E., Mosley, T. H., Mosley, T. H., Sharrett, A. R., et al. (2015). Vitamin D, vitamin D binding protein gene polymorphisms, race and risk of incident stroke: the atherosclerosis risk in communities (ARIC) study. Eur. J. Neurol. 22, 1220–1227. doi: 10.1111/ene.12731
Si, J., Li, K., Shan, P., and Yuan, J. (2019). The combined presence of hypertension and vitamin D deficiency increased the probability of the occurrence of small vessel disease in China. BMC Neurol. 19:164. doi: 10.1186/s12883-019-1395-2
Skaaby, T., Husemoen, L. L., Borglykke, A., Jørgensen, T., Thuesen, B. H., Pisinger, C., et al. (2014). Vitamin D status, liver enzymes, and incident liver disease and mortality: a general population study. Endocrine 47, 213–220. doi: 10.1007/s12020-013-0107-8
Sun, Q., Pan, A., Hu, F. B., Manson, J. E., and Rexrode, K. M. (2012). 25-Hydroxyvitamin D levels and the risk of stroke: a prospective study and meta-analysis. Stroke 43, 1470–1477. doi: 10.1161/strokeaha.111.636910
Suthar, O. P., Mathur, S., Gupta, V., Agarwal, H., Mathur, A., Singh, P., et al. (2018). Study of correlation of serum Vitamin D levels with arterial stiffness and cardiovascular morbidity in elderly individuals of western rajasthan. J. Assoc. Physicians. India 66, 18–21.
Tao, L., ShiChuan, W., DeTai, Z., and Lihua, H. (2020). Evaluation of lipoprotein-associated phospholipase A2, serum amyloid A, and fibrinogen as diagnostic biomarkers for patients with acute cerebral infarction. J. Clin. Lab Anal. 34:e23084.
Theodoratou, E., Tzoulaki, I., Zgaga, L., and Ioannidis, J. P. (2014). Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ 348:g2035. doi: 10.1136/bmj.g2035
Tu, W. J., Zhao, S. J., Xu, D. J., and Chen, H. (2014). Serum 25-hydroxyvitamin D predicts the short-term outcomes of Chinese patients with acute ischaemic stroke. Clin. Sci. 126, 339–346. doi: 10.1042/cs20130284
Wu, W. X., and He, D. R. (2018). Low Vitamin D levels are associated with the development of deep venous thromboembolic events in patients with ischemic stroke. Clin. Appl. Thromb. Hemost. 24, 69S–75S.
Yalbuzdag, S. A., Sarifakioglu, B., Afsar, S. I., Celik, C., Can, A., Yegin, T., et al. (2015). Is 25(OH)D associated with cognitive impairment and functional improvement in stroke? a retrospective clinical study. J. Stroke Cerebrovasc. Dis. 24, 1479–1486. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.007
Yang, G., Wang, Y., Zeng, Y., Gao, G. F., Liang, X., Zhou, M., et al. (2013). Rapid health transition in China, 1990-2010: findings from the global burden of disease study 2010. Lancet 381, 1987–2015. doi: 10.1016/s0140-6736(13)61097-1
Zainel, A. A. L., Qotba, H., Al Nuaimi, A., and Syed, M. (2019). Vitamin D status among adults (18-65 years old) attending primary healthcare centres in Qatar: a cross-sectional analysis of the Electronic Medical Records for the year 2017. BMJ Open 9:e029334. doi: 10.1136/bmjopen-2019-029334
Zhou, M., Wang, H., Zeng, X., Yin, P., Zhu, J., Chen, W., et al. (2019). Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet 394, 1145–1158. doi: 10.1016/s0140-6736(19)30427-1
Zhou, R., Wang, M., Huang, H., Li, W., Hu, Y., and Wu, T. (2018). Lower Vitamin D status is associated with an increased risk of ischemic stroke: a systematic review and meta-analysis. Nutrients 10:277. doi: 10.3390/nu10030277
Keywords: ischemic stroke, vitamin D, fibrinogen, National Institute of Health Stroke Scale score, Chinese
Citation: Miao H, Zhu H, Luan X, Huang G, Chen M, Yuan Z and Wang Z (2021) Risk Factors of Vitamin D Deficiency in Chinese Ischemic Stroke Patients: A Cross-Sectional Study. Front. Aging Neurosci. 12:613498. doi: 10.3389/fnagi.2020.613498
Received: 02 October 2020; Accepted: 21 December 2020;
Published: 18 January 2021.
Edited by:
Aurel Popa-Wagner, University Hospital Essen, GermanyReviewed by:
Ricki Colman, University of Wisconsin-Madison, United StatesMauro Silvestrini, Marche Polytechnic University, Italy
Copyright © 2021 Miao, Zhu, Luan, Huang, Chen, Yuan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhen Wang, d2FuZ3poZW5Ad3pob3NwaXRhbC5jbg==; Zhengzhong Yuan, d3p5enoyMDA4QDEyNi5jb20=; Meixia Chen, Y214Nzc4MUAxMjYuY29t
†These authors have contributed equally to this work
 Hanpei Miao
Hanpei Miao Hanyu Zhu2†
Hanyu Zhu2† Zhengzhong Yuan
Zhengzhong Yuan Zhen Wang
Zhen Wang