- 1Department of Epidemiology and Biostatistics, Indiana University, Bloomington, IN, United States
- 2Department of Obstetrics and Gynecology, Columbia University Irving Medical Center, New York, NY, United States
- 3Department of Epidemiology, Columbia University Irving Medical Center, New York, NY, United States
- 4Indiana Department of Natural Resources, Bloomington, IN, United States
Introduction: Studies examining associations between pet ownership and cardiovascular disease have yielded inconsistent results. These discrepancies may be partially explained by variations in age and sex across study populations. Our study included 6,632 American Gut Project participants who are US residents ≥40 years.
Methods: We first estimated the association of pet ownership with cardiovascular disease risk using multivariable-adjusted logistic regression, and further investigated effect modifications of age and sex.
Results: Cat but not dog ownership was significantly associated with lower cardiovascular disease risk (OR: 0.56 [0.42, 0.73] and OR: 1.17 [0.88, 1.39], respectively). Cat and dog ownership significantly interacted with age but not sex, indicating that cardiovascular risk varies by the age-by-pet ownership combination. Compared to the reference group (40–64 years, no cat or dog), participants 40–64 years with only a cat had the lowest cardiovascular disease risk (OR: 0.40 [0.26, 0.61]). Those ≥65 years with no pets had the highest risk (OR: 3.85 [2.85, 5.24]).
Discussion: This study supports the importance of pets in human cardiovascular health, suggesting optimal pet choice is age-dependent. Having both a cat and dog can be advantageous to people ≥65 years, while having only a cat may benefit those 40–64 years. Further studies are needed to assess causality.
Introduction
Despite recent advances in medical and pharmaceutical treatments, cardiovascular disease (CVD) remains the leading cause of mortality in the US and worldwide (1, 2). CVD is responsible for 37% of deaths attributable to noninfectious causes of individuals under 70 years of age worldwide (3), and approximately one in four deaths in the US (4). In 2018, the prevalence of CVD excluding hypertension was 11.8% among adults over 18 years of age in the US (2). The prevalence also increases by age and was 28.5% among those age ≥ 65 years (2).
A large, multinational cohort study found that approximately 70% of CVD cases are attributable to modifiable risk factors (5). Thus, non-medical interventions that can reduce CVD and its underlying risk factors, such as management of anxiety and social isolation, exercise, and a healthy diet, are critical. There is also considerable interest in the beneficial role that companion animals play in human health, including the potentially protective effect of pet ownership on CVD. In 2020, 45 and 26% of US households had a dog or a cat, respectively (6). Thus, a positive association between pet ownership and CVD could provide a strong basis for implementation of a population-based prevention strategy.
Several hypotheses have been proposed that may explain the potential relationship between pet ownership and CVD. First, it is hypothesized that the pet ownership-CVD association is mediated by psychological and physiological changes that occur when a pet is present (7–12). For example, Allen et al. (7) found that the increase of heart rate and blood pressure while performing challenging math problems was significantly smaller among people who had their pet present than those without their pet present. In 1993, Patronek and Glickman (10) coined the term “pet preventable fraction” as the percent of myocardial infarctions and death that pet ownership could prevent. However, this fraction has not been firmly established for CVD. Second, it is hypothesized that the protective benefit of pet ownership is partly mediated by increased exercise (13, 14), particularly in the case of dog ownership. Some studies have found that dog owners have higher levels of physical activity than non-dog owners (15–18). In contrast, cat ownership has not been found to be associated with physical activity (15, 18). Thus, reduced CVD risk among pet owners may not be merely mediated by increased physical activity.
However, existing studies regarding the association between pet ownership and CVD have not yielded consistent results, showing either positive, negative, mixed, or no associations. Several meta-analyses have attempted to clarify the relationship, but their findings have also differed. For instance, one meta-analysis found modestly lower cardiovascular mortality among cat owners and pet owners compared to non-cat and non-pet owners, respectively, but the differences were not statistically significant (19). Another meta-analysis found that dog owners had a reduced risk of cardiovascular mortality compared to non-dog owners, but the study did not adjust for potential confounding factors (20). In a meta-analysis by Yeh et al. (21), pet ownership was associated with a lower adjusted cardiovascular mortality in the general population compared with CVD patients.
These discrepancies may result from several methodological differences across the studies. First, as discussed in a systematic review, the CVD risk factors considered in these studies differed (22). One of the meta-analyses excluded covariates from their analysis (20), while others included them (19, 21). Second, the studies considered populations with varying age groups. For instance, Chowdhury et al. (23) evaluated the association between pet ownership and survival among hypertensive adults between 65 and 84 years of age, while Maugeri et al. (24) evaluated the association between dog ownership and CVD among adults between 25 and 44 years. A few existing meta-analyses were also conducted by integrating results from studies with participants of various age groups. For example, Kramer et al. included a study with participants between 33 and 85 (25), a study with participants between 65 and 84 (23), and an earlier study with participants who were “adults” with unspecified age (12). El-Qushayri et al. also included studies with participants of varying age from 5 to 17 years (26) to 50–95 years (27). Yeh et al. included studies whose participants were 44.5–72.6 years.
The association between pet ownership and CVD may differ between age groups due to changes in the relationship between the pet and owner across the lifespan. Pets may be sole companions for some senior people, particularly women who are more likely to live alone than age-matched men (3). Pets may also mitigate feelings of loneliness and social isolation among senior people who live alone leading to a reduced risk of CVD.
In this study, we aim to evaluate the association between pet ownership and CVD risk while considering a comprehensive list of risk factors and confounders. We hypothesize that the effect of pet ownership on CVD risk may differ by sex and age groups. Therefore, we further evaluate potential effect modification due to age and sex, which has not been well understood in the literature. The varying effect of pet ownership across subgroups of participants may explain the inconsistent results from previous studies.
Methods
Study population
Our study population included 6,632 individuals who were participants of the American Gut Project (AGP) between 2012 and 2020. The AGP employed a cross-sectional study design with voluntary response sampling. Participants enrolled in the project through either the Indiegogo or FundRazr crowdsourcing websites and completed a demographics, health, and lifestyle survey. Our study was limited to participants ≥40 years of age who resided in the US and answered multiple choice survey questions about pet ownership, cardiovascular disease, and age (28) (see Supplementary Survey). The lower age limit in this study was chosen as individuals ≥40 years are significantly more likely to have age-related forms of CVD compared with those <40 years who are more likely to have hereditary forms (29).
Ethical considerations
Participants’ consent for the AGP was obtained under Institutional Review Board human research subject protocols from University of Colorado, Boulder (Protocol 12-0582, 12/2012-03/2015) or University of California, San Diego (Protocol 141853, 02/2015-present). All data were deidentified and publicly available. Raw data were obtained using redbiom, a utility that allows for accessing and processing of publicly available data stored in Qiita (30). The protocol of this study was reviewed by the Institutional Review Board at Indiana University and was determined to be non-human subjects research (Protocol 1910657990).
Exposure—pet ownership
The main exposures of interest were cat ownership and/or dog ownership. Cat ownership was defined as having a cat(s) and dog ownership as having a dog(s).
Outcome—CVD
The outcome of interest was history of CVD. The answer to the survey question, “Have you ever been diagnosed with coronary artery disease, heart disease, heart attack, or stroke?” determined the history of CVD. Cases were defined as participants who were diagnosed with CVD by a medical professional. CVD controls were defined by those participants who answered “No” to this question.
Covariates
The AGP collected a comprehensive list of covariates that may impact the association between CVD and pet ownership. Demographic factors included age group (40–64 years and ≥ 65 years), sex (female or male), and the highest level of education attained (up to some high school, high school graduate to undergraduate, some graduate school or graduate degree). We dichotomized age into two age groups using the cut point of ≥65 years as previous studies have suggested that the rate of increased CVD risk is relatively stable up to age 65, then increases significantly after age 65 (31). We conducted sensitivity analysis using alternative cut off values (i.e., 60 years) to evaluate the robustness of our analysis. Race or ethnicity was self-reported by participants as Caucasian, Asian or Pacific Islander, African American, Hispanic, or “other.” As more than 90% of participants self-identified as Caucasian, race or ethnicity was collapsed into two levels, Caucasian and non-Caucasian. Height and weight were self-reported by participants and used to calculate body mass index (BMI).
Statistical analysis
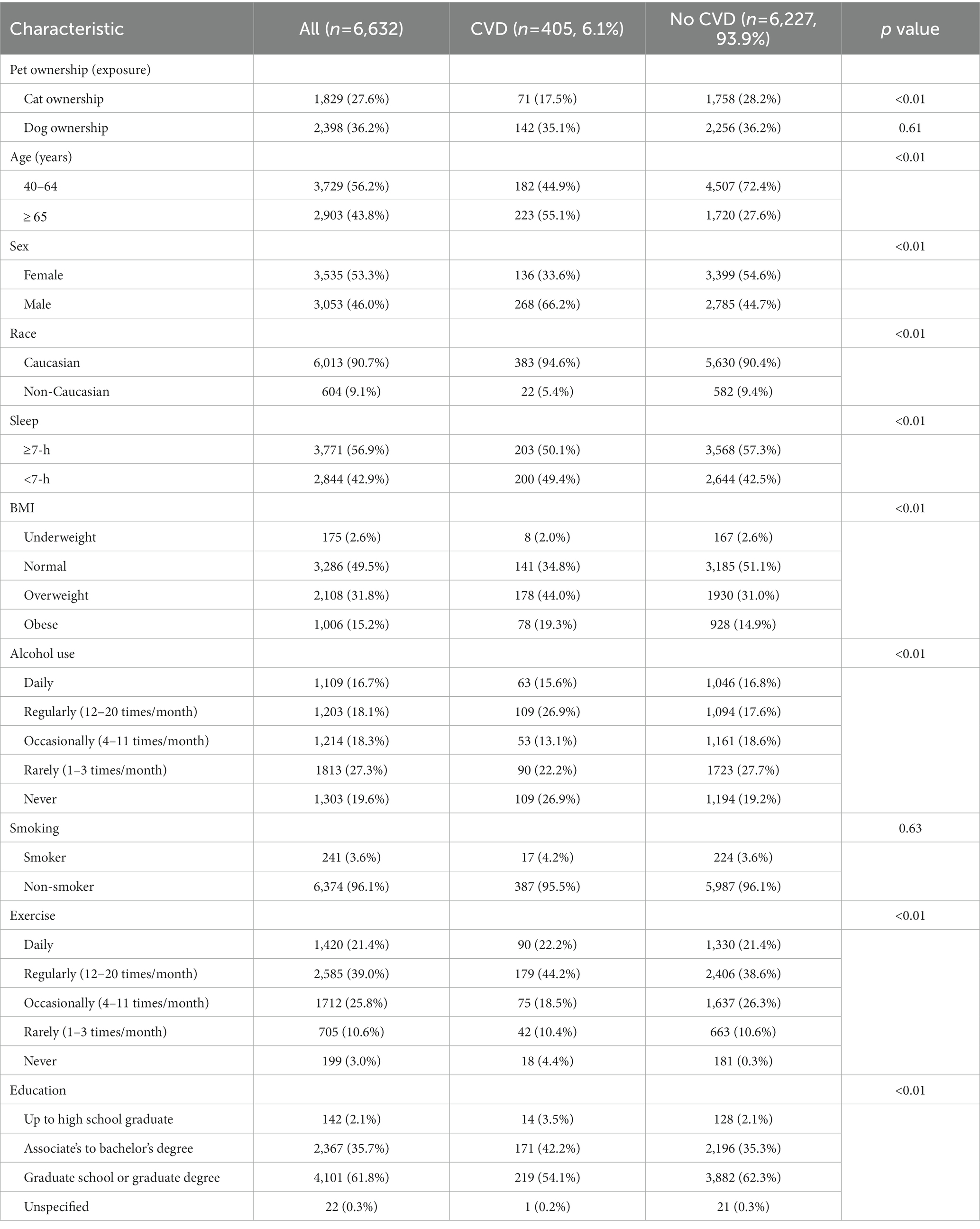
Data analysis was conducted using RStudio, Version 4.1.4 (32). The univariate comparisons of covariates between cases and controls were conducted by Pearson’s Chi-square test and two-sample t-test for categorial and continuous variables, respectively (Table 1). The association between pet ownership on CVD (odds ratio, or OR) was estimated via multivariable-adjusted logistic regression models. Potential confounders were included as covariates in the logistic regression models.
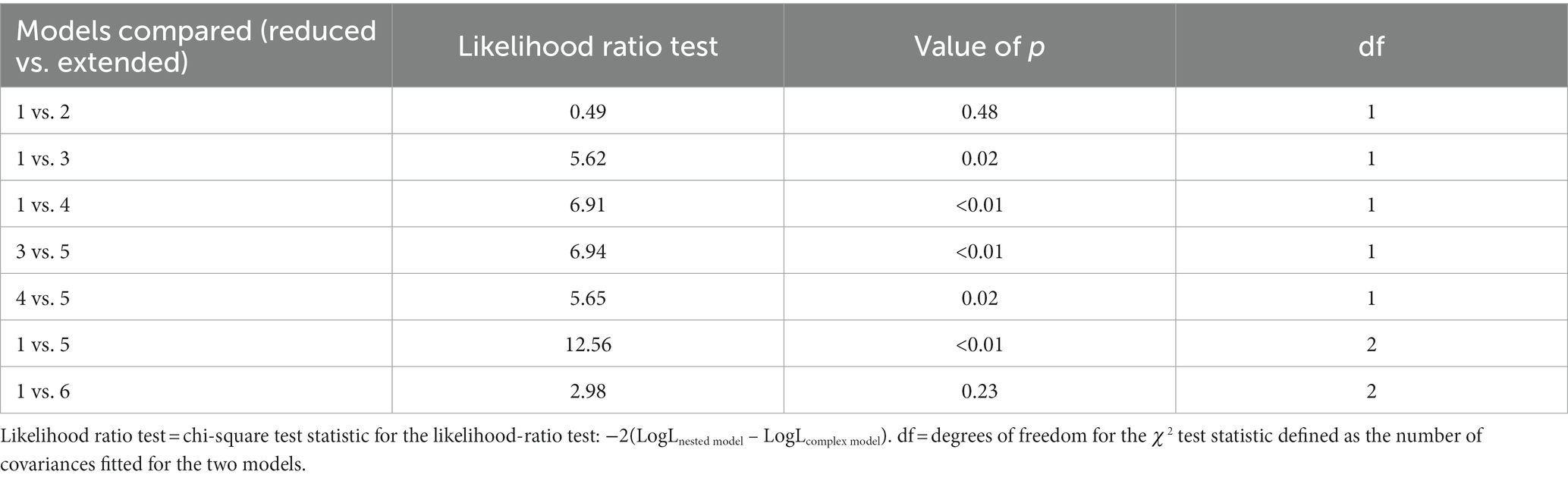
We further tested the secondary hypotheses that there are interactions among cat ownership, dog ownership, age, and sex. We considered five additional logistic regression models with various combinations of interaction terms representing potential effect modification among these factors (Table 2). We first evaluated the effect of cat ownership and dog ownership on CVD risk using a multivariate logistic regression model without considering any potential interactions (i.e., Model 1). We adjusted for age, sex, race, BMI, sleep, alcohol use, smoking, exercise, and education. Model 2 included a cat-by-dog interaction term. Model 3 included an age-by-cat ownership interaction term. Model 4 included an age-by-dog ownership interaction term. Model 5 included both age-by-cat and age-by-dog ownership interaction terms. Model 6 included interaction terms for sex-by-cat ownership and sex-by-dog ownership. All models adjusted for the same covariates other than pet ownership, age, and sex. We conducted stepwise model selection using likelihood ratio tests to determine the optimal model based on the data (33). The likelihood ratio test is calculated as the ratio of the log likelihood of the simpler model relative to the more complex model, with the test statistic approximating a chi-square distribution. When comparing two models, a nested model that was more parsimonious was preferred unless an extended model significantly improved the model fit (p < 0.05).
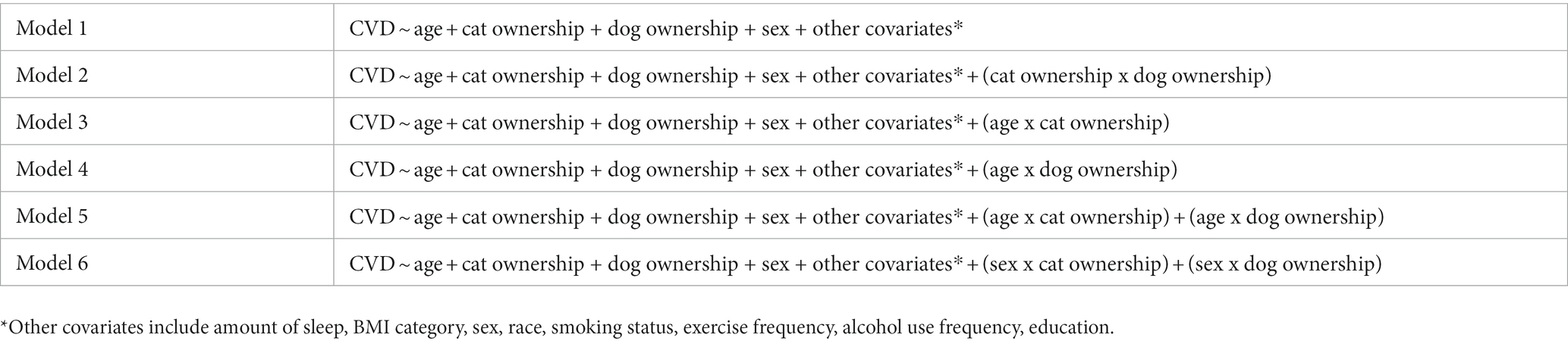
Table 2. Logistic regression models for estimating effect of pet ownership with or without interactions.
Results
Participant characteristics
The participants’ characteristics and univariate comparisons between cases and controls are shown in Table 1. Our study population included 405 CVD cases (6.1%) and 6,227 controls (93.9%). Cat owners comprised 27.6% of the population and showed significantly lower proportion in cases than in controls (17.5% vs. 28.2%; p < 0.01). Dog owners comprised 36.2% of the population and had comparable proportions between cases and controls (35.1% vs. 36.2%, p = 0.61). For dichotomized covariates, a higher proportion of the population was 40–64 years (56.2%), female (53.3%), Caucasian (90.7%), sleep over 7 h/day (56.9%), and current non-smokers (96.1%). Significant differences were found between cases and controls for most of these covariates, including ≥65 years (55.1% vs. 27.6%), female (33.6% vs. 54.6%), Caucasian (94.6% vs. 90.4%), and sleep over 7 h/day (50.1% vs. 57.3%). The proportion of non-smokers did not show significant difference between cases and controls (95.5% vs. 96.1%). A few covariates (BMI, alcohol use, exercise, education) had three or more levels. The levels with the highest proportion were normal BMI (49.5%), rarely alcohol use (27.3%), exercise regularly (39.0%), and some graduate school or graduate degree (61.8%). The distributions of all these covariates were significantly different between cases and controls. For example, the cases were less likely to have normal BMI than controls (34.8% vs. 51.1%).
The association between pet ownership and CVD
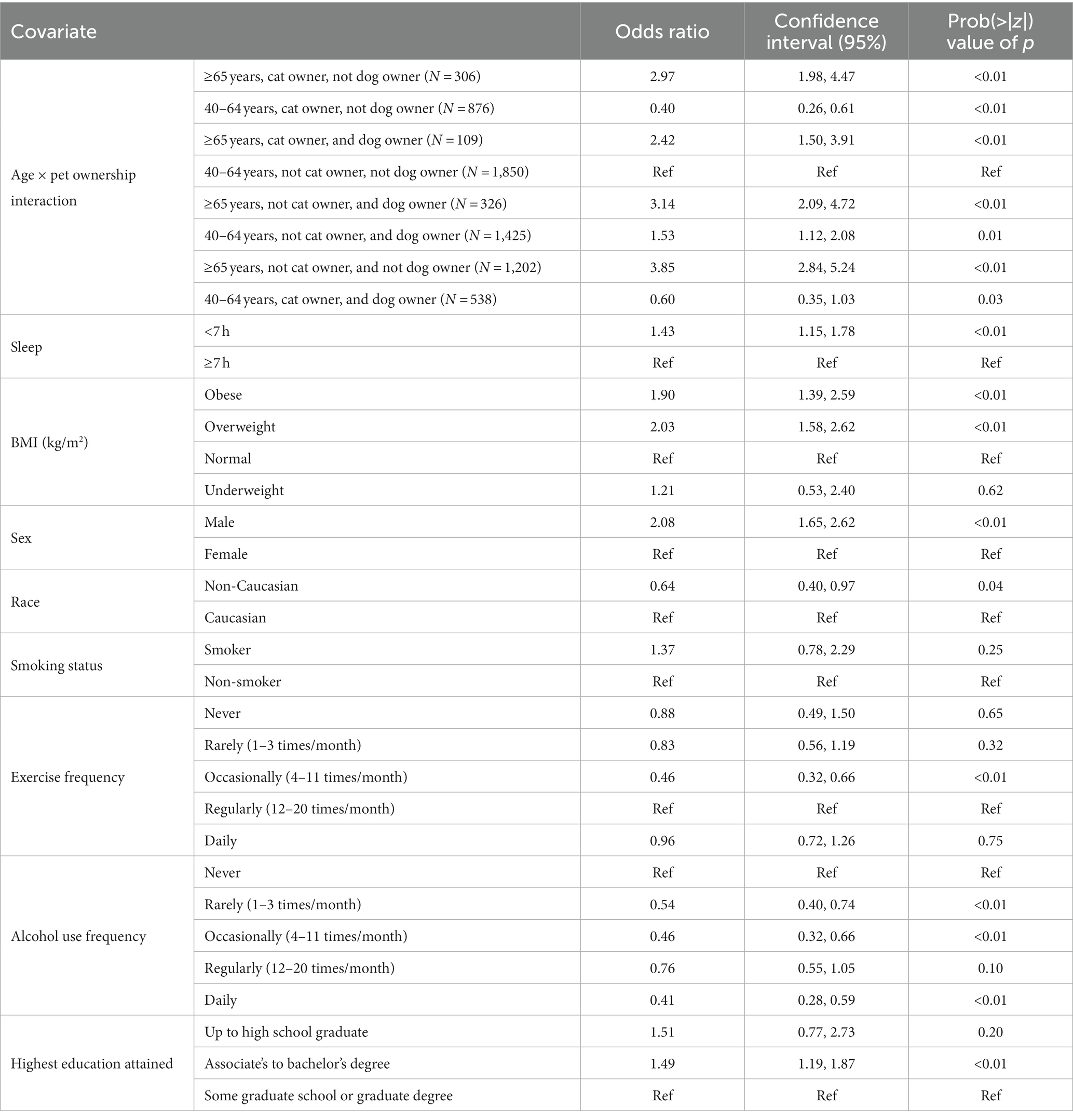
The results of the adjusted model without interaction terms are summarized in Table 3. Cat owners had significantly lower risk of CVD compared with non-cat owners (OR: 0.56 [0.42, 0.73]). There was no significant difference in the risk of CVD between dog owners and non-dog owners (p = 0.17). The risk of CVD was approximately 3.5 times higher among participants aged ≥65 years than among those age 40–64 (OR: 3.51 [2.80, 4.40]) and approximately 2 times higher among men than women (OR: 2.07 [1.65, 2.61]). Both obese and overweight had significantly increased risk over normal BMI, while underweight did not show any significant difference. Exercise, alcohol use and education were all significantly associated with CVD risk, while smoking was not.
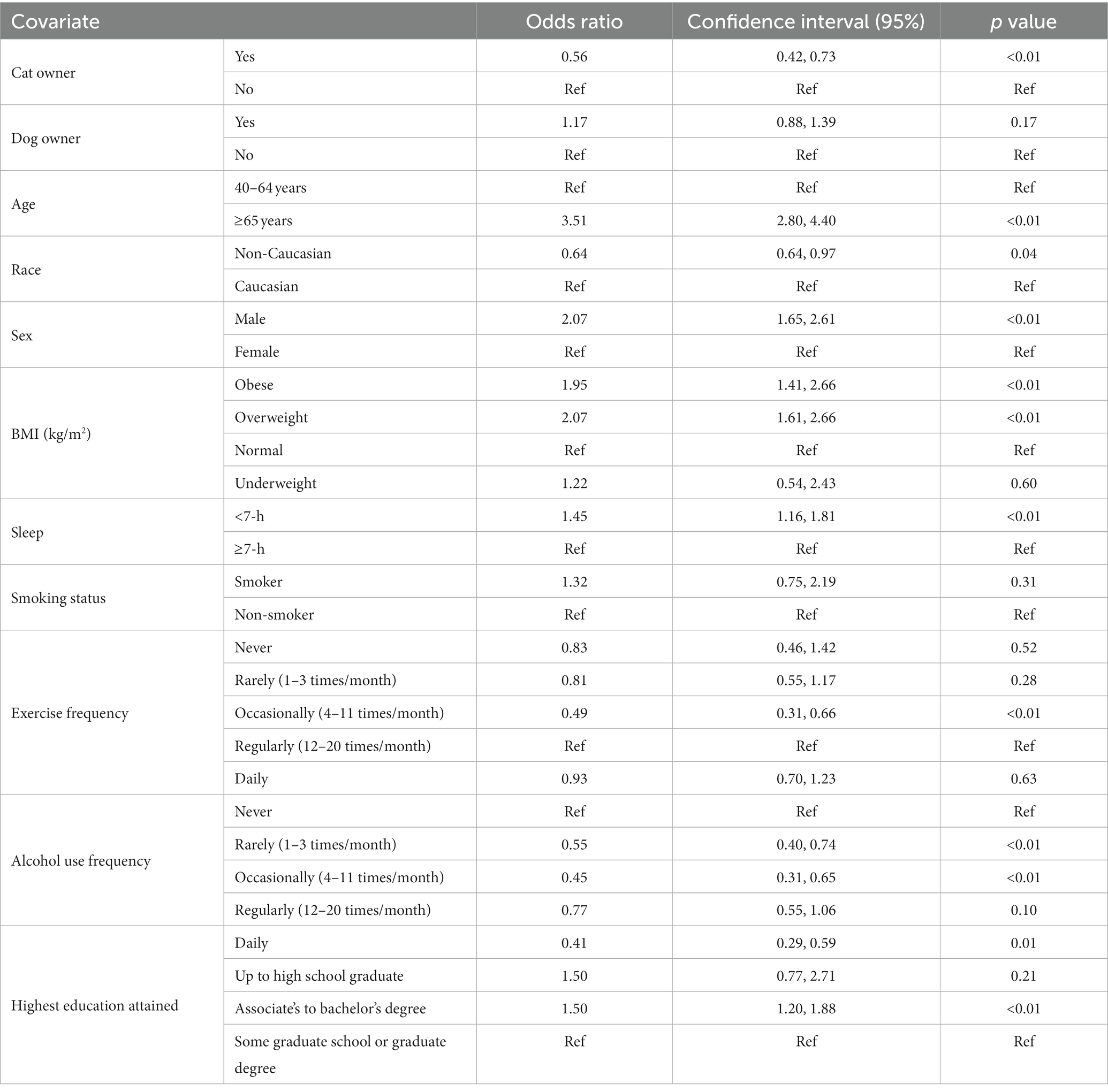
Table 3. Estimated effects of covariates without consideration of potential interactions (i.e., Model 1).
Interactions between pet ownership and age or sex
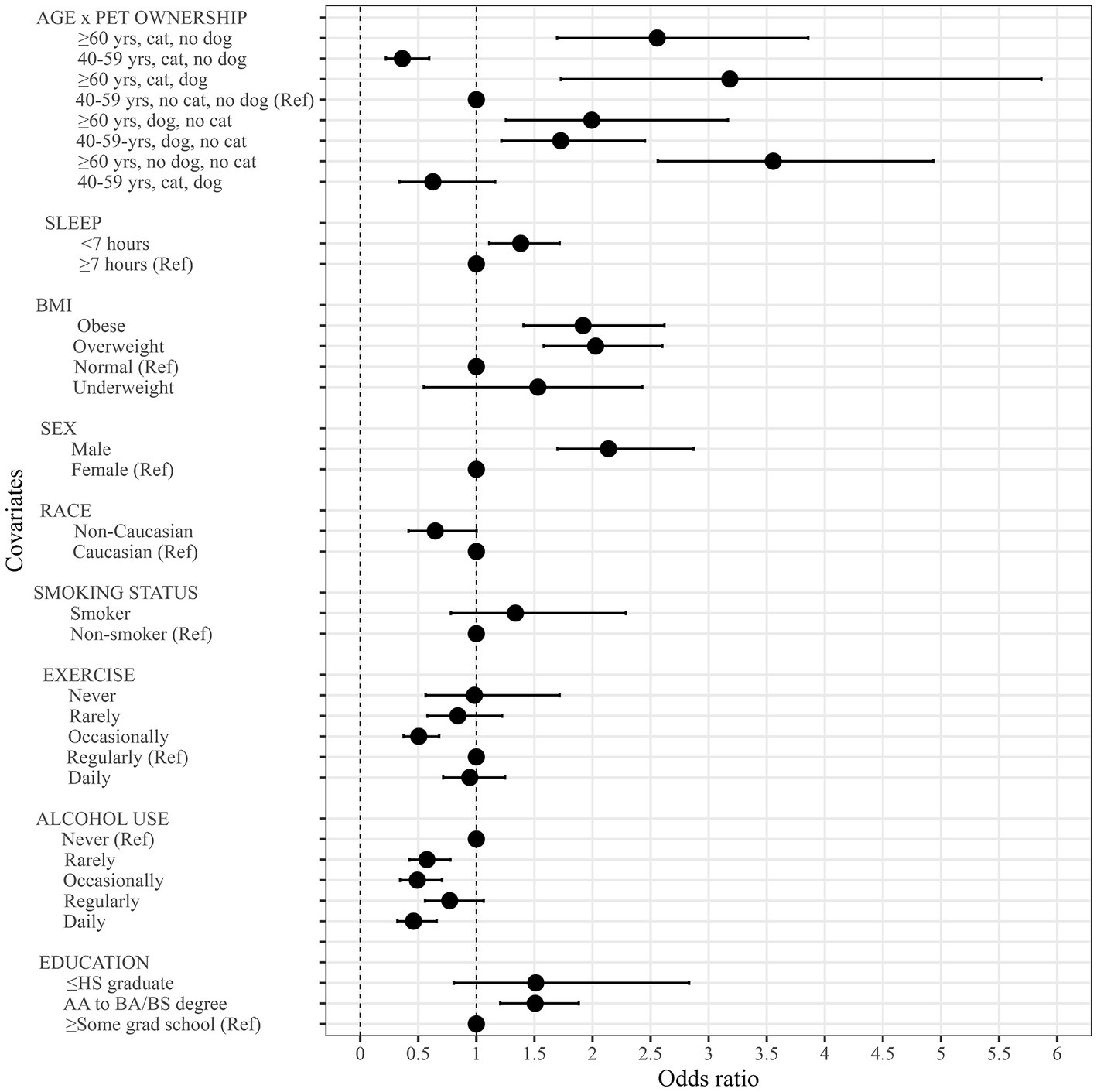
Results of the likelihood ratio tests are shown in Table 4. Model 5 performed significantly better than the other models and was selected as the final model. We followed the principle of parsimony during model selection, wherein an extended model is only selected if it fits the data significantly better than a reduced model (p < 0.05). Sex-by-pet ownership interactions did not improve the data fitting over the non-interaction model (Model 6 vs. Model 1) so were not considered further in additional models. The results of Model 5, which included interaction terms for age-by-cat ownership and age-by-dog ownership, are shown in Table 5. Adjusted ORs, 95% confidence intervals, and value of ps for the final model are shown in Table 5. As a result of the interactions, each participant falls into one of eight groups depending on their level of cat ownership, dog ownership, and age group. Each of these eight groups has a different CVD risk (Table 5).Participants who were 40–64 years, non-cat owners, and non-dog owners were considered the reference group. Compared to the reference group, all other groups had a significantly different risk of CVD.
Participants who were 40–64 years who owned a cat had lower risk of CVD than age-matched participants without a cat, regardless of whether they also owned a dog. Cat-owning Participants who were 40–64 years who did not own a dog had the lowest risk of CVD (OR: 0.40 [0.26, 0.61]) compared to the reference group. Participants aged 40–64 years who owned both a cat and dog had the second lowest risk (OR: 0.60 [0.35, 1.03]) compared to the reference group.
For participants ≥65 years, those who owned both a cat and dog had the lowest CVD risk (OR: 2.42 [1.50, 3.91]). On the other hand, participants ≥65 years who did not own a cat or a dog had the highest risk (OR: 3.85 [2.84, 5.24]). The other participants ≥65 years had varying levels of CVD risk based on the profiles of cat and dog ownership with odds ratios ranging from 2.97 to 3.85. The risk of CVD for all age and pet ownership groups was significantly different from the reference group at p < 0.05 significance level. The risks of CVD for these groups are summarized in Table 5 and depicted in Figure 1.
To illustrate this relationship due to the complex interactions, we further described the effect modification of age on pet ownership in Figure 2. In this figure, we estimated participants’ risk of CVD for the most common covariate profile of participants in the study. For all participants, the estimated risk of CVD increases with age, but at a varying rate by the pet ownership status. For ≥65-year participants, owning no pets was associated with the highest risk of CVD. In contrast, for 40-64-year participants, owning a dog but no cat was associated with the highest CVD risk. Owning both a cat and a dog was associated with the lowest CVD risk among participants ≥65 years, while owning a cat but no dog was associated with the lowest risk among those 40–64 years.

Figure 2. Estimated probability of CVD as a function of pet ownership and age, assuming an individual with a fixed covariate profile (i.e., >7 h sleep, normal BMI, female, white, non-smoker, regular exerciser, rare drinker, and some grad school; i.e. the most common people in our study).
We further repeated all analyses using an alternative cut-off value for age groups (i.e., 40–59 years and ≥60 years) as a sensitivity analysis. There were no appreciable difference from these results; thus, the conclusion remains the same.
Discussion
We found a significant association between pet ownership and CVD risk in our study population. In addition, we found that age group was an effect modifier of this association. For those ≥65 years, owning both a cat and dog was associated with the lowest risk of CVD, while owning no cat or dog was associated with the highest risk of CVD. Further, for those 40–64 years, the lowest risk of CVD was associated with having a cat but no dog, while those with a dog but no cat had the highest CVD risk. A participant’s sex did not significantly modify the associations between pet ownership and CVD. While some prior studies have shown that owning a pet may be associated with reduced risk of CVD, others showed no association. Our findings may help explain the discrepancies in prior studies. Our results suggest that it could be especially beneficial for people ≥65 years to have both cat and dog with respect to cardiovascular health. However, for people aged 40–64 years, having a cat may have sufficient benefit, while having a dog will increase rather than decrease the risk of CVD.
Owning both a cat and dog may be associated with the lowest risk of CVD among ≥65-year participants due to reduced feelings of loneliness and social isolation. This is consistent with existing literature (34). Feelings of loneliness are lowest in middle-aged adults and highest in late adulthood (35). For adults 65–84 years, one study found that feelings of loneliness or social isolation were significantly lower among current or past dog owners than never dog owners (36). In a study of adults ≥60 years, pet owners were 36% less likely to report a feeling of loneliness compared with non-pet owners (37).
Our findings also suggest that owning a dog may increase the risk of CVD among those who are 40–64 years and cat owners. One potential reason is that dog ownership adds responsibilities to life, such as providing food, water, and exercise and managing veterinary care. While cat owners also provide daily food and water, they may not spend time as much time exercising their animals. Cat owners also visit the veterinarian less frequently than dog owners. A 2016 American Veterinary Medical Association survey found 54% of cat owners and 83% of dog owners visited the veterinarian at least once in 2016 (38). Adding these at a time in life when many people are already busy with work and family demands may be a source of stress. Further, dog owners aged 40–64 years may tend to own breeds that confer more stress or other demands.
Another reason the association between pet ownership and cardiovascular disease might differ depending on age may be that cardiovascular reactivity tends to be higher in older than younger individuals. For example, blood vessel responses to stress are impaired as people age due to vascular aging (39). Several experimental studies have found an association between pet ownership and cardiovascular parameters among adults, especially blood pressure and heart rate (7, 40, 41). Maintaining a healthy blood pressure can reduce the rate of vascular aging (42, 44). As pet ownership was associated with blood pressure reductions in several studies, pets may help reduce the rate of vascular aging in people as they age.
Our findings should be viewed considering a few limitations. For example, future studies may benefit from adjusting for pet breed and for pet care demands, such as time spent feeding or walking pets. In addition, further investigation of the association between pet ownership and the adult gut microbiome, contrasting people with and without CVD, may also elucidate the mechanism by which pet ownership is associated with CVD.
Another limitation is that the cases and controls were significantly different, as shown in Table 1. Compared to cases, controls tended to be younger, female and Caucasian, in the normal BMI category, more likely to have attended graduate school and be occasional exercisers, and more likely to be regular alcohol users. While these variables were controlled covariates in the logistic regression models, it is possible that there could be unmeasured confounding of some of the variables, such as BMI. It is possible that residual differences between cases and controls could confound results. It is also likely that the imbalance with respect to other unmeasured factors may contribute to the observed association. Future studies could resolve this with propensity scores.
A shortcoming of this dataset is that, while there was a race and ethnicity question on the questionnaire, the response encoders ultimately classified participants by race (i.e., Caucasian, Asian or Pacific Islander, African American, Hispanic, or “other”). Thus, information about ethnicity was missing in this analysis.
There are also public health measures that could be implemented based on these findings. In particular, the benefit of pet ownership to the cardiovascular health of those ≥65 years suggests that people of this age group should not give up their pets, including people who reside in retirement or assisted living centers. However, not all retirement or assisted living centers accept pets. In 2019, approximately 75% of for-profit retirement living residences accepted pets and the proportion of non-profit residences accepting pets is much lower (43). This is contrary to the US Department of Housing and Urban Development requirement that all properties designated for “elderly or handicapped persons” may not discriminate against individuals with a “common household pet” (45).
Finally, as this study is cross-sectional, a cause-and-effect relationship between pet ownership, some covariates (exercise, sleep, alcohol use, and exercise frequency), and CVD cannot be drawn. Reverse causation can not be ruled out with this study as the order of events is unknown. For instance, a participant may have been advised to obtain a pet after being diagnosed with CVD. However, the finding of effect modification of the pet ownership by age by CVD relationship suggests that future prospective studies, or propensity score analyses, where cause and effect may more easily be interpreted, are indicated.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://www.ebi.ac.uk/ena/browser/view/PRJEB11419.
Author contributions
KW conceived and designed the study, performed the statistical analysis, and wrote the first manuscript draft. ML and KK provided study design guidance. ML contributed to the statistical analysis. TS edited the final manuscript and assisted with data visualization. All authors contributed to the manuscript revisions, read, and approved the submitted version.
Funding
Research funding to KW and ML has been provided by the Human Animal Bond Research Institute, Grant ID# HAB20-010. ML is supported by the National Heart, Lung and Blood Institute under award number K01HL140333.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2023.1168629/full#supplementary-material
References
1. Ahmad, FB, and Anderson, RN. The leading causes of death in the US for 2020. JAMA. (2021) 325:1829–30. doi: 10.1001/jama.2021.5469
2. Tsao, CW, Aday, AW, Almarzooq, ZI, Alonso, A, Beaton, AZ, Bittencourt, MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. (2022) 145:e153–639. doi: 10.1161/CIR.0000000000001052
3. Association for Community Living . Profile of Older Americans.” U.S. Department of Health and Human Services. (2020). https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2019ProfileOlderAmericans508.pdf (Accessed December 01, 2022).
4. Virani, SS, Alonso, A, Aparicio, HJ, Benjamin, EJ, Bittencourt, MS, Callaway, CW, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. (2021) 143:e254–743. doi: 10.1161/CIR.0000000000000950
5. Yusuf, S, Joseph, P, Rangarajan, S, Islam, S, Mente, A, Hystad, P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. (2020) 395:795–808. doi: 10.1016/S0140-6736(19)32008-2
6. Larkin, M. . “Pet Population Still on the Rise, with Fewer Pets per Household.” JAVMA News. (2021) https://www.avma.org/javma-news/2021-12-01/pet-population-still-rise-fewer-pets-household (Accessed December 01, 2022).
7. Allen, K, Blascovich, J, and Mendes, WB. Cardiovascular reactivity and the presence of pets, friends, and spouses: the truth about cats and dogs. Psychosom Med. (2002) 64:727–39. doi: 10.1097/01.psy.0000024236.11538.41
8. Friedmann, E, and Thomas, SA. Pet ownership, social support, and one-year survival after acute myocardial infarction in the cardiac arrhythmia suppression trial (CAST). Am J Cardiol. (1995) 76:1213–7. doi: 10.1016/s0002-9149(99)80343-9
9. Friedmann, E, Thomas, SA, Stein, PK, and Kleiger, RE. Relation between pet ownership and heart rate variability in patients with healed myocardial infarcts. Am J Cardiol. (2003) 91:718–21. doi: 10.1016/s0002-9149(02)03412-4
10. Patronek, GJ, and Glickman, LT. Pet ownership protects against the risks and consequences of coronary heart disease. Med Hypotheses. (1993) 40:245–9. doi: 10.1016/0306-9877(93)90049-v
11. Raina, P, Waltner-Toews, D, Bonnett, B, Woodward, C, and Abernathy, T. Influence of companion animals on the physical and psychological health of older people: an analysis of a one-year longitudinal study. J Am Geriatr Soc. (1999) 47:323–9. doi: 10.1111/j.1532-5415.1999.tb02996.x
12. Friedmann, E, Katcher, AH, Lynch, JJ, and Thomas, SA. Animal companions and one-year survival of patients after discharge from a coronary care unit. Public Health Rep. (1980) 95:307–12.
13. Arhant-Sudhir, K, Arhant-Sudhir, R, and Sudhir, K. Pet ownership and cardiovascular risk reduction: supporting evidence, conflicting data and underlying mechanisms. Clin Exp Pharmacol Physiol. (2011) 38:734–8. doi: 10.1111/j.1440-1681.2011.05583.x
14. Ogechi, I, Snook, K, Davis, BM, Hansen, AR, Liu, F, and Zhang, J. Pet ownership and the risk of dying from cardiovascular disease among adults without major chronic medical conditions. High Blood Press Cardiovasc Prev. (2016) 23:245–53. doi: 10.1007/s40292-016-0156-1
15. Albright, AE, Cui, R, and Allen, RS. Pet ownership and mental and physical health in older white and black males and females. Int J Environ Res Public Health. (2022) 19. doi: 10.3390/ijerph19095655
16. Brown, SG, and Rhodes, RE. Relationships among dog ownership and leisure-time walking in Western Canadian adults. Am J Prev Med. (2006) 30:131–6. doi: 10.1016/j.amepre.2005.10.007
17. Cutt, H, Giles-Corti, B, Knuiman, M, Timperio, A, and Bull, F. Understanding dog owners’ increased levels of physical activity: results from RESIDE. Am J Public Health. (2008) 98:66–9. doi: 10.2105/AJPH.2006.103499
18. Taniguchi, Y, Seino, S, Nishi, M, Tomine, Y, Tanaka, I, Yokoyama, Y, et al. Physical, social, and psychological characteristics of community-dwelling elderly Japanese dog and cat owners. PLoS One. (2018) 13:e0206399. doi: 10.1371/journal.pone.0206399
19. el-Qushayri, AE, Kamel, AMA, Faraj, HA, Vuong, NL, Diab, OM, Istanbuly, S, et al. Association between pet ownership and cardiovascular risks and mortality: a systematic review and meta-analysis. J Cardiovasc Med. (2020) 21:359–67. doi: 10.2459/JCM.0000000000000920
20. Kramer, CK, Mehmood, S, and Suen, RS. Dog ownership and survival: a systematic review and Meta-analysis. Circ Cardiovasc Qual Outcomes. (2019) 12:e005554. doi: 10.1161/CIRCOUTCOMES.119.005554
21. Yeh, TL, Lei, WT, Liu, SJ, and Chien, KL. A modest protective association between pet ownership and cardiovascular diseases: a systematic review and meta-analysis. PLoS One. (2019) 14:e0216231. doi: 10.1371/journal.pone.0216231
22. Barroso, CS, Brown, KC, Laubach, D, Souza, M, Daugherty, LM, and Dixson, M. Cat and/or dog ownership, cardiovascular disease, and obesity: a systematic review. Vet Sci. (2021) 8. doi: 10.3390/vetsci8120333
23. Chowdhury, EK, Nelson, MR, Jennings, GL, Wing, LM, and Reid, CM, ANBP2 Management Committee. Pet ownership and survival in the elderly hypertensive population. J Hypertens. (2017) 35:769–75. doi: 10.1097/HJH.0000000000001214
24. Maugeri, A, Medina-Inojosa, JR, Kunzova, S, Barchitta, M, Agodi, A, Vinciguerra, M, et al. Dog ownership and cardiovascular health: results from the Kardiovize 2030 project. Mayo Clin Proc Innov Qual Outcomes. (2019) 3:268–75. doi: 10.1016/j.mayocpiqo.2019.07.007
25. Friedmann, E, Thomas, SA, and Son, H. “Pets, Depression and Long-term Survival in Community Living Patients Following Myocardial Infarction.”. Anthrozoös. (2011) 14:273–285. doi: 10.2752/175303711X13045914865268
26. Xu, SL, Trevathan, E, Qian, Z, Vivian, E, Yang, BY, Hu, LW, et al. Prenatal and postnatal exposure to pet ownership, blood pressure, and hypertension in children: the Seven Northeastern Cities study. J Hypertens. (2017) 35:259–65. doi: 10.1097/HJH.0000000000001166
27. Wright, JD, Kritz-Silverstein, D, Morton, DJ, Wingard, DL, and Barrett-Connor, E. Pet ownership and blood pressure in old age. Epidemiology. (2007) 18:613–8. doi: 10.1097/EDE.0b013e3181271398
28. McDonald, D, Hyde, E, Debelius, JW, Morton, JT, Gonzalez, A, Ackermann, G, et al. American gut: an open platform for citizen science microbiome research. mSystems. (2018) 3:e00031-18. doi: 10.1128/mSystems.00031-18
29. Merz, AA, and Cheng, S. Sex differences in cardiovascular ageing. Heart. (2016) 102:825–31. doi: 10.1136/heartjnl-2015-308769
30. McDonald, D, Kaehler, B, Gonzalez, A, DeReus, J, Ackermann, G, Marotz, C, et al. Redbiom: a rapid sample discovery and feature characterization system. mSystems. (2019) 4. doi: 10.1128/mSystems.00215-19
31. Sidney, S, Go, A, Jaffe, M, Solomon, M, Ambrosy, A, and Rana, J. Association between aging of the US population and heart disease mortality from 2011 to 2017. JAMA Cardiol. (2019) 4:1280–6. doi: 10.1001/jamacardio.2019.4187
32. R Core Team . “R: A language and environment for statistical computing.” R Foundation for Statistical Computing, Vienna, Austria. (2020). https://www.R-project.org/.
33. Greenland, S . Modeling and variable selection in epidemiologic analysis. Am J Public Health. (1989) 79:340–9. doi: 10.2105/ajph.79.3.340
34. Xia, N, and Li, H. Loneliness, social isolation, and cardiovascular health. Antioxid Redox Signal. (2018) 28:837–51. doi: 10.1089/ars.2017.7312
35. Pinquart, M, and Sorensen, S. Influences on loneliness in older adults: a meta-analysis. Basic Appl Soc Psychol. (2001) 23:245–66. doi: 10.1207/S15324834BASP2304_2
36. Ikeuchi, T, Taniguchi, Y, Abe, T, Seino, S, Shimada, C, Kitamura, A, et al. Association between experience of pet ownership and psychological health among socially isolated and non-isolated older adults. Animals. (2021) 11. doi: 10.3390/ani11030595
37. Stanley, IH, Conwell, Y, Bowen, C, and van Orden, KA. Pet ownership may attenuate loneliness among older adult primary care patients who live alone. Aging Ment Health. (2014) 18:394–9. doi: 10.1080/13607863.2013.837147
38. Burns, K . “AVMA Pet Ownership And Demographics Sourcebook.” AVMA Pet Ownership and Demographics Sourcebook. https://www.avma.org/javma-news/2019-01-15/pet-ownership-stable-veterinary-care-variable (Accessed December 01, 2022).
39. Ungvari, Z, Tarantini, S, Donato, AJ, Galvan, V, and Csiszar, A. Mechanisms of vascular aging. Circ Res. (2018) 123:849–67. doi: 10.1161/CIRCRESAHA.118.311378
40. Allen, KM, Blascovich, J, Tomaka, J, and Kelsey, RM. Presence of human friends and pet dogs as moderators of autonomic responses to stress in women. J Pers Soc Psychol. (1991) 61:582–9. doi: 10.1037/0022-3514.61.4.582
41. Allen, K, Shykoff, B, and Izzo, JL. Pet ownership, but not ACE inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. (2001) 38:815–20. doi: 10.1161/hyp.38.4.815
42. Blood Pressure Lowering Treatment Trialists' Collaboration . Age-stratified and blood-pressure-stratified effects of blood-pressure-lowering pharmacotherapy for the prevention of cardiovascular disease and death: an individual participant-level data meta-analysis. Lancet. (2021) 398:1053–64. doi: 10.1016/S0140-6736(21)01921-8
43. Gordon, R . “How to Find a Pet-Friendly Retirement Community.” Forbes. https://www.forbes.com/sites/nextavenue/2019/01/18/how-to-find-a-pet-friendly-retirement-community/?sh=4b6a49ad27b4 (Accessed December 01, 2022).
44. Bruno, RM, Masi, S, Taddei, M, Taddei, S, and Virdis, A. Essential hypertension and functional microvascular ageing. High Blood Press. Cardiovasc. Prevent. (2018) 25:35–40. doi: 10.1007/s40292-017-0245-9
45. US Department of Housing and Urban Development . Pets in properties that serve the elderly or handicapped. (n.d.). Available at: https://www.hud.gov/states/shared/working/west/mf/petpolicy
Keywords: human animal bond, cardiovascular disease, pet ownership, one health, age, aging
Citation: Watson KM, Kahe K, Shier TA and Li M (2023) Age modifies the association between pet ownership and cardiovascular disease. Front. Vet. Sci. 10:1168629. doi: 10.3389/fvets.2023.1168629
Edited by:
Inês Pereira-Figueiredo, ThekidsFellows, PortugalReviewed by:
Pablo Carmona Munoz, University of Salamanca, SpainNicola Jane Rooney, University of Bristol, United Kingdom
Copyright © 2023 Watson, Kahe, Shier and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katharine M. Watson, a2FtaXdhdHNAaXUuZWR1
 Katharine M. Watson
Katharine M. Watson Ka Kahe2,3
Ka Kahe2,3