
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Vet. Sci. , 26 April 2022
Sec. Veterinary Epidemiology and Economics
Volume 9 - 2022 | https://doi.org/10.3389/fvets.2022.864813
 Mahmoud Eltholth1,2*
Mahmoud Eltholth1,2* Gurrappanaidu Govindaraj3
Gurrappanaidu Govindaraj3 Banani Das3
Banani Das3 M. B. Shanabhoga3
M. B. Shanabhoga3 H. M. Swamy3
H. M. Swamy3 Abin Thomas1
Abin Thomas1 Jennifer Cole4
Jennifer Cole4 Bibek R. Shome3
Bibek R. Shome3 Mark A. Holmes5
Mark A. Holmes5 Dominic Moran1
Dominic Moran1This study investigates factors influencing veterinarians' antibiotic prescribing behaviors and their understanding of antimicrobial resistance (AMR). The study used a telephone survey of 50 veterinarians conducted in five districts in Assam state, India. The survey sought information on the most prevalent animal diseases, veterinarians' awareness of potential preventive measures, including factors determining antimicrobial prescribing; the types of antimicrobials used for different health conditions in different species, and possible options to reduce antimicrobial use (AMU). The majority (86%) of respondents worked for the government, 98% reported having no written policy for the use of veterinary health products, and 58% have no on-site diagnostic facilities. Ceftriaxone, Enrofloxacin, and Oxytetracycline were the antibiotics (ABX) most frequently prescribed, by 76, 68, and 54% of veterinarians, respectively. These ABX were prescribed mainly for respiratory health problems and mastitis in cattle, and gastrointestinal infections in buffaloes, sheep, goat, and pigs. Severity of clinical symptoms, economic status of the livestock owner, and withdrawal period for ABX were ranked as very important factors for giving ABX. Less than two thirds (64%) were aware of the government ban for Colistin and only 2% were aware of a national plan for AMR. This study highlighted that ABX prescription is mostly based on tentative diagnosis given the lack of diagnostic facilities in most veterinary clinics. There is a need to enhance veterinary healthcare and to improve communication between policy makers and field veterinarians and, importantly, a need to disseminate clear prescribing guidelines on prudent AMU.
Antimicrobial use (AMU) in livestock production has beneficial impacts on animal health and welfare, and on household livelihoods, food security, and food safety (1, 2). However, there is increasing concern about the role of livestock production in the emergence of antimicrobial resistance (AMR) and consequent human exposure to resistant pathogens and/or antibiotic residues through the food chain, direct contact with livestock, or indirectly, via a contaminated environment (3–6). The loss of antibiotic efficacy due to AMR is a global public health challenge and a complex problem driven by many interconnected biological and socio-economic factors. Consequently, isolated interventions and non-coordinated actions may have limited impact on its management. Instead, effective mitigation of AMR risks requires dialogue and coordinated engagement between stakeholders from public and private sectors along the animal and antibiotics (ABX) value chains, implicating veterinarians, public health scientists, microbiologists, environmental scientists (ecologists), agricultural/forestry scientists, and epidemiologists (2, 7–9). Broader regulatory oversight is required, including of importation, distribution, sale, and use (7, 10). This regulatory complexity is part of a quintessential One Health (OH) approach implying the need to coordinate action across human, animal and environmental settings.
In the animal setting, veterinarians are key stakeholders in terms of diagnosis and treatment decisions for livestock. Yet, the international evidence on veterinary antimicrobial stewardship (AMS) is conflicting. Even in developed countries like Australia, small companion animal veterinarians reported prescribing broad-spectrum ABX of higher importance to human health more frequently than was the case for livestock veterinarians (11). The same study observed that the cost of bacterial culture to identify the causative agent, antimicrobial susceptibility testing (AST), and the lack of access to rapid and affordable diagnostics were barriers to appropriate ABX prescribing. A systematic review for non-clinical factors influencing veterinarians' prescribing behavior of ABX (12) indicated that fear of possible complications or losing customers if ABX were not prescribed (identified in 19 out of 34 studies), self-confidence (19/34), business factors (19/34), and complacency (16/34) are influencing veterinarians' decisions. Other influencing factors were; lack of awareness of animal owners regarding AMS (16/34) and demand for ABX (12/34), lack of appropriate regulations (10/34), cost and time for culture and AST (10/34), and inadequate farm hygiene (8/34) (12) with AMU as a “quick fix” to cover for poor hygiene and biosecurity practices (13).
There are conspicuous evidence gaps in low and middle-income countries (LMICs), where pharmaceutical regulation continues to be weak and diagnosis hampered by poor access to laboratory tests, poor training, negligible awareness, and lack of biosecurity measures (12, 14). Other factors influencing AMU are a higher burden of animal diseases such as mastitis in dairy cattle (15, 16). Identifying and understanding these barriers and drivers is important for designing strategies for rationalizing AMU in livestock production (12). A survey of Nigerian veterinarians revealed that only 21% were able to define the term “antimicrobial stewardship,” and 60% were unaware of the National Action Plan guidelines for AMR. More than half perceived prophylactic AMU as appropriate under poor farm biosecurity, and only 20% frequently conducted AST before deciding to administer ABX for treatment (17). A similar situation pertains in known global AMR hotspots, such as China and India, where livestock production is projected to grow in line with income growth and consumption preferences (18), and where there is an urgent need to evaluate the feasibility and acceptability of veterinary AMU control measures.
Accordingly, this study aimed to assess factors influencing antimicrobial prescribing behavior of a sample of veterinarians in Assam, India, where access to medicines is poorly regulated (19–21). The output of this study would inform the design of potential AMR control interventions, and to bridge the gap between prescribing guidelines and clinical usage. The research builds on evidence indicating that Indian veterinarians liberally prescribed ABX for animal cases based on the initial diagnosis, and that there is no strong relationship with farmers to ensure active involvement of stakeholders in more rational AMU (7, 9, 19, 22).
A purposive sampling method was used to interview veterinarians from Kamrup, Nagaon, Dhubri, Mangaldloi, and Dhemaji districts of Assam and from the state capital Guwahati. Contact details of veterinarians were obtained from the Animal Husbandry and Veterinary Department (AHVD). Due to COVID-19 restrictions, it was not possible to conduct face-to-face interviews, so all interviews were conducted by telephone; 100% of veterinarians in the list had telephone number. A structured questionnaire was used to collect socio-demographic data on veterinarians, and further information was collected on livestock health management, the most prevalent livestock health problems, factors influencing AMU and understanding of AMR, and potential interventions (the survey questionnaire is available as Supplementary Material 1). Questions used a 3-point Likert scale to assess levels of (dis)agreement with statements (1 = Disagree, 2 = Neutral, 3 = Agree and 99 = Don't know), and a 5-point Likert scale to rank items in order of importance (1 = Not important; 2 = Slightly important; 3 = Fairly important; 4 = Important; 5 = Very important). The survey also used open-ended questions probing ABX use and veterinarians' awareness and understanding of opportunities for reducing AMU in livestock production.
The questionnaire was piloted with five veterinarians working at the College of Veterinary Science, Assam Agricultural University. It was developed in English and conducted by dual lingual English/Assamese speaking members of the research team. The questionnaire was the only data collection tool used for this study.
The enumerators filled in hard copies of the questionnaire during the telephone call to avoid any recall bias. Data were stored electronically in a Microsoft Excel database and anonymised for further analysis. Statistical analyses were conducted using Excel and SPSS Statistics v24.0 (IBM SPSS Statistics for Windows Version 24.0, New York: IBM Corp). The Likert scale questions were analyzed using mean and mode values, and standard deviations. Mean values were used to summarize questions to which most respondents agreed or disagreed (23). Verbatim responses for some open-ended questions were summarized without rephrasing.
The characteristics of veterinarians participated in this survey (n = 50) are summarized in Table 1. The average age was 27.96 (SD = 4.63) years and the number of males (56%) was higher than females (44%). A high proportion (64%) had 3–10 years of experience and the majority (86%) were working for the AHVD, Government of Assam. Only 4% reported selling veterinary health products in addition to providing other veterinary services, probably in private clinics. Almost all (98%) veterinarians reported that they didn't have a written policy for the use of veterinary health products, and 58% have no diagnostic facilities in their clinics. The distance to the nearest diagnostic facility ranged from 0.2 to 40 km with an average of 2.91 km and a mode of 1 km.
In cattle, parasitic diseases (PD), mastitis, Foot and Mouth Disease (FMD), and Lumpy Skin Disease (LSD), were reported as the most prevalent diseases by 74, 50, 44, and 40% of veterinarians, respectively. In buffaloes, FMD and ketosis were reported by 16 and 12% of veterinarians, respectively. In goats, PD, Peste des petits ruminants (PPR), Listeriosis and Orf were reported by 42, 40, 24, and 24% of veterinarians, respectively. In pigs, FMD and PD were reported by 16 and 10% of veterinarians, respectively (Supplementary Table 1). The top five health problems in poultry were Newcastle disease (ND), E. coli/Colibacillosis, Salmonellosis, Infectious Bursal Disease (IBD), and Fowl Pox reported by 64, 20, 12, 10, and 10% of veterinarians, respectively (Supplementary Table 2). Respondents suggested a range of preventive measures for prevalent diseases and health conditions in different animal species, Supplementary Table 3. Regular vaccination was highly recommended for FMD in cattle, PPR in goat, Classical Swine Fever (CSF) in pigs, and ND in poultry by 48, 40, 48, and 64% of respondents, respectively. Deworming was recommended for PD in cattle, buffaloes, goat and pigs by 68, 16, 40, and 10% of veterinarians, respectively. Proper management was highly recommended for the prevention of mastitis in cattle by 28% of respondents.
The average daily number of cases investigated by a veterinarian was highest in poultry 12.32 (Median = 4, SD = 19.17) followed by cattle 6.34 (Median = 4, SD = 6.23), Table 2. In addition to treatment of diseased animals, veterinarians participated in other activities such as awareness campaigns/programmes for farmers (58%), insurance (36%), castration (18%), and artificial insemination 12%.
Almost all respondents (96%) stated that they prescribe ABX for animals with health problems. The percentage of veterinarians and the proportion of cases per animal species for which ABX were prescribed are shown in Figure 1 (veterinarians were asked “out of 10 cases for how many do you prescribe ABX?”). In cattle, over the 3 months prior to the interviews a high proportion of veterinarians (88%) reported using ABX for respiratory health problems, followed by mastitis (82%). The average number of cases of gastrointestinal tract infections (42.58) and mastitis (14.59) were higher in cattle compared with other animal species. The highest average number of cases of lameness was in buffaloes (34.50), Table 3. Ceftriaxone, Enrofloxacin, and Oxytetracycline were the top ABX reportedly prescribed by 76, 68, and 54% of veterinarians, respectively (Figure 2).
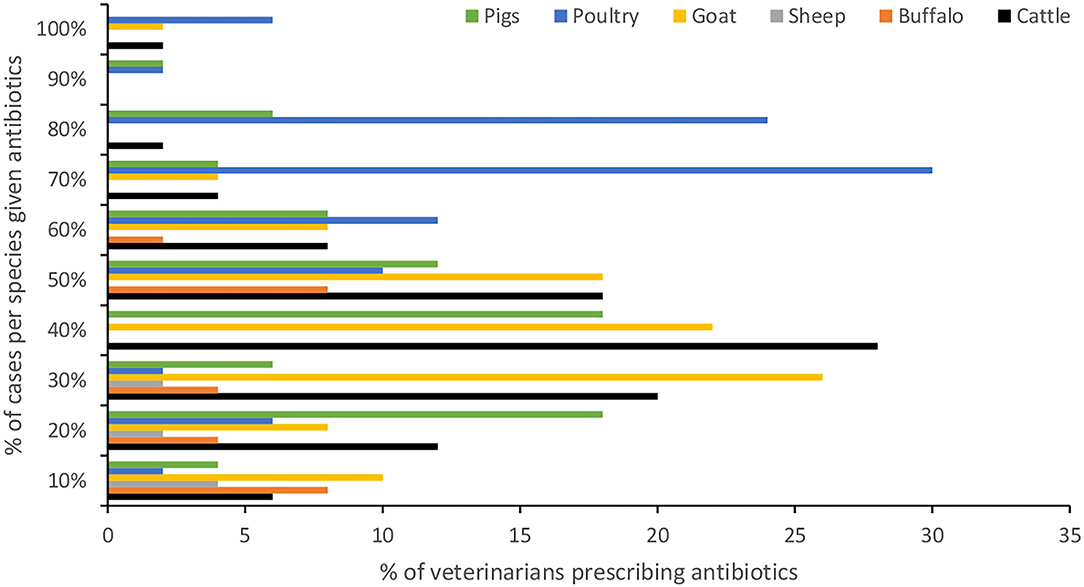
Figure 1. Proportion of cases of different animal species for which antibiotics were prescribed by veterinarians.
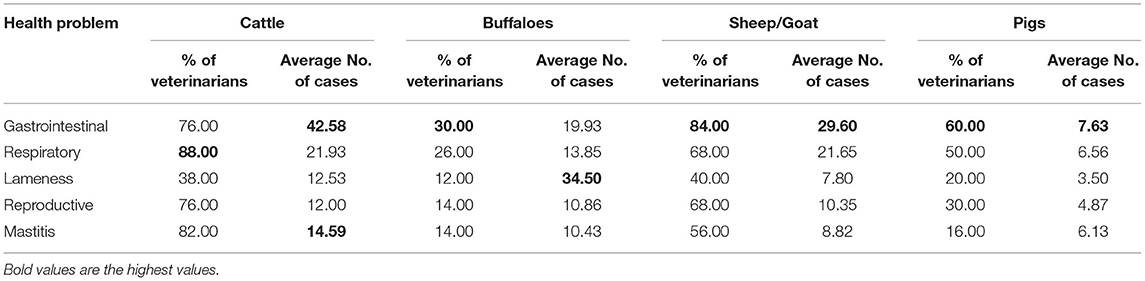
Table 3. Average number of cases for different health problems given antibiotics over the last 3 months.
Fifty six percent of veterinarians reported performing surgery for animals, of which 10.71% sometimes give ABX as prophylactic for 1–2 days before surgery. However, the majority of veterinarians (97.7%) reported always giving ABX post-surgery for 3–7 days with an average of 4.68 (SD = 0.98) days. Specific ABX reported as used before surgery were Enrox®, Cefotaxin®, Xyrofur®, Ciprofloxacin, Amoxycillin, and Intacef-Tazo®. Less than one third of veterinarians reported conducting AST and taking samples for bacterial culture before AMU. Disease condition/severity of clinical symptoms, results of laboratory diagnosis, economic status of the animal owner, and withdrawal period were reported as very important factors influencing decision for prescribing ABX by 52, 62, 54, and 46% of veterinarians, respectively (Figure 3 and Supplementary Table 4). The main factors for calculating the dose of ABX (Figure 4 and Supplementary Table 4) were animal weight, severity of illness, and animal age. Only one veterinarian indicated that all of his clients complete the recommended course of ABX, while 26% of veterinarians indicated 70% of their clients complete the recommended course of ABX.
All veterinarians believed that ABX are effective and indicated that they have heard about AMR. The main source of their knowledge about AMR was from their undergraduate (BVSc) and postgraduate courses (MVSc/PhD). More than half of participants believe that it is possible to raise livestock without AMU, and 77% stated they prescribe alternatives to ABX; while 23% claimed that ABX alternatives are not easily available. Veterinarians' perceptions of AMU and AMR are summarized in Figure 5 and Supplementary Table 5. All veterinarians agreed with the statement that AMR is a major human and animal health problem caused by over use and/or improper use of ABX.
Less than two thirds (64%) of veterinarians were aware of the government ban for Colistin. The main reasons understood for the ban, amongst, amongst those who were aware of it, (Table 4) were “Due to development of resistance” (28%) and “To prevent AMR and Colistin is the ABX of last resort, so if humans become resistant to this there will be no ABX left to treat” (18.75%). Only 2% of respondents stated they are aware of a national and/or a state policy plan for AMU in livestock.
Continued education (for veterinarians, para veterinarians, and farmers), disease eradication, improving animal housing, and restricting unnecessary treatments were ranked as very important measures to control the excess AMU in livestock production by the majority of participants (Figures 6, 7, and Supplementary Table 6). Among others, central government, state governments, and veterinarians were ranked as very important key stakeholders to control the excess AMU, Figures 8, 9, and Supplementary Table 6.
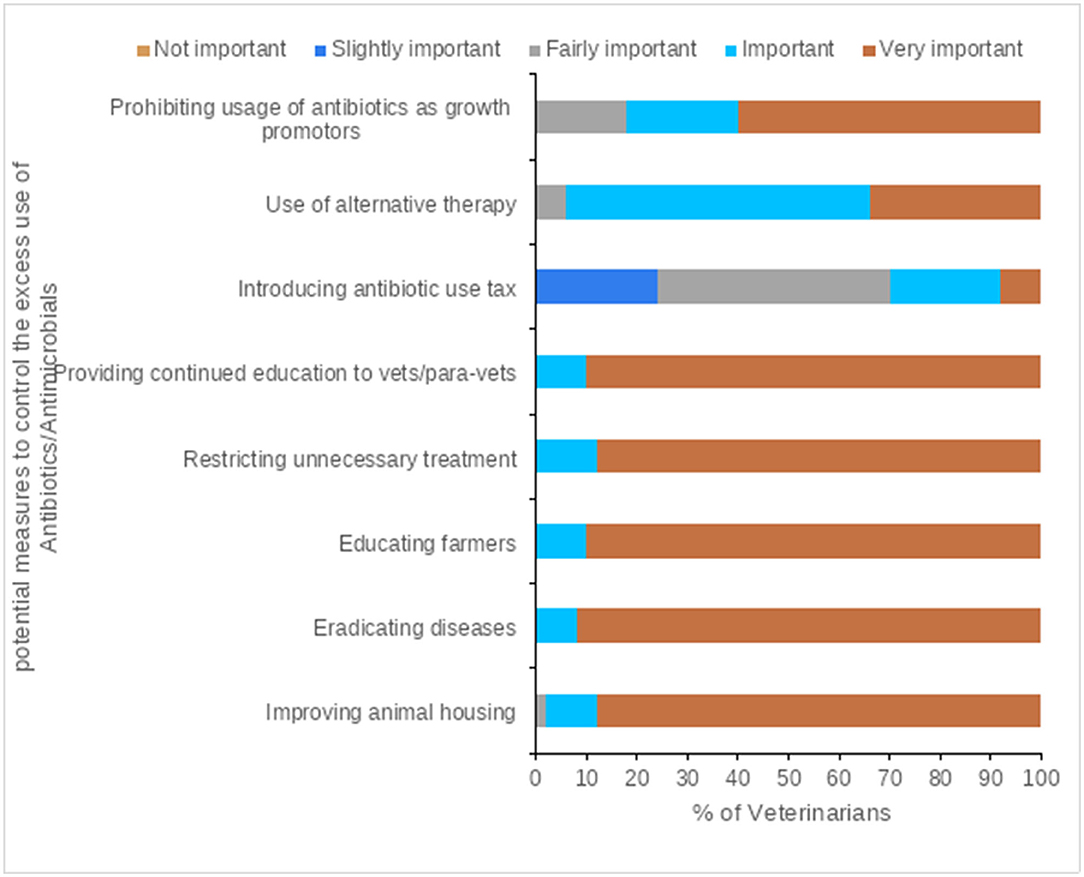
Figure 6. Veterinarians' attitudes to the potential measures to control the excess use of Antibiotics/Antimicrobials.
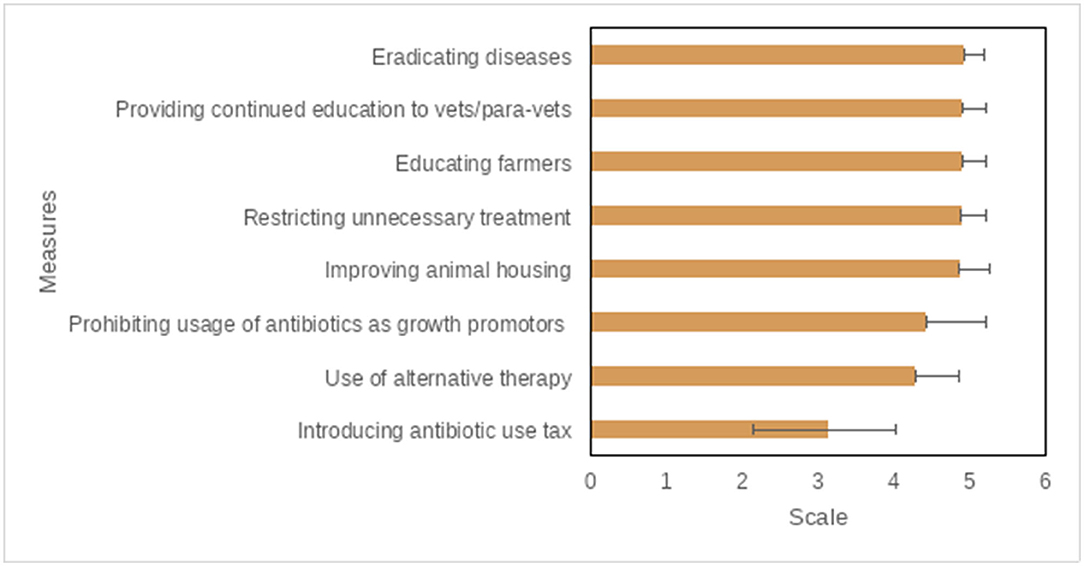
Figure 7. Potential measures to control the excess use of antibiotics/antimicrobials, questions were scored on a 5-point Likert scale (1 = Not important; 2 = Slightly important; 3 = Fairly important; 4 = Important; 5 = Very important), the mean score is displayed here from lowest to highest.
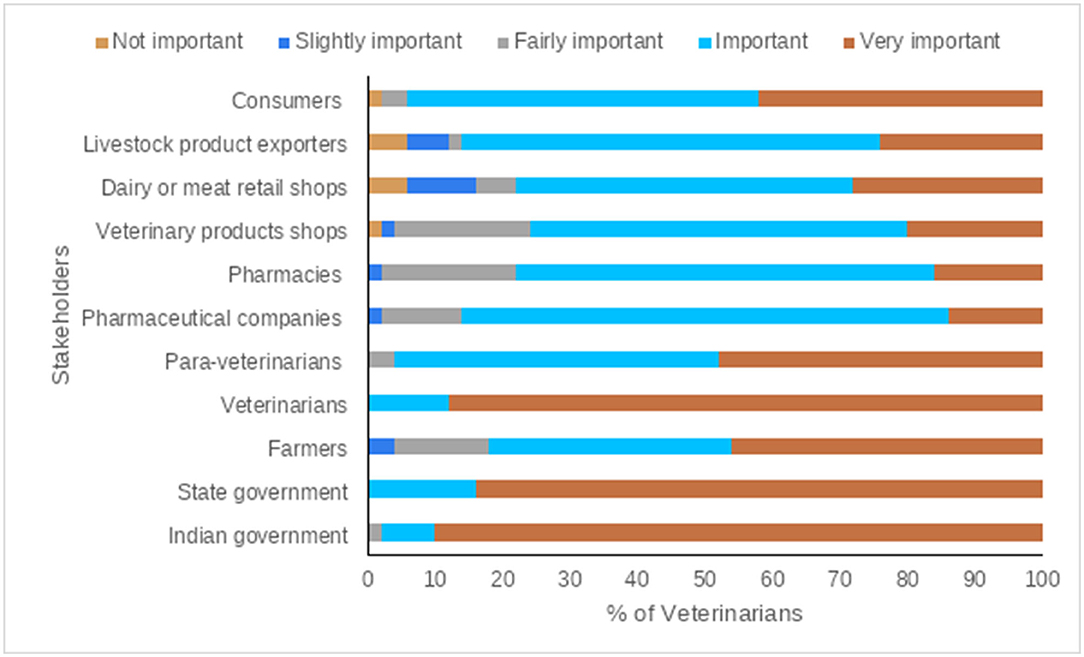
Figure 8. Veterinarians' opinions of the main stakeholders in the control the excess use of Antibiotics/Antimicrobials.
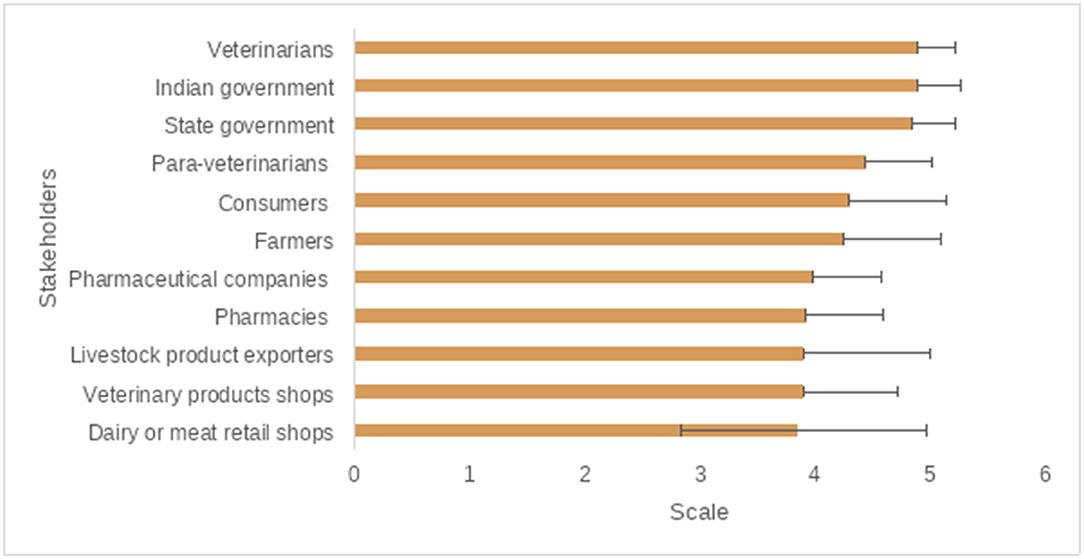
Figure 9. The main/key stakeholders to control the excess use of antibiotics/antimicrobials, questions were scored on a 5-poinet Likert scale (1 = Not important; 2 = Slightly important; 3 = Fairly important; 4 = Important; 5 = Very important), the mean score is displayed here from lowest to highest.
Veterinarians suggested potential prophylactic measures for animal diseases to be able to raise animals without AMU, Table 5. The most frequently mentioned measures were vaccination, deworming, hygiene, and biosecurity, suggested by 88, 40, 32, and 28% of veterinarians, respectively.
The main suggestions to reduce ABR/AMR among the farming community (Table 6) were: farmers should consult veterinarians for any diseased animal (34%), complete the course of treatment (34%), and pay more attention to farm hygiene, sanitation, and management (20%). Other actions included establishment of diagnostic labs, using ABX alternatives, and proper animal nutrition.
Only 26% of veterinarians reported having attended at least one seminar/training workshop related to AMU in livestock and AMR since graduation from veterinary school. Training providers were mostly government organizations including AHVD of Assam, universities and research centers. Only one veterinarian was willing to keep a record of the veterinary health products prescribed for animals, for a 3 months prospective study, though 50% said they were possibly willing to participate.
The survey results indicate a lack of awareness of the national and/or state policy/plan, despite the existence of a national action plan for AMR (NAP-AMR 2017–2021),1 which among other aims seeks to improve “awareness and understanding of AMR through effective communication, education and training.” In Assam, the AHVD has a Professional Efficiency Development scheme to regulate veterinary practices according to the Indian Veterinary Council Act, 1984. The Council is also responsible for the development of training modules and continued training of field veterinarians. Another project, “Assistance to States for Control of Animal Diseases,” is also supporting the training needs of veterinarians, para-veterinarians as well as laboratory persons. However, the extent of AMU training and awareness in these is unclear and there is a need to improve collaboration between different organizations such as veterinary colleges and the AHVD (15, 19, 25), and for them to be aligned with the objectives of the NAP. Despite this, only 26% of the survey respondents reported having attended at least one training/awareness seminar since graduating however, suggesting that opportunities for continued professional development (CDP) are limited. Less than two thirds (64%) of participants were aware of the government ban for Colistin and the reasons for this decision in their opinions were varied. The verbatim responses (Table 4) showed a potential confusion or lack of understanding over whether it is human/animals who developed resistance to the antibiotics or the pathogens. Veterinarians might have used “animal/humans resistance” as a proxy or indicator for not responding to treatment with ABX. Core competencies among veterinarians have been found to be lacking or inefficient and it has been suggested that training and attending national and international seminars/workshops are appropriate ways to acquire competencies (26). There is a continuing education and training needs for veterinary students, working veterinarians, para-veterinarians and other stakeholders for which online and open and distance learning programmes in animal welfare need to be developed (27). In India and other LMICs with limited resources, private sector and non-governmental organizations (NGOs) could play an important role to support continuous education and training of veterinarians. “Vet Sustain” is an example of a UK-based social enterprise working to enable and inspire veterinary professionals to continually improve the health and wellbeing of animals, people and the environment. It is also supporting veterinary professionals to drive change toward a more sustainable future and to become leading forces for sustainability.2 Guidelines, provided by NGOs such as the British Veterinary Association, the British Small Animal Veterinary Association, and the British Cattle Veterinary Associations, have been considered a key step for appropriate AMU (28, 29). Such activities provide opportunities for keeping stakeholders up to date with the latest government advice and regulation, better ways to support training and CPD in India using a similar model could be investigated.
As found in previous studies (11, 30–32), low levels of laboratory diagnosis for animal diseases continues to be a factor in speculative AMU, and arises due to a lack of onsite diagnostic facilities. In this study, 58% of veterinary clinics have no diagnostic laboratories and 70% of veterinarians never use AST before AMU. The AHVD has a scheme for assisting states to set up infrastructure for new veterinary hospitals and dispensaries and to strengthen/equip the existing ones.3 However, coverage and access are still not universal for all states. In 2015–16, the contribution by the central government was increased from 60 to 90% for 11 states (8 North-East and 3 Himalayan states) which may improve the veterinary services in Assam. There are disease diagnostic laboratories only at the state and district level. A field veterinarian who wants to conduct basic tests has to send samples to these laboratories, which is time consuming. Hence, equipping the veterinary clinics and dispensaries with basic equipment including microscopes, on-farm diagnostic kits and other tools for screening some of the diseases will help field veterinarians to diagnose quickly and to prescribe appropriate ABX based on confirmed infection instead of depending on clinical signs alone. A survey of animal health professionals in 20 sub-Saharan African countries concluded that the development of on-farm diagnostics and management tools for animal diseases are essential to considerably improve AMU (32).
Respondents in this study reported that farmers often call and/or consult them only after trying other options. This can lead to the progression of health problems that are less likely to respond to medications and more likely to develop resistance. Non-responsive cases also drives a lack of confidence between farmers and veterinarians (15). This behavior might be due to the shortage of veterinarians in Assam; there are around 1,000 veterinarians but the required number is estimated at 2,529 (one veterinarian per 5,000 cattle head) according to the National Commission of Agriculture.4 Ethnographic work with farmers in Assam (conducted under this project but yet to be published) identified lack of access to veterinarians and veterinary services as a major barrier to proper management of animal health; farmers in peri-urban villages such as Garchuk and Nagaom around Guwahati reported that veterinarians were reluctant to make in-person diagnoses due the time taken to travel to and from remote farms. This suggests that access—to veterinarians in general and, when veterinarians are available to their access to laboratories—is a serious issue that needs to be further addressed. A shortage of veterinarians results in over prescription and/or irrational AMU by untrained caregivers or informal prescribers, known as “private doctors” among Indian dairy farmers (19). In India, like many other LMICs, veterinarians are not the only prescribers of ABX for animal use. Para-veterinarians and other untrained community members might be more accessible, charging less for consultations compared to veterinarians. Over-the-counter access of ABX, without prescriptions, and direct marketing of drugs to farmers are also common practices in India (15).
In Assam, the most frequently observed diseases in cattle, goats, and poultry are potentially associated with the lack of hygiene, biosecurity, and non-adherence to the vaccination schedule for endemic diseases. A high proportion of veterinarians reported AMU for cattle with respiratory health problems, mostly caused by viral infections, followed by mastitis. This was also reported in a previous study that identified AMU mostly for mastitis cases (15). This could be prevented by improving environment and animal hygiene, prober nutrition and dry cow therapy (33). Veterinarians are prescribing ABX listed as highest priority, critically important antimicrobials (HPCIA) by the World Health Organization (WHO). This confirms the results of previous studies, in India and other LMICs, in which veterinarians used Quinolones and 3rd generation Cephalosporins for animal treatment (9, 10). In India, 76.8 and 47.8% of veterinarians were found to prescribe Quinolones and 3rd generation Cephalosporins for dairy farms (9).
Among many factors influencing veterinarians' decisions for AMU, the economic status of livestock owners was a significant determinant, with veterinarians assessing the ability of farmers to pay before prescribing ABX. In Bangladesh, it was found that the farmer's economic condition highly influenced the selection of ABX for treatment of livestock and poultry (31). Such subjective assessments are common in veterinary practice where prescription has been shown to be determined by perceived ease of administration and compliance, willingness of pet owners to give ABX, as well as animal characteristics (24). Cost of ABX was typically a factor in areas of varying socioeconomic status (24). We also found that the manufacturer's instructions were ranked as “very important” in calculating the dose of ABX by only 6% of respondent veterinarians. Other studies have also identified non-adherence to manufacturers' instructions as a reason for indiscriminate AMU in the agriculture sector (34). These findings contradict the observations in Bangladesh where drug instructions had a high-to-moderate influence on AMU (31).
Our results indicated that all respondents agreed that AMR is a major human and animal health problem caused by over use and/or improper AMU. However, in practice veterinarians are still prescribing ABX without prober laboratory diagnosis or AST. As discussed above this is due to the lack of on-site diagnostic facilities. These findings are similar to those from other LMICs such as Bangladesh (31) but contradict observations in developed countries where the majority of veterinarians followed AST before AMU (30, 35). However, availability and affordability of diagnostic tools and other facilities are different in developed and LMICs. Veterinarians suggested a wide range of preventive measures like proper animal nutrition, hygiene, and vaccination for the most frequently occurring animal diseases in the study area. This would result in reducing AMU and AMR in livestock production. They also identified key stakeholders responsible for implementing these prophylactic measures. However, they were not willing to participate in future work aiming to collect qualitative and quantitative data for AMU in animals. This is due to the lack of strict guidelines and regulations of AMU and having no time to keep records. As indicated in the results, in addition to the treatment of diseased animals, veterinarians are burdened with many other tasks as conducting extension services on animal production and health, implementing various government schemes, and running surveillance. Veterinarians' negative attitude toward keeping records for AMU may be due to the difficulties of being able to adhere to recommendations and guidelines if they did; they are not unaware of the dangers of inappropriate AMU but face very real barriers to improving practice. Further studies are required to understand the reasons behind veterinarians' negative attitudes toward keeping medical records and how better AMU can be supported. Unfortunately, it was impossible to do so due to COVID-19 restrictions but future research should use ethnographic assessments and qualitative research methods such as focus group discussions and in-depth interviews with veterinarians and farmers to properly address the problem and co-design solutions. Mixed methods provide deep understanding of the pattern and reasons of AMU that would not be identified using quantitative surveys alone (36, 37).
This study sought to provide insights on prescribing behavior and opinions of veterinarians regarding AMU and AMR. Although veterinarians are aware of AMR risks, the lack of diagnostic facilities in most veterinary clinics means that most prescribe ABX based on clinical symptoms. They are unaware of the existing national and state level regulations, guidelines, and strategies for AMR. Furthermore, there is a need for improved communication between policy makers and field veterinarians to bridge a gap between prescribing guidelines and clinical usage. Future initiatives should explore ways of better connecting all stakeholders with policy makers to drive the uptake and evaluation of key regulatory messages associated with key policies. To moderate AMU in livestock production in India and other LMICs with similar production systems, strategies should focus on: (1) enhancing communication and regular dissemination of updated AMU guidelines between relevant stakeholders; (2) CPD for veterinarians and other key stakeholders; and (3) provision of affordable and accessible veterinary services. In designing interventions to meet these objectives, attention need to be paid to the evaluation of their effectiveness. There is currently a conspicuous gap in the evidence on what works in different animal health systems including the role of veterinarians in the diagnostic, prescribing and treatment process. This is a significant challenge in under regulated dispensary settings in LMICs.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Human Ethical Review Committee (HERC), Royal (Dick), School of Veterinary Studies, The University of Edinburgh (Ref No. HERC_673_21). Local ethical approval was not acquired as there was no Ethical Committee for social science research in our partner's institute. However, a permission from the head of the Animal Husbandry and Veterinary Department (AHVD) in Assam to interview veterinarians. As interviews were conducted via telephone calls, oral consents were obtained after assurance of confidentiality and anonymity of respondents (University of Edinburgh).
ME contributed to the concept, survey design, data analysis, and writing up. JC, GG, and AT contributed to the research design and editing of article. BS and HS participated in preparing questionnaires and editing the article. BD piloted the questionnaires and collected the necessary data from the respondents. MH and BS provided the necessary logistics and overall supervision for executing the work. DM contributed to the concept and proof reading. All authors contributed to manuscript revision, read, and approved the submitted version.
This work was funded by the UK Newton Fund awards co-funded by the Economic and Social Research Council grant numbers ES/S000186/1 and the Department of Biotechnology (DBT), Government of India (BT/IN/Indo-UK/AMR/06/BRS/2018-19). For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer SK declared a shared affiliation, though no other collaboration, with one of the author MH to the handling Editor.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank all participating veterinarians who took the time to answer the questionnaire evaluated here and who are participants in the piloting. Many thanks also to the Animal Husbandry and Veterinary Department of Assam.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2022.864813/full#supplementary-material
1. ^https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/national-action-plan-on-amr-(india).pdf?sfvrsn=9f396e90_1&download=true
3. ^“Establishment and Strengthening of Veterinary Hospital and Dispensaries”. Available online at: https://animalhusbandry.assam.gov.in/projects/livestock-health-and-disease-control-lhdc-programme
4. ^https://animalhusbandry.assam.gov.in/portlets/strategy-papers-of-ah-veterinary-department (Strategy Papers on Manpower & Human Resource Rationalization).
1. Rushton J, Ferreira JP, Stärk KD. Antimicrobial Resistance: The Use of Antimicrobials in the Livestock Sector. OECD Food, Agriculture and Fisheries Papers, No. 68, OECD Publishing. (2014). doi: 10.1787/5jxvl3dwk3f0-en
3. Angulo FJ, Collignon P, Wegener HC, Braam P, Butler CD. The routine use of antibiotics to promote animal growth does little to benefit protein undernutrition in the developing world. Clin Infect Dis. (2005) 41:1007–13. doi: 10.1086/433191
4. Ibrahim M, Ahmad F, Yaqub B, Ramzan A, Imran A, Afzaal M, et al. Current trends of antimicrobials used in food animals and aquaculture. Antibiot Antimicrob Resist Genes Environ. (2020) 1:39–69. doi: 10.1016/B978-0-12-818882-8.00004-8
5. Landers TF, Cohen B, Wittum TE, Larson EL. A review of antibiotic use in food animals: perspective, policy, and potential. Public Health Rep. (2012) 127:4–22. doi: 10.1177/003335491212700103
6. Turnidge J, Christiansen K. Antibiotic use and resistance–proving the obvious. Lancet. (2005) 365:548–9. doi: 10.1016/S0140-6736(05)70770-4
7. Kumar V, Gupta J, Meena H. Assessment of awareness about antibiotic resistance and practices followed by veterinarians for judicious prescription of antibiotics: an exploratory study in eastern Haryana region of India. Trop Anim Health Prod. (2019) 51:677–87. doi: 10.1007/s11250-018-1742-0
8. Magouras I, Carmo LP, Stärk KD, Schüpbach-Regula G. Antimicrobial usage and-resistance in livestock: where should we focus? Front Vet Sci. (2017) 4:148. doi: 10.3389/fvets.2017.00148
9. Vijay D, Bedi JS, Dhaka P, Singh R, Singh J, Arora AK, et al. Knowledge, Attitude, and Practices (KAP) Survey among veterinarians, and risk factors relating to antimicrobial use and treatment failure in dairy herds of India. Antibiotics. (2021) 10:216. doi: 10.3390/antibiotics10020216
10. Poupaud M, Putthana V, Patriarchi A, Caro D, Agunos A, Tansakul N, et al. Understanding the veterinary antibiotics supply chain to address antimicrobial resistance in Lao PDR: roles and interactions of involved stakeholders. Acta Trop. (2021) 220:105943. doi: 10.1016/j.actatropica.2021.105943
11. Norris JM, Zhuo A, Govendir M, Rowbotham SJ, Labbate M, Degeling C, et al. Factors influencing the behaviour and perceptions of Australian veterinarians towards antibiotic use and antimicrobial resistance. PloS ONE. (2019) 14:e0223534. doi: 10.1371/journal.pone.0223534
12. Servia-Dopazo M, Taracido-Trunk M, Figueiras A. Non-clinical factors determining the prescription of antibiotics by veterinarians: a systematic review. Antibiotics. (2021) 10:133. doi: 10.3390/antibiotics10020133
13. Willis LD, Chandler C. Quick fix for care, productivity, hygiene and inequality: reframing the entrenched problem of antibiotic overuse. BMJ Glob Health. (2019) 4:e001590. doi: 10.1136/bmjgh-2019-001590
14. Grace D. Review of Evidence on Antimicrobial Resistance and Animal Agriculture in Developing Countries. (2015). doi: 10.12774/eod_cr.june2015.graced
15. Mutua F, Sharma G, Grace D, Bandyopadhyay S, Shome B, Lindahl J. A review of animal health and drug use practices in India, and their possible link to antimicrobial resistance. Antimicrob Resist Infect Control. (2020) 9:103. doi: 10.1186/s13756-020-00760-3
16. Verma H, Rawat S, Sharma N, Jaiswal V, Singh R, Harshit V. Prevalence, bacterial etiology and antibiotic susceptibility pattern of bovine mastitis in Meerut. J Entomol Zool Stud. (2018) 6:706–9. Available online at: https://www.entomoljournal.com/archives/2018/vol6issue1/PartJ/5-6-93-641.pdf
17. Adekanye UO, Ekiri AB, Galipó E, Muhammad AB, Mateus A, La Ragione RM, et al. Knowledge, Attitudes and practices of veterinarians towards antimicrobial resistance and stewardship in Nigeria. Antibiotics. (2020) 9:453. doi: 10.3390/antibiotics9080453
18. Van Boeckel TP, Pires J, Silvester R, Zhao C, Song J, Criscuolo NG, et al. Global trends in antimicrobial resistance in animals in low-and middle-income countries. Science. (2019) 365:eaaw1944. doi: 10.1126/science.aaw1944
19. Chauhan AS, George MS, Chatterjee P, Lindahl J, Grace D, Kakkar M. The social biography of antibiotic use in smallholder dairy farms in India. Antimicrob Resist Infect Control. (2018) 7:60. doi: 10.1186/s13756-018-0354-9
20. Nye C, Watson T, Kubasiewicz L, Raw Z, Burden F. No prescription, no problem! A mixed-methods study of antimicrobial stewardship relating to working equines in drug retail outlets of Northern India. Antibiotics. (2020) 9:295. doi: 10.3390/antibiotics9060295
21. Laxminarayan R, Chaudhury RR. Antibiotic resistance in India: drivers and opportunities for action. PLoS MED. (2016) 13:e1001974. doi: 10.1371/journal.pmed.1001974
22. Thulasiraman Parkunan MA, Sukumar B, Chera JS, Ramadas S, Chandrasekhar B, Kumar SA, et al. Antibiotic resistance: a cross-sectional study on knowledge, attitude, and practices among veterinarians of Haryana state in India. Vet World. (2019) 12:258–65. doi: 10.14202/vetworld.2019.258-265
23. Hopman NE, Mughini-Gras L, Speksnijder DC, Wagenaar JA, Van Geijlswijk IM, Broens EM. Attitudes and perceptions of Dutch companion animal veterinarians towards antimicrobial use and antimicrobial resistance. Prev Vet Med. (2019) 170:104717. doi: 10.1016/j.prevetmed.2019.104717
24. Mateus AL, Brodbelt DC, Barber N, Stärk KD. Qualitative study of factors associated with antimicrobial usage in seven small animal veterinary practices in the UK. Prev Vet Med. (2014) 117:68–78. doi: 10.1016/j.prevetmed.2014.05.007
25. Rao SE, Natchimuthu K, Ramkumar S, Sasidhar P. Improving the delivery of veterinary services in India. Rev Sci Tech. (2015) 34:767–77. doi: 10.20506/rst.34.3.2394
26. Sasidhar P, Suvedi M. Assessment of the core competencies of veterinarians: implications for policy decisions in India. Rev Sci Tech. (2018) 37:785–95. doi: 10.20506/37.3.2885
27. Sasidhar P, Jayasimha N. Scope for animal welfare education in open and distance learning: findings from a needs assessment study in India. Rev Sci Tech. (2015) 34:689–97. doi: 10.20506/rst.34.3.2389
28. Mateus A, Brodbelt D, Stärk K. Evidence-based use of antimicrobials in veterinary practice. Practice. (2011) 33:194–202. doi: 10.1136/inp.d2873
29. Vilen A. Antimicrobial FECAVA Initiative. Making the responsible use of antimicrobials work in clinical practice. Eur J Comp Anim Pract. (2013) 23:31–36. Available online at: https://www.fecava.org/wp-content/uploads/2019/09/Winter-2013.pdf#page=31
30. Fowler H, Davis M, Perkins A, Trufan S, Joy C, Buswell M, et al. Survey of veterinary antimicrobial prescribing practices, Washington State (2015). Vet Rec. (2016) 179:651. doi: 10.1136/vr.103916
31. Kalam M, Rahman M, Alim M, Shano S, Afrose S, Jalal FA, et al. Knowledge, attitudes, and common practices of livestock and poultry veterinary practitioners regarding the AMU and AMR in Bangladesh. Antibiotics. (2022) 11:80. doi: 10.3390/antibiotics11010080
32. Tebug SF, Mouiche MMM, Abia WA, Teno G, Tiambo CK, Moffo F, et al. Antimicrobial use and practices by animal health professionals in 20 sub-Saharan African countries. Prev Vet Med. (2021) 186:105212. doi: 10.1016/j.prevetmed.2020.105212
33. Zigo F, Vasil M, Ondrašovičová S, Výrostková J, Bujok J, Pecka-Kielb E. Maintaining optimal mammary gland health and prevention of mastitis. Front Vet Sci. (2021) 8:607311. doi: 10.3389/fvets.2021.607311
34. Manyi-Loh C, Mamphweli S, Meyer E, Okoh A. Antibiotic use in agriculture and its consequential resistance in environmental sources: potential public health implications. Molecules. (2018) 23:795. doi: 10.3390/molecules23040795
35. De Briyne N, Atkinson J, Pokludová L, Borriello S, Price S. Factors influencing antibiotic prescribing habits and use of sensitivity testing amongst veterinarians in Europe. Vet Rec. (2013) 173:475. doi: 10.1136/vr.101454
36. Mangesho PE, Caudell MA, Mwakapeje ER, Ole-Neselle M, Kimani T, Dorado-García A, et al. Knowing is not enough: a mixed-methods study of antimicrobial resistance knowledge, attitudes, and practises among maasai pastoralists. Front Vet Sci. (2021) 8:645851. doi: 10.3389/fvets.2021.645851
Keywords: antibiotics, antimicrobial resistance, livestock, veterinarians, prescribing, behavior
Citation: Eltholth M, Govindaraj G, Das B, Shanabhoga MB, Swamy HM, Thomas A, Cole J, Shome BR, Holmes MA and Moran D (2022) Factors Influencing Antibiotic Prescribing Behavior and Understanding of Antimicrobial Resistance Among Veterinarians in Assam, India. Front. Vet. Sci. 9:864813. doi: 10.3389/fvets.2022.864813
Received: 28 January 2022; Accepted: 22 March 2022;
Published: 26 April 2022.
Edited by:
Latiffah Hassan, Universiti Putra Malaysia, MalaysiaReviewed by:
Joseph O. Fadare, Ekiti State University, NigeriaCopyright © 2022 Eltholth, Govindaraj, Das, Shanabhoga, Swamy, Thomas, Cole, Shome, Holmes and Moran. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mahmoud Eltholth, TV9lbHRob2x0aEB5YWhvby5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.