- 1College of Veterinary Medicine, Qingdao Agricultural University, Qingdao, China
- 2Qingdao Center for Animal Disease Control and Prevention, Qingdao, China
- 3Laizhou Zhenzhu Station for Animal Husbandry and Veterinary Medicine, Yantai, China
Introduction
Rabies is a zoonotic viral disease that causes encephalitis in humans and other mammals, such as dogs, bats, raccoons, and foxes (1). This disease generally includes two clinical forms, namely furious rabies and paralytic rabies (2). The former is characterized by hyperactivity and hallucinations; the latter is characterized by paralysis and coma. Rabies induces progressive and fatal inflammation of the brain and spinal cord. Once its clinical sign begins, the mortality rate is virtually 100% in humans. Rabies is still a serious public problem in over 150 countries and territories, mainly in Asia and Africa (3).
The etiological agent of rabies is rabies virus (RV), a typical neurotropic virus. Its transmission is commonly through saliva, bites, scratches, or direct contact with mucosa (4). According to the latest taxonomic classification, RV has been renamed lyssavirus rabies, classified into the genus Lyssavirus in the family Rhabdoviridae. The virion is a bullet-shaped particle with envelope, containing a single-stranded, negative-sense RNA genome, ~11.9 nt in length, encoding five proteins in order: nucleoprotein (N), phosphoprotein (P), matrix protein (M), glycoprotein (G), and RNA-dependent RNA polymerase (RdRp or L protein).
The RV genome can be readily modified to accommodate a foreign antigen sequence for rescuing a recombinant virus using revere genetics (5). The recombinant, if demonstrated to be able to induce specific immune responses in vivo, would play a potential role in developing the RV-vectored vaccine. To date, there have been three types of RV-vectored vaccines: live-attenuated, inactivated and replication-deficient patterns. They showed their individual strengths and weaknesses, both of which were critically discussed here.
Reverse genetics for recovery of antigen-expressing RV
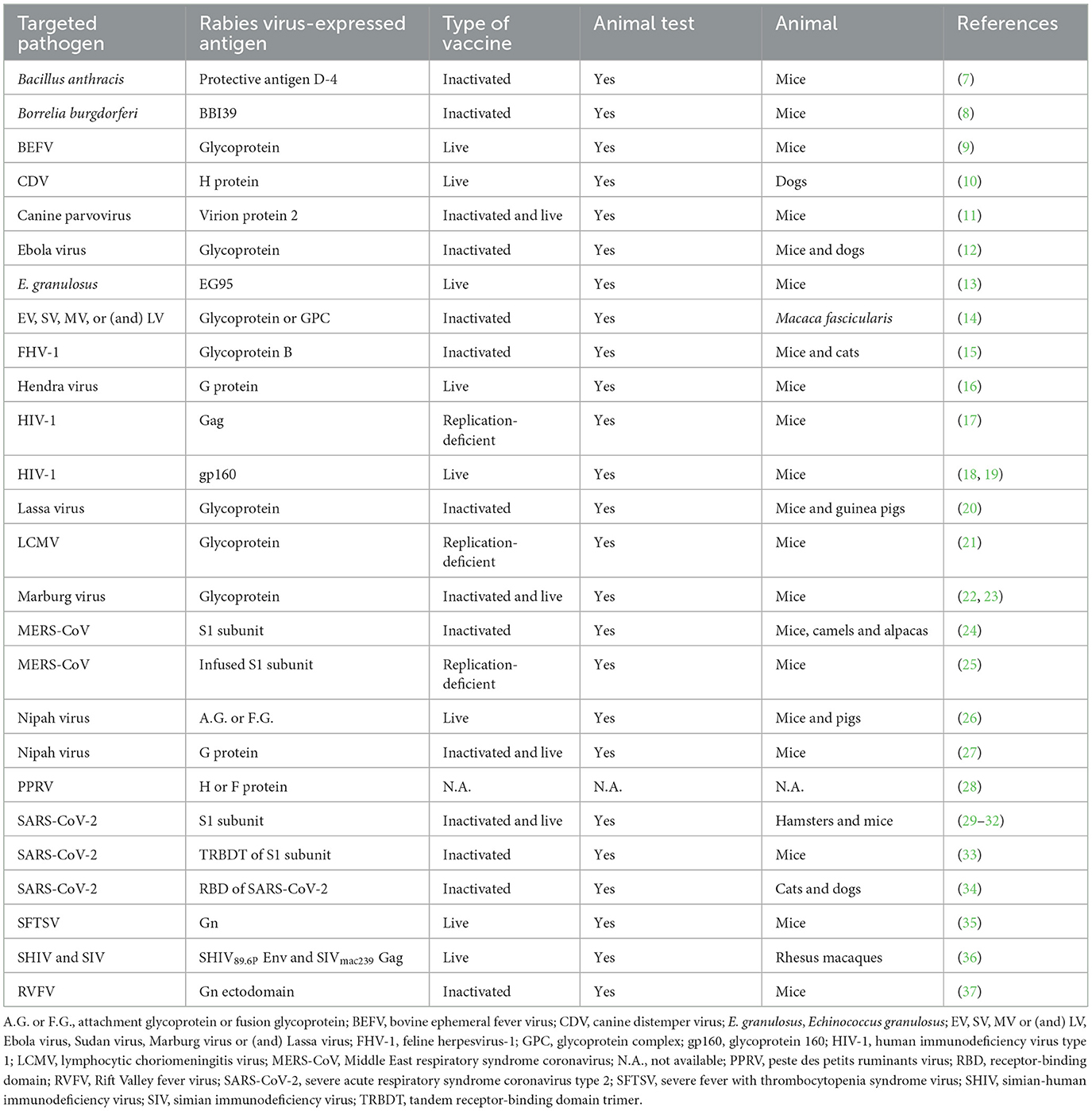
The reverse genetics platform of RV was initially reported in 1994 (6), subsequently revolutionizing the researches on RV and even on other RNA viruses. This reverse genetics platform includes four plasmids, and one cell line. The four-plasmid system contains one viral cDNA clone, and three helper plasmids that separately express N, P and L proteins. An RV-vectored cDNA clone generally possesses an extra transcriptional unit of foreign antigen. Recovery of RV involves co-transfection of these four plasmids into a cell line [for a review on the protocol, see (5)]. The rescued chimeric RV will be characterized for verifying its ability in the expression of foreign antigen in vitro, and then subjected to the animal test for unveiling its potential in eliciting specific immune responses. Table 1 exhibits a range of RV-vectored candidate vaccines against distinct pathogens.
Live-attenuated RV-vectored vaccine
The requirements for developing live-attenuated RV-vectored vaccines (LRVs) include many basic features: no or low virulence in hosts, ability of reaching high-level titers via cell culture, continuously eliciting cellular and humoral immune responses, thermal stability, and last but not least, genetic stability of foreign sequence. LRVs are factually the replication-competent RVs, able to replicate continuously in animals. They usually require fewer doses, and moreover provide more long-lasting protection than inactivated vaccines. A single-dose vaccination schedule is enough to induce high titers of specific antibodies in vivo (27). Moreover, LRVs offer more comprehensive and long-lasting protection in animals from pathogens.
Besides the humoral immunity, the LRVs also induce cellular immunity, because viable RVs propagate in host's cells and express endogenous antigens for further processing and presentation. The cell-mediated immune response is crucial for eliminating pathogens inside the host's cells. Zheng et al. (9) evaluated T-cell-mediated immune responses in mice elicited by an LRV that expressed the glycoprotein of bovine ephemeral fever virus (BEFV). Both RV- and BEFV-specific cytokines, interferon-γ and interleukin-4, could be identified to secrete in lymphocytes. This LRV induced more robust T helper 1 (Th1) and Th2 cell-mediated immunities than the parent RV via the single-dose immunization strategy (9). However, not all LRVs can induce the cellular immunity. McKenna et al. (36) previously demonstrated the immunogenicity of LRV expressing simian-human immunodeficiency virus (SHIV)89.6P Env in rhesus macaques. Humoral immunity against RV G protein and SHIV89.6P Env was detectable after the initial immunization, whereas the cell-mediated immune response was not identified against the SHIV antigens (36).
Although LRVs have been widely demonstrated to be powerful in eliciting protective immune responses in animals, there are still two weaknesses that should not be neglected for the development of LRVs. The first one is the potential risk in reversion to virulence. Most RNA viruses are genetically unstable during genomic replication, due to the low-fidelity characteristics of their RdRps (38). RVs have been rapidly evolving (39), and been even recombining with one another (40). A single mutation of amino acid in its G protein will quicken its spread, and even intensify its pathogenicity (41, 42). Therefore, the potential reversion to virulence hampers the further application of LRVs. The other weakness, albeit rarely reported as yet, should not also be neglected to design an LRV. This weakness is that a foreign sequence is possibly unstable in a chimeric RV genome, since the foreign sequence is theoretically uninvolved in virus-associated events. If a certain foreign sequence is deleted from a chimeric RV genome, the resultant RV would be still a replication-competent strain, but lose its own primary properties of vector vaccine.
Inactivated RV-vectored vaccine
The inactivated RV-vectored vaccine (IRV) is produced as a killed version of antigen-expressing RV. The prerequisite for developing a certain IRV is that a target antigen must be incorporated into the envelope of chimeric RV virion (43). Some viral glycoproteins, if expressed through the RV vector in cells, can be further processed, modified and finally transported to the cell surface. These viral glycoproteins, as membrane-spanning proteins, will be embedded into the cell envelope. Along with the viral budding, the foreign antigen can be incorporated into the envelope of RV virion. Many viral glycoproteins, like those of Lassa virus (20) and Ebola virus (12), were reported to have such a feature, therefore playing a potential role in the development of the IRVs.
However, not all viral glycoproteins can be directly used as a complete foreign antigen for preparing the IRV. Some ones need to be modified for the incorporation into RV virions. For instance, Rift Valley fever virus (RVFV) morphogenesis is by means of budding from the Golgi complex. In other words, the RVFV glycoprotein is unable to be transported to the cell membrane, therefore requiring the replacement of its trans-membrane domain and cytoplasmic tail with those of RV G protein for the incorporation of a fusion protein into the RV virion (37). Such a fusion modification was also reported to be used in non-viral proteins for preparing the IRV (7).
Compared with that of LRV, the most significant advantage of IRV is its good safety profile in animals, due to the recombinant RV functioning as an inactivated virion. Neither RV mutation nor virulence reversion can occur in IRV-inoculated animals. Although the recombinant RV is chemically inactivated, its immunogenicity can be even completely retained. The inactivated recombinant RV induces not only its own immune responses, but also more importantly, specific neutralizing antibodies against the target pathogen. One research group recently constructed an IRV, named CORAVAX™, against severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (32). A single dose of CORAVAX™ vaccine was demonstrated not only to elicit the high-level SARS-CoV-2-specific antibodies, but also to prevent weight loss, viral loads, lung inflammation, and cytokine storm in hamsters (29). Subsequently using the mouse models, this group further screened adjuvants for the maximum level of antibody titers, negated the concerns about pre-existing RV-vectored immunity, and determined its potential as a long-lasting IRV against SARS-CoV-2 (31). Extra experiments should be conducted to demonstrate whether the candidate vaccine CORAVAX™ is also effective in nonhuman primates.
Although the IRVs show a great potential in clinical use, there are still a few disadvantages to them. The most representative one is that they are generally less effective than their live counterparts. An LRV induces the immune response so robust that a single dose is enough to the immunization of animals, whereas an IRV commonly requires booster injections (23, 27). The immunity effect is involved in a dose-dependent manner for IRV-inoculated animals. The prime-boost immunization strategy is inconvenient, because at least two rounds of injection are needed. Another non-negligible issue is the potential risk of incomplete inactivation during IRV production. Such a risk can be excluded to the maximum extent through use of more reliable inactivants following a standard procedure of virulence inactivation.
Replication-deficient RV-vectored vaccine
Replication-deficient viruses are functionally defective in genome replication or (and) virion assembly (44). Construction of replication-deficient RV was reported as early as 1995 (45). A replication-deficient RV is a pseudo-live virion, which is able to infect a cell, but completes only one single-cycle replication, and more importantly cannot produce the replication-competent progenies. The replication-deficient RV-vectored vaccine (RRV) provides a new form of RV-vectored vaccine that combines many advantages of LRV and IRV, such as good safety and robust immunogenicity (Table 1).
It has been showed that the M gene-deleting RV confers 4-fold higher titers of neutralizing antibodies than does a commercially available vaccine in monkeys within 10 days after vaccination (46). The RV P protein is a multifunctional protein, required not only for RV replication, but also for innate immunity evasion (47). Takayama-Ito et al. (21) constructed a P gene-deficient RV that expressed the glycoprotein precursor of lymphocytic choriomeningitis virus (LCMV). Such a replication-deficient RV was subsequently proven to be a promising RRV candidate, characterized by dual immunities against LCMV and RV (21).
The G gene can be removed from a chimeric RV genome for the development of RRV. Gomme et al. (17) constructed a replication-deficient RV through deleting the G gene from an RV vector that expressed the HIV-1 Gag. This RRV was demonstrated to induce weaker RV-specific antibody responses, but equivalent HIV-1 Gag-specific CD8+ T cell responses. These responses could be considerably enhanced through boosting with the G gene-deleting RV complemented with one heterologous glycoprotein (17). Thus, the labor-consuming prime-boost strategy may be necessary for the RRV-based immunization. The G gene-deficient RV is also named single-cycle virus, which is still capable of budding from the cell membrane, but shows a 30-fold lower efficiency (48). The budded virions are able neither of attachment nor of entry into secondary host cells (49). Therefore, another drawback to RRVs is the difficulty in obtaining a high-titer viral stock through cell culture.
Conclusions
RV is an attractive candidate for designing and producing virus-vectored vaccines. This virus allows for foreign antigen expression, and even incorporation into the mature virions. A large number of reports, concerning LRVs, IRVs, and RRVs (Table 1), have highlighted their immune efficacies, antigen-delivering abilities, and safety profiles in animals. Nevertheless, a few issues should not be neglected regarding their production and application. Firstly, although the LRVs are functionally robust in eliciting both humoral and cellular immunities, all safety risks must be eliminated before they can be used. Secondly, manufacturers should pay attention to some accidents, caused by the incomplete inactivation of viruses. Last but not least, because the RV G protein is highly immunogenic in animals, the immune response to it may interfere with responses an RV-vectored vaccine confers to foreign proteins (43).
Author contributions
YL: Conceptualization, Writing – original draft. HZ: Conceptualization, Writing – original draft. QL: Formal analysis, Writing – original draft. XD: Funding acquisition, Writing – original draft. FL: Funding acquisition, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Qingdao Demonstration Project for People-benefit from Science and Techniques (Grant No.: 24-1-8-xdny-4-nsh).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Acharya KP, Chand R, Huettmann F, Ghimire TR. Rabies elimination: is it feasible without considering wildlife? J Trop Med. (2022) 2022:5942693. doi: 10.1155/2022/5942693
2. Hemachudha T, Ugolini G, Wacharapluesadee S, Sungkarat W, Shuangshoti S, Laothamatas J. Human rabies: neuropathogenesis, diagnosis, and management. Lancet Neurol. (2013) 12:498–513. doi: 10.1016/S1474-4422(13)70038-3
3. Taylor E, Del Rio Vilas V, Scott T, Coetzer A, Prada JM, Alireza G, et al. Rabies in the Middle East, Eastern Europe, Central Asia and North Africa: building evidence and delivering a regional approach to rabies elimination. J Infect Public Health. (2021) 14:787–94. doi: 10.1016/j.jiph.2021.02.009
4. Lewis T, Baack K, Gomez L, Nichols H, Lemmons C, Zeger W. Rabies post-exposure prophylaxis in the emergency department. Am J Emerg Med. (2024) 78:202–5. doi: 10.1016/j.ajem.2024.01.027
5. Osakada F, Callaway EM. Design and generation of recombinant rabies virus vectors. Nat Protoc. (2013) 8:1583–601. doi: 10.1038/nprot.2013.094
6. Schnell MJ, Mebatsion T, Conzelmann KK. Infectious rabies viruses from cloned cDNA. EMBO J. (1994) 13:4195–203. doi: 10.1002/j.1460-2075.1994.tb06739.x
7. Smith ME, Koser M, Xiao S, Siler C, McGettigan JP, Calkins C, et al. Rabies virus glycoprotein as a carrier for anthrax protective antigen. Virology. (2006) 353:344–56. doi: 10.1016/j.virol.2006.05.010
8. Rios S, Bhattachan B, Vavilikolanu K, Kitsou C, Pal U, Schnell MJ. The development of a rabies virus-vectored vaccine against Borrelia burgdorferi, targeting BBI39. Vaccines. (2024) 12:78. doi: 10.3390/vaccines12010078
9. Zheng W, Zhao Z, Tian L, Liu L, Xu T, Wang X, et al. Genetically modified rabies virus vector-based bovine ephemeral fever virus vaccine induces protective immune responses against BEFV and RABV in mice. Transbound Emerg Dis. (2021) 68:1353–62. doi: 10.1111/tbed.13796
10. Wang FX, Zhang SQ, Zhu HW, Yang Y, Sun N, Tan B, et al. Recombinant rabies virus expressing the H protein of canine distemper virus protects dogs from the lethal distemper challenge. Vet Microbiol. (2014) 174:362–71. doi: 10.1016/j.vetmic.2014.10.023
11. Luo J, Shi H, Tan Y, Niu X, Long T, Zhao J, et al. Two potential recombinant rabies vaccines expressing canine parvovirus virion protein 2 induce immunogenicity to canine parvovirus and rabies virus. Vaccine. (2016) 34:4392–8. doi: 10.1016/j.vaccine.2016.07.020
12. Shuai L, Wang X, Wen Z, Ge J, Wang J, Zhao D, et al. Genetically modified rabies virus-vectored Ebola virus disease vaccines are safe and induce efficacious immune responses in mice and dogs. Antiviral Res. (2017) 146:36–44. doi: 10.1016/j.antiviral.2017.08.011
13. Xu T, Liu L, Shi C, Liu W, Wang M, Tian L, et al. A recombinant rabies virus expressing Echinococcus granulosus EG95 induces protective immunity in mice. Transbound Emerg Dis. (2022) 69:e254–66. doi: 10.1111/tbed.14292
14. Kurup D, Fisher CR, Scher G, Yankowski C, Testa A, Keshwara R, et al. Tetravalent rabies-vectored filovirus and lassa fever vaccine induces long-term immunity in nonhuman primates. J Infect Dis. (2021) 224:995–1004. doi: 10.1093/infdis/jiab014
15. Jiao C, Liu D, Jin H, Huang P, Zhang H, Li Y, et al. Immunogenicity evaluation of a bivalent vaccine based on a recombinant rabies virus expressing gB protein of FHV-1 in mice and cats. Vet J. (2024) 304:106096. doi: 10.1016/j.tvjl.2024.106096
16. Kurup D, Wirblich C, Feldmann H, Marzi A, Schnell MJ. Rhabdovirus-based vaccine platforms against henipaviruses. J Virol. (2015) 89:144–54. doi: 10.1128/JVI.02308-14
17. Gomme EA, Faul EJ, Flomenberg P, McGettigan JP, Schnell MJ. Characterization of a single-cycle rabies virus-based vaccine vector. J Virol. (2010) 84:2820–31. doi: 10.1128/JVI.01870-09
18. Schnell MJ, Foley HD, Siler CA, McGettigan JP, Dietzschold B, Pomerantz RJ. Recombinant rabies virus as potential live-viral vaccines for HIV-1. Proc Natl Acad Sci USA. (2000) 97:3544–9. doi: 10.1073/pnas.97.7.3544
19. McGettigan JP, Foley HD, Belyakov IM, Berzofsky JA, Pomerantz RJ, Schnell MJ. Rabies virus-based vectors expressing human immunodeficiency virus type 1 (HIV-1) envelope protein induce a strong, cross-reactive cytotoxic T-lymphocyte response against envelope proteins from different HIV-1 isolates. J Virol. (2001) 75:4430–4. doi: 10.1128/JVI.75.9.4430-4434.2001
20. Abreu-Mota T, Hagen KR, Cooper K, Jahrling PB, Tan G, Wirblich C, et al. Non-neutralizing antibodies elicited by recombinant Lassa-Rabies vaccine are critical for protection against Lassa fever. Nat Commun. (2018) 9:4223. doi: 10.1038/s41467-018-06741-w
21. Takayama-Ito M, Lim CK, Yamaguchi Y, Posadas-Herrera G, Kato H, Iizuka I, et al. Replication-incompetent rabies virus vector harboring glycoprotein gene of lymphocytic choriomeningitis virus (LCMV) protects mice from LCMV challenge. PLoS Negl Trop Dis. (2018) 12:e0006398. doi: 10.1371/journal.pntd.0006398
22. Bi J, Wang H, Han Q, Pei H, Jin H, Jin S, et al. A rabies virus-vectored vaccine expressing two copies of the Marburg virus glycoprotein gene induced neutralizing antibodies against Marburg virus in humanized mice. Emerg Microbes Infect. (2023) 12:2149351. doi: 10.1080/22221751.2022.2149351
23. Keshwara R, Hagen KR, Abreu-Mota T, Papaneri AB, Liu D, Wirblich C, et al. A recombinant rabies virus expressing the Marburg virus glycoprotein is dependent upon antibody-mediated cellular cytotoxicity for protection against marburg virus disease in a murine model. J Virol. (2019) 93:e01865-18. doi: 10.1128/JVI.01865-18
24. Chi H, Wang Y, Li E, Wang X, Wang H, Jin H, et al. Inactivated rabies virus vectored MERS-coronavirus vaccine induces protective immunity in mice, camels, and alpacas. Front Immunol. (2022) 13:823949. doi: 10.3389/fimmu.2022.823949
25. Kato H, Takayama-Ito M, Iizuka-Shiota I, Fukushi S, Posadas-Herrera G, Horiya M, et al. Development of a recombinant replication-deficient rabies virus-based bivalent-vaccine against MERS-CoV and rabies virus and its humoral immunogenicity in mice. PLoS ONE. (2019) 14:e0223684. doi: 10.1371/journal.pone.0223684
26. Shuai L, Ge J, Wen Z, Wang J, Wang X, Bu Z. Immune responses in mice and pigs after oral vaccination with rabies virus vectored Nipah disease vaccines. Vet Microbiol. (2020) 241:108549. doi: 10.1016/j.vetmic.2019.108549
27. Keshwara R, Shiels T, Postnikova E, Kurup D, Wirblich C, Johnson RF, et al. Rabies-based vaccine induces potent immune responses against Nipah virus. NPJ Vaccines. (2019) 4:15. doi: 10.1038/s41541-019-0109-5
28. Wang H, Bi J, Feng N, Zhao Y, Wang T, Li Y, et al. Construction of recombinant rabies virus vectors expressing H or F protein of peste des petits ruminants virus. Vet Sci. (2022) 9:555. doi: 10.3390/vetsci9100555
29. Kurup D, Wirblich C, Zabihi Diba L, Lambert R, Watson M, Shaikh N, et al. A single dose of the deactivated rabies-virus vectored COVID-19 vaccine, CORAVAX, is highly efficacious and alleviates lung inflammation in the Hamster model. Viruses. (2022) 14:1126. doi: 10.3390/v14061126
30. Kurup D, Malherbe DC, Wirblich C, Lambert R, Ronk AJ, Zabihi Diba L, et al. Inactivated rabies virus vectored SARS-CoV-2 vaccine prevents disease in a Syrian hamster model. PLoS Path. (2021) 17:e1009383. doi: 10.1371/journal.ppat.1009383
31. Yankowski C, Wirblich C, Kurup D, Schnell MJ. Inactivated rabies-vectored SARS-CoV-2 vaccine provides long-term immune response unaffected by vector immunity. NPJ Vaccines. (2022) 7:110. doi: 10.1038/s41541-022-00532-7
32. Kurup D, Wirblich C, Ramage H, Schnell MJ. Rabies virus-based COVID-19 vaccine CORAVAX™ induces high levels of neutralizing antibodies against SARS-CoV-2. NPJ Vacc. (2020) 5:98. doi: 10.1038/s41541-020-00248-6
33. Huang J, Wang W, Li H, Bai Y, Song Y, Jiao C, et al. Three in one: an effective and universal vaccine expressing heterologous tandem RBD trimer by rabies virus vector protects mice against SARS-CoV-2. Antiviral Res. (2024) 227:105905. doi: 10.1016/j.antiviral.2024.105905
34. Zhang H, Jin H, Yan F, Song Y, Dai J, Jiao C, et al. An inactivated recombinant rabies virus chimerically expressed RBD induces humoral and cellular immunity against SARS-CoV-2 and RABV. Virol Sin. (2023) 38:244–56. doi: 10.1016/j.virs.2022.12.006
35. Tian L, Yan L, Zheng W, Lei X, Fu Q, Xue X, et al. A rabies virus vectored severe fever with thrombocytopenia syndrome (SFTS) bivalent candidate vaccine confers protective immune responses in mice. Vet Microbiol. (2021) 257:109076. doi: 10.1016/j.vetmic.2021.109076
36. McKenna PM, Koser ML, Carlson KR, Montefiori DC, Letvin NL, Papaneri AB., et al. Highly attenuated rabies virus-based vaccine vectors expressing simian-human immunodeficiency virus896P Env and simian immunodeficiency virusmac239 Gag are safe in rhesus macaques and protect from an AIDS-like disease. J Infect Dis. (2007) 195:980–8. doi: 10.1086/512243
37. Zhang S, Hao M, Feng N, Jin H, Yan F, Chi H, et al. Genetically modified rabies virus vector-based rift valley fever virus vaccine is safe and induces efficacious immune responses in mice. Viruses. (2019) 11:919. doi: 10.3390/v11100919
38. Liu F, Huang Y, Wang Q, Li J, Shan H. Rescue of Senecavirus A to uncover mutation profiles of its progenies during 80 serial passages in vitro. Vet Microbiol. (2021) 253:108969. doi: 10.1016/j.vetmic.2020.108969
39. Fisher CR, Streicker DG, Schnell MJ. The spread and evolution of rabies virus: conquering new frontiers. Nat Rev Microbiol. (2018) 16:241–55. doi: 10.1038/nrmicro.2018.11
40. Deviatkin AA, Lukashev AN. Recombination in the rabies virus and other lyssaviruses. Infect Genet Evol. (2018) 60:97–102. doi: 10.1016/j.meegid.2018.02.026
41. Takayama-Ito M, Inoue K, Shoji Y, Inoue S, Iijima T, Sakai T, et al. A highly attenuated rabies virus HEP-Flury strain reverts to virulent by single amino acid substitution to arginine at position 333 in glycoprotein. Virus Res. (2006) 119:208–15. doi: 10.1016/j.virusres.2006.01.014
42. Faber M, Faber ML, Papaneri A, Bette M, Weihe E, Dietzschold B, et al. A single amino acid change in rabies virus glycoprotein increases virus spread and enhances virus pathogenicity. J Virol. (2005) 79:14141–8. doi: 10.1128/JVI.79.22.14141-14148.2005
43. Scher G, Schnell MJ. Rhabdoviruses as vectors for vaccines and therapeutics. Curr Opin Virol. (2020) 44:169–82. doi: 10.1016/j.coviro.2020.09.003
44. Dudek T, Knipe DM. Replication-defective viruses as vaccines and vaccine vectors. Virology. (2006) 344:230–9. doi: 10.1016/j.virol.2005.09.020
45. Mebatsion T, Schnell MJ, Conzelmann KK. Mokola virus glycoprotein and chimeric proteins can replace rabies virus glycoprotein in the rescue of infectious defective rabies virus particles. J Virol. (1995) 69:1444–51. doi: 10.1128/jvi.69.3.1444-1451.1995
46. Cenna J, Hunter M, Tan GS, Papaneri AB, Ribka EP, Schnell MJ, et al. Replication-deficient rabies virus-based vaccines are safe and immunogenic in mice and nonhuman primates. J Infect Dis. (2009) 200:1251–60. doi: 10.1086/605949
47. Okada K, Ito N, Yamaoka S, Masatani T, Ebihara H, Goto H, et al. Roles of the rabies virus phosphoprotein isoforms in pathogenesis. J Virol. (2016) 90:8226–37. doi: 10.1128/JVI.00809-16
48. Mebatsion T, Konig M, Conzelmann KK. Budding of rabies virus particles in the absence of the spike glycoprotein. Cell. (1996) 84:941–51. doi: 10.1016/S0092-8674(00)81072-7
Keywords: rabies virus, reverse genetics, live-attenuated RV-vectored vaccine, inactivated RV-vectored vaccine, replication-deficient RV-vectored vaccine
Citation: Li Y, Zhou H, Li Q, Duan X and Liu F (2024) Rabies virus as vector for development of vaccine: pros and cons. Front. Vet. Sci. 11:1475431. doi: 10.3389/fvets.2024.1475431
Received: 03 August 2024; Accepted: 12 September 2024;
Published: 25 September 2024.
Edited by:
Jin Cui, Northeast Agricultural University, ChinaReviewed by:
Yongqiang Zhang, China Animal Health and Epidemiology Center, ChinaLiang Li, Anhui Agricultural University, China
Copyright © 2024 Li, Zhou, Li, Duan and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fuxiao Liu, bGF1ZGF3biYjeDAwMDQwOzEyNi5jb20=; Xiaoxiao Duan, ZHh4NDUmI3gwMDA0MDsxNjMuY29t
†These authors have contributed equally to this work
 Yan Li1,2†
Yan Li1,2† Fuxiao Liu
Fuxiao Liu