
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 17 March 2025
Sec. Orthopedic Surgery
Volume 12 - 2025 | https://doi.org/10.3389/fsurg.2025.1531104
This article is part of the Research Topic Advances in Surgical and Basic Research in Hip Surgery: Complications, Artificial Intelligence and Surgery Robotics View all 4 articles
 Hana M. A. Fakhoury1*
Hana M. A. Fakhoury1* Mohamad Nassereddine2
Mohamad Nassereddine2 Hani Tamim1,3
Hani Tamim1,3 Ziad A. Memish1,4,5
Ziad A. Memish1,4,5 Muhammad Affan Elahi1
Muhammad Affan Elahi1 Sarah Daher1
Sarah Daher1 Ali H. Hajeer6,7
Ali H. Hajeer6,7
Introduction: This retrospective cohort study investigated the “Hajeer score” (age/BMI) as a predictor of 30-day postoperative outcomes pertaining to morbidity and mortality following total hip arthroplasty.
Methods: Using the National Surgical Quality Improvement Project database from 2011 to 2021, this study analyzed perioperative factors and 30-day postoperative complications in relation to age, BMI, and the Hajeer score. The complications evaluated included venous thromboembolism, pneumonia, acute myocardial infarction, readmission rates, and 30-day mortality. Patients were categorized based on their age, BMI, and Hajeer score and adjusted odds ratios (aORS) for morbidities and mortality were calculated by multivariate logistic regression.
Results: A total of 321,973 patients who underwent total hip arthroplasty were included in this study. Risk of mortality and various other outcomes (including cardiac, respiratory, urinary, and central nervous system diseases, thromboembolism, sepsis, blood transfusion, and composite morbidity) increased with age. Conversely, a higher BMI was linked to a lower risk of mortality, cardiac and respiratory diseases, and blood transfusion. A higher Hajeer score (>3) was strongly associated with an increased risk of mortality [adjusted odds ratio [OR]: 20.06, 95% confidence interval [CI]: 2.81–143.08, p < 0.05], cardiac diseases (adjusted OR: 8.53, 95% CI: 1.19–60.96, p < 0.0001), respiratory diseases (adjusted OR: 1.40, 95% CI: 1.40–1.41, p < 0.0001), and blood transfusion (adjusted OR: 2.12, 95% CI: 1.73–2.60, p < 0.05).
Conclusion: The Hajeer score could be a more effective predictor of short-term (30-day) postoperative outcomes than either age or BMI alone.
Total hip arthroplasty (THA), also known as total hip replacement, has become a critical intervention for patients suffering from advanced degenerative joint disease. It offers significant pain relief and improved mobility (1), leading to a higher quality of life. As the number of THA procedures is projected to rise in the coming years, optimizing patient selection and perioperative care becomes increasingly important (2).
However, current methods for predicting patient outcomes after THA have limitations. Body mass index (BMI) is a commonly used metric, but research on its association with THA outcomes paints a complex picture. Studies have shown both morbid obesity and being underweight can increase mortality risk after THA (3, 4). Additionally, Hung et al. found that advanced age, rather than BMI, was a more significant risk factor for complications (5). The U-shaped relationship between BMI and all-cause mortality, with the lowest risk in the 22.5–25 kg/m2 range (6), further highlights the limitations of BMI as a sole predictor.
To address these limitations and potentially improve patient selection for THA, we propose the Hajeer score as a novel prognostic tool. The Hajeer score is a simple ratio of age to body mass index (age/BMI). Previous studies have shown its effectiveness in predicting mortality across diverse patient populations, including patients with COVID-19 (7) and those undergoing laparoscopic cholecystectomy (8). In this study, we leverage the National Surgical Quality Improvement Program (NSQIP) database to evaluate the Hajeer score's ability to predict postoperative complications and mortality following THA. This large database allows for a comprehensive assessment of the Hajeer score's usefulness as a prognostic tool in THA patients.
In this retrospective cohort study, we used the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. This prospective, validated variable-based outcomes registry provides feedback to affiliated hospitals regarding 30-day risk-adjusted surgical mortality and morbidity. It comprises acronymized data from over 600 participating non-Veteran Affairs administration hospitals for patients undergoing major surgery. The data includes patient demographics, functional statuses, laboratory data, admission sources, preoperative risk factors, perioperative variables as well as 30-day postoperative outcomes. This data is collected upon admission by trained surgical clinical reviewers from the medical record, operative log, anesthesia record, and interviews with both the surgical attending and patients (8).
In this study, we identified 321,973 patients who underwent total hip arthroplasty between 2011 and 2021 using Current Procedural Terminology (CPT) codes 27130, 27134, 27137, and 27138 maintained by the American Medical Association.
The Institutional Review Board (IRB) of the American University of Beirut (AUB) waived the need for ethical approval and a consent form, as this retrospective cohort study used de-identified data previously collected as part of a quality assurance program.
Continuous variables such as age, BMI, and Hajeer (age/BMI) score were converted to categorical variables to facilitate an adjusted multivariable risk assessment for each variable. Patients were stratified by age into four groups, namely group 1 (<40 years), group 2 (40– <59.9 years), group 3 (60–79.9), and group 4 (≥80 years). Patient were also divided based on BMI into three groups i.e., underweight (<25 kg/m2), normal weight (25–29.9 kg/m2), and obese (>30 kg/m2). The Hajeer score was calculated by dividing age (years) by the BMI (kg/m2) which was used to categorize patients into 4 groups: group 1: ≤1.0, group 2: 1.1–2.0, group 3: 2.1–3.0, and group 4: >3.0. The stratification of the Hajeer score into those 4 distinctive groups was done in accordance with our previously published study about the use of the Hajeer score in patients undergoing laparoscopic cholecystectomy (8).
The collected demographic data included age, sex, height, weight, BMI, and race. The assessed characteristics included obesity, smoking status, diabetes, hypertension, steroid use, systemic sepsis within last 48 h prior surgery, dyspnea, congestive heart failure within 30 days prior surgery, severe chronic obstructive pulmonary disease (COPD), ascites, esophageal varices within last 6 months, renal failure, dialysis, impaired sensorium within last 48 h, hemiplegia, paraplegia, quadriplegia, coma lasting greater than 24 h, history of transient ischemic attacks, history of cerebrovascular accidents with neurologic deficits, tumors involving the CNS, bleeding disease, weight loss >10% within the last 6 months, disseminated cancer, chemotherapy within last 30 days, radiotherapy within the last 90 days, open wound (with or without infection), preoperative levels of serum sodium, blood urea nitrogen (BUN), total bilirubin, serum creatinine, SGOT, alkaline phosphatase, and counts of WBCs and platelets as well as INR. The operative characteristics included total operating time, inpatient/outpatient status and the American Society of Anesthesiologists (ASA) classification. The ASA score, ranging from I to V, assesses patient's overall health and comorbidities. ASA I is a healthy patient with no comorbidities, ASA II is mild systemic disease without functional limitations, ASA III is severe systemic disease with substantive functional limitations, ASA IV is severe systemic disease that is a constant threat to life, ASA V is a moribund patient not expected to survive without the operation, and ASA VI is a declared brain-dead patient whose organs are being removed for donor purposes.
The assessed outcomes in this study were: mortality, wound outcome, cardiac disease, respiratory disease, urinary disease, central nervous system (CNS) disease, thromboembolism, sepsis, and return to the operation room (OR).
Statistical analysis was performed using Statistical Analysis Software (SAS) version 9.4. Descriptive statistics were employed, reporting number and percentages for categorical variables and means with standard deviations for continuous variables. Assessment of associations between exposures (e.g., age, BMI, Hajeer score) and the various characteristics and outcomes were assessed using the chi-square test for categorical variables, independent samples t-test for continuous variables associated with a 2-group categorical variable, or ANOVA for continuous variables associated with a group of 3 or more categorical variables.
To mitigate the confounding effects of patient characteristics, univariate and multivariate logistic regression was used given the large sample size with statistically significant or clinically relevant variables being included in the model. Adjusted odds ratios (aORS) for morbidities and mortality were calculated by logistic regression and reported with 95% confidence intervals (CIs) with the level of significance for the p-value being set at <0.05. The odds ratios were adjusted for the following variables: congestive heart failure within 30 days prior to surgery, severe COPD, preoperative acute renal failure, bleeding disorders, cancer, ascites within 30 days before surgery, as well as preoperative treatments (e.g., dialysis, ventilation, chemotherapy, and radiation therapy), and the aforementioned ASA classification. For the multivariate analysis, missing data were replaced by the average for continuous variable, or the null value for categorical variables. It is worth nothing, that most of the variables included in the model had very little missing data (<1%).
321,973 patients who underwent total hip arthroplasty were included in this study. The baseline demographics are presented in Table 1 and stratified by the Hajeer score. As the Hajeer score increased, the surgical duration, smoking prevalence, and COPD decreased, while the prevalence of hypertension and transfusions increased across the groups.
Table 2 summarizes the results of the ordered regression analysis of the age groups with various outcomes. As age increased, a greater prevalence of cardiac disease, respiratory disease, urinary disease, and blood transfusion was noted. This was particularly striking in the age ≥80 years group with the following adjusted odds ratios: mortality (OR 3.25, CI 2.71–2.90), cardiac disease (OR 1.88, CI 1.49–2.38), respiratory disease (OR 1.55, CI 1.29–1.88), urinary disease (OR 1.29, CI 0.91–1.82), and blood transfusion (OR 1.57, CI 1.48–1.67). On the other hand, older patients were less likely to develop adverse wound outcomes when compared to younger patients.
Table 3 presents the postoperative outcomes following total hip arthroplasty categorized by BMI. While the risk of wound infection, urinary disease, return to the OR and composite morbidity significantly increased as the BMI increased, however, a decline in mortality, blood transfusion, and cardiac disease was observed as the BMI increased. The adjusted odds ratios (OR) for BMI > 30 group were as follows: mortality (OR 0.39, CI 0.34–0.45), wound outcome (OR 2.13, CI 1.79–2.53), cardiac disease (OR 0.62 CI 0.51–0.76), respiratory disease (OR 0.70, CI 0.60–0.81), urinary disease (OR 1.67, CI 1.19–2.35), CNS disease (OR 0.62, CI 0.43–0.89), blood transfusion (OR 0.51, CI 0.49–0.54), return to OR (OR 1.18, CI 1.08–1.29), and composite morbidity (OR 1.16, CI 1.07–1.27).
Table 4 outlines the results of the ordered regression analysis of Hajeer score groups with different outcomes. As the Hajeer score increased, there was a greater risk of respiratory disease, cardiac disease, and composite morbidity decreased. Conversely, a decrease in the risk of wound outcomes was associated with an increasing Hajeer score. However, the risk of composite morbidity, CNS diseases, return to OR, sepsis, thromboembolism, and urinary issues did not significantly vary across the Hajeer score groups. The adjusted odds rations for Hajeer score group 4 were as follows: mortality (OR 20.06, CI 2.81–143.08), wound outcome (OR 0.23, CI 0.15–0.36), cardiac disease (OR 8.53, CI 1.19–60.96), respiratory disease (OR 1.40, CI 1.40–1.41), and blood transfusion (OR 2.12, CI 1.73–2.60).
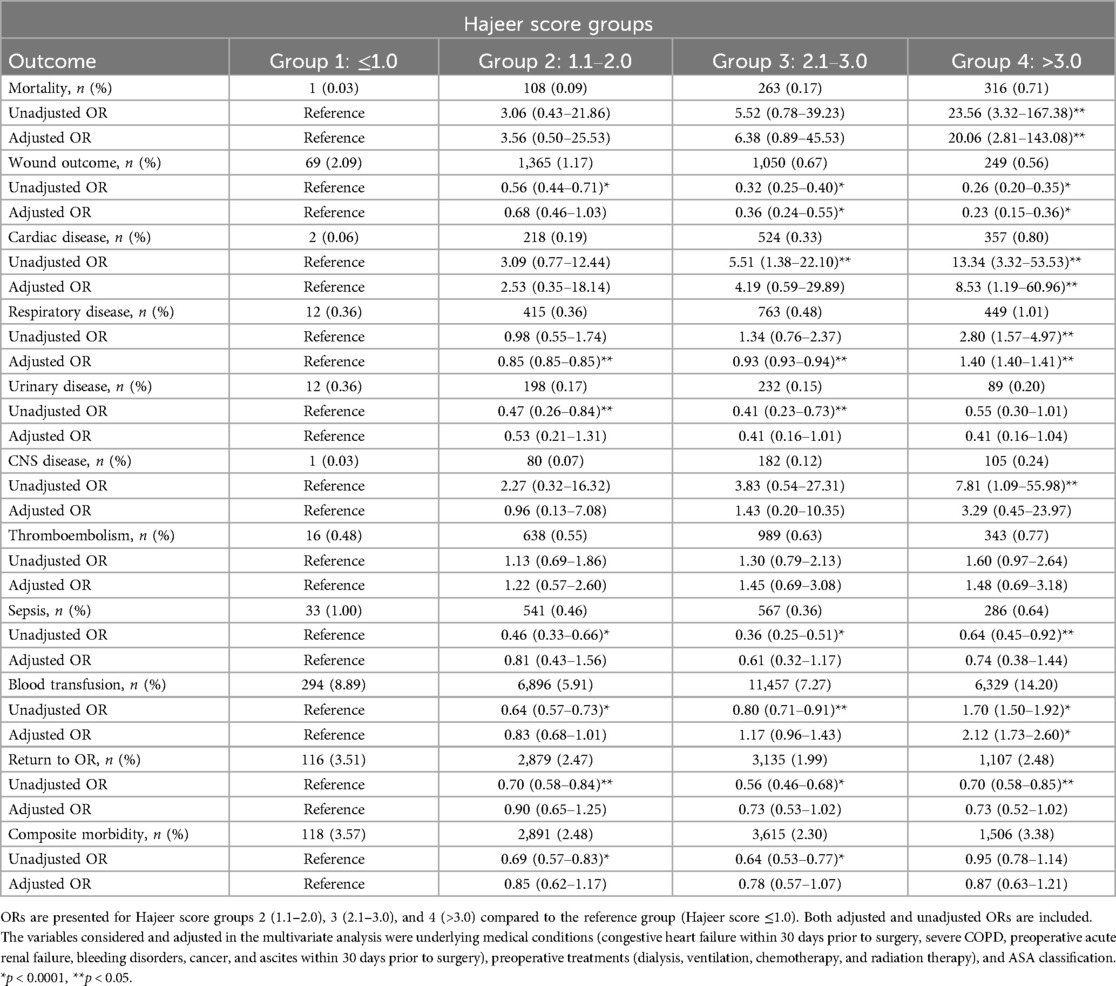
Table 4. Association between hajeer score and postoperative outcomes following total Hip arthroplasty.
Total hip arthroplasty (THA) is one of the most successful orthopedic procedures and involves resection of disease articular surfaces of the hip with subsequent replacement with prosthetic hip components. In a population-based cohort study with over 60,000 patients who underwent THA, over 90% of patients had successful results, were pain-free, and developed no complications within a 15-year postoperative period (9).
This study investigated the association between age, BMI, and the Hajeer score with postoperative outcomes following THA. Our results demonstrate that a higher Hajeer score is a strong predictor of increased risk cardiac and respiratory complications, as well as blood transfusions. These findings suggest that the Hajeer score, incorporating both age and BMI, offers a more comprehensive assessment of patient risk compared to either factor alone.
Increasing age was associated with a broader spectrum of negative outcomes, including mortality, various organ system complications, thromboembolism, sepsis, and blood transfusion. Conversely, a higher BMI was associated with a decreased risk of mortality and cardiac and respiratory complications.
Our findings align with several previously published studies demonstrating that overweight and obese patients have a higher long-term survival rate (10, 11), including after surgery (12). Conversely, those who are underweight face a higher risk of mortality (10) and developing post-operative complications (12) when compared to individuals with a higher BMI. A 2022 meta-analysis by Yang et al. reported an inverse association between body weight and postoperative mortality in older adults undergoing hip fracture surgery (13). Similarly, Woo et al. (4) found that underweight (BMI < 18.5 kg/m2) was a significant risk factor for mortality after THA in older individuals (4).
A study conducted in Australia on patients undergoing primary THA found that those who were classified as overweight or obese class II had lower odds of perioperative complications, especially cardiac complications (14). Similarly, an earlier study also using data from the ACS-NSQIP database by Scully et al. (15) analyzed the impact of BMI on 30-day complications in THA patients, albeit with a smaller sample size and shorter duration (15). Their findings revealed a nonlinear J-shaped relationship between BMI and complications such as readmission, reoperation, superficial infection, prosthetic joint infection, and sepsis, with the lowest risk observed in patients with a BMI of 27–28 kg/m2 (15). They also found that BMI was a more effective predictor when treated as a continuous variable rather than a categorical variable, indicating that the risk of mortality and blood transfusion had a reverse J-shaped relationship with BMI (15). Moreover, those studies have also highlighted the limitations of using BMI alone as a predictor, especially in older individuals, emphasizing the need for a more nuanced approach to risk assessment in this population (10–12).
To further clarify these associations, it is important to explore the underlying biological mechanisms driving these outcomes. The “obesity paradox” concept has been illustrated in multiple studies and may be applicable in this context as well. Obesity is thought to confer a paradoxical protective effect in certain populations by providing greater metabolic reserves during physiological stress, as evidenced by studies from Yang et al. (13) and Modig et al. (16). The latter study specifically examined patients with hip fractures and found that overweight and even obese patients had better one-year survival rates compared to those with a normal BMI, whereas a low BMI was associated with worse survival outcomes (16). Additionally, patients with a BMI below 22 kg/m2 had a reduced likelihood of returning home after a fracture (16).
The “obesity paradox” may also be explained by the role of chronic low-grade inflammation commonly observed in individuals with higher BMI. This baseline inflammatory state may prime the immune system to respond more efficiently to surgical stress, ultimately leading to a protective effect (8). Furthermore, lower levels of natriuretic peptides in obese individuals may provide additional protection against endotoxin- and cytokine-mediated inflammation (13), further supporting the paradoxical benefits of obesity in certain clinical scenarios.
Nonetheless, the paradoxical association between BMI and mortality highlights potential risks at both ends of the spectrum. Woo et al. (4) also reported increased short-term mortality risk for obese patients (BMI > 30 kg/m2) (4). On the other hand, underweight individuals undergoing total knee arthroplasty are at higher risk of surgical site infections and blood transfusions, possibly due to lower preoperative hemoglobin levels (17).
The association between lower body weight and poorer outcomes in older adults is likely due to several factors. Age-related muscle loss (sarcopenia) contributes to decreased functional capacity and may hinder recovery from surgery (18, 19). In individuals with already low body weight, this muscle loss can further increase mortality risk (20). Frailty, characterized by sarcopenia, is highly prevalent in older, underweight individuals and is a significant risk factor for poor surgical outcomes (10, 21, 22). Sarcopenia has been linked to delayed wound healing, increased susceptibility to infections, and prolonged recovery times (23, 24) possibly due to their low immunity as evidenced by a reduction in cellular immune function due to decreased glutamine and an increased level of proinflammatory mediators (24, 25). In addition, sarcopenic patients are at risk of postoperative pulmonary complications such as aspiration and atelectasis due in part to impaired respiratory muscle function (25). Malnutrition, often associated with low BMI, can also be an overlapping condition contributing to poorer outcomes in older individuals (11, 16, 22).
Regular physical activity, even at modest levels, can help frail older adults maintain muscle mass and mitigate the negative effects of aging and disease on body composition (26). Exercise interventions may improve tolerance to surgery and potentially reduce postoperative complications (26).
Overall, our findings are also consistent with another published study on patients undergoing laparoscopic cholecystectomy, another relatively safe surgical procedure in which an increased Hajeer score was strongly associated with an increased risk of mortality and composite morbidity (8).
Despite a large sample size (n = 321,973), the relatively low number of mortality and morbidity events within the NSQIP database limited our ability to detect some associations. Additionally, the database only provides information on 30-day outcomes. Future studies with longer follow-up periods (>30 days) are warranted to confirm these findings and explore the broader utility of the Hajeer score. Investigating the Hajeer score's effectiveness in predicting outcomes in other surgical procedures would be valuable.
In conclusion, the Hajeer score, combining age and BMI, emerged as a strong predictor of postoperative outcomes after THA, outperforming individual measures of age or BMI. This score has the potential to improve preoperative risk stratification. However, further research with longer follow-up periods and a broader range of surgical procedures is necessary to fully validate these findings and explore the Hajeer score's potential applications.
The data for this study was obtained from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Participant Use Data File.
The studies involving humans were approved by The Institutional Review Board (IRB) of the American University of Beirut (AUB). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because because it involved de-identified data previously collected as part of a quality assurance program.
HF: Conceptualization, Project administration, Supervision, Writing – original draft, Writing – review & editing. MN: Data curation, Resources, Writing – original draft, Writing – review & editing. HT: Data curation, Formal analysis, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. ZM: Writing – original draft, Writing – review & editing. ME: Writing – original draft, Writing – review & editing. SD: Writing – original draft, Writing – review & editing. AH: Conceptualization, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research and/or publication of this article.
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yan L, Ge L, Dong S, Saluja K, Li D, Reddy KS, et al. Evaluation of comparative efficacy and safety of surgical approaches for total hip arthroplasty: a systematic review and network meta-analysis. JAMA Netw Open. (2023) 6(1):e2253942. doi: 10.1001/jamanetworkopen.2022.53942
2. Shichman I, Roof M, Askew N, Nherera L, Rozell JC, Seyler TM, et al. Projections and epidemiology of primary hip and knee arthroplasty in medicare patients to 2040–2060. JB JS Open Access. (2023) 8(1). doi: 10.2106/jbjs.Oa.22.00112
3. Tohidi M, Brogly SB, Lajkosz K, Harrison MM, Campbell AR, VanDenKerkhof E, et al. Ten-year risk of complication and mortality after total hip arthroplasty in morbidly obese patients: a population study. Can J Surg. (2019) 62(6):442–9. doi: 10.1503/cjs.017318
4. Woo SH, Cha DH, Park E-C, Kim SJ. The association of under-weight and obesity with mortality after hip arthroplasty. Age Ageing. (2019) 48(1):94–100. doi: 10.1093/ageing/afy161
5. Hung CY, Chang CH, Lin YC, Lee SH, Chen SY, Hsieh PH. Predictors for unfavorable early outcomes in elective total hip arthroplasty: does extreme body mass Index matter? Biomed Res Int. (2019) 2019:4370382. doi: 10.1155/2019/4370382
6. Chen Z, Yang G, Offer A, Zhou M, Smith M, Peto R, et al. Body mass index and mortality in China: a 15-year prospective study of 220 000 men. Int J Epidemiol. (2012) 41(2):472–81. doi: 10.1093/ije/dyr208
7. Al Balwi W, Al Turki M, Memish ZA, Fakhoury HMA, Al Balwi M, Hajeer AH. Age/BMI is a stronger predictor of death in COVID-19 patients than age alone: a pilot study. J Epidemiol Glob Health. (2022) 12(4):548–51. doi: 10.1007/s44197-022-00075-z
8. Fakhoury HMA, Yousef Z, Tamim H, Daher S, Attasi AA, Al Ajlan A, et al. Combined effect of age and body mass index on postoperative mortality and morbidity in laparoscopic cholecystectomy patients. Front Surg. (2023) 10:1243915. doi: 10.3389/fsurg.2023.1243915
9. Evans JT, Evans JP, Walker RW, Blom AW, Whitehouse MR, Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. (2019) 393(10172):647–54. doi: 10.1016/s0140-6736(18)31665-9
10. Ryg J, Anru PL, Engberg H, Jorgensen MG, Masud T, Christensen K, et al. Association of body mass index with all-cause mortality in acutely hospitalized older patients. J Am Med Dir Assoc. (2022) 23(3):507–13.e1. doi: 10.1016/j.jamda.2021.07.015
11. Winter JE, MacInnis RJ, Wattanapenpaiboon N, Nowson CA. BMI And all-cause mortality in older adults: a meta-analysis. Am J Clin Nutr. (2014) 99(4):875–90. doi: 10.3945/ajcn.113.068122
12. Tjeertes EE, Hoeks SS, Beks SS, Valentijn TT, Hoofwijk AA, Stolker RJR. Obesity–a risk factor for postoperative complications in general surgery? BMC Anesthesiol. (2015) 15:1–7. doi: 10.1186/1471-2253-15-1
13. Yang TI, Chen YH, Chiang MH, Kuo YJ, Chen YP. Inverse relation of body weight with short-term and long-term mortality following hip fracture surgery: a meta-analysis. J Orthop Surg Res. (2022) 17(1):249. doi: 10.1186/s13018-022-03131-3
14. Gurunathan U, Anderson C, Berry KE, Whitehouse SL, Crawford RW. Body mass index and in-hospital postoperative complications following primary total hip arthroplasty. Hip Int. (2018) 28(6):613–21. doi: 10.1177/1120700017754058
15. Scully W, Piuzzi NS, Sodhi N, Sultan AA, George J, Khlopas A, et al. The effect of body mass index on 30-day complications after total hip arthroplasty. Hip Int. (2020) 30(2):125–34. doi: 10.1177/1120700019826482
16. Modig K, Erdefelt A, Mellner C, Cederholm T, Talbäck M, Hedström M. “Obesity paradox” holds true for patients with hip fracture: a registry-based cohort study. JBJS. (2019) 101(10):888–95. doi: 10.2106/JBJS.18.01249
17. Manrique J, Chen AF, Gomez MM, Maltenfort MG, Hozack WJ. Surgical site infection and transfusion rates are higher in underweight total knee arthroplasty patients. Arthroplasty Today. (2017) 3(1):57–60. doi: 10.1016/j.artd.2016.03.005
18. Seidell JC, Visscher TL. Body weight and weight change and their health implications for the elderly. Eur J Clin Nutr. (2000) 54(Suppl 3):S33–9. doi: 10.1038/sj.ejcn.1601023
19. Nilwik R, Snijders T, Leenders M, Groen BB, van Kranenburg J, Verdijk LB, et al. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol. (2013) 48(5):492–8. doi: 10.1016/j.exger.2013.02.012
20. Myrskylä M, Chang VW. Weight change, initial BMI, and mortality among middle- and older-aged adults. Epidemiology. (2009) 20(6):840–8. doi: 10.1097/EDE.0b013e3181b5f520
21. Guo K, Wang X, Lu X, Yang Y, Lu W, Wang S, et al. Effects of sarcopenia and frailty on postoperative recovery in elderly patients: a prospective cohort study. J Cachexia Sarcopenia Muscle. (2023) 14(6):2642–52. doi: 10.1002/jcsm.13337
22. Gingrich A, Volkert D, Kiesswetter E, Thomanek M, Bach S, Sieber CC, et al. Prevalence and overlap of sarcopenia, frailty, cachexia and malnutrition in older medical inpatients. BMC Geriatr. (2019) 19:1–10. doi: 10.1186/s12877-019-1115-1
23. Lieffers J, Bathe O, Fassbender K, Winget M, Baracos V. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. (2012) 107(6):931–6. doi: 10.1038/bjc.2012.350
24. Yang Y, Sun M, Chen W-M, Wu S-Y, Zhang J. Adverse postoperative outcomes in elderly patients with sarcopenia. BMC Geriatr. (2024) 24(1):561. doi: 10.1186/s12877-024-05066-2
25. Zhang X, Deng C, Wan Q, Zhao R, Han L, Wang X. Impact of sarcopenia on postoperative pulmonary complications after gastric cancer surgery: a retrospective cohort study. Front Surg. (2023) 9:1013665. doi: 10.3389/fsurg.2022.1013665
Keywords: Hajeer score, total hip arthroplasty, postoperative outcomes, preoperative risk stratification, short-term mortality
Citation: Fakhoury HMA, Nassereddine M, Tamim H, Memish ZA, Elahi MA, Daher S and Hajeer AH (2025) Age/BMI is a strong predictor of 30-day mortality and morbidity following total hip arthroplasty. Front. Surg. 12:1531104. doi: 10.3389/fsurg.2025.1531104
Received: 19 November 2024; Accepted: 4 March 2025;
Published: 17 March 2025.
Edited by:
Wanbo Zhu, University of Wisconsin-Madison, United StatesReviewed by:
Quan Liu, Anhui Provincial Hospital, ChinaCopyright: © 2025 Fakhoury, Nassereddine, Tamim, Memish, Elahi, Daher and Hajeer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hana M. A. Fakhoury, aGFuYS5mYWtob3VyeUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.