
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Vet. Sci. , 30 November 2022
Sec. Veterinary Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fvets.2022.1004637
Tibial Plateau Leveling Osteotomy (TPLO) or Tibial Tuberosity Advancement (TTA) are commonly used surgical techniques for correction of cranial cruciate ligament (CCL) rupture in dogs. This systematic review aims to investigate whether one technique is superior to the other. Seventy-two studies on surgical management of CCL rupture have been identified and evaluated in regard of subjective and objective gait analysis criteria, development of osteoarthritis (OA), thigh circumference measurements, goniometry, joint stability, pain and complication rates. Almost half (47.2 %) of the studies were considered of low quality of evidence, leading to high heterogeneity in quality among studies; this posed a major limitation for an evidence-based systematic review of both surgical techniques. Out of 72 studies, there were only eleven blinded randomized clinical trials, of which five were rated with a low overall risk of bias. However, both techniques were considered to be successful management options. Subjective and objective gait analysis revealed no lameness at long-term evaluation for the majority of the patients. However, it appeared that TTA lead to better OA scores up to 6 months postoperatively, while TPLO had a lower rate of surgical site infections. In summary, no method can be clearly preferred, as most of the study evaluated were subpar. Studies with a high level of evidence are therefore urgently needed for such a common surgical procedure.
Cranial cruciate ligament (CCL) rupture is one of the most frequent causes for pelvic limb lameness in dogs (1) posing substantial economical and clinical consequences (2). The origin and development of CCL disease has been widely discussed in many studies (3–8). Currently, a variety of surgical treatment options have been developed, with Tibial Plateau Leveling Osteotomy (TPLO) and Tibial Tuberosity Advancement (TTA) being well established and frequently used surgical procedures (9, 10). Both techniques produce a biomechanical alteration and, thus, stabilization of the stifle joint (11, 12).
The clinical outcomes of TPLO and TTA have been studied and compared with respect to various clinical parameters (13). A previous systematic review (13) suggested that TPLO achieves better results in objective gait analyses in restoring limb function, while subjective gait analyses found no differences between TPLO and TTA. At first glance, the analysis of the multiple studies allows the hypothesis that TPLO is superior to TTA in terms of long-term clinical outcomes, although further research and systematic analyses of the data to date are needed to confirm this.
The outcome of stifle joint osteotomies can be assessed clinically and radiographically, while the occurrence or rate of complications can be used as an additional outcome measure. Clinically, the gait can be assessed with both subjective and objective criteria. The subjective evaluation is based on a scale ranging between severe (no-weight-bearing) to normal gait (14, 15). Objective gait evaluation is based on the force gait plate analysis (16). This approach is less prone to bias and allows objective assessment of even non-visible changes in gait (17). Functional outcome also includes thigh circumference measurements, goniometry, joint stability and pain as these parameters provide information on the joint's mobility (18–21).
Surgical intervention leads to radiographically detectable osteoarthritis (22–26). Osteotomies are highly invasive surgical procedures and carry the risk of multiple complications associated with functional limitations and the need of further therapy (27, 28). Hence, it is necessary to assess the complication rates and most common causes of complications with the aim to address them in the future.
This systematic review aims to compare TPLO and TTA with regard to various outcome criteria and to evaluate the most current studies (2016–2021) on both surgical techniques. Specifically, we hypothesize that:
• TPLO has a better functional outcome on subjective and objective gait analysis than TTA
• TPLO has a better radiographical outcome on osteoarthritis than TTA
• TPLO has a better functional outcome on thigh circumference measurements than TTA
• TPLO has a better functional outcome on goniometry than TTA
• TPLO has a better functional outcome on joint stability than TTA
• TPLO has a better functional outcome on pain than TTA
• TPLO results in less complications than TTA.
Several electronic databases have been searched to identify studies examining clinical outcomes of TPLO and/or TTA surgery. Search was performed from May 2021 until July 2021 using the terms “[cranial cruciate ligament AND (dog OR canine)] OR [cranial cruciate ligament AND (dog OR canine) AND surgery] OR [cranial cruciate ligament AND (dog OR canine) AND complication] OR [cranial cruciate ligament AND (dog OR canine) AND injury] OR [stifle AND surgery AND (dog OR canine)] OR (osteotomy AND stifle AND dog) OR” Tibial Plateau Leveling Osteotomy “OR” Tibial Tuberosity Advancement “OR Kreuzband Hund OR Kreuzbandriss Hund OR TPLO OR TTA.” Electronic databases included Pubmed, Web of Science, CAB Abstracts and the catalog of the library of the University of Veterinary Medicine Hannover.
A two-stage screening process was performed to identify studies for inclusion (29). Firstly, the search identified studies of relevance that seemed to fulfill inclusion criteria after screening titles and abstracts. Also, articles referenced in studies have been elected for further analysis. After searching databases, the full texts of the selected studies were examined in detail and included or excluded depending on the following criteria (stage 1):
• Type of study: Peer reviewed studies written in English or German, full text available, published between February 2016 and July 2021 were included. Clinical studies, case series, cohort studies, case reports, case-control studies and observational studies were included. Ex-vivo or experimental studies, literature reviews and studies with <5 subjects per group were excluded.
• Case definition: Patients diagnosed with CCL disease and eligible for surgery were included. Studies that investigated CCL disease plus any comorbidity were excluded whenever the second disease has been an obligatory inclusion criterion (e.g., dogs with amputated limbs plus CCL disease in another limb).
• Intervention: Only studies describing TTA or TPLO were included. Studies were excluded if dogs received another surgical procedure (e.g., combined TPLO and tibial tuberosity transposition).
• Outcome: Studies examining results on subjective lameness evaluation, objective lameness evaluation, osteoarthritis, thigh circumference measurements/muscle atrophy, goniometry, joint stability, pain and complications were included. Studies that did not differentiate between the results of each outcome parameter (e.g., using one score for several outcomes and not stating each outcome) were excluded.
Stage 2 consisted of a detailed evaluation of the studies' full texts regarding the studies' quality of evidence and treatment outcomes. Treatment outcomes have been evaluated as described in “Assessment of outcome measures.”
Several factors have been identified to contribute to the overall quality of evidence of each study. Assessment of quality of evidence has been performed for all included studies. Quality assessment is based on the study design (blinding, randomization, use of a control group), study group size, duration of the study, subject enrolment quality/disease characterization and the assessment of risk of bias.
Studies were categorized into three groups providing different quality of evidence. The first group (Group A) included blinded randomized clinical trials (bRCTs) and non-blinded randomized clinical trials (nbRCTs) and was considered to produce high quality of evidence (the bRCTS were considered as the studies with the highest quality of evidence). To meet conditions for Group A, studies have been examined on their level of blinding, methods of randomization and use of a control group. Clinical trials not fulfilling these conditions were categorized in Group B, i.e., non-randomized clinical trials (NRCTs) and uncontrolled clinical trials (UCTs). These studies were considered to produce less quality of evidence than bRCTs. The third group (Group C) includes case series (CS), case reports (CR), cohort studies (CoS), case-control studies (CCS), observational studies (ObS) and all other types of non-interventional studies. They are considered to produce the lowest quality of evidence.
Based on the study group sizes, studies were defined as “good” when >50 subjects per group, “moderate” when 20–50 subjects per group, “small” when 10–19 subjects per group and “very small” when <10 subjects per group were included (29). Studies with <5 subjects per group were excluded. Moreover, subject in terms of CCL surgery is defined as dogs enrolled in the study, not by knees that TPLO or TTA has been performed on. Bilateral surgery counts as one subject.
Outcome parameters were evaluated at different time frames following surgery. Study duration is defined as the time between surgery (t0) and last examination (t1). Studies were categorized as “short-term,” i.e., up to 8 weeks, “mid-term,” i.e., 8 weeks−6 months and “long-term,” i.e., >6 months.
Disease characterization was performed by confirming the rupture of the CCL. The subjects' enrolment quality was considered to be “well,” “fairly,” “poorly” or “unclear” based on the following examination:
• “well” = patients underwent clinical and orthopedic examination (lameness evaluation, cranial drawer test, tibial thrust) AND x-ray of the affected joint AND confirmation of the rupture via MRI or arthroscopy or arthrotomy
• “fairly” = patients underwent clinical and orthopedic examination (lameness evaluation, cranial drawer test, tibial thrust) AND x-ray of the affected joint
• “poorly” = patients underwent clinical and orthopedic examination (lameness evaluation, cranial drawer test, tibial thrust)
• “unclear” = no or indistinct information given on the confirmation of CCL rupture.
The risk of bias was addressed using the Cochrane Handbook for Systematic Reviews of Interventions tool (30). Potential sources of bias were selection bias (sequence generation, allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting) and other bias such as conflicts of interests. Each element was characterized as providing “high,” “moderate,” “unclear” or “low” risk of bias (scale: 3 = high risk of bias, 2 = moderate or unclear risk of bias, 1 = low risk of bias). These numbers were summed up to a total score and, hence, the studies were further categorized on the grounds of their overall risk of bias score:
• Score 7–9 = overall “low” risk of bias
• Score 10–12 = overall “low/moderate” risk of bias
• Score 13–15 = overall “moderate” risk of bias
• Score 16–18 = overall “moderate/high” risk of bias
• Score 19–21 = overall “high” risk of bias.
The outcome of TPLO or TTA surgery can be measured using the following parameters: gait analysis (subjective), gait analysis (objective), osteoarthritis, thigh circumference measurements, goniometry, joint stability, pain and complications. At least one of these parameters should have been assessed in each included study. The efficacy of TPLO and TTA was evaluated based on the aforementioned outcome criteria and the timing of the last examination (short-term, mid-term and long-term results; pre-operative vs. post-operative). One standardized scale was applied to each outcome criterion so that the results can be compared and evaluated in a homogenous process.
The following scale was used to assess the gait analysis in each study:
- 0 = no lameness
- 1 = mild lameness
- 2 = moderate lameness
- 3 = severe lameness
- 4 = non-weight bearing lameness.
The outcome was also characterized based on the time frame, i.e., short-term (up to 8 weeks) and mid-term (up to 6 months):
- No lameness (score </= 0.5)
- Improvement (in %) of a minimum of 50 % (as decrease in lameness score between preoperative and postoperative evaluation).
The objective gait analysis was performed (i) either on a force plate or pressure platform and ground reaction forces were expressed as peak vertical force and vertical impulse or (ii) on a static stance analyser and were expressed in percent of body weight on all four legs. The outcome was also characterized based on the time frame, i.e., short-term (up to 8 weeks) and mid-term (up to 6 months):
- Significant improvement between preoperative and postoperative evaluation
- Improvement (in %) of a minimum of 30 % between preoperative and postoperative evaluation to account for a potential placebo effect and to ensure clinical efficacy.
Osteoarthritis was evaluated based on radiographic diagnostic images by a veterinary clinician. The following scale was used:
- 0 = no OA
- 1 = mild OA
- 2 = moderate OA
- 3 = severe OA.
The outcome was also characterized based on the time frame, i.e., short-term (up to 8 weeks) and mid-term (up to 6 months):
- No OA (score </= 0.5) at mid-term or long-term evaluation
- Progression (in %) of a maximum of 10 % (>/=) between preoperative evaluation and mid-term or long-term evaluation.
The thigh circumference was measured with a tape measure by a veterinary clinician. The reported outcome of each study was expressed either as symmetry index (ratio in thigh circumference between the affected and the healthy hind limb) or as the difference in thigh circumference in the affected limb pre-operatively and post-operatively.
Outcome was considered successful with a post-operative symmetry index > 0.95 or when there was no significant loss in muscle mass between pre-operative and post-operative measurements.
ROM (Range of Motion) or flexion and extension in degree was measured with a goniometer by a veterinary clinician or fluoroscopic images. Outcome was considered successful when the ROM or flexion or extension was increased pre-operative compared to post-operative level or when there was no difference between the healthy and affected pelvic limb at the final post-operative examination.
Joint stability was assessed either by a fluoroscopic examination or the tibial compression test. The outcome was considered successful when the limb was stable, i.e., negative in tibial compression test or no abnormalities, such as femorotibial craniocaudal translation, shown in fluoroscopy.
The pain score was assessed by a veterinary clinician and expressed using a validated instrument (standardized questionnaire), or using a scale or simply stating “pain is present” or “pain is absent.” The following scale was used:
- 0 = no pain
- 1 = mild pain
- 2 = moderate pain
- 3 = severe pain.
The outcome was also characterized based on the time frame, i.e., short-term (up to 8 weeks) and mid-term (up to 6 months) and considered successful when pain score </= 0.5.
Operation-related complications were categorized into major (any complication that needed further surgical intervention) or minor (any complication that did not require surgical intervention). A distinction in complication rates based on the size (mean body weight) of the dogs in each study was also used:
- Small dogs (group S): < 15 kg
- Medium dogs (group M): 15–40 kg
- Large dogs (group L): > 40 kg.
A Mann-Whitney-U-Test was calculated to determine if there were differences in mean osteoarthritis scores between TPLO and TTA. For the comparison groups' studies, a further approach was conducted to identify statistical differences between studies with regards to reported complications. For each study, the total number of surgeries with reported complications in the treated groups (TPLO vs. TTA) were retrieved. The odds ratio (OR) was then estimated in order to indicate the increased or decreased odds of observing a specific complication for the TPLO compared to TTA. Statistical analysis was undertaken following the guidelines of the Handbook of the Cochrane Collaboration 5.4.1. The OR for dichotomous data was calculated using the random-effects model in Review Manager 5.4.1. Heterogeneity between studies was calculated using the Chi square test and was considered to be heterogeneous when P ≤ 0.1. I2 values of <25, 26–74, and >75 % were considered as “low,” “moderate” and “high” heterogeneity, respectively. Associations were considered to be statistically significant at P < 0.05.
The search identified a total number of 72 studies fulfilling the inclusion criteria (see Supplementary material). The database searches delivered about 7,000 results and after screening titles, abstracts and full texts for keywords, the number of eligible studies was 156. Then, 84 of these studies were excluded due to a lack of detailed results, investigations on CCL disease plus comorbidities or indistinct definition of which orthopedic surgery has been performed, which left a total of 72 studies for inclusion. Two studies have been published twice (31–34) with the same study population and study design, but each paper focussed on different outcome parameters.
Less than half (34 studies, 47.2 %) of the studies was assigned to group C and considered to have least overall quality. There were 20 studies (27.8 %) in group B and 18 studies (25.0%) in group A. Out of 18 studies in group A, there were eleven bRCTs, of which five were rated with a low overall risk of bias (35–40) (see Supplementary material).
Information on study group size was provided in all of the included studies. However, the definition of “cases” or “subjects” was inconsistent between studies. The authors counted the number of surgeries per subject for evaluation, hence, dogs with a bilateral CCL rupture were counted as two independent cases or subjects. Others differentiate between the number of dogs they included and the number of surgeries performed. Some authors (31–34, 36–38, 41–57) only included dogs with unilateral CCL rupture, so the number of dogs and number of cases were the same. Study group sizes varied between five subjects per group (56, 58) and 1,732 subjects per group. The highest total number of subjects in one study was 1,732 dogs with 1,768 surgeries (59).
Study duration varied from 3 days (37) up to 5 years (58, 60–64). Twenty-eight, 26 and 18 studies evaluated mid-term, short-term and long-term outcomes, respectively.
The majority of the studies (36 studies) provided detailed information based on common and validated methods for the diagnosis of CCL disease. Their subject enrolment quality was therefore considered of high standard. Eight studies diagnosed CCL disease “fairly” and one study did poorly. There were 27 studies that provided unclear information on how diagnosis of CCL disease was confirmed.
All studies in group A used randomization to allocate subjects to groups. Random sequence generation and allocation concealment were evaluated to assess selection bias. Twelve studies were considered to produce low risk of selection bias (Table 1) regarding random sequence generation and allocation concealment (as they used adequate methods to generate the allocation sequence: these studies assign subjects via computer-assisted lists (31, 36, 37, 39, 48, 54, 65, 66) such as Excel or commonly available online tools, via coin toss (35, 38, 44) or by referring to a random number table (40).
Three studies only stated that they “randomly assigned” (32, 49) or used a “simple randomization procedure” (51) without giving detailed information on the procedure applied. One study (47) assigned subjects via a randomized block cohort study on the basis of patient-related data that might had introduced a source of bias.
One study (67) assigned dogs to a treatment group alternately and another study (68) used pre-labeled notecards in a pile. Both did not give information on how allocation concealment was guaranteed.
A very uncommon methodology of comparing two surgical treatments was used in one experimental study (69) that artificially transected the cranial cruciate ligament. Specifically, each hindlimb was randomly assigned (via coin toss) to receive either a TTA or TPLO technique. Every dog was treated with TTA on one leg and TPLO on the contralateral. The comparison between TTA and TPLO was based on the evaluation of limbs of the same dog, rather than between different dogs. This study was considered a NRCT.
Eleven studies were categorized as blinded, however only seven (35, 36, 38–40, 47, 54) of them described in detail a complete blinding of patients, personnel and outcome assessors. They were therefore considered to have a low risk of performance and detection bias (Table 1). Some studies described blinding to some extent (37, 65) or it was not possible to blind all personnel and owners to all treatments (31, 32).
Low risk of attrition bias was attributed to 27.8 % of the studies as they reported either no missing outcome data or no reasons for missing outcome data which could affect the outcomes (Table 1). In 51.4 % of the studies, insufficient information was provided on whether all included dogs completed the trial until the end or it was unclear whether missing outcome data affected the outcomes. 20.8 % of the studies had a high risk of attrition bias. In retrospective studies, in particular, it was a common limitation for the study that dogs were not even included since no follow-up examination was possible; the reasons for this could be related to the outcome of the treatment, i.e., when it is unsatisfactory and the owners might opt for a re-evaluation in another veterinary clinic.
Most studies (51.4 %) deliver an unclear risk of bias as they did not correctly report every detail concerning study design and outcome data. Unclear or high risk of bias was also seen in studies (54, 56, 60–64, 68, 70–77) that were (partly) based on results stated by the owners or referring vets (Table 1). These might not have followed standard protocols, but be influenced by the owners' or referring vets' personal opinion and bias toward the treatment.
In several studies, other potential sources of bias have been identified (Table 1). Many studies were of retrospective nature (42, 50, 52, 53, 55, 56, 58–61, 63, 64, 71–95) which imposes a high risk of bias as protocols have not been standardized beforehand. Also, reported outcomes which might be different from the true outcome as potential follow-up losses cannot be identified. Studies with unclear financial support (62, 63, 83, 87, 96, 97), support of financial nature, consultant activity, company collaboration or speaker engagement (31–33, 36–38, 40, 44, 46, 47, 56, 60, 65, 69, 71, 72, 76, 98) (e.g., financial funding) or other potential conflicts of interests (39, 50, 51, 54, 57, 59, 67, 73, 80, 92) led to an unclear risk of bias.
A total of 72 studies were included in this review. Forty-six studies examined the results of TPLO surgery, 20 studies focused on TTA surgery and six studies considered TPLO and TTA outcome. In addition to the surgical intervention itself, 24 (20 TPLO, four TTA) studies evaluated the results of additional (postoperative) treatments or other factors that contributed to surgical outcome.
Number of studies for each outcome parameter can be found in Table 2.
Twenty-two studies with a total of 876 surgeries (349 TPLO, 527 TTA) evaluated the outcome of CCL surgery based on this criterion. Eleven studies reported TPLO outcome, nine studies TTA outcome and two studies compared results of TPLO und TTA surgery. The quality of evidence varied between TPLO and TTA studies. High quality of evidence was provided in eight studies on TPLO and only one study on TTA.
At short-term evaluation, four of eleven (36 %) TPLO treatment groups (36, 38, 51, 78) and two of seven (29 %) TTA treatment groups (70, 99) showed a successful outcome regarding a lameness score </= 0.5 (no lameness) (Table 3). The mean lameness score for TPLO was 0.87 (median 0.71) and 0.83 (median 0.7) for TTA. Lameness scores ranged from 0.3 to 2.4 for TPLO and 0.3–1.6 for TTA. Four of nine (44 %) TPLO treatment groups (36, 38, 51) and four of six (67 %) TTA treatment groups (55, 70, 99) had successful outcome with an improvement of a minimum of 50 % between pre-operative and short-term postoperative evaluation (Table 3). Improvement varied between 0–72.5 % for TPLO and 20–81.3 % for TTA.
The mid-term outcome was successful in five out of six (83 %) TPLO treatment groups (48, 51, 67, 69) and five out of five (100 %) TTA treatment groups (79, 99, 100) showing no lameness. Five out of five (100 %) TPLO treatment groups (48, 51, 67) and three out of four (75 %) TTA treatment groups (99, 100) had successful outcome with an improvement of a minimum of 50 % between pre-operative and mid-term postoperative evaluation (Table 4). The mean lameness score for TPLO was 0.16 (median 0.09) and 0.09 (median 0.12) for TTA. Lameness score ranged between 0–0.6 for TPLO and 0–0.2 for TTA and improvement between 50–61.5 % and 49.1–85.5 % for TPLO and TTA, respectively.
When only high-quality studies were compared, only one could be assessed for TTA showing a better mid-term result, but no information was available for short-term success, whereas the short- and mid-term results were similar for TPLO (Tables 3, 4).
Overall, the studies provided evidence that both TPLO and TTA surgery were highly effective in treating CCL disease regarding the subjectively evaluated lameness. For both procedures, lameness scores decreased continuously and resulted in “no lameness” 6 months postoperatively in all treatment groups, except in one TPLO surgery group.
Objective gait analysis was performed in 16 studies: 13 studies evaluated the outcome of TPLO, one of TTA and two studies compared TPLO and TTA outcome. Overall, 519 surgeries (453 TPLO, 66 TTA) on CCL disease with concurrent objective gait analysis were reported. High quality of evidence was provided in nine studies on TPLO and in one study on TTA.
Regarding the short-term assessment: For TPLO, several studies on objective gait parameters already showed a significant improvement (31, 46, 48, 66, 67) [16 of 22 (73 %) study groups with successful outcome] as well as a clinically visible improvement of at least 30 % (38, 40–42, 47) [17 of 38 (45 %) study groups with successful outcome]. For TTA surgery, there was only one eligible study providing sufficient information on significant differences pre- and postoperatively. This study is of high quality of evidence and reports a significant improvement (48). The two studies reporting on the overall improvement showed that there was no improvement of more than 30 % in the different gait parameters (45, 48).
At mid-term evaluation, all studies reported a significant improvement in ground reaction forces in all (100 %) groups compared to pre-operative assessment and therefore a successful outcome on TPLO as well as TTA surgery (31, 40, 42, 45, 48, 60, 67). This result was consistent with subjective gait analysis.
Overall, the studies provided evidence that both TPLO and TTA surgery were highly effective in treating CCL disease regarding the objectively evaluated lameness up to 6 months after surgery. However, both studies with high and low quality of evidence were combined for attaining this comparison.
Fourteen studies investigated the development of osteoarthritis after CCL surgery with seven studies evaluating TPLO surgery, four studies evaluating TTA surgery and three studies comparing the outcome between TPLO and TTA. A total of 447 surgeries (329 TPLO, 148 TTA) have been performed. High quality of evidence was provided in six studies on TPLO and in one study on TTA.
The majority of the studies (32, 36, 48, 51, 61, 62, 67, 69, 84, 91) focused on short- and mid-term outcome, whereas only three authors (49) considered long-term outcomes.
All studies with available outcome data reported the occurrence of osteoarthritis postoperatively as relatively severe. At short- and mid-term evaluation, four out of twelve (33 %) TPLO study groups (32, 36, 61) and three out of seven (43 %) TTA study groups (62, 91) showed a progression in osteoarthritis of <10 % and were therefore considered successful. Mild osteoarthritis was seen in seven (58 %) TPLO (32, 48, 61, 67, 69) and seven (100 %) TTA study groups (48, 61, 62, 69, 84, 91), moderate osteoarthritis also in five (42 %) TPLO study groups (32, 36, 51). The mean OA score was 1.44 (median 1.5) for TPLO and 0.96 (median 0.9) for TTA.
Long-term outcome was not successful in any of the evaluated studies (49, 61, 62), since all the osteoarthritis scores showed at least mild osteoarthritis and a progression of more than 10 % compared with preoperative levels. The mean OA score was 1.57 (median 1.5) for TPLO and 1.55 (median 1.55) for TTA.
Overall, the studies showed evidence that osteoarthritis was developed radiographically after TPLO and TTA surgery at short-, mid- as well as long-term evaluation. There was a statistically significant difference in OA scores between TPLO and TTA (p < 0.05). After TTA, OA scores were significantly lower than after TPLO (Figure 1).
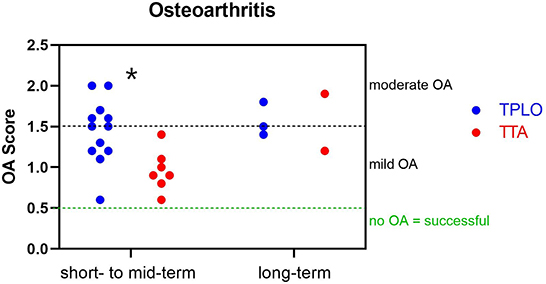
Figure 1. Outcome on osteoarthritis. Mean osteoarthritis scores in short- to mid-term and long-term outcome for TPLO and TTA. No study showed successful outcome in terms of no detectable osteoarthritis. The majority of the studies for TPLO and all TTA studies showed mild osteoarthritis up to 6 months postoperatively. TTA had a significant lower rate of cases developing an osteoarthritis (*P < 0.05, Mann-Whitney U-Test).
Eight studies perform measurements of thigh circumference, five for TPLO and three for TTA surgery. In total, 316 (201 TPLO, 115 TTA) have been taken into consideration. High quality of evidence is provided in four studies on TPLO, but in no study on TTA.
Most studies reported a successful outcome, either considering that there is no significant difference in thigh circumference between the healthy and the affected leg (31, 62, 99) or that there was no loss in muscle mass after surgery (46, 66).
One study that investigated the effect of Fortetropin reported a reduction in thigh circumference between pre-operative measurement and the 8-week evaluation in the control group whereas the treatment group did not show a significant difference in muscle mass (40). Another study showed inconsistent results between treatment groups: all three groups showed statistically significant values when comparing pre-operative and post-operative levels; even though the two treatment groups showed a decrease in thigh circumference, the control group showed the opposite (39).
Overall, there was evidence that CCL disease does not have clinically relevant effects on thigh circumference in affected hind limbs after TPLO or TTA surgery.
Seven studies with a total of 189 CCL surgeries (74 TPLO, 115 TTA) reported pre- and post-operative investigations on the Range of Motion (flexion + extension) of affected joints. High quality of evidence was provided in three studies describing TPLO only.
Evidence was provided that TPLO and TTA surgery both had a successful outcome in joint mobility as the ROM, either increased (39, 66, 100) or did not change or decrease significantly (36, 57) compared to pre-operative levels, by the time of the final evaluation. However, comparison between affected and the contralateral healthy limbs showed significant differences (62, 99) with a decreased ROM in affected joints. For this outcome measure was no study with high quality of evidence for TTA, the results of TTA's effectiveness cannot be adequately determined.
Joint stability, evaluated by fluoroscopy (33, 34, 57, 93) or tibial compression test (58, 69), was assessed in six studies (four TPLO studies, one TTA study, one study comparing TPLO and TTA) with a total of 82 CCL surgeries (57 TPLO, 25 TTA). None of these studies was considered of high quality of evidence.
Fluoroscopic imaging showed that patellofemoral as well as femorotibial translation and rotation remained abnormal after TPLO surgery (33, 34, 57). While it was found that the changes in patellofemoral kinematics may be caused by an increased flexion of the stifle (33), another study did not support the findings that flexion is different from the unaffected control limb (57). However, authors agreed that there were profound changes in gait cycle in CCL affected joints even after stabilizing surgery (33, 34, 57). Cranio-caudal translation in femorotibial kinematics was also found in the fluoroscopic investigation on joints after TTA surgery (93).
In an experimental setting, one study artificially caused CCL rupture in both joints and surgically stabilized both limbs with TTA and TPLO, respectively (69). Twelve weeks post-surgery, joint stability was tested with the tibial compression test and identified a positive test (instability) in 33 % of the TTA-operated and in 13 % of the TPLO-operated stifles. When evaluating the outcome only of partial CCL rupture and therefore stable joints pre-operatively, one study finds that these joints remain stable after TPLO surgery (58).
Pain was assessed in six TPLO and five TTA studies with a total of 382 surgeries (169 TPLO, 213 TTA). Several validated instruments and their modifications were used to classify pain on a scale (36–39, 43, 60, 65, 66) while other authors created their own scale in expressing pain in grades (31, 100) or as absent or present (99). High quality of evidence was provided in six studies on TPLO and one of the studies on TTA.
Immediate post-operative evaluation can only be detected on TPLO studies and therefore, a comparison to TTA results was not possible. The outcome was inconsistent: in one study (38), both study groups showed pain at 24 h post-surgery whereas the other study showed successful outcome (66). All studies showed successful results regarding short-term outcome after TPLO as well as TTA (36, 38, 43, 66, 100).
There were no TPLO studies evaluating mid-term outcome of TPLO. Mid-term outcome of TTA showed that pain was still present in two of five (40 %) study groups (43, 60), while outcome was considered successful in three (60 %) groups (99, 100).
Complications were recorded in the majority of the studies (58 studies in total, 36 TPLO, 17 TTA and five studies comparing TPLO and TTA). Not all of these studies have been considered into the systematic analysis due to a lack of complete data (43, 79) or recorded data which only included certain types of complications (52, 56, 76, 83, 84, 86, 88, 89, 94). Some studies could not be matched to Group S, M or L as they did not provide information on mean body weight (35, 97).
The most commonly reported minor complications were surgical site infection, fibula fracture, seroma, tibial tuberosity fracture/fissure, incision dehiscence, screw loosening, plate cracks, patellar tendonitis, tissue swelling, osteomyelitis and septic arthritis (order by frequency of mention in considered studies) following TPLO and tibial tuberosity fracture/fissure, surgical site infection, incision dehiscence, implant loosening, implant rupture, seroma, tissue sweeling, patellar ligament desmitis, septic arthritis and lick granuloma following TTA. Most common major complications in both techniques were meniscal lesions, surgical site infections, tibial tuberosity fractures and implant loosing.
Most of the operated stifles were related to medium sized dogs in both TPLO and TTA. Comparing TPLO and TTA in medium sized dogs, complication rates did not differ between surgical techniques, with a mean of 20.0 % (weighted mean 22.3 %, range 0–53.3 %) in TPLO and a mean of 26.5 % (weighted mean 22.0 %, range 0–67.7 %) in TTA (Tables 5, 6).
In small dogs, TPLO surgery showed a mean complication rate of 9.4 % (weighted mean 10.4 %, range 0–22.7 %), while TTA showed a mean complication rate of 6.7 % (weighted mean 9.2 %, range 0–14.6 %) (Tables 5, 6). Due to the comparably low number and a medium to low quality of evidence, the outcome was not supported by strong evidence.
Large dogs overall had a mean complication rate of 35.7 % (weighted mean 25.4 %, range 18.4–49 %) when operated with TPLO and 21.4 % (weighted mean 27 %, range 8.6–34.1 %) when treated with TTA (Tables 5, 6). There seemed to be a higher incidence in overall complications as well as major and minor complications following TPLO surgery compared to TTA. Both TPLO and TTA studies provided a low quality of evidence, thus, any definite conclusions are precluded.
Overall, it was shown that the complication rates were comparably lower in small sized dogs. This could be observed in both TPLO and TTA surgery with no difference between the treatment option. The higher the body weight, the higher the complications rates were.
In all groups, a total of 2,547 TPLO and 1,242 TTA surgeries have been performed. The overall complication rate for TPLO was 20.4 % (weighted mean 21.9 %, range 0–53.3 %) which did not differ to the complication rate for TTA, 21.6 % (weighted mean 21.1 %, range 0–67.7 %).
The common estimated OR was 1.33 (95% CI: 0.22–8.18), showing a statistically non-significant association (P = 0.76) between the two surgical techniques. Moderate heterogeneity was shown between studies (chi2 = 2.56, P = 0.11) (Figure 2).
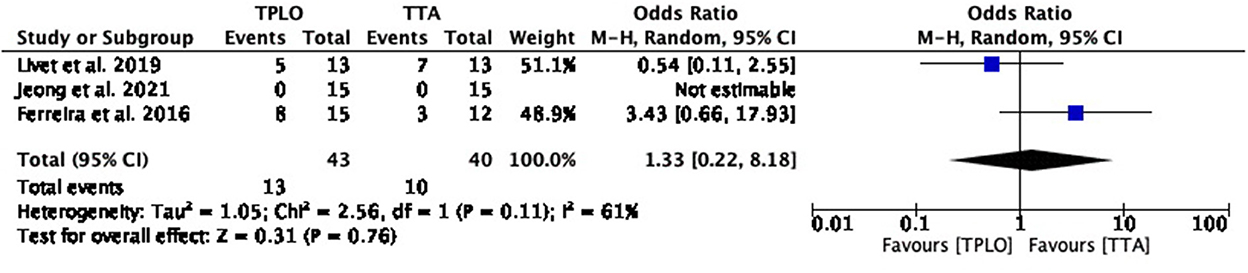
Figure 2. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of total complications for TPLO and TTA.
The common estimated OR was 1.16 (95% CI: 0.02–1.00), showing a statistically significant association (P = 0.05) between the two surgical techniques, with reduced odds of this adverse effect in TPLO. Heterogeneity calculation was not applicable for this comparison (Figure 3).
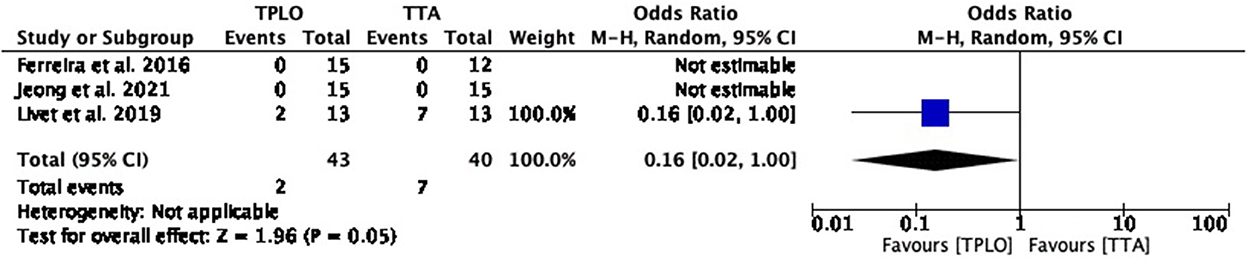
Figure 3. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of surgical site infection as a complication for TPLO and TTA.
The common estimated OR could not be estimated for this complication since this complication was not reported in any of the studies (Figure 4).
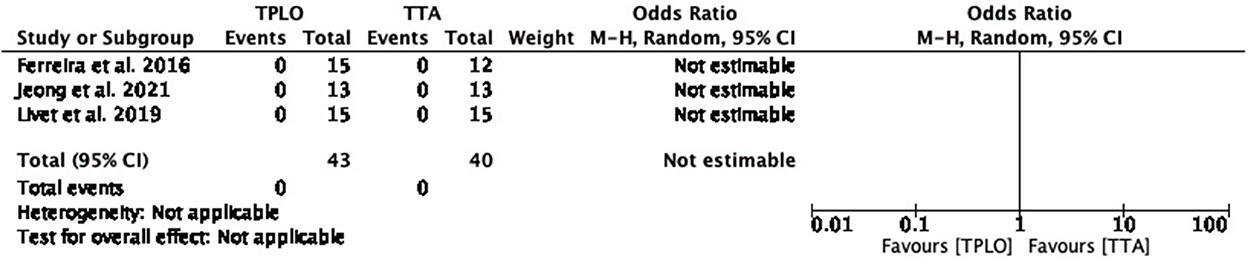
Figure 4. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of seroma formation as a complication for TPLO and TTA.
The common estimated OR was 0.39 (95% CI: 0.05–3.26), and there was no association (P = 0.38) between the two surgical techniques. Low heterogeneity was shown between studies (chi2 = 0.50, P = 0.48) (Figure 5).
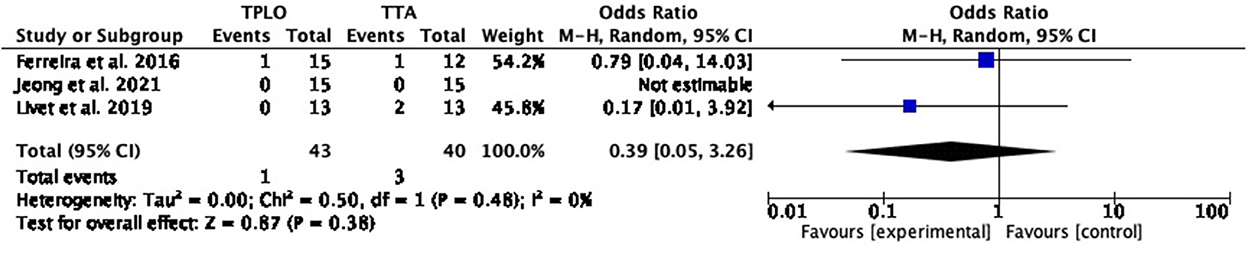
Figure 5. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of implant failure as a complication for TPLO and TTA.
The common estimated OR was 1.00 (95% CI: 0.12–8.42), without a difference between the two surgical techniques (P = 1.00). Heterogeneity calculation was not applicable (Figure 6).

Figure 6. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of late meniscal injury as a complication for TPLO and TTA.
The common estimated OR was 0.17 (95% CI: 0.01–3.92), showing a statistically non-significant association (P = 0.27) between the two surgical techniques. Heterogeneity calculation was not applicable (Figure 7).

Figure 7. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of tibial tuberosity fracture as a complication for TPLO and TTA.
The common estimated OR was 2.32 (95% CI: 0.31–17.32) not showing a difference between the two surgical studies (P = 0.41). Low heterogeneity was shown between studies (chi2 = 0.01, P = 0.94) (Figure 8).
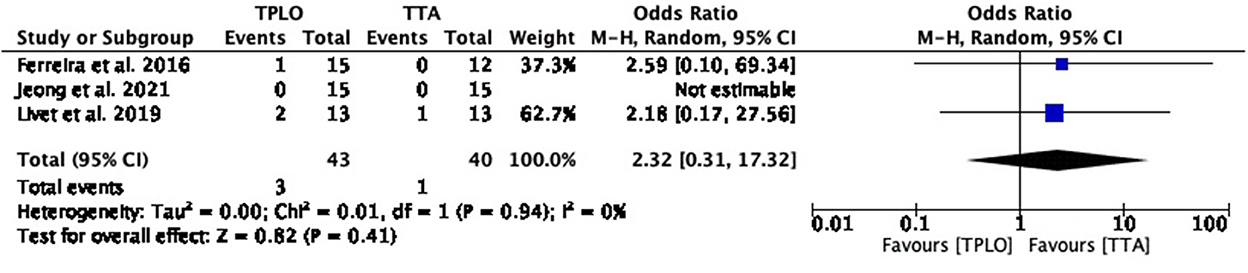
Figure 8. Forest plot comparing TPLO vs. TTA. Odd ratios (95% CI) of fibular fracture as a complication for TPLO and TTA.
This systematic review evaluated 72 studies regarding the outcome of TPLO and/or TTA, two highly relevant and common surgical interventions for CCL rupture. The results of the systematic review showed that both techniques are effective with no difference in outcome. Some former studies with either client-assessed subjective approaches (61, 101) or based on objective parameters (102) suggest that TPLO could be superior to TTA. Studies with subjective lameness assessment by a veterinarian, however, did not show differences between their outcome (48, 69), confirmed by the current study. There were also studies included that could not be evaluated within the systematic analysis as they lacked detailed data on lameness scores or scores were expressed in combination with other criteria (31, 39, 43, 49, 62, 65, 96, 97). Still, these studies confirm the assumption that both procedures can result in decreased lameness scores over time.
Using objective gait analysis measurements, studies showed that TPLO and TTA both lead to a return to normal limb function (45) with a relatively fast recovery in TTA (48) whereas one study indicated TPLO's superiority over TTA in long-term assessment (102). Our results showed significant differences in ground reaction forces at mid-term evaluation in all study groups in both TPLO and TTA indicating that both treatment options may lead to a successful outcome. However, even though a significant improvement was seen in all study groups, the improvement in ground reaction forces was often below 30 %. This might indicate that the improvement may be too small to be clinically relevant. The studies on objective gait analysis that were included use a variety of different parameters, expressed either as kinetic data, relative weight-bearing or as symmetry index. A lack of comparability can be considered when interpreting the results in the systematic approach. However, the results consistently indicated that both procedures can improve limb function when assessed with objective parameters.
Our investigations on the development of osteoarthritis confirmed recent findings (13, 23) that stifle surgery does not prevent osteoarthritis after CCL disease. However, we did not observe superiority of one technique over the other in contrast to another systematic review which reported TPLO to have a favorable effect on osteoarthritis development compared to TTA (13). Actually, our results even indicated a lower mean OA score at short- to mid-term outcome after TTA surgery and therefore a less rapid development of OA. Current investigations lack long-term results as most studies focus on a horizon up to 6 months postoperatively. Osteoarthritis usually has a long-term effect and worsens over time (23, 24). It is also affected by other factors, such as meniscal lesions (23), stability due to partial or complete rupture (24) as well as the timing of surgery as a lower stage of osteoarthritis prior to surgery is suspected to slow down osteoarthritis progression (91). Several of the included studies investigated the presence and extent of meniscal lesions during surgery (41–43), but the results do not allow conclusions whether one surgical technique is superior to the other in regard of osteoarthritis development when concurrent meniscal damage was present.
The functional outcome of joint surgery could also be assessed by goniometry and thigh circumference measurements. The affected limb may show a reduced ROM as well as a loss in muscle mass (18, 20, 103). Our findings showed improvement or at least no worsening in both parameters, however, the ROM was abnormal compared to contralateral unaffected pelvic limbs. This is also consistent with previous findings (103). Our results did not favor one surgical technique over the other regarding ROM or thigh circumference. There may be positive effects of additional treatments, which is indicated by some of the included studies (31, 36, 39, 40), but not relevant to our results.
Kinematic fluoroscopy revealed abnormal gait and instability in the stifle joint due to CCL disease (20). TPLO as well as TTA aim to alter biomechanical dynamics and restore stability, which in fact seems to be only partly achieved (20, 93). Our results showed that femorotibial, craniocaudal subluxation is still apparent after TPLO as well as TTA (57, 69, 93) with a suspected slightly higher incidence after TTA. Further research on the impact of joints' instability on the functional outcome and the underlying biomechanical alterations is needed.
We were not able to compare TPLO and TTA outcome regarding immediate post-operative or mid- to long-term pain due to a lack of availability of relevant studies and lack of or inhomogeneous data to allow a thorough statistical analysis. Short-term outcomes revealed successful results for both surgical techniques. Included studies used different approaches in assessing pain, either using established and standardized instruments (36–39, 43, 60, 65, 66) or after clinical examination stating pain is present or absent (99). There was no homogenous definition of pain in the included studies.
Previous literature indicated lower complications rates for TPLO compared to TTA (13), which is not supported by our findings. We calculated an overall mean complications rate of 20.4 % for TPLO and 21.6 % for TTA. However, if one takes a closer look at the type of complication as well as the size of the dog, differences nevertheless may become apparent. Both techniques showed higher complication rates in medium and large breed dogs, which confirmed recent findings that weight is associated with a higher risk for complications (27, 28, 71). Due to a lack of prospective, controlled, randomized and blinded studies, we were not able to perform a complete meta-analysis on outcome parameters. Three of the studies comparing TPLO and TTA however delivered sufficient data for a meta-analytic approach on complications. For the total complication rate, our meta-analytic approach confirmed that none of the surgical techniques is superior to the other. Surgical site infections were commonly reported after TPLO and TTA (59, 68, 72, 77, 82, 87, 98). Similar to previous systematic review (13) our study also favored TPLO regarding complication rates. Further research in a prospective, controlled trial is needed to verify these findings and evaluate the causes and preventive strategies. The retrospective nature of the majority of studies assessing complications carry the risk of over- or underreported complications. Owners tend to come back to the primary care hospital when a complication occurs so dogs with complications may be overreported. Dogs that do not suffer complications may not be presented again as owners do not see the need to. On the other hand, owners may be unsatisfied with the surgical outcome when facing a complication and may choose another veterinarian; thus, the primary surgeon is not informed about the complication. Another challenge is the inconsistent definition of major and minor complications. In our study, we used a standardized scale to address this inhomogeneity. However, since some authors reported the same rates for major and overall complications, it is questionable whether minor complications have been monitored and stated.
There are several limitations in our study which may preclude definite conclusions. First, the number of studies with high quality of evidence was very low. Only five of 72 included studies fulfilled all requirements to be rated as low risk of bias and there was a total of 18 studies providing high quality of evidence. Overall, due to the lack of studies with high quality of evidence, we compared TPLO and TTA outcomes using an heterogenous population of high and low quality studies. There was only one randomized, clinical trial comparing the surgical techniques of TPLO and TTA directly with each other. Retrospective design, lack of detailed outcome description as well as low numbers of included patients lead to inconsistent results and questionable comparability. Therefore, solid conclusions are precluded. Further research, especially with randomized, surgical clinical trials is required to compare surgical techniques for CCL rupture in a controlled and standardized setting.
TPLO and TTA are both effective surgical approaches to treat naturally occurring CCL disease/rupture. There is evidence that both techniques provide good outcome and restore functionality and mobility for affected canines. However, long-term development of osteoarthritis must be considered and long-term follow up data are spare. There is no clear recommendation regarding the choice of one technique over the other, but the current evidence indicates that TPLO is favorable regarding certain complications, such as SSIs. Further research providing high quality of evidence is vital to confirm our findings and further assess the differences in outcome parameters between the two surgical interventions.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
AW collected the data for the study, assessed the data, and wrote the first draft of the manuscript. MC and HV performed statistical analysis and meta-analytic approach. All authors helped to draft the manuscript, participated in its design, read, and approved the final manuscript.
This Open Access publication was funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) 491094227 Open Access Publication Costs and the University of Veterinary Medicine Hannover, Foundation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2022.1004637/full#supplementary-material
AB, Attrition bias; bRCT(s), Blinded randomized clinical trial(s); CCL, Cranial cruciate ligament; CCS, Case-control study(ies); CI, Confidence Interval; CoS, Cohort study(ies); CR, Case report(s); CS, Case series; DB, Detection bias; L, Large; M, Medium; nbRCT(s), Non-blinded randomized clinical trial(s); No., Number; NRCT(s), Non-randomized clinical trial(s); OA, Osteoarthritis; ObS, Observational studies; OR, Odds Ratio; PB, Performance bias; RB, Reporting bias; ROM, Range of Motion; S, Small; SB A, Selection bias (allocation concealment); SB R, Selection bias (random sequence generation; SSI, Surgical site infection; TPLO, Tibial Plateau Leveling Osteotomy; TTA, Tibial Tuberosity Advancement; UCT(s), Uncontrolled clinical trial(s).
1. Johnson JA, Austin C, Breur GJ. Incidence of canine appendicular musculoskeletal disorders in 16 veterinary teaching hospitals from 1980 through 1989. Vet Comp Orthop Traumatol. (1994) 7:56–69. doi: 10.1055/s-0038-1633097
2. Wilke VL, Robinson DA, Evans RB, Rothschild MF, Conzemius MG. Estimate of the annual economic impact of treatment of cranial cruciate ligament injury in dogs in the United States. J Am Vet Med Assoc. (2005) 227:1604–7. doi: 10.2460/javma.2005.227.1604
3. Cook SR, Conzemius MG, McCue ME, Ekenstedt KJ. SNP-based heritability and genetic architecture of cranial cruciate ligament rupture in labrador retrievers. Anim Genet. (2020) 51:824. doi: 10.1111/age.12978
4. Comerford EJ, Smith K, Hayashi K. Update on the aetiopathogenesis of canine cranial cruciate ligament disease. Vet Comp Orthop Traumatol. (2011) 24:91–8. doi: 10.3415/VCOT-10-04-0055
5. Adams P, Bolus R, Middleton S, Moores AP, Grierson J. Influence of signalment on developing cranial cruciate rupture in dogs in the UK. J Small Anim Pract. (2011) 52:347–52. doi: 10.1111/j.1748-5827.2011.01073.x
6. Taylor-Brown FE, Meeson RL, Brodbelt DC, Church DB, McGreevy PD, Thomson PC, et al. Epidemiology of cranial cruciate ligament disease diagnosis in dogs attending primary-care veterinary practices in England. Vet Surg. (2015) 44:777. doi: 10.1111/vsu.12349
7. Engdahl K, Emanuelson U, Höglund O, Bergström A, Hanson J. The epidemiology of cruciate ligament rupture in an insured Swedish dog population. Sci Rep. (2021) 11:9546. doi: 10.1038/s41598-021-88876-3
8. Wilke VL, Conzemius MG, Kinghorn BP, Macrossan PE, Cai W, Rothschild MF. Inheritance of rupture of the cranial cruciate ligament in Newfoundlands. J Am Vet Med Assoc. (2006) 228:61–4. doi: 10.2460/javma.228.1.61
9. Bergh MS, Sullivan C, Ferrell CL, Troy J, Budsberg SC. Systematic review of surgical treatments for cranial cruciate ligament disease in dogs. J Am Anim Hosp Assoc. (2014) 50:315–21. doi: 10.5326/JAAHA-MS-6356
10. Duerr FM, Martin KW, Rishniw M, Palmer RH, Selmic LE. Treatment of canine cranial cruciate ligament disease. a survey of ACVS diplomates and primary care veterinarians. Vet Comp Orthop Traumatol. (2014) 27:478–83. doi: 10.3415/VCOT-14-03-0047
11. Montavon PM, Damur DM, Tepic S, editors. Advancement of the tibial tuberosity for the treatment of cranial cruciate deficient canine stifle 2002. Cremona: European Society of Veterinary Orthopaedics and Traumatology.
12. Slocum B, Slocum TD. Tibial plateau leveling osteotomy for repair of cranial cruciate ligament rupture in the canine. Vet Clin North Am Small Anim Pract. (1993) 23:777–95. doi: 10.1016/S0195-5616(93)50082-7
13. Beer P, Bockstahler B, Schnabl-Feichter E. Tibial plateau leveling osteotomy and tibial tuberosity advancement - a systematic review. Tierarztl Prax Ausg K Kleintiere Heimtiere. (2018) 46:223–35. doi: 10.15654/TPK-170486
14. Brunnberg L. Lahmheitsdiagnostik beim Hund. Parey: Untersuchung - Diagnose – Therapiehinweise (1999).
16. Conzemius MG, Torres BT, Muir P, Evans R, Krotscheck U, Budsberg S. Best practices for measuring and reporting ground reaction forces in dogs. Vet Surg. (2022) 51:385–96. doi: 10.1111/vsu.13772
17. Quinn MM, Keuler NS, Lu Y, Faria MLE, Muir P, Markel MD. Evaluation of agreement between numerical rating scales, visual analogue scoring scales, and force plate gait analysis in dogs. Vet Surg. (2007) 36:360–7. doi: 10.1111/j.1532-950X.2007.00276.x
18. Pinna S, Lanzi F, Tassani C. The effect of cranial cruciate ligament rupture on range of motion in dogs. Vet Sci. (2021) 8:119. doi: 10.3390/vetsci8070119
19. Mostafa AA, Griffon DJ, Thomas MW, Constable PD. Morphometric characteristics of the pelvic limb musculature of labrador retrievers with and without cranial cruciate ligament deficiency. Vet Surg. (2010) 39:380–9. doi: 10.1111/j.1532-950X.2010.00657.x
20. Rey J, Fischer MS, Böttcher P. Sagittal joint instability in the cranial cruciate ligament insufficient canine stifle. caudal slippage of the femur and not cranial tibial subluxation. Tierarztl Prax Ausg K Kleintiere Heimtiere. (2014) 42:151–6. doi: 10.1055/s-0038-1623760
21. Murrell JC. Application of a modified form of the Glasgow pain scale in a veterinary teaching centre in the Netherlands. Vet Rec. (2008) 162:403–8. doi: 10.1136/vr.162.13.403
22. Rayward RM, Thomson DG, Davies JV, Innes JF, Whitelock RG. Progression of osteoarthritis following TPLO surgery: a prospective radiographic study of 40 dogs. J Small Anim Pract. (2004) 45:92–7. doi: 10.1111/j.1748-5827.2004.tb00209.x
23. Imholt KM, Möller S, Fehr M, Meyer-Lindenberg A. [Lameness and osteoarthritis development following Tibial Plateau Leveling Osteotomy (TPLO) and potential prognostic predictors. a long-term retrospective study]. Tierarztl Prax Ausg K Kleintiere Heimtiere. (2011) 39:323–35. doi: 10.1055/s-0038-1623596
24. Shimada M, Mizokami N, Ichinohe T, Kanno N, Suzuki S, Yogo T, et al. Long-term outcome and progression of osteoarthritis in uncomplicated cases of cranial cruciate ligament rupture treated by tibial plateau leveling osteotomy in dogs. J Vet Med Sci. (2020) 82:908–16. doi: 10.1292/jvms.19-0613
25. MacDonald TL, Allen DA, Monteith GJ. Clinical assessment following tibial tuberosity advancement in 28 stifles at 6 months and 1 year after surgery. Can Vet J. (2013) 54:249–54.
26. Hoffmann DE, Miller JM, Ober CP, Lanz OI, Martin RA, Shires PK. Tibial tuberosity advancement in 65 canine stifles. Vet Comp Orthop Traumatol. (2006) 19:219–27. doi: 10.1055/s-0038-1633004
27. Fitzpatrick N, Solano MA. Predictive variables for complications after TPLO with stifle inspection by arthrotomy in 1000 consecutive dogs. Vet Surg. (2010) 39:460–74. doi: 10.1111/j.1532-950X.2010.00663.x
28. Wolf RE, Scavelli TD, Hoelzler MG, Fulcher RP, Bastian RP. Surgical and postoperative complications associated with tibial tuberosity advancement for cranial cruciate ligament rupture in dogs: 458 cases (2007-2009). J Am Vet Med Assoc. (2012) 240:1481–7. doi: 10.2460/javma.240.12.1481
29. Charalambous M, Shivapour SK, Brodbelt DC, Volk HA. Antiepileptic drugs' tolerability and safety–a systematic review and meta-analysis of adverse effects in dogs. BMC Vet Res. (2016) 12:79. doi: 10.1186/s12917-016-0703-y
30. Higgins J, Thomas J. Cochrane Handbook for Systematic Reviews of Interventions. (2022). Available online at: https://training.cochrane.org/handbook/current/part-2 (accessed July 25, 2022).
31. Baltzer WI, Smith-Ostrin S, Warnock JJ, Ruaux CG. Evaluation of the clinical effects of diet and physical rehabilitation in dogs following tibial plateau leveling osteotomy. J Am Vet Med Assoc. (2018) 252:686–700. doi: 10.2460/javma.252.6.686
32. Verpaalen VD, Baltzer WI, Smith-Ostrin S, Warnock JJ, Stang B, Ruaux CG. Assessment of the effects of diet and physical rehabilitation on radiographic findings and markers of synovial inflammation in dogs following tibial plateau leveling osteotomy. J Am Vet Med Assoc. (2018) 252:701–9. doi: 10.2460/javma.252.6.701
33. Kim SE, Zann GJ, Tinga S, Moore EJ, Pozzi A, Banks SA. Patellofemoral kinematics in dogs with cranial cruciate ligament insufficiency: an in-vivo fluoroscopic analysis during walking. BMC Vet Res. (2017) 13:250. doi: 10.1186/s12917-017-1186-1
34. Zann GJ, Kim SE, Tinga S, Pozzi A, Banks SA. The effect of tibial plateau leveling osteotomy on patellofemoral kinematics in dogs: an in vivo study. Vet Surg. (2020) 49:207–13. doi: 10.1111/vsu.13300
35. Spencer DD, Daye RM, A. prospective, randomized, double-blinded, placebo-controlled clinical study on postoperative antibiotherapy in 150 arthroscopy-assisted tibial plateau leveling osteotomies in dogs. Vet Surg. (2018) 47:E79–87. doi: 10.1111/vsu.12958
36. Kennedy KC, Martinez SA, Martinez SE, Tucker RL, Davies NM. Effects of low-level laser therapy on bone healing and signs of pain in dogs following tibial plateau leveling osteotomy. Am J Vet Res. (2018) 79:893–904. doi: 10.2460/ajvr.79.8.893
37. Heffernan AE, Katz EM, Sun Y, Rendahl AK, Conzemius MG. Once daily oral extended-release hydrocodone as analgesia following tibial plateau leveling osteotomy in dogs. Vet Surg. (2018) 47:516–23. doi: 10.1111/vsu.12792
38. Rogatko CP, Baltzer WI, Tennant R. Preoperative low level laser therapy in dogs undergoing tibial plateau levelling osteotomy: a blinded, prospective, randomized clinical trial. Vet Comp Orthop Traumatol. (2017) 30:46–53. doi: 10.3415/VCOT-15-12-0198
39. von Freeden N, Duerr F, Fehr M, Diekmann C, Mandel C, Harms O. Comparison of two cold compression therapy protocols after tibial plateau leveling osteotomy in dogs. Tierarztl Prax Ausg K Kleintiere Heimtiere. (2017) 45:226–33. doi: 10.15654/TPK-170049
40. White DA, Harkin KR, Roush JK, Renberg WC, Biller D. Fortetropin inhibits disuse muscle atrophy in dogs after tibial plateau leveling osteotomy. PLoS ONE. (2020) 15:e0231306. doi: 10.1371/journal.pone.0231306
41. Amimoto H, Koreeda T. Evaluation of recovery of limb function by use of force plate gait analysis after tibial plateau leveling osteotomy for management of dogs with unilateral cranial cruciate ligament rupture. Am J Vet Res. (2019) 80:461–8. doi: 10.2460/ajvr.80.5.461
42. Amimoto H, Koreeda T, Ochi Y, Kimura R, Akiyoshi H, Nishida H, et al. Force plate gait analysis and clinical results after tibial plateau levelling osteotomy for cranial cruciate ligament rupture in small breed dogs. Vet Comp Orthop Traumatol. (2020) 33:183–8. doi: 10.1055/s-0039-1700990
43. Arican M, Parlak K, Sahin H. Evaluation and application of the TTA-rapid method in dogs with cranial cruciate ligament rupture. Acta Veterinaria. (2017) 67:238–53. doi: 10.1515/acve-2017-0020
44. Barnhart MD, Watson AT, Thatcher LG, Wotton H, Naber SJ. Prospective randomized clinical and radiographic evaluation of a novel bioabsorbable biocomposite tibial tuberosity advancement cage implant. Vet Surg. (2016) 45:651–8. doi: 10.1111/vsu.12502
45. Ferreira MP, Ferrigno CR, de Souza AN, Caquias DF, de Figueiredo AV. Short-term comparison of tibial tuberosity advancement and tibial plateau levelling osteotomy in dogs with cranial cruciate ligament disease using kinetic analysis. Vet Comp Orthop Traumatol. (2016) 29:209–13. doi: 10.3415/VCOT-15-01-0009
46. Frank I, Duerr F, Zanghi B, Middleton R, Lang L. Diagnostic ultrasound detection of changes in femoral muscle mass recovery after tibial plateau levelling osteotomy in dogs. Vet Comp Orthop Traumatol. (2019) 32:394–400. doi: 10.1055/s-0039-1688985
47. Kieves NR, Canapp SO, Lotsikas PJ, Christopher SA, Leasure CS, Canapp D, et al. Effects of low-intensity pulsed ultrasound on radiographic healing of tibial plateau leveling osteotomies in dogs: a prospective, randomized, double-blinded study. Vet Surg. (2018) 47:614–22. doi: 10.1111/vsu.12798
48. Livet V, Baldinger A, Viguier E, Taroni M, Harel M, Carozzo C, et al. Comparison of outcomes associated with tibial plateau levelling osteotomy and a modified technique for tibial tuberosity advancement for the treatment of cranial cruciate ligament disease in dogs: a randomized clinical study. Vet Comp Orthop Traumatol. (2019) 32:314–23. doi: 10.1055/s-0039-1684050
49. Macri F, Cicero L, Angileri V, Biondi V, Miele P, Scaletta L, et al. Locking compression plates versus locking plates for tibial plateau levelling osteotomy in dogs: progression of osteoarthritis, bone healing score and lameness degree. BMC Vet Res. (2021) 17:193. doi: 10.1186/s12917-021-02899-6
50. Marin K, Unis MD, Horgan JE, Roush JK. Risk factors for short-term postoperative complications in the 8 weeks after tibial plateau leveling osteotomy in dogs weighing less than 15 kilograms: a retrospective study. PLoS ONE. (2021) 16:e0247555. doi: 10.1371/journal.pone.0247555
51. Martini FM, Brandstetter de Bellesini A, Miolo A, Del Coco L, Fanizzi FP, Crovace A. Combining a joint health supplement with tibial plateau leveling osteotomy in dogs with cranial cruciate ligament rupture An exploratory controlled trial. Int J Vet Sci Med. (2017) 5:105–12. doi: 10.1016/j.ijvsm.2017.09.006
52. McDougall RA, Spector DI, Hart RC, Dycus DL, Erb HN. Timing of and risk factors for deep surgical site infection requiring implant removal following canine tibial plateau leveling osteotomy. Vet Surg. (2021) 50:999–1008. doi: 10.1111/vsu.13634
53. McGregor RE, Buffa EA, Tan CJ, Schembri MA, Badcock CA, Lai A, et al. Retrospective study using the string of pearls tibial plateau levelling osteotomy locking plate for the treatment of cranial cruciate ligament disease. Vet Comp Orthop Traumatol. (2019) 32:483–91. doi: 10.1055/s-0039-1692189
54. Renwick SM, Renwick AI, Brodbelt DC, Ferguson J, Abreu H. Influence of class IV laser therapy on the outcomes of tibial plateau leveling osteotomy in dogs. Vet Surg. (2018) 47:507–15. doi: 10.1111/vsu.12794
55. Retallack LM, Daye RM, A. modified Maquet-tibial tuberosity advancement technique for treatment of canine cranial cruciate ligament disease: short term outcome and complications. Vet Surg. (2018) 47:44–51. doi: 10.1111/vsu.12733
56. Seo S, Rahman M, Jeong I. Importance of meniscal injury diagnosis and surgical management in dogs during reconstruction of cranial cruciate ligament rupture: a retrospective study. J Adv Vet Anim Res. (2017) 4:31–8. doi: 10.5455/javar.2017.d223
57. Tinga S, Kim SE, Banks SA, Jones SC, Park BH, Burtch M, et al. Femorotibial kinematics in dogs treated with tibial plateau leveling osteotomy for cranial cruciate ligament insufficiency: an in vivo fluoroscopic analysis during walking. Vet Surg. (2020) 49:187–99. doi: 10.1111/vsu.13356
58. Barger B, Piazza A, Muir P. Treatment of stable partial cruciate rupture (Grade 1 sprain) in five dogs with tibial plateau levelling osteotomy. Vet Rec Case Rep. (2016) 4:e000315. doi: 10.1136/vetreccr-2016-000315
59. Ferrell CL, Barnhart MD, Herman E. Impact of postoperative antibiotics on rates of infection and implant removal after tibial tuberosity advancement in 1,768 canine stifles. Vet Surg. (2019) 48:694–9. doi: 10.1111/vsu.13250
60. Trisciuzzi R, Fracassi L, Martin HA, Monopoli Forleo D, Amat D, Santos-Ruiz L, et al. 41 Cases of treatment of cranial cruciate ligament rupture with porous TTA: three years of follow up. Vet Sci. (2019) 6:18. doi: 10.3390/vetsci6010018
61. Moore EV, Weeren R, Paek M. Extended long-term radiographic and functional comparison of tibial plateau leveling osteotomy vs tibial tuberosity advancement for cranial cruciate ligament rupture in the dog. Vet Surg. (2020) 49:146–54. doi: 10.1111/vsu.13277
62. Medeiros RM, Silva MAM, Teixeira PPM, Chung DG, Conceição MEBAM, Chierice GO, et al. Long-term assessment of a modified tibial tuberosity advancement technique in dogs. Arq Bras Med Vet Zootec. (2018) 70:1053–9. doi: 10.1590/1678-4162-9594
63. Brown G, Maddox T, Baglietto Siles MM. Client-assessed long-term outcome in dogs with surgical site infection following tibial plateau levelling osteotomy. Vet Rec. (2016) 179:409. doi: 10.1136/vr.103688
64. Bureau S. Owner assessment of the outcome of tibial plateau levelling osteotomy without meniscal evaluation for treatment of naturally occurring cranial cruciate ligament rupture: 130 cases (2009 to 2013). J Small Anim Pract. (2017) 58:468–75. doi: 10.1111/jsap.12691
65. Serra Aguado CI, Ramos-Pla JJ, Soler C, Segarra S, Moratalla V, Redondo JI. Effects of oral hyaluronic acid administration in dogs following tibial tuberosity advancement surgery for cranial cruciate ligament injury. Animals. (2021) 11:1264. doi: 10.3390/ani11051264
66. Barnes K, Faludi A, Takawira C, Aulakh K, Rademacher N, Liu CC, et al. Extracorporeal shock wave therapy improves short-term limb use after canine tibial plateau leveling osteotomy. Vet Surg. (2019) 48:1382–90. doi: 10.1111/vsu.13320
67. Knebel J, Eberle D, Steigmeier-Raith S, Reese S, Meyer-Lindenberg A. Outcome after tibial plateau levelling osteotomy and modified maquet procedure in dogs with cranial cruciate ligament rupture. Vet Comp Orthop Traumatol. (2020) 33:189–97. doi: 10.1055/s-0040-1701502
68. Giannetto JJ, Aktay SA. Prospective evaluation of surgical wound dressings and the incidence of surgical site infections in dogs undergoing a tibial plateau levelling osteotomy. Vet Comp Orthop Traumatol. (2019) 32:18–25. doi: 10.1055/s-0038-1676352
69. Jeong J, Jeong SM, Kim SE, Lewis DD, Lee H. Subsequent meniscal tears following tibial tuberosity advancement and tibial plateau leveling osteotomy in dogs with cranial cruciate ligament deficiency: an in vivo experimental study. Vet Surg. (2021) 50:966–74. doi: 10.1111/vsu.13648
70. Dyall B, Schmokel H. Tibial tuberosity advancement in small-breed dogs using TTA Rapid implants: complications and outcome. J Small Anim Pract. (2017) 58:314–22. doi: 10.1111/jsap.12654
71. Engdahl KS, Boge GS, Bergstrom AF, Moldal ER, Hoglund OV. Risk factors for severe postoperative complications in dogs with cranial cruciate ligament disease - a survival analysis. Prev Vet Med. (2021) 191:105350. doi: 10.1016/j.prevetmed.2021.105350
72. Hagen CRM, Singh A, Weese JS, Marshall Q, Linden AZ, Gibson TWG. Contributing factors to surgical site infection after tibial plateau leveling osteotomy: a follow-up retrospective study. Vet Surg. (2020) 49:930–9. doi: 10.1111/vsu.13436
73. Hans EC, Barnhart MD, Kennedy SC, Naber SJ. Comparison of complications following tibial tuberosity advancement and tibial plateau levelling osteotomy in very large and giant dogs 50 kg or more in body weight. Vet Comp Orthop Traumatol. (2017) 30:299–305. doi: 10.3415/VCOT-16-07-0106
74. Knight R, Danielski A. Long-term complications following tibial plateau levelling osteotomy in small dogs with tibial plateau angles > 30 degrees. Vet Rec. (2018) 182:461. doi: 10.1136/vr.104491
75. Matchwick AIM, Bridges JP, Scrimgeour AB, Worth AJ. A retrospective evaluation of complications associated with forkless tibial tuberosity advancement performed in primary care practice. Vet Surg. (2021) 50:121–32. doi: 10.1111/vsu.13502
76. Selmic LE, Ryan SD, Ruple A, Pass WE, Withrow SJ. Association of tibial plateau leveling osteotomy with proximal tibial osteosarcoma in dogs. J Am Vet Med Assoc. (2018) 253:752–6. doi: 10.2460/javma.253.6.752
77. Tuan J, Solano MA, Danielski A. Risk of infection after double locking plate and screw fixation of tibial plateau leveling osteotomies in dogs weighing greater than 50 kilograms. Vet Surg. (2019) 48:1211–7. doi: 10.1111/vsu.13308
78. Barnes DC, Trinterud T, Owen MR, Bush MA. Short-term outcome and complications of TPLO using anatomically contoured locking compression plates in small/medium-breed dogs with “excessive” tibial plateau angle. J Small Anim Pract. (2016) 57:305–10. doi: 10.1111/jsap.12486
79. Butterworth SJ, Kydd DM. TTA-Rapid in the treatment of the canine cruciate deficient stifle: short- and medium-term outcome. J Small Anim Pract. (2017) 58:35–41. doi: 10.1111/jsap.12610
80. Cappelle KK, Barnhart MD. Short-term complications following single-session versus staged bilateral tibial plateau levelling osteotomies stabilized with locking plates for treatment of bilateral cranial cruciate ligament disease: a retrospective study. Vet Comp Orthop Traumatol. (2019) 32:460–6. doi: 10.1055/s-0039-1693153
81. Chiu KW, Amsellem PM Yu J, Ho PS, Radasch R. Influence of fixation systems on complications after tibial plateau leveling osteotomy in dogs greater than 45.4 kilograms (100 lb). Vet Surg. (2019) 48:505–12. doi: 10.1111/vsu.13151
82. Clark AC, Greco JJ, Bergman PJ. Influence of administration of antimicrobial medications after tibial plateau leveling osteotomy on surgical site infections: a retrospective study of 308 dogs. Vet Surg. (2020) 49:106–13. doi: 10.1111/vsu.13337
83. Costa M, Craig D, Cambridge T, Sebestyen P, Su Y, Fahie MA. Major complications of tibial tuberosity advancement in 1613 dogs. Vet Surg. (2017) 46:494–500. doi: 10.1111/vsu.12649
84. Crovace AM, Staffieri F, Monopoli D, Artiles A, Fracassi L, Crovace A, et al. Role of tibial tuberosity fracture/fissure through the maquet hole in stifle osteoarthritis after porous tibial tuberosity advancement in dogs at mid-term follow-up. Vet Sci. (2019) 7:1. doi: 10.3390/vetsci7010001
85. de Lima Dantas B, Sul R, Parkin T, Calvo I. Incidence of complications associated with tibial tuberosity advancement in boxer dogs. Vet Comp Orthop Traumatol. (2016) 29:39–45. doi: 10.3415/VCOT-15-02-0036
86. Geier CM, Frederick SW, Cross AR. Evaluation of the risk of patella fracture as the result of decreasing tibial plateau angle following tibial plateau leveling osteotomy. Vet Surg. (2021) 50:984–9. doi: 10.1111/vsu.13640
87. Lopez DJ, VanDeventer GM, Krotscheck U, Aryazand Y, McConkey MJ, Hayashi K, et al. Retrospective study of factors associated with surgical site infection in dogs following tibial plateau leveling osteotomy. J Am Vet Med Assoc. (2018) 253:315–21. doi: 10.2460/javma.253.3.315
88. Mehrkens LR, Hudson CC, Cole GL. Factors associated with early tibial tuberosity fracture after tibial plateau leveling osteotomy. Vet Surg. (2018) 47:634–9. doi: 10.1111/vsu.12915
89. Morgan MJ, Frazho JK. Comparison of TPLO tibial tuberosity fractures with and without an in situ rotational pin. BMC Res Notes. (2018) 11:368. doi: 10.1186/s13104-018-3474-7
90. Peress R, Mejia S, Unis M, Sotgiu G, Dore S, Bruecker K. Comparison of intra- and postoperative complications between bilateral simultaneous and staged tibial plateau levelling osteotomy with arthroscopy in 176 cases. Vet Comp Orthop Traumatol. (2021) 34:91–8. doi: 10.1055/s-0040-1716682
91. Pinna S, Lanzi F, Cordella A, Diana A. Relationship between the stage of osteoarthritis before and six months after tibial tuberosity advancement procedure in dogs. PLoS ONE. (2019) 14:e0219849. doi: 10.1371/journal.pone.0219849
92. Polajnar P, Szanto Z, Gruborovic S, Willmitzer F, Medl N. Tibial plateau levelling osteotomy using a dome-shaped saw blade for canine cranial cruciate ligament insufficiency. Vet Rec. (2021) 188:e241. doi: 10.1002/vetr.241
93. Schwede M, Rey J, Bottcher P. In vivo fluoroscopic kinematography of cranio-caudal stifle stability after tibial tuberosity advancement (TTA): a retrospective case series of 10 stifles. Open Vet J. (2018) 8:295–304. doi: 10.4314/ovj.v8i3.8
94. Stine SL, Odum SM, Mertens WD. Protocol changes to reduce implant-associated infection rate after tibial plateau leveling osteotomy: 703 dogs, 811 TPLO (2006-2014). Vet Surg. (2018) 47:481–9. doi: 10.1111/vsu.12796
95. Wilson ML, Roush JK, Renberg WC. Comparison of the Effect of Dog, Surgeon and surgical procedure variables on improvement in eight-week static weight-bearing following tibial plateau levelling osteotomy. Vet Comp Orthop Traumatol. (2018) 31:396–404. doi: 10.1055/s-0038-1667139
96. Aydin Kaya D, Altunatmaz K. The clinical and radiological evaluation of canine cranial cruciate ligament rupture treatment with tibial plateau leveling osteotomy. J Fac Vet Med Istanbul Univ. (2015) 42:89–97. doi: 10.16988/iuvfd.2016.50881
97. Medeiros RM, Silva MAM, Teixeira PPM, Dias L, Chung DG, Zani CC, et al. Use of castor bean polymer in developing a new technique for tibial tuberosity advancement for cranial cruciate ligament rupture correction in dogs. Vet Med. (2016) 61:382–8. doi: 10.17221/168/2015-VETMED
98. Lofqvist K, Kjelgaard-Hansen M, Nielsen MBM. Usefulness of C-reactive protein and serum amyloid A in early detection of postoperative infectious complications to tibial plateau leveling osteotomy in dogs. Acta Vet Scand. (2018) 60:30. doi: 10.1186/s13028-018-0385-5
99. Ferreira AJA, Bom RM, Tavares SO. Tibial tuberosity advancement technique in small breed dogs: study of 30 consecutive dogs (35 stifles). J Small Anim Pract. (2019) 60:305–12. doi: 10.1111/jsap.12991
100. Bernardi-Villavicencio C, Jimenez-Socorro AN, Rojo-Salvador C, Robles-Sanmartin J, Rodriguez-Quiros J. Short-term outcomes and complications of 65 cases of porous TTA with flange: a prospective clinical study in dogs. BMC Vet Res. (2020) 16:279. doi: 10.1186/s12917-020-02469-2
101. Christopher SA, Beetem J, Cook JL. Comparison of long-term outcomes associated with three surgical techniques for treatment of cranial cruciate ligament disease in dogs. Vet Surg. (2013) 42:329–34. doi: 10.1111/j.1532-950X.2013.12001.x
102. Krotscheck U, Nelson SA, Todhunter RJ, Stone M, Zhang Z. Long term functional outcome of tibial tuberosity advancement vs. tibial plateau leveling osteotomy and extracapsular repair in a heterogeneous population of dogs. Vet Surg. (2016) 45:261–8. doi: 10.1111/vsu.12445
Keywords: canine (dog), orthopedic disease, stifle surgery, cranial cruciate ligament rupture, Tibial Plateau Leveling Osteotomy (TPLO), Tibial Tuberosity Advancement (TTA)
Citation: Wemmers AC, Charalambous M, Harms O and Volk HA (2022) Surgical treatment of cranial cruciate ligament disease in dogs using Tibial Plateau Leveling Osteotomy or Tibial Tuberosity Advancement–A systematic review with a meta-analytic approach. Front. Vet. Sci. 9:1004637. doi: 10.3389/fvets.2022.1004637
Received: 27 July 2022; Accepted: 11 November 2022;
Published: 30 November 2022.
Edited by:
Julia Maria Matera, University of São Paulo, BrazilReviewed by:
Antoine Bernardé, CHV St. Martin, FranceCopyright © 2022 Wemmers, Charalambous, Harms and Volk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annika Christina Wemmers, YW5uaWthLndlbW1lcnNAdGloby1oYW5ub3Zlci5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.