
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Vet. Sci. , 08 September 2022
Sec. Veterinary Humanities and Social Sciences
Volume 9 - 2022 | https://doi.org/10.3389/fvets.2022.974665
 Lucía Platero1†
Lucía Platero1† Paula Garcia-Sanchez2,3,†,‡
Paula Garcia-Sanchez2,3,†,‡ Talía Sainz1,3,4,5,6
Talía Sainz1,3,4,5,6 Cristina Calvo1,3,4,5,6
Cristina Calvo1,3,4,5,6 Irene Iglesias7
Irene Iglesias7 Fernando Esperon8‡
Fernando Esperon8‡ Ricardo de la Fuente9
Ricardo de la Fuente9 Esteban Frauca6,10
Esteban Frauca6,10 Antonio Perez-Martinez1,3,6,11
Antonio Perez-Martinez1,3,6,11 Ana Mendez-Echevarria1,3,4,5,6*
Ana Mendez-Echevarria1,3,4,5,6*Pets have many health, emotional and social benefits for children, but the risk of zoonotic infections cannot be underestimated, especially for immunosuppressed patients. We report the recommendations given by health professionals working with pediatric transplant recipients to their families regarding pet ownership. An online survey addressing zoonosis knowledge and recommendations provided by health care practitioners regarding pets was distributed to clinicians treating pediatric transplant recipients. The European Society of Pediatric Infectious Disease (ESPID) and the European Reference Network ERN-TransplantChild, which works to improve the quality of life of transplanted children, allowed the online distribution of the survey. A total of 151 practitioners from 28 countries participated in the survey. Up to 29% of the respondents had treated at least one case of zoonosis. Overall, 58% of the respondents considered that the current available evidence regarding zoonotic risk for transplanted children of having a pet is too scarce. In addition, up to 23% of the surveyed professionals recognized to be unaware or outdated. Still, 27% of the respondents would advise against buying a pet. Practitioners already owning a pet less frequently advised patients against pet ownership, whereas non-pet-owners were more keen to advise against pet ownership (p = 0.058). 61% of the participants stated that there were no institutional recommendations regarding pets in their centers/units. However, 43% of them reported therapeutic initiatives that involved animals in their centers. Infectious disease specialists were more likely to identify zoonotic agents among a list of pathogens compared to other specialists (p < 0.05). We have observed a huge heterogeneity among the recommendations that health care providers offer to families in terms of risk related to pet ownership for transplant recipients. The lack of evidence regarding these recommendations results in practitioners' recommendations based on personal experience.
About 88 million households in the European Union own a pet (1), with rates of household penetration for pet-ownership ranging from 38 to 68% in the European Union and U.S.A. (1, 2). Animal-assisted therapies (AAT) have also been increasingly promoted in recent years, both outside and within health centers (3). Animal contact is known to have beneficial psychological and physical effects, stimulating emotional well-being, physical activity and more time spent outdoors (4). Children who have pets present emotional disorders less frequently than those without pets (5) and patients visited by animals reported decreased anxiety levels compared with patients who receive visits only from volunteers (6). The presence of a dog during venipuncture procedures reduces pain and distress in children (7).
However, animal contact also entails certain risks. Bites and scratches are not uncommon, patients might develop allergies and contact with animals entails risk of zoonoses. In the particular case of immunocompromised patients, opportunistic infections can lead to fatal outcomes. This is especially relevant for children, which are at higher risk of zoonosis due to their close contact with animals and behavioral habits.
However, families facing the diagnosis of a chronic disease in one of their children often acquire pets in an attempt to provide emotional support for the patient, and to increase the quality of life of that child (8). These include pediatric transplant recipients as well. Most guidelines on healthy lifestyles for transplant recipients include recommendations regarding pet ownership. However, these are mostly based on experts' opinion or on case reports, without providing the strength of the recommendations and the quality of evidence grade (9), or provide poor quality and strength regarding most recommendations (10). The decision is therefore left to the discretion of the attending healthcare practitioner (9, 11–13). The lack of evidence translates into great heterogeneity in clinical practice, in a context characterized by an increasing numbers of transplant recipients, along with a generalization of AATs.
A study in the United Kingdom found that only 4 out of 20 pediatric oncology centers offered specific recommendations regarding contact with animals (13). This lack of evidence-based recommendations could lead to unexpected zoonotic exposures. In fact, high-risk exposures (such a as bed sharing or face licking) have been reported in hemato-oncology patients who own pets (14). Potentially zoonotic pathogens were common among asymptomatic dogs and cats that took part in a university-based AAT program, and among pets living with immunocompromised children (15, 16).
To address the risk perception of health care practitioners in terms of pet ownership, and to analyze the heterogeneity and determinants of professional recommendations, a survey was conducted among healthcare practitioners working in the field of pediatric transplantation in different countries.
We conducted an international, observational, cross-sectional study among health care providers involved in pediatric transplant. An anonymous questionnaire designed by pediatric infectious disease specialists and veterinarians was distributed online by the participating scientific societies (Supplementary File 1). The European Reference Network ERN-TransplantChild approved the distribution of the questionnaire among 124 professionals working in 40 healthcare centers from the European Network, between June and December 2020. The surveyed professionals were allowed to send the survey to other colleagues working in pediatric transplantation in their center. During the same period, the survey was also online distributed through the European Society for Pediatric Infectious Diseases to all its members, although only those specialists attending transplant patients were asked to answer it. The survey was sent twice during the 6-month period.
The questionnaire included questions addressing risk perception, knowledge of transmission routes, screening for zoonosis in routine clinical practice and general recommendations provided by the professionals and their institutions. Epidemiological data were collected simultaneously to identify the determinants of recommendations, such as years of experience, previous experience treating zoonosis or pet ownership. The risk awareness was stratified by clinical specialties to address the potential contribution of infectious disease specialist. The study was approved by the Ethics Committee of Hospital La Paz (PI-4770). Qualitative data were expressed as absolute frequencies and/or percentages; quantitative data were expressed as either medians and interquartile ranges (IQR), ranges, or means and standard deviations, depending on data distribution. We used chi-squared test and Fisher's exact test for categorical variables, and Student's t-test or non-parametric tests as appropriate for the continuous variables. A two-sided value of p ≤ 0.05 was considered statistically significant. The statistical analysis was performed using Stata v17.0 (StataCorp LP, College Station, TX, USA) and Prism v.7.0 (GraphPad, Inc., La Jolla, CA, USA).
A total of 151 healthcare practitioners from 78 hospitals in 28 countries participated in the survey, of which 79% were European (106/134) (Supplementary File 2). Table 1 summarizes the main characteristics of the study participants, who were mainly pediatricians treating pediatric solid-organ transplant recipients, hematologists specializing in hematopoietic stem cell transplantation, and pediatric infectious disease specialists. Over 47% of the respondents had up to 15 years of experience in transplantation and worked in units treating up to 100 pediatric transplant recipients.
A total of 69% (93/151) of the participants acknowledged that they do not provide specific recommendations regarding pets and animal contact to their patients. However, 42.6% (64/150) worked in units or centers in which initiatives involving animals were ongoing. Excluding the responses of the pediatric infectious disease specialists, 33.9% (38/112) of the respondents stated that their transplantation team did not include an infectious disease specialist.
Up to 23.3% (34/146) of study participants acknowledged to be unaware of current pet ownership recommendations, while 58.2% (85/146) of the respondents considered the evidence insufficient as to lead to evidence-based recommendations. Among the participants working in units/centers with no specific recommendations regarding pets, only 58.2% (53/91) actively asked about pet ownership during the anamnesis, and 67.5% (102/151) acknowledged to be unaware of the rate of pet ownership among their patients.
In terms of the recommendations provided to families, 27% (40/149) of the respondents would recommend against buying a new pet. However, in cases where the patient already owns a pet, only 9% (13/149) of the respondents would advise against, while 78% (116/149) would recommend keeping the pet, with no significant differences between the various specialist groups. The hematopoietic stem cell transplantation specialists and the infectious disease specialists advised against pet ownership more frequently than the solid organ transplantation specialists (p = 0.02; Figure 1). Health care practitioners owning pets were less likely to advise against pet ownership [40% (60/150) vs. 60% (90/150); p = 0.058].
Regarding the perception of risk for various types of pets, we compared the respondents' answers to the published guidelines (9–13). These guidelines discourage patients to own reptiles and turtles. However, one out of three responders believed that there are no health risks in having turtles in the household, and one out of four responders for reptiles (Table 2).
Healthcare practitioners were asked whether they actively searched for a zoonosis during the differential diagnosis of fever of unknown origin. A 72.2% (26/36) of the infectious disease specialists stated that they routinely include zoonosis screening among their pet-owning patients, compared to 28.8% (32/111) of other specialists (p < 0.001). Twenty-nine percent (43/147) of the respondents had previously treated at least one zoonosis (Supplementary File 3). These professionals more frequently search for zoonosis when studying a transplant recipient with fever who owns pets, compared with those responders who have never treated zoonoses [57% (24/42) vs. 31% (32/103); p = 0.03].
The respondents were asked to select among a list of 23 pathogens that can be transmitted from animals to humans based on literature reports (Figures 2A–C) (13, 16–20). We observed that 52% (12/23) of the pathogens were identified as related to animal contact by more than 70% of the infectious disease specialists, while only 13% (3/23; Chlamydia psittaci, Toxoplasma gondii and Toxocara spp.) were identified by more than 70% of the remaining specialists (p = 0.004). For most pathogens, 20–25% of the respondents were unable to categorize the infection as a zoonosis, 11% (IQR 5–13) for the infectious disease specialists compared with 27% (IQR 24–32) for the other specialists (p < 0.001).
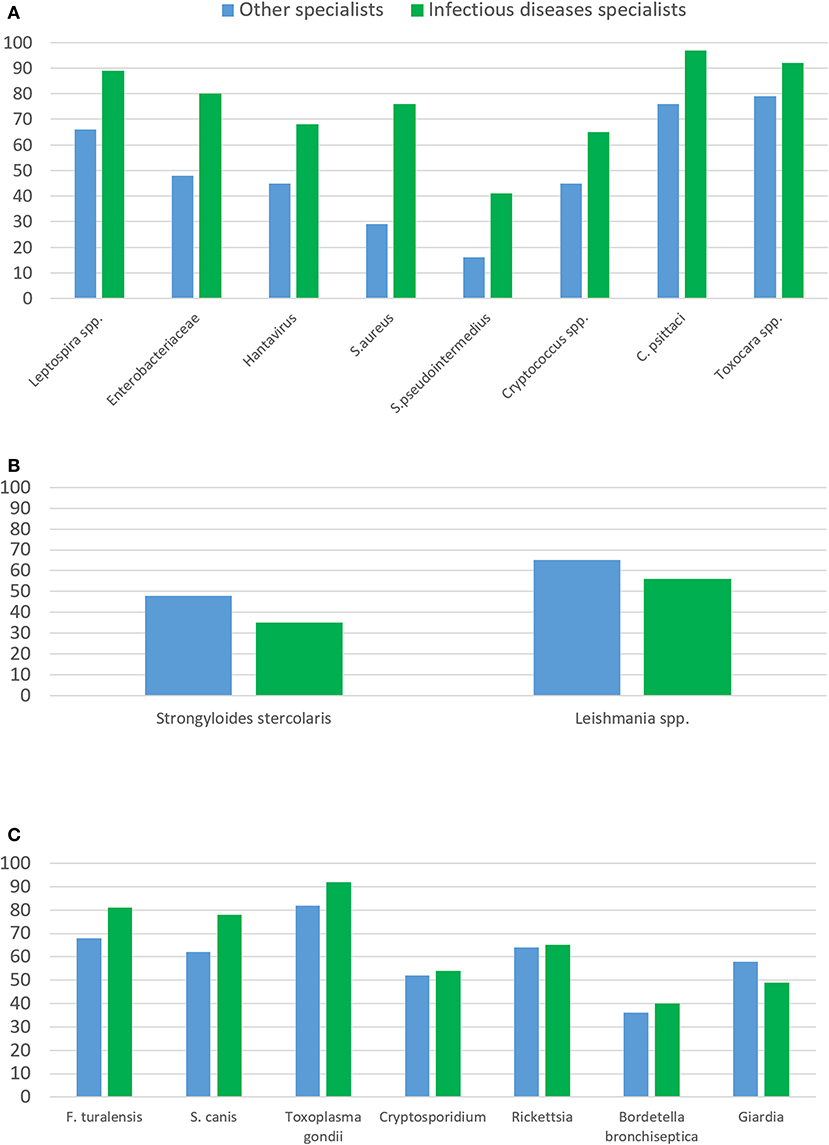
Figure 2. Differences in the identification of pathogens according to the type of medical specialist. (A) Zoonotic pathogens significantly identified more frequently by the infectious disease specialists than by the other specialists (p < 0.05). Enterobacteriaceae include Campylobacter, E. coli and Salmonella. Atypical mycobacteria and Microsporidium canis were also more frequently identified by infectious diseases specialists (57 vs. 76% and 63 vs. 78%, respectively); (B) Zoonotic pathogens significantly identified more frequently by the other specialists than by the infectious disease specialists; (C) Pathogens with no significant difference in their identification comparing infectious disease specialists with other specialists.
Twelve pathogens were identified significantly more by the infectious disease specialists than by the other specialists (Figure 2A); however, two pathogens (Strongyloides stercoralis and Leishmania spp.) were more readily identified by the other specialists than by the infectious disease specialists (Figure 2B). We analyzed the geographical location of these practitioners, given that most cases of strongyloidiasis and leishmaniasis have been reported in southwestern Europe (21, 22). We observed that, regardless of their specialty, 86% (49/57) of the respondents from Spain, Portugal and Italy could identify Leishmania spp. as a possible zoonotic agent, compared to 47% (45/94) of the respondents from other countries (p < 0.0001). No significant differences were found for Strongyloides stercoralis when comparing respondents from southern Europe (52%; 26/50) and other regions (40.5%; 41/60; p = 0.1).
Our results suggest that experienced healthcare practitioners involved in pediatric transplantation do not perceive pets as a potential associated health risk and do not systematically collect information regarding contact with pets. Most centers do not have standardized protocols and official recommendations for animal contact for immunosuppressed patients. The survey reveals a significant variability in clinical practice. Over 30% of the respondents had treated at least one case of zoonosis, however there is a lack of knowledge of the risks associated with the different types of pets and most clinicians do not include zoonosis in the differential diagnosis of fever.
These results likely reflect the lack of evidence-based recommendations, which are mainly based on expert opinion, on anecdotal clinical experiences, extrapolation from experiences on other immunocompromised hosts, and risk warnings arising from case series (9). It is therefore unsurprising that clinical practice varies widely. The recommendations provided by healthcare practitioners are heterogeneous, and usually are based on personal experiences. Practitioners that are pet owners often encourage their patients to have companion animals; hemato-oncologists, infectious disease specialists and practitioners who have treated zoonoses more frequently advise against them. The lack of evidence certainly places practitioners in a complex dilemma when it comes to offer recommendations to patients, however, practitioners should not ignore the risk imposed by pets. A complete anamnesis should always include information regarding animal contact, and the possibility of zoonosis has to be contemplated when evaluating these patients. As there is no evidence to estimate the risk of infection associated to certain pets, there are some recommendations that we can offer to at least minimize the risks, such as a strict veterinary control of the pets, which is included in most guidelines (9, 10).
Several authors highlight that only a few immunocompromised patients are asked about pets or receiving recommendations on safe animal contact (8, 14). However, up to 70% of new pets acquired by families of children with chronic disease are considered as a high infectious risk, either due to the pets age (puppies younger than 6 months) or due to factors related to the animal species (8). Families of immunocompromised children are often unaware about the possibility of acquiring infections from their pets (8). The fact that most healthcare practitioners do not actively include this information in the anamnesis reinforces the idea that pets are not a matter of concern. A recent study that assessed the knowledge and perceptions regarding infectious disease transmission in AAT settings reported that up to 70% of animal handlers working in these programs were not concerned about infectious disease transmission (15). Proper infection control practices by these individuals were lacking despite having undergone animal handler education (15).
The fact that many transmittable infections by pets were not identified as zoonosis by our respondents also explain their low-risk perception. Acute diarrhea caused by Salmonella spp. is usually cataloged as a foodborne illness but has been largely reported as a zoonotic infection (23). The suspicion and rate of zoonosis identified by the infectious disease specialists was significantly higher, prompting them to systematically screen for zoonoses during the anamnesis. Multidisciplinary teams including infectious diseases would provide better screening protocols, and promote a prompt detection and treatment of zoonotic infections in immunocompromised children.
A significant percentage of infectious disease specialists were unable to identify pathogens that commonly colonize pets as potentially transmissible to humans, such as Staphylococcus pseudintermedius, Bordetella bronchiseptica, Cryptococcus neoformans or Mycobacterium tuberculosis/Mycobacterium bovis (24). Bordetella bronchiseptica has been reported to cause pneumonia in transplant recipients after exposure to dogs that have recently been vaccinated with the live-vaccine (25). C. neoformans has been found in a high percentage of avian pets' feces and is transmitted through the inhalation of aerosolized organisms from feces (18, 26). Although pets are unlikely to spread M. bovis, there are reports of some transmitted cases associated to cats (27).
Transplantation is a complex process that causes high levels of stress for families and patients, as well as increased financial and time burdens, disrupted family interactions, and major restructuring of daily routines. Improved family adjustment following pediatric transplantation has been associated with beneficial medical and psychosocial outcomes (28), and pets could be an additional benefit. Up to 70% of the families of chronically ill children reported that the benefits of pet ownership outweighed the health risks, and 92% of the pet-owning respondents felt that removing their pets would have a negative impact (8). Healthcare practitioners should therefore address this issue with the families, and should communicate both the benefits and risks imposed by pet ownership.
The role of health care professionals in preventing zoonosis is determinant. Expectations and concerns should be discussed with the family. Clinicians should evaluate individual risk based on immunosuppression and local epidemiology. Clear written information should be provided, including timing of new pet acquisition, veterinary and hygiene requirements and additional sources on information. Infectious disease specialists and veterinarians can support the decision making, and need to be involved (29).
Regarding the type of pet, some animals should be avoided such as puppies and kittens younger than 6 months of age, exotic pets, stray and wild animals, reptiles, turtles or amphibians (9, 10). Transplant recipients should avoid cleaning pet litter boxes, bird cages, bird feeders, and fish tanks, disposing of animal waste, or handling animal feces (9, 10). Hands should be washed before and after coming into contact with animals, their food, or supplies. Kissing animals, being licked by animals, bedding with dogs or cats, sharing food with animals, activities with high risk for scratches or bites, or keeping cages or pets' pillows in the patient room should be avoided (9, 10).
On the other hand, routine and proper veterinary care is an essential. The relevance of securing the pet's health should be emphasized by healthcare providers, and individual veterinary procedures should be adjusted (9, 10, 30). Knowledge regarding zoonosis, parasite prevention, dental care or animal feeding should be routinely checked and reinforced. Pet vaccination schedules should be checked (9, 10, 30).
Our study has several limitations, including the missing data, the lack of knowledge about the total number of professionals who initially received the survey, and therefore, the rate of responders, as well as the selection bias inherent to the study design which was based on an online questionnaire. The geographical distribution of the participants is an additional limitation, since most of the clinicians worked in Europe and we report the current knowledge on pet-associated zoonoses and the recommendations provided by pediatric transplantation specialists across 28 different counties.
In summary, our results suggest high heterogeneity and a low-risk perception regarding zoonosis among healthcare professionals that manage pediatric transplant recipients. Further evidence is urgently needed in order to establish evidence-based guidelines for transplant recipients who own pets. In the meantime, health care professionals should address animal contact among other risk factors, ideally from a multidisciplinary approach and with an individual risks-benefits perspective. Health professionals should communicate this information to families in order to improve the quality of life of pediatric transplant recipients.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
LP: participated in the writing of the initial draft, participated in data analysis, and participated in the performance of the research. PG-S: participated in the performance of the research, data collection, and reviewing the definitive manuscript. TS: participated in research design, participated in the writing of the initial draft, and participated in data analysis. CC: participated in research design, reviewing the definitive manuscript, and participated in data analysis. II, FE, RF, EF, and AP-M: participated in the performance of the research and reviewing the definitive manuscript. AM-E: participated in research design, participated in the writing of the initial draft, participated in data analysis, participated in the performance of the research, and reviewing the definitive manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This study was supported by the Health Institute Carlos III, Grant No. PI18CIII/00372 [Carlos III Spanish Health Institute (ISCIII) and Fondos FEDER; EU], by the Spanish Pediatrics Association (AEP) INVEST-AEP 2021 Research Grant and, by the MAPFRE Foundation (Research grants by Ignacio H. de Larramendi 2021). TS has been funded by Carlos III Health Institute-Fondos Feder (BAE21/00022). The funding bodies did not have a role in the design or conduct of the study, the analysis and interpretation of the results, the writing of the report, or the decision to publish.
To Kinga A. Sandor-Bajusz for the revision of the English language.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2022.974665/full#supplementary-material
Supplementary File 1. Online survey distributed by the European Reference Network TransplantChild and the European Society for Pediatric Infectious Diseases among their members.
Supplementary File 2. Participants' countries and hospitals.
Supplementary File 3. Type of infections related to animal contact previously treated by the 151 respondents.
1. FEDIAF. Annual Report 2019. (2019). 2019: 52. Available online at: http://www.fediaf.org/annual-report.html (Accessed April 1, 2022).
2. The 2017-2018 American Pet Products Association (APPA) survey (2022). Available online at: https://www.mceldrewyoung.com/wp-content/uploads/2018/08/2017-2018-Pet-Survey.pdf (Accessed 1st April 2022).
3. Lundqvist M, Carlsson P, Sjödahl R, Theodorsson E, Levin LÅ. Patient benefit of dog-assisted interventions in health care: a systematic review. BMC Comp Altern Med. (2017) 17:358. doi: 10.1186/s12906-017-1844-7
4. Owen CG, Nightingale CM, Rudnicka AR, Ekelund U, McMlnn AM, Van Sluijs EMF, et al. Family dog ownership and levels of physical activity in childhood: findings from the child heart and health study in England. Am J Public Health. (2010) 100:1669–71. doi: 10.2105/AJPH.2009.188193
5. Christian H, Mitrou F, Cunneen R, Zubrick SR. Pets are associated with fewer peer problems and emotional symptoms, and better prosocial behavior: findings from the longitudinal study of Australian children. J Pediatr. 202:200–6. doi: 10.1016/j.jpeds.2020.01.012
6. Kaldy J. Alternative therapies for a new era of health care. Consult Pharm. (2013) 28:84–90. doi: 10.4140/TCP.n.2013.84
7. Vagnoli L, Caprilli S, Vernucci C, Zagni S, Mugnai F, Messeri A. Can presence of a dog reduce pain and distress in children during venipuncture? Pain Manag Nurs. (2015) 2:89–95. doi: 10.1016/j.pmn.2014.04.004
8. Stull JW, Brophy J, Sargeant JM, Peregrine AS, Lawson ML, Ramphal R, et al. Knowledge, attitudes, and practices related to pet contact by immunocompromised children with cancer and immunocompetent children with diabetes. J Pediatr. (2014) 165:348–55. doi: 10.1016/j.jpeds.2014.04.045
9. Avery RK, Michaels MG, AST Infectious diseases community of practice. Strategies for safe living following solid organ transplantation-guidelines from the American society of transplantation infectious diseases community of practice. Clin Transplant. (2019) 33:e13519. doi: 10.1111/ctr.13519
10. Tomblyn M, Chiller T., Einsele H., Gress R., Sepkowitz K., Storek J., et al. Guidelines for Preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Biol Blood Marrow Transplant. (2009) 15:1143–238. doi: 10.1016/j.bbmt.2009.06.019
11. Blair BM. Safe living following solid organ transplantation. Surg Clin North Am. (2019) 99:153–61. doi: 10.1016/j.suc.2018.09.011
12. Sirvent A, Delorme J, Godin S, Grain A, Jubert C, Pertuisel S, et al. Children and adolescents discharge guidelines after allogeneic stem cell transplantation for healthcare professionals: recommendations of the francophone society of bone marrow transplantation and cellular therapy. Bull Cancer. (2020) 107:S62–7. doi: 10.1016/j.bulcan.2019.03.006
13. Hemsworth S, Pizer B. Pet ownership in immunocompromised children–a review of the literature and survey of existing guidelines. Eur J Oncol Nurs. (2006) 10:117–27. doi: 10.1016/j.ejon.2005.08.001
14. Gurry GA, Campion V, Premawardena C, Woolley I, Shortt J, Bowden DK, et al. High rates of potentially infectious exposures between immunocompromised patients and their companion animals: an unmet need for education. Intern Med J. (2017) 47:333–5. doi: 10.1111/imj.13361
15. Boyle SF, Corrigan VK. Buechner-Maxwell V, Pierce BJ. Evaluation of risk of zoonotic pathogen transmission in a university-based animal assisted intervention (AAI) program. Front Vet Sci. (2019) 6:1–10. doi: 10.3389/fvets.2019.00167
16. Peña A, Abarca K, Weitzel T, Gallegos J, Cerda J, García P, et al. One health in practice: a pilot project for integrated care of zoonotic infections in immunocompromised children and their pets in Chile. Zoonoses Public Health. (2016) 63:403–9. doi: 10.1111/zph.12241
17. Pomba C, Rantala M, Greko C, Baptiste KE, Catry B, Van Duijkeren E, et al. Public health risk of antimicrobial resistance transfer from companion animals. J Antimicrob Chemother. (2017) 72:957–68. doi: 10.1093/jac/dkw481
18. Bretón-Martínez JR, Alcolea A, Quintero-García D, Méndez-Echevarria A, Ramos E, Bueno F, et al. Non-wild-type cryptococcosis in a child with multivisceral organ transplant who owned bird pets. Transpl Infect Dis. (2021) 23:e13558. doi: 10.1111/tid.13558
19. Chomel BB. Diseases transmitted by less common house pets. Microbiol Spectr. (2015) 3:1–23. doi: 10.1128/microbiolspec.IOL5-0012-2015
20. O'Neil J. Zoonotic infections from common household pets. J Nurse Pract. (2018) 14:363–70. doi: 10.1016/j.nurpra.2017.12.025
21. Ready PD. Leishmaniasis emergence in Europe. Euro Surveill. (2010) 15:29–39. doi: 10.2807/ese.15.10.19505-en
22. Jaleta TG, Zhou S, Bemm FM, Schär F, Khieu V, Muth S, et al. Different but overlapping populations of Strongyloides stercoralis in dogs and humans—Dogs as a possible source for zoonotic strongyloidiasis. PLOS Negl Trop Dis. (2017) 11:1–21. doi: 10.1371/journal.pntd.0005752
23. Marin C, Vega S, Marco-Jiménez F. Tiny turtles purchased at pet stores are a potential high risk for salmonella human infection in the Valencian region, eastern Spain. Vector Borne Zoonotic Dis. (2016) 16:455–60. doi: 10.1089/vbz.2016.1950
24. Lozano C, Rezusta A, Ferrer I, Pérez-Laguna V, Zarazaga M, Ruiz-Ripa L, et al. Staphylococcus pseudintermedius human infection cases in Spain: dog-to-human transmission. Vector Borne Zoonotic Dis. (2017) 17:268–70. doi: 10.1089/vbz.2016.2048
25. Gisel JJ, Brumble LM, Johnson MM. Bordetella bronchiseptica pneumonia in a kidney-pancreas transplant patient after exposure to recently vaccinated dogs. Transpl Infect Dis. (2010) 12:73–6. doi: 10.1111/j.1399-3062.2009.00451.x
26. Nosanchuk JD, Shoham S, Fries BC, Shapiro DS, Levitz SM, Casadevall A. Evidence of zoonotic transmission of Cryptococcus neoformans from a pet cockatoo to an immunocompromised patient. Ann Intern Med. (2000) 132:205–8 doi: 10.7326/0003-4819-132-3-200002010-00006
27. O'Connor CM, Abid M, Walsh AL, Behbod B, Roberts T, Booth LV, et al. Cat-to-human transmission of Mycobacterium bovis, United Kingdom. Emerg Infect Dis. (2019) 25:2284–6. doi: 10.3201/eid2512.190012
28. Cushman GK, Eaton CK, Gutierrez-Colina AM, Quast LF, Lee JL, Reed-Knight B, et al. Looking beyond the individual: How family demands and capabilities affect family adjustment following pediatric solid organ transplant. Fam Syst Health. (2019) 37:291–301. doi: 10.1037/fsh0000449
29. Ganapathi L, Danziger-Isakov L, Kotton C, et al. Trainee needs in pediatric transplant infectious diseases education. J Pediatric Infect Dis Soc. (2017) 6:301–4. doi: 10.1093/jpids/piw062
Keywords: pets, transplant, zoonosis, children, survey
Citation: Platero L, Garcia-Sanchez P, Sainz T, Calvo C, Iglesias I, Esperon F, de la Fuente R, Frauca E, Perez-Martinez A and Mendez-Echevarria A (2022) Pets for pediatric transplant recipients: To have or not to have. Front. Vet. Sci. 9:974665. doi: 10.3389/fvets.2022.974665
Received: 21 June 2022; Accepted: 16 August 2022;
Published: 08 September 2022.
Edited by:
Ioannis Magouras, City University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Ilda Gomes Rosa, Universidade de Lisboa, PortugalCopyright © 2022 Platero, Garcia-Sanchez, Sainz, Calvo, Iglesias, Esperon, de la Fuente, Frauca, Perez-Martinez and Mendez-Echevarria. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ana Mendez-Echevarria, YW1lbmRlemVzQHlhaG9vLmVz
†These authors have contributed equally to this work and share first authorship
‡ORCID: Paula Garcia-Sanchez orcid.org/0000-0003-4866-6656
Fernando Esperon orcid.org/0000-0002-8810-5071
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.